Abstract
Objective
To explore longitudinal associations between bottle-feeding and maternal encouragement of infant bottle-emptying during the first 6 months of infancy.
Design
Mothers completed questionnaires during the third trimester of pregnancy, then monthly during the first 6 months postpartum. Questionnaires assessed family demographics, maternal and infant weight status, infant feeding patterns and maternal encouragement of infant bottle-emptying.
Setting
The Infant Feeding Practices Study 2, conducted by the US Centers for Disease Control and Prevention and the Food and Drug Administration.
Subjects
Mothers (n 1776).
Results
Repeated-measures regression was used to explore associations between bottle-feeding intensity (BFI; defined as the percentage of daily feedings that were from a bottle) and encouragement of bottle-emptying. Mothers who reported consistently high or consistently low BFI also exhibited consistently higher or lower frequency of encouraging their infants to empty the bottle (respectively) across the first 6 months of infancy, whereas mothers who reported increases in their BFI also exhibited concomitant increases in the frequency to which they encouraged their infants to finish the bottle. More frequent encouragement of bottle-emptying was also associated with feeding expressed breast milk (P<0·001), and lower parity (P=0·01), pre-pregnancy BMI (P=0·002) and infant birth weight (P=0·001).
Conclusions
More frequent use of bottles for infant feeding was significantly associated with more frequent encouragement of bottle-emptying. Further research using causal designs is needed to better understand whether the use of bottles promotes this controlling feeding practice or whether mothers with more controlling feeding practices opt to bottle-feed.
Keywords: Bottle-feeding, Breast-feeding, Infant feeding, Child feeding practices, Mothers, Expressed breast milk, Infant formula
It has been long hypothesized that the experience of breast-feeding influences the development of mothers’ feeding practices and styles, leading to more optimal dietary patterns, satiety responsiveness and growth trajectories for infants( 1 – 8 ). In particular, it is widely held that the inability of a breast-feeding mother to assess infant consumption may be beneficial, helping the mother learn to trust her infant’s developing abilities to self-regulate intake and to feed in response to hunger and satiation cues( 4 , 7 – 9 ). In contrast, it is hypothesized that a bottle-feeding mother’s greater ability to assess and control how much the infant consumes may lead her to develop more controlling bottle-feeding practices during milk-feeding (e.g. encouraging the infant to finish the bottle)( 10 ), further leading to the continued use of controlling feeding practices during later solid-food feeding( 11 ).
Prospective and retrospective studies aimed at testing this hypothesis have shown that mothers who breast-feed for longer durations report less restrictive feeding practices at 12( 7 , 8 ) and 24 months( 2 ), less pressuring feeding practices at 12 months( 2 ) and greater use of monitoring at 12 months of age( 2 ), even after adjusting for relevant covariates such as infant sex and mothers’ sociodemographic, economic and anthropometric predictors of breast-feeding continuation( 2 , 8 ). Additionally, one study illustrated that mothers who reported greater bottle-feeding intensities (defined as the percentage of daily feedings that were from a bottle) later reported greater use of pressuring feeding practices when their children were 6 years old( 11 ). Although consistent in their findings, the majority of studies examining this issue have a common limitation: the lack of repeated measures of mothers’ feeding practices. Thus, although many studies conclude that breast-feeding has positive effects and bottle-feeding has negative effects on mothers’ developing feeding practices and styles, none has actually assessed whether experience with breast- v. bottle-feeding predicts change in controlling feeding practices over time.
This consideration is important in light of a growing body of research illustrating that certain mothers may choose to formula/bottle-feed because they prefer the higher level of control it affords. For example, pregnant mothers who reported more concern for their unborn child’s risk for over- or undereating had significantly shorter breast-feeding durations( 8 ). Additionally, mothers who report greater levels of dietary restraint( 12 ) and anxiety( 13 ) are more likely to initiate formula-feeding at birth. Thus, attitudes and beliefs that promote controlling feeding practices may be in place prior to bottle-feeding and drive decisions related to infant feeding. It is important to note, however, that while these studies test an alternative perspective, they also lack longitudinal measures of mothers’ feeding practices and it is unknown whether maternal attitudes and behaviours precede or proceed the development of infant feeding practices.
In sum, the nature of the association between early feeding mode (breast- v. bottle-feeding) and the development of mothers’ feeding practices is unclear, partially because longitudinal analyses are needed to better understand associations between early feeding experiences and mothers’ feeding practices. To this end, the objective of the present study was to analyse longitudinal data on one facet of controlling infant feeding practices – encouragement of bottle-emptying – to explore the degree of stability or change in controlling feeding practices during early infancy, as well as the possible association between bottle-feeding intensity and controlling feeding practices, during the first 6 months of infancy.
Methods
Participants
Data for the present study came from the Infant Feeding Practices Study 2 (IFPS II), a longitudinal study conducted by the Centers for Disease Control and Prevention and the Food and Drug Administration in the USA. The sample consisted of women who were selected from a national consumer opinion panel; inclusion criteria for participation included healthy women aged 18 years or older with singleton, full-term or near-term infants weighing at least 2·25 kg at birth. A total of 4902 women participated in the IFPS II. Assessment occurred during the third trimester, then at postpartum months 1, 2, 3, 4, 5, 6, 7, 9, 10 and 12 (eleven assessments total); the current study focuses on the first 6 months given that this is a time when infants are predominantly milk-fed( 14 ). Further details regarding the IFPS II design and response rates are published elsewhere( 15 ).
