Abstract
Aims
Traffic noise may play an important role in the development and deterioration of ischaemic heart disease. Thus, we sought to determine the mechanisms of cardiovascular dysfunction and inflammation induced by aircraft noise in a mouse model of myocardial infarction (MI) and in humans with incident MI.
Methods and results
C57BL/6J mice were exposed to noise alone (average sound pressure level 72 dB; peak level 85 dB) for up to 4 days, resulting in pro-inflammatory aortic gene expression in the myeloid cell adhesion/diapedesis pathways. The noise alone promoted adhesion and infiltration of inflammatory myeloid cells in vascular/cardiac tissue, paralleled by an increased percentage of leucocytes with a pro-inflammatory, reactive oxygen species (ROS)-producing phenotype and augmented expression of nicotinamide adenine dinucleotide phosphate (NADPH)-oxidase type 2 (Nox2)/phosphorylation of nuclear factor ‘kappa light chain enhancer’ of activated B-cells (phospho-NFκB) in peripheral blood. Ligation of the left anterior descending artery resulted in worsening of cardiac function, pronounced cardiac infiltration of CD11b+ myeloid cells and Ly6Chigh monocytes, and induction of interleukin (IL) 6, IL-1β, CCL-2, and Nox2, being aggravated by noise exposure prior to MI. MI induced stronger endothelial dysfunction and more pronounced increases in vascular ROS in animals preconditioned with noise. Participants of the population-based Gutenberg Health Cohort Study (median follow-up:11.4 years) with incident MI revealed elevated C-reactive protein at baseline and worse left ventricular ejection fraction (LVEF) after MI in case of a history of noise exposure and subsequent annoyance development.
Conclusion
Aircraft noise exposure before MI substantially amplifies subsequent cardiovascular inflammation and aggravates ischaemic heart failure, facilitated by a pro-inflammatory vascular conditioning. Our translational results suggest that measures to reduce environmental noise exposure will be helpful in improving the clinical outcome of subjects with MI.
Key question
How does exposure to aircraft noise impact cardiovascular inflammation?
What is the impact of prior aircraft noise annoyance and inflammation in a mouse model of MI and in patients with incident MI?
Key finding
Aircraft noise exposure induces pro-inflammatory transcriptional changes in the vasculature and primes cardiovascular inflammation.
Aircraft noise exposure prior to MI worsens cardiac and vascular function.
Patients with incident MI have higher C-reactive protein levels at baseline and show worse left ventricular fraction when they had a history of aircraft noise exposure and annoyance.
Take-home-MessageAircraft noise exposure before MI substantially amplifies cardiovascular inflammation and aggravates cardiac impairment after MI.
Keywords: Noise pollution, Aircraft noise, Oxidative stress, Endothelial dysfunction, Inflammation, Myocardial infarction
Graphical Abstract
Graphical Abstract.
Aircraft noise exposure leads to a systemic stress response with activation of myeloid cells and promoting adhesion and infiltration into cardiovascular tissue due to a pro-inflammatory, reactive oxygen species (ROS)-producing phenotype and an augmented expression of Nox2 and phospho-NFκB. Induction of myocardial infarction by permanent ligation of the left anterior descending artery results in worsening of cardiac function, pronounced cardiac infiltration, and increased mitochondrial ROS production aggravated by noise exposure prior to cardiac ischaemia. Created with BioRender.com.
Translational perspective.
In addition to the established traditional cardiovascular risk factors, environmental stressors-like noise exposure should be recognized as targets to prevent and treat CVD. In addition, our observations should help to convince Health organizations, cardiac societies, and legal bodies to control and limit environmental noise pollution at the population level. This will not only protect subjects with established coronary artery disease and patients hospitalized with an acute myocardial infarction but may also reduce incident MI in a population at risk.
1. Introduction
Transportation noise (including aircraft, road, and railway noise) induces an activation of the cerebral cortex, the hypothalamus–pituitary–adrenal axis, and the sympathetic nervous system characterized by an augmented release of their effector hormones cortisol, adrenaline, and noradrenaline.1 These environmental noise-triggered stress reactions were established in models of noise exposure in animals and humans 2–6 and might cause oxidative stress and inflammation, as well as dysregulation of circadian clock genes, mainly mediated via the phagocytic nicotinamide adenine dinucleotide phosphate (NADPH)-oxidase type 2 (Nox2).5,7 Night-time aircraft noise was recently established to be associated with acute cardiovascular mortality.8 Importantly, there is a close link between psychosocial stress and the future development of cardiovascular disease (CVD).9,10 Chronic stress leads to higher circulating levels of pro-inflammatory cytokines like interleukin 6 (IL-6), tumour necrosis factor α (TNFα), or C-reactive protein (CRP) as well as an increased number of circulating leucocytes in humans and may activate myeloid precursor cells in the bone marrow.11 Also, acute psychosocial stress such as mass sports events or natural catastrophes can mediate the up-regulation of inflammatory cytokines and adhesion molecules such as IL-6 and IL-1β as well as vascular adhesion molecule 1 (VCAM-1) or CC-chemokine ligand 2 (CCL-2) in subjected people.12 Epigenetic changes promoting a pro-inflammatory gene regulation centred on CRP in the context of transportation noise exposure were replicated in a large human cohort.13 In mouse models, aircraft noise promotes arterial hypertension, endothelial dysfunction, increased oxidative stress, and infiltration of the vasculature with immune cells.4,5,14 Depletion of myelomonocytic cells ameliorated hypertension, endothelial dysfunction, vascular inflammation, and oxidative stress in the peripheral vessels evoked by noise exposure.15 Aircraft noise also promoted leucocyte–endothelium interaction in arterioles and microvascular dysfunction by a pro-atherothrombotic phenotypic shift of the plasma proteome, all of which was prevented by Nox2 deletion.16
Heart failure resulting from acute myocardial infarction (MI) is a leading cause of morbidity and mortality worldwide.17 Sterile inflammation is crucial for sufficient healing and survival after an acute MI.18–21 However, an excessive or dysregulated immune response post MI is associated with an impaired healing after cardiac ischaemia.22 Both, increased numbers of circulating neutrophils or monocytes and elevated pro-inflammatory cytokines like IL-6 or CRP are connected to a worse outcome post MI, resulting from insufficient scar formation, adverse remodelling, and the development of heart failure.23,24 Since noise exposure leads to neuro-immunological activation and systemic inflammation, we aimed to unravel the mechanisms of how this environmental stressor impacts cardiac and vascular inflammation after MI in a murine model of aircraft noise exposure.
2. Methods
We used C57BL/6J mice as experimental animals. In brief, exposure to aircraft noise was performed following a standardized protocol.4,5 The animals were exposed to a constant (around-the-clock) previously recorded playback of aircraft noise over 48 and 96 h [average sound pressure level of 72 dB(A) and peak sound pressure levels of 85 dB(A)]. Control animals were kept at comparable conditions without aircraft noise exposure. MI was induced by permanent ligation of the left anterior descending artery (LAD) as described previously.25 Mice were anaesthetized with medetomidine (500 µg/kg body weight [bw]), fentanyl (50 µg/kg bw), and midazolam (5 mg/kg bw), and anaesthesia was maintained by endotracheal ventilation with isoflurane (2–3%/1000 mL O2/min). To antagonize the anaesthesia, we injected atipamezol (2.5 mg/kg bw) and flumazenil (0.5 µg/kg bw). Sham surgery followed the same way except for ligation of the LAD. Mice received buprenorphine (0.01 mg/kg i.p.) twice daily for 2 days, starting on the day of surgery. Characterization by high-frequency ultrasound echocardiography was performed 6 days post MI under standardized conditions with 1.5 Vol% isoflurane. Mice were euthanized after administration of subcutaneous injection of buprenorphine (0.075 mg/kg body weight) under deep isoflurane anaesthesia (5 Vol%). Once unresponsive to toe pinch, blood, vascular, and cardiac tissue was collected. Phenotyping of the vessels was performed by vascular relaxation studies. Transcriptome anaylsis was conducted by RNAseq and reverse transcriptase–polymerase chain reaction (RT–PCR), and protein expression analysis by western blot. Cardiovascular inflammation was assessed by intravital videomicroscopy imaging, flow cytometry analysis, and (immuno)histochemistry. All animal procedures performed conform to the guidelines from Directive 2010/63/EU of the European Parliament on the protection of animals used for scientific purposes and were approved by the Animal Care and Use Committee from Rhineland-Palatinate, approval numbers 23 177-07/G 15-1-094 and 23 177-07/G21-1-064. The Gutenberg Health Study is a prospective population-based cohort study including 15 010 individuals (age range 35–74 years) enrolled between April 2007 and April 2012. In a translational approach, we extracted the biodata from individuals in the GHS who experienced an MI in the follow-up (n = 100) and had a history of aircraft noise exposure and annoyance at the time of enrolment. The study conformed to the principles outlined in the Declaration of Helsinki and written informed consent was obtained from each participant. The Gutenberg health study (GHS) was approved by the ethics committee of the Statutory Physician Board of the State Rhineland-Palatinate [Reference No. 837.020.07(5555)] and the local data safety commissioners. For a detailed description of all materials and methods, see the Supplementary material online.
