Abstract
Objective
The aim of the present study was to systematically review and perform a meta-analysis of prospective cohort studies exploring the association between dietary legume consumption and CVD risk, including CHD and stroke.
Design
The PubMed and EMBASE databases were searched up to December 2015. A meta-analysis of the highest v. lowest (reference) category of dietary legume consumption was performed through random-effects models.
Results
Fourteen studies conducted on eleven cohorts and accounting for a total of 367 000 individuals and 18 475 cases of CVD (7451 CHD and 6336 stroke cases) were considered for the analyses. Compared with lower legume consumption, the highest category of exposure was associated with a decreased risk of 10 % in both CVD and CHD (relative risk=0·90; 95 % CI 0·84, 0·97) with no or little evidence of heterogeneity and no publication bias. Null results were found regarding legume consumption and stroke risk. No substantial confounding factors were evident in stratified analyses.
Conclusions
Legume consumption was associated with lower risk of CVD. Legumes’ intrinsic characteristics, because they are often part of an overall healthy diet, or because they are a substitute for unhealthy sources of protein may potentially explain the current findings.
Keywords: CVD, Fibre, Legumes, Meta-analysis, Mortality
CVD represent the main causes of death globally, accounting for nearly one-third of all deaths worldwide( 1 ). Moreover, as life expectancy has improved in both developed and developing countries, the number of healthy years lost due to disability has been increasing consistently( 2 ). Within this scenario, primary prevention of CVD-related morbidity and mortality represents a major priority for public health strategies to reduce the burden of such conditions( 3 ). Lifestyle factors have been considered main targets to prevent CVD, because they are modifiable behaviours that could highly affect both the risk and the prognosis of the disease. A number of healthy dietary patterns have demonstrated beneficial effects in decreasing the burden of CVD-related risk factors and CVD incidence and mortality( 4 , 5 ). Scientific literature suggests that a diet rich in antioxidants (such as vitamins and polyphenols), fibre, n-3 fatty acids, MUFA and PUFA may decrease the risk of the aforementioned conditions( 6 , 7 ). Among the potential mechanisms of protection, the antioxidant and anti-inflammatory action of these compounds may mediate their effects( 8 , 9 ). From a nutritional point of view, legumes are a source of some of these nutrients and bioactive compounds as well as an excellent source of fibre and vegetable proteins( 10 , 11 ). Despite not being associated with decreased risk of CVD themselves, vegetable proteins may be a valuable alternative to animal proteins, which on the contrary are associated with saturated fats and possible adverse outcomes( 12 ).
Meta-analyses of studies on legume consumption and cardiovascular health demonstrated no association with stroke or diabetes( 13 , 14 ). Legumes considered as part of a Mediterranean dietary pattern have been associated with a decreased risk of CVD risk and mortality in studies evaluating Mediterranean diet as main exposure( 15 ), but a comprehensive evaluation of their independent role on such outcomes is lacking. The aim of the present study was to systematically review and perform a meta-analysis of prospective cohort studies exploring the association between dietary legume consumption and CVD risk, including CHD and stroke.
Participants and methods
Search strategy
We performed a systematic search in PubMed (http://www.ncbi.nlm.nih.gov/pubmed/) and EMBASE (http://www.embase.com/) databases of all English-language studies published up to December 2015. The search terms used for the study selection were ‘legume’, ‘Mediterranean diet’, ‘soy products’, ‘protein sources’ combined with ‘cardiovascular disease’, ‘coronary heart disease’ and ‘mortality’. Inclusion criteria were: (i) having a prospective cohort design; (ii) evaluating the association between dietary consumption of legumes and CVD; and (iii) assessing and reporting hazard ratios (HR) and the corresponding 95 % CI for the outcome considered. Reference lists of included studies were examined for any additional article not previously identified. If more than one study was conducted on the same cohort, only the most comprehensive or most updated was included in the meta-analysis. The selection process was performed independently by two authors (G.G. and J.G.).
Data extraction and study quality assessment
Data were abstracted from each identified study by using a standardized extraction form. The following information was collected: (i) author name; (ii) year of publication; (iii) country; (iv) number, sex and age of participants; (v) HR and 95 % CI for all categories of exposure; and (vi) covariates used in adjustments.
The quality of each study was assessed by applying the Newcastle–Ottawa Quality Assessment Scale( 16 ). The instrument consists of three domains indicating the study quality as follows: selection (4 points), comparability (2 points) and outcome (3 points), for a total score of 9 points (with 9 points representing the highest quality). Studies scoring 7–9 points, 3–6 points and 0–3 points were identified as of high, moderate and low quality, respectively.
Statistical analysis
HR with 95 % CI for all categories of exposure were extracted for the analysis and random-effects models were used to calculate pooled relative risks (RR) with 95 % CI for the highest v. lowest (reference) category of exposure. The risk estimate from the most fully adjusted models in the analysis of the pooled RR was used. When analyses were presented by sex, stratified results were taken into account for the pooled analysis. Since most of the studies considered a composite outcome of CVD incidence or mortality, when studies presented separate analyses for the two outcomes, a pooled RR was estimated within the same study and only secondarily it was included in the general analysis in order to compare more homogeneous outcomes. Heterogeneity was assessed by using the Q test and I 2 statistic. The level of significance for the Q test was defined as P<0·10. The I 2 statistic represented the amount of total variation that could be attributed to heterogeneity. I 2 values of ≤25 %, ≤50 %, ≤75 % and >75 % indicated no, small, moderate and significant heterogeneity, respectively. A sensitivity analysis by exclusion of one study at a time was performed to assess the stability of results and potential sources of heterogeneity. Subgroup analyses were also performed to check for potential source of heterogeneity according to geographical area, sample size, year of publication, study quality, type of exposure ascertainment method and length of follow-up. Publication bias was evaluated by a visual investigation of funnel plots for potential asymmetry. All analyses were performed with Review Manager (RevMan) software version 5.2 (The Nordic Cochrane Centre, The Cochrane Collaboration).