Measures
Bottle-feeding intensity
At each postpartum survey, mothers completed an FFQ for their infants in which they were asked how often in the past 7 d they fed their infants breast milk, formula, other types of milk (e.g. soya, almond) or solid foods. Mothers were also asked how often they fed their infants expressed breast milk. Hereafter, the term ‘milk’ includes any type of milk fed to infants, including breast milk and non-human milks such as formula milk, cow’s milk and other milks (soya, almond, etc.). However, note that during the first 6 months, <1 % of infants consumed cow’s milk or other milks.
Bottle-feeding intensity (BFI) was calculated as previously described by Li and colleagues( 11 , 16 ). Specifically, we first estimated the percentage of total milk feedings that were at the breast (BF%), expressed breast milk (EBM%) or non-human milk (NHM%), including formula, cow’s milk or other milks (BF%+EBM%+NHM%=100 %). We then calculated BFI as the proportion of milk feedings given by bottle (EBM%+NHM%).
Encouragement of bottle-emptying
At the 2-, 3-, 4-, 5- and 6-month assessments, one facet of controlling feeding practices, maternal encouragement of bottle-emptying, was assessed by two questions that referred to formula and expressed breast milk feedings, respectively: ‘How often is your baby encouraged to finish the bottle if he or she stops drinking before the formula is all gone?’ and ‘How often is your baby encouraged to finish a cup or bottle if he or she stops drinking before the pumped breast milk is all gone?’ Response options were presented on a 5-point Likert scale (1=never; 2=rarely; 3=sometimes; 4=most of the time; 5=always). While mothers who were exclusively formula-feeding answered the first question only, mothers who were exclusively breast milk-feeding answered the second question only, and mothers who were feeding a mix of formula and breast milk answered both questions, responses to these questions were included in the model as a single response (i.e. how often the baby is encouraged to finish a cup or bottle if he or she stops drinking before the pumped breast milk or formula is all gone). The type of milk (expressed breast milk v. formula) was coded and included as a covariate in the model along with additional covariates discussed in the following section.
Covariates
Maternal and familial demographic characteristics were assessed in the prenatal survey. Consistent with previous research that has used the IFPS II data set to examine infant outcomes associated with bottle-feeding, the following variables were included as potentially confounding factors( 11 , 16 , 17 ): maternal age, race/ethnicity, maternal education, poverty-income ratio (defined as a ratio of household income to the poverty threshold by household size), marital status, number of hours per week the infant was cared for by non-maternal caregivers, number of feedings per week that were given by non-maternal caregivers, parity, postpartum participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and pre-pregnancy BMI (self-reported by mothers and calculated as weight in kilograms divided by the square of height in metres). We also included several infant characteristics as potentially confounding factors: infant sex, birth weight (reported by mothers), gestational age, age at solid food introduction, number of sweet drinks consumed per day at each assessment (including juice drinks, soft drinks, soda, sweet tea, Kool-Aid, etc.) and daily frequency of solid food consumption at each assessment. Solid foods included dairy foods other than milk (e.g. yoghurt, cheese), soya foods other than soya milk (e.g. tofu), and all other foods such as baby cereal, other cereals and starches (e.g. breakfast cereals), fruits, vegetables, meat, poultry, fish, shellfish, nuts, nut butters, eggs and sweet foods (e.g. cookies, cake). Infants’ age at introduction of solid foods was determined as the age at which mothers first reported infants consumed solid foods in addition to milk. Daily frequency of solid food consumption was determined as the number of feedings per day that included any type of solid food.
Statistical analyses
The final analytical sample size was 1776 after excluding 3126 women and infants with any of the following qualities: (i) missing 100 % of data from months 2 to 6; (ii) missing all data for the primary response (mothers’ frequency of encouraging bottle-emptying); (iii) infant gestational age less than 36 weeks; (iv) mother reported a serious illness for herself or her infant at any assessment; (v) mother reported only breast-feeding her infant from the breast across months 2 to 6 (i.e. the infant never received a bottle); or (vi) mother reported her infant spent more than 70 h/week in the care of another person at any assessment.
Data were analysed using the statistical software packages SAS version 9.4 and JMP Pro version 12.1.0. All data were assessed for normality prior to inferential analysis. Mothers’ pre-pregnancy BMI and parity were skewed; thus, a log transformation was performed on these variables to limit the influence of outliers and skewness. The log transformation for parity was implemented after adding 1 to all existing values of parity. Descriptive statistics were calculated for all variables of interest. BFI was analysed as both a continuous variable and categorical variable: high BFI (bottles were used for >80 % of feedings), medium BFI (bottles were used for 20–80 % of feedings) or low BFI (bottles were used for <20 % of feedings) at each assessment( 11 , 16 , 17 ).
Repeated-measures regression was used to explore associations between BFI and mothers’ frequency of encouraging bottle-emptying across the first 6 months of infancy. The primary predictors of interest, time and BFI, were mean-centred in all regression models. Subject was specified as the random effect and encouragement of bottle-emptying scores were specified as the response. Two models were explored: (i) Model 1=longitudinal associations between BFI and mothers’ frequency of encouraging bottle-emptying, controlling for the type of milk (breast v. formula) in the bottle; and (ii) Model 2=Model 1+maternal and infant covariates. Inclusion of maternal and infant characteristics as covariates in Model 2 were determined using the Benjamini–Hochberg procedure (α=0·05) to limit the false discovery rate( 18 ). Preliminary analysis for Model 2 revealed the best-fit model included the following explanatory variables: time, BFI, the interaction between time and BFI (time × BFI), milk type (expressed breast milk v. formula), birth weight, parity and pre-pregnancy BMI. Other maternal and infant characteristics that were tested but not included in Model 2 because they were not significant predictors of encouragement of bottle-emptying scores were: maternal age, race/ethnicity, education, poverty-income ratio, marital status, number of hours per week the infant spent with non-maternal caregivers, number of feedings per week that were given by non-maternal caregivers and postpartum participation in WIC; and infant sex, gestational age, age at solid food introduction, number of sweet drinks consumed per day at each assessment (including juice drinks, soft drinks, soda, sweet tea, Kool-Aid, etc.) and daily frequency of solid food consumption at each assessment. Model requirements were examined and although there was statistically significant evidence for non-normality at the 0·05 significance level (Kolmogorov–Smirnov, D=0·06, P<0·01), the final model was selected because the overall distribution of the residuals was symmetric and bell-shaped, and there was no evidence of heteroscedasticity. Where applicable, results are presented as means and standard deviations. P<0·05 indicated significant effects.
