Abstract
Objective
The purpose of the present systematic review was to synthesize evidence from the literature to assess efficacy of the Mediterranean dietary pattern in childhood asthma.
Design/Setting
A systematic search of six databases, three clinical trial registries and hand-search of peer-reviewed articles was conducted up to 29 October 2016. Inclusion criteria included exposure to a Mediterranean dietary pattern, measurement of asthma symptoms and study population of children aged <18 years. Quality assessment was conducted. Due to significant heterogeneity, meta-analysis was not feasible.
Results
Of the 436 articles identified, after removal of duplicates and based on inclusion criteria, fifteen observational studies conducted in Mediterranean and non-Mediterranean countries were relevant. No randomized controlled trials were retrieved. Twelve studies reported an inverse association between adherence to a Mediterranean dietary pattern and asthma in children, two studies showed no association and one study showed an increase in asthma symptoms. In fourteen out of fifteen studies, quality assessment checks revealed good reliability and validity among study methodologies.
Conclusions
The current systematic review revealed a consistent inverse relationship (protective) between a Mediterranean dietary pattern and asthma in children. Future well-designed randomized controlled trials are needed to provide solid evidence. Nevertheless, the existing level of evidence adds to the public health message relating to the beneficial effects of a Mediterranean-type diet in children suffering with asthma.
Keywords: Mediterranean dietary pattern, Mediterranean diet, Asthma, Child, Nutrition
Asthma remains a global public health problem of epic proportions, especially in children and adolescents. Asthma is a complex respiratory disorder characterized by symptoms that include wheezing, chest tightness, coughing (especially at night) and breathlessness resulting from air flow obstruction triggered by the interaction of genetic and environmental factors( 1 , 2 ).
Diet has been implicated as one of the environmental factors contributing to the pathogenesis of this disease( 3 , 4 ). In many Westernized countries today, dietary intakes are generally low in fruit, vegetables, wholegrain cereals and fish, and high in fast foods, sweets and salty snacks that are high in saturated fat, sugar and salt and low in fibre and antioxidants. Earlier studies suggested that the low prevalence of asthma symptoms in children from Mediterranean countries compared with English-speaking countries is possibly due to the different dietary patterns of these regions( 5 , 6 ).
The traditional Mediterranean diet is a collection of eating habits traditionally followed by people in countries around the Mediterranean basin during the early 1960s( 7 , 8 ). The main characteristics of traditional Mediterranean diets are that all foods consumed are minimally processed, seasonally fresh and locally grown. Furthermore, this pattern is characterized by high intakes of fruits, vegetables, wholegrain cereals, legumes and nuts, low to moderate consumption of dairy products (mainly as cheese and yoghurt), fish, poultry and red wine (usually with meals), fewer than four eggs weekly, small amounts of red meat and liberal use of olive oil as the primary source of added fat( 9 ). Consequently, this pattern is low in SFA, high in MUFA and n-3 fatty acids, and rich in fibre, vitamins D and E, Mg and antioxidants( 8 , 9 ).
Most studies on diet and asthma have focused on individual nutrients or food groups and results have been inconsistent. A limitation of these studies is that they fail to take account of the interaction or synergistic effect between dietary components( 10 ). People consume a variety of foods and food groups in a meal, rather than individual nutrients or food groups, and for this reason it has been stated that dietary patterns represent a better picture of the true diet and nutrient intakes of a given population( 11 , 12 ). Hence, it may be more appropriate to better understand the effect of a dietary pattern such as the Mediterranean diet, rather than specific foods or nutrients, on childhood asthma.
Few studies have investigated the association of dietary patterns with childhood asthma and most published reviews are narrative and reflect an opinion rather than an objective analysis of the evidence. To date, only one systematic review and meta-analysis of eight observational studies up to 2013 has been published which examined the influence of the Mediterranean diet on childhood asthma( 13 ). Results of the meta-analysis showed that adherence to a Mediterranean diet during childhood might protect against ‘asthma ever’ and ‘current wheeze’. Therefore, the purpose of the present systematic review was to conduct an up-to-date extensive database search to collate and analyse the literature on the effectiveness of a Mediterranean dietary pattern in childhood asthma. The review will add further to the evidence base that links the Mediterranean diet with lower asthma symptoms in children.
Methods
Literature search/data collection
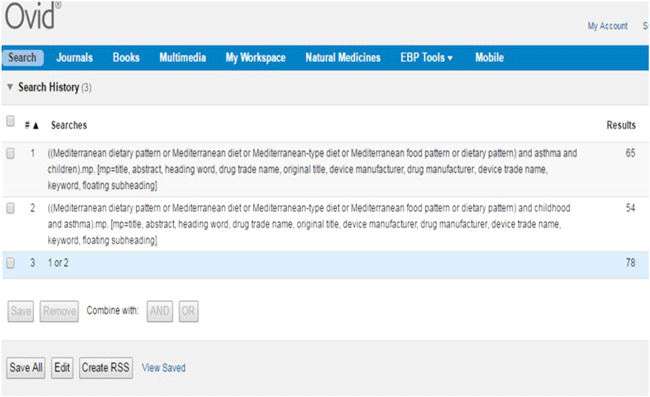
The current systematic review was prepared and reported according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines( 14 ). Relevant studies were identified by systematic search from PUBMED, MEDLINE, EMBASE, Cochrane Library, EBSCO (Ovid) and SCOPUS databases for articles published up to 29 October 2016 and extended back to 1946. Furthermore, in an effort to capture all published studies from a variety of international journals, no restrictions were applied on language, age or publication dates. Additional studies were sought from conference proceedings as well as clinical trial registries (international, European, Australia and New Zealand) in order to identify published/unpublished trials focusing on the Mediterranean dietary pattern and asthma in children. Other citations were identified by hand-searching the reference lists of potential articles. Finally, cross-checks were done to compare relevant articles in our review with previous reviews and systematic reviews.
Search terms were as follows: [‘Mediterranean dietary pattern’ OR ‘Mediterranean diet’ OR ‘Mediterranean-type diet’ OR ‘Mediterranean food pattern’ OR ‘dietary pattern’ AND ‘asthma’ AND ‘children’] OR [‘Mediterranean dietary pattern’ OR ‘Mediterranean diet’ OR ‘Mediterranean-type diet’ OR ‘Mediterranean food pattern’ OR ‘dietary pattern’ AND ‘childhood AND asthma’]. The full search strategy is provided in Appendices 1 to 4.
Study eligibility criteria
Type of studies
Since no randomized controlled trials were identified, the literature search included ‘all study types’, primarily observational studies (intervention, case–control, cohorts and cross-sectional) investigating Mediterranean diet as the primary exposure variable associated with asthma as the outcome in the child population.
Outcomes of interest
Primary outcomes were asthma symptoms, risk and prevalence.
Inclusion criteria
Inclusion criteria were based on PICO (population, intervention, comparator, outcomes)( 15 ). A study was included when the population under investigation was ‘children’, ‘Mediterranean diet’ was the intervention and ‘asthma symptoms’ was the outcome. A publication was considered for the systematic review if it focused on human subjects, was published in English or any other language with an English translation available, and the dietary intervention was described in sufficient detail, highlighting the main components of the dietary pattern and being evaluated by a questionnaire or diet history. Regarding assessment of adherence to the Mediterranean dietary pattern, only studies using a score and results presented as odds ratio or relative risk and corresponding 95 % confidence interval were considered. Composite outcomes (e.g. allergy) were eligible when diet was part of a multifaceted intervention and results on the Mediterranean diet and asthma in children could be separated.
