Abstract
Objective
To examine the associations between serum 25-hydroxyvitamin D (25(OH)D), dietary Ca intake and presence of the metabolic syndrome (MetS).
Design
A stratified cluster sample of a population aged 18–75 years from the Victorian Health Monitor survey.
Setting
Non-institutionalized adults living in private dwellings in Victoria, Australia.
Subjects
Adults (n 3404) with complete data and without type 1 or type 2 diabetes.
Results
Adjusted for sociodemographic factors, physical characteristics and dietary covariates including Ca intake, every 10 nmol/l increase in serum 25(OH)D was significantly associated with decreased odds of MetS (adjusted odds ratio (AOR)=0·85, 95 % CI 0·80, 0·89; P<0·001). Relative to the low 25(OH)D tertile (median 33 nmol/l), there was a progressive decrease in odds of MetS that reached significance with the high 25(OH)D tertile (median 77 nmol/l; AOR=0·35, 95 % CI 0·26, 0·48; P<0·001). Every 500 mg/d increase in Ca intake adjusted for 25(OH)D did not reduce odds of MetS (AOR=0·81, 95 % CI 0·66, 1·06; P=0·141) but approached significance if unadjusted for 25(OH)D in the final model (AOR=0·81, 95 % CI 0·64, 1·02; P=0·073). No significant effect was obtained for tertiles of Ca intake. However, Ca and vitamin D tertile combinations suggested a beneficial effect of high Ca (median 1233 mg/d) only at low and medium 25(OH)D. The high 25(OH)D tertile was associated with significantly decreased odds of MetS regardless of Ca intake.
Conclusions
A high vitamin D status significantly reduced the odds of MetS. A high Ca intake may have a similar favourable outcome but only at lower circulating concentrations of 25(OH)D.
Keywords: Metabolic syndrome, Vitamin D, Calcium, 25-Hydroxyvitamin D
Vitamin D is a secosteroid that is produced cutaneously through solar UV-B irradiation of 7-dehydrocholesterol present in the skin( 1 , 2 ). The second source of vitamin D is via food intake and like for Ca, the greatest contribution to intake comes from milk and other dairy products. Vitamin D undergoes two hydroxylation steps, one in the liver and one in the kidney. The final hydroxylation step in the kidney converts 25-hydroxyvitamin D (25(OH)D) to its active metabolite, 1,25-dihydroxyvitamin D (1,25(OH)2D), and the enzyme 1-α-hydroxylase catalyses this conversion( 3 ). Interestingly, expression of the nuclear vitamin D receptor (nVDR) and 1-α-hydroxylase is present not only in the kidneys but also many other tissues of the body( 4 ), including the pancreas( 2 ) and immune cells( 5 – 8 ). Thus many tissues have the ability to locally synthesize 1,25(OH)2D from 25(OH)D and the potential to contribute to circulating concentrations( 4 ). The active metabolite can then bind to the nVDR, where it forms a heterodimer with the retinoid X receptor( 2 ). It is now recognized that nVDR regulates approximately 3 % of the human genome (~700 genes)( 2 , 5 ) and, together with its wide distribution, this provides some foundation for the study of extra-skeletal benefits of vitamin D.
The metabolic syndrome (MetS) is a clustering of risk factors that greatly increases the risk of CVD and type 2 diabetes mellitus (T2DM). Insulin resistance (IR) is a key player in the development of MetS; however, factors other than IR are also important. Clinical diagnosis of MetS is based on the presence of three or more of the following markers of chronic disease: (i) greater waist circumference; (ii) raised fasting plasma glucose; (iii) hypertension (elevated systolic blood pressure or diastolic blood pressure); and (iv) dyslipidaemia (raised TAG and low HDL cholesterol)( 9 ). The prevalence of MetS in Australia is high with ~30 % of adults classified as having the syndrome( 10 ); a figure comparable to that in other developed countries( 11 , 12 ). For a sun-drenched country with abundant milk supplies, it is surprising that both vitamin D insufficiency and low Ca intake are highly prevalent in Australia( 13 – 15 ). Inadequate vitamin D status has been implicated as a causal factor in many chronic conditions( 16 ) including T2DM( 17 ), MetS( 18 , 19 ), CVD( 20 ), hypertension( 21 , 22 ) and IR( 23 , 24 ). We have previously discussed the potential for Ca and vitamin D to regulate body weight( 25 ) and influence the risk of chronic disease( 26 – 29 ). Documented pathways include Ca’s stimulation of fat oxidation, heightened diet-induced thermogenesis, increased faecal fat excretion( 27 ), reduced circulating TAG( 30 ) and the potential for vitamin D to increase resting metabolism( 31 ). Emerging data also support a beneficial effect on IR and T2DM( 27 , 32 – 34 ). However, a consensus document produced by the Institute of Medicine found little convincing evidence available at the time in support of extra-skeletal effects of vitamin D( 35 ). The aim of the present study was to investigate whether there was a link between population-based measures of vitamin D status, dietary Ca intake and the prevalence of MetS.
Methods
To fulfil our objectives we used a state-wide representative survey of Victorian adults: the Victorian Health Monitor (VHM)( 36 ). The VHM was conducted between May 2009 and April 2010. A stratified cluster sample was selected, based on census collection districts within the eight Victorian Government Department of Health regions. Fifty randomly selected census collection districts were included in the sample, twenty-five from metropolitan and twenty-five from rural Victoria. One eligible person (aged 18–75 years) from each household in each census collection district was randomly selected to participate. The VHM was approved by the Human Research Ethics Committee (HREC) of the Baker IDI Heart and Diabetes Institute, Melbourne, Victoria( 37 ). The analysis of the VHM database was also approved by the HREC at Curtin University (HREC approval number: SPH-19-2014).
The VHM involved an initial household visit to participants to collect demographic information, followed by a participant visit to a local test site to collect risk factor information and undergo biomedical and physical examination. Participants were then asked to complete three 24 h dietary recall interviews, which were conducted over a 6-week period. The overall response rate for the VHM was 38 % and a final sample of 3653 participants was achieved.
The response rate in the VHM survey is comparable to similar Australian surveys including the Australian Health Survey: Biomedical Results 2011–12 (response rate 37·1 %)( 38 ) and the Australian Diabetes, Obseity and Lifestyle Study (response rate 37 %)( 39 ). To identify any potential selection bias in the VHM between participants and non-participants, key demographic characteristics were compared. A minimal level of difference was found between the two groups( 37 ). Demographic characteristics of participants of the VHM survey were also similar to those from the annual Victorian Population Health Surveys conducted in 2010 (n 7535) and 2011–12 (n 33 673) by the Victorian Government, which had response rates of 73 %( 40 ) and 67 %( 41 ), respectively. This would suggest that the level of bias in the VHM is probably no different from that in the larger Victorian Population Health Survey.
Test sites for the collection of biomedical and physical measures were set up specifically for the purposes of the study in census collection districts included in the sample. The procedures used for the biomedical examination were closely aligned with the protocol recommended by the WHO( 42 ). Participants provided written informed consent upon arrival at test sites and were asked to stay until all tests were complete. Abnormal test results were reviewed by a study doctor who determined whether a result warranted follow-up with a participant. Further details on the survey protocols and procedures can be found in the VHM report( 36 ) and the VHM food and nutrition report( 43 ).
Sample
In the present study, we excluded: (i) participants with missing glycosylated Hb (HbA1c) data (n 31); (ii) those with HbA1c≥6·7 % as they were classified as having T2DM according to the American Diabetes Association cut-offs (n 39)( 44 ); (iii) those with diagnosed T2DM (n 140); (iv) those with type 1 diabetes (n 9); (v) participants on diabetic medications (n 25); and (vi) those with missing metabolic components for MetS diagnosis (n 5). Hence, a total of 3404 participants were included in the analysis. Information on the use of supplements (Ca or vitamin D) was not available in this survey.
