Abstract
Objective
Dietary Ca is now being recognized to play an important role not only in skeletal integrity, but also in the regulation of energy and metabolism. The aim of the present study was to estimate the relationship of dairy Ca intake with BMI and blood pressure (BP) in a sample derived from the Polish population.
Design
Ca intake was calculated from an interviewer-administered semi-quantitative FFQ. BMI was calculated from measured weight and height, and BP was measured by a physician.
Setting
Cross-sectional epidemiological study on osteoporosis risk factors in Poland.
Subjects
Randomly selected healthy adult persons (n 1259; 750 women and 509 men).
Results
Dairy Ca intake was significantly lower in individuals with overweight/obesity (BMI≥25·00 kg/m2) and/or with elevated BP (systolic/diastolic ≥140/≥90 mmHg) than in those with normal body mass and BP, respectively. Ca intake was negatively correlated with BMI (r=−0·12, P<0·001), systolic BP (r=−0·11, P<0·001) and diastolic BP (r=−0·08, P<0·01). Daily dairy Ca intake below 1000 mg was a predictor for BMI≥25·0 kg/m2 (OR=1·44, P<0·005). This relationship was stronger in women, particularly premenopausal women.
Conclusions
The obtained results indicate the role of low dairy Ca intake in the development of obesity and hypertension, notably in premenopausal women.
Keywords: Calcium intake, Obesity, Hypertension
In recent years several published reports have suggested a new role for Ca, which seems not only to be a component of bone structure, a trigger for neurotransmitter release and a factor necessary for muscle contraction and blood coagulation, but also a regulator of energy and metabolism( 1 ). According to this concept, low dietary Ca intake may be involved in the pathogenesis of obesity( 2 ), hypertension( 3 – 5 ), insulin resistance and type 2 diabetes( 6 ). There are several data on the beneficial effects of Ca intake on the reduction of blood pressure (BP) in patients with hypertension( 3 – 5 ), on improving body composition( 7 ) and on lowering body weight( 1 ). It should be mentioned that data on the influence of dairy products on body mass loss are inconclusive and difficult to compare owing to different time intervals and sources of Ca (supplements v. diet). However, the results of a meta-analysis of twenty-nine clinical trials regarding the influence of dairy consumption on body mass and body fat did not support the favourable effect of increasing dairy consumption, yet showed modest benefits in facilitating body mass loss in short-term or energy-restricted randomized controlled trials( 8 ). The mechanism by which dairy food consumption may reduce body mass and improve body composition is not clear. Ca may enhance fecal excretion of fatty acids( 1 ), reduce appetite( 9 ) and increase energy loss( 1 , 9 ) by reducing lipogenesis and stimulating lipolysis, thermogenesis and lipid oxidation( 1 ). A hypothesis of the involvement of the Ca-sensing receptor (CaSR), detected in adipose tissue in the pathogenesis of obesity, was proposed( 9 ). Associations between Ca and obesity development may also be related to vitamin D deficiency in obese individuals( 10 ), especially since a close functional relationship between 1,25-dihydroxyvitamin D and the CaSR in adipocytes has been documented( 9 ). Activation of the CaSR in fat tissue can cause greater expression of lipogenic markers, lower expression of lipolytic enzymes and elevation of pro-inflammatory markers in visceral fat, all of which could contribute to the complications of obesity( 9 ).
There are some controversies regarding the influence of Ca intake on cardiovascular risk. On one hand, a reduction of BP in patients with hypertension consuming a Ca-rich diet was shown( 3 – 5 ); on the other, administration of Ca supplements was related to an increased risk of myocardial infarction when taken alone without vitamin D( 11 ). Low Ca supply induces compensatory elevation of parathyroid hormone and 1,25-dihydroxyvitamin D, contributing to BP increase. 1,25-Dihydroxyvitamin D elevates Ca concentration in vascular smooth muscle cells, increasing peripheral vascular resistance and BP( 12 ), being also a negative regulator of the renin–angiotensin system( 13 ). Moreover, elevated parathyroid hormone concentration also has been associated with hypertension( 14 ).
The aim of the present study was to evaluate the associations of Ca intake with BMI and BP in a randomized sample of the Polish population in participants derived from the EPOLOS study.
Materials and methods
Study design
EPOLOS was a cross-sectional epidemiological study on osteoporosis risk factors in Poland. Polish citizens aged 20–80 years were randomly selected on the basis of personal identity number (PESEL) from the registry of the Department of National Registry of the Polish Ministry of Home Affairs and Administration. Selected citizens received a letter with an invitation to participate in the study and explanation of its goals. Those who were interested were called to the research centre, where, after explanation of any doubts, they signed an informed consent to participate in the study (n 1603). The exclusion criteria were a documented history of osteoporosis and other metabolic bone diseases, pregnancy, cancer and fracture(s) experienced in the previous year. We included in the present investigation the data from individuals who did not use Ca supplements/medications, were not treated for hypertension and had completed anthropometric, BP and Ca intake measurements. Finally, 1259 individuals (750 women and 509 men) were included in the present study.
Calcium intake assessment
Ca intake was estimated with a semi-quantitative method that measured food consumption frequency based on the intake of Ca in dairy products, according to the data gathered in an FFQ( 15 , 16 ). The questionnaire allowed dietary Ca intake to be assessed on the basis of the Ca content in twenty-one different types of food most common in Poland and the frequency of eating. The products included milk (in beverages and soups), different types of cheese (rennet, cottage, cream, processed), yoghurt and ice cream. Ca content in particular dairy products was determined by means of the Polish database of nutritional values of food products( 17 ). Standard measurement error of the FFQ calculated on the basis of fifty measurements (two for each patient with repetition within the period of 6 weeks) was 200 mg Ca and the median difference between the two estimations of daily Ca intake was 14 %. The FFQ was administered by an experienced interviewer.