Exclusion criteria
Exclusion criteria were based on PICO characteristics and reasons for study exclusion were summarized. Types of studies not included were: reviews, systematic reviews, editorials, comments, letters, dissertations, newspapers, case studies and animal studies, as well as those with no abstract, full text or English translation available. Studies conducted in adults, infants and pregnant women were not the population under investigation. In addition, interventions or risk factors other than Mediterranean diet such as supplementation, specific nutrients, intake of single food groups, other dietary patterns (e.g. Western), probiotics, medication, pollution, urban environment, obesity and BMI, as well as studies focusing on maternal nutrition or the role of genetics in asthma, were excluded. Also deemed inappropriate were studies investigating the role of diet in relation to other outcomes, for example dermatitis, eczema, CVD, rheumatoid arthritis, obstructive lung disease, metabolic syndrome, cognitive function, or growth and development.
Selection of studies
The titles and abstracts of all articles identified were reviewed by two authors (M.M.P., C.I.) to assess eligibility and duplicates removed. Papers were screened for relevance based on the information contained in titles and abstracts. Potentially eligible abstracts were selected for full-text reading provided that all inclusion criteria were satisfied. Also, when there was insufficient information in the abstract to warrant exclusion of the article, the full text was retrieved. Finally, full-text articles satisfying inclusion criteria were reviewed by both reviewers and details were extracted. Discrepancies were resolved by discussion and consensus that led to agreement.
Quality assessment
Two authors (M.M.P., N.H.S.) assessed the quality of each study independently using a validated quality assessment tool modified from Zaza et al.( 16 ). The quality assessment tool included a checklist of: description of the study design; description of the study population and how it was selected; how the exposure (Mediterranean diet score) and outcome (asthma in children) were measured; whether the measurements were valid and reliable; the appropriateness of the statistical analysis to answer the research question; and finally how each study controlled for potential bias (i.e. recall bias, measurement bias) or any potential bias that may have been missed. Results were evaluated as the percentage of how many points each study scored out of the maximum number of points it could have achieved, as not every study had the same maximum score due to factors such as different study design or statistical analysis. Finally, scores from both authors were averaged and became the final score. We used a score of 70 % or above to define high study quality and a score below 70 % as low study quality. Any disagreements that arose between the authors were resolved through discussion or with a third author (B.E.).
Data extraction
The data extracted from relevant studies included specific details about the author, year of publication, study design, study name, geographic area, sample size, age of target population, Mediterranean dietary assessment tool, outcome measure, exposure estimate, confounders and main findings. Where available, data analysis results were reported as odds ratios and 95 % confidence intervals, with P value at 5 % significance level.
Results
Electronic search
The database searches identified a total of 435 potential articles, of which 318 original articles remained after removal of duplicates (Fig. 1). One citation was found by cross-checking of reference lists. No trials (published or unpublished) were identified from international clinical trial registries. Of the remaining eligible articles, 319 were screened by two authors (M.M.P., C.I.) independently scanning titles and abstracts. A total of 270 articles were excluded as they did not examine the specific exposure (Mediterranean diet) in relation to the outcome (asthma symptoms) in the study population (children) or satisfy the publication type (original article) (not outcome, n 117; not intervention, n 20; not study population, n 9; no abstract, n 16; reviews, n 107; no English translation, n 1), leaving forty-nine full-text articles to be read for relevance. Of the remaining forty-nine potential studies, thirty-four full texts were considered inappropriate based on the exclusion criteria (not study population, n 6; not intervention, n 12; not study type, n 11; no abstract or full text available, n 5), leaving a total of fifteen studies relevant to the topic. Specifically, eleven cross-sectional, one intervention (with no control group), one case–control and two cohort studies investigating the association between children’s adherence to a Mediterranean dietary pattern and asthma( 17 – 31 ).
Fig. 1.
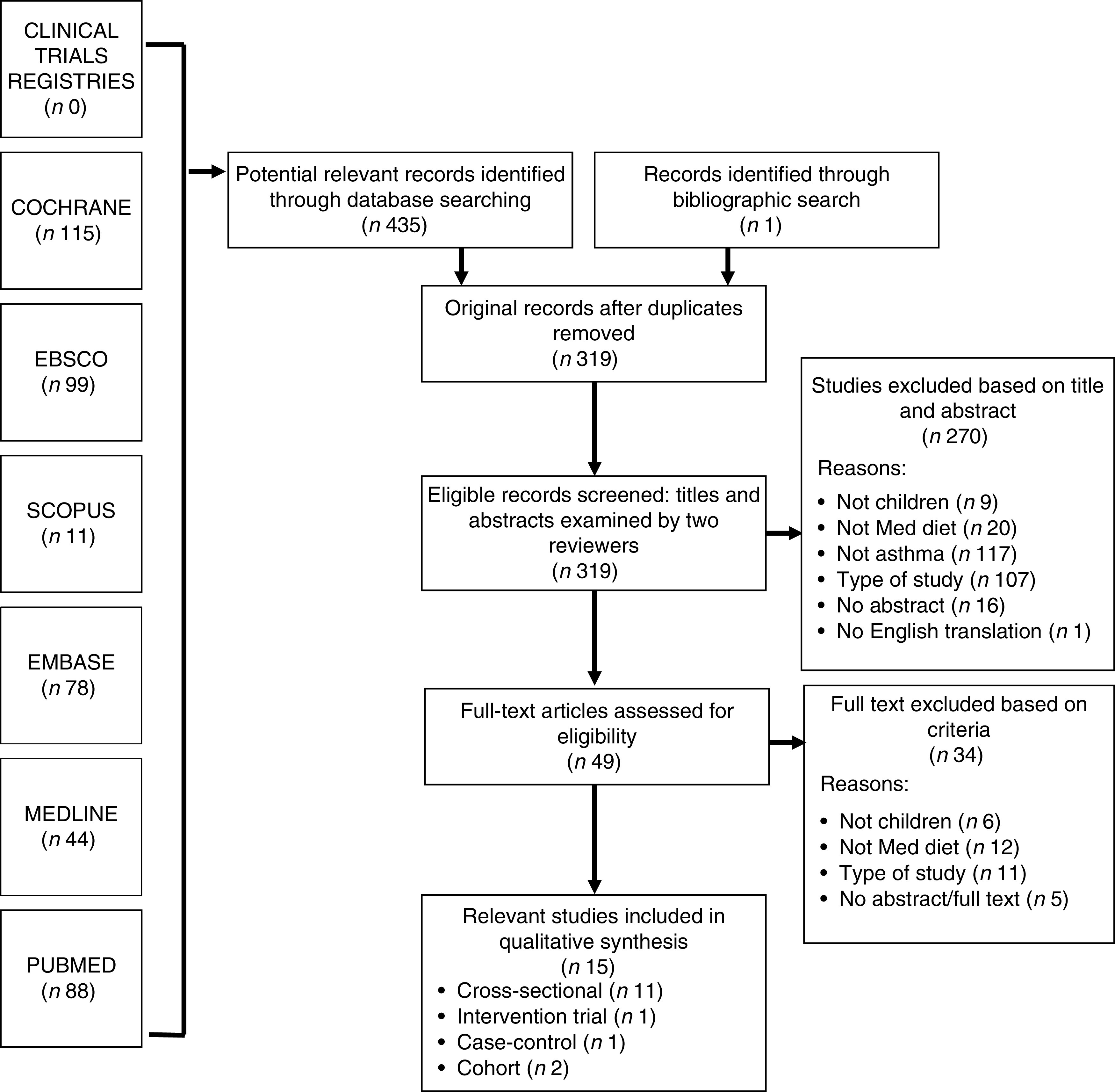
Flowchart detailing the study search for the present systematic review on the Mediterranean dietary pattern (Med diet) and childhood asthma
Study characteristics
