Abstract
Objective
Gaining too much or too little weight in pregnancy (according to Institute of Medicine (IOM) guidelines) negatively affects both mother and child, but many women find it difficult to manage their gestational weight gain (GWG). Here we describe the use of the intervention mapping protocol to design ‘Come On!’, an intervention to promote adequate GWG among healthy pregnant women.
Design
We used the six steps of intervention mapping: (i) needs assessment; (ii) formulation of change objectives; (iii) selection of theory-based methods and practical strategies; (iv) development of the intervention programme; (v) development of an adoption and implementation plan; and (vi) development of an evaluation plan. A consortium of users and related professionals guided the process of development.
Results
As a result of the needs assessment, two goals for the intervention were formulated: (i) helping healthy pregnant women to stay within the IOM guidelines for GWG; and (ii) getting midwives to adequately support the efforts of healthy pregnant women to gain weight within the IOM guidelines. To reach these goals, change objectives and determinants influencing the change objectives were formulated. Theories used were the Transtheoretical Model, Social Cognitive Theory and the Elaboration Likelihood Model. Practical strategies to use the theories were the foundation for the development of ‘Come On!’, a comprehensive programme that included a tailored Internet programme for pregnant women, training for midwives, an information card for midwives, and a scheduled discussion between the midwife and the pregnant woman during pregnancy. The programme was pre-tested and evaluated in an effect study.
Keywords: Intervention development, Gestational weight gain, Nutritional advice, Promoting healthy pregnancy, Goal setting
Women who gain too much or too little weight during pregnancy are more likely to experience a variety of health problems during their pregnancies and in their later lives. Healthy gestational weight gain (GWG) yields the best obstetric outcomes and improves the long-term outcomes for the health and weight of mothers and their babies( 1 ).
In 2009, the Institute of Medicine (IOM) published revised guidelines for weight gain during pregnancy, providing recommendations for GWG based on a woman’s pre-pregnancy BMI. According to these guidelines, women who begin their pregnancy being underweight (BMI less than 18·5 kg/m2) should gain 12·5–18·0 kg during their pregnancy; normal weight women (BMI of 18·5–24·9 kg/m2) should gain 11·5–16·0 kg; women who are overweight (BMI of 25·0–29·9 kg/m2) should gain 7–11·5 kg; and obese women (BMI of 30·0 kg/m2 or above) should gain 5–9 kg( 1 ). The percentage of women in high-income countries who gain weight within these recommendations varies from 18·9 to 51·9 %( 2 – 4 ), demonstrating a clear need to focus on healthy GWG to improve the health prospects of mothers and babies.
Several interventions for promoting healthy GWG have been studied( 5 – 14 ). Reviews of these studies show these interventions to have varied effects, depending in large part on their target group (i.e. a general population or a specific risk group). The majority of GWG studies target specific groups, such as overweight or obese women, or women with hypertension or gestational diabetes. Interventions adopting a dietary approach, increasing physical activity and setting weight gain goals proved to be most effective at reaching healthy GWG( 14 ).
Interventions to encourage appropriate GWG fit well with the midwifery model of care( 15 ). A recent review of midwifery in the UK underscored the relationship between public health and midwifery( 16 ), emphasizing the importance of public health interventions during pregnancy and the postnatal period. Community midwives are in a unique position to improve the health of young families because they have regular contact (about twelve times) with pregnant women. In the Netherlands, 85 % of pregnant women begin care with community midwives and more than 50 % continue their pregnancy under guidance of the midwife( 17 ). Community midwives are authorized to care for healthy pregnant women, a group that stands to benefit from the prevention of weight-related disorders.
The theoretical and methodological tools used in health psychology can increase the effectiveness of health-related interventions( 9 , 18 , 19 ). However, as Hill et al. found in their review, it is very difficult to identify the theoretical assumptions of existing interventions designed to promote healthy GWG( 10 ). In the present paper we provide insights into the theoretical assumptions used in GWG interventions by describing the development of our ‘Come On!’ intervention promoting healthy GWG among healthy pregnant women. Our use of intervention mapping, a systematic approach for the development of interventions based on established theory and empirical data, makes explicit the theories we used to design our programme( 18 ). Intervention mapping also recognizes that individual behaviour is influenced by factors in the environment, namely individual, family, social network, organizations, communities and society( 18 ).
Methods
Intervention mapping consists of six steps: (i) needs assessment; (ii) formulation of change objectives; (iii) selection of theory-based methods and practical strategies; (iv) development of the intervention programme; (v) development of an adoption and implementation plan; and (vi) development of an evaluation plan. Here we describe the consecutive steps and will apply them in the Results section.
Step I: Needs assessment
Intervention mapping starts with the identification of the health problem, its behavioural factors and their associated individual and environmental determinants. The aim of this first step is to establish the relevant target groups and programme outcomes.
In our case, the needs assessment included a systematic review and meta-analysis of the literature on existing interventions for achieving a healthy GWG( 19 ). We also analysed the literature on the determinants and correlates of GWG in pregnant women, including the role of predefined behavioural (i.e. physical activity and dietary behaviour) and environmental risk factors.
In addition, we conducted a quantitative survey among healthy pregnant woman to investigate the percentages of women reaching healthy GWG and to assess the relationship between, among other factors, diet and physical activity and reaching a healthy GWG( 20 ). Furthermore, we scheduled individual interviews with community midwives to identify their behaviours with respect to promoting healthy GWG and the determinants of their behaviours( 21 ). The interview protocol was based on the Attitude–Social Influence–Self-Efficacy model( 22 ), a model useful in explaining or changing a variety of behaviours( 23 , 24 ). We used the information from the interviews and literature to construct our study model and questionnaire for the quantitative survey to measure midwives’ self-reported behaviours and determinants( 25 ).
During the needs assessment we established a project consortium including several midwives practising in primary care, a dietitian, a physiotherapist, a psychologist working with young mothers, an employee of the Royal Dutch Organization of Midwives (KNOV) and health educators. During the needs assessment, the project team met three times, to discuss the research findings, contribute to the decision-making process on the selection of target groups and advise on the outcomes of the behavioural programme. Between the meetings, we consulted with individual project members as needed.
Step II: Formulation of change objectives
In this second intervention mapping step, programme outcomes were subdivided into performance objectives. Performance objectives are related to sub-behaviours that must be accomplished by the target groups in order to achieve the programme outcomes. By linking the performance objectives with relevant behavioural determinants, the general formulations of the performance objectives were translated into very specific change objectives. The consortium was also involved in step II. Members offered advice about the relevance and changeability of the selected behavioural determinants and approved the formulation and selection of change objectives.
Step III: Selection of theory-based methods and practical strategies
In step III we identified and selected the theoretical methods; that is, general techniques or processes for influencing changes in behavioural determinants of the target groups. To do so, the change objectives were organized per determinant. Subsequently, methods were matched to the determinants. Methods were mainly selected from the summary of theoretical methods provided by Bartholomew et al.( 18 ). We organized a brainstorming session with the consortium in order to select the practical strategies to be used, identifying the specific techniques for employing theoretical methods in ways that fit our intervention population and the context in which our intervention would be conducted. We also relied on our systematic literature review of existing interventions for information on feasible working mechanisms( 19 ).
Step IV: Development of the intervention programme
In step IV we combined information from previous steps, which allowed us to operationalize the theoretical methods and develop the practical applications required to accomplish the change objectives. We decided upon programme scope and sequence and designed scripts and documents needed for the production of the programme. During this process we pre-tested our materials among members of the target groups, including consortium members and pregnant women.
Step V: Development of an adoption and implementation plan
The fifth step focused on the planning of the adoption and implementation of the intervention. The consortium meetings provided important information about the factors that would impede and enhance implementation in midwifery practices.
Step VI: Development of an evaluation plan
In this last step we developed a plan to evaluate the programme effectiveness and the quality of intervention. Our measurement instruments for evaluating programme effects were based on the instruments used in the needs assessment (step I) and on instruments for process evaluation described by Steckler and Linnan( 26 ).