3. Results
3.1. Aircraft noise alone primes cardiovascular inflammation via differential regulation of leucocyte adhesion and diapedesis genes, augmented myelopoiesis, and cardiovascular infiltration of myeloid cells
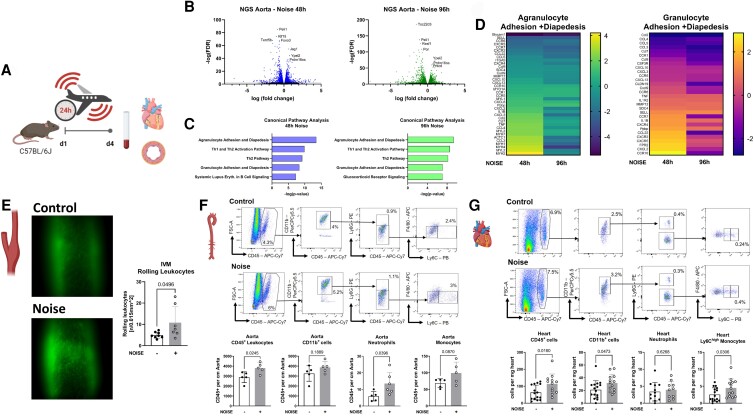
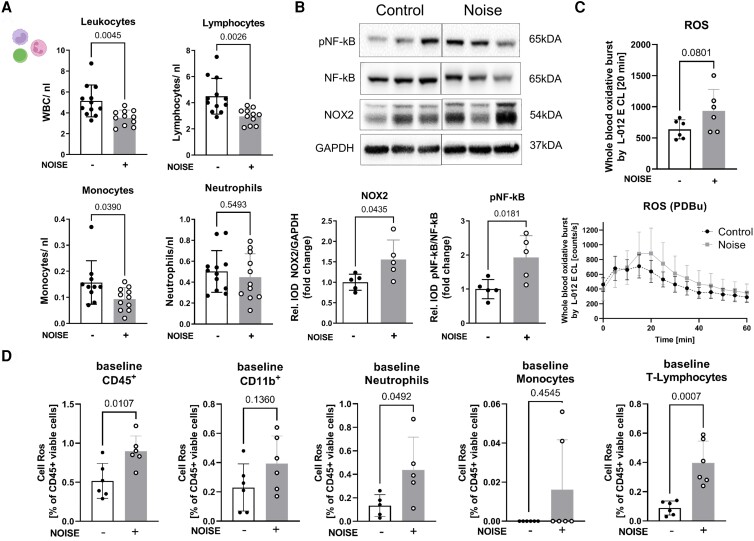
Vascular inflammation is a hallmark of CVD and the magnitude of vascular inflammation predisposes to adverse CVD events such as MI. We, therefore, performed a series of unbiased next-generation RNA sequencing studies of mouse aortas exposed for 48 and 96 h to aircraft noise (Study scheme, Figure 1A) before induction of MI. Our analyses revealed that after 48 h, 312 genes (out of 24 031 detectable transcripts) were expressed differentially of which 137 (44%) were up- and 175 (56%) down-regulated and after 96 h 422 genes (out of 21 126 detectable transcripts) were expressed differentially of which 125 (30%) were up- and 297 (70%) down-regulated (false discovery rate P-value < 0.05, log fold change ≥ ± 1, Figure 1B). Canonical pathway analysis of the top five affected pathways revealed that differentially expressed genes were found on both time points, especially in pathways of leucocyte cell adhesion and diapedesis (Figure 1C and D). Permanent aircraft noise exposure may increase systemic plasma levels of stress hormones, especially norepinephrine and dopamine, as well as the glucocorticoid levels in the kidneys.4 We here observed a trend of higher norepinephrine levels and significantly elevated dopamine concentrations in the plasma of mice with MI and noise (see Supplementary material online, Figure S4). Excitingly, further signalling pathway analysis showed that genes involved in vascular glucocorticoid receptor signalling are differentially regulated due to noise (see Supplementary material online, Figure S1). To follow up on this observation, we performed fluorescence intravital video microscopy imaging of carotid arteries of mice with or without 96 h exposure to aircraft noise and observed aggravated rolling of leucocytes to the endothelium (Figure 1E, see Supplementary material online, Videos S1 and S2). Likewise, flow cytometry analysis of the aorta and heart showed an increased infiltration of total CD45+ leucocytes, with a significant increase of Ly6G+ neutrophils in the aortic tissue and CD11b+ myeloid cells including Ly6Chigh inflammatory monocytes in cardiac tissue in response to 4 days of aircraft noise (Figure 1F and G). Peripheral blood cell count showed a significant reduction of immune cells, in particular monocytes, in the circulation (Figure 2A). Isolation of peripheral mononuclear cells revealed an up-regulation of phagocytic Nox2 as well as increased phosphorylation of nuclear factor ‘kappa light chain enhancer’ of activated B-cells (pNFkB) in response to aircraft noise, reflecting a pro-inflammatory phenotype of these cells (Figure 2B). This is in line with an augmented production of reactive oxygen and nitrogen species at baseline and with stimulation of phorbol 12,13-dibutyrate (PDBu) (Figure 2C) and cellular reactive oxygen species (ROS)-specific flow cytometry of leucocytes (Figure 2D). Taken together, aircraft noise exposure induces pro-inflammatory transcriptional changes in the vasculature and primes cardiovascular inflammation.
Figure 1.
Pre-infarction period: aircraft noise for up to 4 days amplifies leucocyte adhesion and diapedesis and infiltration of immune cells into cardiovascular tissue. (A) Study scheme; (B) volcano plots demonstrating differentially expressed genes 48 h (left) and 96 h (right) after around-the-clock aircraft noise exposure in aortic tissue, noise vs. control animals, n = 4 mice per group; (C) canonical pathway analysis with ingenuity pathway analysis of the five most affected pathways in aortas 48 h (left) and 96 h (right) after around-the-clock aircraft noise exposure, n = 4 mice per group. (D) Heat map displaying differential regulated genes of the agranulocyte and granulocyte diapedesis and adhesion pathway after 48 and 96 h around-the-clock aircraft noise exposure in the aorta. n = 4 mice per group. Expression in Expr Log Ratio. (E) Intravital microscopy imaging of carotids of endothelial rolling leucocytes. Nucleated cells were visualized with acridine orange (green fluorescence). Left: representative images, right: quantification of rolling leucocytes; adherent leucocytes did not significantly differ (P-value 0.1548); n = 6–8 animals per group; mean + SD, Student’s t-test. (F) Flow cytometry of aortic tissue with representative plots and quantification after 96 h of aircraft noise exposure vs. control with quantification of CD45+ leucocytes, CD11b+ myeloid cells, Ly6G+ neutrophils, and monocytes, n = 5 animals per group, mean + SD, Student’s t-test. (G) Flow cytometry of heart tissue with representative plots and quantification after 96 h of aircraft noise exposure vs. control with quantification of CD45+ leucocytes, CD11b+ myeloid cells, Ly6G+ neutrophils, and Ly6Chigh inflammatory monocytes, n = 10–15 animals per group, mean + SD, Student’s t-test.