The database search revealed fifteen original studies investigating children’s adherence to the Mediterranean dietary pattern and asthma (Tables 1 and 2). Ten of these studies were conducted in Mediterranean regions including Greece (n 4)( 18 , 19 , 22 , 27 ), Spain (n 5)( 20 , 21 , 23 , 25 , 26 ) and Turkey (n 1)( 17 ); four were conducted in non-Mediterranean countries, namely Mexico (n 2)( 24 , 30 ), Peru (n 1)( 29 ) and Brazil (n 1)( 31 ); and the ISAAC (International Study on Allergies and Asthma in Childhood)( 28 ) involved twenty countries globally. Collectively, 103 248 children and adolescents aged 1 to 19 years participated, with sample sizes ranging from 104 to 50 004. In all these studies children’s dietary intake was evaluated using an FFQ that was either self-administered or completed by parents. Regarding assessment of asthma symptoms, thirteen studies( 17 – 28 , 31 ) used the ISAAC respiratory questionnaire( 33 ) and two studies used spirometry( 29 , 30 ). A variety of outcomes were measured which included: prevalence of asthma, wheeze, exercise wheeze, any asthma symptoms, night-time cough, sleep disturbance due to wheeze, persistent asthma, atopic asthma, current severe asthma, spirometry (forced expiratory volume 1, forced vital capacity), bronchial inflammation, medication use, number of episodes/attacks, hospital admissions, severity of attacks, asthma control, asthma severity and bronchial hyper-responsiveness. All studies, except for one( 20 ), adjusted for confounding factors although the confounding variables differed between studies. Children’s adherence to the Mediterranean dietary pattern was assessed using three indices. Three studies( 22 , 24 , 30 ) used the original Mediterranean diet score developed by Trichopoulou et al.( 34 ), seven studies( 17 , 21 , 25 , 26 , 28 , 29 , 31 ) used the scoring system by Psaltopoulou et al.( 35 ) and six studies( 18 , 19 , 20 , 22 , 23 , 27 ) used the KIDMED index developed by Serra-Majem et al.( 36 ). In the studies that used the scoring system based on Psaltopoulou, dietary intake was further categorized into two eating patterns: (i) a ‘Pro-Mediterranean’ pattern which correlated with intakes of fruit, vegetables, fish, cereals, pasta, rice and potatoes; and (ii) an ‘Anti-Mediterranean’ pattern as intakes of milk, meat, eggs, fast foods, soft drinks and butter( 17 , 21 , 25 , 26 , 28 , 29 , 31 ).
Table 1.
Characteristics of cross-sectional studies included in the present systematic review on the Mediterranean dietary pattern and childhood asthma
| Author(s), year, name of study, location, study design | Sample size | Age (years) | Exposure | Tool used to evaluate adherence to Med diet | Asthma outcome measured | Exposure estimate | Confounders | Findings |
|---|---|---|---|---|---|---|---|---|
| Antonogeorgos et al. ( 18 ), 2014, PANACEA study, Greece, cross-sectional | 1125 | 10–12 | Med diet | KIDMED index* (Range 0–16) <8, improvement needed ≥8, optimal | ● Current asthma ● Ever had asthma | Path analysis Standardized β=–0·224, P=0·02 | Age, gender, parental atopy | High adherence to Med diet inversely related to asthma symptoms |
| Arvaniti et al.( 19 ), 2011, PANACEA study, Greece, cross-sectional | 700 | 10–12 | Med diet | KIDMED index* 0–3, poor 4–7, average 8–12, good | ● Overall lifetime prevalence asthma ● Ever had wheeze ● Exercise wheeze ● Night cough ● Ever had diagnosed wheeze ● Any asthma symptoms | ● Prevalence asthma symptoms: OR=0·86 (95 % CI 0·75, 0·98) | Age, sex, BMI, physical activity, energy intake | High adherence to Med diet inversely associated with ‘ever had wheeze’ (high v. low adherence: 8 v. 29 %; P=0·001); ‘exercise wheeze’ (0 v. 11 %; P=0·004); ‘ever had diagnosed wheeze’ (3 v. 6 %; P=0·002); and ‘any asthma’ (5 v. 34 %; P<0·001). Med diet consumers had 89 % lower likelihood of having asthma symptoms and 48 % lower likelihood of having diagnosed asthma v. non-consumers. 1-unit increase in score associated with 14 % lower likelihood of having asthma symptoms (OR=0·86; 95 % CI 0·75, 0·98) |
| Grigoropoulou et al.( 27 ), 2011, PANACEA study, Greece, cross-sectional | 1125 | 10–12 | Med diet | KIDMED index* ≤3, very low 4–7, improvement needed ≥8, optimal | ● Any asthma symptoms ever ● Night cough ● Exercise wheeze ● Wheeze limiting speech ● Wheeze disturbing sleep | ● Ever had wheeze: OR=0·88 (95 % CI 0·78, 0·98) ● Exercise wheeze: OR=0·79 (95 % CI 0·6, 0·93) ● Lower likelihood asthma in urban (OR=0·81; 95 % CI 0·73, 0·91) and rural areas (OR=0·87, 95 % CI 0·75, 1·00) | Urban/rural, sex, BMI, energy intake, physical activity | High adherence to Med diet inversely associated with ‘ever had wheeze’ and ‘exercise wheeze’. 1-unit increase in KIDMED score, 16 % lower likelihood of asthma symptoms in urban and rural areas |
| Nagel et al.( 28 ), 2010, in 20 countries, cross-sectional | 50 004 | 8–12 | Med diet | Med diet score based on food frequency consumption in FFQ | ● Current wheeze ● Asthma ever ● BHR | ● Current wheeze: OR=0·97; 95 % CI 0·94, 0·99 ● Asthma ever: OR=0·95 (95 % CI 0·92, 0·99) | Gender, age, tobacco smoke, no. of siblings, exercise, atopy, maternal education, parental atopic & non-atopic wheeze | High adherence to Med diet, lower prevalence of ‘current wheezing’ and ‘asthma ever’ (P-trend=0·03) |