Results
Step I: Needs assessment
In the literature, unhealthy GWG is described as both serious and widespread. The majority of published studies have focused on risk groups, such as obese pregnant women. As noted above, the percentage of women in high-income countries who gain weight within the IOM guidelines varies from 18·9 to 51·9 %( 2 , 3 , 27 ). In the Netherlands at the time of the study, the incidence of women who gained weight below, within and above the IOM guidelines was respectively 18·8–33·4 %, 39·9–43·8 % and 26·7–37·6 %( 4 , 28 ). For neonates, GWG below the guidelines was associated with prematurity and babies too small for their gestational age( 29 ). GWG above the guidelines was associated with, among other things, low 5-min Apgar scores, seizures, hypoglycaemia, polycythaemia, meconium aspiration syndrome and large for gestational age( 11 ). For women, GWG above the guidelines was associated with pregnancy-induced hypertension, gestational diabetes mellitus, pre-eclampsia, caesarean delivery, postpartum weight retention and long-term obesity( 11 , 30 ). A number of studies found that diet and physical activity are not the only mediators of healthy GWG( 31 , 32 ): the behaviour of health professionals also plays an important role( 33 , 34 ). Midwives, as the providers of regular check-ups during pregnancy, are important players in the process of reaching healthy GWG.
Our cross-sectional survey among 455 healthy Dutch pregnant women showed that GWG within the guidelines occurred in 42·4 % of the women, 13·8 % of the women gained too little and 43·9 % too much( 20 ). There was no significant correlation between GWG and pre-pregnancy BMI, diet or motivation to engage in healthy PA( 20 ). Weight gain below the IOM guidelines, v. within, was seen more often in women who reported more sleep shortage. Weight gain above the IOM guidelines (v. within) was seen less often in Dutch than in non-Dutch women, in women who maintained their physical activity level and in non-smoking women compared with women who stopped smoking( 20 ). The mean weekly vegetable consumption was 953 (sd 447) g. Recommended intake of vegetables, fruit and fish (respectively: ≥200 g/d; ≥2 pieces/d; ≥twice during the last week) was met by respectively 13·6, 47·2 and 6·8 %( 20 ). Nevertheless, the dietary behaviour of our sample was better than that of non-pregnant women of comparable ages in the Netherlands( 35 ), indicating that pregnant women do improve their diet during pregnancy. However, none of the measured dietary behaviours were significantly associated with healthy GWG( 20 ). More than half of the women reported a decline in physical activity during pregnancy and the self-reported mean pre-pregnancy physical activity was moderately active. A decline in physical activity was associated with GWG above the guidelines( 20 ).
Our qualitative study of six community midwives showed that midwives did monitor GWG (weighing and discussing GWG), offer education about diet and, to a lesser degree, offer education about healthy physical activity( 21 ). Behavioural determinants, originating from the Attitude–Social Influence–Self-Efficacy model( 36 ), were confirmed and other relevant themes, including midwives’ perception of their role in health promotion, were added to our hypothetical model explaining midwives’ behaviour in respect to promoting healthy GWG( 21 ).
Our cross-sectional survey study of midwives included 112 practising community midwives( 25 ). We found that midwives considered measuring weight, discussing GWG, education about healthy diet and, to a lesser extent, education about healthy physical activity to be part of their practice( 25 ). Midwives also agreed that discussion about public health issues (i.e. women’s health) was very important and they regularly discussed health promotion issues (e.g. physical well-being, social support, emotional coping) with their clients. Midwives offered more GWG monitoring when they had more positive attitudes towards it, experienced more supportive social influences concerning monitoring GWG and had fewer barriers to GWG monitoring( 25 ). Education about diet and physical activity was more likely among midwives with more positive attitudes towards it, higher reported self-efficacy, more social influences supporting education on diet and physical activity, and greater activity in health promotion( 25 ).
The literature on existing interventions aiming at healthy GWG revealed that most interventions were developed in the USA and Europe; half of the interventions focused on a single theme (e.g. on diet or physical activity), while the other half combined diet, physical activity and attention to weight. A meta-analysis showed that interventions focused on diet for obese women resulted in a mean difference of −8·41 kg (95 % CI −10·49, −6·34 kg), interventions focused on physical activity resulted in a mean difference of −0·83 kg (95 % CI −1·47, −0·19 kg) and interventions with multiple content had no significant effects. Secondary outcomes (e.g. change in diet) were inconsistent. We found only one study of healthy pregnant women( 36 ).
As a result of our needs assessment (and including the advice of the consortium) we decided that our intervention should target two groups: (i) healthy pregnant women; and (ii) community midwives.
For each target group, a behavioural objective was formulated. Our intervention was designed to:
-
1.
Help healthy pregnant women to stay within the IOM guidelines; and
-
2.
Get midwives to adequately support the efforts of healthy pregnant women to gain weight within the IOM guidelines.
Step II: Formulation of change objectives
Table 1 shows the behavioural objectives translated into performance objectives providing answers to the question: ‘What do participants of the programme need to do to succeed in the recommended health-related behaviour?’
Table 1.
Performance objectives for pregnant women and midwives
| Help healthy pregnant women to stay within the IOM guidelines | |
|---|---|
| PO1. | Pregnant women determine their BMI |
| PO2. | Pregnant women monitor their GWG |
| PO3. | Pregnant women select ways to accomplish healthy GWG |
| PO4. | Pregnant women follow midwives’ advice about healthy GWG |
| PO5. | Pregnant women follow midwives’ advice about referral to a dietitian, psychologist and/or an exercise programme |
| Get midwives to adequately support the efforts of healthy pregnant women to gain weight within the IOM guidelines | |
| PO1. | Midwives facilitate information supply about healthy GWG to all pregnant women in their first trimester |
| PO2. | At a gestational age of about 16 weeks, midwives adapt their care concerning healthy GWG to individual needs of pregnant women |
| PO3. | Midwives support pregnant women with monitoring and appraisal of their weight alteration during pregnancy |
| PO4. | Midwives identify clients who are at greater risk for unhealthy GWG |
| PO5. | Midwives empower those clients who are at greater risk for inappropriate GWG in reaching a healthy GWG |
| PO6. | Midwives identify pregnant women who need special care that is beyond the capabilities of midwives |
| PO7. | Midwives refer pregnant women, if necessary, to other health-care professionals, e.g. a dietitian |
| PO8. | In case of referral of pregnant women to other health-care professionals, midwives remain in contact with these professionals |
| PO9. | In case of referral of pregnant women to other health-care professionals, midwives support the care of those professionals |
PO, performance objective; IOM, Institute of Medicine; GWG, gestational weight gain.
We identified important and changeable behavioural determinants based on our literature review( 19 ), the surveys of pregnant women and midwives( 20 , 21 , 25 ), existing literature about determinants of (un)healthy GWG and feedback from the consortium.
The determinants of pregnant women’s behaviour included: awareness of the importance of healthy diet and sufficient physical activity in relation with their GWG and their (baby’s) health( 37 ); knowledge of their own height and weight( 38 ), calculation of their BMI and GWG recommendations( 39 ), negative consequences of too low and too high GWG( 20 , 33 , 40 ), positive consequences of healthy GWG( 20 ) and the positive influence of a healthy diet and healthy physical activity on GWG( 20 , 38 , 41 , 42 ); attitudes towards a healthy GWG( 20 , 43 , 44 ), a healthy diet and healthy physical activity, and following the advice of midwives( 20 , 28 , 34 , 45 – 48 ); social influence of family members (such as partners and mothers; information aroused during consortium meetings) and midwives( 20 , 33 , 34 , 49 ); self-efficacy expectations/skills with regard to assessing one’s BMI( 20 ), monitoring GWG( 20 , 45 ), healthy diet and healthy physical activity( 20 , 45 ), discussing exceeding IOM recommendations with the midwife and resisting well-meant advice from friends and family members; and barriers like no scale at home (information aroused during consortium meetings), pregnancy-related changes in diet preferences( 41 ), morning sickness and other physical complaints( 50 ), and the combination of pregnancy with care for other young children( 50 ).