Figure 2.
Exposure to aircraft noise leads to a reduction of circulating immune cells with a pro-inflammatory and ROS-producing phenotype. (A) Blood cell count of leucocytes, lymphocytes, monocytes, and neutrophils in the blood, n = 11–12 mice per group, mean + SD, Student’s t-test. (B) Western blot analysis of isolated peripheral blood mononuclear cells (PBMCs) and the expression of Nox2 (gp91phox), NfκB/P NfκB after noise exposure. Top: representative western blot images, bottom: quantification. n = 5 per group. mean + SD, Student’s t-test. (C) Superoxide formation in whole blood was measured by enhanced chemiluminescence after stimulation with PDBu, n = 5–6 per group. mean + SD, Student’s t-test. (D) Cell-ROS flow cytometry and quantification of CD45+ leucocytes, CD11b+ myeloid cells, Ly6G+ neutrophils, monocytes, and CD90.2+ T-lymphocytes. n = 6 per group. Mean + SD, Student’s t-test.
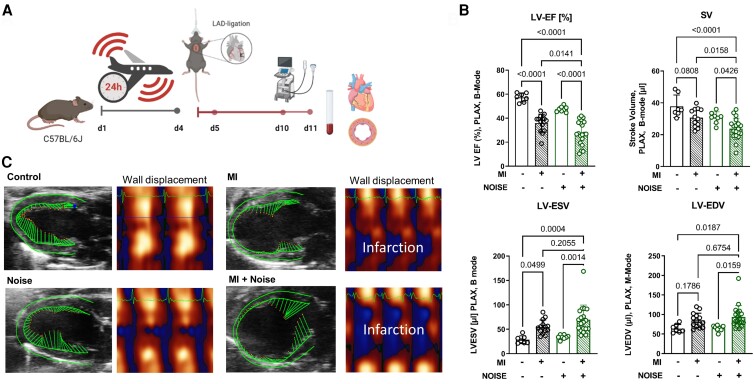
3.2. Aircraft noise exposure prior to acute MI worsens cardiac dysfunction and amplifies vascular inflammation
To investigate the implications of noise-induced inflammatory conditioning of the vasculature on subsequent cardiac injury, we induced MI by permanent ligation of the LAD in mice that had continuously been exposed to aircraft noise for 4 days. We performed high-frequency ultrasound imaging 6 days after MI to assess cardiac function (Study scheme, Figure 3A). Six days after MI, we could not detect a difference in LV geometry assessed by left ventricular end-diastolic volume (LV-EDV), and heart rate increases were comparable between the groups. Importantly, aircraft noise-exposed animals with MI had a reduced left ventricular ejection fraction (LV-EF) and stroke volume (SV) compared to the group only experiencing a MI (Figure 3B and C, Supplementary material online, Table S1).
Figure 3.
Noise exposure worsens cardiac function after acute MI. (A) Experimental study scheme. (B) High-frequency ultrasound echocardiography 6 days after permanent LAD ligation or sham operation with or without noise exposure. Quantification of left-ventricular ejection fraction (LV-EF in %), stroke volume (SV in µL), left-ventricular end-systolic volume (LV-ESV in µL), left-ventricular end-diastolic volume (LV-EDV in µL) in B-Mode images in the parasternal long axis (PLAX). (C) Representative B-Mode images in the parasternal long axis (PLAX) and heat map of wall displacement, n = 7–20, mean + SD, one-way ANOVA with Tukey’s multiple comparison.
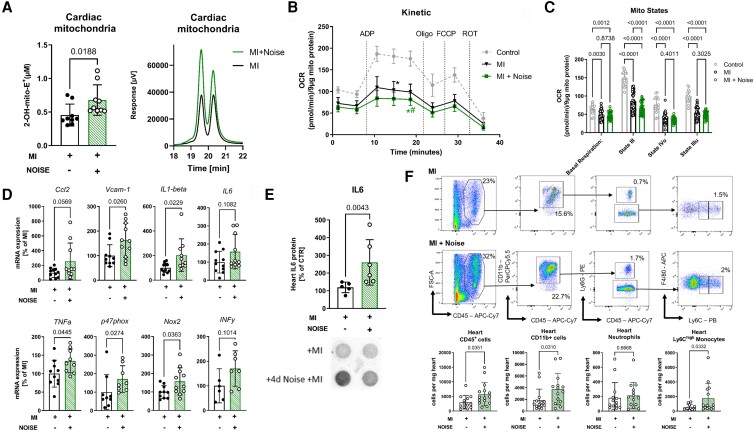
To elucidate the mechanism of impaired cardiac function after MI and previous exposure to aircraft noise, we investigated isolated cardiac mitochondria and observed an augmented mitochondrial ROS production in the ischaemic myocardium, which was already augmented by prior noise exposure (Figure 4A). This was paralleled by the aggravation of MI-induced dysfunction of the mitochondrial respiratory chain specifically in state III, indicating a disturbed oxidative phosphorylation in conditions of adenosine diphosphate (ADP) saturation (Figure 4B and C).
Figure 4.
Post-infarction period: aircraft noise amplifies immune cell infiltration pro-inflammatory cytokines in the ischaemic myocardium and leads to increased myocardial dysfunction. (A) HPLC-based quantification of mitochondrial superoxide formation using specific fluorescent 2-hydroxy-MitoSOX oxidation product, left: quantification, right: representative chromatograms, n = 9 animals per group, mean + SD, Student’s t-test. (B and C) Kinetics of oxygen consumption rate (OCR) in isolated cardiac mitochondria and OCR at different mitochondrial respiratory complexes (e.g. state III or IV upon addition of specific inhibitors/uncouplers: ADP, oligomycin, FCCP, and rotenone), measured by Sea Horse using point-to-point measurements; n = 4–8 animals per group, mean + SD, two-way ANOVA with Bonferroni’s multiple comparison test. (D) mRNA expression of Ccl-2, Vcam-1, Il6, Il1b, tnfα, p47phox, nox2, and infγ in the ischaemic myocardium 7 days post acute myocardial infarction (AMI) with or without aircraft noise exposure, n = 6–12 animals per group, mean + SD, Student’s t-test. (E) Dot plot analysis of cardiac interleukin 6 expression 7 days post AMI with or without aircraft noise exposure, top: quantification, bottom: representative plots, n = 5–6 animals per group, mean + SD, Student’s t-test. (F) Flow cytometry of ischaemic heart tissue 7 days post AMI with or without noise exposure with top: representative plot, bottom: quantification of CD45+ leucocytes, CD45+ CD11b+ myeloid cells, CD45+ CD11b+ Ly6G+ neutrophils and CD45+ CD11b+Ly6G+ Ly6Chigh inflammatory monocytes, n = 13–16 animals per group. mean + SD, Student’s t-test with Mann–Whitney U test.
In line, real-time PCR analysis demonstrated an augmented expression of pro-inflammatory cytokines interleukin 1ß (Il1ß) and TNFα as well as adhesion molecules like vascular cell adhesion molecule 1 (Vcam1) in the ischaemic myocardium of noise-exposed mice in comparison to infarct controls. Interestingly, cardiac expression of the phagocytic Nox2 catalytic subunit as well as regulatory subunit (p47phox) was strongly up-regulated by the aircraft noise exposure alone (Figure 4D), recapitulating the findings made in circulating mononuclear cells. Dot blot analysis of the ischaemic myocardium revealed elevated IL-6 levels (Figure 4E). We carried out flow cytometry examinations of the ischaemic myocardium and observed an increased infiltration of immune cells into the infarcted area of the heart dominated by myeloid CD45 + CD11b+ cells especially CD45 + CD11b + Ly6G− Ly6Chigh inflammatory monocytes (Figure 4F). Collectively, aircraft noise-induced systemic and vascular inflammation amplifies the innate immune response post MI, worsens cardiac function and remodelling, and impairs cardiac mitochondrial function.