Results
Sample characteristics
Sample characteristics are presented in Table 1. Fifty per cent of infants were female, and mean gestational age was 39 weeks, mean birth weight was 3·5 kg and mean age at solid food introduction was 5·1 months. Mothers were approximately 29 years of age and reported a pre-pregnancy BMI of 26·6 kg/m2. Twenty-nine per cent of mothers were primiparous and 73 % were married. With respect to mothers’ socio-economic status, 40 % received federal assistance and 43 % reported a family income level less than $US 40 000 per annum. During the prenatal assessment, 58 % of mothers reported they intended to exclusively breast-feed their infant, 14 % reported they intended to exclusively formula-feed their infant, 24 % reported they intended to feed their infant a mix of breast milk and formula, and 3 % were undecided.
Table 1.
Characteristics of the sample of mothers and their infants (n 1776) from the Infant Feeding Practices Study 2 (USA)
| % or Mean | n or sd | |
|---|---|---|
| Infant characteristics | ||
| Sex (% female) | 50·2 | 890 |
| Gestational age (weeks) | 39·4 | 1·3 |
| Birth weight (kg) | 3·5 | 0·5 |
| Age at solid food introduction (months) | 5·1 | 1·7 |
| Maternal/familial characteristics | ||
| Age at study entry (years) | 28·9 | 5·4 |
| Pre-pregnancy BMI (kg/m2) | 26·6 | 6·7 |
| Parity (number of children) | 1·1 | 1·2 |
| Federal assistance (% participating) | 40·0 | 710 |
| Annual family income level | ||
| <$US 20 000 | 13·3 | 237 |
| $US 20 000–39 999 | 29·5 | 524 |
| $US 40 000–59 999 | 23·7 | 421 |
| $US 60 000–99 999 | 25·5 | 453 |
| ≥$US 100 000 | 8·0 | 141 |
| Level of education | ||
| Did not complete high school | 2·7 | 48 |
| High-school degree | 15·8 | 281 |
| Some college/vocational degree | 37·6 | 668 |
| Bachelor’s or graduate degree | 36·4 | 647 |
| Not reported or no data | 7·4 | 132 |
| Race/ethnicity | ||
| White | 84·5 | 1501 |
| Black | 4·0 | 71 |
| Asian/Pacific Islander | 2·8 | 49 |
| Other | 5·9 | 106 |
| Not reported or no data | 2·8 | 49 |
| Marital status | ||
| Married | 73·4 | 1304 |
| Widowed | 0·3 | 5 |
| Divorced | 2·7 | 49 |
| Separated | 1·2 | 21 |
| Never married | 15·4 | 274 |
| Not reported or no data | 7·0 | 123 |
| Prenatal feeding intentions | ||
| Breast-feeding only | 58·4 | 1036 |
| Formula-feeding only | 13·7 | 244 |
| Both breast- and formula-feeding | 24·4 | 433 |
| Undecided | 3·3 | 59 |
| Not reported or no data | 0·2 | 4 |
During the month 2 assessment, mean BFI was 55·7 (sd 44·6) % of milk feedings. Mean BFI increased to 65·5 (sd 42·5) % of milk feedings by the month 6 assessment. Additionally, during the month 2 assessment, 48 % of mothers reported high BFI (bottles were used for >80 % of feedings), 13 % of mothers reported medium BFI (bottles were used for 20–80 % of feedings) and 38 % of mothers reported low BFI (bottles were used for <20 % of feedings). During the month 6 assessment, 58 % of mothers reported high BFI, 15 % of mothers reported medium BFI and 27 % of mothers reported low BFI. When examining change in BFI over time, the majority of mothers (81 %) could be classified as having either: (i) relative stability in their BFI (e.g. high BFI across all assessments); or (ii) increases in their BFI between months 2 and 6 (e.g. moved from low BFI at month 2 to high BFI at month 6). Specifically, 40 % of mothers were classified as high BFI across all assessments, whereas 22 % of mothers were classified as low BFI across all assessments. Additionally, 4 % of mothers reported an earlier increase in BFI (e.g. moved from a lower BFI classification at month 2 or 3 to a higher BFI classification at month 6) and 15 % of mothers reported a later increase in BFI (e.g. moved from a lower BFI classification at month 4 or 5 to a higher BFI classification at month 6).
Associations between bottle-feeding intensity and encouragement of bottle-emptying scores across the first 6 months of infancy
Repeated-measures regression analysis examining associations between BFI and mothers’ frequency of encouraging bottle-emptying revealed that BFI (P<0·001), the interaction between time and BFI (time×BFI; P=0·03) and milk type (P<0·001) were all significant predictors of mothers’ frequency of encouraging bottle-emptying (Table 2, Model 1). Effects of BFI (P<0·001) and milk type (P<0·001) remained significant in the final, covariate-adjusted model (Table 2, Model 2); birth weight (P<0·001), parity (P=0·01) and pre-pregnancy BMI (P<0·001) were also significant predictors of mothers’ frequency of encouraging bottle-emptying.
Table 2.
