Abstract
Background
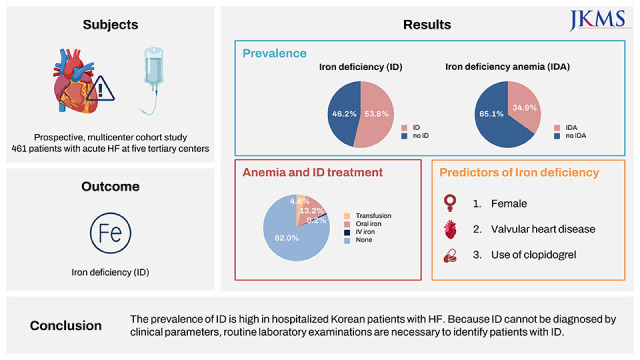
Although iron deficiency (ID) is an important and treatable risk factor for heart failure (HF), data on ID are scarce in Asian patients with HF. Therefore, we sought to determine the prevalence and clinical characteristics of ID in hospitalized Korean patients with HF.
Methods
In this prospective, multicenter cohort study, 461 patients with acute HF seen at five tertiary centers from January to November 2019 in Korea were enrolled. ID was defined as serum ferritin < 100 μg/L or ferritin 100–299 μg/L in combination with transferrin saturation < 20%.
Results
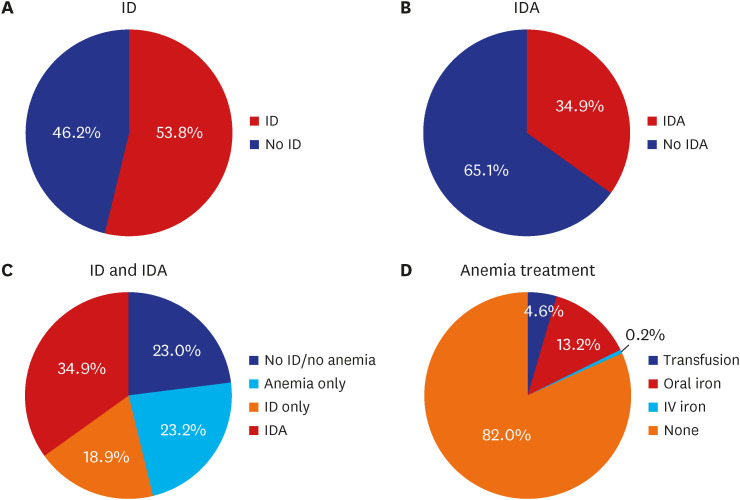
The patients’ mean age was 67.6 ± 14.9 years, and 61.8% were male. Among total 461 patients, ID was present in 248 patients (53.8%). The prevalence of ID was significantly higher in women than in men (65.3% vs. 47.3%, P < 0.001). In a multivariable logistic regression analysis, the independent predictors of ID were female sex (odds ratio [OR], 2.19; 95% confidence interval [CI], 1.47–3.30), valvular heart disease (OR, 2.10; 95% CI, 1.10–4.17), higher heart rate (OR, 1.10; 95% CI, 1.01–1.21), anemia (OR, 1.60; 95% CI, 1.07–2.40), and the use of clopidogrel (OR, 1.56; 95% CI, 1.00–2.45). Among women, the prevalence of ID did not significantly differ between younger and older women (< 65 years: 73.7% vs. ≥ 65 years: 63.0%, P = 0.222), those with low and high body mass index (BMI < 25 kg/m2: 66.2% vs. BMI ≥ 25 kg/m2: 69.6%, P = 0.703), or those with low and high natriuretic peptide (NP) levels (NP < median: 69.8% vs. NP ≥ median: 61.1%, P = 0.295). Only 0.2% patients with acute HF received intravenous iron supplementation in Korea.
Conclusion
The prevalence of ID is high in hospitalized Korean patients with HF. Because ID cannot be diagnosed by clinical parameters, routine laboratory examinations are necessary to identify patients with ID.
Trial Registration
ClinicalTrials.gov Identifier: NCT04812873
Keywords: Iron Deficiency, Iron Deficiency Anemia, Heart Failure, Anemia
Graphical Abstract
INTRODUCTION
Iron is an important trace element and an essential component of hemoglobin, myoglobin, cytochromes, and proteins responsible for oxygen storage, transport, and utilization.1,2,3 It is critical for oxidative energy generation. Therefore, cells with high energy demand, such as cardiac myocytes, are especially sensitive to iron underutilization.4 Iron deficiency (ID), regardless of the presence of anemia, can manifest as reduced quality of life, exercise capacity,5 and survival.6
The prevalence of ID ranges between 2% and 10% in the general population.7,8 In patients with heart failure (HF), dietary iron intake9 and enteral absorption are reduced10 and systemic inflammation is elevated,11 with prevalence of ID being as high as 50–60%.12,13,14 Patients with ID had worse prognosis,13,15,16 but its correction with intravenous (IV) iron supplementation improved the clinical outcomes.17,18,19,20
Despite the clinical importance of ID in HF, data on its prevalence are scarce, especially in East Asians.21 Therefore, in this prospective, multicenter study, we sought for the first time to determine the prevalence and risk factors of ID and ID anemia (IDA) in Korean patients with HF.
METHODS
Study population
In the FErrous Renown and UpShot in Korean Acute Heart Failure Patients (FERUS-HF) study, we prospectively enrolled patients hospitalized for acute HF at five tertiary university hospitals from January to November 2019 in Korea (clinical trials.gov: NCT04812873). Patients ≥ 19 years of age who had objective findings of structural and/or functional disorder of the heart with one of the following criteria were enrolled: 1) symptoms of HF, 2) signs of HF, or 3) lung congestion in chest X-ray. Patients who declined consent were excluded. Total 465 patients were enrolled initially in this study, and 4 patients were additionally excluded because of missing laboratory tests.
Study variables and definitions
Routine blood sampling and tests were conducted by laboratories at each center that were certified by the Korean Association of Quality Assurance for Clinical Laboratory at the index admission. Laboratory measurements regarding iron status were performed in laboratories of the participating centers after study enrollment and before discharge. Hematological measurements were performed using fresh venous blood with ethylenediaminetetraacetic acid. Ferritin (ng/mL), serum iron (μg/dL), total iron binding capacity (TIBC, μg/dL), and transferrin (mg/dL) were measured directly. Transferrin saturation was calculated as the ratio of serum iron and TIBC multiplied by 100. ID was defined as serum ferritin < 100 μg/L or ferritin 100–299 μg/L in combination with transferrin saturation of < 20%.18,19 Anemia was defined as a hemoglobin concentration of < 12 g/dL in women and < 13 g/dL in men. IDA was defined as the presence of both ID and anemia. Chronic kidney disease (CKD) was defined as estimated glomerular filtration rate < 60 mL/min/1.73 m2.
All echocardiographic studies were performed using a standard ultrasound machine with a 2.5-MHz probe. Left ventricular ejection fraction (LVEF) was measured using Simpson’s biplane method unless this method was not possible. Based on the echocardiographic findings performed at the index acute HF hospitalization, patients were classified into those with HF with reduced ejection fraction (LVEF ≤ 40%), HF with mildly reduced ejection fraction (LVEF, 41–49%), and HF with preserved ejection fraction (LVEF ≥ 50%).22,23,24 Valvular heart disease was defined as greater than mild stenosis or regurgitation, and previous valve surgery.