| Castro-Rodriguez et al.( 21 ), 2008, Spain, cross-sectional | 1784 | 3–4 | Med diet | Med Diet Score† (Range 14–36) Pro-Med/Anti-Med dietary pattern | ● Current wheezing | ● Current wheeze: OR=0·54 (95 % CI 0·33, 0·88), P=0·014 | Age, birth weight, livestock during pregnancy, delivery by caesarean, antibiotics during first year life, acetaminophen use during past 12 months, rhinoconjunctivitis, dermatitis, paternal/maternal asthma, maternal age, maternal educational level, current parent/maternal smoking, vigorous physical activity, cats in the last 12 months | High adherence to Med diet, lower risk of ‘current wheezing’ |
| de Batlle et al.( 24 ), 2008, Mexico, cross-sectional | 1476 | 6–7 | Med diet | Med Diet Score‡ (Range 0–8) (Mean score 3·7) Ist tertile: 0–3 2nd tertile: 4 3rd tertile: 5–8 | ● Asthma ever ● Wheezing ever ● Current wheezing | ● Asthma ever: OR=0·60 (95 % CI 0·40, 0·91), P-trend=0·034 ● Wheezing ever: OR=0·64 (95 % CI 0·47, 0·87), P-trend=0·001 | Gender, birth weight, BMI, no. of siblings (older/younger), breast-feeding, parental educational level, children’s exercise, smoking exposure during pregnancy, parental asthma and atopy, pets during pregnancy, pet at home during first year of life, living on a farm during pregnancy, premature birth, respiratory infections during early life, body changes since 4 years old, type of fuel for cooking, sleeping alone, mould/dampness at home | High adherence to Med diet inversely associated with asthma and wheezing |
| Garcia-Marcos et al.( 25 ), 2007, Spain, cross-sectional | 20 106 | 6–7 | Med diet | Med Diet Score§ (Median score 13) (Range 4–20) Pro-Med/Anti-Med dietary pattern | ● Current severe asthma (CSA) ● Current occasional asthma (COA) | Girls: ● CSA: OR=0·90 (95 % CI 0·82, 0·98) Boys: ● CSA: OR=0·98 (95 % CI 0·91, 1·06) | Obesity, maternal smoking, no. of siblings, exercise | High adherence to Med diet decreased CSA in girls. 1-unit increase in score, 10 % protective effect. No statistically significant result found for COA |
| Chatzi et al.( 22 ), 2007, Crete, Greece, cross-sectional | 690 | 7–18 | Med diet | KIDMED index* ≤3, very low 4–7, improvement needed ≥8, optimal Med Diet Score‡ (Range 0–8) | ● Wheezing ever ● Current wheezing ● Wheezing ever with atopy ● Nocturnal dry cough | ● Wheezing ever: OR=0·67 (95 % CI 0·34, 1·32), P=0·229 ● Current wheezing: OR=0·64 (95 % CI 0·20, 2·05), P=0·564 ● Nocturnal dry cough: OR=0·49 (95 % CI 0·23, 0·96), P=0·095 ● Wheezing ever with atopy: OR=0·53 (95 % CI 0·16, 1·80), P=0·417 | Age, gender, BMI, parental asthma, no. of older siblings | High adherence to Med diet beneficial effect on asthma, but not statistically significant |
| Akcay et al.( 17 ), 2014, Turkey, cross-sectional | 9991 | 13–14 | Med diet | Med Diet Score§ (Range 0–22) (Median score 12·5) Pro-Med/Anti-Med dietary pattern | ● Wheeze ever, wheeze in last 12 months ● Doctor-diagnosed asthma ● Severe attacks of wheeze ● Exercise wheeze ● Night cough ● Sleep disturbed by wheeze | – | Gender, family atopy, television viewing, paracetamol use, no. of siblings at home, born in Istanbul, time lived in Istanbul, education level of mother/father, parent/guardian, smoking, tonsillectomy, adenoidectomy, pets at home (cat, dog, fish, bird) | No significant difference between Med diet scores and asthma in asthmatic and non-asthmatic children, P=0·85 |
| Silviera et al.( 31 ), 2015, Brazil, cross-sectional | 394 (268 persistent asthma, 126 control) | 3–12 | Med diet | No score Qualitative (yes/no): Pro-Med/Contra-Med dietary pattern║ | ● Persistent asthma (mild, moderate, severe) ● Intermittent asthma | ● Pro-Med dietary pattern: OR=1·20 (95 % CI 0·78, 1·86), P=0·40 ● Contra-Med dietary pattern: OR=0·82 (95 % CI 0·53, 1·27), P=0·38 | Maternal smoking during pregnancy, preterm birth, gender, skin colour, maternal schooling, income, paternal schooling and smoking during pregnancy, allergens in home, gestational age, birth weight, family history of allergic rhinitis, exposure to passive smoking, dietary variable, obesity | No association was found between Pro-Med dietary pattern and asthma severity in both groups (intermittent/persistent) of children |
| Gonzales Barcala et al.( 26 ), 2010, Spain, cross-sectional | 14 700 | 6–7 & 13–14 | Med diet | Med Diet Score§ (Mean score: 13·1 in 6–7 years; 12 in 13–14 years) Pro-Med/Anti-Med dietary pattern | ● Asthma ever ● Current asthma ● Severe asthma ● Exercise-induced asthma | ● Severe asthma: OR=2·26 (95 % CI 1·21, 4·22) | Parental smoking, BMI, maternal education | Adherence to Med diet, higher risk of severe asthma in 6–7-year-old girls. No significant association for other asthma categories in girls or boys in both age groups |
Med diet, Mediterranean diet; Pro-Med, Pro-Mediterranean dietary pattern; Anti-Med, Anti-Mediterranean dietary pattern; Contra-Med, Contra-Mediterranean dietary pattern; BHR, hyper-responsiveness.
KIDMED index, a Mediterranean diet quality index evaluating food habits in Spanish children developed by Serra-Majem et al.( 36 ).
Mediterranean diet score developed by Castro-Rodriguez et al.( 21 ) also based on the scoring system of Psaltopoulou et al.( 35 ).
Mediterranean diet score based on the score developed by Trichopoulou et al.( 34 ).
Mediterranean diet score developed by Garcia-Marcos et al.( 25 ) and based on the scoring system of Psaltopoulou et al.( 35 ).
Mediterranean dietary pattern developed by Gonzalez Barcala et al.( 26 ).
Table 2.