The determinants of midwife behaviour included: awareness of their role in promoting healthy diet and physical activity( 21 , 25 ); knowledge, including consequences, of healthy GWG, diet and physical activity, of cut-off points of healthy GWG and of diet and physical activity advice( 21 , 25 , 33 , 46 ); attitudes towards encouraging healthy GWG, healthy diet and physical activity( 25 ); perceived social influences from clients, clients’ partners, colleagues, the Royal Dutch Organization of Midwives, obstetricians( 25 ) and from established guidelines( 51 ); self-efficacy expectations/skills towards tailoring their care to the individual needs of women during the course of pregnancy( 25 ); and barriers including lack of time and lack of guidelines( 25 ).
Tables 2 and 3 show the matrices of change objectives that linked objectives and determinants, based on our performance objectives and selected determinants. Each change objective specified what participants need to learn to accomplish the performance objective. For instance, Table 2 shows a cell in which the performance objective ‘pregnant women determine their BMI’ is linked with the determinant ‘knowledge’. The question used to address this cell is: ‘What knowledge do pregnant women need to determine their BMI?’ Answers to this question create the change objectives ‘Describe height and weight’ and ‘Describe the calculation of BMI’ (Tables 2 and 3).
Table 2.
Change objectives for pregnant women
| Determinants→PO | Awareness (aw) | Knowledge (k) | Attitudes (a) | Social influences (si) | Self-efficacy/skills (se) | Barriers (b) |
|---|---|---|---|---|---|---|
| PO1. Pregnant women determine their BMI | k1a. Describe height and weight k1b. Describe the calculation of BMI | a1a. Believe it is important to know their personal BMI | si1a. Describe that midwives consider knowing your BMI as important | se1a. Express confidence in calculation of BMI (including measuring height and weight) | ||
| PO2. Pregnant women monitor their weight gain every week | aw2a. Accord the value of monitoring their weight gain every week | k2a. Describe the guidelines for healthy GWG k2b. Describe the healthy first-trimester GWG for their BMI k2c. Describe the healthy GWG for their BMI after the first trimester k2d. Describe the healthy GWG for their BMI at the end of pregnancy k2e. Describe the negative consequences (short- and long-term) of unhealthy GWG k2f. Describe the positive consequences (short- and long-term) of healthy GWG | a2a. Believe it is important to reach a healthy GWG a2b. Believe it is important to protect their fetus’ health with a healthy GWG a2c. Believe it is important to protect their own health with a healthy GWG a2d. Believe it is important to return to their pre-pregnancy weight after birth a2e. Believe it is important to monitor their GWG | si2a. Describe that it is midwives’ ambition to reach a healthy GWG si2b. Describe that their midwife stimulates them to monitor their GWG | se2a. Express confidence in monitoring GWG | b2a. Express the usage of a scale every week |
| PO3. Pregnant women select ways to accomplish healthy GWG | aw3a. Accord the value of finding a way to accomplish healthy GWG | k3a. Describe the contribution of healthy diet to GWG k3b. Describe the contribution of healthy PA to GWG k3c. Describe the contribution of well-being to GWG k3d. Describe the advantages of monitoring GWG during pregnancy k3e. Describe the advantages of discussing unhealthy GWG with the midwife k3f. Describe frequently heard well-meant untrue advice | a3a. Feel positive about reaching a healthy GWG with a healthy diet a3b. Feel positive about reaching a healthy GWG with healthy PA a3c. Feel positive about reaching a healthy GWG with well-being a3d. Believe it is important to determine a personal target weight a3e. Believe it is important to regularly monitor their GWG a3f. Believe it is important to discuss unhealthy GWG with the midwife | si3a. Describe that a healthy lifestyle (diet, PA) is their midwife’s ambition si3b. Describe that their midwife stimulates them to reach a healthy GWG si3c. Describe that they feel supported by their midwife in making GWG negotiable si3d. Describe being able to resist social pressure (‘eat for two’, ‘stay inactive’) si3e. Describe being able to resist social pressure of their offspring to snack unhealthily or to be inactive | se3a. Express confidence in realizing a healthy diet se3b. Express confidence in realizing healthy PA se2c. Express confidence in protecting their own well-being se3d. Demonstrate discussing unhealthy GWG with their midwife se3e. Express confidence to resist well-meant untrue advice se3f. Express confidence in resisting pressure from their offspring | b3a. Believe that they can handle changing dietary needs b3b. Believe that they can maintain a healthy diet in case of physical complaints b3c. Believe that they can maintain healthy PA in case of physical complaints b3d. Believe that they can have a healthy lifestyle in combination with the care for their offspring |
| PO4. Pregnant women follow midwives’ advice about healthy GWG | aw4a. Accord the value of following midwives’ advice about healthy GWG | k4a. Recall midwives’ advice concerning GWG | a4a. Believe it is important to follow midwives’ advice a4b. Believe that midwives’ advice belongs to themselves | si4a. Describe that others in their environment endorse the importance of following midwives’ advice | se4a. Express confidence in following midwives’ advice | b4a. Plan how to cope with barriers that hinder following midwives’ advice (tiredness, care for offspring, time, etc.) b4b. Describe how they include midwives’ advice into daily routine |
| PO5. Pregnant women follow midwives’ advice about referral to a dietitian, psychologist, an exercise programme | aw5a. Accord the value of visiting a dietitian, psychologist, an exercise programme | a5a. Believe it is important to visit, if relevant, a dietitian, psychologist, an exercise programme | si5a. Recognize that is normal to visit a dietitian, psychologist, an exercise programme |
PO, performance objective; GWG, gestational weight gain; PA, physical activity.
Table 3.