The primary endpoint was the prevalence of ID and IDA. Anemia and ID treatment was investigated between study enrollment and discharge.
Statistical analysis
Categorical variables are reported as frequencies (percentages). Continuous variables are expressed as means ± standard deviations or medians with interquartile ranges. For comparison between groups, the χ2 test (or Fisher’s exact test when any expected cell count was < 5 for a 2 × 2 table) was used for categorical variables, while the unpaired Student’s t-test or Mann-Whitney U test were used for continuous variables. A logistic regression model was used to determine the predictor of ID and IDA. Variables found to be statistically significant (P < 0.1) in the univariable analysis were included in the final multivariable model, except for variables with > 10% missing values or variables that were closely related to the other variables.
All tests were two-tailed, and a P value < 0.05 was considered statistically significant. Statistical analyses were performed by using R version 4.2.0 (The R Foundation for Statistical Computing, Vienna, Austria) and SAS Version 9.4 (SAS Institute, Cary, NC, USA) by a professional statistician.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-1811/504-302). Informed consent was submitted by all subjects when they were enrolled. This study complied with the principles of the Declaration of Helsinki.
RESULTS
Patients
Finally, we analyzed 461 patients with acute HF (Table 1). The mean age was 67.6 ± 14.9 years, and 61.8% were male. Furthermore, 53.2% had hypertension, 38.6% had diabetes, 37.6% had atrial fibrillation, 60.1% had CKD, and 17.8% were current smokers. The mean LVEF was 35.4 ± 16.1%. Based on the hematological measurements, the following mean values were noted: hemoglobin, 12.1 ± 2.4 g/dL; iron, 65.0 ± 39.3 µg/dL; TIBC, 290.5 ± 82.7 µg/dL; transferrin saturation, 23.6 ± 14.6% and ferritin, 224.6 ± 453.8 ng/mL. Regarding antithrombotic medication, 11.3%, 34.5%, 36.9%, and 28.6% received warfarin, new oral anticoagulants, aspirin, and P2Y12 inhibitors, respectively.
Table 1. Baseline characteristics of the study population.
| Characteristics | All patients (N = 461) | ID | IDA | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ID (n = 248) | No ID (n = 213) | P value | IDA (n = 161) | No IDA (n = 300) | P value | ||||
| Age, yr | 67.6 ± 14.9 | 68.0 ± 14.9 | 67.2 ± 15.0 | 0.445 | 71.5 ± 12.1 | 65.51 ± 15.9 | < 0.001 | ||
| Men | 285 (61.8) | 133 (53.6) | 152 (71.4) | < 0.001 | 87 (54.0) | 198 (66.0) | 0.012 | ||
| Body mass index, kg/m2 (n = 291) | 24.7 ± 5.0 | 24.5 ± 4.8 | 25.0 ± 5.3 | 0.445 | 23.5 ± 3.8 | 25.26 ± 5.4 | 0.012 | ||
| De novo HF | 169 (36.7) | 100 (40.3) | 69 (32.4) | 0.096 | 55 (34.2) | 114 (38.0) | 0.475 | ||
| Ischemic etiology | 110 (23.8) | 65 (26.2) | 45 (21.1) | 0.243 | 46 (28.6) | 64 (21.3) | 0.105 | ||
| Comorbidities | |||||||||
| Hypertension | 245 (53.2) | 135 (54.4) | 110 (51.6) | 0.549 | 88 (54.7) | 157 (52.3) | 0.633 | ||
| Diabetes mellitus | 178 (38.6) | 107 (43.2) | 71 (33.3) | 0.031 | 78 (48.5) | 100 (33.3) | 0.002 | ||
| Chronic kidney disease | 277 (60.1) | 145 (58.5) | 132 (62.0) | 0.503 | 104 (66.2) | 173 (56.9) | 0.066 | ||
| Ischemic heart disease | 159 (34.5) | 90 (36.3) | 69 (32.4) | 0.380 | 64 (39.8) | 95 (31.7) | 0.082 | ||
| Valvular heart disease | 50 (10.9) | 35 (14.1) | 15 (7.0) | 0.015 | 27 (16.8) | 23 (7.7) | 0.003 | ||
| Atrial fibrillation | 173 (37.6) | 90 (36.4) | 83 (39.0) | 0.577 | 59 (36.9) | 114 (38.0) | 0.813 | ||
| COPD | 53 (11.5) | 27 (10.9) | 26 (12.2) | 0.658 | 19 (11.8) | 34 (11.3) | 0.881 | ||
| Cerebrovascular disease | 38 (8.2) | 19 (7.7) | 19 (8.9) | 0.624 | 18 (11.2) | 20 (6.7) | 0.093 | ||
| Malignancy | 39 (8.5) | 24 (9.7) | 15 (7.0) | 0.311 | 16 (9.9) | 23 (7.7) | 0.404 | ||
| Current smoking | 82 (17.8) | 37 (14.9) | 45 (21.1) | 0.082 | 15 (9.3) | 67 (22.3) | < 0.001 | ||
| Physical exam (at admission) | |||||||||
| Systolic BP, mmHg | 121.2 ± 25.7 | 123.1 ± 27.5 | 119.1 ± 23.4 | 0.310 | 123.6 ± 27.6 | 119.9 ± 24.6 | 0.371 | ||
| Diastolic BP, mmHg | 73.0 ± 17.8 | 74.0 ± 17.7 | 71.9 ± 18.0 | 0.214 | 70.8 ± 15.4 | 74.2 ± 18.9 | 0.089 | ||
| Heart rate, beats/min | 85.3 ± 22.2 | 87.2 ± 22.8 | 83.0 ± 21.3 | 0.046 | 83.6 ± 21.1 | 86.2 ± 22.7 | 0.265 | ||
| Laboratory test results | |||||||||
| Iron, µg/dL | 65.0 ± 39.3 | 52.0 ± 33.3 | 80.2 ± 40.4 | < 0.001 | 45.9 ± 33.2 | 75.3 ± 38.6 | < 0.001 | ||
| TIBC, µg/dL | 290.5 ± 82.7 | 316.7 ± 85.0 | 260.0 ± 68.6 | < 0.001 | 301.5 ± 68.0 | 284.6 ± 89.2 | 0.008 | ||
| Transferrin saturation, % | 23.6 ± 14.6 | 16.7 ± 9.4 | 31.6 ± 15.4 | < 0.001 | 15.5 ± 9.6 | 27.9 ± 15.0 | < 0.001 | ||
| Ferritin, ng/mL | 224.6 ± 453.8 | 80.5 ± 60.3 | 392.4 ± 624.5 | < 0.001 | 81.6 ± 63.2 | 301.4 ± 545.6 | < 0.001 | ||
| Hemoglobin, mg/dL | 12.1 ± 2.4 | 11.8 ± 2.3 | 12.5 ± 2.5 | 0.001 | 10.4 ± 1.3 | 13.0 ± 2.4 | < 0.001 | ||