Results
Study characteristics
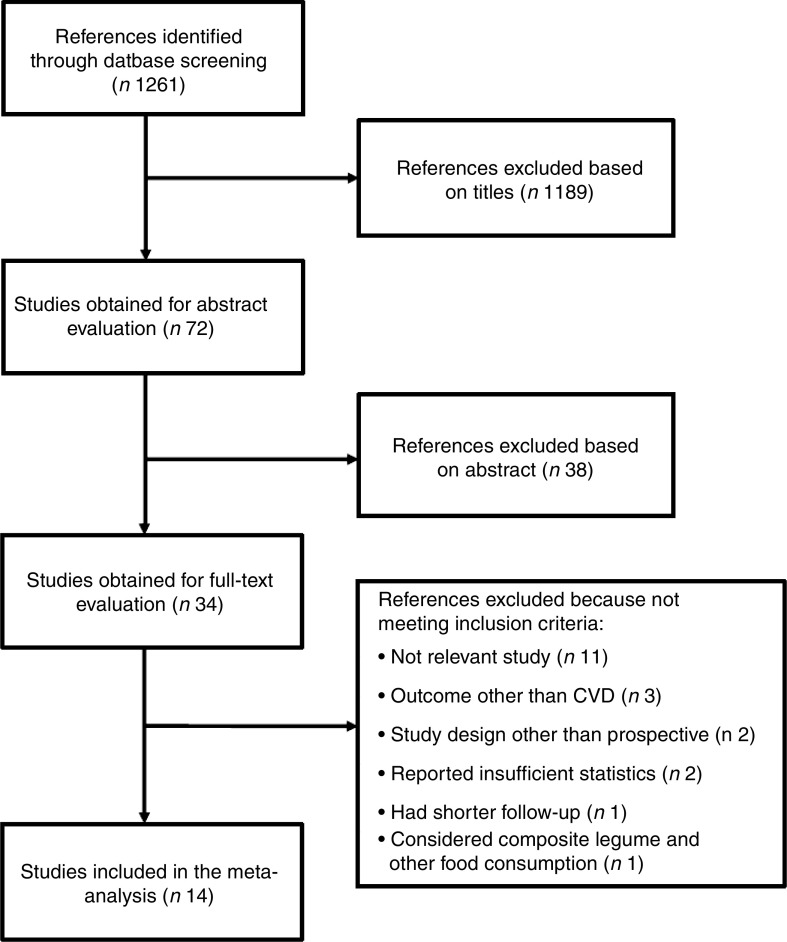
The process of study selection following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines is summarized in Fig. 1. Among the thirty-four articles obtained after screening on the basis of title and abstract, twenty studies were excluded after a full-text examination because they were not relevant for the research (n 11), did not study CVD as outcome (n 3), had a study design other than prospective (n 2), reported insufficient statistics (n 2), were conducted on the same cohort of another study but had shorter follow-up (n 1) or considered composite legume and other foods consumption (n 1). This inclusion strategy resulted in the final inclusion of fourteen studies( 17 – 30 ) and thirty-two data sets eligible to be considered for the quantitative analysis. Studies included were conducted on eleven cohorts and accounted for a total of 367 000 individuals and 18 475 cases of CVD, including 7451 CHD and 6336 stroke cases.
Fig. 1.
Flowchart indicating the selection of relevant studies for the systematic review exploring the association between dietary legume consumption and CVD risk
Table 1 shows the main characteristics extracted from all selected studies. The studies were conducted on cohorts based in the USA( 17 , 18 , 23 , 26 , 28 , 29 ), Japan( 19 , 22 ), Spain( 20 , 24 ), Greece( 25 , 27 ), Finland( 21 ) and Iran( 30 ). The results of quality assessment yielded a score of 8 or above for all studies with no substantial limitations or significant weaknesses across studies. Most of the studies included more than 10 000 individuals and follow-up periods were long enough to plausibly observe occurrence of the outcomes considered in the present review. The amount of dietary legumes considered as the highest category of exposure varied across studies in terms of measurements, but in summary could be roughly estimated as <1 serving/d or 3–4 servings/week.
Table 1.