Change objectives for midwives
| Determinants→PO | Awareness of public health role (aw) | Knowledge (k) | Attitudes (a) | Social influences (si) | Self-efficacy/skills (se) | Barriers (b) |
|---|---|---|---|---|---|---|
| PO1. Midwives facilitate information supply about healthy GWG to all pregnant women in their first trimester | aw1a. Confirm the value of education about GWG on pregnant women’s behaviour | a1a. Believe it is important to stimulate healthy GWG a1b. Believe it is important to provide information about healthy GWG a1c. Believe it is important to draw pregnant women’s attention to strategies for reaching healthy GWG a1d. Believe it is important to inform pregnant women about healthy GWG | ||||
| PO2. At a gestational age of about 16 weeks, midwives adapt their care concerning healthy weight gain to individual needs of pregnant women | aw2a. Confirm the impact of societal temptations that inhibit healthy GWG | k2a. Describe advantages of healthy GWG for pregnant women and their offspring (short- and long-term) k2b. Describe short- and long-term consequences of unhealthy GWG k3c. Describe ways to reach a healthy GWG (diet, PA, well-being in general) k3d. Describe the content of healthy dietary behaviour k2e. Describe the content of healthy PA k2f. Describe the ingredients of well-being in general (WHO definition: physical, mental, societal well-being) k2g. Describe for each BMI category the appropriate target weight and healthy GWG per time episode (first trimester, after first trimester weekly GWG) k2h. Describe that information supply about GWG to pregnant women promotes reaching healthy GWG k2i. Describe a clear plan for the care of GWG, diet and PA k2j. Explain effective medical communication (interactive, effectual, etc.) k2k. Explain the effect of goal setting with regard to GWG at the end of pregnancy | a2a. Believe it is important to determine, together with the pregnant women, a target weight for the complete pregnancy | si2a. Recognize that pregnant women expect them to provide education about healthy GWG | se2a. Express confidence in matching BMI categories with specific target weights and specific GWG per time episode se2b. Demonstrate the ability to combine target weight according the guidelines with the personalized target weight of a pregnant woman se2c. Feel confidence in bringing healthy GWG under attention of pregnant overweight/obese women | b2a. Plan how to cope with time barriers that hinder providing GWG education b2b. Use a protocol to perform a weight anamnesis |
| PO3. Midwives support pregnant women with monitoring, appraisal of their GWG | aw3a. Confirm the value of midwife’s support on GWG and well-being | k3a. Explain the contribution of monitoring and evaluating GWG during pregnancy k3b. Describe how to monitor and evaluate GWG | a3a. Believe it is important to stimulate pregnant women to monitor and evaluate their GWG a3b. Believe it is important that pregnant women take responsibility for their GWG a3c. Believe it is important to show interest in pregnant women’s GWG | si3a. Believe that pregnant women think it is important to monitoring their (pregnant women’s) GWG | se3a. Express confidence in supporting pregnant women in monitoring and evaluating GWG se3b. Demonstrate the ability to proactively ask pregnant women about their GWG | |
| PO4. Midwives identify clients who are at greater risk for unhealthy GWG | k4a. Describe risk groups for gaining unhealthy GWG. k4b. Describe adequate weight anamneses k4c. Describe an healthy weight curve and the dangers of deviation from the curve | a4a. Believe it is important to identify those pregnant women who need support a4b. Believe it is important to carry out an adequate weight anamnesis a4c. Believe it is important to identify deviations from the curve | se4a. Demonstrate the ability to take an adequate weight anamnesis se4b. Express confidence in being able to detect a deviation from the curve | b4a. Plan sufficient time to perform an adequate weight anamnesis | ||
| PO5. Midwives empower those clients who are at greater risk for unhealthy GWG in reaching a healthy GWG | aw5a. Acknowledge the relationship between GWG/lifestyles and pregnant women’s well-being aw5b. Confirm the value of midwives’ support aw5c. Confirm the value of other professionals’ contribution in regard to GWG | k5a. Describe pregnancy complaints that increase the chance of unhealthy GWG | a5a. Believe it is important to support pregnant women in reaching a healthy GWG a5b. Express openness to questions and concerns from pregnant women about their GWG/lifestyle a5c. Believe it is important to search, together with the pregnant woman, for causes and solutions for GWG/lifestyle-related problems in order to retrieve a healthy GWG a5d. Believe it is important to refer pregnant women, if necessary, to professionals specialized in diet, exercise, well-being a5e. Express positive feelings towards engagement in collaborative partnership | si5a. Recognize that other midwives think that midwives’ support in reaching healthy GWG is important si5b. Recognize that pregnant women think that midwives’ support in reaching healthy GWG is important si5c. Recognize that pregnant women think it is important to find ways to reach healthy GWG si5d. Recognize that colleagues think it is important to find ways to reach healthy GWG | se5a. Express confidence in supporting pregnant women to a healthy GWG/lifestyle se5b. Express confidence in searching with pregnant women for causes for deviation from the curve se5c. Express confidence in searching with pregnant women for solutions to deviation from the curve se5d. Express confidence in supplying advice about diet, exercise and well-being in general se5e. Express confidence in discussing the GWG curve | b5a. Plan sufficient time to discuss with pregnant women healthy GWG/lifestyle and ways how to achieve it b5b. Make use of practical tools/guidelines for the coaching of a healthy GWG/lifestyle b5c. Plan sufficient time to coach pregnant women to healthy GWG/lifestyle b5d. Plan sufficient time to discuss causes with pregnant women who experience GWG/lifestyle problems and to find ways to return to a healthy GWG |
| PO6. Midwives identify those pregnant women who need special care, which exceeds midwives’ capabilities | k6a. Describe criteria for referral to specialized caregivers k6b. Explain that gaining unhealthy GWG necessitates specialized care | a6a. Believe it is important to identify those pregnant women who need support of other specialized professionals | b6a. Use guidelines to perform adequate lifestyle anamnesis | |||
| PO7. Midwives refer pregnant women, if necessary, to other health-care professionals | se7a. Express confidence to refer to professionals specialized in diet, PA, exercise programmes | b7a. Prepare/adapt a list of eligible local health-care professionals | ||||
| PO8. In case of referral of pregnant women to other health-care professionals, midwives support the care of those professionals | se8a. Express confidence to support professionals specialized in diet, PA, exercise programmes |
PO, performance objective; GWG, gestational weight gain; PA, physical activity.
Step III: Selection of theory-based methods and practical strategies
Tables 4 and 5 show the theory-based methods and practical strategies we chose to accomplish the change objectives for pregnant women and midwives.
Table 4.
Methods and strategies per determinant for pregnant women
| Determinant | Change objectives | Method | Theory | Strategy |
|---|---|---|---|---|
| Awareness (aw) | aw2a, aw3a, aw4a, aw5a | Tailoring Using imagery Providing cues Chunking | TTM( 52 ) SCT( 53 ) | Personal communication with midwife Tailored web-based programme with information about specialized professionals combined with visual representation of pregnant woman’s individual GWG compared with healthy GWG |
| Knowledge (k) | k1a, k1b, k2a, k2b, k2c, k2d, k2e, k2f, k3a, k3b, k3c, k3d, k3e, k3f, k4a | Tailoring Active learning Chunking Using imagery | TTM( 52 ) SCT( 53 ) | Personal communication with midwife Tailored web-based programme (dosed information on individual BMI, on healthy GWG tailored on participant pre-pregnancy BMI, tailored information about healthy diet, PA, general information about a relaxed lifestyle, risks/advantages of (un)healthy GWG) Active participation in monitoring own BMI, GWG |
| Attitudes (a) | a1a, a2a, a2b, a2c, a2d, a2e, a3a, a3b, a3c, a3d, a3e, a3f, a4a, a5a | Self-re-evaluation Individualization Tailoring | TTM( 52 ) SCT( 53 ) | Personal communication with midwife, about e.g. healthy GWG, healthy diet, PA, monitoring weight, referral to relevant health-care professionals Tailored web-based programme: when gaining too much or too little weight an advice comes up to discuss this freely with midwife, or to consult a specialist A short film in the tailored web-based programme: a role model provides information and arguments on individual healthy GWG tailored on participant pre-pregnancy BMI, PA; with general information about healthy diet and relaxed lifestyle, risks/advantages of (un)healthy GWG |
| Social influences (si) | si1a, si2a, si2b, si3a, si3b, si3c, si3d, si3e, si4a, si5a | Information about other’s approval | TTM( 52 ) SCT( 53 ) | Regular personal communication with midwife Tailored web-based programme: stimulating messages to discuss GWG problems with midwives, with suggestions e.g. how to cope with children disliking vegetables Tailored web-based programme: reinforcing messages from the pregnant woman’s midwife A quote on midwives‘ website about the cooperation with specialized health professionals Tailored web-based programme: in case of unhealthy GWG, an advice comes up to discuss this freely with midwife, to consult a specialist Tailored web-based programme: videos with peers talking about their visit to a dietitian/exercise programme |
| Self-efficacy/skills (se) | se1a, se2a, se3a, se3b, se3c, se3d, se3e, se3f, se4a | Goal setting Verbal persuasion Guided practice | SCT( 53 ) GST( 54 ) | Personal communication with midwife Tailored web-based programme with FAQ about personal weight gain goal followed by feedback, short films with e.g. demonstration of peers buying/preparing vegetables, exercising, and peers discussing their coping with too high GWG |
| Barriers (b) | b2a, b3a, b3b, b3c, b3d, b4a, b4b | Facilitation | SCT( 53 ) | Personal communication with midwife Tailored web-based programme with visual representation of barriers (e.g. physical complaints, care for offspring) and information about how to overcome them |
TTM, Transtheoretical Model; SCT, Social Cognitive Theory; GST, Goal Setting Theory; GWG, gestational weight gain; PA, physical activity; FAQ, frequently asked questions.
Table 5.
