Abstract
Objectives. To estimate county-level cigarette smoking prevalence in Virginia and examine cigarette use disparities by rurality, Appalachian status, and county-level social vulnerability.
Methods. We used 2011–2019 Virginia Behavioral Risk Factor Surveillance System proprietary data with geographical information to estimate county-level cigarette smoking prevalence using small area estimation. We used the Centers for Disease Control and Prevention’s social vulnerability index to quantify social vulnerability. We used the 2-sample statistical t test to determine the differences in cigarette smoking prevalence and social vulnerability between counties by rurality and Appalachian status.
Results. The absolute difference in smoking prevalence was 6.16 percentage points higher in rural versus urban counties and 7.52 percentage points higher in Appalachian versus non-Appalachian counties in Virginia (P < .001). Adjusting for county characteristics, a higher social vulnerability index is associated with increased cigarette use. Rural Appalachian counties had 7.41% higher cigarette use rates than did urban non-Appalachian areas. Tobacco agriculture and a shortage of health care providers were significantly associated with higher cigarette use prevalence.
Conclusions. Rural Appalachia and socially vulnerable counties in Virginia have alarmingly high rates of cigarette use. Implementation of targeted intervention strategies could reduce cigarette use, ultimately reducing tobacco-related health disparities. (Am J Public Health. 2023;113(7):811–814. https://doi.org/10.2105/AJPH.2023.307298)
Cigarette smoking remains the leading cause of preventable morbidity and mortality in the United States.1 Although the prevalence of current cigarette smoking among US adults has decreased over the past several decades to 13.7% in 2018,2 this decrease has not been as pronounced in rural areas,3 such as rural Appalachia (as high as 33% in some counties).4 The Appalachian region, which extends across 13 states, has historically been characterized by its mountainous terrain, poverty, limited health care access, and reliance on tobacco agriculture and coal mining, which may contribute to elevated smoking rates. Smokers living in rural Appalachia are more likely to smoke earlier in life and to smoke more heavily, and they are less likely to successfully quit.3,4 Consequently, smokers in Appalachia are disproportionately affected by smoking-related illnesses.5
Although individual (e.g., attitudes, beliefs) and socioeconomic (e.g., education, income, occupation) factors have been used to explain smoking patterns across the United States,6 much less is known about environmental factors. The Centers for Disease Control and Prevention developed the social vulnerability index (SVI), which evaluates 4 spheres of influence on health: (1) socioeconomic status, (2) household composition and disability, (3) minority status and language, and (4) housing type and transportation. These components are closely tied to a population’s health care access and adherence to health guidelines, which may affect the effectiveness of tobacco control initiatives in rural areas with scarce resources or areas with a high SVI. Although the SVI has been studied extensively with natural disasters and disease outbreaks, we are not aware of any studies that have investigated the association between SVI and cigarette use and how it differs by rurality and Appalachian status.
Disentangling predictors and drivers of tobacco use disparities is a vital step toward promoting tobacco-related health equity. We aimed to fill this gap by examining and comparing county-level disparities in cigarette smoking prevalence by rurality, Appalachian status, and SVI score in Virginia. Specifically, we hypothesized that rural counties, Appalachian counties, and counties with higher SVI scores would have higher cigarette use prevalence. Furthermore, we hypothesized that rural Appalachian counties with a higher SVI score would have the highest prevalence rate.
METHODS
We estimated county-level cigarette smoking prevalence using Virginia Behavioral Risk Factor Surveillance System (BRFSS) data, which surveyed approximately 8832 respondents, representing the approximately 7 million Virginian adults, annually between 2011 and 2019. BRFSS is designed to produce reliable estimates at the state level; however, sample sizes for counties are too small to provide representative area-level estimates. Therefore, to estimate smoking prevalence rates at the county level, we used the small area estimation method.7 To obtain reliable estimates for counties with missing or small sample sizes, we followed standard procedure and combined BRFSS data from 2011 to 2019 into 3 periods of 3 years each (2011–2013, 2014–2016, 2017–2019). We incorporated survey weights into all analyses.