| Anemia | 268 (58.1) | 161 (64.9) | 107 (50.2) | 0.001 | 161 (100.0) | 107 (35.7) | < 0.001 | ||
| WBC, 109/L | 7.47 ± 2.94 | 7.24 ± 2.85 | 7.73 ± 3.03 | 0.121 | 6.91 ± 2.79 | 7.77 ± 2.98 | 0.002 | ||
| Platelet, 109/L | 213.5 ± 82.3 | 218.5 ± 79.5 | 207.8 ± 85.2 | 0.152 | 216.6 ± 85.7 | 211.9 ± 80.4 | 0.911 | ||
| BUN, mg/dL | 28.8 ± 17.1 | 28.6 ± 16.5 | 29.1 ± 17.8 | 0.787 | 31.3 ± 18.3 | 27.5 ± 16.3 | 0.021 | ||
| Creatinine, mg/dL | 1.56 ± 1.32 | 1.49 ± 1.17 | 1.65 ± 1.47 | 0.432 | 1.66 ± 1.37 | 1.51 ± 1.29 | 0.062 | ||
| eGFR, mL/min/1.73 m2 | 62.6 ± 34.2 | 61.8 ± 33.2 | 63.5 ± 35.4 | 0.657 | 57.2 ± 34.4 | 65.5 ± 33.9 | 0.004 | ||
| BNP, pg/mL (n = 207) | 843 (476–2,060) | 843 (522–1,793) | 844 (367–3,013) | 0.837 | 852 (540–1,980) | 834 (439–2,263) | 0.205 | ||
| NT-proBNP, pg/mL (n = 269) | 4,430 (2,211–10,533) | 4,394 (2,320–11,437) | 4,448 (2,131–10,480) | 0.979 | 5,467 (2,283–12,890) | 4,249 (2,147–96,587) | 0.205 | ||
| NP above median (n = 459) | 230 (50.1) | 124 (50.4) | 106 (49.8) | 0.965 | 86 (55.1) | 144 (47.5) | 0.149 | ||
| Echocardiography (n = 346) | |||||||||
| LVEF, % | 35.4 ± 16.1 | 36.1 ± 16.5 | 34.4 ± 15.6 | 0.352 | 37.9 ± 16.6 | 33.9 ± 15.7 | 0.024 | ||
| Heart failure type | 0.362 | 0.225 | |||||||
| HF with reduced EF | 233 (67.3) | 122 (64.6) | 111 (70.7) | 77 (61.6) | 156 (70.6) | ||||
| HF with mildly reduced EF | 39 (11.3) | 25 (13.2) | 14 (8.9) | 16 (12.8) | 23 (10.4) | ||||
| HF with preserved EF | 74 (21.4) | 42 (22.2) | 32 (20.4) | 32 (25.6) | 42 (19.0) | ||||
| Medication at admission | |||||||||
| ARNI/ACEi/ARB (n = 382) | 278 (72.8) | 153 (73.2) | 125 (72.3) | 0.835 | 94 (67.6) | 184 (75.7) | 0.087 | ||
| Beta-blocker (n = 382) | 263 (68.9) | 140 (67.0) | 123 (71.1) | 0.388 | 91 (65.5) | 172 (70.8) | 0.281 | ||
| MRA (n = 382) | 208 (54.5) | 120 (57.4) | 88 (50.9) | 0.201 | 73 (52.5) | 135 (55.6) | 0.566 | ||
| Ivabradine (n = 382) | 30 (7.9) | 21 (10.1) | 9 (5.2) | 0.080 | 11 (7.9) | 19 (7.8) | 0.974 | ||
| Loop diuretics (n = 382) | 322 (84.3) | 185 (88.5) | 137 (79.2) | 0.013 | 123 (88.5) | 199 (81.9) | 0.088 | ||
| Warfarin | 52 (11.3) | 26 (10.5) | 26 (12.2) | 0.560 | 18 (11.2) | 34 (11.3) | 0.961 | ||
| NOAC | 159 (34.5) | 91 (36.7) | 68 (31.9) | 0.283 | 56 (34.8) | 103 (34.3) | 0.923 | ||
| Aspirin | 170 (36.9) | 93 (37.5) | 77 (36.2) | 0.765 | 71 (44.1) | 99 (33.0) | 0.019 | ||
| P2Y12 inhibitors | 132 (28.6) | 79 (31.9) | 53 (24.9) | 0.099 | 62 (38.5) | 70 (23.3) | < 0.001 | ||
| Clopidogrel | 123 (26.7) | 76 (30.7) | 47 (22.1) | 0.038 | 60 (37.3) | 63 (21.0) | < 0.001 | ||
| SGLT2 inhibitors | 25 (5.4) | 15 (6.1) | 10 (4.7) | 0.522 | 9 (5.6) | 16 (5.3) | 0.908 | ||
| Anemia and ID treatment | |||||||||
| Transfusion | 21 (4.6) | 10 (4.0) | 11 (5.2) | 0.561 | 8 (5.0) | 13 (4.3) | 0.755 | ||
| Iron supplement | |||||||||
| Oral | 61 (13.2) | 38 (15.3) | 23 (10.8) | 0.153 | 36 (22.4) | 25 (8.3) | < 0.001 | ||
| Intravenous | 1 (0.2) | 1 (0.4) | 0 (0) | > 0.999 | 1 (0.6) | 0 (0) | 0.349 | ||
| In-hospital death | 6 (1.3) | 3 (1.2) | 3 (1.4) | > 0.999 | 3 (1.9) | 3 (1.0) | 0.414 | ||
Values are expressed as number (%), mean ± standard deviation, or median (interquartile range).
ACEi = angiotensin-converting enzyme inhibitor, ARNI = angiotensin receptor-neprilysin inhibitor, ARB = angiotensin II receptor blocker, BNP = B-type natriuretic peptide, BP = blood pressure, BUN = blood urea nitrogen, COPD = chronic obstructive pulmonary disease, EF = ejection fraction, eGFR = estimated glomerular filtration rate, HF = heart failure, ID = iron deficiency, IDA = iron deficiency anemia, LVEF = left ventricular ejection fraction, MRA = mineralocorticoid receptor antagonist, NOAC = non-vitamin K oral anticoagulants, NP = natriuretic peptide, NT-proBNP = N-terminal pro-B-type natriuretic peptide, SGLT2 = sodium glucose cotransporter 2, TIBC = total iron binding capacity, WBC = white blood cell.
ID
Among total patients, 53.8% of patients had ID (Fig. 1). Table 1 shows the baseline characteristics of patients with and without ID. Patients with ID were more likely to be female (46.4% vs. 28.6%, P < 0.001), have diabetes (43.2% vs. 33.3%, P = 0.031), have a valvular heart disease (14.1% vs. 7.0%, P = 0.015), and have a higher heart rate (87.2 ± 22.8 beats/min vs. 83.0 ± 21.3 beats/min, P = 0.046). Regarding laboratory findings, patients with ID had lower hemoglobin levels (11.8 ± 2.3 mg/dL vs. 12.5 ± 2.5 mg/dL, P = 0.001) and ferritin levels (80.5 ± 60.3 mg/dL vs. 392.4 ± 624.5 mg/dL, P < 0.001) than patients without ID. The prescription of clopidogrel was more prevalent in the ID group (30.7% vs. 22.1%, P = 0.038). The prevalence of CKD and malignancy did not differ significantly between patients with and without ID. The prevalence of ID was not significantly different between patients with ischemic HF or non-ischemic HF (59.1% vs. 52.1%, P = 0.243).