Methods and strategies per determinant for midwives
| Determinant | Change objectives | Method | Theory | Strategy |
|---|---|---|---|---|
| Awareness (aw) | aw1a, aw2a, aw3a, aw5a, aw5b, aw5c | Consciousness raising | TTM( 52 ) SCT( 53 ) | Presentation at start of training with information, confrontation about prevalence, causes and consequences of unhealthy GWG, and invitation for feedback Attention on the easy access to junk food and on healthy alternatives (like raw vegetables instead of cookies) Attending, gaining experience with the programme during the training session |
| Knowledge (k) | k2a, k2b, k2c, k2d, k2e,k2f, k2g, k2h, k2i, k2j, k2k | Active learning Cooperative learning Discussion | ELM( 55 ) SCT( 53 ) | At the start of the training, the trainer identifies with participants’ most eye-catching issues related to GWG (health advantages, consequences of too high/low GWG, diet, PA, well-being, appropriate GWG, etc.) followed by a discussion about difficult situations in participants’ midwifery practices Information card Attending, gaining experience with the web-based tailored programme together with colleagues during the training session |
| Attitudes (a) | a1a, a1b, a1c, a1d, a2a, a3a, a3b, a3c, a4a, a4b,a4c, a5a, a5b, a5c, a5d, a5e, a6a | Arguments Active learning | ELM( 55 ) SCT( 53 ) | Presentation at start of training with information, confrontation about the discrepancy of what midwives think pregnant women need and women’s actual needs (at the start of pregnancy) Group discussion during training session about important learning questions related to GWG, disclosing the existing pros and cons. Discussion results in a collective casus that will later in the training be used as an exercise example Attending, gaining experience with the programme (e.g. with the GWG curve) together with colleagues during the training session During training a group discussion to prime and underpin the significance of the update of midwives’ social network (dietitian, physiotherapist, coach); who can help them, how is the actual/ideal cooperation, what can help to stimulate an effective cooperation |
| Social influences (si) | si2a, si3a, si5a, si5b, si5c, si5d | Information about others’ approval | SCT( 53 ) | Presentation (oral and visual) during training with information about pregnant women’s needs for information about GWG in particular and lifestyle in general, early in pregnancy Attending, gaining experience with the programme together with colleagues during the training session Discussion with midwives: during training a group discussion to prime and underpin the significance of the update of midwives’ social network (dietitian, physiotherapist, coach); who can help them, how is the actual/ideal cooperation, what can help to stimulate an effective cooperation |
| Self-efficacy/skills (se) | se2a, se2b, se2c, se3a, se3b, se4a, se4b, se5a, se5b, se5c, se5d, se5e, se7a, se8a | Guided practice Training Planning coping responses | SCT( 53 ) | During the training: Instructions about exercise with feedback on the use of the information card with special attention to appropriate interview techniques Instructions about calculation of adequate GWG categories and practising with information card according to pre-pregnancy BMI group Instructions for appropriate anticipating on specific barriers of pregnant women Instructions about communication with other professionals about appropriate referrals in case of unhealthy GWG Attending, gaining experience with the programme (e.g. with shaping the GWG curve) together with colleagues during the training session |
| Barriers (b) | b2b, b5b, b6a, b7a | Facilitating Enactive mastery | SCT( 53 ) | Information card for midwives and web-based tailored programme for pregnant women to structure GWG education and to make more efficient use of expensive time Guidelines for weight anamneses, for referral to relevant health-care professionals During training: start with/adapt social card with eligible local health-care professionals (dietitians/exercise programmes/coach) Explain during training that making use of the web-based tailored programme saves time of the midwife. Prepare midwives that further in pregnancy they need to invest some time to pay extra attention to GWG with their clients |
TTM, Transtheoretical Model; SCT, Social Cognitive Theory; ELM, Elaboration Likelihood Model; GWG, gestational weight gain; PA, physical activity.
Pregnant women
As described above, we focused on pregnant women’s awareness, knowledge, attitudes, social influences, self-efficacy expectations and barriers regarding weight gain within the IOM guidelines. Two models provided us with a theoretical foundation for motivation change: the Transtheoretical Model (TTM)( 52 ) and Social Cognitive Theory (SCT)( 53 ). TTM conceives a change as a process involving progress through five stages, starting with pre-contemplation and then moving to contemplation, preparation, action, with final arrival at the maintenance stage. For behavioural change purposes, the first stage needs to focus on raising one’s awareness, followed by providing knowledge and arguments in the second phase. During the preparation phase one needs to acquire practical information about behavioural change recognizing the value of social approval for strengthening intention to change. A critical feature of the action phase is the provision of information about the threats to the newly acquired behaviour( 52 ). SCT identifies the essential elements for behavioural change, including person–behaviour–environment interaction, behavioural capability (knowledge and skills), observational learning, reinforcements, expectations and self-efficacy( 53 ). Drawing on these theories we identified methods for change: consciousness raising (TTM), tailoring (TTM), individualization (TTM), active learning (SCT), self-re-evaluation (TTM), modelling (SCT), guided practice (SCT), verbal persuasion (SCT) and facilitation (SCT). In addition we drew on Goal Setting Theory (GST)( 54 ) to motivate change in self-efficacy expectations (Table 4).
We next developed practical strategies to apply these methods of change. For instance, computer tailoring was used to provide personalized information aimed at changes in awareness, attitudes, social influences and self-efficacy expectations. The tailoring programme included a self-monitoring device at different time points during pregnancy with visual feedback showing gaining below, within or above IOM guidelines. According to Bartholomew et al.( 18 ), tailoring will be effective if there is a clear link between the characteristics of the person and the messages that address those characteristics. We created short films to provide women with information aimed at changing social influences, self-efficacy expectations and the perception of barriers. In creating the videos we selected those role models that pregnant women could easily identify with. Regular face-to-face communication between the midwife and pregnant woman was intended to reinforce the client’s awareness, attitudes, social influences and self-efficacy expectations and to reduce the influence of barriers (Table 4).
Midwives
In designing the change strategies for midwives we again used the TTM( 52 ), SCT( 53 ) and a third model: the Elaboration Likelihood Model (ELM)( 55 ). The first two theories are explained above. Using the insights of TTM, we sought to increase midwives’ awareness of the problem of unhealthy GWG. Discussion, arguments, active learning and cooperative learning, methods derived from the SCT, were used to increase midwives’ knowledge, influence their attitudes, correct misconceptions and create a virtual client of the type that midwives were supposed to support during pregnancy. Information about others’ approval (SCT) was included to change midwives’ perceptions of the social norms of their colleagues. Finally, guided practice and planning coping responses (SCT) were used to help midwives become more familiar with the new programme and to help them to anticipate pregnant women’s objections to change.
The ELM suggests that people have two different ways of processing information: central and peripheral. Central processing occurs when a message is carefully considered and compared against other messages and beliefs. Peripheral processing occurs when a message is processed without thoughtful consideration and comparison( 55 ). According to Bartholomew et al.( 18 ) processing is related to higher persistence of attitude change, higher resistance to counter persuasion and a stronger consistency between attitude and behaviour. For this reason, central processing should be promoted as much as possible. Following the ELM recommendations, we derived three ways to stimulate a thoughtful approach to our message: make the message personally relevant, unexpected and repeat it regularly (Table 5).
Like we did with pregnant women, the methods chosen were combined into practical strategies. First, during training sessions midwives were informed about issues related to adequate GWG, in order to raise awareness of the problem and of their role as midwives as guardians of adequate GWG. Furthermore, the training included discussions (about participants’ experiences, facts, perceived barriers all related to GWG) and active learning (working with the tailoring programme, composing an individualized and regional overview of available health professionals they might consult). To support midwives’ face-to-face communication with pregnant women, an information sheet about healthy GWG and with suggestions about proper communication was developed (Table 5).
Step IV: Development of the intervention programme
Content of intervention
Our intervention – targeting both pregnant women and community midwives – was titled ‘Come On!’, a play on words (in Dutch) that refers to both GWG and to the need to do something.