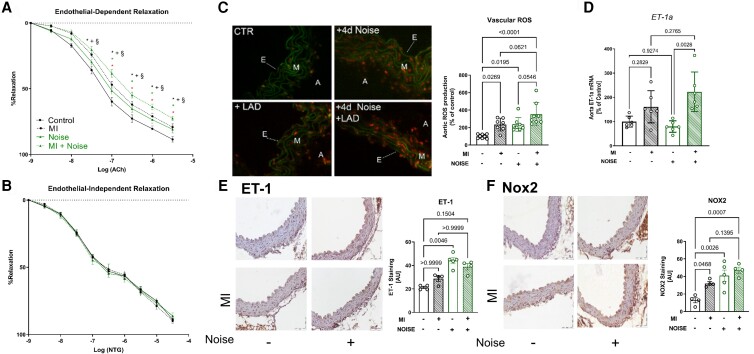
3.3. Establishment of endothelial dysfunction due to increased vascular and systemic ROS production
Ischaemic heart failure is known to cause systemic endothelial dysfunction mediated by vascular infiltration of Nox2+ myeloid cells and augmented ROS formation.25 Thus, we tested, whether additional noise exposure would impact MI-induced systemic and vascular inflammation and ROS formation. Isometric dose–response curves 24 h after MI demonstrated endothelial dysfunction, assessed as attenuation of acetylcholine-induced relaxation of mouse aortas, which was further deteriorated in mice with previous aircraft noise exposure (Figure 5A). Responses to the endothelium-independent vasodilator nitroglycerin were not significantly altered after MI with or without additional noise exposure. (Figure 5B). Noise exposure before MI amplified vascular ROS production as demonstrated via dihydroethidium staining and thus explains the worsening of vascular function (Figure 5C). Cerebral ROS production was equally exaggerated by exposure to noise and cardiac ischaemia. However, we could not determine an additional increase in ROS levels by exposing MI mice to aircraft noise (see Supplementary material online, Figure S5). Determination of aortic mRNA levels of the receptor of the vasoconstrictor endothelin-1 (ET-1a) revealed a significant increase in response to ischaemia and to the combination of noise and ischaemia, while noise alone had no effect. (Figure 5D). Immunohistochemical staining demonstrated an augmented expression of endothelin-1 in mice with previous exhibition to aircraft noise, but we did not detect a significant difference between mice with MI with or without earlier noise exposure. In addition, vascular expression of Nox2 in the aorta was increased after cardiac ischaemia and was further exacerbated by the previous exposure to aircraft noise (Figure 5E and F). Together, MI induced by permanent LAD ligation induces systemic vascular inflammation and ROS formation, which is in part further exaggerated by prior noise exposure.
Figure 5.
Noise exposure aggravates MI-induced vascular dysfunction and vascular ROS production (A) Endothelium-dependent (ACh) and (B) endothelium-independent relaxation of thoracic aortic rings measured by isometric tension method. Data points are measurements from individual samples, n = 8; mean + SD, two-way ANOVA with Bonferroni’s multiple comparison test, *P < 0.05 vs. untreated control; +P < 0.05 vs. + MI, and §P < 0.05 vs. +Noise. (C) Dihydroethidium staining of aortic cryosections and their representative photomicrographs show ROS formation as red fluorescence and autofluorescence from aortic laminae as green. A, adventitia; E, endothelium; M, media; n = 6 individual animals per group, mean + SD, one-way ANOVA with Tukey’s multiple comparison test. (D) mRNA expression ET-1a in aortic tissue post AMI with or without aircraft noise exposure, n = 6, mean + SD, one-way ANOVA with Tukey’s multiple comparison test. (E and F) Immunostaining of Endothelin-1 and NADPH-oxidase 2 (brown colour), n = 4 individual animals per group, mean + SD, one-way ANOVA with Tukey’s multiple comparison test.
3.4. Translational studies: aircraft noise exposure and the resulting annoyance reaction worsen cardiac function and elevate C-reactive protein levels in individuals with incident MI
In the study cohort of the Gutenberg Health Study of 15 010 participants, 100 individuals had experienced an MI at a median follow-up of 11.4 years (Study scheme, see Supplementary material online, Figure S6). Study participants answered a standardized questionnaire concerning the degree of noise annoyance. In total, 54 (54%) of the MI patients reported annoyance with aircraft noise, while 46 (46%) were not annoyed by noise. Comparison of the study populations concerning cardiovascular risk factors (CVRF), comorbidities, laboratory parameters, or medication did not show any statistically significant difference (Table 1), but we established a significantly reduced left ventricular ejection fraction (LV-EF) as well as elevated CRP-levels in patients with incident MI and an additional history of aircraft noise exposure and annoyance reaction (Table 2). We further stratified the patients based on the degree of aircraft noise annoyance reaction in no (46%), slight (23%), moderate (20%), strong (8%), and extreme (3%) annoyance. CVRF, comorbidities, and medication did not differ between the different cohorts (see Supplementary material online, Table S2), but we observed significant differences in LV-EF, the left ventricular mass index, and CRP-levels in the blood of the study participants in relation to the magnitude of noise annoyance (see Supplementary material online, Table S3). This illustrates that a history of aircraft noise exposure and the resulting annoyance elevates inflammatory markers and adversely affects cardiac function in patients with incident MI extracted from a population-based prospective cohort study.
Table 1.
Characteristics of the study population with MI and with or without noise annoyance
| Aircraft noise annoyance | No (n = 46) | Yes (n = 54) | P-value |
|---|---|---|---|
| General parameters | |||
| Sex (women) | 19.6% | 25.9% | 0.48 |
| Age (y) | 61.0 (8.3) | 59.6 (9.4) | 0.43 |
| WHtR | 0.58 (0.08) | 0.6 (0.09) | 0.16 |
| BMI (kg/m2) | 29.0 (25.5/32.0) | 29.2 (26.5/33.6) | 0.31 |
| SBP (mmHg) | 138 (126/151) | 136 (126/149) | 0.68 |
| DBP (mmHg) | 83.0 (10.1) | 83.5 (8.2) | 0.79 |
| HR (bpm) | 68.2 (11.3) | 72.0 (11.0) | 0.09 |
| CVRF | |||
| Diabetes mellitus | 8.9% (4/45) | 18.5% (10/54) | 0.25 |
| Arterial hypertension | 65.2% (30/46) | 72.2% (39/54) | 0.52 |
| Smoking | 30.4% (14/46) | 33.3% (18/54) | 0.83 |
| Obesity | 37.0% (17/46) | 38.9% (21/54) | 1.00 |
| Dyslipidemia | 62.2% (28/45) | 68.5% (37/54) | 0.53 |
| FH of MI/stroke | 23.9% (11/46) | 33.3% (18/54) | 0.38 |
| Comorbidities | |||
| CAD | 6.5% (3/46) | 7.4% (4/54) | 0.68 |
| Stroke | 4.4% (2/45) | 1.9% (1/54) | 0.72 |
| AFib | 13.0% (6/46) | 22.2% (12/54) | 0.30 |
| PAD | 2.2% (1/46) | 5.6% (3/54) | 0.62 |
| Depression (PHQp >= 10) | 4.4% (2/45) | 7.5% (4/53) | 0.68 |
| Cancer | 8.7% (4/46) | 11.1% (6/54) | 0.75 |
| Alcohol (>24/12 g/d) | 28.3% (13/46) | 25.9% (14/54) | 0.82 |
| Laboratory parameters | |||
| Glucose (mg/dL) | 94.0 (88.1/101) | 97.1 (90/104.1) | 0.17 |
| HbA1c (%) | 5.7 (5.3/6) | 5.7 (5.5/5.91) | 0.27 |
| LDL (mg/dL) | 157.2 (32.8) | 150 (34.6) | 0.3 |
| HDL (mg/dL) | 46 (41.0/57.3) | 47 (41.9/55) | 0.62 |
| Cholesterol (mg/dL) | 233 (37) | 228 (37) | 0.45 |
| Triglycerides (mg/dL) | 108 (88/161) | 135 (103/171.3) | 0.07 |
| Medication (ATC code) | |||
| Antihypertensives (c02) | 4.3% (2/46) | 0% (0/54) | 0.21 |
| Diuretics (c03) | 8,7% (4/46) | 5.6% (3/54) | 0.7 |
| Beta-blockers (c07) | 15.2% (7/46) | 24.1% (13/54) | 0.32 |
| Calcium channel blockers (c08) | 8.7% (4/46) | 20.4% (11/54) | 0.16 |
| Agents acting on the RAAS (c09) | 32.6% (15/46) | 35.2% (19/54) | 0.83 |
| Lipid modifying agents (c10) | 17.4% (8/46) | 14.8% (8/54) | 0.79 |
| Diabetic drugs (a10) | 8.7% (4/46) | 7.4% (4/54) | 1.0 |
| Antithrombotic agents (b10) | 10.9% (5/46) | 11.1% (6/54) | 1.0 |
Data are described as mean ± standard deviation (or with median Q1, Q3 if they are skew > 3) or percentage.