Repeated-measures regression models predicting mothers’ frequency of encouraging bottle-emptying across months 2–6, Infant Feeding Practices Study 2 (USA)
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Term | Estimate | se | P value | Estimate | se | P value |
| Intercept | 2·386 | 0·048 | <0·0001 | 4·244 | 0·380 | <0·0001 |
| Time | −0·005 | 0·007 | 0·495 | −0·005 | 0·007 | 0·502 |
| BFI | 0·004 | 0·001 | <0·0001 | 0·004 | 0·001 | <0·0001 |
| BFI×time | −0·001 | 0·001 | 0·032 | −0·001 | 0·001 | 0·061 |
| Milk type (breast milk) | 0·1444 | 0·030 | <0·0001 | 0·141 | 0·030 | <0·0001 |
| Birth weight | −0·083 | 0·025 | 0·001 | |||
| Log(parity+1) | −0·303 | 0·120 | 0·011 | |||
| Log(pre-pregnancy BMI) | −0·808 | 0·260 | 0·002 | |||
BFI, bottle-feeding intensity.
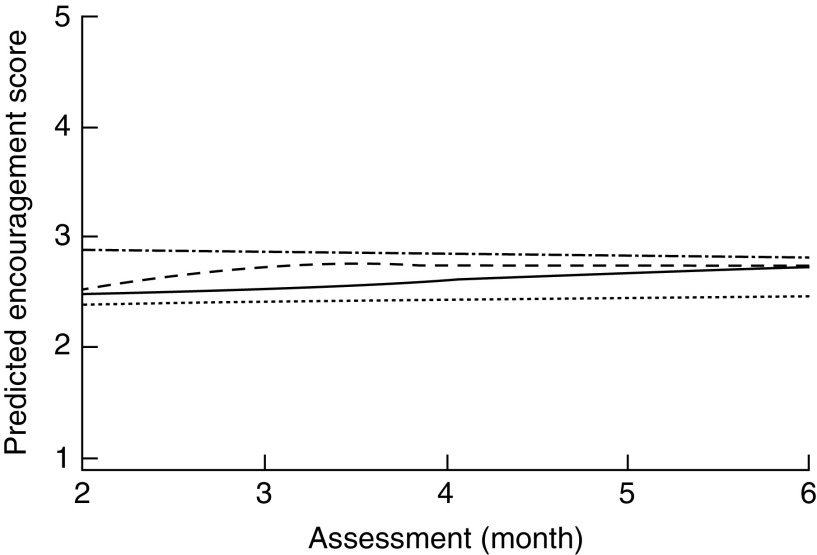
Given that the majority (81 %) of mothers reported consistently high BFI (40 %), consistently low BFI (22 %), or increases in BFI that occurred earlier (4 %) or later (15 %), Fig. 1 illustrates mothers’ frequency of encouraging bottle-emptying for these groups. As illustrated in Fig. 1, mothers with high BFI exhibited consistently high frequency of encouraging bottle-emptying across months 2 to 6. Mothers with earlier increases in BFI exhibited increases in their frequency of encouraging bottle-emptying between months 2 and 3, then exhibited relatively stable frequency of encouraging bottle-emptying between months 3 and 6. Mothers with later increases in BFI exhibited gradual increases in their frequency of encouraging bottle-emptying between months 2 and 6. Mothers with consistently low BFI showed consistently low frequency of encouraging bottle-emptying across months 2 to 6. At the month 6 assessment, frequency of encouraging bottle-emptying was not significantly different for mothers with high BFI, earlier increases in BFI and later increases in BFI, whereas mothers with low BFI reported the lowest frequency of encouraging bottle-emptying compared with all other groups (P<0·001).
Fig. 1.
Predicted trajectories for longitudinal associations between bottle-feeding intensity (BFI) and mothers’ frequency of encouraging bottle-emptying across months 2–6 ( high, i.e. consistently high (>80 % of feedings) BFI at all assessments;
high, i.e. consistently high (>80 % of feedings) BFI at all assessments;  earlier increase, i.e. BFI changed from a lower to a higher BFI classification between months 2 and 6 or months 3 and 6;
earlier increase, i.e. BFI changed from a lower to a higher BFI classification between months 2 and 6 or months 3 and 6;  later increase, i.e. BFI changed from a lower to a higher BFI classification between months 4 and 6 or months 5 and 6;
later increase, i.e. BFI changed from a lower to a higher BFI classification between months 4 and 6 or months 5 and 6;  low, i.e. consistently low (<20 % of feedings) BFI at all assessments) among 1776 mothers from the Infant Feeding Practices Study 2 (USA)
low, i.e. consistently low (<20 % of feedings) BFI at all assessments) among 1776 mothers from the Infant Feeding Practices Study 2 (USA)
With respect to maternal and infant predictors included in the fully adjusted model, a number of notable associations between maternal and infant characteristics and mothers’ frequency of encouraging bottle-emptying were seen. Mothers’ frequency of encouraging bottle-emptying was significantly greater when expressed breast milk was in the bottle compared with when formula was in the bottle (P<0·001). Greater frequency of encouraging bottle-emptying was also associated with lower infant birth weight (P=0·001), lower parity (P=0·011) and lower pre-pregnancy BMI (P=0·002).
Discussion
The aim of the present study was to describe longitudinal associations between feeding mode and feeding practices using repeated measures of one facet of controlling infant feeding practices – encouragement of bottle-emptying – during the first 6 months postpartum. Key study findings were that mothers who reported greater intensity of bottle-feeding also reported more frequent encouragement of bottle-emptying, but more frequent encouragement of bottle-emptying was also associated with feeding expressed breast milk and characteristics of both mothers (i.e. lower parity, lower pre-pregnancy BMI) and infants (i.e. lower birth weight).
