Abstract
The aim of this study was to identify how previously existing burnout and its changes during the pandemic contributed to PTSD symptoms and psychological distress in a cohort of 388 healthcare workers (HCWs). Each HCW was surveyed in Sep 2019 (before COVID-19) and again in Dec 2020-Jan 2021 (during the pandemic) to assess burnout (MBI); and in the second wave only to assess PTSD (PCL-5-SF), psychological distress (GHQ-12) and resilience (CD-RISC-10). Changes in emotional exhaustion (EE) and depersonalisation (DEP) were stronger in HCWs with lower EE and DEP baseline values. HCWs with higher baseline poor personal accomplishment (PPA) improved more than those with lower baseline values. In multivariable-adjusted models, pre-pandemic EE and its changes were equally associated to both outcomes: standardised-βs of 0.52 and 0.54 for PTSD, respectively; and 0.55 and 0.53 for psychological distress. Changes in DEP were associated with PTSD only (0.10). Changes in PPA had a higher association with psychological distress (0.29) than pre-pandemic PPA (0.13). Resilience was associated with lower psychological distress (-0.25). Preventive actions aimed at reducing EE, e.g., addressing organisational dysfunctions, are needed to mitigate the impact of future crises, whereas improving personal accomplishment levels is a key target to protect HCWs from mental health disorders during a pandemic.
Keywords: PTSD, Burnout, Healthcare workers, Psychological distress, COVID-19
1. Introduction
Among the multiple issues forming the heavy burden placed by the COVID-19 pandemic on the shoulders of healthcare workers (HCWs), direct and indirect exposure to highly aversive events was one of the heaviest (Andhavarapu et al., 2022). HCWs had to face an unknown disease with initially high in-hospital mortality rates in the absence of both effective treatments and personal protective equipment. The context featured work stress resulting from sudden organisational changes and long shifts, also involving contact with patients who were themselves experiencing an adverse situation, an aspect that can lead to secondary traumatisation (Frenkel et al., 2022). Not surprisingly, the prevalence of post-traumatic stress disorder (PTSD), a psychological condition affecting individuals exposed to traumatic events, whose symptoms include intrusive re-experiencing, avoidance, alterations of cognition and mood, and excessive arousal, was estimated at about 34% of the HCWs (Andhavarapu et al., 2022). This prevalence, which is higher than that of the general population (Schou-Bredal et al., 2022), did not resolve itself after the early stages of the pandemic, but rather increased over time (Ouyang et al., 2022). Alongside this condition, psychological distress emerged as the main mental health problem faced by HCWs during the pandemic (Sun et al., 2021). Psychological distress had a very high prevalence, with 33% to 36% of HCWs showing depression symptoms, and 37% to 42% showing anxiety symptoms (Aymerich et al., 2022; Sun et al., 2021). Remarkably, this prevalence persisted unaltered even after the pandemic curve flattened (Spiller et al., 2022). Due to their prevalence and disabling potential, it is essential to understand both protective and risk factors of PTSD and psychological distress in order to develop targeted psychological treatments and prevent their occurrence in future emergencies.
There is a multitude of studies on factors associated with PTSD both in past epidemics, during COVID-19, and in the absence of an epidemic, but almost all are characterised by a cross-sectional design and cannot, therefore, provide strong evidence for the association of each predictor with PTSD (Al Falasi et al., 2021; Hill et al., 2022; Hilton et al., 2022; Preti et al., 2020; Yuan et al., 2021). In addition, their results are often conflicting, with only the level of exposure to the epidemic being consistently associated with PTSD (Al Falasi et al., 2021; Hill et al., 2022; Preti et al., 2020).
Since exposure to trauma in HCWs during the pandemic occurred in the workplace, work-related factors must be taken into account among the possible predictors of PTSD. It can be hypothesised that pre-pandemic work-related stress and burnout might have created conditions favouring its onset in a highly stressful situation, such as the pandemic. Burnout is a syndrome resulting from chronic work-related stress characterised by feelings of energy depletion or emotional exhaustion, increased mental distance from one's job, and poor personal accomplishment (World Health Organization, 2019). Previously existing burnout and job stress have been linked to PTSD symptoms in firefighters, police officers and child welfare workers (Jo et al., 2018; Ogińska-Bulik and Juczyński, 2021; Regehr et al., 2004). This association is explained by the imbalance between constant demand for work and perceived personal resources. Moreover, the depletion of energy associated with burnout might reduce the resources required to deal with adverse situations and to provide care to traumatised patients (Shoji et al., 2015), thus increasing the likelihood of PTSD (Ogińska-Bulik and Juczyński, 2021).
In addition, burnout might be a contributing factor to the high levels of psychological distress observed in HCWs. However, its predictive role during the pandemic has not been studied as yet in longitudinal studies. Burnout and depression exhibit a correlation of medium-to-large magnitude (i.e., between 0.49 and 0.52; Koutsimani et al., 2019; Meier et al., 2022), which has sparked a debate between those asserting that burnout is a distinct form of depression (Bianchi et al., 2015) and others advocating that burnout and depression represent theoretically distinct diagnostic entities (Parker and Tavella, 2021). In their systematic review with meta-analysis, Meier et al. (Meier et al., 2022) showed that the correlation between burnout and depression is dynamic and depends, among other factors, on age and years of service, suggesting that years of exposure to stressful working conditions may lead burnout to develop with symptoms overlapping those of depression. In a longitudinal study on 542 early career workers, the analysis of cross-sectional and cross-lagged relationships showed that burnout and depression are separate constructs influencing each other over time (Tóth-Király et al., 2021), thus supporting both the role of burnout as an antecedent and as a consequence of depression. The mechanism by which burnout precedes depression is that distress resulting from the contrast between work-related stress and the depletion of personal resources associated with burnout spills over to other areas of life, generating depression (Hakanen and Schaufeli, 2012). It can be hypothesised that this mechanism may have been in play during the pandemic as, from the onset, the medical emergency created a strong and unexpected work stressor for HCWs, which might have extended to the family and to the other areas of life. However, this hypothesis has not been studied as yet in HCWs during the pandemic.