WHtR, waist-to-height ratio; BMI, body–mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate; CVRF, cardiovascular risk factors; FH, family history; CAD, coronary artery disease; AFib, atrial fibrillation; PAD, peripheral arterial disease; HbA1c, glycated haemoglobin; LDL, low-density lipoprotein; HDL, high-density lipoprotein; RAAS, renin–angiotensin–aldosterone system.
Table 2.
Echocardiographic and inflammatory parameters of the study population with MI and with or without noise annoyance
| Aircraft noise annoyance | No (n = 46) | Yes (n = 54) | P-value |
|---|---|---|---|
| Echocardiography | |||
| LV-EF (%) | 65.6 (5.6) | 62.5 (5.2) | 0 .0053 |
| E/E′ | 8.71 (6.92/10.1) | 8.21 (6.8/10.42) | 0.6 |
| LVMI (g/m^2.7) | 38.8 (34.1/47.4) | 44.3 (37.8/51.6) | 0.088 |
| RWT | 0.44 (0.11) | 0.43 (0.08) | 0.5 |
| Inflammatory parameters | |||
| C-reactive protein | 1.5 (1.2/3.3) | 3.05 (1.77/5.81) | 0 .0094 |
Data are described as mean ± standard deviation (or with median Q1, Q3 if they are skew > 3) or percentage.
Significance p<0.05 is indicated by bolt values in the last column. LV-EF, left ventricular ejection fraction; LVMI, left ventricular mass index; RW, Relative wall thickness.
4. Discussion
With the present studies, we demonstrate that aircraft noise alone induces a pro-inflammatory transcriptional programme that promotes the infiltration of immune cells into cardiovascular tissue in animals with acute MI. In particular, we established an augmented infiltration of CD45+ cells into the vessels and heart, dominated by neutrophils in the vascular tissue and Ly6Chigh monocytes in cardiac tissue. This creates a pro-inflammatory milieu with a subsequent detrimental impact on the outcome after induction of a MI by predisposing cardiac tissue to more ischaemic damage and functional impairment. Exposure to aircraft noise prior to the initiation of MI by LAD ligation worsens left ventricular function and increases infarct size after cardiac ischaemia driven by an intensified infiltration of pro-inflammatory immune cells and up-regulation of adhesion molecules. It further affects peripheral vessels by worsening MI-induced endothelial dysfunction as early as 24 h post LAD ligation driven by vascular ROS production originating from Nox2 in infiltrated myeloid cells. Our translational study revealed that individuals with a history of aircraft noise exposure and subsequent development of annoyance who experienced an MI had based on the degree of noise annoyance poorer cardiac function and higher systemic CRP levels, suggesting a detrimental impact of aircraft noise on MI outcomes on the population level.
Several epidemiological studies indicate that traffic noise is associated with an increased risk of CVD.1,7,26,27 According to a systematic analysis of the 2018 WHO Environmental Noise Guidelines for the European Region, road traffic noise increases the risk for ischaemic heart disease (IHD).28 The pooled relative risk for IHD was 1.08% (95% confidence interval 1.01–1.115) per 10 dB(A) increase in noise exposure, with clearly evident adverse health effects at noise levels >50 dB(A).29 The effect of transportation noise on the development of heart failure could be observed in five longitudinal studies from London, Switzerland, Stockholm, and in the Rhine-Main region in Germany.30–34 Consistently, these studies reported that aircraft, road, and railway noise increase the incidence and mortality of heart failure by 2–8% per 10 dB(A). Long-term exposure to environmental noise is estimated to cause 48 000 new cases of IHD per year in Europe, on top of inducing sleep disturbance in 6.5 Mio and high annoyance reactions in 22 Mio people.7,35
Even more striking are the recent data by Saucy et al.8: In almost 25 000 cases of death from CVD from the Swiss National Cohort around Zürich Airport, exposure levels 2 h preceding night-time deaths were significantly associated with mortality for all causes of CVD in the highest exposure group.8 Most consistent associations were observed for ischaemic heart diseases, MI, heart failure, and arrhythmia. The authors concluded that night-time aircraft noise can indeed trigger acute cardiovascular mortality. The association was similar to that previously observed for long-term aircraft noise exposure.8 Thus, it is tempting to speculate that night-time noise-induced stress associated with increased heart rate and blood pressure is causing plaque rupture that in turn may trigger these acute events.36
With our current data, we provide a novel mechanism and potential explanation for increased mortality in subjects with ischaemic heart failure in regions with high environmental noise pollution.28,37 Exposure to nocturnal aircraft noise worsens vascular endothelial function measured by flow-mediated dilatation in healthy subjects, and even more so in patients with coronary heart disease.3,38 In mice, aircraft noise induces Nox2 expression and uncoupling of the NO synthase4 leading to increased vascular superoxide formation, which could be reduced by the depletion of myeloid cells.15 It further induces phosphorylation of p47phox at Ser328 and activation of protein kinase C in the aortas of exposed mice. Importantly, knockout of Nox2 strongly ameliorates aircraft noise-induced cardiovascular and cerebral side effects.5 In line with these earlier reports, we demonstrate here that noise exposure worsens aortic endothelial dysfunction in mice with acute MI, at least in part due to increased inflammatory processes and oxidative stress.
Epidemiological studies have linked poor quality of sleep and sleep deprivation to an increased cardiovascular risk.39,40 Additional animal studies and unbiased next generation sequencing analysis demonstrated the impact of noise pollution on circadian clock genes.5 Recent mouse studies link insufficient sleep and cardiovascular inflammation to the secretion of hypocretin.41 This hormone normally restricts myeloid cell production in the bone marrow. In the context of CVDs, sleep deprivation may lead to a progression of atherosclerotic lesions.41 A randomized crossover study enrolling participants exposed to 30 or 60 train noise events as well as 30–120 aircraft noise events per night robustly confirmed the poor quality of sleep induced by this stressor.2,6,38 Sleep deprivation, therefore, seems to be an additional mechanism of annoyance and stress induction hardwired to an activation of innate immune cells. We show now that acute noise exposure over 96 h activates the immune system, induces pro-inflammatory transcriptional changes in the vasculature, and leads to the infiltration of predominantly myeloid cells into cardiac tissue. It is, therefore, very likely that this inflammatory conditioning paves the grounds for impaired cardiac remodelling post MI.