Characteristics of cohort and case–control studies included in the present systematic review on the Mediterranean dietary pattern and childhood asthma
| Author(s), year, location, study design | Sample size | Duration of study | Age (years) | Exposure | Tool used to evaluate adherence to Med diet | Asthma outcome measured | Exposure estimate | Confounders | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Calatayud-Saez et al.( 20 ), 2016, Spain, prospective intervention (no control group) | 104 asthmatic children | Follow-up at 1 year | 1–5 | Med diet | KIDMED index* | ● Wheezing ● Cough ● BHR ● Episodes ● Medication use ● Antibiotics ● Infections ● Hospital/emergency admissions ● Intensity of attacks | Corticosteroid therapy: ● Pre (1 year before): 3·92 (sd 1·61) ● Post (1 year after): 1·11 (sd 1·09) Bronchodilator therapy: ● Pre: 4·14 (sd 1·61) ● Post: 1·11 (sd 1·11) Symptomatic treatment: ● Pre: 7·5 (sd 2·88) ● Post: 3·4 (sd 1·24) | – | Adherence to Med diet resulted in improvement in lung function (BHR; P<0·001), decrease in episodes, bronchodilators and corticosteroids use (P=0·001). Also decrease in hospital admissions, infections and respiratory infections in asthmatic children. 32·2 % of patients remained ‘free of crisis, 35·3 % had 1 attack during the year, 24·9 % had 2 episodes v. 4·73 episodes (average) during the past year |
| Chatzi et al.( 23 ), 2008, Spain, cohort | 460 | Follow-up at 6 years | 6·5 | Med diet | KIDMED index* ≤3, low quality 4–6, medium ≥8, optimal | ● Persistent wheeze ● Atopic wheeze ● Atopy | ● Persistent wheeze: OR=0·46 (95 % CI 0·1, 2·17), P=0·529 ● Atopic wheeze: OR=0·64 (95 % CI 0·1, 4·06), P=0·902 ● Atopy: OR=0·49 (95 % CI 0·18, 1·32), P=0·213 | Gender, paternal asthma, maternal age at pregnancy, maternal asthma/atopy, social class, education, smoking and supplement use during pregnancy, breast-feeding, birth weight, no. of siblings, lower respiratory tract infection at age 1 and older, gestational age, BMI at 6·5 years | High adherence to Med diet inversely related to wheeze, but not statistically significant (P>0·05) |
| Romieu et al.( 30 ), 2009, Mexico, cohort | 208 (158 asthmatics, 50 control) | 22 weeks | 6–14 | Med diet | Med Diet Score† (Range 1–8) | ● IL-8, FEV1, FVC ● eNO ● EBC ● Asthma (mild, moderate, persistent) | – | Air pollution, gender, BMI, climate, age, temperature, corticoid use, socio-economic status (maternal education, school type), outdoor activities, atopic status, exposure to tobacco smoke, use of allergy medicine, season, vitamin supplementation | Med diet improved lung function and decreased inflammation in asthmatic children. Med diet score positively related to lung function (P-trend<0·05). High adherence to Med diet increased FEV1 by 15·3 % and FVC by 16·3 % in asthmatic children (P<0·12) v. non-asthmatics (P-trend<0·06). No statistical significant association observed for non-asthmatics (P>0·05) |
| Rice et al.( 29 ), 2015, Peru, case–control | 383 (287 asthmatic, 96 control) | – | 9–19 | Med diet | Med Diet Score‡ (Range 0-22) (Median=15) Pro-Med/Anti-Med dietary pattern | ● Current asthma ● Asthma control ● FEV1 | ● Asthma: AOR=0·55 (95 % CI 0·33, 0·92), P=0·02 ● Asthma in children with educated mothers: AOR=0·31 (95 % CI 0·14, 0·71), P<0·01 | Age, sex, BMI, maternal education | Med diet was inversely associated with asthma especially in children with educated mothers, but did not improve asthma severity. Med diet scores were not associated with asthma control (P=0·3) or FEV1 (P=0·24) in children |
Med diet, Mediterranean diet; –, not indicated in study; Pro-Med, Pro-Mediterranean dietary pattern; Anti-Med, Anti-Mediterranean dietary pattern; BHR, bronchial hyper-responsiveness; FEV1, forced expiratory volume 1 (spirometry measure); FVC, forced vital capacity (spirometry measure); eNO, exhaled nitric oxide level; EBC, exhaled breathe condensate; AOR, adjusted odds ratio.
KIDMED index, a Mediterranean diet quality index evaluating food habits in Spanish children developed by Serra-Majem et al.( 36 ).
Mediterranean diet score based on the score developed by Trichopoulou et al.( 34 ).
In six of these studies( 17 , 21 , 25 , 26 , 28 , 29 ) a score was allocated according to frequency of intake, whereas in the study undertaken by Silveira et al., adherence to the Mediterranean dietary pattern was measured qualitatively. Intake of at least five foods in each dietary pattern at a frequency of at least 3 times/week was classified as ‘yes’( 31 ).
Summarizing the findings of the literature search, the majority of studies reported a beneficial effect of adherence to a Mediterranean dietary pattern on asthma in children. Overall, twelve of these studies reported an inverse association between children’s adherence to the Mediterranean diet and asthma symptoms( 18 – 25 , 27 – 30 ) and/or improvement in lung function( 20 , 30 ), although the results of two studies were not statistically significant( 22 , 23 ). On the other hand, two studies documented no association between Mediterranean diet and asthma symptoms( 17 , 31 ) and one an increase in asthma symptoms( 26 ).
Quality assessment
After assessment of the quality of each study included the averaged quality score was 79 %, the highest score was 88 % and lowest score was 64 % (Table 3). Almost all studies (14/15) were of high quality( 17 – 19 , 20 – 31 ) as they described the study population, measured the exposure and outcome clearly, used appropriate statistical analysis and considered bias in the analysis or discussed any potential bias. The only low-quality study (Calatayud-Saez et al.) suffered from inappropriate statistical analysis and lack of consideration of potential bias such as non-response and dropout bias that led to unreliable results and ambiguity in study population characteristics which made it difficult to compare the results against other studies( 20 ). Due to heterogeneity among study methodologies, namely differences between age, exposure measurements and outcome measures, meta-analysis of the fifteen observational studies was deemed inappropriate.
Table 3.
Summary table of quality assessment* of relevant studies included in the present systematic review on the Mediterranean dietary pattern and childhood asthma
| Study | Population | Population | Time | Outcome | Eligibility | Exposure measures | Outcome measures | Statistical test | Adjustment for | Bias | Bias not | Overall mean | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Reviewers | design | density | description | points | measures | criteria | Validity | Reliability | Validity | Reliability | suitable | confounders | discussed | covered | score (%) |
| Calatayud-Saez et al.( 20 ), 2016 | N.H.S./M.M.P. | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | × | 64 |
| Antonogeorgos et al. ( 18 ), 2014 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 75 |
| Arvaniti et al.( 19 ), 2011 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 79 |
| Grigoropoulou et al.( 27 ), 2011 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 82 |
| Nagel et al.( 28 ), 2010 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 86 |
| Garcia-Marcos et al.( 25 ), 2007 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 74 |
| Castro-Rodriguez et al.( 21 ), 2008 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 79 |
| Chatzi et al.( 23 ), 2008 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 88 |
| Chatzi et al.( 22 ), 2007 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 79 |
| de Batlle et al.( 24 ), 2008 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 75 |
| Romieu et al.( 30 ), 2009 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 88 |
| Gonzales Barcala et al.( 26 ), 2010 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 77 |
| Rice et al.( 29 ), 2015 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 82 |
| Akcay et al.( 17 ), 2014 | N.H.S./M.M.P. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 75 |
| Silviera et al.( 31 ), 2015 | N.H.S./M.M.P. | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 81 |
✓, assessment criteria satisfied; ×, assessment criteria not satisfied.
Using validated quality assessment tools modified from Zaza et al.( 16 ).
Discussion
The current systematic review identified recent evidence suggesting that adherence to a Mediterranean dietary pattern is inversely related to, and provides a potentially protective effect against, asthma symptoms in children residing in Mediterranean and non-Mediterranean regions( 18 – 25 , 27 – 30 ). The majority of studies documented a reduction in wheeze( 19 , 21 – 24 , 27 , 28 ), nocturnal cough( 22 ), exercise wheeze( 19 , 27 ) asthma episodes( 20 ), hospital admissions( 20 ), medication use( 20 ) and improvement in lung function( 20 , 30 ). A one-unit increase in the KIDMED score was associated with a 14–16 % lower likelihood of having asthma symptoms( 19 , 27 ) irrespective of potential confounders.