Conversely, resilience, i.e., the process of effectively negotiating, adapting to, or managing significant sources of stress or trauma, might have exerted a protective effect against PTSD and psychological distress. Resilience is generally regarded as a major protective factor for both outcomes, and its effect can be particularly significant in helping HCWs deal with adverse situations caused by the pandemic (Li et al., 2022; Snijders et al., 2018). However, both the detrimental role of burnout and the protective effect of resilience have as yet to be tested by studies on HCWs and using longitudinal designs.
Hence, the main objective of this study was to assess the effects of burnout experienced both before and during the COVID-19 pandemic on PTSD symptoms and psychological distress during the pandemic on HCWs.
2. Methods
2.1. Study population and design
The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic in Health Care Workers is a two-wave study conducted on a representative sample of HCWs in a University hospital in the town of Varese, Lombardy. Briefly, a representative sample of 1286 doctors, nurses, nurse assistants and clerks were invited to respond to an online survey on work-related stress between August and September 2019 (pre-pandemic wave). The n = 805 respondents to the first wave were then invited to attend a second survey conducted between December 2020 and January 2021 (during the second peak of the COVID-19 pandemic and before the start of vaccinations) to assess the impact of COVID-19 on their mental health. The rate of participation in the second survey was 53.5% (431/805). More detailed information about the study population, the representativeness of the sample, and the study procedures have already been published (Veronesi et al., 2022). In this study, we excluded data from clerks and analysed the data of doctors, nurses and nurse assistants who responded to both surveys (n = 388). All participants provided their informed consent. The study was approved by the Institutional Ethics Committee (approval ID 69/2020).
2.2. Measurement instruments
The Maslach Burnout Inventory (MBI; Maslach and Jackson, 1981) is a self-report measure of burnout. It includes 22 items assessing the frequency of feelings or attitudes reflecting the three theoretical components of burnout, namely emotional exhaustion (EE), depersonalisation (DEP) and poor personal accomplishment (PPA). The items are scored using a 0 (“never”) to 6 (“every day”) Likert scale. Higher scores reflect higher burnout levels. The MBI has shown adequate construct validity (Shoman et al., 2021). In this study, we employed the refined version of the MBI described by Giusti et al., which showed adequate internal consistency, structural validity and longitudinal invariance (Giusti et al., 2022). The MBI was administered during both surveys.
The Connor-Davidson Resilience scale – 10 (CD-RISC-10; Connor and Davidson, 2003) is a self-report measure of resilience as defined by Connor and Davidson, i.e., the ability to thrive in the face of adversity (Connor and Davidson, 2003). It includes 10 items scored on a Likert scale ranging from 0 (“not true at all”) to 4 (“true nearly all the time”), whose content reflects agreement with statements about how the respondent deals with stress and pressure. Higher scores reflect higher levels of resilience. The Italian version of the CD-RISC-10 showed adequate internal consistency and structural and concurrent validity (Di Fabio and Palazzeschi, 2012). The CD-RISC was administered during the second survey.
The General Health Questionnaire - 12 (GHQ-12; Goldberg and Hillier, 1979) is a self-report general measure of psychological distress. It includes 12 items on a 0 (“less than usual”) to 4 (“much more than usual”) Likert scale, whose content reflects the severity of mental problems over the previous two weeks. Higher scores indicate higher psychological distress. The Italian version of the GHQ-12 has shown acceptable test-retest reliability and structural validity (Piccinelli et al., 1993). The GHQ-12 was administered during the second survey.
The PTSD Checklist for DSM-5 - Short Form (PCL-5-SF; Blevins et al., 2015) is a self-report measure of the frequency of PTSD symptoms as defined by the DSM-5 (American Psychiatric Association, 2013). It includes 5 items scored on a Likert scale ranging from 1 (“not at all”) to 5 (“extremely”). Higher scores reflect worse PTSD symptomatology. The PCL-5-SF has been translated into Italian, and has shown adequate internal consistency as well as structural, construct and criterion validity (Di Tella et al., 2022). The PCL-5-SF was administered during the second survey.
2.3. Statistical analyses
Categorical variables were described using counts and percentages; numerical variables were summarised using means and standard deviations. Differences in PTSD and psychological distress in groups created based on sociodemographic and work-related variables were ascertained by performing ANOVA tests followed by Tukey's post-hoc tests.
Frequencies and patterns of missing data were explored using frequencies, graphical methods and Little's MCAR test to ascertain that missing data followed a Missing Completely At Random (MCAR) mechanism (Little, 1988). Since Little's MCAR test was not significant (χ2 = 285, p=.77) and visual inspection of the missing data patterns revealed that there were no distinct patterns, a multiple imputation procedure was performed using predictive mean matching for numeric variables and logistic regression imputation for categorical variables to account for missing data. Fifty multiple imputed datasets were created using 50 iterations, and were employed to perform the subsequent analyses.
Differences between the levels of burnout measured before and during COVID-19 were assessed using paired t-tests. Age and sex-adjusted associations between PTSD, psychological distress, resilience and the components of burnout both before and during COVID-19 were assessed using partial correlations, the strength of the association classified according to the established cut-off values for the correlation coefficient (Cohen, 1992). Least Square means based on linear models assessing the effect on changes in the MBI subscales of the interaction between job title and having pre-COVID-19 MBI levels either below or above the respective median were calculated. Contrasts were run to assess the differences between job titles, and between the groups defined by pre-COVID-19 MBI levels. Similarly, Least Square means based on linear models assessing the effect on PTSD and psychological distress of the interaction between having pre-COVID-19 MBI levels either below or above the respective median before COVID-19 and during COVID-19 were calculated and displayed using graphical methods.
Multiple linear regression analyses were performed to explore the variables associated with PTSD symptoms and psychological distress. The variables included were MBI levels before COVID-19, their changes between the study waves (ΔEE, ΔDEP and ΔPPA), resilience (dichotomised based on the median value, i.e., 26), and the socio-demographic and work-related confounders or effect modifiers associated with the outcomes in bivariate analyses. In both analyses, the assumptions of linearity, normality and homoscedasticity of the residuals were assessed using graphical methods.
The significance threshold was set at 0.05. The results of the regressions were reported using standardised coefficients with 95% confidence intervals. The analyses were performed using R (version 4.2.1).