Recent work by Hinterdobler et al. demonstrated that acute stress promotes the rapid expansion of inflammatory leucocytes inside different tissues especially hearts, lungs, and skin, but also atherosclerotic plaques, with norepinephrine-mediated modulation of endothelial cells as a central mechanism.42 In healthy individuals, increased noise exposure caused an increased amygdala activity as well as vascular inflammation assessed by 18F-deoxyglucose positron emission tomography/computed tomography imaging (PET), all of which was associated with a higher risk of major cardiovascular events (MACE).43 Importantly, resilience to noise-induced stress protected from amygdala activation, vascular inflammation, and MACE.44 In the Swiss SAPALDIA study, independent DNA methylation patterns were associated with source-specific exposure to transportation noise and air pollution and shared enrichment for pathways related to inflammation, cellular development, and immune response.45,46 In our study, MI-induced oxidative stress was augmented by noise exposure in the vasculature, but not in the brain. Here, noise exposure per se caused oxidative stress, corroborating earlier findings, but was not incremental to the cerebral stress reaction induced by MI (see Supplementary material online, Figure S5). This suggests, that in our model, cardiovascular inflammation was increased by noise exposure independent of further perturbations of cerebral function.
4.1. Conclusion and clinical implications
Our present findings demonstrated for the first time that aircraft noise exposure for 4 days causes infiltration of predominantly myeloid cells into the heart and the vessels. This pro-inflammatory milieu leads to an excessive immune response and cardiac infiltration of innate immune cells adversely affecting the subsequent myocardial remodelling process after induction of an acute MI leading to a substantial impairment of blood vessel function. Chronic MI induces in septal coronary arteries47 and the thoracic aorta,25 endothelial dysfunction as a major cardiovascular complication in response to MI. In this setting, endothelial dysfunction has been shown to be a direct consequence of MI-induced activation of LysM+ inflammatory cells, exacerbated infiltration of Nox2+ myeloid cells to vascular tissues, and subsequent elevation of ROS formation, all of which was corrected by angiotensin II receptor type 1 (AT1)-receptor blockade or angiotensin-converting enzyme (ACE) inhibition.25,48 Importantly, we now demonstrate that pre-existing endothelial dysfunction induced by aircraft noise exposure leads to an aggravation of ischaemic heart damage post MI, primarily driven by pro-inflammatory transcriptional changes in the vasculature. This pro-inflammatory vascular conditioning (‘negative preconditioning’) may provide a mechanistic explanation for the deterioration of cardiovascular phenotypes such as chronic heart failure or acute coronary syndrome in response to environmental noise exposure.
Supplementary material
Supplementary material is available at Cardiovascular Research online.
Authors’ contributions
H.K.: formal analysis: supporting and visualization: supporting; S.S.: investigation: supporting, methodology: supporting, resources: supporting, and writing—review & editing: supporting; A.S.: data curation: supporting and formal analysis: supporting; R.B.: conceptualization: supporting, writing—original draft: supporting, and writing—review & editing: supporting; S.R.: data curation: supporting and formal analysis: supporting; S.K.: conceptualization: supporting, formal analysis: supporting, resources: equal, and writing—review & editing: supporting; T.M.: conceptualization: lead, funding acquisition: lead, methodology: lead, project administration: lead, resources: lead, supervision: lead, validation: lead, writing—original draft: lead, writing–review & editing: lead; P.W.: conceptualization: lead, formal analysis: lead, funding acquisition: lead, Investigation: lead, methodology: lead, resources: lead, supervision: lead, validation: lead, writing—original draft: lead, and writing—review & editing: lead; A.D.: funding acquisition: equal, investigation: equal, methodology: lead, project administration: lead, resources: equal, writing—original draft: equal, and writing—review & editing: lead; W.R.: resources: equal and supervision: equal; P.W.: investigation: supporting, resources: equal, and supervision: supporting; J.L.: data curation: supporting, formal analysis: supporting, methodology: supporting, and writing—review & editing: supporting; C.W.: data curation: equal, formal analysis: supporting, and writing—original draft: supporting); S.F.: data curation: supporting, formal analysis: supporting, writing—original draft: supporting, writing—review & editing: supporting; O.H.: conceptualization: supporting, data curation: equal, formal analysis: supporting, writing—original draft: supporting, and writing—review & editing: supporting; M.M.: conceptualization: lead, data curation: lead, formal analysis: lead, funding acquisition: lead, investigation: lead, project administration: lead, validation: lead, visualization: lead, writing—original draft: lead, and writing—review & editing: lead; M.T.B.-J.: data curation: equal, formal analysis: equal, methodology: supporting, writing—review & editing: supporting; V.S.G.: data curation: supporting, formal analysis: supporting, writing—original draft: supporting, and writing—review & editing: supporting; M.A.: data curation: equal, formal analysis: equal, methodology: equal, and writing—review & editing: supporting); J.W.: data curation: supporting, methodology: supporting, supervision: equal, visualization: supporting, and writing—review & editing: supporting; T.K.B.: data curation: equal, formal analysis: equal, methodology: supporting, writing—review & editing: supporting; S.K.: data curation: equal, formal analysis: equal, methodology: supporting, visualization: supporting, and writing—review & editing: supporting; T.K.: data curation: equal, formal analysis: equal, methodology: equal, and writing—review & editing: supporting.
Supplementary Material
Acknowledgements
We thank Jörg Schreiner, Nicole Glas, Angelica Karpi as well as Katharina Perius, and Anne-Kathrin Conze for their technical assistance.
Contributor Information
Michael Molitor, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Maria T Bayo-Jimenez, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Omar Hahad, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Claudius Witzler, Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Stefanie Finger, Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Venkata S Garlapati, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Sanela Rajlic, Department of Cardiothoracic and Vascular Surgery, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Tanja Knopp, Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Tabea K Bieler, Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Melania Aluia, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Johannes Wild, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Jeremy Lagrange, Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Université de Lorraine, Inserm, DCAC, Nancy, France; CHRU Nancy, Vandœuvre-lès-Nancy, France.
Recha Blessing, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Steffen Rapp, Department of Cardiology, Preventive Medicine, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Andreas Schulz, Department of Cardiology, Preventive Medicine, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Hartmut Kleinert, Department of Pharmacology, Johannes Gutenberg University Medical Center, Langenbeckstraße 1, 55131 Mainz, Germany.
Susanne Karbach, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Sebastian Steven, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Wolfram Ruf, Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Philipp Wild, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main; Department of Cardiology, Preventive Medicine, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany.
Andreas Daiber, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Thomas Münzel, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Philip Wenzel, Department of Cardiology – Cardiology I, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; Center for Thrombosis and Haemostasis, University Medical Center Mainz, Langenbeckstraße 1, 55131 Mainz, Germany; German Center for Cardiovascular Research (DZHK), partner site Rhine-Main.
Funding
The work was supported by research grants from the Boehringer Ingelheim Foundation for the collaborative research group ‘Novel and neglected risk factors: molecular mechanisms and their therapeutic implications to study the effects of aircraft noise exposure on vascular function and oxidative stress (to M.M., S.S., S.K., W.R., A.D., P.W., T.M.). This work was supported by grants from the Bundesministerium für Bildung und Forschung (BMBF) (BMBF01EO1003 and BMBF01EO1503) and a German Research Foundation (DFG) grant of the Major Research Instrumentation Programme (DFG INST 371/47-1 FUGG). A research grant from the Else-Kröner-Fresenius Foundation was awarded to S.S. (2017_A10) and M.M. (2021_ 2020_EKEA.144). A research grant from the DZHK (Deutsches Zentrum für Herz-Kreislaufforschung was awarded to M.M. (FKZ 81X3210105). W.R. was supported by the Humboldt Foundation. P.W. received funds from the German Research Foundation (DFG) in support of his work (DFG WE 4361/7-1). M.T.B.J. holds a PhD stipend from TransMed PhD Program at the University Medical Center Mainz that was funded by the Boehringer Ingelheim Foundation. W.R., P.W., P.W. and T.M. are Principle Investigators of the DZHK, Partner Site Rhine-Main. The figures and illustrations were created with BioRender.com.