Background characteristics of the studies included in the present meta-analysis exploring the association between dietary legume consumption and CVD risk
| Author, year, reference | Study cohort (country) | Sex | Age range (years) | No. of subjects | Outcome | Follow-up (years) | No. of cases | Adjustments | Study quality |
|---|---|---|---|---|---|---|---|---|---|
| Bazzano et al. (2001)( 17 ) | NHANES I (USA) | M and F | 25–74 | 9632 | Incident/fatal CVD | 19 | CVD: 3680 CHD: 1802 | Age, sex, race, history diabetes, PA, education, alcohol intake, current smoker, energy intake, BMI, serum TC, SBP, meat and poultry intake, fruit and vegetable intake, saturated fat intake | 9 |
| Kelemen et al. (2005)( 18 ) | IWHS (USA) | F | 55–69 | 29 017 | Fatal CHD | 15 | Fatal CHD: 739 | Age, total energy, saturated fat, polyunsaturated fat, monounsaturated fat, trans-fat, total fibre, dietary cholesterol, dietary methionine, alcohol, smoking, activity level, BMI, history of hypertension, postmenopausal hormone use, multivitamin use, vitamin E supplement use, education, family history cancer | 9 |
| Kokubo et al. (2007)( 19 ) | JPHC (Japan) | M and F | 40–59 | 40 462 | Incident/fatal MI/CBVD | 12·5 | CBVD: 587 MI: 308 | Age, sex, smoking, alcohol use, BMI, history hypertension or diabetes mellitus, medication use for hypercholesterolaemia, education level, sports, dietary intake of fruits, vegetables, fish, salt and energy, menopausal status for women | 9 |
| Buckland et al. (2009)( 20 ) | EPIC (Spain) | M and F | 29–69 | 41 078 | Incident/fatal CHD | 10·4 | Total CHD: 609 | Education, PA, BMI, smoking status, diabetes, hypertension, hyperlipidaemia status, energy intake | 8 |
| MI: 459 | |||||||||
| Fatal MI: 9 | |||||||||
| Angina pectoris: 141 | |||||||||
| Mizrahi et al. (2009)( 21 ) | Finnish Mobile Clinic Health Examination Survey (Finland) | M and F | 40–74 | 3932 | Incident/fatal CBVD | 24 | Total CBVD: 625 | Age, sex, BMI, smoking, PA, serum TC, blood pressure, energy intake | 8 |
| Nagura et al. (2009)( 22 ) | JACC (Japan) | M and F | 40–79 | 59 485 | Fatal CVD | 13 | Fatal CVD: 1207 M, 1036 F | Sex, age, BMI, smoking status, alcohol intake, hours of walking, hours of sleep, education, perceived mental stress, cholesterol intake, SFA intake, n-3 fatty acids intake, Na intake, history hypertension, history diabetes, bean and vegetable intake | 9 |
| Bernstein et al. (2010)( 23 ) | NHS (USA) | F | 30–55 | 84 136 | Incident/fatal MI | 26 | MI: 2210 Fatal CHD: 952 | Age, time period, energy, cereal fiber, alcohol, trans-fat, BMI, smoking, menopausal status, parental history MI, multivitamin use, vitamin E use, aspirin, PA | 9 |
| Martinez-Gonzalez et al. (2011)( 24 ) | SUN (Spain) | M and F | 34–43 | 13 609 | Incident CVD | 4·9 | CVD: 100 Fatal CVD: 8 | Age, sex, family history CHD, total energy intake, PA, smoking, BMI, diabetes at baseline, use of aspirin, history hypertension, history hypercholesterolaemia | 8 |
| Dilis et al. (2012)( 25 ) | EPIC (Greece) | M and F | 20–86 | 23 929 | Incident/fatal CHD | 10 | CHD: 636 Fatal CHD: 240 | Age, energy, education, height, BMI, PA, smoking status, blood pressure, intake of alcohol, fruits and nuts, vegetables, cereals, dairy products, meat and meat products, fish and seafood, potatoes, eggs, sweets, non-alcoholic beverages, olive oil, SFA, MUFA, PUFA, ratio MUFA to SFA | 9 |
| Misirli et al. (2012)( 27 ) | EPIC (Greece) | M and F | 25–67 | 23 601 | Incident/fatal CBVD | 10·6 | CBVD: 395; Fatal CBVD: 196 | Age, education, smoking status, BMI, PA, hypertension, diabetes, energy intake | 8 |
| Bernstein et al. (2012)( 26 ) | NHS (USA) | F | 30–55 | 84 010 | Incident/fatal CBVD | 26 | CBVD: 2633 | Age, time period, BMI, cigarette smoking, physical exercise, parental history early MI, menopausal status, multivitamin use, vitamin E supplement use, aspirin use at least once per week, total energy, cereal fibre, alcohol, trans-fat, fruit and vegetables, other protein sources | 9 |
| Bernstein et al. (2012)( 26 ) | HPFS (USA) | M | 40–75 | 43 150 | Incident/fatal CBVD | 22 | CBVD: 1397 | Age, time period, BMI, cigarette smoking, physical exercise, parental history early MI, multivitamin use, vitamin E supplement use, aspirin use at least once per week, total energy, cereal fibre, alcohol, trans-fat, fruit and vegetables, other protein sources | 9 |
| Haring et al. (2014)( 28 ) | ARIC (USA) | M and F | 45–64 | 12 066 | Incident/fatal CHD | 22 | CHD: 1147 | Age, sex, race, study centre, total energy intake, smoking, education, SBP, use of antihypertensive medication, HDL-C, TC, use of lipid-lowering medication, BMI, WHR, alcohol intake, PA, carbohydrate intake, fibre intake, Mg intake | 9 |
| Haring et al. (2015)( 29 ) | ARIC (USA) | M and F | 45–64 | 11 601 | Incident/fatal CBVD | 22 | CBVD: 699 | Age, sex, race, study centre, total energy intake, smoking, education, SBP, use of antihypertensive medication, HDL-C, TC, use of lipid-lowering medication, BMI, WHR, alcohol intake, PA, carbohydrate intake, fibre intake, Mg intake | 9 |
| Nouri et al. (2016)( 30 ) | Isfahan Cohort Study (Iran) | M and F | >35 | 6504 | Incident/fatal CVD | 6·8 | Total CVD: 427 | Age, sex, income, marital status, education, job, ever smoke, leisure-time PA, legume-adjusted dietary score, antihyperlipidaemia medicine, BMI, shared frailty | 8 |
| MI: 89 | |||||||||
| Stroke: 91 | |||||||||
| Sudden cardiac death: 54 | |||||||||
| Angina: 193 | |||||||||
NHANES I, First National Health and Nutrition Examination Survey; IWHS, Iowa Women’s Health Study; JPHC, Japan Public Health Center-based; EPIC, European Prospective Investigation into Cancer and Nutrition; JACCS, Japan Collaborative Cohort Study; NHS, Nurses’ Health Study; SUN, Seguimiento Universidad de Navarra; HPFS, Health Professionals’ Follow-up Study; ARIC, Atherosclerosis Risk in Communities; M, male; F, female; MI, myocardial infarction; CBVD, cerebrovascular disease; PA, physical activity; TC, total cholesterol; SBP, systolic blood pressure; HDL-C, HDL cholesterol; WHR, waist-to-hip ratio.