Other measurements
Each participant was weighed and measured by means of a weighing scale/height measure, then BMI was calculated and classified by the WHO criteria( 18 ). Office BP was measured by a physician with a standard aneroid manometer according to the standards of the European Society of Hypertension Working Group on Blood Pressure Monitoring( 19 ). We recognized BP as elevated when systolic BP was ≥140 mmHg and/or diastolic BP was ≥90 mmHg.
Statistical analyses
The Kolmogorov–Smirnov test was used for checking the distribution of variables. Non-parametric statistics were used, with median and quartiles (Q1–Q3) presented. Significance of the differences between the analysed quantitative variables among particular groups was assessed with the Mann–Whitney U test and Kruskal–Wallis ANOVA. Associations of Ca intake with BMI and BP were investigated with Spearman’s correlation coefficient. Odds ratios were calculated based on 2×2 contingency tables. The χ 2 test or Fisher’s statistic was used, depending on the sample size; P<0·05 was considered statistically significant. Calculations were performed by means of the software Statistica 10 PL (StatSoft Inc., Tulsa, OK, USA).
Results
Data from 1259 participants (750 women and 509 men) were included in the analysis. Characteristics of the studied population are presented in Table 1. Elevated BP was found in 25·9 % of the investigated population and 56·1 % were overweight or obese. Median Ca intake from dairy products in the studied group was low, 816 (525–1065) mg; higher values were present in younger participants and in women, the lowest value was observed in the group of men over 50 years old (Table 1).
Table 1.
Characteristics of the investigated randomized sample of Polish citizens aged 20–80 years (n 1259)
| Women | Men | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Whole population (n 1259) | All women(n 750) | Premenopausal women (n 421) | Postmenopausal women (n 329) | All men (n 509) | Men aged <50 years (n 228) | Men aged ≥50 years (n 281) | ||||||||
| Median | Q1–Q3 | Median | Q1–Q3 | Median | Q1–Q3 | Median | Q1–Q3 | Median | Q1–Q3 | Median | Q1–Q3 | Median | Q1–Q3 | |
| Age (years) | 49·4 | 36·7–60·9 | 47·9 | 35·7–60·2 | 37·3 | 29·09–44·2 | 61·68 | 55·5–69·7 | 51·9 | 39·0–63·1 | 37·23 | 19·5–49·9 | 61·6 | 55·6–68–9 |
| BMI (kg/m2) | 26·0 | 22·6–28·8 | 25·0 | 21·9–28·7 | 22·9 | 20·6–25·9 | 28·0 | 24·8–31·1 | 26·6 | 24·0–29·0 | 25·6 | 17·1–38·9 | 27·4 | 24·8–29·5 |
| Systolic BP (mmHg) | 130 | 12–140 | 120 | 115–140 | 120 | 110–130 | 140 | 120–150 | 130 | 120–145 | 123 | 120–135 | 140 | 120–150 |
| Diastolic BP (mmHg) | 81 | 75–90 | 80 | 70–86 | 77 | 70–80 | 80 | 80–90 | 85 | 80–90 | 84 | 80–90 | 85 | 80–90 |
| Ca intake (mg/d) | 816 | 500–1049 | 772 | 525–1065 | 804 | 568–1102 | 731 | 463–1017 | 724 | 467–1026 | 798 | 525–1180 | 668 | 427–959 |
Q1, first quartile; Q3, third quartile; BP, blood pressure.
Analysis of relationship between calcium intake and BMI
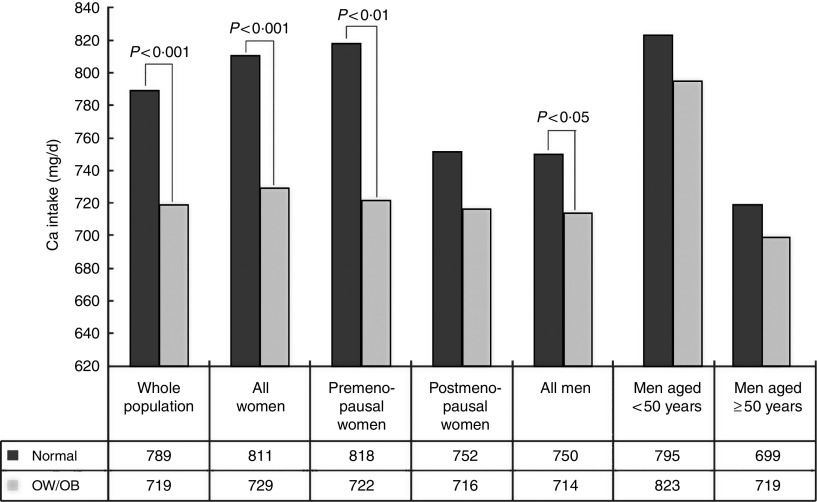
We demonstrated significantly lower daily Ca intake from dairy products in participants who were overweight and obese (BMI≥25·00 kg/m2) compared with participants with normal BMI (719 (464–1006) v. 789 (551–1113) mg, P<0·001; Fig. 1). Analysing Ca intake in BMI ranges we observed in the whole population a statistically significant difference between the group with normal BMI (18·50–24·99 kg/m2) and the overweight/obese group (Fig. 2(a)). We also showed a weak, however significantly negative correlation between daily Ca intake and BMI (r=−0·11, P<0·001) in the whole population.