Assessment of vitamin D status
Blood samples were collected via venepuncture after an overnight fast of 10 h or more. Blood was immediately transported to an accredited central laboratory in Melbourne, Australia. The measurement of serum 25(OH)D concentration was based on the DiaSorin Corporation Liaison® 25(OH)D total assay. The assay is an automated, direct competitive chemiluminescent immunoassay that measures ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3) to provide a total value for circulating vitamin D in nmol/l. The detection limit was 10 nmol/l. The ALTM (All Laboratory Trimmed Mean) was not computed by the laboratory, nor were results compared with a TV (‘Target Value’) assigned by the NIST (National Institute of Standards and Technology) Reference Measurement Procedure.
Assessment of dietary calcium intake
Dietary intake data were obtained by multiple-pass 24 h diet recall using computer-assisted telephone interviews. The first diet recall interview was conducted within 5 to 7 d of the participants attending the biomedical examination. Two subsequent diet recall interviews were conducted at 2-week intervals following the first diet recall interview. A total of 3653 participants attended and participated in survey components at test sites. Three dietary recalls were conducted, with a total of 10 307 dietary recalls completed, where 96 % completed one dietary recall, 94 % completed two dietary recalls and 92 % completed three dietary recalls. Details of the dietary recall and post-interview processing methodology employed are described in the VHM food and nutrition report( 43 ).
All dietary recall interviews were conducted by certified dietitians from the Department of Nutrition and Dietetics, Monash University. Interviewers were trained to assure competency and consistency in collected dietary recall information. Interviewers used a food model book to aid participants with their description of portion sizes of the foods and beverages they had consumed. The food model book prompted dietary recall by including frequently forgotten foods and eating occasions, and assisted with portion size estimation with ‘to scale’ photographs of food and beverage containers, measuring spoons and cups( 43 ).
The FoodWorks® nutrition software (FoodWorks® Interview) was employed for implementation of dietary recalls. The dietary recall used a multiple-pass approach to assist participants to sufficiently recall their food and beverage intakes. The software includes a scripted guide for interviewers to help prompt participants for food recall in each interview. Interviewers were able to interrupt and prompt for further details on food items if required. Further information on the multiple-pass dietary recall process has been described in detail in the VHM food and nutrition report( 43 ).
On completion of the interviews, volume conversion factors were developed to convert food volumes into food weights. Conversions of food volumes to weights were done by ‘reference to published data, by measuring the weight and volume of specific foods, or by considering the food as very similar to another food for which a volume conversion factor was already available’( 43 ). The AUSNUT 2007( 45 ) nutrient composition data were used to calculate nutrient intakes based on estimated food intakes. The mean intake for each nutrient was computed for each participant based on information collected from three 24 h dietary recalls and was used in the analysis. This information was used to get a single measure of nutrient intake for each participant( 43 ).
Physical activity level
The following criteria were used to define each participant’s level of physical activity: (i) sufficiently physically active (≥150 min of ‘physical activity time’ per week); (ii) insufficiently physically active (1–149 min of ‘physical activity time’ per week); and (iii) physically inactive (0 min of ‘physical activity time’ per week)( 36 ). ‘Physical activity time’ was calculated as the sum of the time spent walking or performing moderate activity plus double the time spent in vigorous physical activity (to reflect its greater intensity)( 46 ).
Anthropometric measurements
Anthropometric measurement methods for weight, height and waist circumference have been previously described in the VHM report( 36 ).
Biomedical measurements
Blood collection was conducted via venepuncture after an overnight fast of 10 h or more. Blood samples were assessed for the following factors: total cholesterol, HDL cholesterol, TAG, Hba1c and fasting plasma glucose levels. Blood samples were centrifuged on site and were analysed at a separate central laboratory on a Siemens ADVIA 2400 Clinical Chemistry System. Blood components were measured as following: total cholesterol using enzymatic (oxidase/peroxidase) methods; HDL cholesterol using the elimination/catalase method; TAG using the GPO Trinder reagent set with serum blank; blood glucose using the hexokinase method; and HbA1c was measured by immunoassay (Roche Integra chemistry analyser)( 36 ).
Blood pressure measurements
Sitting blood pressure measurements (GE Dinamap 8100 Vital Signs Monitor) were performed in triplicate on each participant, after a rest period of 5 min. The average of the two closest measurements (<10 mmHg for systolic blood pressure and <6 mmHg for diastolic blood pressure) were used in the analysis. Further details have been presented in the VHM report( 36 ).
Classification of metabolic syndrome
MetS was classified according to the criteria from the joint interim statement of several major organizations( 9 ). Individuals were classified as having MetS if they had three or more of the following five components: (i) elevated TAG ≥1·7 mmol/l (≥150 mg/dl); (ii) reduced HDL-C <1·0 mmol/l (<40 mg/dl) in males and <1·3 mmol/l (<50 mg/dl) in females, or on lipid-lowering therapy; (iii) hypertension (systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥85 mmHg), or on anti-hypertensive medications; (iv) elevated fasting plasma glucose ≥5·6 to 6·9 mmol/l (≥100 to 124 mg/dl) but free of diabetes; and (v) elevated waist circumference ≥94 cm for males or ≥90 cm for Aboriginal and Torres Strait Islander, Asian and South American males and ≥80 cm for females. In the current analysis participants were categorized into having or not having MetS (yes/no).
Statistical analysis
The main outcome variable was the status of MetS (yes/no). The primary exploratory variables of interest were serum 25(OH)D concentration and Ca intake, which were both categorized into tertiles: low 25(OH)D (range 10–44 nmol/l; median 33 nmol/l), medium 25(OH)D (range 45–65 nmol/l; median 54 nmol/l) and high 25(OH)D (range 65–204 nmol/l; median 77 nmol/l); and low Ca (range 72–719 mg/d; median 579 mg/d), medium Ca (range 720–1009 mg/d; median 858 mg/d) and high Ca (range 1010–3726 mg/d; median 1233 mg/d). The association between all possible combinations of serum 25(OH)D concentration and Ca intake tertiles (thereby nine levels in total) and MetS was examined in the present study, with mutual adjustment for the other components. Serum 25(OH)D concentration was also tested as a continuous variable for every 10 nmol/l increment, while Ca intake was tested as a continuous variable for every 500 mg/d increment.
In the first stage of the analysis, demographic statistics and differences between the serum 25(OH)D concentration and Ca intake tertiles were tested by the independent-samples t test and frequency tabulation. Furthermore, to investigate the effect of the categorical predictors of interest on the risk of having MetS and higher value of its components, a χ 2 test and simple binary logistic regression analysis were then conducted to obtain the crude unadjusted odds ratios and corresponding 95 % confidence intervals.
Multiple logistic regression analysis was then carried out to calculate the adjusted odds ratios (AOR) and 95 % confidence intervals for the relationships between serum 25(OH)D concentration or Ca intake and having MetS. Analyses were conducted using the statistical software package IBM SPSS Statistics for Windows, Version 21.0. Complex samples analysis was applied to adjust for the unequal selection probability due to the multistage stratified cluster-sampling procedure used in the VHM survey. Appropriate clustering and weighting variables were used to compute appropriate standard errors and confidence intervals in the complex samples analysis procedure. A P value of less than 0·05 was accepted as statistical significance.
Confounders
In our analysis we considered and tested several risk modifiers, based on our experience( 47 ) and that of others( 18 , 48 – 50 ). Accordingly we included the following demographic factors: weight, age, gender, country of birth, income, education level, physical activity level, smoking status and season. Dietary factors included intakes of: alcohol, dietary fibre, energy, Mg, retinol, 25(OH)D concentration (Ca intake model only) and Ca intake (25(OH)D concentration model only). Age, weight, alcohol, dietary fibre, energy intake, Mg, retinol, 25(OH)D concentration and Ca intake were entered into the regression model as continuous variables. Country of birth was identified according to those born in Australia and those born overseas. Education level was categorized according to three levels: tertiary education, TAFE/diploma/certificate and high school or less. Smoking status was assessed on the basis of three categories: current smoker, ex-smoker and non-smoker. Income levels were categorized according to four categories: ≥$AU 70 000, $AU 30 001–70 000, <$AU 30 000 and don’t know/refused. Season of biomedical examination was categorized as summer, autumn, winter and spring.