Mothers who reported consistently high or consistently low intensity of bottle-feeding also exhibited consistently higher or lower frequency of encouraging their infants to empty the bottle (respectively), whereas mothers who reported increases in their intensity of bottle-feeding also exhibited concomitant increases in the frequency with which they encouraged their infants to finish the bottle.
Previous research suggests that mothers’ use of controlling feeding practices may have long-term consequences for children’s eating and weight outcomes by lowering responsiveness to internal hunger and satiation cues, increasing responsiveness to external food cues (e.g. the availability of food, the amount of food on the plate), increasing tendencies to eat in the absence of hunger, and promoting excess weight gain (see Birch and co-workers( 19 , 20 ) for a review). Additionally, the importance of understanding early influences on mothers’ use of controlling feeding practices is underlined by a number of studies illustrating that mothers’ tendencies to control the amount their children eat translates from milk- to solid-food feeding and across different feeding modes (i.e. bottle-feeding to self-feeding). For example, Li and colleagues recently found that mothers who frequently encouraged their infants to finish the bottle during the first 6 months postpartum had a higher likelihood of pressuring these same children to finish their plates when they were 6 years old( 11 ). Similarly, Duke and colleagues reported that one of the strongest predictors of mothers’ tendencies to pressure their 7-year-old daughters to eat was the mothers’ retrospective report of using a ‘pushy’ feeding style when their daughters were infants( 21 ). It has also been shown that both pressuring and restrictive feeding practices are stable between 1–2 years( 2 ), 3–4 years( 22 ) and 5–7 years( 23 ). Given these findings, an important question for prevention and intervention efforts is: what factors determine mothers’ feeding practices during early infancy and what leads some mothers to be more controlling than others?
In the present study, we explored the long-held hypothesis that mothers’ early experience with bottle- v. breast-feeding is a key early-life factor that may promote (in the case of bottle-feeding) or hinder (in the case of breast-feeding) the development of controlling feeding practices( 1 – 3 , 7 – 9 , 24 – 26 ). Possibly in support of this hypothesis, we found that mothers’ intensity of bottle-feeding was indeed a significant predictor of their frequency of encouragement of infant bottle-emptying, but the correlational nature of our data precludes our ability to draw causal conclusions. Thus, we present several possible explanations for these findings.
First, it is possible that mothers’ increases in BFI promoted their use of controlling feeding practices. Feeding from a bottle is a fundamentally different experience from feeding from a breast( 27 ), in part because the mother has more information about the feeding (e.g. the amount of milk left in the bottle) and more ability to exert control over the feed initiation and termination( 9 ). Indeed, a recent experimental study illustrated that when formula-feeding mothers fed their infants using a bottle with no visual or weight cues related to how much formula was left in the bottle (i.e. an opaque, weighted bottle), these mothers exhibited greater responsiveness to their infants’ cues and trended towards feeding their infants less formula compared with when they fed their infants using a conventional clear bottle( 10 ), possibly suggesting that the nature of bottle-feeding negatively impacts mothers’ feeding practices. However, it is important to note that the effect of bottle type (opaque, weighted v. conventional, clear) was moderated by mothers’ level of pressuring feeding style in that using opaque, weighted bottles significantly increased responsiveness and decreased the amount of formula fed for mothers with higher levels of pressuring feeding style, but not for mothers with lower levels of pressuring feeding style( 10 ). These findings may suggest that bottle-feeding facilitates, rather than promotes, a pressuring feeding style for some mothers, and that other factors beyond the experience of bottle-feeding, per se, also influence mothers’ infant feeding practices and styles. Thus, a second possible explanation is that certain mothers desire more control over infant feeding and these mothers choose to bottle-feed because of the greater level of control it affords( 12 , 28 – 30 ). This explanation may be more consistent with our findings given that mothers with consistently higher v. lower intensities of bottle-feeding reported significantly higher v. lower (respectively) frequency of encouragement of bottle-emptying across all assessments. This explanation would also suggest that mothers’ level of, or increase in, intensity of bottle-feeding was not a driver of their level of, or increase in, frequency of infant bottle-emptying; rather, mothers who desired more control over their infants’ intake elected to do more bottle-feeding. Consistent with this possibility, Brown and colleagues found that mothers who initiated breast-feeding and who breast-fed for longer durations reported lower levels of controlling feeding from birth compared with mothers who never initiated breast-feeding or had short breast-feeding durations( 30 , 31 ). Additionally, several studies have illustrated that, among mothers who initiated breast-feeding, those mothers who exhibited greater responsiveness to their infant’s cues during the period immediately after birth were more likely to still be breast-feeding at 6 weeks( 32 ) and through 6 months( 33 ). Thus, mothers who adhere to a more responsive and infant-led feeding style during early infancy may have more motivation for and success with breast-feeding and less desire to bottle-feed.
However, a related and third possible explanation is that prenatal and neonatal factors drive both mothers’ success with breast-feeding and their tendencies towards controlling feeding practices. Previous research illustrates that mothers who report greater concerns for their unborn child’s over- or undereating go on to have shorter breast-feeding durations in the postpartum period( 8 ) and mothers’ perception of, or concern about, low milk supply (and subsequent poor infant growth) is one of the most prevalent reasons for early breast-feeding cessation( 34 – 36 ). Similarly, infant birth weight is inversely associated with mother’s concern for her child’s weight and monitoring and encouraging milk feedings( 30 ) and mothers are more likely to encourage infant bottle-emptying when their infants exhibit slow weight gain( 17 ). A number of other factors influencing both breast-feeding success and tendencies towards controlling feeding practices have also been highlighted, including family structure and sociodemographics( 37 – 40 ) and maternal weight status( 41 – 43 ). The present study highlighted a similar set of maternal and infant characteristics that were predictive of mothers’ frequency of encouragement of bottle-emptying, but significant associations between feeding mode and encouragement of bottle-emptying remained even after controlling for these factors.