Our qualitative synthesis showed that for ten out of the twelve observational studies documenting a protective effect, statistically significant findings were observed for high adherence to the Mediterranean dietary pattern and asthma symptoms even though heterogeneity existed among study methodologies, namely Mediterranean diet scores, cut-off points, FFQ and asthma outcomes( 18 , 20 , 21 , 24 , 25 , 27 – 30 , 32 ). These findings coincide with two earlier systematic reviews( 13 , 37 ) and one meta-analysis( 13 ) investigating the role of the Mediterranean diet in relation to childhood asthma that was performed on seven observational studies (cross-sectional)( 19 , 21 – 25 , 28 ) included in our manuscript. Both systematic reviews documented that despite the heterogeneity and inherent limitations of cross-sectional studies included, the evidence is suggestive of a protective effect between the Mediterranean diet and asthma in children, particularly in Mediterranean areas( 13 ).
A possible explanation for the beneficial/prophylactic effects observed is that the Mediterranean diet is characterized by low consumption of red meat and saturated fats, high intakes of fruit, vegetables, wholegrain cereals, legumes and fish, and abundance of olive oil, which are rich in antioxidants (vitamins A, C and E, β-carotene, polyphenols, glutathione, lycopene, flavonoids), micronutrients (Mg, Se, Zn) and vitamin D( 9 , 12 ). These bioactive compounds may prevent or limit inflammatory responses in the airways by reducing reactive oxygen species and inhibiting lipid peroxidation, thus reducing asthma symptoms. In addition, the high content of long-chain n-3 PUFA found in fish triggers the production of EPA-derived eicosanoids which have anti-inflammatory effects and influence the differentiation of T-lymphocytes modulating immune responses, thereby also improving pulmonary function and decreasing asthma symptoms( 38 ).
In contrast, two studies reported no association( 17 , 31 ) and one an adverse effect( 26 ) of adherence to a Mediterranean dietary pattern in asthmatic children. In the study undertaken by Gonzales Barcala et al.( 26 ), adherence to the Mediterranean diet was associated with an increase in asthma symptoms in children with ‘severe asthma’. This outcome may have been due to a reverse-causal effect. It is well established that the family environment, particularly parents, plays a major role in the dietary habits of young children( 39 , 40 ). More specifically, in those families with children suffering from severe asthma, parents may improve the quality of the child’s diet in an effort to improve overall health. No association was reported by Silveira et al.( 31 ) in the study examining the impact of adherence to a Mediterranean diet in children with persistent and intermittent asthma. A possible explanation may be the coexistence of other environmental factors not analysed in their study that could modify the prevalence or severity of asthma. Possible limitations of that study are the small sample size and no tool such as the Asthma Control Questionnaire was used to evaluate asthma severity. Also, mild, moderate and severe persistent asthma were categorized collectively as ‘persistent asthma’ rather than being assessed separately, which may have led to some effects being overlooked. Medication remains the cornerstone of asthma management. Perhaps medication use might have masked any beneficial effects of the Mediterranean diet. Regarding the study undertaken by Akcay et al.( 17 ) in adolescents, no association was reported between adherence to the Mediterranean diet and asthma symptoms. Adolescence is a period when youth defy authority, especially parental advice, gain autonomy and are influenced by peer-group pressure. Adolescents are known to practise poor dietary habits including high intakes of fast foods, sweets and soft drinks, which are rich sources of saturated fats, sugar and salt, and have low intakes of nutritious foods such as fruit, vegetables, cereals and fish that are high in fibre, antioxidants and n-3 fatty acids( 41 , 42 ). These poor dietary habits may have concealed the beneficial effects of adherence to a Mediterranean dietary pattern, hence explaining why no association was documented. In addition, Akcay et al. mentioned that adolescents had a high consumption of pickled and salted foods. Research has shown that a high intake of salt is associated with asthma symptoms( 32 , 43 ). In addition, adolescents have been known to misreport dietary intake( 44 , 45 ).
Strengths/limitations of studies reviewed
Limitations must be considered in the present systematic review, some of which may be due to gaps in the literature. There was heterogeneity in study design, age groups considered, time periods of exposure, sample population (asthmatics v. non-asthmatics), outcome measures, outcome parameters and associations studied, thus limiting the possibility of drawing strong and consistent conclusions. The majority of studies reviewed were cross-sectional and hence a cause–effect relationship cannot be determined; however, hypotheses might be suggested for further exploration in more robust clinical trials. Diversity in results documented may be due to differences in the design of FFQ used to collect information on the dietary habits of children; for example, number of food items included and frequency of food consumption categories. Some FFQ were not validated( 17 , 22 , 29 ), however research has shown that FFQ produce valid and reproducible estimates of dietary intake of children and adolescents( 46 ). Another weakness in these studies is that dietary questionnaires were self-administered or completed by parents, which may have led to recall or information bias. On the other hand, research often uses parents as proxy reporters for children’s dietary intake( 47 ) and parental report of children’s fruit and vegetable intake is an accurate estimate( 48 ). Regarding assessment of asthma outcome, respiratory function was evaluated using a questionnaire and by parent report of symptoms. This method is inferior to the use of pulmonary function tests such as spirometry( 49 ). In studies undertaken in non-English speaking countries, the ISAAC questionnaire had been translated but not validated for that specific population( 17 , 18 , 22 ). Cultural differences cannot be excluded in the assessment of asthma symptoms and report of wheezing, as was delineated by the differences in asthma outcome in the fifteen studies analysed. It is well recognized that, in children younger than 3 years, wheezing is often transient due to respiratory infection and diminishes as the child grows older( 49 , 50 ). Regarding differences in Mediterranean dietary scores used to assess adherence, not all scores have been developed for use in children and adolescents( 34 , 35 ).
A strength is the extensive literature search focusing exclusively on the Mediterranean dietary pattern as opposed to food groups or nutrients, although publication bias cannot be dismissed. Nevertheless, the studies reviewed were of high quality. In comparison to studies investigating the effect of nutrients or single food groups, the use of a Mediterranean diet score takes account of the synergistic effect or interactions between foods and nutrients( 12 ), as dietary scores are designed to reflect the whole dietary pattern. In addition, the use of scores improves the statistical power as compared with single nutrients or food groups that might account for small effects. The present systematic review highlights the need for future clinical trials investigating the effect of a Mediterranean dietary pattern on asthma symptoms in order to verify the promising findings documented in the literature. To enhance validity and reliability of the results published, there is a need for homogeneity between study methodologies and statistical tests in evaluation of the data compiled.
Conclusion
In conclusion, the present systematic review assessed evidence for the effectiveness of a Mediterranean dietary pattern in childhood asthma. Although the available evidence is limited, it is nevertheless supportive that adherence to a Mediterranean dietary pattern may reduce asthma symptoms in children. However, well-designed randomized controlled trials are warranted to confirm the prophylactic effects of this dietary pattern. The present findings have important public health implications because they suggest a non-pharmacological means for preventing childhood asthma.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: All authors have contributed equally in the literature search, analysis of data published and manuscript writing, and each has seen and approved the final version of the manuscript submitted. Ethics of human subject participation: Not applicable.
Appendix 1
Websites accessed
PUBMED: http://www.ncbi.nlm.nih.gov/ (accessed 29 October 2016).