Legume consumption and CVD risk
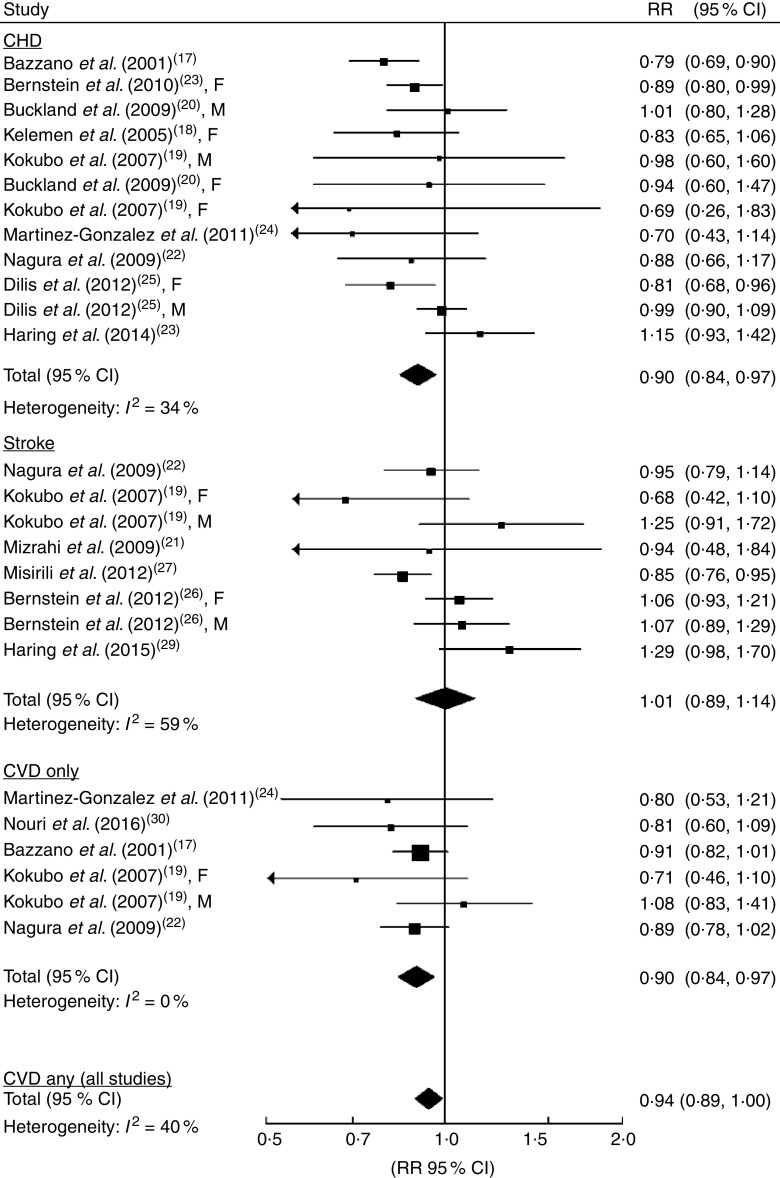
All fourteen studies including CVD, CHD and/or stroke incidence or mortality were considered for the analysis of the extreme categories of legume consumption and total CVD. RR with 95 % CI of CVD for the highest v. the lowest legume consumption category were calculated for eighteen data sets and resulted in a 6 % decreased risk of CVD (RR=0·94; 95 % CI 0·89, 1·00; Fig. 2) with little heterogeneity (I 2=40 %). Sensitivity analysis led to evidence that heterogeneity was mainly due to one cohort( 28 , 29 ) after exclusion of which heterogeneity was significantly reduced and risk estimates remained significant. No publication bias was found for this analysis (see online supplementary material, Supplementary Fig. 1(d)). Subgroup analyses were conducted to test the stability of results or potential confounding factors (Table 2). Overall, higher legume consumption had a protective effect against CVD in most subgroups. However, the association was not significant when analyses included men only, when studies were conducted in non-Mediterranean countries and after controlling for dietary variables (Table 2).
Fig. 2.