We defined smokers as adults who reported having smoked more than 100 cigarettes in their lifetime and a current smoking frequency of “every day” or “some days.” We classified counties using the 2013 rural–urban continuum codes, with code values 1 to 3 classified as urban and code values 4 to 9 classified as rural.8 We determined whether a county was Appalachian or non-Appalachian based on the Appalachian Regional Commission database.9
We used the SVI to identify counties’ social vulnerability levels10 through 15 social factors across 4 dimensions of vulnerability (range = 0–1, with higher values indicating more vulnerability). We compared current smoking prevalence between rural versus urban and between Appalachian versus non-Appalachian counties using the 2-sample t test. We analyzed the impact of SVI level and the combination of rurality with Appalachian status on county-level cigarette smoking prevalence, controlling for factors such as coal mining, tobacco agriculture, and health care provider shortages using multivariate regression analysis with robust SEs. We mapped SVI with estimated current smoking prevalence along with rural identifiers on Virginia counties using Census shape data files. We performed analyses and mapping in Stata version 16 (StataCorp LP, College Station, TX).
RESULTS
Virginia comprises 133 counties, including 80 (60.15%) urban and 53 (39.85%) rural counties, of which 25 (18.8%) are in the Appalachian region (including 17 rural Appalachian and 8 urban Appalachian). Average SVI level in Virginia was 0.49, whereas average SVI level in rural areas was 0.63 compared with 0.40 in urban areas (P < .001). We found no statistically significant difference in SVI score between Appalachian and non-Appalachian counties (0.51 vs 0.50). However, average SVI score in rural Appalachian counties was higher than in urban Appalachian counties (0.58 vs 0.35; P < .001).
Overall cigarette smoking prevalence in Virginia was 14.80%, whereas cigarette use prevalence among rural counties was 19.38% compared with 13.20% in urban counties (difference = 6.16 percentage points; P < .001). Moreover, cigarette use was significantly higher in Appalachian (20.89%) compared with non-Appalachian (13.37%) counties (difference = 7.52 percentage points; P < .001). Overall, the highest cigarette smoking prevalence was seen in rural Appalachian counties (mean = 22.47%). There were 28 counties in Virginia with a cigarette smoking prevalence higher than 20% and an average SVI score of 0.62 (located in the third quartile of SVI distribution). Of these, the majority were classified as rural (71.43% rural and 35.80% rural Appalachian).
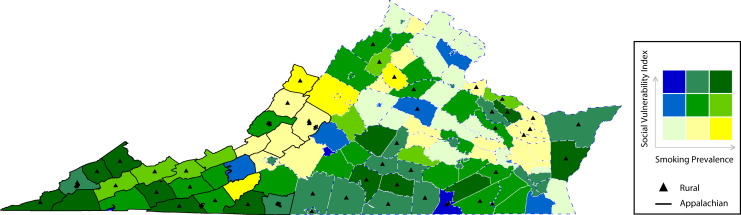
Figure 1 demonstrates the association of high SVI level with high cigarette smoking rates in counties across Virginia for the period of 2017 to 2019. Adjusting for county characteristics, a higher SVI level is associated with increased cigarette use. Rural Appalachian counties had 7.41 percentage points higher cigarette use rates than did urban non-Appalachian areas. Tobacco agriculture and a shortage of health care providers were also significantly associated with higher SVI level and being an Appalachian county (Tables A and B, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
Association of Smoking Prevalence and Social Vulnerability by Rurality and Appalachian Status: Virginia Counties, 2017–2019
Note. We estimated current cigarette smoking prevalence using the small area estimation method. The US Centers for Disease Control and Prevention developed the social vulnerability index; a higher social vulnerability index refers to higher vulnerability. We based urban–rural classifications on the 2013 urban–rural continuum codes developed by the Department of Agriculture and the Rural Health Research Center.8 Counties with code values of 1–3 are classified as urban, and those with code values of 4–9 are considered as rural. We obtained county centroid locations from US Census Bureau shapefiles.