Rationale of analysis
In the current analysis we examined the relationship of serum 25(OH)D concentration and Ca intake on MetS through a series of questions that resulted in different models:
-
1.
What was the unadjusted relationship between 25(OH)D and Ca intake with MetS? (crude model).
-
2.
What was the confounding influence of sociodemographic factors on the relationship of 25(OH)D/Ca intake with MetS? (model 1).
-
3.
What was the potential influence of dietary factors on the relationship of 25(OH)D/Ca intake with MetS? (model 2).
Results
The present study population consisted of a total of 3404 adults with a mean age of 49 years. The overall prevalence of MetS was 21·6 %, with a larger proportion of males (22 %) having MetS than females (14 %; P<0·001). The mean serum 25(OH)D concentration of those with MetS was 49·6 nmol/l, significantly lower than that of participants without MetS which was 57·5 mmol/l (P<0·001). The mean dietary Ca intake was 849 mg/d in those with MetS and 926 mg/d in those without MetS (P<0·001; Table 1).
Table 1.
Demographic and clinical characteristics by the presence/absence of metabolic syndrome (MetS) among non-diabetic adults (n 3404) aged 18–75 years from the Victorian Health Monitor survey, May 2009–April 2010
| Absence of MetS (n 2669) | Presence of MetS (n 735) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | % | Mean | se | n | % | Mean | se | P value |
| Age (years) | 41 | 0·9 | 52 | 1·0 | <0·001 | ||||
| Weight (kg) | 75·7 | 0·5 | 91·6 | 0·8 | <0·001 | ||||
| Gender | <0·001 | ||||||||
| Male | 1237 | 78 | 2·0 | 344 | 22 | 2·0 | |||
| Female | 1565 | 86 | 1·1 | 257 | 14 | 1·1 | |||
| Country of birth | 0·541 | ||||||||
| Born in Australia | 2139 | 82 | 1·4 | 454 | 18 | 1·4 | |||
| Born overseas | 658 | 81 | 2·0 | 153 | 19 | 2·0 | |||
| Education level | <0·001 | ||||||||
| Tertiary education | 1136 | 87 | 1·5 | 170 | 13 | 1·5 | |||
| TAFE/diploma/certificate | 580 | 80 | 2·3 | 140 | 20 | 2·3 | |||
| High school or less | 1075 | 78 | 1·7 | 303 | 22 | 1·7 | |||
| Income | 0·098 | ||||||||
| ≥$AU 70 001 | 1341 | 84 | 1·4 | 250 | 16 | 1·4 | |||
| $AU 30 001–70 000 | 837 | 79 | 2·1 | 220 | 21 | 2·1 | |||
| <$AU 30 000 | 456 | 81 | 2·6 | 110 | 19 | 2·6 | |||
| Don’t know/refused | 157 | 82 | 3·8 | 33 | 18 | 3·8 | |||
| Physical activity level | 0·011 | ||||||||
| Sufficient physical activity (≥150 min/week) | 1929 | 83 | 1·5 | 384 | 17 | 1·5 | |||
| Insufficient physical activity (<149 min/week) | 704 | 81 | 1·9 | 168 | 19 | 1·9 | |||
| Inactive (0 min/week) | 153 | 71 | 4·8 | 62 | 29 | ||||
| Smoking status | <0·001 | ||||||||
| Current smoker | 423 | 80 | 2·5 | 109 | 20 | 2·5 | |||
| Ex-smoker | 694 | 75 | 2·1 | 224 | 25 | 2·1 | |||
| Non-smoker | 1669 | 85 | 1·4 | 283 | 15 | 1·4 | |||
| Season of biomedical examination | 0·182 | ||||||||
| Summer | 155 | 75 | 5·2 | 52 | 25 | 5·2 | |||
| Autumn | 677 | 84 | 2·0 | 131 | 16 | 2·0 | |||
| Winter | 964 | 84 | 1·8 | 182 | 16 | 1·8 | |||
| Spring | 991 | 80 | 2·8 | 252 | 20 | 2·8 | |||
| Vitamin D status | |||||||||
| Serum 25(OH)D (nmol/l) | 57·5 | 2·1 | 49·6 | 2·1 | <0·001 | ||||
| 25(OH)D tertile | <0·001 | ||||||||
| Low 25(OH)D (33 nmol/l)† | 857 | 77 | 2·1 | 252 | 23 | 2·1 | |||
| Medium 25(OH)D (54 nmol/l)† | 925 | 80 | 2·3 | 237 | 21 | 2·3 | |||
| High 25(OH)D (77 nmol/l)† | 1013 | 89 | 1·3 | 120 | 11 | 1·3 | |||
| Dietary variables | |||||||||
| Dietary Ca intake (mg/d) | 926·0 | 11·4 | 849·0 | 20·0 | <0·001 | ||||
| Ca tertile | 0·001 | ||||||||
| Low Ca intake (579 mg/d)† | 847 | 77 | 1·8 | 245 | 23 | 1·8 | |||
| Medium Ca intake (858 mg/d)† | 908 | 83 | 1·4 | 187 | 17 | 1·4 | |||
| High Ca intake (1233 mg/d)† | 924 | 85 | 1·5 | 163 | 15 | 1·5 | |||
| Total energy intake (kJ/d) | 9768 | 134 | 9442 | 163 | 0·021 | ||||
| Alcohol (g/d) | 12·3 | 0·7 | 15·3 | 0·9 | <0·001 | ||||
| Dietary fibre (g/d) | 26·5 | 0·4 | 25·3 | 0·5 | 0·006 | ||||
| Mg (mg/d) | 418·9 | 6·6 | 397·2 | 7·6 | 0·008 | ||||
| Retinol (µg/d) | 433·8 | 23·2 | 454·5 | 56·1 | 0·428 | ||||
| Metabolic components | |||||||||
| Waist circumference (cm) | 86·4 | 0·7 | 102·5 | 0·7 | <0·001 | ||||
| Fasting plasma glucose (mmol/l) | 4·9 | 0·02 | 5·5 | 0·04 | <0·001 | ||||
| HDL cholesterol (mmol/l) | 1·5 | 0·02 | 1·2 | 0·02 | <0·001 | ||||
| TAG (mmol/l) | 1·1 | 0·02 | 2·1 | 0·06 | <0·001 | ||||
| Systolic blood pressure (mmHg) | 122 | 0·7 | 136 | 0·9 | <0·001 | ||||
| Diastolic blood pressure (mmHg) | 71 | 0·5 | 81 | 0·4 | <0·001 | ||||
Data are presented as mean estimate (weighted) % for categorical variables, and mean estimate (weighted) and se for continuous variables. Differences in the continuous and categorical variables between groups were assessed by the independent-samples t test and the χ 2 test, respectively.
Median of the tertile group.
Association between tertiles of serum 25-hydroxyvitamin D concentration, calcium intake and presence of metabolic syndrome
Every 10 nmol/l increment in serum 25(OH)D concentration reduced the likelihood of having MetS by 15 % (model 2; Table 2). The crude model indicated that those in the highest tertile of serum 25(OH)D concentration had a 60 % lower odds of having MetS. After adjusting for sociodemographic variables (model 1), the significant inverse association between serum 25(OH)D concentration and presence of MetS remained. After adjustment for dietary variables (alcohol, dietary fibre, energy, Mg, Ca and retinol), participants in the highest 25(OH)D tertile had a 65 % lower odds of having MetS compared with those in the lowest 25(OH)D tertile (model 2; Table 2).
Table 2.