A particularly novel aspect of the present study is the finding that mothers reported significantly greater encouragement of bottle-emptying when expressed breast milk was in the bottle compared with when formula was in the bottle. This finding may stem from the popular perception of expressed breast milk as ‘liquid gold’ given the perceived time and effort necessary to produce and express breast milk( 44 , 45 ). It is also possible that factors that lead mothers to express and bottle-feed breast milk – such as difficulties with breast-feeding, anxiety over infant intake or needing to return to work – may also influence mothers’ feeding attitudes and practices. Few studies have explored the outcomes of infants fed significant amounts of expressed breast milk from a bottle, despite the fact that almost 70 % receive expressed breast milk from a bottle on a regular basis( 46 ). In a short-term pilot study comparing infants fed breast milk via a breast v. a bottle, Bartok( 47 ) did not find an association between feeding mode and infant weight gain between birth and 4 months. However, in a longer-term study with a significantly larger sample, Li et al.( 16 ) noted that, among infants who only received breast milk, those who were fed predominantly from a bottle gained significantly more weight during the first year postpartum compared with those who were fed predominantly from the breast. In light of these findings, further research is needed to better understand how feeding interactions and outcomes may differ when infants are fed breast milk via a breast v. a bottle and to understand how to best promote healthy feeding attitudes and practices for mothers who are bottle-feeding expressed breast milk.
The limitations of the present study provide some additional potential avenues for future research. First, we did not have a prenatal or neonatal (i.e. prior to 2 months) assessment of mothers’ encouragement of bottle-emptying or tendencies towards controlling feeding practices. Thus, it is possible that mothers’ use of bottles during the first 2 months promoted increases in controlling feeding practices and we failed to capture this change given the nature of the assessments available in the IFPS II data set. Further longitudinal research that includes prenatal and neonatal measures of mothers’ feeding attitudes, beliefs and practices is warranted. Second, all data were self-reported by mothers and our measure of controlling feeding practices – encouragement to finish the bottle – was assessed by a single question. Further research that includes repeated measures of a broader array of controlling feeding practices (e.g. restriction and pressure to eat) using validated measures will provide additional insights into how mothers’ feeding practices develop across infancy. Third, our consideration of infant characteristics was limited to weight status and sex primarily because measures of other infant characteristics – in particular, eating behaviours and temperament – were not available in the IFPS II data set. Previous research illustrates that consideration of what the infant ‘brings to the table’ is important for fully understanding the dynamics of early feeding interactions and the development of mothers’ feeding attitudes and practices( 48 – 52 ). Fourth, our sample was only 29 % primiparous, which is on the lower range of what has been seen in other infant feeding studies (e.g. as reviewed elsewhere( 53 )). It is possible that the primiparous mothers who participated in the present study were different from those who did not and those differences may have influenced our findings. The relevance of understanding influences on and implications of early feeding decisions is underlined by a growing body of research illustrating that weight gain patterns during infancy are a strong predictor of later risk for obesity and metabolic disease( 54 – 56 ). In particular, infants who are overfed and, consequently, gain weight too rapidly have significantly heightened risk for obesity and poor metabolic health during childhood( 54 , 56 , 57 ), adolescence( 58 , 59 ) and adulthood( 60 , 61 ). Much research has focused on the influence of mothers’ choice to breast- v. formula/bottle-feed on infant outcomes, with a consensus among these studies being that formula/bottle-feeding places infants at higher risk for overfeeding and rapid weight gain( 16 , 62 ). However, given the lack of longitudinal data specifically focused on how mothers’ feeding attitudes and practices develop during infancy, the mechanisms underlying this association are still unclear. The findings of the present study illustrate how patterns of infant feeding track across the first 6 months and highlight associations between feeding mode and one facet of controlling feeding practices during early infancy. These findings provide a foundation for further longitudinal studies aimed at better understanding how early feeding and infant rearing experiences shape mothers’ feeding practices and infant development.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: A.K.V. formulated the research question, obtained the data set and drafted the manuscript. P.G. and A.A.S. analysed the data and assisted with interpreting the findings and revising the manuscript. All authors reviewed and approved the final manuscript. Ethics of human subject participation: As a secondary analysis of de-identified data, the present study was exempt from Institutional Review Board approval as determined by the California Polytechnic State University Human Subjects Committee.