Intervention component for pregnant women
For pregnant women we developed an online GWG programme, with the aim of informing pregnant women, in an early stage of pregnancy, about healthy GWG, healthy diet and physical activity, and providing ways to accomplish a healthy GWG. The first part of the programme consisted of a web-based, tailored programme, the completion of which took about 45 min. We tailored the programme based on pre-pregnancy BMI group (underweight, normal, overweight, obese), their TTM stages of change regarding achieving a healthy GWG, healthy diet and physical activity, and their need for information. Participants received an email with a link to the website and answered online questions on weight, height, struggles with their body weight, and knowledge of benefits and harms of too low or too high GWG. Information and tailored feedback was provided in next pages on the programme based on participants’ answers. Barriers to healthy diet were discussed when women indicated that those barriers existed. Depending on the woman’s pre-pregnancy BMI and her self-expressed weight gain goal, an ideal goal was suggested during the session. In addition, the programme included thirteen informational films on healthy GWG, pregnancy-related and healthy diet (i.e. advice on listeriosis, toxoplasmosis, intake of fish, fruits and vegetables) with an actor ‘Peggy’ in the role of health professional. Depending on answers given to questions about pre-pregnancy activities, a film on physical activity was shown. Inactive women were online, in the film, advised to become active and active women were encouraged to continue their active lifestyle. Active women performing a ‘high risk’ sport (e.g. diving, football) were advised to switch to an alternative ‘low risk’ sport (e.g. swimming, biking).
The second part of the online programme consisted of a monitoring tool. Women were invited to note their weight during their first visit and furthermore after invitation by email regularly. This invitation was sent weekly during the first ten weeks, biweekly in weeks 11 to 19, every third week in weeks 22 to 28, and at a gestational age of 32, 36 and 40 weeks. If a woman did not respond to an email invitation, she was not invited again.
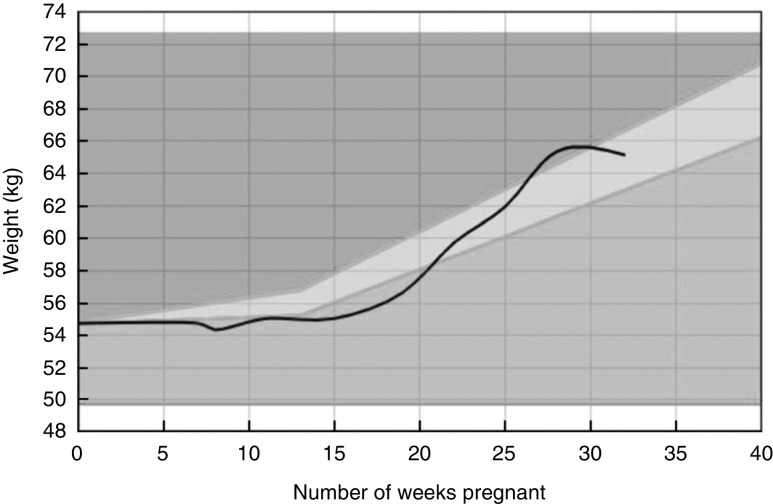
Figure 1 provides an example of an individualized graphical GWG growth curve adjusted to women’s pre-pregnancy BMI, indicating whether GWG was within, above or below the IOM guidelines. At each interval, participants received feedback plus the advice to discuss the feedback with their midwife. Each following visit to the programme ‘Come On!’, the woman was invited to watch one or more of the ten short films showing pregnant women dealing with recognizable situations. These films aimed to increase women’s awareness of healthy GWG and related behaviours (i.e. diet and physical activity), to demonstrate positive social support (e.g. from peers), to increase self-efficacy expectations (e.g. towards reaching healthy diet and healthy physical activity) and to suggest ways to overcome barriers (e.g. how to cope with cravings). Each short film lasted about 3 min. Films from the first session with ‘Peggy’ could be reviewed as well.
Fig. 1.
Example of an individualized graphical gestational weight gain (GWG) growth curve ( ) adjusted to women’s pre-pregnancy BMI, indicating whether GWG is within (
) adjusted to women’s pre-pregnancy BMI, indicating whether GWG is within ( ), above (
), above ( ) or below (
) or below ( ) the Institute of Medicine guidelines for a healthy GWG
) the Institute of Medicine guidelines for a healthy GWG
The online programme was illuminated with a consistent logo and illustrations to increase attractiveness. Written language was kept at a level appropriate for women with low and moderate levels of education.
Intervention component for midwives
The intervention component for midwives included training and an information card. Because some midwives delegate certain activities (e.g. intake interview, lifestyle education) to practice assistants, these assistants were invited for the training as well. Midwives/assistants received 4 h of training at a location in or nearby their working environment. The training was led by the first author (A.M.) who is experienced in professional education. In total the training was delivered ten times; sixty midwives and twelve assistants participated. At the start of the training, participants were invited to talk about their experiences and perceived problems in relation to GWG with the aim of raising awareness of appropriate GWG and of their care provided to achieve appropriate GWG. They received oral and written information on the IOM guidelines on GWG, the consequences of (un)healthy GWG, pregnant women’s behaviours related to GWG, the determinants of those behaviours, and the behaviours of Dutch midwives concerning GWG and the determinants of those behaviours. The goal was to make midwives aware of the gap between pregnant women’s needs and the current practice of midwives. The training introduced the online GWG programme for pregnant women. Finally, midwives were advised to discuss GWG at least once during antenatal care, to discuss healthy diet and physical activity, and to refer women to a dietitian and/or a physical activity programme for pregnant women. Midwives were instructed about the use of the information card, which included summarized information, arguments for referral to a dietitian, psychologist or physical activity programme, and suggestions for questions. During the training, midwives created a list of regional health-care workers they might refer their clients to or ask for advice. They were also encouraged to take a look at their own websites, in order to identify gaps in information about healthy lifestyles.
Step V: Development of an adoption and implementation plan
Because the ‘Come On!’ intervention is a newly developed programme, we followed the recommendation of Bartholomew et al. to include step V in the overall programme planning( 18 ). Consortium midwives functioned as intermediaries between developers and the final users (pregnant women and midwives) during steps I–IV. Building on a relationship of trust with their pregnant clients, midwives collect broad understanding of their clients. The consortium midwives and dietitian provided valuable information about relevant impeding and enhancing factors concerning implementation in midwifery practices. For instance, to minimize midwives’ time spent discussing healthy GWG, pregnant women can use the online ‘Come On!’ programme with minimal interference of the midwife, except for one single referral to the website. Midwives in the consortium consulted with their colleagues in the field about the relevant (important and changeable) determinants that formed the starting point for ‘Come On!’ and about selected practical strategies that were included. An essential part of ‘Come On!’ was the training for midwives, organized to inform them about the purpose and procedures of the intervention and to practise skills that were part of the intervention, and at the same time to facilitate adoption and implementation. The pilot test (step VI) of the intervention produced information from pregnant women and midwives about their experiences and appreciation of the programme, both of which were relevant for implementation.
Step VI: Development of an evaluation plan
The effect of ‘Come On!’ was evaluated in a non-randomized pre–post intervention study among pregnant women, comparing a historic control cohort (running May–August 2013) with an intervention cohort (running April–July 2014). First, consortium midwives recruited seventeen midwives. Then, the participating midwives were entrusted with the task of including pregnant women for the control cohort and the intervention cohort. Midwives or their practice assistants informed adult pregnant women with a singleton pregnancy about the study during the first telephone contact. If women were open to information about the study, their name and email address were collected and sent to the researcher (A.M.). The researcher then emailed the woman detailed information about the aim and procedures of the study. When the woman agreed to participate, she was invited to send a confirmation email to the researcher. Following this email, the researcher sent a link to the first digital questionnaire. Before their first antenatal visit to the midwife, and at about 36 weeks of pregnancy, pregnant women completed an online questionnaire that was similar to the questionnaire used in the needs assessment. Except for items on demographics in the first questionnaire (e.g. age, education), both questionnaires consisted of items on weight, diet and physical activity. For process evaluation purposes( 26 ), pregnant women from the intervention cohort answered questions related to exposure, use and appreciation of ‘Come On!’ in the second questionnaire. Likewise, the midwives answered questions related to the quality of the training, fidelity and dose of the programme delivered, usefulness of the ‘Come On!’ programme and barriers for use. Furthermore, the online programme reported user analytics about programme use. The Research Ethics Committee of Atrium-Orbis-Zuyd reviewed the study protocol and provided ethical approval (number 14-N-41). The trial study was registered in the Netherlands National Trial Register (NTR) under number NTR4717. We are in the process of presenting the results of this evaluation study.