Fig. 1.
Median calcium intake from dairy products in the randomized sample of Polish citizens aged 20–80 years (n 1259), according to population group and BMI (normal, BMI=18·50–24·99 kg/m2; overweight/obese, BMI≥25·00 kg/m2). Median Ca intake was significantly different between normal BMI and overweight/obese groups (OW/OB): P<0·001 (for the whole population and all women), P<0·01 (for premenopausal women), P<0·05 (for all men)
Fig. 2.
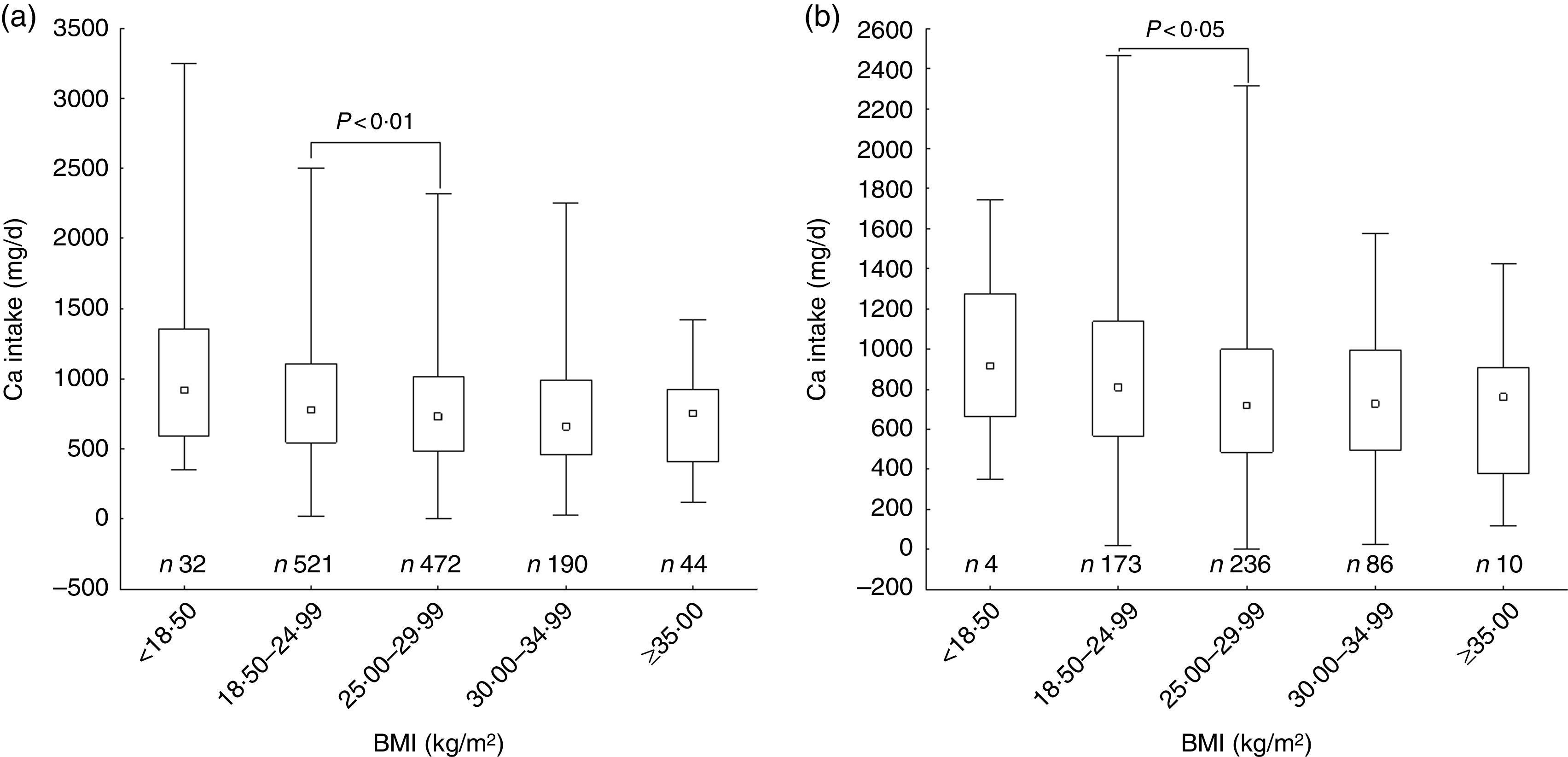
Box-and-whisker plots showing calcium intake from dairy products in the randomized sample of Polish citizens aged 20–80 years (n 1259), according to BMI, in (a) the whole population and (b) all women. The small square within the box represents the median; the bottom and top edges of the box represent the first quartile (Q1) and third quartile (Q3), respectively; and the ends of the bottom and top whiskers represent the minimum and maximum values, respectively. Median Ca intake was significantly different between the normal group (BMI=18·50–24·99 kg/m2) and the overweight/obese group (BMI≥25·00 kg/m2): P<0·01 (for the whole population), P<0·05 (for all women)
The analysis according to gender revealed significantly lower Ca intake in overweight and obese women (BMI≥25·00 kg/m2) than in women with normal BMI (729 (484–990) v. 811 (568–1133) mg, P<0·001; Fig. 1) and a negative correlation between dietary Ca and BMI (r=−0·15, P<0·001). When we analysed Ca intake in BMI ranges among women, we observed in all women a statistically significant difference between the group with normal BMI (18·50–24·99 kg/m2) and the overweight/obese group (Fig. 2(b)). When pre- and postmenopausal women were analysed separately, a statistically significant difference was found only in the premenopausal women; similarly, a negative correlation between Ca intake and BMI was present only in the premenopausal women (r=−0·18, P<0·001). For postmenopausal women, that relationship was not statistically significant (r=−0·04, P=0·50).