References
- 1. Bernal J & Richards MP (1970) The effects of bottle and breast feeding on infant development. J Psychosom Res 14, 247–252. [DOI] [PubMed] [Google Scholar]
- 2. Blissett J & Farrow C (2007) Predictors of maternal control of feeding at 1 and 2 years of age. Int J Obes (Lond) 31, 1520–1526. [DOI] [PubMed] [Google Scholar]
- 3. Wright P, Fawcett J & Crow R (1980) The development of differences in the feeding behaviour of bottle and breast fed human infants from birth to two months. Behav Processes 5, 1–20. [DOI] [PubMed] [Google Scholar]
- 4. DiSantis KI, Hodges EA & Fisher JO (2013) The association of breastfeeding duration with later maternal feeding styles in infancy and toddlerhood: a cross-sectional analysis. Int J Behav Nutr Phys Act 10, 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dunn J (1980) Feeding and sleeping. In The Scientific Foundations of Developmental Psychiatry, pp. 119–128 [M Rutter, editor]. London: Heinemann Medical Books. [Google Scholar]
- 6. Farrow C & Blissett J (2006) Breast-feeding, maternal feeding practices and mealtime negativity at one year. Appetite 46, 49–56. [DOI] [PubMed] [Google Scholar]
- 7. Fisher JO, Birch LL, Smiciklas-Wright H et al. (2000) Breast-feeding through the first year predicts maternal control in feeding and subsequent toddler energy intakes. J Am Diet Assoc 100, 641–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Taveras EM, Scanlon KS, Birch LL et al. (2004) Association of breastfeeding with maternal control of infant feeding at age 1 year. Pediatrics 114, e577–e583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crow RA, Fawcett JN & Wright P (1980) Maternal behavior during breast- and bottle-feeding. J Behav Med 3, 259–277. [DOI] [PubMed] [Google Scholar]
- 10. Ventura AK & Golen RP (2015) A pilot study comparing opaque, weighted bottles with conventional, clear bottles for infant feeding. Appetite 85, 178–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li R, Scanlon KS, May A et al. (2014) Bottle-feeding practices during early infancy and eating behaviors at 6 years of age. Pediatrics 134, Suppl. 1, S70–S77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brown A & Arnott B (2014) Breastfeeding duration and early parenting behaviour: the importance of an infant-led, responsive style. PLoS One 9, e83893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brown A & Jordan S (2014) Active management of the third stage of labor may reduce breastfeeding duration due to pain and physical complications. Breastfeed Med 9, 494–502. [DOI] [PubMed] [Google Scholar]
- 14. Fox MK, Reidy K, Novak T et al. (2006) Sources of energy and nutrients in the diets of infants and toddlers. J Am Diet Assoc 106, 1 Suppl. 1, S28–S42. [DOI] [PubMed] [Google Scholar]
- 15. Fein SB, Labiner-Wolfe J, Shealy KR et al. (2008) Infant Feeding Practices Study II: study methods. Pediatrics 122, Suppl. 2, S28–S35. [DOI] [PubMed] [Google Scholar]
- 16. Li R, Magadia J, Fein SB et al. (2012) Risk of bottle-feeding for rapid weight gain during the first year of life. Arch Pediatr Adolesc Med 166, 431–436. [DOI] [PubMed] [Google Scholar]
- 17. Li R, Fein SB & Grummer-Strawn LM (2008) Association of breastfeeding intensity and bottle-emptying behaviors at early infancy with infants’ risk for excess weight at late infancy. Pediatrics 122, Suppl. 2, S77–S84. [DOI] [PubMed] [Google Scholar]
- 18. Benjamini Y & Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 57, 289–300. [Google Scholar]
- 19. Ventura AK & Birch LL (2008) Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 5, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Anzman SL, Rollins BY & Birch LL (2010) Parental influence on children’s early eating environments and obesity risk: implications for prevention. Int J Obes (Lond) 34, 1116–1124. [DOI] [PubMed] [Google Scholar]
- 21. Duke RE, Bryson S, Hammer LD et al. (2004) The relationship between parental factors at infancy and parent-reported control over children’s eating at age 7. Appetite 43, 247–252. [DOI] [PubMed] [Google Scholar]
- 22. Gregory JE, Paxton SJ & Brozovic AM (2010) Maternal feeding practices, child eating behaviour and body mass index in preschool-aged children: a prospective analysis. Int J Behav Nutr Phys Act 7, 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Faith MS, Berkowitz RI, Stallings VA et al. (2004) Parental feeding attitudes and styles and child body mass index: prospective analysis of a gene–environment interaction. Pediatrics 114, e429–e436. [DOI] [PubMed] [Google Scholar]
- 24. Crow R & Wright P (1975) The development of feeding behaviour in early infancy. Nurs Mirror Midwives J 142, 57–59. [PubMed] [Google Scholar]
- 25. Dunn J & Richards M (1977) Observations on the developing relationship between mother and baby in the neonatal period. In Studies in Mother–Infant Interaction, pp. 427–455 [R Schaffer, editor]. New York: Academic Press. [Google Scholar]
- 26. Taveras EM, Rifas-Shiman SL, Scanlon KS et al. (2006) To what extent is the protective effect of breastfeeding on future overweight explained by decreased maternal feeding restriction? Pediatrics 118, 2341–2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ventura AK & Terndrup H (2016) Breasts versus bottles for infant feeding: what’s the difference?. In Infant Feeding: Parental Perceptions, Behaviors, and Health Effects, pp. 103–128 [J Worobey, editor]. Hauppauge, NY: Nova Publishers. [Google Scholar]
- 28. Brown A (2014) Maternal restraint and external eating behaviour are associated with formula use or shorter breastfeeding duration. Appetite 76, 30–35. [DOI] [PubMed] [Google Scholar]
- 29. Brown A (2014) Maternal trait personality and breastfeeding duration: the importance of confidence and social support. J Adv Nurs 70, 587–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brown A & Lee M (2013) Breastfeeding is associated with a maternal feeding style low in control from birth. PLoS One 8, e54229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brown A, Raynor P & Lee M (2011) Maternal control of child-feeding during breast and formula feeding in the first 6 months post-partum. J Hum Nutr Diet 24, 177–186. [DOI] [PubMed] [Google Scholar]