Odds ratio of having metabolic syndrome by tertiles of serum 25-hydroxyvitamin D (25(OH)D) concentration among non-diabetic adults (n 3404) aged 18–75 years from the Victorian Health Monitor survey, May 2009–April 2010
| Crude model | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| COR | 95 % CI | AOR | 95 % CI | AOR | 95 % CI | |
| 25(OH)D, continuous (10 nmol/l) | 0·87 | 0·82, 0·92 | 0·82 | 0·78, 0·85 | 0·85 | 0·80, 0·89 |
| P value | <0·001 | <0·001 | <0·001 | |||
| 25(OH)D tertile | ||||||
| Low 25(OH)D (33 nmol/l)† | Ref. | Ref. | Ref. | |||
| Medium 25(OH)D (54 nmol/l)† | 0·87 | 0·66, 1·14 | 0·69* | 0·52, 0·90 | 0·77 | 0·58, 1·04 |
| High 25(OH)D (77 nmol/l)† | 0·40* | 0·29, 0·56 | 0·29* | 0·22, 0·38 | 0·35* | 0·26, 0·48 |
| P value for trend | <0·001 | <0·001 | <0·001 | |||
COR, crude odds ratio; AOR, adjusted odds ratio; Ref., lowest 25(OH)D tertile served as the reference group.
Model 1: adjusted for age, gender, country of birth, income, education, smoking and season.
Model 2: adjusted for model 1 covariates plus energy intake, physical activity level, body weight, alcohol, dietary fibre, Mg, Ca and retinol.
Significant in comparison to the reference group at 5 % significance level.
Median of the tertile group.
Table 3 shows that every 500 mg/d increment in dietary Ca intake reduced the likelihood of having MetS by 25 % after adjusting for sociodemographic variables in model 1, but the reduction became non-significant after adding dietary variables (alcohol, dietary fibre, energy, Mg and serum 25(OH)D concentration) in model 2. If we did not control for serum 25(OH)D in the latter model, the AOR approached significance (AOR=0·81, 95 % CI 0·64, 1·02; P=0·073) but was non-significant on controlling for 25(OH)D (Table 3, model 2; P=0·141). Those in the highest tertile of dietary Ca intake had significantly reduced odds of having MetS by 39 % in the crude model and 37 % in model 1 in comparison with those in the lowest tertile of dietary Ca intake; however, the comparison was not significant when dietary factors were added to model 2 (Table 3). Based on previous evidence we tested for potential interactions between serum 25(OH)D concentration, Ca intake and age, gender, smoking status, physical activity, county of birth and education level; however, no significant interactive effects were found( 13 ). Furthermore, interactions between serum 25(OH)D concentration, Ca and dietary variables (alcohol, dietary fibre, energy, Mg and retinol) were tested but none were significant.
Table 3.
Odds ratio of having metabolic syndrome by tertiles of dietary calcium intake among non-diabetic adults (n 3404) aged 18–75 years from the Victorian Health Monitor survey, May 2009–April 2010
| Crude OR | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| COR | 95 % CI | AOR | 95 % CI | AOR | 95 % CI | |
| Ca intake, continuous (500 mg/d) | 0·74 | 0·62, 0·89 | 0·75 | 0·61, 0·91 | 0·81 | 0·66, 1·06 |
| P value | 0·002 | 0·004 | 0·141 | |||
| Ca tertile | ||||||
| Low Ca (579 mg/d)† | Ref. | Ref. | Ref. | |||
| Medium Ca (858 mg/d)† | 0·71* | 0·56, 0·90 | 0·73* | 0·56, 0·96 | 0·92 | 0·63, 1·33 |
| High Ca (1233 mg/d)† | 0·61* | 0·46, 0·81 | 0·63* | 0·46, 0·86 | 0·83 | 0·56, 1·21 |
| P value for trend | 0·002 | 0·012 | 0·613 | |||
COR, crude odds ratio; AOR, adjusted odds ratio; Ref., lowest Ca tertile served as the reference group.
Model 1: adjusted for age, gender, country of birth, income, education, smoking and season.
Model 2: adjusted for model 1 covariates plus energy intake, physical activity level, body weight, alcohol, dietary fibre, Mg and 25-hydroxyvitamin D concentration.
Significant in comparison to reference group at 5 % significance level.
Median of the tertile group.
Association between combined effects of serum 25-hydroxyvitamin D concentration and calcium intake and presence of metabolic syndrome
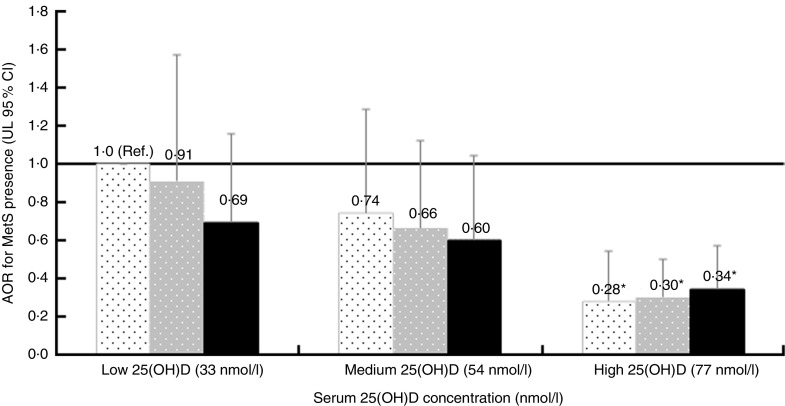
In view of finding no significant interaction between serum 25(OH)D status and Ca intake (P=0·651), the regression analysis was extended to examine the effect of combining serum 25(OH)D concentration and Ca intake tertiles on MetS (Fig. 1). The combination of low serum 25(OH)D tertile (median 33 nmol/l) and low Ca intake tertile (median 579 mg/d) was the reference group. After controlling for confounding factors, the combination of high serum 25(OH)D and low, medium or high Ca intake significantly reduced the odds of having MetS by 72, 70 and 66 %, respectively (Fig. 1).
Fig. 1.
Combined effects of serum 25-hydroxyvitamin D (25(OH)D) concentration (median of the tertile group given in parentheses) and dietary calcium intake ( , low calcium, median 579 mg/d;
, low calcium, median 579 mg/d;  , medium calcium, median 858 mg/d;
, medium calcium, median 858 mg/d;  , high calcium, median 1233 mg/d) on the presence of metabolic syndrome (MetS) among non-diabetic adults (n 3404) aged 18–75 years from the Victorian Health Monitor survey, May 2009–April 2010. Adjusted odds ratios (AOR), with the upper limit (UL) of the 95 % confidence interval represented by vertical bars, adjusted for age, gender, country of birth, income, education, smoking, season, physical activity level, weight, alcohol, dietary fibre, magnesium, retinol and energy intake. ‘Ref.’ indicates that the lowest 25(OH)D and lowest calcium tertile served as the reference group; *significant in comparison to reference group at 5 % significance level
, high calcium, median 1233 mg/d) on the presence of metabolic syndrome (MetS) among non-diabetic adults (n 3404) aged 18–75 years from the Victorian Health Monitor survey, May 2009–April 2010. Adjusted odds ratios (AOR), with the upper limit (UL) of the 95 % confidence interval represented by vertical bars, adjusted for age, gender, country of birth, income, education, smoking, season, physical activity level, weight, alcohol, dietary fibre, magnesium, retinol and energy intake. ‘Ref.’ indicates that the lowest 25(OH)D and lowest calcium tertile served as the reference group; *significant in comparison to reference group at 5 % significance level
Discussion
We investigated the individual and combined association of serum 25(OH)D concentration with dietary Ca intake on MetS. In addition to many confounders, we controlled for Ca intake in the 25(OH)D model and for 25(OH)D concentration in the Ca model, to investigate their effect, independent of each other. The results of this representative sample of adults from an Australian state have indicated that higher serum 25(OH)D concentration per se was associated with significantly reduced odds of MetS (Table 2). However, this was not statistically significant for every model of Ca intake tested (Table 3). As a continuous variable the overall pattern for Ca was in the same direction as 25(OH)D and with a lower AOR (Table 3). If we did not control for 25(OH)D in the Ca intake continuous model, the AOR approached significance (AOR=0·81, 95 % CI 0·64, 1·02; P=0·073) but on controlling for 25(OH)D (Table 3, model 2; P=0·141), this was non-significant. Such outcomes suggest that prevailing serum 25(OH)D concentrations could modulate the potential effect of Ca on MetS.