3. Results
3.1. Demographic and work-related characteristics of the sample and links between study variables
Demographic and work-related characteristics of the sample are reported in Table 1 . ANOVA analyses with post-hoc tests revealed that there were significant differences in PTSD and psychological distress levels by age groups (younger HCWs showed higher levels of both variables), educational attainment (graduated HCWs showed higher PTSD and psychological distress levels than HCWs with lower education), job title (nurses showed higher levels of PTSD and psychological distress than nurse assistants), and work seniority (HCWs with work seniority <5 years showed higher PTSD and psychological distress than HCWs with work seniority >16 years). In addition, there were significant differences in PTSD considering work scheduling (with night-shift HCWs presenting a higher incidence of PTSD than day-shift HCWs). Finally, HCWs working in a COVID-19 ward and HCWs who were infected by COVID-19 showed higher levels of psychological distress.
Table 1.
Distribution of sample demographics and work-related characteristics, and their associations with the study outcomes PTSD and psychological distress.
| Variable | PTSD | Psychological distress | ||||
|---|---|---|---|---|---|---|
| n (%) | Mean | pa | Mean | pa | ||
| Sex | Female | 309 (79.6) | 10.9 | 0.18 | 16.9 | 0.24 |
| Male | 79 (20.4) | 10.2 | 15.9 | |||
| Age groups | From 25 to 34 | 62 (16.0) | 12.4 | <0.01 | 18.4 | .01 |
| From 35 to 44 | 84 (21.7) | 11.4 | 17.6 | |||
| From 45 to 54 | 176 (45.4) | 10.5 | 16.6 | |||
| Over 55 | 66 (17.0) | 9.5 | 14.4 | |||
| Educational attainment | Primary school | 44 (11.3) | 8.9 | <0.01 | 15 | .01 |
| Secondary school | 151(38.9) | 10.4 | 16 | |||
| University degree | 137 (35.3) | 11.9 | 18.4 | |||
| Postgraduate programmes or specialisation | 56 (14.4) | 10.4 | 16.0 | |||
| Job title | Doctor | 42 (10.8) | 10.2 | <0.01 | 15.5 | <0.01 |
| Nurse | 261 (67.3) | 11.4 | 17.6 | |||
| Nurse assistant | 85 (21.9) | 9.2 | 14.7 | |||
| Work seniority | Less than 5 years | 108 (27.8) | 11.6 | .02 | 17.9 | .04 |
| From 6 to 15 years | 102 (26.3) | 11.0 | 17.1 | |||
| More than 16 years | 178 (45.9) | 10.2 | 15.8 | |||
| Type of contract | Fixed-term | 4 (1.0) | 10.5 | 0.89 | 14.5 | 0.52 |
| Permanent | 384 (99.0) | 10.8 | 16.8 | |||
| Type of employment | Full-time | 333 (85.8) | 10.8 | 0.90 | 16.8 | 0.74 |
| Part-time | 55 (14.2) | 10.8 | 16.4 | |||
| Work scheduling | Non-shift work | 35 (9.0) | 10.4 | 0.03 | 15.8 | 0.30 |
| Shift work (with nights) | 278 (71.6) | 11.1 | 17.1 | |||
| Shift work (without nights) | 75 (19.3) | 9.9 | 15.9 | |||
| Worked in a COVID-19 ward | No | 169 (43.6) | 10.4 | 0.09 | 15.9 | 0.03 |
| Yes | 219 (56.4) | 11.1 | 17.4 | |||
| Having been infected by COVID-19 | No | 278 (71.6) | 10.7 | 0.74 | 16.3 | 0.04 |
| Yes | 107 (27.6) | 10.9 | 17.9 | |||
Note. a based on ANOVA F tests.
The means and standard deviation of the study variables, and the age and sex-adjusted partial correlations between them are reported in Table 2 . EE and DEP components of burnout increased (p<.001) between the study waves, whereas the poor personal accomplishment component decreased (p<.001). PTSD and psychological distress presented large correlations with EE during COVID-19, medium correlation with resilience, EE before COVID-19, DEP during COVID-19 and PPA during COVID-19, and low correlation with DEP before COVID-19. Pre-COVID-19 EE had a moderate correlation with EE during COVID-19, and low correlations with DEP and PPA during COVID-19. DEP before COVID-19 had a moderate correlation with DEP during COVID-19 and low correlations with DEP and PPA during COVID-19. Finally, PPA before COVID-19 was not correlated with EE during COVID-19 and had low correlations with DEP and PPA during COVID-19.
Table 2.
Descriptive statistics and age and sex-adjusted partial correlations between PTSD, psychological distress, resilience and the components of burnout before and during COVID-19.
| Period | Variable | Mean (sd) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before COVID-19 | MBI - EE | 20.1 (9.3) | 1 | – | |||||||
| MBI - DEP | 10.4 (5.4) | 2 | 0.53* | – | |||||||
| MBI - PPA | 20.1 (8.6) | 3 | 0.15* | 0.18* | – | ||||||
| During COVID-19 | MBI - EE | 26.4 (9.9) | 4 | 0.46* | 0.26* | 0.07 | – | ||||
| MBI - DEP | 11.8 (6.5) | 5 | 0.29* | 0.48* | 0.13* | 0.52* | – | ||||
| MBI - PPA | 16.5 (7.2) | 6 | 0.17* | 0.28* | 0.27* | 0.27* | 0.44* | – | |||
| Resilience | 25.4 (6.3) | 7 | -0.30* | -0.19* | -0.28* | -0.37* | -0.28* | -0.50* | – | ||
| PTSD | 10.8 (4.1) | 8 | 0.30* | 0.20* | 0.03 | 0.65* | 0.46* | 0.33* | -0.38* | – | |
| Psychological distress | 16.7 (6.9) | 9 | 0.36* | 0.23* | 0.01 | 0.69* | 0.47* | 0.41* | -0.46* | 0.65* |
Note. MBI = Maslach Burnout Inventory; EE = emotional exhaustion; DEP = depersonalisation; PPA = poor personal accomplishment.
p<.05.
3.2. Changes in burnout between the study waves and association with PTSD and psychological distress
Table 3 shows the age and sex-adjusted changes in MBI subscales between the two waves stratified by job title and by having pre-COVID-19 MBI levels either below or above the respective median. HCWs who had lower EE and DEP before the pandemic showed a worsening in their EE and DEP levels. These changes were stronger than those of HCWs presenting higher EE and DEP levels before the pandemic. In contrast, only HCWs with pre-COVID-19 PPA above the median showed a reduction in this factor, stronger in nurse assistants compared to doctors. There were no other differences across job titles.