Discussion and conclusion
The current paper presents a detailed outline of the process we used to develop ‘Come On!’, a programme intended to promote healthy GWG among healthy pregnant women. The needs assessment (intervention mapping step I) provided the information about personal and environmental factors related to GWG that was needed to formulate programme goals and specific change objectives. The use of a consortium of advisors, starting with the first step of intervention mapping, ensured that we took into account individual and environmental factors related to GWG, and that we continuously incorporated the adoption and implementation preferences of the intended users. The goal of the ‘Come On!’ programme was to make healthy pregnant women aware of an adequate GWG and to provide them with tools to help them stay within the IOM guidelines for healthy GWG. The web-based part could be used at any time, at any place, was widely accessible in a relatively inexpensive way, and allowed for tailoring, all of which are favourable for effective health promotion efforts( 56 , 57 ). The training for midwives fit with the current movement of lifelong learning( 58 ).
One of the challenges during the development process was to translate results of existing studies focusing on specific target groups (e.g. overweight, obese, diabetes) to our population of healthy pregnant women. We dealt with this through our quantitative study of healthy pregnant women from the practices of community midwives( 20 ) and through the continuous interaction between the developers and the consortium (midwives, dietitian), who provided insights into GWG-related behaviours, specific needs and applicability of selected strategies within our target groups. This interaction provided the empirical and theoretical foundation for the decision-making process.
Although we found intervention mapping to be useful, it was also time-consuming. Intervention mapping is typically applied to simple and unidimensional behaviours and can become unwieldy when applied to complex behaviours such as healthy GWG promotion( 59 ). During the needs assessment the complexity of GWG became clear, and use of intervention mapping resulted in the collection of a large and complex amount of information. Prioritizing based on impact and changeability resulted in the elimination of some relevant factors in favour of others judged to be more changeable and with a higher impact. The results of the effect and process evaluation studies will provide insights into the wisdom of these judgements (A Merkx, M Ausems, L Bude, et al., unpublished results).
We used a purposive sample of midwives and thus it is plausible that these midwives had above-average interest in issues regarding GWG and were highly motivated to find solutions. This may distort a realistic view of the factors and solutions related to the problem of healthy GWG. However, according to Roger’s Diffusion of Innovation Theory, the involvement of early adopters – an apt description of the consortium midwives – is necessary for the development and implementation of new initiatives( 18 , 60 ). Also the recruitment of participants for the effect study by the consortium midwives might have resulted in a study population that is not generalizable to the larger population of healthy pregnant women.
The ‘Come On!’ intervention was developed in a careful and comprehensive way. We look forward to the evaluation of the programme in a representative sample of pregnant women.
Acknowledgements
Financial support: This study is part of the research project ‘Promoting healthy pregnancy’, funded by Regional Attention and Action for Knowledge (RAAK PRO 2-014). RAAK is managed by the Foundation Innovation Alliance (SIA, Stichting Innovatie Alliantie) with funding from the Dutch Ministry of Education, Culture and Science (OCW). RAAK, SIA and OCW had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: A.M. is the first author and conducted the study. M.A. prepared and supervised the study and contributed to the writing process. R.d.V. is responsible for the whole study, supervised the study and edited the paper. M.N. is responsible for the study, prepared and supervised the study and edited the paper. Ethics of human subject participation: The Research Ethics Committee of Atrium-Orbis-Zuyd reviewed the study protocol and provided ethical approval (number 14-N-41). The trial study was registered in the Netherlands National Trial Register (NTR) under number NTR4717.
References
- 1. Rasmussen KM & Yaktine AL (2009) Weight Gain During Pregnancy, Reexamining the Guidelines. Washington, DC: Institute of Medicine. [PubMed] [Google Scholar]
- 2. Rauh K, Gabriel E, Kerschbaum E et al. (2013) Safety and efficacy of a lifestyle intervention for pregnant women to prevent excessive maternal weight gain: a cluster-randomized controlled trial. BMC Pregnancy Childbirth 13, 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hunt KJ, Alanis MC, Johnson ER et al. (2013) Maternal pre-pregnancy weight and gestational weight gain and their association with birthweight with a focus on racial differences. Matern Child Health J 17, 85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daemers DO, Wijnen HA, van Limbeek EB et al. (2013) Patterns of gestational weight gain in healthy, low-risk pregnant women without co-morbidities. Midwifery 29, 535–541. [DOI] [PubMed] [Google Scholar]
- 5. Campbell F, Johnson M, Messina J et al. (2011) Behavioural interventions for weight management in pregnancy: a systematic review of quantitative and qualitative data. BMC Public Health 11, 491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Currie S, Sinclair M, Murphy MH et al. (2013) Reducing the decline in physical activity during pregnancy: a systematic review of behaviour change interventions. PLoS One 8, e66385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dodd JM, Grivell RM, Crowther CA et al. (2010) Antenatal interventions for overweight or obese pregnant women: a systematic review of randomised trials. BJOG 117, 1316–1326. [DOI] [PubMed] [Google Scholar]
- 8. Furber CM, McGowan L, Bower P et al. (2013) Antenatal interventions for reducing weight in obese women for improving pregnancy outcome. Cochrane Database Syst Rev 1, CD009334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gardner B, Wardle J, Poston L et al. (2011) Changing diet and physical activity to reduce gestational weight gain: a meta-analysis. Obes Rev 12, e602–e620. [DOI] [PubMed] [Google Scholar]
- 10. Hill B, Skouteris H & Fuller-Tyszkiewicz M (2013) Interventions designed to limit gestational weight gain: a systematic review of theory and meta-analysis of intervention components. Obes Rev 14, 435–450. [DOI] [PubMed] [Google Scholar]
- 11. Muktabhant B, Lumbiganon P, Ngamjarus C et al. (2012) Interventions for preventing excessive weight gain during pregnancy. Cochrane Database Syst Rev 4, CD007145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ronnberg AK & Nilsson K (2010) Interventions during pregnancy to reduce excessive gestational weight gain: a systematic review assessing current clinical evidence using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system. BJOG 117, 1327–1334. [DOI] [PubMed] [Google Scholar]
- 13. Thangaratinam S, Rogozinska E, Jolly K et al. (2012) Interventions to reduce or prevent obesity in pregnant women: a systematic review. Health Technol Assess 16, iii–iv, 1–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thangaratinam S, Rogozinska E, Jolly K et al. (2012) Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ 344, e2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Renfrew MJ, McFadden A, Bastos MH et al. (2014) Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet 384, 1129–1145. [DOI] [PubMed] [Google Scholar]
- 16. Chief Nursing Officers of England, Northern Ireland, Scotland and Wales (2010) Midwifery 2020: Delivering Expectations. London: Midwifery 2020 Programme. [Google Scholar]
- 17. Stichting Perinatale Registratie (2013) Nederland Grote Lijnen 1999–2012 (Perinatal Care in the Netherlands 1999–2013). Utrecht: Stichting Perinatale Registratie. [Google Scholar]
- 18. Bartholomew L, Parcel G, Kok G et al. (2011) Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco, CA: Jossey-Bass. [Google Scholar]
- 19. Merkx A (2012) Gewichtstoename in de zwangerschap: een review en meta-analyse van interventies (Gestational weight gain: a review and meta-analyses of interventions). Presented at Symposium Passie voor Gezondheid (Passion for Health Symposium), Nederlands Congres VolksGeZondheid (NCVGZ), Amsterdam, 11 April 2012.