Our findings are consistent with other cross-sectional and prospective studies where an inverse association between 25(OH)D concentration, Ca intake and MetS was observed( 18 , 19 , 48 , 51 – 53 ). One cross-sectional study found a 67 % reduction in the odds of having MetS among those in the highest 25(OH)D tertile (68–231 nmol/l) v. the lowest tertile (9–45 nmol/l)( 48 ). Our study obtained relatively similar results where the highest tertile of 25(OH)D was found to contribute a 65 % reduced odds for MetS in comparison to the lowest tertile (Table 2). The study by Hypponen et al.( 48 ) had double the sample size but adjusted only for gender, month and hour of blood measurement. In comparison we controlled for additional sociodemographic, anthropometric and dietary covariates. A more recent prospective study in the elderly also found an inverse association between MetS and high 25(OH)D (≥75 nmol/l), although the magnitude of their findings was much lower( 53 ). Furthermore, a large prospective study reflected our results and found a 36 % reduction in odds of having MetS in the highest Ca intake group (1005–2596 mg/d) in comparison to the lowest Ca group. Overall, despite differences between such studies in sample sizes, study design (cross-sectional v. prospective), age of subjects and confounders used, the protective effect of vitamin D in reducing the odds of having MetS appears consistent.
We also examined the potential additive effects of tertile combinations of serum 25(OH)D concentration and Ca intake on MetS (Fig. 1). The outcomes were interesting since they suggested that at low and medium tertiles of 25(OH)D, there was a trend for increasing Ca intake to reduce AOR of MetS (Fig. 1). However, in the highest 25(OH)D tertile this trend disappeared, with significantly reduced AOR across the range from low to high Ca intakes. This was suggestive of a plateau effect, raising the possibility of a threshold to the interplay between Ca and 25(OH)D on functional outcomes.
It is now well known that increasing Ca intake increases passive Ca absorption from the gastrointestinal tract( 54 ). A higher Ca intake also increases the half-life of 25(OH)D in circulation( 55 ) and together these actions may explain the effect of high Ca in the lowest 25(OH)D tertile (Fig. 1). However, a key physiological function of 25(OH)D is the maintenance of Ca homeostasis via active intestinal Ca absorption( 54 , 56 , 57 ). So an improvement in vitamin D status from the low to medium tertile (Fig. 1) would further increase active Ca absorption and possibly allow for a greater effect of Ca on MetS. In support of such a paradigm was the observation that the overall effect of Ca in the medium 25(OH)D tertile was stronger than in the low 25(OH)D tertile (Fig. 1). While 25(OH)D and Ca absorption have a positive relationship, there is a plateau to this effect. Above ~80 nmol/l, active Ca absorption does not respond to further increases in 25(OH)D( 54 ). It is notable that the latter concentration falls within the highest tertile of 25(OH)D in the present study and may explain why increasing Ca intake ceases to have any added benefit in the highest tertile (Fig. 1).
There is another related and important facet to these relationships. A raised parathyroid hormone concentration is associated with an increased risk of MetS( 29 , 58 , 59 ). Increases in dietary Ca and in serum 25(OH)D would lower circulating parathyroid hormone. Recent data have described the exponential decline in parathyroid hormone with increases in 25(OH)D( 60 ). The analysis indicated two inflection points in the relationship, with the second plateau at 25(OH)D concentrations above ~70 nmol/l where parathyroid hormone was maximally suppressed( 60 ). We acknowledge that this threshold value of 25(OH)D is not universally accepted( 61 ) and that further work is necessary. However, it serves the argument that, at the highest tertile of 25(OH)D in the present study, the negative effects of a raised parathyroid hormone level on MetS could be significantly diminished relative to the previous tertiles. Overall, our results argue that Ca intake has an added effect with 25(OH)D on reducing MetS, but this applies only up to the medium tertile of 25(OH)D (Fig. 1). Above the latter the observed effects are due mainly to 25(OH)D per se. There is some evidence in the literature in support of threshold effects, especially for outcomes that impinge on MetS. A randomized controlled trial has demonstrated that following vitamin D supplementation, significant increases in insulin sensitivity (HOMA%S) were observed only in those who achieved a 25(OH)D concentration of 80 nmol/l and had maintained that value for 6 months( 24 ). In a weight-loss randomized controlled trial, participants who achieved 80 nmol/l at 12 months demonstrated significantly greater losses in weight, percentage fat mass and waist circumference, compared with those who did not( 62 ). We cannot predict the threshold value of 25(OH)D from our study. Moreover, as the outcomes of these randomized controlled trials were derived from post hoc analyses, they only support the hypothesis rather than validate an 80 nmol/l cut-off.
Potential mechanisms
There are many mechanistic pathways to support our observations of a protective effect of 25(OH)D concentrations on MetS. An animal study suggests an independent effect of 25(OH)D on β cells, with improvements in impaired glucose tolerance and insulin secretion, despite prevailing plasma Ca concentrations( 63 ). 1,25(OH)2D has a role in insulin secretion( 64 ), where it stimulates the expression of the insulin receptor and increases the responsiveness to glucose transport. During vitamin D deficiency β-cell function is inhibited, leading to a decrease in insulin secretion( 65 ). In addition, inadequate 25(OH)D concentration is associated with IR( 66 – 68 ). While we acknowledge that IR does not always explain all of MetS( 69 – 71 ), it is a key feature in the pathophysiology of the syndrome( 72 ). The nVDR and 1-α-hydroxylase enzyme are found in tissues not related Ca metabolism, such as in cardiac myocytes, endothelial and smooth vascular muscle cells( 70 ); potentially underscoring a role of 25(OH)D in cardiovascular health. The renin–angiotensin system is important in the regulation of blood pressure( 73 ) and low 25(OH)D concentration may dysregulate control of the renin–angiotensin system( 71 ). In this context lower 25(OH)D concentration has been found to be inversely correlated with measures of arterial stiffness and also to increased arterial resistance, hypertension and endothelial dysfunction( 74 – 77 ). Moreover higher vitamin D status could also reduce islet β-cell damage by reducing islet renin–angiotensin system activity, thereby reducing the risk of hyperglycaemia( 78 ).
The beneficial effect of Ca on features of MetS may arise from both its absorbed fraction and its unabsorbed fraction in the gastrointestinal tract( 27 ). There is now increasing evidence that Ca intake may influence fat balance and hence energy balance. Dietary Ca increases whole-body fat oxidation and this could, potentially, reduce circulating fatty acids/lipids( 27 , 79 ). Unabsorbed Ca is not without metabolic effects( 27 ). A meta-analysis indicates that for dairy Ca intake of ~1200 mg/d, an increase of ~5 g/d in faecal fat can be expected( 80 ). This arises from the interaction of non-absorbed Ca and dietary fat in the gastrointestinal lumen, leading to Ca–fatty acid soap formation and hence its eventual excretion. These outcomes may contribute to lower circulating TAG and other lipid fractions seen with Ca supplementation( 30 ). Finally, as with other chronic non-communicable conditions, MetS is a low-grade chronic inflammatory state. We, and others, are of the opinion that adequate vitamin D has a significant role in ameliorating the inflammatory state in chronic disease( 8 , 81 , 82 ).
Study limitations
The cross-sectional design has permitted only an examination of associations between Ca intake, vitamin D status and MetS. Although we have controlled for recognized confounders, we cannot establish which came first, lower 25(OH)D concentration and Ca intake or having MetS. An increased requirement for these nutrients in chronic conditions like MetS is a possibility and may account for a reverse causation. Unlike some European countries, there is no mandatory fortification of the Australian food supply for these nutrients. Unfortunately the VHM survey did not include information on Ca and vitamin D supplement usage. Such information would have potentially allowed us to tease out the effect of food-derived Ca and sunlight-derived vitamin D status (since vitamin D in Australian foods is low) v. pharmacological intake. However, we approached the potential confounding effect of supplement Ca intake by using random generated surrogate data for different age groups, based on the Ca supplement intake percentages collected in the Australian Health Survey 2011–12( 83 ). We found that the change between crude and adjusted effect estimates was much less than 10 %; a cut-off criterion for being a sizeable confounder in epidemiology research( 84 ). Hence, we do not anticipate significant confounding by supplement-derived Ca intake on the association between dietary Ca intake and the risk of MetS in the current study.