MEDLINE: http://www.ovidsp.tx.ovid.com (accessed 29 October 2016).
EMBASE: http://www.ovidsp.tx.ovid.com (accessed 29 October 2016).
Cochrane Central Registry of Controlled trials: http://onlinelibrary.wiley.com (accessed 29 October 2016).
EBSCO (CINAHL): http://www.web.b.ebxco.host.com (accessed 29 October 2016).
SCOPUS: https://www-scopus-com (accessed 29 October 2016).
International clinical trials registry: http://www.clinicaltrials.gov (accessed 29 October 2016).
Australian & New Zealand Clinical Trials Registry (ANZCTR): http://www.anzctr.org.au (accessed 29 October 2016).
European Clinical Trials Registry: https://www.clinicaltrialsregister.eu (accessed 29 October 2016).
Appendix 2
Details of PUBMED database search: Medical Subject Headings (MESH) terms
(Mediterranean [All Fields] AND (‘diet’ [MeSH Terms] OR ‘diet’ [All Fields] OR ‘dietary’ [All Fields]) AND pattern [All Fields]) OR (‘diet, mediterranean’ [MeSH Terms] OR (‘diet’ [All Fields] AND ‘mediterranean’ [All Fields]) OR ‘mediterranean diet’ [All Fields] OR (‘mediterranean’ [All Fields] AND ‘diet’ [All Fields])) OR (Mediterranean-type [All Fields] AND (‘diet’ [MeSH Terms] OR ‘diet’ [All Fields])) OR (Mediterranean [All Fields] AND (‘food’ [MeSH Terms] OR ‘food’ [All Fields]) AND pattern [All Fields]) OR ((‘diet’ [MeSH Terms] OR ‘diet ’[All Fields] OR ‘dietary’ [All Fields]) AND pattern [All Fields]) AND (‘asthma’ [MeSH Terms] OR ‘asthma’ [All Fields]) AND (‘child’ [MeSH Terms] OR ‘child’ [All Fields] OR ‘children’ [All Fields])) OR ((((Mediterranean [All Fields] AND (‘diet’ [MeSH Terms] OR ‘diet’ [All Fields] OR ‘dietary’ [All Fields]) AND pattern [All Fields]) OR (‘diet, Mediterranean’ [MeSH Terms] OR (‘diet’ [All Fields] AND ‘mediterranean’ [All Fields]) OR ‘mediterranean diet’ [All Fields] OR (‘mediterranean’ [All Fields] AND ‘diet’ [All Fields])) OR (Mediterranean-type [All Fields] AND (‘diet’ [MeSH Terms] OR ‘diet’ [All Fields])) OR (Mediterranean [All Fields] AND (‘food’ [MeSH Terms] OR ‘food’ [All Fields]) AND pattern [All Fields]) OR ((‘diet’ [MeSH Terms] OR ‘diet’ [All Fields] OR ‘dietary’ [All Fields]) AND pattern [All Fields])) AND (‘Childhood’ [Journal] OR ‘childhood’ [All Fields])) AND (‘asthma’ [MeSH Terms] OR ‘asthma’ [All Fields])) Sort by: Relevance
Appendix 3
PUBMED database search details
| Search no. | PUBMED search details | No. of articles retrieved |
|---|---|---|
| 3 | Search ((Mediterranean dietary pattern OR Mediterranean diet OR Mediterranean-type diet OR Mediterranean food pattern OR dietary pattern AND asthma AND children)) OR (Mediterranean dietary pattern OR Mediterranean diet OR Mediterranean-type diet OR Mediterranean food pattern OR dietary pattern AND childhood AND asthma) | 88 |
| 2 | Search (((Mediterranean dietary pattern OR Mediterranean diet OR Mediterranean-type diet OR Mediterranean food pattern OR dietary pattern)) AND childhood) AND asthma | 49 |
| 1 | Search (Mediterranean dietary pattern OR Mediterranean diet OR Mediterranean-type diet OR Mediterranean food pattern OR dietary pattern AND asthma AND children) | 83 |
Articles retrieved from https://www.ncbi.nlm.nih.gov/pubmed (accessed 29 October 2016).
Appendix 4
Screenshot of EMBASE database search
References
- 1. Devereux G (2006) The increase in the prevalence of asthma and allergy: food for thought. Nat Rev Immunol 6, 869–874. [DOI] [PubMed] [Google Scholar]
- 2. Hopkin JM (2012) The diagnosis of asthma, a clinical syndrome. Thorax 67, 660–662. [DOI] [PubMed] [Google Scholar]
- 3. Eder W, Ege MJ & von Mutius E (2006) The asthma epidemic. N Engl J Med 355, 2226–2235. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization (2013) Asthma. Fact sheet no. 307. http://www.who.int/mediacentre/factsheets/fs307/en/ (accessed November 2015).
- 5. Asher M, Anderson H, Stewart A et al. (1998) Worldwide variations in the prevalence of asthma symptoms: the International Study of Asthma and Allergies in Childhood (ISAAC). Eur Respir J 12, 315–335. [DOI] [PubMed] [Google Scholar]
- 6. Lai C, Beasley R, Crane J et al. (2009) Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 64, 476–483. [DOI] [PubMed] [Google Scholar]
- 7. Trichopoulou A (2001) Mediterranean diet: the past and the present. Nutr Metab Cardiovasc Dis 11, 1–4. [PubMed] [Google Scholar]
- 8. Simopoulos AP (2001) The Mediterranean diets: what is so special about the diet of Greece? The scientific evidence. J Nutr 131, 11 Suppl., 3065S–3073S. [DOI] [PubMed] [Google Scholar]
- 9. Willett WC, Sacks F, Trichopoulou A et al. (1995) Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 61, 6 Suppl., 1402S–1406S. [DOI] [PubMed] [Google Scholar]
- 10. Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13, 3–9. [DOI] [PubMed] [Google Scholar]
- 11. Sofi F, Cesari F, Abbate R et al. (2008) Adherence to Mediterranean diet and health status: meta-analysis. BMJ 337, a1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Trichopoulou A & Lagiou P (1997) Healthy traditional Mediterranean diet: an expression of culture, history, and lifestyle. Nutr Rev 55, 383–389. [DOI] [PubMed] [Google Scholar]
- 13. Garcia‐Marcos L, Castro‐Rodriguez J, Weinmayr G et al. (2013) Influence of Mediterranean diet on asthma in children: a systematic review and meta‐analysis. Pediatr Allergy Immunol 24, 330–338. [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J et al. (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Ann Intern Med 151, 264–269. [DOI] [PubMed] [Google Scholar]
- 15. Liberati A, Altman D, Tetzlaff J et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6, e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zaza S, Wright-De Aguero LK, Briss PA et al. (2000) Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Task Force on Community Preventive Services. Am J Prev Med 18, 44–74. [DOI] [PubMed] [Google Scholar]
- 17. Akcay A, Tamay Z, Hocaoglu AB et al. (2014) Risk factors affecting asthma prevalence in adolescents living in Istanbul, Turkey. Allergol Immunopathol (Madr) 42, 449–458. [DOI] [PubMed] [Google Scholar]
- 18. Antonogeorgos G, Panagiotakos D, Grigoropoulou D et al. (2014) Investigating the associations between Mediterranean diet, physical activity and living environment with childhood asthma using path analysis. Endocr Metab Immune Disord Drug Targets 14, 226–233. [DOI] [PubMed] [Google Scholar]