Fig. 1. Prevalence of various parameters regarding iron deficiency and anemia. (A) Prevalence of iron deficiency. (B) Prevalence of iron deficiency anemia. (C) Prevalence of iron deficiency and iron deficiency anemia. (D) Treatment pattern of anemia.
ID = iron deficiency, IDA = iron deficiency anemia, IV = intravenous.
Regarding the treatment of anemia and ID, 4.6%, 13.2%, and 0.2% received blood transfusion, oral iron replacement, and IV iron replacement, respectively. The treatment did not differ between patients with and without ID. Among total 461 patients, 6 patients died before discharge. The in-hospital mortality rate did not differ between ID and non-ID patients (3/248 vs. 3/213; P > 0.999).
Logistic regression models to determine the predictor of ID are shown in Table 2. In the multivariable logistic regression analysis, the independent predictors of ID were female sex (odds ratio [OR], 2.19; 95% confidence interval [CI], 1.47–3.30), valvular heart disease (OR, 2.10; 95% CI, 1.10–4.17), heart rate (OR, 1.10; 95% CI, 1.01–1.21), anemia (OR, 1.60; 95% CI, 1.07–2.40), and the use of clopidogrel (OR, 1.56; 95% CI, 1.00–2.45) (Table 2).
Table 2. Predictors of ID and IDA.
| Variables | Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||
| Predictor of ID | |||||||
| Age, per 10 yr | 1.03 | 0.92–1.18 | 0.538 | ||||
| Female | 2.15 | 1.47–3.19 | < 0.001 | 2.19 | 1.47–3.30 | < 0.001 | |
| BMI, kg/m2 | 0.98 | 0.94–1.02 | 0.360 | ||||
| Ischemic heart disease | 1.19 | 0.81–1.75 | 0.380 | ||||
| Diabetes mellitus | 1.51 | 1.03–2.22 | 0.031 | 1.47 | 0.98–2.21 | 0.060 | |
| Chronic kidney disease | 0.86 | 0.59–1.26 | 0.444 | ||||
| Valvular heart disease | 2.17 | 1.17–4.20 | 0.017 | 2.10 | 1.10–4.17 | 0.028 | |
| Malignancy | 1.41 | 0.73–2.82 | 0.313 | ||||
| Smoking | 0.65 | 0.40–1.06 | 0.084 | ||||
| Heart rate, per 10 b.p.m | 1.09 | 1.00–1.19 | 0.049 | 1.10 | 1.01–1.21 | 0.025 | |
| Anemia | 1.83 | 1.26–2.67 | 0.002 | 1.60 | 1.07–2.40 | 0.021 | |
| Above NP | 1.03 | 0.71–1.48 | 0.891 | ||||
| LVEF, per % | 1.01 | 0.99–1.02 | 0.346 | ||||
| Warfarin | 0.84 | 0.47–1.50 | 0.560 | ||||
| NOAC | 1.23 | 0.84–1.82 | 0.283 | ||||
| Aspirin | 1.06 | 0.73–1.55 | 0.765 | ||||
| Clopidogrel | 1.56 | 1.03–2.39 | 0.039 | 1.56 | 1.00–2.45 | 0.049 | |
| Predictor of IDA | |||||||
| Age, per 10 yr | 1.35 | 1.17–1.56 | < 0.001 | 1.24 | 1.06–1.46 | 0.008 | |
| Female | 1.77 | 1.19–2.62 | 0.005 | 1.45 | 0.93–2.26 | 0.103 | |
| BMI, kg/m2 | 0.92 | 0.88–0.97 | 0.002 | ||||
| Ischemic heart disease | 1.39 | 0.93–2.08 | 0.105 | ||||
| Diabetes mellitus | 1.78 | 1.21–2.65 | 0.004 | 1.62 | 1.07–2.47 | 0.024 | |
| Chronic kidney disease | 1.46 | 1.00–2.23 | 0.053 | ||||
| Valvular heart disease | 2.54 | 1.40–4.63 | 0.002 | 3.03 | 1.62–5.76 | < 0.001 | |
| Malignancy | 1.37 | 0.70–2.69 | 0.339 | ||||
| Smoking | 0.37 | 0.20–0.66 | 0.001 | 0.54 | 0.27–0.98 | 0.044 | |
| Heart rate, per 10 b.p.m | 0.95 | 0.87–1.04 | 0.306 | ||||
| Above NP | 1.36 | 0.92–2.00 | 0.123 | ||||
| LVEF, per % | 1.02 | 1.00–1.03 | 0.017 | ||||
| Warfarin | 1.03 | 0.55–1.87 | 0.928 | ||||
| NOAC | 1.08 | 0.72–1.62 | 0.702 | ||||
| Aspirin | 1.51 | 1.02–2.24 | 0.040 | 1.26 | 0.81–1.97 | 0.300 | |
| Clopidogrel | 2.06 | 1.34–3.14 | < 0.001 | 1.96 | 1.22–3.15 | 0.005 | |
Variables found to be statistically significant (P < 0.1) in the univariable analysis were included in the final multivariable model, except for variables with > 10% missing values or variables that were closely related to the other variables.
BMI = body mass index, CI = confidence interval, ID = iron deficiency, IDA = iron deficiency anemia, LVEF = left ventricular ejection fraction, NOAC = non-vitamin K oral anticoagulants, NP = natriuretic peptide; OR = odds ratio.
ID in women
Because female sex was the most important predictor of ID, we performed various post-hoc analyses according to sex, age, body mass index (BMI), NP levels and menopause, among others (Table 3). The prevalence of ID was significantly higher in females than in males (65.3% vs. 47.3%, P < 0.001). Interestingly, when stratifying the patients according to age, both the younger and older subgroups of females had a higher prevalence of ID than their male counterparts. Furthermore, there was no difference in the ID prevalence between the younger and older women. Similar findings were observed in subgroups stratified by different BMI cutoffs; females classified with low and high BMI had a trend toward higher ID prevalence than their male counterparts. Again, there was no difference in the ID prevalence between the women with low and high BMI. Similar findings were observed when stratified based on the median NP levels. Lastly, the prevalence of ID did not differ between those with and without menopause (menopause: 103/157 [65.6%] vs. no menopause: 12/19 [63.2%], P = 0.832).
Table 3. Prevalence of iron deficiency according to subtype.