Dietary Ca was lower in overweight and obese men (BMI≥25·00 kg/m2) than in men with normal BMI (714 (432–972) v. 750 (520–1063) mg, P<0·05; Fig. 1). In men there was no statistically significant difference in Ca intake according to BMI ranges. No correlation was found between Ca intake and BMI in men (r=−0·06, P=0·16). Correlations of Ca intake and BMI are shown in Table 2.
Table 2.
Correlations of calcium intake with BMI and blood pressure (BP) among the randomized sample of Polish citizens aged 20–80 years (n 1259)
| n | r | P | |
|---|---|---|---|
| Correlation between Ca intake and BMI | |||
| Whole population | 1259 | –0·12 | <0·001 |
| All men | 509 | –0·06 | 0·16 |
| All women | 750 | –0·15 | <0·001 |
| Premenopausal women | 421 | –0·18 | <0·001 |
| Postmenopausal women | 329 | –0·04 | 0·50 |
| Correlation between Ca intake and systolic BP | |||
| Whole population | 1259 | –0·11 | <0·001 |
| All women | 750 | –0·12 | <0·001 |
| All men | 509 | –0·07 | <0·05 |
| Correlation between Ca intake and diastolic BP | |||
| Whole population | 1259 | –0·08 | <0·01 |
| All Women | 750 | –0·08 | <0·05 |
r, Spearman’s correlation coefficient.
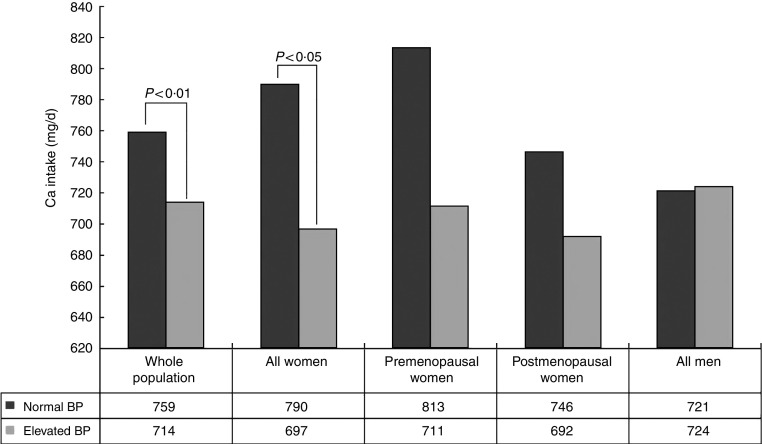
Analysis of relationship between calcium intake and blood pressure
In the whole population, participants with elevated BP had Ca intake from dairy products that was significantly lower than in participants with normal BP (714 (460–993) v. 759 (518–1079) mg, P<0·001; Fig. 3). Moreover, a weak but significantly negative correlation between BP and Ca intake was found (r=−0·11, P<0·001). Correlations of Ca intake and BP are shown in Table 2.
Fig. 3.
Median calcium intake from dairy products in the randomized sample of Polish citizens aged 20–80 years (n 1259), according to population group and blood pressure (BP). Median Ca intake was significantly different between the group with normal BP (systolic/diastolic <140/<90 mmHg) and elevated BP (systolic/diastolic ≥140/≥90 mmHg): P<0·01 (for the whole population), P<0·05 (for all women)
In all women with elevated BP, median Ca intake from dairy products was significantly lower compared with all women with normal BP (697 (468–944) v. 790 (541–1097) mg, P<0·05; Fig. 3). A negative correlation between Ca intake and BP was also present in all women (r=−0·12, P<0·001). Postmenopausal women had higher BP than premenopausal women (P<0·001). In premenopausal women with normal BP the median Ca intake was slightly higher than in women with elevated BP (813 v. 711 mg), but the difference was not statistically significant (P=0·10). However, in the investigated group of premenopausal women, only thirty-six had elevated BP. On the contrary, median Ca intake was similar in both groups of all men with and without elevated BP (721 (422–1023) v. 724 (486–1028) mg, P=0·33; Fig. 3). In all men, only a slight tendency to correlation between Ca intake and systolic BP was shown (Table 2).
Moreover, a strong positive correlation between age and BMI was demonstrated (r=0·44, P<0·001 for the whole population; r=0·53, P<0·001 for all women; r=0·24, P<0·001 for all men) when subgroups were analysed separately.