Table 3.
Age and sex-adjusted changes in MBI subscales between the two waves of the study.
| Whole sample | Job title | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Doctor | Nurse | Nurse assistant | pa | ||||||
| Mean change | 95% CI | Mean change | 95% CI | Mean change | 95% CI | Mean change | 95% CI | ||
| MBI-EE before COVID-19 | |||||||||
| < median | 9.86 | [8.82, 11.53]* | 8.21 | [4.02, 12.4]* | 10.24 | [8.31, 12.17]* | 9.34 | [6.44, 12.24]* | 0.61 |
| ≥ median | 1.97 | [−0.32, 3.62] | 0.27 | [−3.96, 4.50] | 2.18 | [0.30, 4.06]* | 1.94 | [−1.20, 5.07] | 0.69 |
| pb | <0.01 | <0.01 | <0.01 | <0.01 | |||||
| MBI-DEP before COVID-19 | |||||||||
| < median | 2.60 | [1.56, 3.64]* | 3.70 | [0.97, 6.43]* | 3.04 | [1.78, 4.3]* | 1.40 | [−0.25, 3.05] | 0.17 |
| ≥ median | −0.49 | [−1.59, 0.62] | −1.14 | [−3.80, 1.52] | −0.31 | [−1.52, 0.89] | −0.86 | [−3.36, 1.63] | 0.80 |
| pb | <0.01 | <0.01 | <0.01 | <0.01 | |||||
| MBI-PPA before COVID-19 | |||||||||
| < median | 0.48 | [−1.04, 2.00] | 0.31 | [−3.15, 3.76] | 0.55 | [−1.25, 2.36] | 0.34 | [−2.25, 2.93] | 0.98 |
| ≥ median | −9.39 | [−10.86, −7.91]* | −7.52 | [−11.71, −3.33]* | −8.64 | [−10.25, −7.02]* | −12.9 | [−15.66, −10.13]* | 0.02 |
| pb | <0.01 | <0.01 | <0.01 | <0.01 | |||||
Note. Cells contain age and sex-adjusted means of changes in each MBI subscale. Abbreviations: MBI = Maslach Burnout Inventory; EE = emotional exhaustion; DEP = depersonalisation; PPA = poor personal accomplishment.
Significant change in the subscale over time.
p value of contrasts assessing differences between groups based on job title.
p value of contrasts assessing differences between groups based on having MBI levels below or above the median before COVID-19.
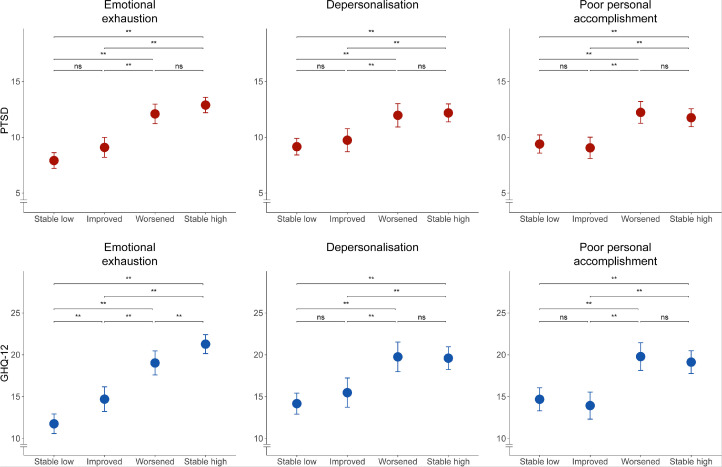
Fig. 1 presents the differences in PTSD and psychological distress levels between groups formed based on MBI levels before and during COVID-19 in relation to their respective median. Regarding PTSD, there were no statistical differences between HCWs with MBI levels below their respective medians during both study waves and HCWs with improved MBI levels, and between HCWs who were above the medians of the MBI subscales during both study waves and HCWs, whose MBI levels had worsened. All other pairwise comparisons were significant. Regarding psychological distress, there were significant changes among all the groups based on EE levels before and during COVID-19. Similarly, there were no differences in psychological distress between HCWs, whose DEP and PPA levels were below the median during both waves, and those whose DEP and PPA levels had improved; and between the groups, whose DEP and PPA levels were above the median during both waves, and those whose DEP and PPA levels had worsened.
Fig. 1.
Sex and age-adjusted means of PTSD symptoms and psychological distress of groups created based on MBI levels before and during COVID-19 in relation to their respective median.
Note. For each burnout component, groups were created based on the levels of that component both before and during COVID-19: “stable low” if both were below the respective medians, “stable high” if both were higher than the respective medians, “improved” if the subcomponent level was above the respective median before COVID-19 and below during COVID-19, “worsened” if the subcomponent level was below the respective median before COVID-19 and above during COVID-19.
3.3. Analysis of the predictors of PTSD symptoms and psychological distress
The results of the regressions performed to assess the predictors of PTSD symptoms and psychological distress are reported in Table 4 . Based on the results of the bivariate analyses, age, educational attainment, job profile, work seniority and work scheduling were included as confounders or effect modifiers in the model predicting PTSD; whereas age, educational attainment, job profile, work seniority, having worked in a COVID-19 ward and having been infected by COVID-19 were included in the model predicting psychological distress. After accounting for these confounders or effect modifiers, PTSD was predicted by EE measured before COVID-19 and by worsening of the burnout components over time. The adjusted R2 of this model was 0.49. Psychological distress was predicted by EE and PPA measured before COVID-19, with the changes in these variables over time, and with resilience. It must be said that the standardised coefficient for change in PPA was larger than for its baseline value, suggesting that worsening PPA has a larger effect on psychological distress rather than the absolute value. The adjusted R2 of this model was 0.57.
Table 4.