| Variables | All (N = 461) | Men (n = 285) | Women (n = 176) | P value | ||
|---|---|---|---|---|---|---|
| Overall | 248 (53.8) | 135 (47.3) | 115 (65.3) | < 0.001 | ||
| Age, yr | ||||||
| < 50 (n = 60) | 33 (55.0) | 24 (50.0) | 9 (75.0) | 0.120 | ||
| ≥ 50 (n = 401) | 215 (53.6) | 109 (46.0) | 106 (64.6) | < 0.001 | ||
| P value | 0.951 | 0.612 | 0.547 | |||
| < 65 (n = 168) | 88 (52.4) | 60 (46.2) | 28 (73.7) | 0.003 | ||
| ≥ 65 (n = 293) | 160 (54.6) | 73 (47.1) | 87 (63.0) | 0.006 | ||
| P value | 0.716 | 0.874 | 0.222 | |||
| Body mass index, kg/m2 (n = 291) | ||||||
| < 20 (n = 42) | 22 (52.4) | 14 (51.9) | 8 (53.3) | 0.927 | ||
| ≥ 20 (n = 249) | 144 (57.8) | 71 (49.3) | 73 (69.5) | 0.001 | ||
| P value | 0.623 | 0.808 | 0.244 | |||
| < 23 (n = 118) | 70 (59.3) | 35 (54.7) | 35 (64.8) | 0.265 | ||
| ≥ 23 (n = 173) | 96 (55.5) | 50 (46.7) | 46 (69.7) | 0.003 | ||
| P value | 0.598 | 0.314 | 0.570 | |||
| < 25 (n = 177) | 103 (58.2) | 54 (52.4) | 49 (66.2) | 0.067 | ||
| ≥ 25 (n = 114) | 63 (55.3) | 31 (45.6) | 32 (69.6) | 0.012 | ||
| P value | 0.710 | 0.381 | 0.703 | |||
| Natriuretic peptide (n = 459) | ||||||
| < Median (n = 229) | 122 (53.3) | 62 (43.4) | 60 (69.8) | < 0.001 | ||
| ≥ Median (n = 230) | 124 (53.9) | 69 (49.3) | 55 (61.1) | 0.105 | ||
| P value | 0.965 | 0.378 | 0.295 | |||
Values are expressed as number (%).
IDA
In this study, 34.9% of patients had IDA. They were older, more likely to be female, have diabetes, have valvular heart disease, and use clopidogrel, among others (Table 1). The independent predictors of IDA were older age, diabetes mellitus, valvular heart disease, non-smoking, and the use of clopidogrel (Table 2).
Stratification according to ID and anemia
Next, we classified the patients according to the presence of anemia and ID. Overall, 193 (41.9%) patients had no anemia, while 268 (58.1%) patients had anemia (Table 4). Patients with anemia were older and had a lower BMI than those without anemia. Interestingly, the baseline characteristics were comparable between non-anemic patients with and without ID. The same was true for anemic patients with and without ID. Also, among patients with ID, patients with IDA were more likely to be older and had a lower BMI, higher prevalence of diabetes and CKD, and higher use of aspirin and clopidogrel, and oral iron supplementation than those with non-anemic ID (Supplementary Table 1).
Table 4. Baseline characteristics according to anemia and iron deficiency.
| Characteristics | All patients | No anemia | Anemia | ||||
|---|---|---|---|---|---|---|---|
| No ID/No anemia | ID only | Anemia only | IDA | ||||
| Total | 461 (100) | 106 (23.0) | 87 (18.9) | 107 (23.2) | 161 (34.9) | ||
| Age, yr | 67.6 ± 14.9 | 63.3 ± 16.7 | 61.5 ± 17.3 | 70.9 ± 11.9 | 71.5 ± 12.1 | ||
| Men | 285 (61.8) | 82 (77.4) | 46 (52.9) | 70 (65.4) | 87 (54.0) | ||
| Body mass index, kg/m2 | 24.7 ± 5.0 | 25.8 ± 5.7 | 25.8 ± 5.6 | 23.9 ± 4.7 | 23.5 ± 3.8 | ||
| De novo HF | 169 (36.7) | 43 (40.1) | 45 (51.7) | 26 (24.3) | 55 (34.2) | ||
| Ischemic etiology | 110 (23.8) | 21 (19.8) | 15 (17.2) | 24 (22.4) | 50 (31.1) | ||
| Comorbidities | |||||||
| Hypertension | 245 (53.2) | 52 (49.1) | 47 (54.0) | 58 (54.2) | 88 (54.7) | ||
| Diabetes mellitus | 178 (38.6) | 30 (28.3) | 29 (33.3) | 41 (38.3) | 78 (48.5) | ||
| Chronic kidney disease | 277 (60.1) | 51 (48.1) | 39 (44.8) | 81 (75.7) | 106 (65.8) | ||
| Ischemic heart disease | 159 (34.5) | 25 (23.6) | 26 (29.9) | 44 (41.1) | 64 (39.8) | ||
| Valvular heart disease | 50 (10.9) | 3 (2.8) | 8 (9.2) | 12 (11.2) | 27 (16.8) | ||
| Atrial fibrillation | 173 (37.6) | 47 (44.3) | 31 (35.6) | 36 (33.6) | 59 (36.8) | ||
| COPD | 53 (11.5) | 13 (12.3) | 8 (9.2) | 13 (12.2) | 19 (11.8) | ||
| Cerebrovascular disease | 38 (8.2) | 7 (6.6) | 1 (1.2) | 12 (11.2) | 18 (11.2) | ||
| Malignancy | 39 (8.5) | 5 (4.7) | 8 (9.2) | 10 (9.4) | 16 (9.9) | ||
| Current smoking | 82 (17.8) | 26 (24.5) | 22 (25.3) | 19 (17.8) | 15 (9.3) | ||
| Physical exam (at admission) | |||||||
| Systolic BP, mmHg | 121.2 ± 25.7 | 118.0 ± 22.2 | 122.1 ± 27.4 | 120.1 ± 24.6 | 123.6 ± 27.6 | ||
| Diastolic BP, mmHg | 73.0 ± 17.8 | 73.8 ± 18.9 | 79.9 ± 20.0 | 70.0 ± 16.8 | 70.8 ± 15.4 | ||
| Heart rate, beats/min | 85.3 ± 22.2 | 84.9 ± 22.9 | 93.9 ± 24.5 | 81.2 ± 19.5 | 83.6 ± 21.1 | ||
| Laboratory test results | |||||||
| Iron, µg/dL | 65.0 ± 39.3 | 86.0 ± 37.5 | 63.1 ± 30.8 | 74.5 ± 42.4 | 45.9 ± 33.2 | ||
| TIBC, µg/dL | 290.5 ± 82.7 | 290.9 ± 60.2 | 344.7 ± 104.5 | 229.4 ± 62.6 | 301.5 ± 68.0 | ||
| Transferrin saturation, % | 23.6 ± 14.6 | 29.9 ± 12.2 | 18.9 ± 8.7 | 33.2 ± 18.0 | 15.5 ± 9.6 | ||
| Ferritin, ng/mL | 224.6 ± 453.8 | 295.1 ± 252.6 | 78.6 ± 54.8 | 488.7 ± 835.4 | 81.6 ± 63.2 | ||
| Hemoglobin, mg/dL | 12.1 ± 2.4 | 14.5 ± 1.4 | 14.2 ± 1.4 | 10.5 ± 1.6 | 10.4 ± 1.3 | ||
| Anemia | 268 (58.1) | 0 (0.0) | 0 (0.0) | 107 (100.0) | 161 (100.0) | ||
| WBC, 109/L | 7.47 ± 2.94 | 7.83 ± 2.44 | 7.86 ± 2.87 | 7.63 ± 3.53 | 6.91 ± 2.79 | ||
| Platelet, 109/L | 213.5 ± 82.3 | 210.2 ± 68.5 | 222.1 ± 66.2 | 205.5 ± 99.1 | 216.6 ± 85.7 | ||
| BUN, mg/dL | 28.8 ± 17.1 | 23.1 ± 11.5 | 23.6 ± 10.7 | 34.8 ± 20.8 | 31.3 ± 18.3 | ||
| Creatinine, mg/dL | 1.56 ± 1.32 | 1.16 ± 0.46 | 1.16 ± 0.53 | 2.13 ± 1.91 | 1.66 ± 1.37 | ||
| eGFR, mL/min/1.73 m2 | 62.6 ± 34.2 | 74.6 ± 29.6 | 70.5 ± 29.3 | 52.6 ± 37.4 | 57.2 ± 34.4 | ||
| BNP, pg/mL (n = 207) | 843 (476–2,060) | 392 (219–1,259) | 828 (500–1,346) | 2,015 (753–3,601) | 851 (534–1,978) | ||
| NT-proBNP, pg/mL (n = 269) | 4,430 (2,211–10,533) | 3,056 (1,518–5,872) | 3,483 (2,194–7,750) | 7,561 (3,788–20,498) | 5,467 (2,320–13,162) | ||
| NP above median (n = 459) | 230 (50.1) | 34 (32.1) | 36 (41.9) | 72 (67.3) | 88 (55.0) | ||