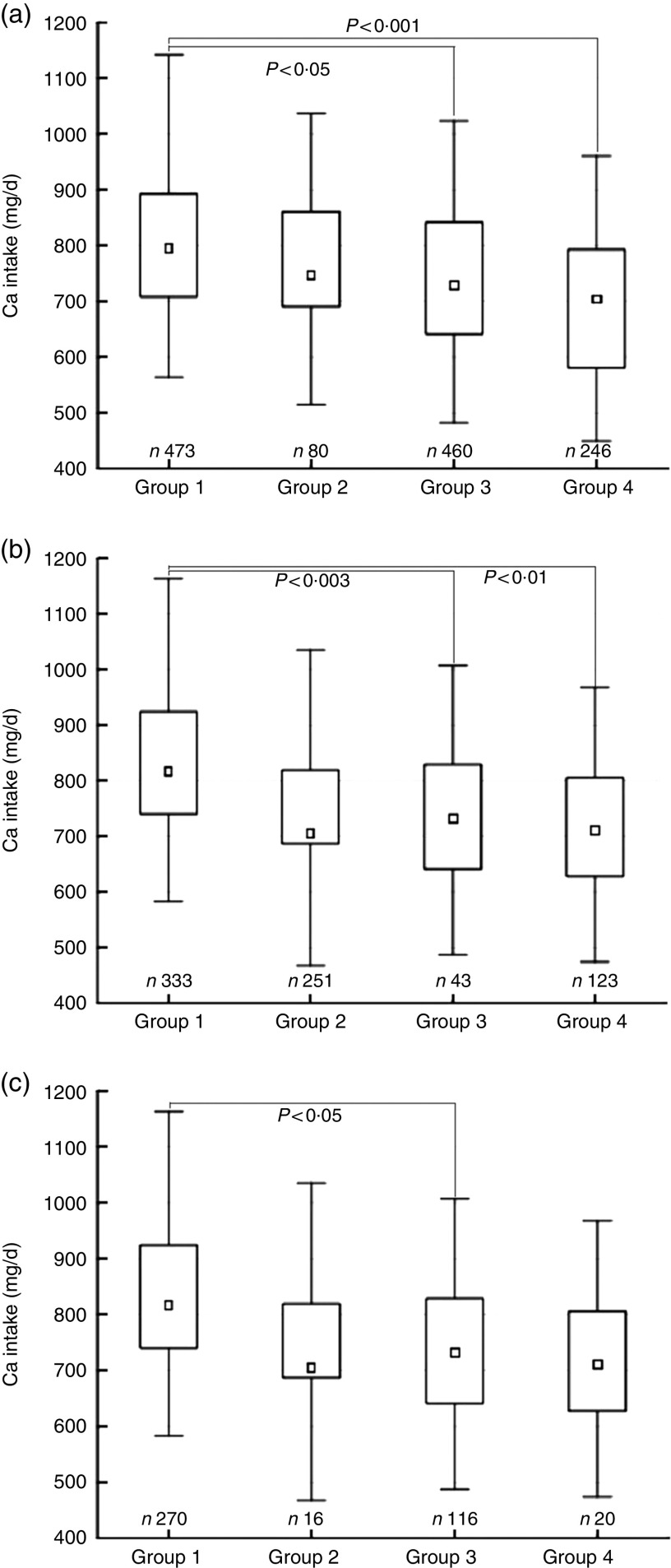
Analysis of influence of calcium intake on both overweight and hypertension
We compared Ca intake from dairy products among four groups: Group 1 with normal BMI (18·50–24·99 kg/m2) and normal BP (systolic/diastolic <140/<90 mmHg; n 473); Group 2 with normal BMI and elevated BP (systolic/diastolic ≥140/≥90 mmHg; n 80); Group 3 with overweight/obesity and normal BP (n 460); and Group 4 with overweight/obesity and elevated BP (n 246). We found significantly lower Ca intake in Group 3 and Group 4 v. Group 1; this relationship was present for the whole population (Fig. 4(a)) and for all women (Fig. 4(b)). In premenopausal women, we noticed a significant difference in Ca intake only for the subgroup that was overweight/obese with normal BP (Fig. 4(c)); however, the small size of Groups 3 and 4 in premenopausal women is a limitation.
Fig. 4.
Box-and-whisker plots showing calcium intake from dairy products in the randomized sample of Polish citizens aged 20–80 years (n 1259), according to BMI and blood pressure (BP) groups, in (a) the whole population, (b) all women and (c) premenopausal women. The small square within the box represents the median; the bottom and top edges of the box represent the first quartile (Q1) and third quartile (Q3), respectively; and the ends of the bottom and top whiskers represent the minimum and maximum values, respectively. Group 1, normal BMI (18·50–24·99 kg/m2) and normal BP (systolic/diastolic <140/<90 mmHg); Group 2, normal BMI and elevated BP (systolic/diastolic ≥140/≥90 mmHg); Group 3, overweight/obese (BMI≥25·00 kg/m2) and normal BP; Group 4, overweight/obese and elevated BP. Median Ca intake was significantly different according to BMI and BP groups: P<0·001 between Group 1 and Group 4, P<0·05 between Group 1 and Group 3 (for the whole population); P<0·01 between Group 1 and Group 4, P<0·003 between Group 1 and Group 3 (for all women); P<0·05 between Group 1 and Group 3 (for premenopausal women)
Low Ca intake (<1000 mg) was a predictor for overweight and obesity (BMI≥25·00 kg/m2) in the whole population (OR=1·44, P<0·005) and in all women (OR=1·66, P<0·005), but not in all men (OR=1·13, P=0·55; Table 3).
Table 3.
Odds ratios for overweight and obesity (BMI≥25·00 kg/m2) in participants with low calcium intake (<1000 mg/d) among the randomized sample of Polish citizens aged 20–80 years (n 1259)
| OR | 95 % CI | P | |
|---|---|---|---|
| Whole population | 1·44 | 1·12, 1·86 | <0·005 |
| All women | 1·66 | 1·20, 2·30 | <0·005 |
| Premenopausal women | 1·94 | 1·14, 3·29 | <0·05 |
| Postmenopausal women | 1·56 | 0·97, 2·51 | 0·062 |
| All men | 1·13 | 0·75, 1·71 | 0·55 |
Low Ca intake (<1000 mg) was a predictor for hypertension only in women (OR=1·50, P<0·05); odds ratios for the whole population and premenopausal women were on the border of statistical significance (Table 4).
Table 4.