- 19. Arvaniti F, Priftis KN, Papadimitriou A et al. (2011) Adherence to the Mediterranean type of diet is associated with lower prevalence of asthma symptoms, among 10–12 years old children: the PANACEA study. Pediatr Allergy Immunol 22, 283–289. [DOI] [PubMed] [Google Scholar]
- 20. Calatayud-Saez FM, Calatayud Moscoso Del Prado B, Gallego Fernandez-Pacheco JG et al. (2016) Mediterranean diet and childhood asthma. Allergol Immunopathol (Madr) 44, 99–105. [DOI] [PubMed] [Google Scholar]
- 21. Castro-Rodriguez JA, Garcia-Marcos L, Alfonseda Rojas JD et al. (2008) Mediterranean diet as a protective factor for wheezing in preschool children. J Pediatr 152, 823–828 828.e1–2. [DOI] [PubMed] [Google Scholar]
- 22. Chatzi L, Apostolaki G, Bibakis I et al. (2007) Protective effect of fruits, vegetables and the Mediterranean diet on asthma and allergies among children in Crete. Thorax 62, 677–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chatzi L, Torrent M, Romieu I et al. (2008) Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax 63, 507–513. [DOI] [PubMed] [Google Scholar]
- 24. de Batlle J, Garcia-Aymerich J, Barraza-Villarreal A et al. (2008) Mediterranean diet is associated with reduced asthma and rhinitis in Mexican children. Allergy 63, 1310–1316. [DOI] [PubMed] [Google Scholar]
- 25. Garcia-Marcos L, Canflanca IM, Garrido JB et al. (2007) Relationship of asthma and rhinoconjunctivitis with obesity, exercise and Mediterranean diet in Spanish schoolchildren. Thorax 62, 503–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gonzalez Barcala FJ, Pertega S, Bamonde L et al. (2010) Mediterranean diet and asthma in Spanish schoolchildren. Pediatr Allergy Immunol 21, 1021–1027. [DOI] [PubMed] [Google Scholar]
- 27. Grigoropoulou D, Priftis KN, Yannakoulia M et al. (2011) Urban environment adherence to the Mediterranean diet and prevalence of asthma symptoms among 10- to 12-year-old children: The Physical Activity, Nutrition, and Allergies in Children Examined in Athens study. Allergy Asthma Proc 32, 351–358. [DOI] [PubMed] [Google Scholar]
- 28. Nagel G, Weinmayr G, Kleiner A et al. (2010) Effect of diet on asthma and allergic sensitisation in the International Study on Allergies and Asthma in Childhood (ISAAC) Phase Two. Thorax 65, 516–522. [DOI] [PubMed] [Google Scholar]
- 29. Rice JL, Romero KM, Galvez Davila RM et al. (2015) Association between adherence to the Mediterranean diet and asthma in Peruvian children. Lung 193, 893–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Romieu I, Barraza-Villarreal A, Escamilla-Nunez C et al. (2009) Dietary intake, lung function and airway inflammation in Mexico City school children exposed to air pollutants. Respir Res 10, 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Silveira DH, Zhang L, Prietsch SOM et al. (2015) Association between dietary habits and asthma severity in children. Indian Pediatr 52, 25–30. [DOI] [PubMed] [Google Scholar]
- 32. Arvaniti F, Priftis KN, Papadimitriou A et al. (2011) Salty-snack eating, television or video-game viewing, and asthma symptoms among 10- to 12-year-old children: the PANACEA study. J Am Diet Assoc 111, 251–257. [DOI] [PubMed] [Google Scholar]
- 33. Asher M, Keil U, Anderson H et al. (1995) International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 8, 483–491. [DOI] [PubMed] [Google Scholar]
- 34. Trichopoulou A, Costacou T, Bamia C et al. (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348, 2599–2608. [DOI] [PubMed] [Google Scholar]
- 35. Psaltopoulou T, Naska A, Orfanos P et al. (2004) Olive oil, the Mediterranean diet, and arterial blood pressure: the Greek European Prospective Investigation into Cancer and Nutrition (EPIC) study. Am J Clin Nutr 80, 1012–1018. [DOI] [PubMed] [Google Scholar]
- 36. Serra-Majem L, Ribas L, Ngo J et al. (2004) Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr 7, 931–935. [DOI] [PubMed] [Google Scholar]
- 37. Nurmatov U, Devereux G & Sheikh A (2011) Nutrients and foods for the primary prevention of asthma and allergy: systematic review and meta-analysis. J Allergy Clin Immunol 127, 724–733.e1–e30. [DOI] [PubMed] [Google Scholar]
- 38. Patterson E, Wall R, Fitzgerald G et al. (2012) Health implications of high dietary omega-6 polyunsaturated fatty acids. J Nutr Metab 2012, 539426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Birch LL & Fisher JO (1998) Development of eating behaviors among children and adolescents. Pediatrics 101, 539–549. [PubMed] [Google Scholar]
- 40. Patrick H & Nicklas TA (2005) A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr 24, 83–92. [DOI] [PubMed] [Google Scholar]
- 41. Jenkins S & Horner SD (2005) Barriers that influence eating behaviors in adolescents. J Pediatr Nurs 20, 258–267. [DOI] [PubMed] [Google Scholar]
- 42. Story M, Neumark-Sztainer D & French S (2002) Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc 102, 3 Suppl., S40–S51. [DOI] [PubMed] [Google Scholar]
- 43. Corbo GM, Forastiere F, De Sario M et al. (2008) Wheeze and asthma in children: associations with body mass index, sports, television viewing, and diet. Epidemiology 19, 747–755. [DOI] [PubMed] [Google Scholar]
- 44. Forrestal SG (2011) Energy intake misreporting among children and adolescents: a literature review. Matern Child Nutr 7, 112–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Livingstone M, Robson P & Wallace J (2004) Issues in dietary intake assessment of children and adolescents. Br J Nutr 92, Suppl. 2, S213–S222. [DOI] [PubMed] [Google Scholar]
- 46. Rockett HR & Colditz GA (1997) Assessing diets of children and adolescents. Am J Clin Nutr 65, 4 Suppl., 1116S–1122S. [DOI] [PubMed] [Google Scholar]
- 47. Livingstone MB & Robson PJ (2000) Measurement of dietary intake in children. Proc Nutr Soc 59, 279–293. [DOI] [PubMed] [Google Scholar]
- 48. Byers T, Trieber F, Gunter E et al. (1993) The accuracy of parental reports of their children’s intake of fruits and vegetables: validation of a food frequency questionnaire with serum levels of carotenoids and vitamins C, A, and E. Epidemiology 4, 350–355. [PubMed] [Google Scholar]
- 49. Katsardis C, Koumbourlis AC, Anthracopoulos MB et al. (2015) Paediatric Pulmonary Function Testing: Indications and Interpretation . Hauppauge. NY: Nova Science Publishers, Inc. [Google Scholar]
- 50. Heymann PW, Carper HT, Murphy DD et al. (2004) Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezing. J Allergy Clin Immunol 114, 239–247. [DOI] [PMC free article] [PubMed] [Google Scholar]