Data availability
The materials and data that support the findings of this study are available from the corresponding author upon reasonable request and discussion.
References
- 1. Munzel T, Sorensen M, Daiber A. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol 2021;18:619–636. [DOI] [PubMed] [Google Scholar]
- 2. Schmidt FP, Basner M, Kroger G, Weck S, Schnorbus B, Muttray A, Sariyar M, Binder H, Gori T, Warnholtz A, Munzel T. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J 2013;34:3508–3514a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schmidt F, Kolle K, Kreuder K, Schnorbus B, Wild P, Hechtner M, Binder H, Gori T, Munzel T. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol 2015;104:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Munzel T, Daiber A, Steven S, Tran LP, Ullmann E, Kossmann S, Schmidt FP, Oelze M, Xia N, Li H, Pinto A, Wild P, Pies K, Schmidt ER, Rapp S, Kroller-Schon S. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J 2017;38:2838–2849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kroller-Schon S, Daiber A, Steven S, Oelze M, Frenis K, Kalinovic S, Heimann A, Schmidt FP, Pinto A, Kvandova M, Vujacic-Mirski K, Filippou K, Dudek M, Bosmann M, Klein M, Bopp T, Hahad O, Wild PS, Frauenknecht K, Methner A, Schmidt ER, Rapp S, Mollnau H, Munzel T. Crucial role for Nox2 and sleep deprivation in aircraft noise-induced vascular and cerebral oxidative stress, inflammation, and gene regulation. Eur Heart J 2018;39:3528–3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Herzog J, Schmidt FP, Hahad O, Mahmoudpour SH, Mangold AK, Garcia Andreo P, Prochaska J, Koeck T, Wild PS, Sorensen M, Daiber A, Munzel T. Acute exposure to nocturnal train noise induces endothelial dysfunction and pro-thromboinflammatory changes of the plasma proteome in healthy subjects. Basic Res Cardiol 2019;114:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Munzel T, Kroller-Schon S, Oelze M, Gori T, Schmidt FP, Steven S, Hahad O, Roosli M, Wunderli JM, Daiber A, Sorensen M. Adverse cardiovascular effects of traffic noise with a focus on nighttime noise and the new WHO noise guidelines. Annu Rev Public Health 2020;41:309–328. [DOI] [PubMed] [Google Scholar]
- 8. Saucy A, Schaffer B, Tangermann L, Vienneau D, Wunderli JM, Roosli M. Does night-time aircraft noise trigger mortality? A case-crossover study on 24 886 cardiovascular deaths. Eur Heart J 2021;42:835–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-amorn C, Sato H, Yusuf S, INTERHEART Investigators . Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:953–962. [DOI] [PubMed] [Google Scholar]
- 10. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, Investigators IS . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 11. Heidt T, Sager HB, Courties G, Dutta P, Iwamoto Y, Zaltsman A, von Zur Muhlen C, Bode C, Fricchione GL, Denninger J, Lin CP, Vinegoni C, Libby P, Swirski FK, Weissleder R, Nahrendorf M. Chronic variable stress activates hematopoietic stem cells. Nat Med 2014;20:754–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wilbert-Lampen U, Nickel T, Leistner D, Guthlin D, Matis T, Volker C, Sper S, Kuchenhoff H, Kaab S, Steinbeck G. Modified serum profiles of inflammatory and vasoconstrictive factors in patients with emotional stress-induced acute coronary syndrome during World Cup Soccer 2006. J Am Coll Cardiol 2010;55:637–642. [DOI] [PubMed] [Google Scholar]
- 13. Eze IC, Jeong A, Schaffner E, Rezwan FI, Ghantous A, Foraster M, Vienneau D, Kronenberg F, Herceg Z, Vineis P, Brink M, Wunderli JM, Schindler C, Cajochen C, Roosli M, Holloway JW, Imboden M, Probst-Hensch N. Genome-wide DNA methylation in peripheral blood and long-term exposure to source-specific transportation noise and air pollution: the SAPALDIA study. Environ Health Perspect 2020;128:67003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Steven S, Frenis K, Kalinovic S, Kvandova M, Oelze M, Helmstadter J, Hahad O, Filippou K, Kus K, Trevisan C, Schluter KD, Boengler K, Chlopicki S, Frauenknecht K, Schulz R, Sorensen M, Daiber A, Kroller-Schon S, Munzel T. Exacerbation of adverse cardiovascular effects of aircraft noise in an animal model of arterial hypertension. Redox Biol 2020;34:101515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Frenis K, Helmstadter J, Ruan Y, Schramm E, Kalinovic S, Kroller-Schon S, Bayo Jimenez MT, Hahad O, Oelze M, Jiang S, Wenzel P, Sommer CJ, Frauenknecht KBM, Waisman A, Gericke A, Daiber A, Munzel T, Steven S. Ablation of lysozyme M-positive cells prevents aircraft noise-induced vascular damage without improving cerebral side effects. Basic Res Cardiol 2021;116:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Eckrich J, Frenis K, Rodriguez-Blanco G, Ruan Y, Jiang S, Bayo Jimenez MT, Kuntic M, Oelze M, Hahad O, Li H, Gericke A, Steven S, Strieth S, von Kriegsheim A, Munzel T, Ernst BP, Daiber A. Aircraft noise exposure drives the activation of white blood cells and induces microvascular dysfunction in mice. Redox Biol 2021;46:102063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD III, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA III, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stockl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen B, Frangogiannis NG. Immune cells in repair of the infarcted myocardium. Microcirculation 2017;24:e12305.. PMID: 27542099. [DOI] [PubMed] [Google Scholar]
- 19. Frangogiannis NG. Inflammation in cardiac injury, repair and regeneration. Curr Opin Cardiol 2015;30:240–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Frangogiannis NG. The inflammatory response in myocardial injury, repair, and remodelling. Nat Rev Cardiol 2014;11:255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Finger S, Knorr M, Molitor M, Schüler R, Garlapati V, Waisman A, Brandt M, Münzel T, Bopp T, Kossmann S, Karbach S, Wenzel P. A sequential interferon gamma directed chemotactic cellular immune response determines survival and cardiac function post-myocardial infarction. Cardiovasc Res 2019;115):1907–1917. [DOI] [PubMed] [Google Scholar]
- 22. Frantz S, Hofmann U, Fraccarollo D, Schafer A, Kranepuhl S, Hagedorn I, Nieswandt B, Nahrendorf M, Wagner H, Bayer B, Pachel C, Schon MP, Kneitz S, Bobinger T, Weidemann F, Ertl G, Bauersachs J. Monocytes/macrophages prevent healing defects and left ventricular thrombus formation after myocardial infarction. FASEB J 2013;27:871–881. [DOI] [PubMed] [Google Scholar]
- 23. Chia S, Nagurney JT, Brown DF, Raffel OC, Bamberg F, Senatore F, Wackers FJ, Jang IK. Association of leukocyte and neutrophil counts with infarct size, left ventricular function and outcomes after percutaneous coronary intervention for ST-elevation myocardial infarction. Am J Cardiol 2009;103:333–337. [DOI] [PubMed] [Google Scholar]
- 24. Groot HE, Al Ali L, van der Horst ICC, Schurer RAJ, van der Werf HW, Lipsic E, van Veldhuisen DJ, Karper JC, van der Harst P. Plasma interleukin 6 levels are associated with cardiac function after ST-elevation myocardial infarction. Clin Res Cardiol 2019;108:612–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Molitor M, Rudi WS, Garlapati V, Finger S, Schüler R, Kossmann S, Lagrange J, Nguyen TS, Wild J, Knopp T, Karbach SH, Knorr M, Ruf W, Münzel T, Wenzel P. Nox2+ myeloid cells drive vascular inflammation and endothelial dysfunction in heart failure after myocardial infarction via angiotensin II receptor type 1. Cardiovasc Res 2021;117:162–177. [DOI] [PubMed] [Google Scholar]
- 26. Hoffmann B, Moebus S, Dragano N, Mohlenkamp S, Memmesheimer M, Erbel R, Jockel KH;Heinz Nixdorf Recall Investigative Group . . Residential traffic exposure and coronary heart disease: results from the Heinz Nixdorf Recall Study. Biomarkers 2009;14(Suppl 1):74–78. [DOI] [PubMed] [Google Scholar]
- 27. Thiesse L, Rudzik F, Spiegel K, Leproult R, Pieren R, Wunderli JM, Foraster M, Heritier H, Eze IC, Meyer M, Vienneau D, Brink M, Probst-Hensch N, Roosli M, Cajochen C. Adverse impact of nocturnal transportation noise on glucose regulation in healthy young adults: effect of different noise scenarios. Environ Int 2018;121:1011–1023. [DOI] [PubMed] [Google Scholar]
- 28. van Kempen E, Casas M, Pershagen G, Foraster M. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health 2018;15:379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization (WHO) . Environmental Noise Guidelines for the European Region. WHO report. World Health Organization. 2018. https://www.euro.who.int/__data/assets/pdf_file/0008/383921/noise-guidelines-eng.pdf(last accessed 04/02/2023).