- 32. Brandt KA, Andrews CM & Kvale J (1998) Mother–infant interaction and breastfeeding outcome 6 weeks after birth. J Obstet Gynecol Neonatal Nurs 27, 169–174. [DOI] [PubMed] [Google Scholar]
- 33. Cernadas JM, Noceda G, Barrera L et al. (2003) Maternal and perinatal factors influencing the duration of exclusive breastfeeding during the first 6 months of life. J Hum Lact 19, 136–144. [DOI] [PubMed] [Google Scholar]
- 34. Brown CR, Dodds L, Legge A et al. (2014) Factors influencing the reasons why mothers stop breastfeeding. Can J Public Health 105, e179–e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Odom EC, Li R, Scanlon KS et al. (2013) Reasons for earlier than desired cessation of breastfeeding. Pediatrics 131, e726–e732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rozga MR, Kerver JM & Olson BH (2015) Self-reported reasons for breastfeeding cessation among low-income women enrolled in a peer counseling breastfeeding support program. J Hum Lact 31, 129–137. [DOI] [PubMed] [Google Scholar]
- 37. Hackman NM, Schaefer EW, Beiler JS et al. (2015) Breastfeeding outcome comparison by parity. Breastfeed Med 10, 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gross RS, Mendelsohn AL, Fierman AH et al. (2014) Maternal infant feeding behaviors and disparities in early child obesity. Child Obes 10, 145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Taveras EM, Gillman MW, Kleinman K et al. (2010) Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics 125, 686–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gibbs BG & Forste R (2014) Socioeconomic status, infant feeding practices and early childhood obesity. Pediatr Obes 9, 135–146. [DOI] [PubMed] [Google Scholar]
- 41. Thompson AL (2013) Intergenerational impact of maternal obesity and postnatal feeding practices on pediatric obesity. Nutr Rev 71, Suppl. 1, S55–S61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Baker JL, Michaelsen KF, Rasmussen KM et al. (2004) Maternal prepregnant body mass index, duration of breastfeeding, and timing of complementary food introduction are associated with infant weight gain. Am J Clin Nutr 80, 1579–1588. [DOI] [PubMed] [Google Scholar]
- 43. Baker JL, Michaelsen KF, Sorensen TI et al. (2007) High prepregnant body mass index is associated with early termination of full and any breastfeeding in Danish women. Am J Clin Nutr 86, 404–411. [DOI] [PubMed] [Google Scholar]
- 44. Burns E, Schmied V, Fenwick J et al. (2012) Liquid gold from the milk bar: constructions of breastmilk and breastfeeding women in the language and practices of midwives. Soc Sci Med 75, 1737–1745. [DOI] [PubMed] [Google Scholar]
- 45. Burns E, Fenwick J, Sheehan A et al. (2013) Mining for liquid gold: midwifery language and practices associated with early breastfeeding support. Matern Child Nutr 9, 57–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Labiner-Wolfe J, Fein SB, Shealy KR et al. (2008) Prevalence of breast milk expression and associated factors. Pediatrics 122, Suppl. 2, S63–S68. [DOI] [PubMed] [Google Scholar]
- 47. Bartok CJ (2011) Babies fed breastmilk by breast versus by bottle: a pilot study evaluating early growth patterns. Breastfeed Med 6, 117–124. [DOI] [PubMed] [Google Scholar]
- 48. Ventura AK, Inamdar LB & Mennella JA (2015) Consistency in infants’ behavioural signalling of satiation during bottle-feeding. Pediatr Obes 10, 180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ventura AK & Mennella JA (2017) An experimental approach to study individual differences in infants’ intake and satiation behaviors during bottle-feeding. Child Obes 13, 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Anzman-Frasca S, Stifter CA, Paul IM et al. (2014) Negative temperament as a moderator of intervention effects in infancy: testing a differential susceptibility model. Prev Sci 15, 643–653. [DOI] [PubMed] [Google Scholar]
- 51. Moding KJ, Birch LL & Stifter CA (2014) Infant temperament and feeding history predict infants’ responses to novel foods. Appetite 83, 218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Doub AE, Moding KJ & Stifter CA (2015) Infant and maternal predictors of early life feeding decisions. The timing of solid food introduction. Appetite 92, 261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ventura AK (2017) Associations between breastfeeding and maternal responsiveness: a systematic review of the literature. Adv Nutr 8, 495–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Evelein AM, Visseren FL, van der Ent CK et al. (2013) Excess early postnatal weight gain leads to thicker and stiffer arteries in young children. J Clin Endocrinol Metab 98, 794–801. [DOI] [PubMed] [Google Scholar]
- 55. Sacco MR, de Castro NP, Euclydes VL et al. (2013) Birth weight, rapid weight gain in infancy and markers of overweight and obesity in childhood. Eur J Clin Nutr 67, 1147–1153. [DOI] [PubMed] [Google Scholar]
- 56. Skilton MR, Marks GB, Ayer JG et al. (2013) Weight gain in infancy and vascular risk factors in later childhood. Pediatrics 131, e1821–e1828. [DOI] [PubMed] [Google Scholar]
- 57. Dennison BA, Edmunds LS, Stratton HH et al. (2006) Rapid infant weight gain predicts childhood overweight. Obesity (Silver Spring) 14, 491–499. [DOI] [PubMed] [Google Scholar]
- 58. Khuc K, Blanco E, Burrows R et al. (2012) Adolescent metabolic syndrome risk is increased with higher infancy weight gain and decreased with longer breast feeding. Int J Pediatr 2012, 478610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ong KK, Emmett P, Northstone K et al. (2009) Infancy weight gain predicts childhood body fat and age at menarche in girls. J Clin Endocrinol Metab 94, 1527–1532. [DOI] [PubMed] [Google Scholar]
- 60. Ekelund U, Ong KK, Linne Y et al. (2007) Association of weight gain in infancy and early childhood with metabolic risk in young adults. J Clin Endocrinol Metab 92, 98–103. [DOI] [PubMed] [Google Scholar]
- 61. Stettler N & Iotova V (2010) Early growth patterns and long-term obesity risk. Curr Opin Clin Nutr Metab Care 13, 294–299. [DOI] [PubMed] [Google Scholar]
- 62. Mihrshahi S, Battistutta D, Magarey A et al. (2011) Determinants of rapid weight gain during infancy: baseline results from the NOURISH randomised controlled trial. BMC Pediatr 11, 99. [DOI] [PMC free article] [PubMed] [Google Scholar]