Forest plot of summary relative risk (RR) of CVD for the highest v. lowest (reference) category of legume consumption. The analysis was stratified by pooling studies exploring as outcome the risk of CHD, stroke, CVD only and any CVD (all studies). The study-specific RR and 95 % CI are represented by the black square and horizontal line, respectively; the area of the black square is proportional to the specific-study weight to the overall meta-analysis. The centre of the diamond represents the pooled RR and its width represents the pooled 95 % CI
Table 2.
Subgroup analyses of studies reporting risk of CVD for the highest v. lowest (reference) category of legume intake
| CVD (any) | Total CVD | CHD | Stroke | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subgroup | No. | RR | 95 % CI | I 2 (%) | No. | RR | 95 % CI | I 2 (%) | No. | RR | 95 % CI | I 2 (%) | No. | RR | 95 % CI | I 2 (%) |
| Total | 18 | 0·94 | 0·89, 1·00 | 40 | 6 | 0·90 | 0·84, 0·97 | 0 | 12 | 0·90 | 0·84, 0·97 | 34 | 8 | 1·01 | 0·89, 1·14 | 59 |
| Sex | ||||||||||||||||
| Men | 4 | 1·01 | 0·94, 1·09 | 0 | 1 | 1·08 | 0·83, 1·41 | – | 3 | 0·99 | 0·91, 1·08 | 0 | 2 | 1·11 | 0·95, 1·30 | 0 |
| Women | 6 | 0·90 | 0·81, 1·00 | 44 | 1 | 0·71 | 0·46, 1·10 | – | 5 | 0·86 | 0·79, 0·94 | 0 | 2 | 0·90 | 0·60, 1·37 | 67 |
| No. of participants | ||||||||||||||||
| <10 000 | 2 | 0·81 | 0·72, 0·91 | 0 | 1 | 0·81 | 0·60, 1·09 | – | 1 | 0·79 | 0·69, 0·90 | – | 1 | 0·94 | 0·48, 1·84 | – |
| >10 000 | 16 | 0·95 | 0·89, 0·70 | 45 | 5 | 0·91 | 0·84, 0·98 | 0 | 11 | 0·90 | 0·84, 0·97 | 34 | 7 | 1·01 | 0·89, 1·15 | 64 |
| Follow-up | ||||||||||||||||
| <10 years | 2 | 0·81 | 0·63, 1·03 | 0 | 2 | 0·81 | 0·63, 1·03 | 0 | 1 | 0·70 | 0·43, 1·14 | – | – | – | – | |
| >10 years | 16 | 0·95 | 0·90, 1·00 | 44 | 4 | 0·91 | 0·84, 0·98 | 0 | 11 | 0·91 | 0·84, 0·98 | 35 | 8 | 1·01 | 0·89, 1·14 | 59 |
| Geographical location | ||||||||||||||||
| Mediterranean | 6 | 0·91 | 0·83, 0·99 | 31 | 1 | 0·80 | 0·53, 1·21 | – | 5 | 0·92 | 0·83, 1·03 | 29 | 1 | 0·85 | 0·76, 0·95 | – |
| Non-Mediterranean | 12 | 0·97 | 0·90, 1·04 | 45 | 5 | 0·90 | 0·84, 0·97 | 0 | 7 | 0·89 | 0·80, 0·99 | 35 | 7 | 1·05 | 0·95, 1·17 | 22 |
| Controlled for other dietary variables | ||||||||||||||||
| Yes | 13 | 0·96 | 0·90, 1·03 | 48 | 4 | 0·91 | 0·84, 0·98 | 0 | 9 | 0·90 | 0·83, 0·98 | 46 | 6 | 1·06 | 0·95, 1·18 | 34 |
| No | 6 | 0·87 | 0·80, 0·94 | 0 | 2 | 0·81 | 0·63, 1·03 | 0 | 3 | 0·94 | 0·78, 1·14 | 0 | 2 | 0·85 | 0·76, 0·95 | 0 |
RR, relative risk.
A second analysis was conducted including only studies that specifically considered CVD as the outcome( 17 , 19 , 22 , 24 , 30 ). Overall, a decreased risk of 10 % (RR=0·90; 95 % CI 0·84, 0·97; Fig. 2) was observed, with no evidence of either heterogeneity or publication bias (see online supplementary material, Supplementary Fig. 1(c)). Stratified analyses were conditioned by the limited number of data sets (Table 2). However, no substantial differences from the primary analysis were found in studies with a larger sample, longer follow-up and adjusted for nutritional factors.
Legume consumption and CHD risk
The analysis relative to CHD risk related to consumption of legumes comprised twelve data sets derived from eight studies( 17 – 20 , 23 , 24 , 25 , 28 ). Comparison of the highest v. the lowest legume consumption category showed a similar risk estimate to the previous analysis considering CVD as outcome (RR=0·90; 95 % CI 0·84, 0·97; Fig. 2). Little heterogeneity (I 2=34 %) and no publication bias were found (see online supplementary material, Supplementary Fig. 1(a)). Exclusion of one study at the time did not change the strength of the association. Subgroup analyses demonstrated stability of results across strata considered, showing a significant decreased risk of CHD by high consumption of legumes in all subgroups with the exception of pooled analysis of studies conducted in the Mediterranean region.