| Echocardiography (n = 346) | |||||||
| LVEF, % | 35.4 ± 16.1 | 30.3 ± 13.1 | 32.6 ± 15.9 | 38.1 ± 16.8 | 37.9 ± 16.6 | ||
| Heart failure type | |||||||
| HF with reduced EF | 233 (67.3) | 60 (81.1) | 45 (70.3) | 51 (61.5) | 77 (61.6) | ||
| HF with mildly reduced EF | 39 (11.3) | 6 (8.1) | 9 (14.1) | 8 (9.6) | 16 (12.8) | ||
| HF with preserved EF | 74 (21.4) | 8 (10.8) | 10 (15.6) | 24 (28.9) | 32 (25.6) | ||
| Medication at admission | |||||||
| ARNI/ACEi/ARB (n = 382) | 278 (72.8) | 65 (78.3) | 59 (84.3) | 60 (66.7) | 94 (67.6) | ||
| Beta-blocker (n = 382) | 263 (68.9) | 66 (79.5) | 49 (70.0) | 57 (63.3) | 91 (65.5) | ||
| MRA (n = 382) | 208 (54.5) | 55 (66.3) | 47 (67.1) | 33 (36.7) | 73 (52.5) | ||
| Ivabradine (n = 382) | 30 (7.9) | 3 (3.6) | 10 (14.3) | 6 (6.7) | 11 (7.9) | ||
| Loop diuretics (n = 382) | 322 (84.3) | 74 (89.2) | 62 (88.6) | 63 (70.0) | 123 (88.5) | ||
| Warfarin | 52 (11.3) | 12 (11.3) | 8 (9.2) | 14 (13.1) | 18 (11.2) | ||
| NOAC | 159 (34.5) | 40 (37.7) | 35 (40.2) | 28 (26.2) | 56 (34.8) | ||
| Aspirin | 170 (36.9) | 33 (31.1) | 22 (25.3) | 44 (41.1) | 71 (44.1) | ||
| P2Y12 inhibitors | 132 (28.6) | 24 (22.6) | 17 (19.5) | 29 (27.1) | 62 (38.5) | ||
| Clopidogrel | 123 (26.7) | 21 (19.8) | 16 (18.4) | 26 (24.3) | 60 (37.3) | ||
| SGLT2 inhibitors | 25 (5.4) | 9 (8.5) | 6 (6.9) | 1 (0.9) | 9 (5.6) | ||
| Anemia and ID treatment | |||||||
| Transfusion | 21 (4.6) | 3 (2.8) | 2 (2.3) | 8 (7.5) | 8 (5.0) | ||
| Iron supplement | |||||||
| Oral iron | 61 (13.2) | 6 (5.7) | 2 (2.3) | 17 (15.9) | 36 (22.4) | ||
| Intravenous | 1 (0.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.6) | ||
| In-hospital death | 6 (1.3) | 2 (1.9) | 0 (0.0) | 1 (0.9) | 3 (1.9) | ||
Values are expressed as number (%), mean ± standard deviation, or median (interquartile range).
ACEi = angiotensin-converting enzyme inhibitor, ARNI = angiotensin receptor-neprilysin inhibitor, ARB = angiotensin II receptor blocker, BNP = B-type natriuretic peptide, BP = blood pressure, BUN = blood urea nitrogen, COPD = chronic obstructive pulmonary disease, EF = ejection fraction, eGFR = estimated glomerular filtration rate, HF = heart failure, ID = iron deficiency, IDA = iron deficiency anemia, LVEF = left ventricular ejection fraction, MRA = mineralocorticoid receptor antagonist, NOAC = non-vitamin K oral anticoagulants, NP = natriuretic peptide, NT-proBNP = N-terminal pro-B-type natriuretic peptide, SGLT2 = sodium glucose cotransporter 2, TIBC = total iron binding capacity, WBC = white blood cell.
DISCUSSION
The main findings of the current study were as follows: 1) more than half and one-third of the patients hospitalized for acute HF had ID and IDA, respectively; 2) the most important predictor of ID was female sex; and 3) the treatment with IV iron supplementation was very low in these patients.In this study of patients with acute HF in Korea, 53.8% had ID, similar to previous reports. In patients with chronic HF, the prevalence of ID was 50% in an international pooled cohort from Poland, Spain, and the Netherlands,12 61% in 574 community-dwelling HF patients in the United States,25 and 61% among Southeast Asian HF patients.26 Meanwhile, in patients with acute HF, ID was present in up to 80%.27,28
We showed that female sex, valvular heart disease, high heart rate, anemia, and the use of clopidogrel were independent predictors of ID. The use of clopidogrel is associated with an increased risk of bleeding, anemia, and iron loss.29 Interestingly, the use of aspirin was not the predictor of ID, which has been reported in other study as well.30 A higher heart rate may be more of a marker rather than a mediator of ID. In our study, CKD and malignancy were not a predictor of ID and IDA. Also, median value of NP and prevalence of NP above the median were not significantly different between patients with ID or without. Furthermore, neither LVEF nor HF type was associated with ID. NP level, which reflects the disease severity of HF, was a powerful predictor of ID in previous studies,13 and the same finding was seen for LVEF.26 The reason for the different results between ours and those may be due to ethnic difference or relatively small sample size of our study. Previous studies suggested that inflammation was associated with ID, and there was more inflammatory milieu in women.31,32 Further researches are needed to evaluate the relationship between ID and inflammation.
Our study confirmed that female sex is an important predictor of ID, which is in line with previous studies.12,26 To elucidate the reasons for this, we performed a few subgroup analyses. The main causes of ID include decreased dietary intake, reduced absorption, and blood loss. The possible causes of ID in HF include cachexia/malnutrition, decreased iron resorption in the intestine due to congestion in the splanchnic area, and decreased iron utilization due to inflammation because HF itself is an inflammatory disease.33
It has been a well-accepted concept that menstruation is the leading cause of ID in females; however, when stratifying the patients according to age (i.e., 50 years and 65 years), the prevalence of ID did not differ between younger and older females, as well as between those with and without menopause. The median age of menopause in Korean women is 50 years.34 These results suggest that blood loss from menstruation is a unlikely cause of ID.26
We believe that stratification by BMI may infer the association between nutritional status and ID. Also, not only malnutrition but obesity is known to be associated with ID.35,36,37 Females had a higher prevalence of ID than males, regardless of their BMI. In addition, there was no difference in the prevalence of ID between females with high and low BMI.