Results of regression models employed to assess the predictive effect of burnout before and during COVID-19 and resilience on PTSD symptoms and psychological distress.
| Variable | PTSD | Psychological distress | ||
|---|---|---|---|---|
| βa | [95% CI] | βb | [95% CI] | |
| MBI - EE before COVID-19 | 0.52 | [0.42, 0.63]* | 0.55 | [0.46, 0.65]* |
| MBI - DEP before COVID-19 | 0.04 | [−0.06, 0.15] | 0.03 | [−0.06, 0.12] |
| MBI - PPA before COVID-19 | 0.09 | [−0.03, 0.21] | 0.13 | [0.02, 0.24]* |
| MBI - ΔEE | 0.54 | [0.45, 0.64]* | 0.53 | [0.44, 0.62]* |
| MBI - ΔDEP | 0.10 | [0.01, 0.19]* | 0.07 | [−0.01, 0.16] |
| MBI - ΔPPA | 0.17 | [0.05, 0.29]* | 0.29 | [0.19, 0.40]* |
| CD-RISC-10 - Resilience | −0.10 | [−0.27, 0.07] | −0.25 | [−0.41, −0.09]* |
Note. MBI = Maslach Burnout Inventory; EE = emotional exhaustion; DEP = depersonalisation; PPA = poor personal accomplishment; ΔEE = change in EE over time; ΔDEP = change in DEP over time; ΔPPA = change in PPA over time.
Coefficients are standardised and adjusted for age, educational attainment, job profile, work seniority and work scheduling.
Coefficients are standardised and adjusted for age, educational attainment, job profile, work seniority, having worked in a COVID-19 ward and having been infected by COVID-19.
p<.05.
4. Discussion
The main results of this study are that PTSD symptoms during COVID-19 were predicted by EE existing before COVID-19 and by increases in EE, DEP and PPA over time, whereas psychological distress was positively associated with previously existing EE and PPA, with increases in EE and PPA over time, and inversely with resilience during COVID-19.
An interesting aspect that, to our knowledge, has not been reported before is that both previously existing levels of EE and the worsening of all burnout components were associated with the occurrence of PTSD. The relationship between burnout and PTSD is complex since they are distinct phenomena, which are caused by external stressors, have some clinical manifestations in common (Jackson et al., 2019; Restauri and Sheridan, 2020; Schuster, 2021), and can co-occur (Einav et al., 2008). Studies on the relationship between the two are few but show that, across different populations, burnout seems to create the conditions for PTSD, and not the reverse (Jo et al., 2018; Regehr et al., 2004; Shoji et al., 2015). This study adds that this relationship exists among HCWs and, more importantly, that both pre-pandemic levels and changes in burnout are associated with PTSD. The effect of pre-pandemic levels suggests that preventive actions targeting EE and DEP should be adopted before the onset of a health crisis. At the same time, the fact that HCWs who had low levels of EE and DEP before COVID-19 presented a higher likelihood of experiencing worse EE and DEP levels during the pandemic, coupled with the fact that the worsening of burnout was associated with levels of PTSD similar to those of HCWs who had high EE and DEP levels both before and during the pandemic, suggests that it is imperative to take timely action to prevent the worsening of burnout in HCWs who might be unprepared for the emotional burden resulting from a crisis.
The variable featuring the highest association with PTSD was EE. This can be explained by the fact that EE captures the component of fatigue and resource depletion, a condition recognised in the literature as the potential link between burnout and secondary traumatisation and PTSD (Ogińska-Bulik and Juczyński, 2021; Shoji et al., 2015). The independent effect of each of the components of burnout on PTSD has been poorly investigated in a longitudinal study, since most of the studies on burnout and PTSD are cross-sectional and/or do not discriminate between burnout components (Jo et al., 2018; Regehr et al., 2004; Yu et al., 2022). A single cross-sectional study on 3289 firefighters evaluated the role of the different components of burnout, and showed that only depersonalisation was associated with PTSD (Katsavouni et al., 2016). The results of our study extend these findings by showing how this relationship manifests over time, and that it is the worsening of depersonalisation, rather than its levels, that is related to PTSD, along with the changes in PPA and both the levels and changes in EE.
The levels and changes in EE showed a high correlation with psychological distress as well. This was expected, since EE is the variable with the greatest overlap with depression (Koutsimani et al., 2019). Similarly, albeit to a lesser degree, the levels and changes in PPA exert an influence on psychological distress. These results are compatible with the spill-over hypothesis, i.e., burnout is due to the presence of continuous stress depleting the worker's emotional resources, and this depletion generates further losses of other resources and subsequent deteriorated well-being spreading to other areas of life (Hakanen and Schaufeli, 2012; Tóth-Király et al., 2021). Since we did not assess alternative models, such as models in which psychological distress is an antecedent of burnout, these results should be extended by other studies.
It is also interesting to note that, while the effect of EE levels and of their pandemic-related change on psychological distress is similar, the effect of changes in PPA was greater than that of its levels. This result should be interpreted in the context of an average reduction in PPA scores over time, which was more marked in HCWs who had high PPA levels before the pandemic and, especially, in nurse assistants. This reduction can be explained as the effect of the social recognition given to HCWs during the pandemic, which might have provided those who felt dissatisfied in terms of personal accomplishment before the pandemic with the opportunity to feel that their work was important and acknowledged by society (Duracinsky et al., 2022). In general, the pandemic caused a major shift in the duties and routines of HCWs, and the comparison with previous levels of accomplishment might have had a greater impact in terms of well-being. The reduction in PPA due to increased social recognition, or its increase due to worsening working conditions were, therefore, more associated with psychological distress than its initial levels.
In our study, resilience was not related to PTSD. This contrasts with the thriving literature showing that resilience is an important protective factor against PTSD (Li et al., 2022; Liu et al., 2022; Wrenn et al., 2011). In our case, the fact that resilience and PTSD were assessed during the same wave did not allow us to study how this relationship unfolds over time. Since that assessment phase was carried out at a time when the healthcare crisis was still present and HCWs were still experiencing an emergency, the role of resilience might not have already been apparent. However, further studies will be needed to evaluate this hypothesis. In contrast, resilience was associated with psychological distress independently from burnout. Our findings on resilience are cross-sectional and cannot, therefore, be interpreted in a causal fashion. However, the protective role of this variable on mental health disorders through an array of biological and psychological processes is known (Curtin et al., 2022; Laird et al., 2019; Watters et al., 2021). Various psychological treatments are available to increase resilience in HCWs, and have already been tested and found to be effective (Angelopoulou and Panagopoulou, 2022).