Legume consumption and stroke risk
Six studies( 19 , 21 , 22 , 26 , 27 , 29 ) comprising eight data sets were considered for the analysis on the highest v. lowest level of dietary legume intake and stroke risk. The pooled analysis showed null results with no substantial risk increment or reduction for higher consumption of legumes (RR=1·01; 95 % CI 0·89, 1·14). The analysis showed moderate heterogeneity (I 2=59 %) due to divergent results reported in two studies( 19 , 29 ). The stratified analysis (Table 2) revealed that heterogeneity was attenuated by pooling studies conducted in non-Mediterranean countries, showing consistently null results, while the study conducted in Greece( 27 ) reported significant decreased risk of stroke for higher intake of legumes. Interestingly, also pooling together studies reporting adjustment for dietary variables led to decreased heterogeneity and no significant risk variation. No evidence of publication bias was found (see online supplementary material, Supplementary Fig. 1(b)).
Discussion
In the present meta-analysis we found an association between legume consumption and decreased risk of CVD incidence or mortality, despite with little heterogeneity across studies. When the analysis was stratified by type of CVD outcome, legume consumption was associated with CHD only and not with stroke risk. The analysis considering the different outcomes showed that the heterogeneity was due to the null results relative to stroke risk. Previous meta-analyses showed similar results on stroke( 13 , 14 ), but to date the current meta-analysis is the first showing a relationship between legume consumption and CHD and overall CVD outcomes.
Research on legumes and CVD-related outcomes has been growing over the last years. The majority of prospective studies included in our meta-analysis reported a significant association between legume consumption and risk of CHD. Legumes have been studied lately due to a number of potential effects that may provide health benefits towards CVD risk factors, such as lowering of blood lipids and improvement in vascular function and insulin sensitivity( 31 , 32 ). Legumes are rich in phytosterols, including soya isoflavones, which have been demonstrated to be associated with a significant reduction in serum total cholesterol, TAG and LDL cholesterol, and a significant increase in HDL cholesterol, in pooled analyses of randomized controlled trials on soya products consumption in the general population( 33 ) and patients with type 2 diabetes mellitus( 34 ). Intakes of these compounds may also protect against atherosclerosis( 35 ). Legumes, as plant-derived foods, are rich in fibre, which has been associated with decreased risk of mortality in prospective cohort studies( 36 ). Dietary fibre is supposed to ameliorate body metabolism and reduce chronic inflammation by affecting body weight, serum lipid levels, blood pressure and insulin resistance, as well as to influence fibrinolysis and coagulation that may be important in the setting of established atherosclerotic plaques( 37 ). Some legume families, such as soya, are also dietary sources of flavonoids, vitamin E and PUFA (α-linolenic acid) which have demonstrated CVD protection in pooled analyses of prospective studies, hypothesized to be exerted probably by their antioxidant effects( 38 ).
Besides the aforementioned potential direct effects of legumes on cardiovascular health, another potential mechanism of protection may depend on the fact that increased consumption of legumes lowers CVD risk simply by reducing the intake of animal sources of protein that may be high in SFA( 39 ). Moreover, legume proteins are not only a source of constructive compounds (such as amino acids) but they may also exert bioactive effects on various physiological functions( 40 ). Indeed, legume protein-derived bioactive peptides have been demonstrated to exert blood pressure-lowering effects, cholesterol-lowering ability, antithrombotic and antioxidant activities in the laboratory setting, suggesting potential benefits that need to be further investigated in the future( 40 ).
The meta-analyses of the studies providing stratified analysis by some selected variables showed that a potential difference between men and women, as well as studies conducted in Mediterranean and non-Mediterranean countries, may occur when examining the relationship between legume consumption and either CVD or CHD risk. A possible explanation for such difference between men and women may rely on the fact that men were generally more likely to be smokers and drink more alcohol( 18 , 20 , 25 ), thus somehow counteracting the potential beneficial effects of legumes. Another methodological issue may depend on lower accuracy in reporting dietary patterns among men than women. It is noteworthy that only a limited number of studies were included in our sub-analysis by sex, thus limiting the strength of such findings. However, current results were quite consistent and this hypothesis needs further attention in future studies. Regarding the geographical origin of the cohorts included in the pooled analysis, risk of CHD was significantly reduced in high legume consumers in studies conducted in non-Mediterranean countries while CVD risk was reduced in Mediterranean countries. The conflicting results may depend on a bias associated with the relative limited number of studies available for the grouping. One possible explanation for the lack of significant results in meta-analyses of studies conducted in Mediterranean countries could be the impact on cardiovascular health of all components of the diet typically consumed in these countries, or at least those included in the individual analyses. Indeed, most of these studies did not explore the effects of dietary legumes alone as the primary variable of interest towards CVD outcomes, but rather included analyses on Mediterranean diet and, secondarily, on legumes as a component of the diet. It is well known that the Mediterranean diet exerts beneficial effects against CVD( 41 ) and thus the effects of legumes, when considered as part of this diet, may be attenuated by the overwhelming effect of all the other components of this dietary pattern. Moreover, consumption of legumes in non-Mediterranean countries is generally associated with a significant lower consumption of red meat, which itself may enhance the lower risk of CHD( 23 ).