Reduced iron absorption can occur in patients with HF who have poor visceral circulation, i.e., congestion. NP is a hormone that is secreted in the ventricles in response to increased myocardial wall stress, which is proportional to the intra-cardiac pressure.38 As such, the NP level can be used as a surrogate for congestion. Interestingly, females had more ID than males, regardless of NP level. In addition, there was no difference in the ID prevalence between females with high and low NP levels.
Taken together, it is unclear why females have more ID than men with HF. Because ID is an important risk factor for outcomes in HF, further research is warranted.
ID occurs in three stages: 1) depletion of iron storage without causing anemia, 2) followed by iron-restricted erythropoiesis, and 3) finally by hypochromic and microcytic anemia. Therefore, one may expect a gradual “aggravation” of the characteristics from normal (no ID/no anemia) to IDA. In this study, the anemic patients had more unfavorable clinical characteristics than the non-anemic patients. More importantly, among the anemic patients, those with and without ID had similar characteristics. The same was observed in the non-anemic patients with and without ID. For example, the mean age of anemic patients with and without ID was 70.9 ± 11.9 years and 71.5 ± 12.1 years, respectively, whereas that of non-anemic patients with and without ID was 63.3 ± 16.7 and 61.5 ± 17.3 years, respectively. These findings have important clinical implications. Because there is no obvious clinical factor that makes the presence of ID highly likely, routine laboratory tests should be performed to detect ID in HF, especially since HF is a disease with increasing prevalence and is associated with high morbidity and mortality.21,39
A striking finding was that only 0.2% of patients received IV iron replacement, and 13.2% received oral iron supplements. Oral iron supplementation did not improve the clinical outcomes,40 whereas IV iron replacement with ferric carboxymaltose improved outcomes in both chronic17,18,20,41 and acute HF.19 Consequently, current practice guidelines recommend IV iron in patients with HF and ID.22,23,24 Although this study enrollment was performed in 2019, the low prescription rate is alarming. Because the prescription rates of renin-angiotensin system modulators and beta-blockers in Korea are comparable to those of the United States and Europe,21,42 both the lack of knowledge and inertia to administer IV iron may be the reasons for the unacceptably low application of adequate ID management.
This study has several limitations. First, since this study was conducted at tertiary university hospitals, the results might not be generalized to other settings (e.g., community or primary settings). Second, our study had a relatively small number of patients, and statistical insignificance of prevalence of ID according to age, BMI, median NP levels, and menopause might be due to small sample size. Third, we could not evaluate the impact of presence of ID in the clinical course of HF except for in-hospital mortality because our study focused on the cross-section of patients’ characteristics. It is expected that further research will be possible in the future by collecting long-term clinical outcomes. Fourth, information on co-morbidities including previous surgery, chemotherapy, liver disease, or thyroid disease was missing, although these co-morbidities are likely to be associated with ID and anemia. Fifth, because not all patients were de-novo HF in our study, some patients might already have an oral or IV iron supplement before the index admission which may have affected the iron profile at the index admission. Despite these limitations, this study had certain strengths, showing prevalence of ID in Asian patients with HF.
In conclusion, the prevalence of ID is high in hospitalized Korean HF patients. Because ID cannot be diagnosed by clinical parameters, routine laboratory examinations are necessary to identify patients with ID.
ACKNOWLEDGMENTS
We thank Dr. Icktae Jin for the statistical analysis of the data.
Footnotes
Funding: This work was sponsored by Seoul National University Bundang Hospital (grant no 06-2018-0300) and JW Pharmaceutical (Seoul, Korea).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Park JJ, Choi DJ.
- Data curation: Park JJ, Yoon M, Cho HW, Lee SE, Choi JO, Yoo BS, Kang SM, Choi DJ.
- Formal analysis: Park JJ, Yoon M, Choi DJ.
- Methodology: Park JJ, Yoon M, Choi DJ.
- Validation: Park JJ, Yoon M, Cho HW, Lee SE, Choi JO, Yoo BS, Kang SM, Choi DJ.
- Writing - original draft: Park JJ, Yoon M, Choi DJ.
- Writing - review & editing: Park JJ, Yoon M, Cho HW, Lee SE, Choi JO, Yoo BS, Kang SM, Choi DJ.
SUPPLEMENTARY MATERIAL
Baseline characteristics between patients with IDA and ID only
References
- 1.Bhattacharya PT, Misra SR, Hussain M. Nutritional aspects of essential trace elements in oral health and disease: an extensive review. Scientifica (Cairo) 2016;2016:5464373. doi: 10.1155/2016/5464373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wessling-Resnick M. Iron homeostasis and the inflammatory response. Annu Rev Nutr. 2010;30(1):105–122. doi: 10.1146/annurev.nutr.012809.104804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang J, Pantopoulos K. Regulation of cellular iron metabolism. Biochem J. 2011;434(3):365–381. doi: 10.1042/BJ20101825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013;34(11):816–829. doi: 10.1093/eurheartj/ehs224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jankowska EA, Rozentryt P, Witkowska A, Nowak J, Hartmann O, Ponikowska B, et al. Iron deficiency predicts impaired exercise capacity in patients with systolic chronic heart failure. J Card Fail. 2011;17(11):899–906. doi: 10.1016/j.cardfail.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Stugiewicz M, Tkaczyszyn M, Kasztura M, Banasiak W, Ponikowski P, Jankowska EA. The influence of iron deficiency on the functioning of skeletal muscles: experimental evidence and clinical implications. Eur J Heart Fail. 2016;18(7):762–773. doi: 10.1002/ejhf.467. [DOI] [PubMed] [Google Scholar]
- 7.Price EA, Mehra R, Holmes TH, Schrier SL. Anemia in older persons: etiology and evaluation. Blood Cells Mol Dis. 2011;46(2):159–165. doi: 10.1016/j.bcmd.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Barton JC, Wiener HH, Acton RT, Adams PC, Eckfeldt JH, Gordeuk VR, et al. Prevalence of iron deficiency in 62,685 women of seven race/ethnicity groups: the HEIRS Study. PLoS One. 2020;15(4):e0232125. doi: 10.1371/journal.pone.0232125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hughes CM, Woodside JV, McGartland C, Roberts MJ, Nicholls DP, McKeown PP. Nutritional intake and oxidative stress in chronic heart failure. Nutr Metab Cardiovasc Dis. 2012;22(4):376–382. doi: 10.1016/j.numecd.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Naito Y, Tsujino T, Fujimori Y, Sawada H, Akahori H, Hirotani S, et al. Impaired expression of duodenal iron transporters in Dahl salt-sensitive heart failure rats. J Hypertens. 2011;29(4):741–748. doi: 10.1097/HJH.0b013e3283434784. [DOI] [PubMed] [Google Scholar]