- 30. Heritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, Thiesse L, Rudzik F, Habermacher M, Kopfli M, Pieren R, Brink M, Cajochen C, Wunderli JM, Probst-Hensch N, Roosli M, SNC study Group . Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur J Epidemiol 2017;32:307–315. [DOI] [PubMed] [Google Scholar]
- 31. Heritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, Thiesse L, Ruzdik F, Habermacher M, Kopfli M, Pieren R, Schmidt-Trucksass A, Brink M, Cajochen C, Wunderli JM, Probst-Hensch N, Roosli M, SNC study Group . Diurnal variability of transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Int J Hyg Environ Health 2018;221:556–563. [DOI] [PubMed] [Google Scholar]
- 32. Halonen JI, Hansell AL, Gulliver J, Morley D, Blangiardo M, Fecht D, Toledano MB, Beevers SD, Anderson HR, Kelly FJ, Tonne C. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur Heart J 2015;36:2653–2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pyko A, Andersson N, Eriksson C, de Faire U, Lind T, Mitkovskaya N, Ogren M, Ostenson CG, Pedersen NL, Rizzuto D, Wallas AK, Pershagen G. Long-term transportation noise exposure and incidence of ischaemic heart disease and stroke: a cohort study. Occup Environ Med 2019;76:201–207. [DOI] [PubMed] [Google Scholar]
- 34. Hahad O, Wild PS, Prochaska JH, Schulz A, Lackner KJ, Pfeiffer N, Schmidtmann I, Michal M, Beutel M, Daiber A, Munzel T. Midregional pro atrial natriuretic peptide: a novel important biomarker for noise annoyance-induced cardiovascular morbidity and mortality? Clin Res Cardiol 2021;110:29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hahad O, Prochaska JH, Daiber A, Muenzel T. Environmental noise-induced effects on stress hormones, oxidative stress, and vascular dysfunction: key factors in the relationship between cerebrocardiovascular and psychological disorders. Oxid Med Cell Longev 2019;2019:Article ID 4623109, pages 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Munzel T, Steven S, Hahad O, Daiber A. Noise and cardiovascular risk: nighttime aircraft noise acutely triggers cardiovascular death. Eur Heart J 2021;42:844–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pershagen G, Van Kempen E, Casas M, Foraster M. Traffic noise and ischemic heart disease – review of the evidence for the WHO environmental noise guidelines for the European region. Eur Heart J 2017;38:710–710. [Google Scholar]
- 38. Schmidt FP, Herzog J, Schnorbus B, Ostad MA, Lasetzki L, Hahad O, Schäfers G, Gori T, Sørensen M, Daiber A, Münzel T. The impact of aircraft noise on vascular and cardiac function in relation to noise event number: a randomized trial. Cardiovasc Res 2021;1171382–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kowall B, Lehnich AT, Erbel R, Moebus S, Jockel KH, Stang A. Associations between sleep characteristics and weight gain in an older population: results of the Heinz Nixdorf Recall Study. Nutr Diabetes 2016;6:e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep 2011;34:1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. McAlpine CS, Kiss MG, Rattik S, He S, Vassalli A, Valet C, Anzai A, Chan CT, Mindur JE, Kahles F, Poller WC, Frodermann V, Fenn AM, Gregory AF, Halle L, Iwamoto Y, Hoyer FF, Binder CJ, Libby P, Tafti M, Scammell TE, Nahrendorf M, Swirski FK. Sleep modulates haematopoiesis and protects against atherosclerosis. Nature 2019;566:383–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hinterdobler J, Schott S, Jin H, Meesmann A, Steinsiek AL, Zimmermann AS, Wobst J, Muller P, Mauersberger C, Vilne B, Baecklund A, Chen CS, Moggio A, Braster Q, Molitor M, Krane M, Kempf WE, Ladwig KH, Hristov M, Hulsmans M, Hilgendorf I, Weber C, Wenzel P, Scheiermann C, Maegdefessel L, Soehnlein O, Libby P, Nahrendorf M, Schunkert H, Kessler T, Sager HB. Acute mental stress drives vascular inflammation and promotes plaque destabilization in mouse atherosclerosis. Eur Heart J 2021;42:4077–4088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Osborne MT, Radfar A, Hassan MZO, Abohashem S, Oberfeld B, Patrich T, Tung B, Wang Y, Ishai A, Scott JA, Shin LM, Fayad ZA, Koenen KC, Rajagopalan S, Pitman RK, Tawakol A. A neurobiological mechanism linking transportation noise to cardiovascular disease in humans. Eur Heart J 2020;41:772–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dar T, Osborne MT, Abohashem S, Abbasi T, Choi KW, Ghoneem A, Naddaf N, Smoller JW, Pitman RK, Denninger JW, Shin LM, Fricchione G, Tawakol A. Greater neurobiological resilience to chronic socioeconomic or environmental stressors associates with lower risk for cardiovascular disease events. Circ Cardiovasc Imaging 2020;13:e010337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Eze IC, Foraster M, Schaffner E, Vienneau D, Heritier H, Rudzik F, Thiesse L, Pieren R, Imboden M, von Eckardstein A, Schindler C, Brink M, Cajochen C, Wunderli JM, Roosli M, Probst-Hensch N. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol 2017;46:1115–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Foraster M, Eze IC, Vienneau D, Schaffner E, Jeong A, Heritier H, Rudzik F, Thiesse L, Pieren R, Brink M, Cajochen C, Wunderli JM, Roosli M, Probst-Hensch N. Long-term exposure to transportation noise and its association with adiposity markers and development of obesity. Environ Int 2018;121:879–889. [DOI] [PubMed] [Google Scholar]
- 47. Gueret A, Harouki N, Favre J, Galmiche G, Nicol L, Henry JP, Besnier M, Thuillez C, Richard V, Kolkhof P, Mulder P, Jaisser F, Ouvrard-Pascaud A. Vascular smooth muscle mineralocorticoid receptor contributes to coronary and left ventricular dysfunction after myocardial infarction. Hypertension 2016;67:717–723. [DOI] [PubMed] [Google Scholar]
- 48. Rudi WS, Molitor M, Garlapati V, Finger S, Wild J, Münzel T, Karbach SH, Wenzel P. ACE inhibition modulates myeloid hematopoiesis after acute myocardial infarction and reduces cardiac and vascular inflammation in ischemic heart failure. Antioxidants (Basel) 2021;10(3):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The materials and data that support the findings of this study are available from the corresponding author upon reasonable request and discussion.