The current review has several strengths. First, all studies included in the pooled analysis were of high quality. Indeed, most of them had a large sample and a long duration of follow-up. Furthermore, all studies provided adjusted analyses for known risk factors, such as smoking, alcohol use and physical activity. Finally, results were not affected by significant heterogeneity and publication bias. Moreover, we included a number of subgroup analyses to test for potential confounders as well as a number of sensitivity analyses to test stability of results. Besides these strengths, the findings have to be considered in light of some limitations. First, the nature of studies included in the meta-analysis was observational, thus no causal relationship can be assessed. Second, despite most studies adjusting multivariate analyses by known confounding factors (smoking, alcohol drinking and physical activity), residual confounders related to dietary and lifestyle factors may still exist. Third, methods of assessment of legume consumption (such as FFQ) may be affected by recall bias. Finally, the number of data sets was sufficient to perform a meta-analysis, but the amount of studies for stratified analyses by sex was relatively low to draft definite assumptions. Moreover, due to the limited information provided in the studies regarding the amount of legumes consumed in each group of exposure, we were unable to perform a dose–response meta-analysis.
Conclusion
In conclusion, results from the current meta-analysis showed that high legume consumption is associated with lower risk of CVD. As legumes have often been reported as part of an overall healthy diet as well as a substitute for unhealthy sources of proteins, a number of bioactive natural compounds may provide the biological plausibility for such potential beneficial effects. Thus, further efforts should be made to explore the specific role of legumes in the diet.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: The authors have no conflicts of interest to disclose. Authorship: G.G. designed and performed the analysis and wrote the paper; C.S.-G. and M.I.P. performed the data set preparation; J.G. performed the study search and data set preparation; S.M. performed the analyses; M.I.P., F.G. and A.S. provided critical revision to the study. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980016002299.
click here to view supplementary material
References
- 1. Wong ND (2014) Epidemiological studies of CHD and the evolution of preventive cardiology. Nat Rev Cardiol 11, 276–289. [DOI] [PubMed] [Google Scholar]
- 2. Salomon JA, Wang H, Freeman MK et al. (2012) Healthy life expectancy for 187 countries, 1990–2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet 380, 2144–2162. [DOI] [PubMed] [Google Scholar]
- 3. Forman D & Bulwer BE (2006) Cardiovascular disease: optimal approaches to risk factor modification of diet and lifestyle. Curr Treat Options Cardiovasc Med 8, 47–57. [DOI] [PubMed] [Google Scholar]
- 4. Grosso G, Mistretta A, Frigiola A et al. (2014) Mediterranean diet and cardiovascular risk factors: a systematic review. Crit Rev Food Sci Nutr 54, 593–610. [DOI] [PubMed] [Google Scholar]
- 5. Sofi F, Macchi C, Abbate R et al. (2014) Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 17, 2769–2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grosso G, Mistretta A, Marventano S et al. (2014) Beneficial effects of the Mediterranean diet on metabolic syndrome. Curr Pharm Des 20, 5039–5044. [DOI] [PubMed] [Google Scholar]
- 7. Hirotani Y, Ozaki N, Tsuji Y et al. (2015) Effects of eicosapentaenoic acid on hepatic dyslipidemia and oxidative stress in high fat diet-induced steatosis. Int J Food Sci Nutr 66, 569–573. [DOI] [PubMed] [Google Scholar]
- 8. Bahadoran Z, Mirmiran P, Tohidi M et al. (2015) Dietary phytochemical index and the risk of insulin resistance and β-cell dysfunction: a prospective approach in Tehran lipid and glucose study. Int J Food Sci Nutr 66, 950–955. [DOI] [PubMed] [Google Scholar]
- 9. Stedile N, Canuto R, de Col CD et al. (2016) Dietary total antioxidant capacity is associated with plasmatic antioxidant capacity, nutrient intake and lipid and DNA damage in healthy women. Int J Food Sci Nutr 67, 479–488. [DOI] [PubMed] [Google Scholar]
- 10. Bouchenak M & Lamri-Senhadji M (2013) Nutritional quality of legumes, and their role in cardiometabolic risk prevention: a review. J Med Food 16, 185–198. [DOI] [PubMed] [Google Scholar]
- 11. Guine RP, Ferreira M, Correia P et al. (2016) Knowledge about dietary fibre: a fibre study framework. Int J Food Sci Nutr 67, 707–714. [DOI] [PubMed] [Google Scholar]
- 12. Berciano S & Ordovas JM (2014) Nutrition and cardiovascular health. Rev Esp Cardiol (Engl Ed) 67, 738–747. [DOI] [PubMed] [Google Scholar]
- 13. Afshin A, Micha R, Khatibzadeh S et al. (2014) Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis. Am J Clin Nutr 100, 278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shi ZQ, Tang JJ, Wu H et al. (2014) Consumption of nuts and legumes and risk of stroke: a meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 24, 1262–1271. [DOI] [PubMed] [Google Scholar]
- 15. Grosso G, Marventano S, Yang J et al. (2015) A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: are individual components equal? Crit Rev Food Sci Nutr (Epublication ahead of print version). [DOI] [PubMed]