This study has an important clinical implication. PTSD symptoms and psychological distress in HCWs should be conceptualised as interconnected with the relationship between HCWs and their workplace. Most of the studies on predictors of PTSD during the pandemic have focused on demographic characteristics of the HCWs and on work routines, such as greater or lesser exposure to the risk of infection, and number of hours worked (Al Falasi et al., 2021; Hill et al., 2022; Hilton et al., 2022; Preti et al., 2020; Yuan et al., 2021). Burnout indicates the presence of chronic stress, which manifests with psychological symptoms and cannot be resolved simply by changing single aspects of the work environment. Both prevention and treatment of PTSD must, therefore, also include thorough changes in work organisation and in psychological treatments by focusing on how HCWs relate to their workplace (West et al., 2018). The opportunity for healthcare systems to cope with future pandemics or disasters lies in increasing public health preparedness, which can be achieved through both policy and funding support, and in terms of work organisation and prevention of burnout (Scales et al., 2022). Since there were no differences between doctors, nurses and nurse assistants concerning changes in EE and DEP, and the worsening of EE, DEP and PPA brought HCWs to PTSD levels similar to those of HCWs who already had high levels of burnout, actions dedicated to all HCWs should be taken during the pandemic to prevent an increase in these dimensions. The decrease in PPA, which was stronger in nurse assistants, might suggest that increasing social recognition of the work of HCWs might be an important strategy to decrease the risk of incurring in PTSD symptoms and psychological distress.
Regarding the implications for research, further longitudinal studies are needed that explore the risk and protective factors of PTSD and psychological distress, as the present study focuses on burnout and resilience, which make up only part of the picture. In addition, it would be interesting to evaluate the role of burnout measured after the pandemic and the subsequent rate of PTSD to assess whether the former variable precedes the latter.
This study has several limitations. First, resilience was measured only during the pandemic, thus limiting the possibility of studying the effects of its pre-pandemic levels on PTSD and psychological distress during COVID-19. Second, although PTSD symptoms and psychological distress were assessed referring to the pandemic period, mental health conditions might have been present also before the pandemic in some of our nurses. Whether previously existing PTSD might have influenced burnout levels before the pandemic is debatable, since there is more evidence in the literature supporting burnout as a predictor of PTSD rather than the other way around (Jo et al., 2018; Ogińska-Bulik and Juczyński, 2021; Regehr et al., 2004). In addition, our longitudinal analyses showed that changes in burnout levels were differential across its dimensions (positive for EE and DEP, negative for PPA), but also across pre-pandemic burnout levels, with those at lower EE and DEP worsening the most, and high PPA subjects improving the most. Hence, it is unlikely that the same underlying mental health condition could have determined such a complex pattern and could explain away the associations with the study outcomes estimated by us. Therefore, our longitudinal design and analyses maintain their validity. However, caution should be paid in interpreting our results in terms of onset of new cases of PTSD and psychological distress. Third, there was a loss of participants from the first to the second survey, which might have caused selection bias. However, the impact of this issue is mitigated by the fact that attrition between the first and the second survey was independent of measured HCWs characteristics (Giusti et al., 2022). Finally, we recruited HCWs from a single hospital in northern Italy and in a particular time frame of the pandemic. Therefore, any generalisation of these findings to other contexts or time frames should be made with caution.
In conclusion, this longitudinal study on HCWs showed that PTSD was associated with previously existing EE and with pandemic-related increases in EE, DEP and PPA, and that psychological distress was associated with previously existing EE and PPA, with increases in EE and PPA over time, as well as with resilience. Actions are required to contrast previously existing EE and to increase personal resources to protect HCWs from MH disorders.
Funding information
The study was supported by a grant given by Fondazione Umberto Veronesi (Grant ID: COVID-19 Insieme per la Ricerca 2020) and by a grant provided by Istituto Nazionale per l'Assicurazione Contro gli Infortuni sul Lavoro (Grant ID: BRIC-2019 ID 29A).
CRediT authorship contribution statement
Emanuele Maria Giusti: Investigation, Formal analysis, Writing – original draft, Writing – review & editing. Giovanni Veronesi: Supervision, Writing – review & editing. Camilla Callegari: Writing – review & editing. Rossana Borchini: Writing – review & editing. Gianluca Castelnuovo: Writing – review & editing. Francesco Gianfagna: Writing – review & editing. Licia Iacoviello: Funding acquisition, Writing – review & editing. Marco Mario Ferrario: Funding acquisition, Visualization, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We wish to thank the Management and administrators of the surveyed hospital for authorising us to conduct this research, and Dr. Simona Boneschi, psychologist, who helped develop the study at the onset. Special thanks go to all healthcare workers enrolled in the study: their participation was a milieu for all of us to give back scientifically valid indications that can help prevent mental health disorders. We would like to acknowledge Dotwords S.r.l. for their valuable language editing support.