Odds ratios for hypertension (systolic/diastolic blood pressure ≥140/≥90 mmHg) in participants with low calcium intake (<1000 mg/d) among the randomized sample of Polish citizens aged 20–80 years (n 1259)
| OR | 95 % CI | P | |
|---|---|---|---|
| Whole population | 1·33 | 0·99, 1·76 | 0·055 |
| All women | 1·50 | 1·01, 2·23 | 0·046 |
| Premenopausal women | 2·40 | 0·98, 5·99 | 0·059 |
| Postmenopausal women | 1·20 | 0·73, 1·99 | 0·45 |
| All men | 1·12 | 0·73, 1·71 | 0·6 |
Discussion
Obesity is a multifactorial disease which is most frequently associated with incorrect habits, mainly overeating. Inappropriate diet in obese people is not only a problem of quantity, but also a problem of quality of food. In many obese patients diet is unbalanced, with high energy intake paralleled by insufficient micronutrient intake( 20 ). Micronutrient deficiencies, among others low Ca intake, have been reported in several studies( 20 – 24 ). Our study, performed on a large group of randomly selected persons, demonstrates a relationship between low Ca intake from dairy foods and obesity. Until now, only a few studies investigating the influence of Ca intake on obesity and its complications have been published in Poland( 21 – 24 ) and very few elsewhere( 2 , 6 , 8 ). In the Polish population, low Ca intake has been demonstrated in individuals with morbid obesity being prepared for a bariatric surgery( 21 ), in obese patients with insulin resistance( 22 ), moreover in patients with hypertension( 23 ) and in men with CVD( 24 ). However, in those studies the number of participants was small and Ca intake was investigated in groups with significant metabolic abnormalities. In contrast, the data from our study are derived from a general population of Polish volunteers.
We observed significantly lower Ca intake from dairy products in the group of participants with high BMI and hypertension. We showed also that Ca deficiency in the diet is a predictor for development of overweight and obesity. The association is not very strong, but statistically significant and potentially modifiable. Our analysis according to gender showed that this relationship was stronger in women than in men, although in women Ca intake was higher. What is surprising, a stronger influence of low Ca intake was present in premenopausal women. The mentioned relationship was noticed despite the fact that obesity and hypertension belong to age-related diseases and greater Ca deficiency was demonstrated in postmenopausal women. In the light of these data, the premenopausal group seems to be metabolically more sensitive to Ca deficiency. Such special sensitivity of premenopausal women was also observed in the Portuguese population by Marques-Vidal et al., who showed a slight negative correlation between Ca intake and BMI in premenopausal women and found a lack of this relationship in older women( 25 ). However, an opposite result was shown in a study from Korea; in that investigation, Ca intake was inversely associated with the risk of metabolic syndrome in the group of postmenopausal but not premenopausal women( 26 ). Other manifestations of the harmful effect of low Ca in the diet of premenopausal women may also include higher frequency of colon and breast cancer in young women who declare reduced dietary Ca intake( 27 , 28 ). Moreover, the preventive role of Ca supplementation in hypertensive disorders during pregnancy has been demonstrated( 5 ). It should be noted that in our study the median of Ca intake from dairy foods was higher in premenopausal women with normal BP when compared with women with elevated BP, but the difference did not reach statistical significance, probably due to a small number with elevated BP in the group of premenopausal women.
The clinical significance of our study is related to a high frequency of occurrence in the Polish population of both epidemiological phenomena: low dietary Ca and obesity and their metabolic consequences, i.e. hypertension, diabetes mellitus and CVD. The problem of low dietary Ca intake in Europe, Poland included, has been confirmed repeatedly( 29 – 31 ). However, so far low dietary Ca has rather been associated with a higher risk of osteoporosis development and fractures, but not with obesity. Data from 2011, derived from the Central Statistical Office of Poland, show that 54 % of the Polish population is overweight or obese( 32 ) and about 25 % suffers from hypertension( 33 ); the data are similar to the prevalence of obesity and elevated BP in our investigated population, which supports the assumption that the investigated sample is representative for the Polish population.
Relationships between BP and Ca intake from dairy in our study were statistically significant, but weak, which may be a consequence of excluding from the study patients treated for hypertension, and appeared clearer when we analysed hypertension with elevated BMI.
We are aware of our study’s limitations. In our study Ca was measured only in dairy products. However, dairy products are the most important sources of Ca in the diet, providing about 70 % of daily Ca intake( 15 ); thus, dietary Ca depends predominantly on its intake from dairy products. A previous study showed that the quantity of Ca coming from non-dairy products in the Polish population can be regarded as being quite constant, amounting to about 250 mg/d( 16 ). Polish data indicate that dairy products are the main source of Ca in the diet because of their high content of elemental Ca, high absorption rate and low cost; they are also an important element of Polish food tradition. Moreover, Ca-enriched non-dairy food is not popular in Poland.
In our study total energy intake was not taken into account. Although including data on energy intake might be useful( 34 ), some pitfalls in interpretation of energy intake data in epidemiological studies have been mentioned( 35 ). The present study, however, was not designed to address this particular issue, as our data are derived from an osteoporosis investigative unit. Furthermore, the lowest Ca intake was found in the group of obese and hypertensive participants. Although theoretically possible, it is, however, rather unlikely that this group would have a lower food intake in comparison to the other subgroups, leading to an overall lower Ca intake. There are, however, some data suggesting that daily metabolizable energy intake might be lower in the obese than in the non-obese( 36 ), yet energy intake per unit of lean body mass (kilojoules per gram of urinary creatinine) was constant regardless of the degree of obesity and was essentially the same as that of non-obese persons( 37 ).