Serum 25(OH)D can be affected by genetic variation of the major transporter, the vitamin D-binding protein( 85 – 87 ). This is seen as variations in vitamin D-binding protein concentration( 86 , 88 ) as well as some vitamin D-binding protein phenotypes potentially having stronger binding abilities than others( 89 ). Serum 25(OH)D can also differ due to genetic variation in its key activation enzyme, CYP27B1( 90 ), that converts 25(OH)D to the active form. Such genetic variant information was not collected in the VHM survey so is a potential confounding factor. Future studies in this area could include this information to provide a more complete picture.
A small proportion of our sample was from South Asia (1·6 %, n 56), an ethnic group associated with high rates of betel nut chewing. Chewing betel nut could increase the risk of developing T2DM( 91 ) and animal studies have indicated that betel nut ingestion in male parents may contribute to inheritable glucose intolerance in their offspring( 92 ). Such data are not available for Australia and were not collected as part of the VHM survey. However, exclusion of these cases (n 56) did not change the direction or magnitude of our results. We therefore anticipate minimal confounding from such a potential habit in our South Asian participants.
Study strengths
We have used a large, representative, population-based sample of one Australian state that covered an age range 18–75 years. The dietary data were collected through a multiple-pass 24 h dietary recall which is the current standard and all blood analysis was conducted centrally by one laboratory based on standard methodology. Our analysis has considered and adjusted for many sociodemographic and nutrient confounders, with further adjustment for energy intake. We acknowledge that this field of research would benefit from the confirmation of a causal role for Ca and vitamin D in MetS. While randomized controlled trials provide Level 1 evidence, they are not necessarily the mainstay of the evidence base for public health nutrition and in deciding nutrition priorities for better health( 93 , 94 ).
Conclusions
The present study demonstrates that high serum 25(OH)D concentration was associated with significant reductions in the odds of MetS. We raise the possibility that the benefit of Ca is restricted to low and medium serum 25(OH)D concentrations, and this may represent a threshold to the interplay between Ca and 25(OH)D on functional outcomes. Overall, these population-based results contribute to the evidence in favour of a role for vitamin D and Ca in modulation of MetS risk.
Acknowledgements
Acknowledgements: M.J.S. acknowledges the School of Public Health, Curtin University for research infrastructure and support, and the Victorian Department of Health and Human Services for use of the VHM survey data set. The authors thank the reviewers and the editorial board for their constructive comments. The opinions and analysis in this manuscript are those of the authors and not those of: the Department of Health and Human Services, Victoria; the Victorian Government; the Secretary to the Department of Health Victoria or the Victorian Minister for Health. Financial support: P.K.P. is the recipient of an Australian Postgraduate Award. Conflict of interest: None. Authorship: P.K.P. analysed data and wrote the first draft. M.J.S. generated the idea, planned the analysis and co-wrote the manuscript. Y.Z. cross-checked the analysis and co-wrote the manuscript. L.S.P. and A.Z. critically reviewed all aspects of the manuscript. Ethics of human subject participation: The VHM was approved by the Human Research Ethics Committee (HREC) of the Baker IDI Heart and Diabetes Institute, Melbourne, Victoria. The analysis of the VHM database was also approved by the HREC at Curtin University (HREC approval number: SPH-19-2014).
References
- 1. Liu J (2012) Vitamin D content of food and its contribution to vitamin D status: a brief overview and Australian focus. Photochem Photobiol Sci 11, 1802–1807. [DOI] [PubMed] [Google Scholar]
- 2. Pilz S, Kienreich K, Rutters F et al. (2013) Role of vitamin D in the development of insulin resistance and type 2 diabetes. Curr Diab Rep 13, 261–270. [DOI] [PubMed] [Google Scholar]
- 3. Wamberg L, Christiansen T, Paulsen SK et al. (2013) Expression of vitamin D-metabolizing enzymes in human adipose tissue – the effect of obesity and diet-induced weight loss. Int J Obes (Lond) 37, 651–657. [DOI] [PubMed] [Google Scholar]
- 4. Dusso AS, Brown AJ & Slatopolsky E (2005) Vitamin D. Am J Physiol Renal Physiol 289, F8–F28. [DOI] [PubMed] [Google Scholar]
- 5. Bouillon R, Carmeliet G, Lieben L et al. (2014) Vitamin D and energy homeostasis – of mice and men. Nat Rev Endocrinol 10, 79–87. [DOI] [PubMed] [Google Scholar]
- 6. Hossein-Nezhad A, Mirzaei K, Keshavarz SA et al. (2013) Evidences of dual role of vitamin D through cellular energy homeostasis and inflammation pathway in risk of cancer in obese subjects. Minerva Med 104, 295–307. [PubMed] [Google Scholar]
- 7. Neve A, Corrado A & Cantatore F (2013) Immunomodulatory effects of vitamin D in peripheral blood monocyte-derived macrophages from patients with rheumatoid arthritis. Clin Exp Med 14, 275–283. [DOI] [PubMed] [Google Scholar]
- 8. Calton EK, Keane KN & Soares MJ (2015) The potential regulatory role of vitamin D in the bioenergetics of inflammation. Curr Opin Clin Nutr Metab Care 18, 367–373. [DOI] [PubMed] [Google Scholar]
- 9. Alberti KG, Eckel RH, Grundy SM et al. (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645. [DOI] [PubMed] [Google Scholar]
- 10. Cameron AJ, Magliano DJ, Zimmet PZ et al. (2007) The metabolic syndrome in Australia: prevalence using four definitions. Diabetes Res Clin Pract 77, 471–478. [DOI] [PubMed] [Google Scholar]
- 11. Beltran-Sanchez H, Harhay MO, Harhay MM et al. (2013) Prevalence and trends of metabolic syndrome in the adult US population, 1999–2010. J Am Coll Cardiol 62, 697–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grundy SM (2008) Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 28, 629–636. [DOI] [PubMed] [Google Scholar]
- 13. Daly RM, Gagnon C, Lu ZX et al. (2012) Prevalence of vitamin D deficiency and its determinants in Australian adults aged 25 years and older: a national, population-based study. Clin Endocrinol (Oxf) 77, 26–35. [DOI] [PubMed] [Google Scholar]
- 14. Nowson CA, McGrath JJ, Ebeling PR et al. (2012) Vitamin D and health in adults in Australia and New Zealand: a position statement. Med J Aust 196, 686–687. [DOI] [PubMed] [Google Scholar]
- 15. Australian Bureau of Statistics (2014) Australian Health Survey: Nutrition First Results – Food and Nutrients, 2011–12. Canberra: ABS. [Google Scholar]
- 16. Peterlik M, Boonen S, Cross HS et al. (2009) Vitamin D and calcium insufficiency-related chronic diseases: an emerging world-wide public health problem. Int J Environ Res Public Health 6, 2585–2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brock KE, Huang WY, Fraser DR et al. (2011) Diabetes prevalence is associated with serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D in US middle-aged Caucasian men and women: a cross-sectional analysis within the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. Br J Nutr 106, 339–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brenner DR, Arora P, Garcia-Bailo B et al. (2011) Plasma vitamin D levels and risk of metabolic syndrome in Canadians. Clin Invest Med 34, E377–E384. [DOI] [PubMed] [Google Scholar]