- 11.Satoh M, Minami Y, Takahashi Y, Nakamura M. Immune modulation: role of the inflammatory cytokine cascade in the failing human heart. Curr Heart Fail Rep. 2008;5(2):69–74. doi: 10.1007/s11897-008-0012-2. [DOI] [PubMed] [Google Scholar]
- 12.Klip IT, Comin-Colet J, Voors AA, Ponikowski P, Enjuanes C, Banasiak W, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(4):575–582.e3. doi: 10.1016/j.ahj.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 13.Jankowska EA, Rozentryt P, Witkowska A, Nowak J, Hartmann O, Ponikowska B, et al. Iron deficiency: an ominous sign in patients with systolic chronic heart failure. Eur Heart J. 2010;31(15):1872–1880. doi: 10.1093/eurheartj/ehq158. [DOI] [PubMed] [Google Scholar]
- 14.Anand I. Iron deficiency in heart failure. Cardiology. 2014;128(4):317–319. doi: 10.1159/000361040. [DOI] [PubMed] [Google Scholar]
- 15.Varma A, Appleton DL, Nusca A, Lipinski MJ, Goudreau E, Cowley MJ, et al. Iron deficiency anemia and cardiac mortality in patients with left ventricular systolic dysfunction undergoing coronary stenting. Minerva Cardioangiol. 2010;58(1):1–10. [PubMed] [Google Scholar]
- 16.Magrì D, De Martino F, Moscucci F, Agostoni P, Sciomer S. Anemia and iron deficiency in heart failure: clinical and prognostic role. Heart Fail Clin. 2019;15(3):359–369. doi: 10.1016/j.hfc.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Anker SD, Kirwan BA, van Veldhuisen DJ, Filippatos G, Comin-Colet J, Ruschitzka F, et al. Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: an individual patient data meta-analysis. Eur J Heart Fail. 2018;20(1):125–133. doi: 10.1002/ejhf.823. [DOI] [PubMed] [Google Scholar]
- 18.Anker SD, Comin Colet J, Filippatos G, Willenheimer R, Dickstein K, Drexler H, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361(25):2436–2448. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 19.Ponikowski P, Kirwan BA, Anker SD, McDonagh T, Dorobantu M, Drozdz J, et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet. 2020;396(10266):1895–1904. doi: 10.1016/S0140-6736(20)32339-4. [DOI] [PubMed] [Google Scholar]
- 20.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. Eur Heart J. 2015;36(11):657–668. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JJ, Lee CJ, Park SJ, Choi JO, Choi S, Park SM, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021;3(4):224–236. doi: 10.36628/ijhf.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim KJ, Cho HJ, Kim MS, Kang J, Kim KH, Kim D, et al. Focused update of 2016 Korean Society of Heart Failure guidelines for the management of chronic heart failure. Int J Heart Fail. 2019;1(1):4–24. doi: 10.36628/ijhf.2019.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 24.Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17):e263–e421. doi: 10.1016/j.jacc.2021.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Parikh A, Natarajan S, Lipsitz SR, Katz SD. Iron deficiency in community-dwelling US adults with self-reported heart failure in the National Health and Nutrition Examination Survey III: prevalence and associations with anemia and inflammation. Circ Heart Fail. 2011;4(5):599–606. doi: 10.1161/CIRCHEARTFAILURE.111.960906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeo TJ, Yeo PS, Ching-Chiew Wong R, Ong HY, Leong KT, Jaufeerally F, et al. Iron deficiency in a multi-ethnic Asian population with and without heart failure: prevalence, clinical correlates, functional significance and prognosis. Eur J Heart Fail. 2014;16(10):1125–1132. doi: 10.1002/ejhf.161. [DOI] [PubMed] [Google Scholar]
- 27.Beale A, Carballo D, Stirnemann J, Garin N, Agoritsas T, Serratrice J, et al. Iron deficiency in acute decompensated heart failure. J Clin Med. 2019;8(10):1569. doi: 10.3390/jcm8101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rocha BM, Cunha GJ, Menezes Falcão LF. The burden of iron deficiency in heart failure: therapeutic approach. J Am Coll Cardiol. 2018;71(7):782–793. doi: 10.1016/j.jacc.2017.12.027. [DOI] [PubMed] [Google Scholar]
- 29.Tsai TT, Ho PM, Xu S, Powers JD, Carroll NM, Shetterly SM, et al. Increased risk of bleeding in patients on clopidogrel therapy after drug-eluting stents implantation: insights from the HMO Research Network-Stent Registry (HMORN-stent) Circ Cardiovasc Interv. 2010;3(3):230–235. doi: 10.1161/CIRCINTERVENTIONS.109.919001. [DOI] [PubMed] [Google Scholar]
- 30.van der Wal HH, Grote Beverborg N, Dickstein K, Anker SD, Lang CC, Ng LL, et al. Iron deficiency in worsening heart failure is associated with reduced estimated protein intake, fluid retention, inflammation, and antiplatelet use. Eur Heart J. 2019;40(44):3616–3625. doi: 10.1093/eurheartj/ehz680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Haehling S, Ebner N, Evertz R, Ponikowski P, Anker SD. Iron deficiency in heart failure: an overview. JACC Heart Fail. 2019;7(1):36–46. doi: 10.1016/j.jchf.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 32.van Veldhuisen DJ, Anker SD, Ponikowski P, Macdougall IC. Anemia and iron deficiency in heart failure: mechanisms and therapeutic approaches. Nat Rev Cardiol. 2011;8(9):485–493. doi: 10.1038/nrcardio.2011.77. [DOI] [PubMed] [Google Scholar]
- 33.Anand IS, Gupta P. Anemia and iron deficiency in heart failure: current concepts and emerging therapies. Circulation. 2018;138(1):80–98. doi: 10.1161/CIRCULATIONAHA.118.030099. [DOI] [PubMed] [Google Scholar]
- 34.Park YJ, Kim HS, Kang HC. The age at menopause and related factors in Korean women. J Korean Acad Nurs. 2002;32(7):1024–1031. [Google Scholar]
- 35.Aigner E, Feldman A, Datz C. Obesity as an emerging risk factor for iron deficiency. Nutrients. 2014;6(9):3587–3600. doi: 10.3390/nu6093587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao L, Zhang X, Shen Y, Fang X, Wang Y, Wang F. Obesity and iron deficiency: a quantitative meta-analysis. Obes Rev. 2015;16(12):1081–1093. doi: 10.1111/obr.12323. [DOI] [PubMed] [Google Scholar]
- 37.McClung JP, Karl JP. Iron deficiency and obesity: the contribution of inflammation and diminished iron absorption. Nutr Rev. 2009;67(2):100–104. doi: 10.1111/j.1753-4887.2008.00145.x. [DOI] [PubMed] [Google Scholar]
- 38.Kang SH, Park JJ, Choi DJ, Yoon CH, Oh IY, Kang SM, et al. KorHF Registry. Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF. Heart. 2015;101(23):1881–1888. doi: 10.1136/heartjnl-2015-307782. [DOI] [PubMed] [Google Scholar]
- 39.Kim MS. The long journey to obtaining the epidemiological data of heart failure in Korea. Int J Heart Fail. 2021;3(4):221–223. doi: 10.36628/ijhf.2021.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lewis GD, Malhotra R, Hernandez AF, McNulty SE, Smith A, Felker GM, et al. Effect of oral iron repletion on exercise capacity in patients with heart failure with reduced ejection fraction and iron deficiency: the IRONOUT HF randomized clinical trial. JAMA. 2017;317(19):1958–1966. doi: 10.1001/jama.2017.5427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lim EA, Sohn HS, Lee H, Choi SE. Cost-utility of ferric carboxymaltose (Ferinject®) for iron-deficiency anemia patients with chronic heart failure in South Korea. Cost Eff Resour Alloc. 2014;12(1):19. doi: 10.1186/1478-7547-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF) Korean Circ J. 2017;47(3):341–353. doi: 10.4070/kcj.2016.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Baseline characteristics between patients with IDA and ID only