- 16. Wells GA, Shea B, O’Connell D et al. (1999) The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa: Ottawa Health Research Institute. [Google Scholar]
- 17. Bazzano LA, He J, Ogden LG et al. (2001) Legume consumption and risk of coronary heart disease in US men and women: NHANES I Epidemiologic Follow-up Study. Arch Intern Med 161, 2573–2578. [DOI] [PubMed] [Google Scholar]
- 18. Kelemen LE, Kushi LH, Jacobs DR Jr et al. (2005) Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol 161, 239–249. [DOI] [PubMed] [Google Scholar]
- 19. Kokubo Y, Iso H, Ishihara J et al. (2007) Association of dietary intake of soy, beans, and isoflavones with risk of cerebral and myocardial infarctions in Japanese populations: the Japan Public Health Center-based (JPHC) study cohort I. Circulation 116, 2553–2562. [DOI] [PubMed] [Google Scholar]
- 20. Buckland G, Gonzalez CA, Agudo A et al. (2009) Adherence to the Mediterranean diet and risk of coronary heart disease in the Spanish EPIC cohort study. Am J Epidemiol 170, 1518–1529. [DOI] [PubMed] [Google Scholar]
- 21. Mizrahi A, Knekt P, Montonen J et al. (2009) Plant foods and the risk of cerebrovascular diseases: a potential protection of fruit consumption. Br J Nutr 102, 1075–1083. [DOI] [PubMed] [Google Scholar]
- 22. Nagura J, Iso H, Watanabe Y et al. (2009) Fruit, vegetable and bean intake and mortality from cardiovascular disease among Japanese men and women: the JACC Study. Br J Nutr 102, 285–292. [DOI] [PubMed] [Google Scholar]
- 23. Bernstein AM, Sun Q, Hu FB et al. (2010) Major dietary protein sources and risk of coronary heart disease in women. Circulation 122, 876–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martinez-Gonzalez MA, Garcia-Lopez M, Bes-Rastrollo M et al. (2011) Mediterranean diet and the incidence of cardiovascular disease: a Spanish cohort. Nutr Metab Cardiovasc Dis 21, 237–244. [DOI] [PubMed] [Google Scholar]
- 25. Dilis V, Katsoulis M, Lagiou P et al. (2012) Mediterranean diet and CHD: the Greek European Prospective Investigation into Cancer and Nutrition cohort. Br J Nutr 108, 699–709. [DOI] [PubMed] [Google Scholar]
- 26. Bernstein AM, Pan A, Rexrode KM et al. (2012) Dietary protein sources and the risk of stroke in men and women. Stroke 43, 637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Misirli G, Benetou V, Lagiou P et al. (2012) Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol 176, 1185–1192. [DOI] [PubMed] [Google Scholar]
- 28. Haring B, Gronroos N, Nettleton JA et al. (2014) Dietary protein intake and coronary heart disease in a large community based cohort: results from the Atherosclerosis Risk in Communities (ARIC) study [corrected]. PLoS One 9, e109552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haring B, Misialek JR, Rebholz CM et al. (2015) Association of dietary protein consumption with incident silent cerebral infarcts and stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Stroke 46, 3443–3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nouri F, Sarrafzadegan N, Mohammadifard N et al. (2016) Intake of legumes and the risk of cardiovascular disease: frailty modeling of a prospective cohort study in the Iranian middle-aged and older population. Eur J Clin Nutr 70, 217–221. [DOI] [PubMed] [Google Scholar]
- 31. Singhal P, Kaushik G & Mathur P (2014) Antidiabetic potential of commonly consumed legumes: a review. Crit Rev Food Sci Nutr 54, 655–672. [DOI] [PubMed] [Google Scholar]
- 32. Souza RG, Gomes AC, Naves MM et al. (2015) Nuts and legume seeds for cardiovascular risk reduction: scientific evidence and mechanisms of action. Nutr Rev 73, 335–347. [DOI] [PubMed] [Google Scholar]
- 33. Anderson JW & Bush HM (2011) Soy protein effects on serum lipoproteins: a quality assessment and meta-analysis of randomized, controlled studies. J Am Coll Nutr 30, 79–91. [DOI] [PubMed] [Google Scholar]
- 34. Yang B, Chen Y, Xu T et al. (2011) Systematic review and meta-analysis of soy products consumption in patients with type 2 diabetes mellitus. Asia Pac J Clin Nutr 20, 593–602. [PubMed] [Google Scholar]
- 35. Schonfeld G (2010) Plant sterols in atherosclerosis prevention. Am J Clin Nutr 92, 3–4. [DOI] [PubMed] [Google Scholar]
- 36. Yang Y, Zhao LG, Wu QJ et al. (2015) Association between dietary fiber and lower risk of all-cause mortality: a meta-analysis of cohort studies. Am J Epidemiol 181, 83–91. [DOI] [PubMed] [Google Scholar]
- 37. Satija A & Hu FB (2012) Cardiovascular benefits of dietary fiber. Curr Atheroscler Rep 14, 505–514. [DOI] [PubMed] [Google Scholar]
- 38. Marventano S, Kolacz P, Castellano S et al. (2015) A review of recent evidence in human studies of n-3 and n-6 PUFA intake on cardiovascular disease, cancer, and depressive disorders: does the ratio really matter? Int J Food Sci Nutr 66, 611–622. [DOI] [PubMed] [Google Scholar]
- 39. Rebello CJ, Greenway FL & Finley JW (2014) A review of the nutritional value of legumes and their effects on obesity and its related co-morbidities. Obes Rev 15, 392–407. [DOI] [PubMed] [Google Scholar]
- 40. Malaguti M, Dinelli G, Leoncini E et al. (2014) Bioactive peptides in cereals and legumes: agronomical, biochemical and clinical aspects. Int J Mol Sci 15, 21120–21135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Estruch R, Ros E, Salas-Salvado J et al. (2013) Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368, 1279–1290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980016002299.
click here to view supplementary material