- 19. Gagnon C, Lu ZX, Magliano DJ et al. (2012) Low serum 25-hydroxyvitamin D is associated with increased risk of the development of the metabolic syndrome at five years: results from a national, population-based prospective study (The Australian Diabetes, Obesity and Lifestyle Study: AusDiab). J Clin Endocrinol Metab 97, 1953–1961. [DOI] [PubMed] [Google Scholar]
- 20. Anderson JL, May HT, Horne BD et al. (2010) Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am J Cardiol 106, 963–968. [DOI] [PubMed] [Google Scholar]
- 21. Kunutsor SK, Apekey TA & Steur M (2013) Vitamin D and risk of future hypertension: meta-analysis of 283,537 participants. Eur J Epidemiol 28, 205–221. [DOI] [PubMed] [Google Scholar]
- 22. Scragg R, Sowers M & Bell C (2007) Serum 25-hydroxyvitamin D, ethnicity, and blood pressure in the Third National Health and Nutrition Examination Survey. Am J Hypertens 20, 713–719. [DOI] [PubMed] [Google Scholar]
- 23. Chiu KC, Chu A, Go VLW et al. (2004) Hypovitaminosis D is associated with insulin resistance and β cell dysfunction. Am J Clin Nutr 79, 820–825. [DOI] [PubMed] [Google Scholar]
- 24. von Hurst PR, Stonehouse W & Coad J (2010) Vitamin D supplementation reduces insulin resistance in South Asian women living in New Zealand who are insulin resistant and vitamin D deficient – a randomised, placebo-controlled trial. Br J Nutr 103, 549–555. [DOI] [PubMed] [Google Scholar]
- 25. Zemel MB, Shi H, Greer B et al. (2000) Reguatlion of adiposity by dietary calcium. FASEB J 14, 1132–1138. [PubMed] [Google Scholar]
- 26. Soares MJ, Chan She Ping-Delfos W & Ghanbari MH (2011) Calcium and vitamin D for obesity: a review of randomized controlled trials. Eur J Clin Nutr 65, 994–1004. [DOI] [PubMed] [Google Scholar]
- 27. Soares MJ, Murhadi LL, Kurpad AV et al. (2012) Mechanistic roles for calcium and vitamin D in the regulation of body weight. Obes Rev 13, 592–605. [DOI] [PubMed] [Google Scholar]
- 28. Soares MJ, Pathak K & Calton EK (2014) Calcium and vitamin D in the regulation of energy balance: where do we stand? Int J Mol Sci 15, 4938–4945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Soares MJ, Ping-Delfos WC, Sherriff JL et al. (2011) Vitamin D and parathyroid hormone in insulin resistance of abdominal obesity: cause or effect? Eur J Clin Nutr 65, 1348–1352. [DOI] [PubMed] [Google Scholar]
- 30. Major GC, Alarie F, Dore J et al. (2007) Supplementation with calcium + vitamin D enhances the beneficial effect of weight loss on plasma lipid and lipoprotein concentrations. Am J Clin Nutr 86, 54–59. [DOI] [PubMed] [Google Scholar]
- 31. Calton EK, Pathak K, Soares MJ et al. (2015) Vitamin D status and insulin sensitivity are novel predictors of resting metabolic rate: a cross-sectional analysis in Australian adults. Eur J Nutr (Epublication ahead of print version). [DOI] [PubMed] [Google Scholar]
- 32. Pittas AG, Dawson-Hughes B, Li T et al. (2006) Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes Care 29, 650–656. [DOI] [PubMed] [Google Scholar]
- 33. Davies KM, Heaney RP, Recker RP et al. (2000) Calcium intake and body weight. J Clin Endocrinol Metab 85, 4635–4638. [DOI] [PubMed] [Google Scholar]
- 34. Drolet R, Richard C, Sniderman AD et al. (2008) Hypertrophy and hyperplasia of abdominal adipose tissues in women. Int J Obes (Lond) 32, 283–291. [DOI] [PubMed] [Google Scholar]
- 35. Institute of Medicine (2011) Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 36. Department of Health (2012) The Victorian Health Monitor. Melbourne: State Government of Victoria. [Google Scholar]
- 37. Kelsall LM, de Gooyer TE, Carey M et al. (2013) Blood lead levels in the adult Victorian population: results from the Victorian Health Monitor. Aust N Z J Public Health 37, 233–237. [DOI] [PubMed] [Google Scholar]
- 38. Australian Bureau of Statistics (2013) Australian Health Survey: Users’ Guide 2011–13 . Canberra: ABS. [Google Scholar]
- 39. Dunstan DW, Zimmet PZ, Welborn TA et al. (2002) The Australian Diabetes, Obseity and Lifestyle Study (AusDiab) – methods and response rates. Diabetes Res Clin Pract 57, 119–129. [DOI] [PubMed] [Google Scholar]
- 40. Department of Health (2012) Victorian Population Health Survey 2010. Melbourne: State Government of Victoria. [Google Scholar]
- 41. Department of Health (2014) Victorian Population Health Survey 2011–12, Survey Findings . Melbourne: State Government of Victoria. [Google Scholar]
- 42. World Health Organization (1999) Diabetes and Non-Communicable Disease Risk Factor Surveys – A Field Guide. Geneva: WHO. [Google Scholar]
- 43. Department of Health (2012) The Victorian Health Monitor Food and Nutrition Report. Melbourne: State Government of Victoria. [Google Scholar]
- 44. American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33, Suppl. 1, S62–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Food Standards Australia New Zealand (2007) AUSNUT 2007: Australian Food, Supplement & Nutrient Database 2007 for Estimation of Population Nutrient Intakes. Canberra: FSANZ. [Google Scholar]
- 46. Armstrong T, Bauman A & Davies J (2000) Physical Activity Patterns of Australian Adults: Results of the 1999 National Physical Activity Survey. Canberra: Australian Institute of Health and Welfare. [Google Scholar]
- 47. Markwick A, Ansari Z, Sullivan M et al. (2015) Social determinants and psychological distress among Aboriginal and Torres Strait Islander adults in the Australian state of Victoria: a cross-sectional population based study. Soc Sci Med 128, 178–187. [DOI] [PubMed] [Google Scholar]
- 48. Hypponen E, Boucher BJ, Berry DJ et al. (2008) 25-Hydroxyvitamin D, IGF-1 and metabolic syndrome at 45 years of age. Diabetes 57, 298–305. [DOI] [PubMed] [Google Scholar]
- 49. Yesil A & Yilmaz Y (2013) Review article: coffee consumption, the metabolic syndrome and non-alcoholic fatty liver disease. Aliment Pharmacol Ther 38, 1038–1044. [DOI] [PubMed] [Google Scholar]
- 50. Reis JP, von Muhlen D & Miller ER 3rd (2008) Relation of 25-hydroxyvitamin D and parathyroid hormone levels with metabolic syndrome among US adults. Eur J Endocrinol 159, 41–48. [DOI] [PubMed] [Google Scholar]
- 51. Ford ES, Ajani UA, McGuire LC et al. (2005) Concentrations of serum vitamin D and the metabolic syndrome among US adults. Diabetes Care 28, 1228–1230. [DOI] [PubMed] [Google Scholar]
- 52. Gradillas-García A, Álvarez J, Rubio JA et al. (2015) Relationship between vitamin D deficiency and metabolic syndrome in adult population of the Community of Madrid. Endocrinol Nutr 62, 180–187. [DOI] [PubMed] [Google Scholar]
- 53. Vitezova A, Zillikens MC, van Herpt TT et al. (2015) Vitamin D status and metabolic syndrome in the elderly: the Rotterdam Study. Eur J Endocrinol 172, 327–335. [DOI] [PubMed] [Google Scholar]
- 54. Heaney RP (2008) Vitamin D and calcium interactions: functional outcomes. Am J Clin Nutr 88, issue 2, 541S–544S. [DOI] [PubMed] [Google Scholar]
- 55. Lips P (2012) Interaction between vitamin D and calcium. Scand J Clin Lab Invest Suppl 243, 60–64. [DOI] [PubMed] [Google Scholar]
- 56. Norman AW (1990) Intestinal calcium absorption: a vitamin D-hormone-mediated adaptive response. Am J Clin Nutr 51, 290–300. [DOI] [PubMed] [Google Scholar]