- 20. Merkx A, Ausems M, Bude L et al. (2015) Weight gain in healthy pregnant women in relation to pre-pregnancy BMI, diet and physical activity. Midwifery 31, 693–701. [DOI] [PubMed] [Google Scholar]
- 21. Merkx A, Ausems M, Bude L et al. (2015) Dutch midwives’ behaviour and determinants in promoting healthy gestational weight gain, phase 1: a qualitative approach. Int J Childbirth 5, 126. [Google Scholar]
- 22. Brug J, Oenema A & Ferreira I (2005) Theory, evidence and intervention mapping to improve behaviour nutrition and physical activity interventions. Int J Behav Nutr Phys Act 2, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Noar SM, Crosby R, Benac C et al. (2011) Application of the attitude–social influence–efficacy model to condom use among African-American STD clinic patients: implications for tailored health communication. AIDS Behav 15, 1045–1057. [DOI] [PubMed] [Google Scholar]
- 24. Temel S, Birnie E, Sonneveld HM et al. (2013) Determinants of the intention of preconception care use: lessons from a multi-ethnic urban population in the Netherlands. Int J Public Health 58, 295–304. [DOI] [PubMed] [Google Scholar]
- 25. Merkx A, Ausems M, Bude L et al. (2015) Dutch midwives’ behaviour and determinants in promoting healthy gestational weight gain, phase 2: a quantitative approach. Int J Childbirth 5, 139. [Google Scholar]
- 26. Steckler A & Linnan L (editors) (2002) Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey-Bass. [Google Scholar]
- 27. Hector D & Hebden L (2013) Prevention of Excessive Gestational Weight Gain: An Evidence Review to Inform Policy and Practice. Sydney: Physical Activity Nutrition & Obesity Research Group. [Google Scholar]
- 28. Althuizen E, van Poppel MN, Seidell JC et al. (2009) Correlates of absolute and excessive weight gain during pregnancy. J Womens Health (Larchmt) 18, 1559–1566. [DOI] [PubMed] [Google Scholar]
- 29. Yu Z, Han S, Zhu J et al. (2013) Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS One 8, e61627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zamora-Kapoor A & Walker L (2015) Excessive gestational weight gain in adolescent and adult pregnancies: an overlooked public health problem. J Pediatr 167, 515–517. [DOI] [PubMed] [Google Scholar]
- 31. Phelan S, Jankovitz K, Hagobian T et al. (2011) Reducing excessive gestational weight gain: lessons from the weight control literature and avenues for future research. Womens Health (Lond) 7, 641–661. [DOI] [PubMed] [Google Scholar]
- 32. Streuling I, Beyerlein A & von Kries R (2010) Can gestational weight gain be modified by increasing physical activity and diet counseling? A meta-analysis of interventional trials. Am J Clin Nutr 92, 678–687. [DOI] [PubMed] [Google Scholar]
- 33. Olander EK, Atkinson L, Edmunds JK et al. (2011) The views of pre- and post-natal women and health professionals regarding gestational weight gain: an exploratory study. Sex Reprod Healthc 2, 43–48. [DOI] [PubMed] [Google Scholar]
- 34. Stengel MR, Kraschnewski JL, Hwang SW et al. (2012) ‘What my doctor didn’t tell me’: examining health care provider advice to overweight and obese pregnant women on gestational weight gain and physical activity. Womens Health Issues 22, e535–e540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Van Rossum CTM, Fransen HP, Verkaik-Kloosterman J et al. (2011) Dutch National Food Consumption Survey 2007–2010: Diet of Children and Adults Aged 7 to 69 Years. Bilthoven: RIVM.
- 36. De Vries H, Dijkstra M, Kuhlman P et al. (1988) Self-efficacy: the third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health Educ Res 3, 273–282. [Google Scholar]
- 37. Szwajcer E, Hiddink G, Maas L et al. (2012) Nutrition awareness before and throughout different trimesters in pregnancy: a quantitative study among Dutch women. Fam Pract 29, Suppl. 1, i82–i88. [DOI] [PubMed] [Google Scholar]
- 38. Herring SJ, Oken E, Haines J et al. (2008) Misperceived pre-pregnancy body weight status predicts excessive gestational weight gain: findings from a US cohort study. BMC Pregnancy Childbirth 8, 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Herring SJ, Nelson DB, Davey A et al. (2012) Determinants of excessive gestational weight gain in urban, low-income women. Womens Health Issues 22, e439–e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Groth SW & Kearney MH (2009) Diverse women’s beliefs about weight gain in pregnancy. J Midwifery Womens Health 54, 452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Herring SJ, Henry TQ, Klotz AA et al. (2012) Perceptions of low-income African-American mothers about excessive gestational weight gain. Matern Child Health J 16, 1837–1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Herring SJ, Rose MZ, Skouteris H et al. (2012) Optimizing weight gain in pregnancy to prevent obesity in women and children. Diabetes Obes Metab 14, 195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Palmer JL, Jennings GE & Massey L (1985) Development of an assessment form: attitude toward weight gain during pregnancy. J Am Diet Assoc 85, 946–949. [PubMed] [Google Scholar]
- 44. Tovar A, Chasan-Taber L, Bermudez OI et al. (2010) Knowledge, attitudes, and beliefs regarding weight gain during pregnancy among Hispanic women. Matern Child Health J 14, 938–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Paul KH, Graham ML & Olson CM (2013) The web of risk factors for excessive gestational weight gain in low income women. Matern Child Health J 17, 344–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cogswell ME, Scanlon KS, Fein SB et al. (1999) Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstet Gynecol 94, 616–622. [DOI] [PubMed] [Google Scholar]
- 47. Stotland N, Tsoh JY & Gerbert B (2012) Prenatal weight gain: who is counseled? J Womens Health (Larchmt) 21, 695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stotland NE, Haas JS, Brawarsky P et al. (2005) Body mass index, provider advice, and target gestational weight gain. Obstet Gynecol 105, 633–638. [DOI] [PubMed] [Google Scholar]
- 49. Stotland NE, Gilbert P, Bogetz A et al. (2010) Preventing excessive weight gain in pregnancy: how do prenatal care providers approach counseling? J Womens Health (Larchmt) 19, 807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cramp AG & Bray SR (2009) A prospective examination of exercise and barrier self-efficacy to engage in leisure-time physical activity during pregnancy. Ann Behav Med 37, 325–334. [DOI] [PubMed] [Google Scholar]
- 51. Jans SM, de Jonge A, Henneman L et al. (2012) Attitudes of general practitioners and midwives towards ethnicity-based haemoglobinopathy-carrier screening. Eur J Hum Genet 20, 1112–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Prochaska J, Redding C & Evers K (2008) The transtheoretical model and stages of change. In Health Behaviour and Health Education: Theory, Research and Practice, 4th ed., pp. 97–121 [K Glanz, B Rimer and K Viswanath, editors]. San Francisco, CA: Jossey-Bass. [Google Scholar]
- 53. Bandura A (1986) Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- 54. Locke E & Latham G (1990) A Theory of Goal Setting and Task Performance. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- 55. Petty R & Caccioppo J (1986) Communication and Persuasion: Central and Peripheral Routes to Attitude Change. New York: Springer. [Google Scholar]
- 56. Bennett GG & Glasgow RE (2009) The delivery of public health interventions via the internet: actualizing their potential. Annu Rev Public Health 30, 273–292. [DOI] [PubMed] [Google Scholar]
- 57. Webb TL, Joseph J, Yardley L et al. (2010) Using the internet to promote health behaviour change: a systematic review and meta-analysis of the impact of theoretical basis, use of behaviour change techniques, and mode of delivery on efficacy. J Med Internet Res 12, e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. World Health Organization (2003) Nurses and Midwives: A Force for Health. WHO European Strategy for Continuing Education for Nurses and Midwives. Copenhagen: WHO Regional Office for Europe. [Google Scholar]
- 59. Kwak L, Kremers SP, Werkman A et al. (2007) The NHF-NRG In Balance-project: the application of intervention mapping in the development, implementation and evaluation of weight gain prevention at the worksite. Obes Rev 8, 347–361. [DOI] [PubMed] [Google Scholar]
- 60. Rogers E (1995) Diffusion of Innovations, 4th ed. New York: The Free Press. [Google Scholar]