References
- Al Falasi B., Al Mazrouei M., Al Ali M., Al Dhamani M., Al Ali A., Al Kindi M., Dalkilinc M., Al Qubaisi M., Campos L.A., Al Tunaiji H., Baltatu O.C. Prevalence and Determinants of Immediate and Long-Term PTSD Consequences of Coronavirus-Related (CoV-1 and CoV-2) Pandemics among Healthcare Professionals: a Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2021;18:2182. doi: 10.3390/ijerph18042182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. American Psychiatric Publishing; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Andhavarapu S., Yardi I., Bzhilyanskaya V., Lurie T., Bhinder M., Patel P., Pourmand A., Tran Q.K. Post-traumatic stress in healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2022;317 doi: 10.1016/j.psychres.2022.114890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelopoulou P., Panagopoulou E. Resilience interventions in physicians: a systematic review and meta-analysis. Appl. Psychol. Health Well Being. 2022;14:3–25. doi: 10.1111/aphw.12287. [DOI] [PubMed] [Google Scholar]
- Aymerich C., Pedruzo B., Pérez J.L., Laborda M., Herrero J., Blanco J., Mancebo G., Andrés L., Estévez O., Fernandez M., Salazar de Pablo G., Catalan A., González-Torres M.Á. COVID-19 pandemic effects on health worker's mental health: systematic review and meta-analysis. Eur. Psychiatry. 2022;65:e10. doi: 10.1192/j.eurpsy.2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi R., Schonfeld I.S., Laurent E. Is burnout separable from depression in cluster analysis? A longitudinal study. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:1005–1011. doi: 10.1007/s00127-014-0996-8. [DOI] [PubMed] [Google Scholar]
- Blevins C.A., Weathers F.W., Davis M.T., Witte T.K., Domino J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J. Trauma Stress. 2015;28:489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol. Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R.T. Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC) Depress. Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Curtin M., Richards H.L., Fortune D.G. Resilience among health care workers while working during a pandemic: a systematic review and meta synthesis of qualitative studies. Clin. Psychol. Rev. 2022;95 doi: 10.1016/j.cpr.2022.102173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Fabio A., Palazzeschi L. Connor-Davidson Resilience Scale: proprietà psicometriche della versione italiana [Connor-Davidson Resilience Scale: psychometric properties of the Italian version] Counsel. Giornale Italiano Ricerca Appl. 2012;5:101–110. [Google Scholar]
- Di Tella M., Romeo A., Zara G., Castelli L., Settanni M. The post-traumatic stress disorder checklist for DSM-5: psychometric properties of the Italian version. Int. J. Environ. Res. Public Health. 2022;19:5282. doi: 10.3390/ijerph19095282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duracinsky M., Marcellin F., Cousin L., Beo V.D., Mahé V., Rousset-Torrente O., Carrieri P., Chassany O. Social and professional recognition are key determinants of quality of life at work among night-shift healthcare workers in Paris public hospitals (AP-HP ALADDIN COVID-19 survey) PLoS One. 2022;17 doi: 10.1371/journal.pone.0265724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einav S., Shalev A.Y., Ofek H., Freedman S., Matot I., Weiniger C.F. Differences in psychological effects in hospital doctors with and without post-traumatic stress disorder. Br. J. Psychiatry. 2008;193:165–166. doi: 10.1192/bjp.bp.108.051532. [DOI] [PubMed] [Google Scholar]
- Frenkel M.O., Pollak K.M., Schilling O., Voigt L., Fritzsching B., Wrzus C., Egger-Lampl S., Merle U., Weigand M.A., Mohr S. Stressors faced by healthcare professionals and coping strategies during the early stage of the COVID-19 pandemic in Germany. PLOS One. 2022;17 doi: 10.1371/journal.pone.0261502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giusti E.M., Veronesi G., Callegari C., Castelnuovo G., Iacoviello L., Ferrario M.M. The North Italian longitudinal study assessing the mental health effects of SARS-CoV-2 pandemic health care workers—Part II: structural validity of scales assessing mental health. Int. J. Environ. Res. Public Health. 2022;19 doi: 10.3390/ijerph19159541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D.P., Hillier V.F. A scaled version of the general health questionnaire. Psychol. Med. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- Hakanen J.J., Schaufeli W.B. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J. Affect. Disord. 2012;141:415–424. doi: 10.1016/j.jad.2012.02.043. [DOI] [PubMed] [Google Scholar]
- Hill J.E., Harris C., Danielle L C., Boland P., Doherty A.J., Benedetto V., Gita B.E., Clegg A.J. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J. Adv. Nurs. 2022 doi: 10.1111/jan.15175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton N.Z., Addison S., Ham E., C Rodrigues N., Seto M.C. Workplace violence and risk factors for PTSD among psychiatric nurses: systematic review and directions for future research and practice. J. Psychiatr. Ment. Health Nurs. 2022;29:186–203. doi: 10.1111/jpm.12781. [DOI] [PubMed] [Google Scholar]
- Jackson T.N., Morgan J.P., Jackson D.L., Cook T.R., McLean K., Agrawal V., Taubman K.E., Truitt M.S. The crossroads of posttraumatic stress disorder and physician burnout: a National Review of United States Trauma and Nontrauma Surgeons. Am. Surg. 2019;85:127–135. [PubMed] [Google Scholar]
- Jo I., Lee S., Sung G., Kim M., Lee S., Park J., Lee K. Relationship between burnout and PTSD symptoms in firefighters: the moderating effects of a sense of calling to firefighting. Int. Arch. Occup. Environ. Health. 2018;91:117–123. doi: 10.1007/s00420-017-1263-6. [DOI] [PubMed] [Google Scholar]
- Katsavouni F., Bebetsos E., Malliou P., Beneka A. The relationship between burnout, PTSD symptoms and injuries in firefighters. Occup. Med. 2016;66:32–37. doi: 10.1093/occmed/kqv144. Lond. [DOI] [PubMed] [Google Scholar]
- Koutsimani P., Montgomery A., Georganta K. The Relationship Between Burnout, Depression, and Anxiety: a Systematic Review and Meta-Analysis. Front Psychol. 2019;10:284. doi: 10.3389/fpsyg.2019.00284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird K.T., Krause B., Funes C., Lavretsky H. Psychobiological factors of resilience and depression in late life. Transl. Psychiatry. 2019;9:1–18. doi: 10.1038/s41398-019-0424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M., Yu X., Wang D., Wang Y., Yao L., Ma Y., Liu X., Zhang Y. Association among resilience, post-traumatic stress disorder, and somatization in frontline healthcare workers in COVID-19: the mediating role of perceived stress. Front. Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.909071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little R.J.A. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 1988;83:1198–1202. [Google Scholar]