- 57. Shapses SA, Sukumar D, Schneider SH et al. (2012) Hormonal and dietary influences on true fractional calcium absorption in women: role of obesity. Osteoporos Int 23, 2607–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ahlström T, Hagström E, Larsson A et al. (2009) Correlation between plasma calcium, parathyroid hormone (PTH) and the metabolic syndrome (MetS) in a community-based cohort of men and women. Clin Endocrinol (Oxf) 71, 673–678. [DOI] [PubMed] [Google Scholar]
- 59. Huang C, Shapses S & Wang X (2013) Association of plasma parathyroid hormone with metabolic syndrome and risk for cardiovascular disease. Endocr Pract 19, 712–717. [DOI] [PubMed] [Google Scholar]
- 60. Durazo-Arvizu RA, Dawson-Hughes B, Sempos CT et al. (2010) Three-phase model harmonizes estimates of the maximal suppression of parathyroid hormone by 25-hydroxyvitamin D in persons 65 years of age and older. J Nutr 140, 595–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lucas R & Neale R (2014) What is the optimal level of vitamin D? Aust Fam Physician 43, 119–122. [PubMed] [Google Scholar]
- 62. Mason C, Xiao L, Imayama I et al. (2014) Vitamin D3 supplementation during weight loss: a double-blind randomized controlled trial. Am J Clin Nutr 99, 1015–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Cade C & Norman AW (1986) Vitamin D3 improves impaired glucose tolerance and insulin secretion in the vitamin D-deficient rat in vivo . Endocrinology 119, 84–90. [DOI] [PubMed] [Google Scholar]
- 64. Cavalier E, Delanaye P, Souberbielle JC et al. (2011) Vitamin D and type 2 diabetes mellitus: where do we stand? Diabetes Metab 37, 265–272. [DOI] [PubMed] [Google Scholar]
- 65. Norman AW, Frankel BJ, Heldt AM et al. (1980) Vitamin D deficiency inhibits pancretic secretion of insulin. Science 209, 823–825. [DOI] [PubMed] [Google Scholar]
- 66. Mathieu C, Gysemans C, Giulietti A et al. (2005) Vitamin D and diabetes. Diabetologia 48, 1247–1257. [DOI] [PubMed] [Google Scholar]
- 67. Palomer X, Gonzalez-Clemente JM, Blanco-Vaca F et al. (2008) Role of vitamin D in the pathogenesis of type 2 diabetes mellitus. Diabetes Obes Metab 10, 185–197. [DOI] [PubMed] [Google Scholar]
- 68. Procopio M & Borretta G (2003) Derangement of glucose metabolism in hyperparathyroidism. J Endocrinol Invest 26, 1136–1142. [DOI] [PubMed] [Google Scholar]
- 69. Cozzolino M, Ketteler M & Zehnder D (2010) The vitamin D system: a crosstalk between the heart and kidney. Eur J Heart Fail 12, 1031–1041. [DOI] [PubMed] [Google Scholar]
- 70. Merke J, Milde P, Lewicka S et al. (1989) Identification and regulation of 1,25-dihydroxyvitamin D3 receptor activity and biosynthesis of 1,25-dihydroxyvitamin D3 . J Clin Invest 83, 1903–1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Vaidya A, Forman JP & Williams JS (2011) Vitamin D and the vascular sensitivity to angiotensin II in obese Caucasians with hypertension. J Hum Hypertens 25, 672–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Nasser M (2009) The metabolic syndrome: insulin resistance. Curr Hypertens Rep 11, 156–158. [DOI] [PubMed] [Google Scholar]
- 73. Schmieder RE, Hilgers KF, Schlaich MP et al. (2007) Renin–angiotensin system and cardiovascular risk. Lancet 369, 1208–1219. [DOI] [PubMed] [Google Scholar]
- 74. Ullah MI, Uwaifo GI, Nicholas WC et al. (2010) Does vitamin D deficiency cause hypertension? Current evidence from clinical studies and potential mechanisms. Int J Endocrinol 2010, 579–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Giallauria F, Milaneschi Y, Tanaka T et al. (2012) Arterial stiffness and vitamin D levels: the Baltimore longitudinal study of aging. J Clin Endocrinol Metab 97, 3717–3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lee JI, Oh SJ, Ha WC et al. (2012) Serum 25-hydroxyvitamin D concentration and arterial stiffness among type 2 diabetes. Diabetes Res Clin Pract 95, 42–47. [DOI] [PubMed] [Google Scholar]
- 77. Alyami A, Soares MJ, Sherriff JL et al. (2014) Vitamin D & endothelial function. Indian J Med Res 140, 483–490. [PMC free article] [PubMed] [Google Scholar]
- 78. Leung PS (2016) The potential protective action of vitamin D in hepatic insulin resistance and pancreatic islet dysfunction in type 2 diabetes mellitus. Nutrients 8, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Gonzalez JT, Rumbold PL & Stevenson EJ (2012) Effect of calcium intake on fat oxidation in adults: a meta-analysis of randomized, controlled trials. Obes Rev 13, 848–857. [DOI] [PubMed] [Google Scholar]
- 80. Christensen R, Lorenzen JK, Svith CR et al. (2009) Effect of calcium from dairy and dietary supplements on faecal fat excretion: a meta-analysis of randomized controlled trials. Obes Rev 10, 475–486. [DOI] [PubMed] [Google Scholar]
- 81. Lai YH & Fang TC (2013) The pleiotropic effect of vitamin D. ISRN Nephrol 2013, 898125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Calton EK, Keane KN, Newsholme P et al. (2015) The impact of vitamin D levels on inflammatory status: a systematic review of immune cell studies. PLoS One 10, e0141770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Australian Bureau of Statistics (2015) Australian Health Survey: Usual Nutrient Intakes, 2011–12. Canberra: ABS. [Google Scholar]
- 84. Kurth T & Sonis J (2007) Assessment and control of confounding in trauma research. J Trauma Stress 20, 807–820. [DOI] [PubMed] [Google Scholar]
- 85. Speeckaert M, Huang G, Delanghe JR et al. (2006) Biological and clinical aspects of the vitamin D binding protein (Gc-globulin) and its polymorphism. Clin Chim Acta 372, 33–42. [DOI] [PubMed] [Google Scholar]
- 86. Lauridsen AL, Vestergaard P, Hermann AP et al. (2005) Plasma concentrations of 25-hydroxy-vitamin D and 1,25-dihydroxy-vitamin D are related to the phenotype of Gc (vitamin D-binding protein): a cross-sectional study on 595 early postmenopausal women. Calcif Tissue Int 77, 15–22. [DOI] [PubMed] [Google Scholar]
- 87. Boucher BJ (2012) Is vitamin D status relevant to metabolic syndrome? Dermatoendocrinology 4, 212–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Fu L, Yun F, Oczak M et al. (2009) Common genetic variants of the vitamin D binding protein (DBP) predict differences in response of serum 25-hydroxyvitamin D [25(OH)D] to vitamin D supplementation. Clin Biochem 42, 1174–1177. [DOI] [PubMed] [Google Scholar]
- 89. Arnaud J & Constans J (1993) Affinity differences for vitamin D metabolites associated with the genetic isoforms of the human serum carrier protein (DBP). Hum Genet 92, 183–188. [DOI] [PubMed] [Google Scholar]
- 90. Hypponen E, Berry DJ, Wjst M et al. (2009) Serum 25-hydroxyvitamin D and IgE – a significant but nonlinear relationship. Allergy 64, 613–620. [DOI] [PubMed] [Google Scholar]
- 91. Tseng CH (2010) Betel nut chewing and incidence of newly diagnosed type 2 diabetes mellitus in Taiwan. BMC Res Notes 3, 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Boucher BJ, Ewen SWB & Stowers JM (1994) Betel nut (Areca catechu) consumption and the induction of glucose intolerance in adult CD1 mice and in their F1 and F2 offspring. Diabetologia 37, 49–55. [DOI] [PubMed] [Google Scholar]
- 93. Mann J (2002) Discrepancies in nutritional recommendations: the need for evidence based nutrition. Asia Pac J Clin Nutr 11, Suppl. 3, S510–S515. [DOI] [PubMed] [Google Scholar]
- 94. Truswell AS (2001) Levels and kinds of evidence for public-health nutrition. Lancet 357, 1061–1062. [DOI] [PubMed] [Google Scholar]