A low dairy Ca intake also indicates a low intake of other biologically active factors that impact obesity and hypertension, not only Ca intake alone. We did not investigate any influence on BMI and BP of the other factors present in dairy products that were the basic dietary source of Ca in our study. A list of such biologically effective substances contains K, Mg, riboflavin, folate, vitamins E and D; such trace minerals as iodine, Se and Zn; and many proteins (whey and casein), branched-chain amino acids and peptides( 38 ).
Strengths of the present study include an investigation carried out on a large group of randomly selected individuals, seeming to be representative enough for the Polish population.
Many factors, both environmental and genetic, affect body mass, but only some of them can be modified; dietary Ca intake belongs to that group. Results of our study allow to introduce qualitative dietary changes in addition to routine energy restriction in diets to reduce body mass and consideration of fortifying foods with Ca, what was shown be effective and safe in a Finnish population( 39 ). However, introducing a formal recommendation should be preceded by the results of intervention studies.
Conclusion
The obtained results indicate a role for low dairy Ca intake in the development of obesity and hypertension in Polish adults, mainly in premenopausal women. It supports the hypothesis about the influence of dietary Ca on the pathogenesis of obesity and hypertension, and can be used to propose a diet effectively reducing body mass and BP in the affected participants.
Acknowledgements
Acknowledgements: The authors would like to thank Professors Edward Czerwiński, Andrzej Milewicz, Marek Spaczyński and Ewa Marcinowska-Suchowierska for their overall contribution in realization of the EPOLOS study in Kraków, Wrocław, Poznań and Warszawa. Financial support: The EPOLOS study was funded by the Polish Ministry of Health and the Committee of Scientific Research (grant number 2483/CP05-4/99). The Polish Ministry of Health and the Committee of Scientific Research had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: E.S.-J. conceived the idea of the present study, participated in collecting of data at Łódź Centre of the EPOLOS study and prepared the manuscript. M.J. analysed data and undertook the statistical analysis. R.L. designed and conducted the EPOLOS study. M.K.-L. provided advice on the analysis process and mentored writing of the manuscript. A.L. conducted the EPOLOS study at Łódź Centre, and as senior author supervised the final version of the manuscript. All authors provided critical inputs, contributed to the final article and approved its contents. Ethics of human subject participation: The present study was approved by Ethics Committee of The Children’s Memorial Health Institute at Warsaw.
References
- 1. Zemel MB, Shi H, Greer B et al. (2000) Regulation of adiposity by dietary calcium. FASEB J 4, 1132–1138. [PubMed] [Google Scholar]
- 2. Lind L, Lithell H, Hvarfner A et al. (1993) The relationships between mineral metabolism, obesity and fat distribution. Eur J Clin Invest 23, 307–310. [DOI] [PubMed] [Google Scholar]
- 3. Hilpert KF, West SG, Bagshaw DM et al. (2009) Effects of dairy products on intracellular calcium and blood pressure in adults with essential HTN. J Am Coll Nutr 28, 142–149. [DOI] [PubMed] [Google Scholar]
- 4. Ruidavets JB, Bongard V, Simon C et al. (2006) Independent contribution of dairy products and calcium intake to blood pressure variations at a population level. J Hypertens 24, 671–681. [DOI] [PubMed] [Google Scholar]
- 5. Hofmeyr GJ, Lawrie TA, Atallah AN et al. (2014) Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev 6, CD001059. [DOI] [PubMed] [Google Scholar]
- 6. Tremblay A & Gilbert JA (2009) Milk products, insulin resistance syndrome and type 2 diabetes. J Am Coll Nutr 28, Suppl. 1, 91S–102S. [DOI] [PubMed] [Google Scholar]
- 7. Larsen SC, Ängquist L, Ahluwalia TS et al. (2014) Interaction between genetic predisposition to obesity and dietary calcium in relation to subsequent change in body mass and waist circumference. Am J Clin Nutr 99, 957–965. [DOI] [PubMed] [Google Scholar]
- 8. Chen M, Pan A, Malik VS et al. (2012) Effects of dairy intake on body mass and fat: a meta-analysis of randomized controlled trials. Am J Clin Nutr 96, 735–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Villarroel P, Villalobos E, Reyes M et al. (2014) Calcium, obesity, and the role of the calcium-sensing receptor. Nutr Rev 72, 627–637. [DOI] [PubMed] [Google Scholar]
- 10. Liel Y, Ulmer E, Shary J et al. (1988) Low circulating vitamin D in obesity. Calcif Tissue Int 43, 199–201. [DOI] [PubMed] [Google Scholar]
- 11. Bolland MJ, Avenell A, Baron JA et al. (2010) Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 341, c3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shan J, Resnick LM, Lewanczuk RZ et al. (1993) 1,25-Dihydroxyvitamin D as a cardiovascular hormone. Effects on calcium current and cytosolic free calcium in vascular smooth muscle cells. Am J Hypertens 6, 983–988. [DOI] [PubMed] [Google Scholar]
- 13. Li YC, Kong J, Wei M et al. (2002) 1,25-Dihydroxyvitamin D3 is a negative endocrine regulator of the renin–angiotensin system. J Clin Invest 110, 229–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Young EW, McCarron DA & Morris CD (1990) Calcium regulating hormones in essential hypertension: importance of gender. Am J Hypertens 3, 8 Pt 2, 161S–166S. [DOI] [PubMed] [Google Scholar]