- Liu Y., Zou L., Yan S., Zhang P., Zhang J., Wen J., Mao J., Li L., Wang Y., Fu W. Burnout and post-traumatic stress disorder symptoms among medical staff two years after the COVID-19 pandemic in Wuhan, China: social support and resilience as mediators. J. Affect. Disord. 2022;321:126–133. doi: 10.1016/j.jad.2022.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach C., Jackson S.E. The measurement of experienced burnout. J. Organ. Behav. 1981;2:99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- Meier S.T., Kim S. Meta-regression analyses of relationships between burnout and depression with sampling and measurement methodological moderators. J. Occup. Health Psychol. 2022;27:195–206. doi: 10.1037/ocp0000273. [DOI] [PubMed] [Google Scholar]
- Ogińska-Bulik N., Juczyński Z. Burnout and posttraumatic stress symptoms in police officers exposed to traumatic events: the mediating role of ruminations. Int. Arch. Occup. Environ. Health. 2021;94:1201–1209. doi: 10.1007/s00420-021-01689-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang H., Geng S., Zhou Y., Wang J., Zhan J., Shang Z., Jia Y., Yan W., Zhang Y., Li X., Liu W. The increase of PTSD in front-line health care workers during the COVID-19 pandemic and the mediating role of risk perception: a one-year follow-up study. Transl. Psychiatry. 2022;12:180. doi: 10.1038/s41398-022-01953-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker G., Tavella G. Distinguishing burnout from clinical depression: a theoretical differentiation template. J. Affect. Disord. 2021;281:168–173. doi: 10.1016/j.jad.2020.12.022. [DOI] [PubMed] [Google Scholar]
- Piccinelli M., Bisoffi G., Bon M.G., Cunico L., Tansella M. Validity and test-retest reliability of the italian version of the 12-item General Health Questionnaire in general practice: a comparison between three scoring methods. Compr. Psychiatry. 1993;34:198–205. doi: 10.1016/0010-440X(93)90048-9. [DOI] [PubMed] [Google Scholar]
- Preti E., Di Mattei V., Perego G., Ferrari F., Mazzetti M., Taranto P., Di Pierro R., Madeddu F., Calati R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr. Psychiatry Rep. 2020;22:43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regehr C., Hemsworth D., Leslie B., Howe P., Chau S. Predictors of post-traumatic distress in child welfare workers: a linear structural equation model. Child. Youth. Serv. Rev. 2004;26:331–346. doi: 10.1016/j.childyouth.2004.02.003. [DOI] [Google Scholar]
- Restauri N., Sheridan A.D. Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: intersection, impact, and interventions. J. Am. Coll. Radiol. 2020;17:921–926. doi: 10.1016/j.jacr.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scales S.E., Patrick E., Stone K.W., Kintziger K.W., Jagger M.A., Horney J.A. Lessons learned from the public health workforce's experiences with the COVID-19 response. Health Secur. 2022;20:387–393. doi: 10.1089/hs.2022.0091. [DOI] [PubMed] [Google Scholar]
- Schou-Bredal I., Bonsaksen T., Ekeberg Ø., Skogstad L., Grimholt T.K., Heir T. A comparison between healthcare workers and non-healthcare workers’ anxiety, depression and PTSD during the initial COVID -19 lockdown. Public Health in Pract. 2022;3 doi: 10.1016/j.puhip.2022.100267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster B.L. Burnout, posttraumatic stress disorder, or both – listen carefully! Am. J. Med. 2021;134:705–706. doi: 10.1016/j.amjmed.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoji K., Lesnierowska M., Smoktunowicz E., Bock J., Luszczynska A., Benight C.C., Cieslak R. What comes first, job burnout or secondary traumatic stress? Findings from two longitudinal studies from the U.S. and Poland. PLoS One. 2015;10 doi: 10.1371/journal.pone.0136730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoman Y., Marca S.C., Bianchi R., Godderis L., van der Molen H.F., Guseva Canu I. Psychometric properties of burnout measures: a systematic review. Epidemiol. Psychiatr. Sci. 2021;30:e8. doi: 10.1017/S2045796020001134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders C., Pries L.K., Sgammeglia N., Al Jowf G., Youssef N.A., de Nijs L., Guloksuz S., Rutten B.P.F. Resilience against traumatic stress: current developments and future directions. Front. Psychiatry. 2018;9:676. doi: 10.3389/fpsyt.2018.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller T.R., Méan M., Ernst J., Sazpinar O., Gehrke S., Paolercio F., Petry H., Pfaltz M.C., Morina N., Aebischer O., Gachoud D., von Känel R., Weilenmann S. Development of health care workers’ mental health during the SARS-CoV-2 pandemic in Switzerland: two cross-sectional studies. Psychol. Med. 2022;52:1395–1398. doi: 10.1017/S0033291720003128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P., Wang M., Song T., Wu Y., Luo J., Chen L., Yan L. The psychological impact of COVID-19 pandemic on health care workers: a systematic review and meta-analysis. Front. Psychol. 2021;12:626547. doi: 10.3389/fpsyg.2021.626547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tóth-Király I., Morin A.J.S., Salmela-Aro K. Reciprocal associations between burnout and depression: an 8-year longitudinal study. Appl. Psychol. 2021;70:1691–1727. doi: 10.1111/apps.12295. [DOI] [Google Scholar]
- Veronesi G., Giusti E.M., D'Amato A., Gianfagna F., Borchini R., Castelnuovo G., Iacoviello L., Ferrario M.M. The north Italian longitudinal study assessing the mental health effects of SARS-CoV-2 pandemic on health care workers—Part I: study design and psychometric structural validity of the HSE indicator tool and work satisfaction scale. Int. J. Environ. Res. Public Health. 2022;19 doi: 10.3390/ijerph19159514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watters E.R., Aloe A.M., Wojciak A.S. Examining the associations between childhood trauma, resilience, and depression: a multivariate meta-analysis. Trauma Violence Abuse. 2021 doi: 10.1177/15248380211029397. 15248380211029396. [DOI] [PubMed] [Google Scholar]
- West C.P., Dyrbye L.N., Shanafelt T.D. Physician burnout: contributors, consequences and solutions. J. Intern. Med. 2018;283:516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 11th ed. 2019. International Statistical Classification of Diseases and Related Health Problems.https://icd.who.int/en [Google Scholar]
- Wrenn G.L., Wingo A.P., Moore R., Pelletier T., Gutman A.R., Bradley B., Ressler K.J. The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients. J. Natl. Med. Assoc. 2011;103:560–566. doi: 10.1016/s0027-9684(15)30381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B., Barnett D., Menon V., Rabiee L., De Castro Y.S., Kasubhai M., Watkins E. Healthcare worker trauma and related mental health outcomes during the COVID-19 outbreak in New York City. PLOS One. 2022;17 doi: 10.1371/journal.pone.0267315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K., Gong Y.M., Liu L., Sun Y.K., Tian S.S., Wang Y.J., Zhong Y., Zhang A.Y., Su S.Z., Liu X.X., Zhang Y.X., Lin X., Shi L., Yan W., Fazel S., Vitiello M.V., Bryant R.A., Zhou X.Y., Ran M.S., Bao Y.P., Shi J., Lu L. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol. Psychiatry. 2021;26:4982–4998. doi: 10.1038/s41380-021-01036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]