- 15. Gonnelli S, Rossi S, Montomoli M et al. (2009) Accuracy of different reduced versions of a validated food-frequency questionnaire in Italian men and women. Calcif Tissue Int 85, 221–227. [DOI] [PubMed] [Google Scholar]
- 16. Szymelfejnik EJ, Wądołowska L, Cichon R et al. (2006) Dairy products frequency questionnaire (ADOS-Ca) calibration for calcium intake evaluation. Pol J Food Nutr Sci 15, 229–236. [Google Scholar]
- 17. Kunachowicz H, Nadolna J, Iwanow K et al. (1997) The Nutritional Value of Some Foods and Typical Dishes. Warsaw: Wyd. PZWL (in Polish). [Google Scholar]
- 18. World Health Organization (2000) Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. WHO Technical Report Series no. 894. Geneva: WHO. [PubMed] [Google Scholar]
- 19. O’Brien E, Asmar R, Beilin L et al.; European Society of Hypertension Working Group on Blood Pressure Monitoring (2003) European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 21, 821–848. [DOI] [PubMed] [Google Scholar]
- 20. Correia Horvath JD, Dias de Castro ML, Kops N et al. (2014) Obesity coexists with malnutrition? Adequacy of food consumption by severely obese patients to dietary reference intake recommendations. Nutr Hosp 29, 292–299. [DOI] [PubMed] [Google Scholar]
- 21. Jastrzębska-Mierzyńska M, Ostrowska L, Hady HR et al. (2012) Assessment of dietary habits, nutritional status and blood biochemical parameters in patients prepared for bariatric surgery: a preliminary study. Wideochir Inne Tech Malo Inwazyjne 7, 156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Suliburska J, Bogdański P, Pupek-Musialik D et al. (2011) Dietary intake and serum and hair concentrations of minerals and their relationship with serum lipids and glucose levels in hypertensive and obese patients with insulin resistance. Biol Trace Elem Res 139, 137–150. [DOI] [PubMed] [Google Scholar]
- 23. Suliburska J, Bogdański P, Duda G et al. (2012) An assessment of dietary intake and state of nutritional in hypertensive patients from rural and urban areas of Greater Poland. Ann Agric Environ Med 19, 339–343. [PubMed] [Google Scholar]
- 24. Anyzewska A, Wawrzyniak A, Wozniak A et al. (2013) Nutritional assessment in Polish men with cardiovascular diseases. Rocz Panstw Zakl Hig 64, 211–215. [PubMed] [Google Scholar]
- 25. Marques-Vidal P, Gonçalves A & Dias CM (2006) Milk intake is inversely related to obesity in men and in young women: data from the Portuguese Health Interview Survey 1998–1999. Int J Obes (Lond) 30, 88–93. [DOI] [PubMed] [Google Scholar]
- 26. Cho GJ, Park HT, Shin JH et al. (2009) Calcium intake is inversely associated with metabolic syndrome in postmenopausal women: Korea National Health and Nutrition Survey, 2001 and 2005. Menopause 16, 992–997. [DOI] [PubMed] [Google Scholar]
- 27. Massa J, Cho E, Orav EJ et al. (2014) Total calcium intake and colorectal adenoma in young women. Cancer Causes Control 25, 451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hjartåker A, Thoresen M, Engeset D et al. (2010) Dairy consumption and calcium intake and risk of breast cancer in a prospective cohort: the Norwegian Women and Cancer study. Cancer Causes Control 21, 1875–1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Skowrońska-Jóźwiak E, Jaworski M, Grzywa A et al. (2014) Influence of calcium intake on bone mineral density and fractures incidence in the treatment-naive women from Lodz urban area – part of EPOLOS study. Ann Agric Environ Med 21, 201–204. [PubMed] [Google Scholar]
- 30. Bruyere O, De Cock C, Mottet C et al. (2009) Low dietary calcium in European postmenopausal osteoporotic women. Public Health Nutr 12, 111–114. [DOI] [PubMed] [Google Scholar]
- 31. Włodarek D, Głąbska D, Kołota A et al. (2014) Calcium intake and osteoporosis: the influence of calcium intake from dairy products on hip bone mineral density and fracture incidence – a population-based study in women over 55 years of age. Public Health Nutr 17, 383–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Central Statistical Office of Poland (2012) Health and health care in 2011 (in Polish) http://stat.gov.pl/cps/rde/xbcr/gus/zo_zdrowie_i_ochrona_zdrowia_w_2011.pdf (accessed November 2016).
- 33. Janszky I, Vatten L, Romundstad P et al. (2011) Metabolic syndrome in Poland – the PONS Study. Ann Agric Environ Med 18, 270–272. [PubMed] [Google Scholar]
- 34. Willett W & Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124, 17–27. [DOI] [PubMed] [Google Scholar]
- 35. Hulshof KF, Löwik MR, Kistemaker C et al. (1993) Comparison of dietary intake data with guidelines: some potential pitfalls (Dutch Nutrition Surveillance System). J Am Coll Nutr 12, 176–185. [DOI] [PubMed] [Google Scholar]
- 36. Bandini LG, Schoeller DA, Cyr HN et al. (1990) Validity of reported energy intake in obese and nonobese adolescents. Am J Clin Nutr 52, 421–425. [DOI] [PubMed] [Google Scholar]
- 37. Strain GW, Hershcopf RJ & Zumoff B (1992) Food intake of very obese persons: quantitative and qualitative aspects. J Am Diet Assoc 92, 199–203. [PubMed] [Google Scholar]
- 38. Pripp AH (2008) Effect of peptides derived from food proteins on blood pressure: a meta-analysis of randomized controlled trials. Food Nutr Res 2008, 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hirvonen T, Tapanainen H, Valsta L et al. (2006) Efficacy and safety of food fortification with calcium among adults in Finland. Public Health Nutr 9, 792–797. [DOI] [PubMed] [Google Scholar]