DISCUSSION
Current cigarette smoking rates in Virginia were close to the national average11; however, rates are much higher in rural counties, especially in rural Appalachian counties, signaling the heightened need for action in those areas. Furthermore, rural counties had the highest SVI scores, which also corresponded with higher smoking prevalence. Despite rural Appalachian counties having the highest cigarette smoking rates in Virginia, they did not have the highest SVI levels. We found that tobacco agriculture and lack of health care providers were significantly associated with cigarette smoking prevalence. Further research is needed to examine whether other factors, such as pro-tobacco culture, or multidimensional indexes, such as social deprivation index, also play roles in the high cigarette use rates in rural Appalachia.
Furthermore, it is also possible that the SVI level does not adequately capture the unique social vulnerability characteristics of rural Appalachia. For instance, despite it having a high level of poverty, 84% of the population is non-Hispanic White, and multiunit housing is not common in this region.12 Because these factors make up 2 dimensions of the SVI, the association of SVI score with smoking prevalence by rurality and Appalachian status in our study warrants further investigation to identify the role each dimension of the SVI plays in the elevated smoking prevalence in rural Appalachia. Our findings further underscore the need for both smoking prevention and cessation programs in the rural Appalachian counties of Virginia.
PUBLIC HEALTH IMPLICATIONS
Although smoking has been decreasing over the past decade, residents in rural Appalachian counties of Virginia exhibit alarmingly high rates of cigarette smoking, which likely will result in remarkable and yet preventable health and economic consequences. Implementation of targeted, evidence-based interventions is warranted to reduce tobacco-related disease faced by rural Appalachian residents. Strategies should provide incentives to farmers to grow economically sustainable alternatives to tobacco, increase access to cessation resources in counties with health care shortages, and target campaigns for rural communities on the dangers of tobacco.5
ACKNOWLEDGMENTS
This work was supported by the Cancer Control and Population Health program at the University of Virginia Cancer Center, provided through the National Institutes of Health Cancer Center Support (grant P30CA044579) and the National Cancer Institute (award R01CA267963). The Population Health and Cancer Outcomes Core at the University of Virginia Comprehensive Cancer Center provided percent effort funding support and access to proprietary Behavioral Risk Factor Surveillance System data.
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of these funding agencies.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because no human participants were involved in this study.
REFERENCES
- 1.US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Tobacco product use and cessation indicators among adults—United States. MMWR Morb Mortal Wkly Rep. 2019; 2018;68(45):1013–1019. doi: 10.15585/mmwr.mm6845a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ziller EC, Lenardson JD, Paluso NC, Talbot JA, Daley A. Rural–urban differences in the decline of adolescent cigarette smoking. Am J Public Health. 2019;109(5):771–773. doi: 10.2105/AJPH.2019.304995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardarelli K, Westneat S, Dunfee M, May B, Schoenberg N, Browning S. Persistent disparities in smoking among rural Appalachians: evidence from the Mountain Air Project. BMC Public Health. 2021;21(1):1–12. doi: 10.1186/s12889-021-10334-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beatty K, Hale N, Meit M.Appalachian Regional Commission. 2019. https://www.arc.gov/wp-content/uploads/2020/06/HealthDispairitiesRelatedtoSmokinginAppalachiaApr2019.pdf
- 6. US Department of Health and Human Services Smoking Cessation: A Report of the Surgeon General 2020. https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf
- 7.Rao JNK, Molina I. Small Area Estimation. Hoboken, NJ: Wiley; 2015. [DOI] [Google Scholar]
- 8.US Department of Agriculture. The 2013 urban-rural continuum codes. 2020. https://www.ers.usda.gov/data-products/rural–urban-continuum-codes.aspx
- 9.Appalachian Regional Commission. Appalachian counties. 2022. https://www.arc.gov/appalachian-counties-served-by-arc
- 10.Centers for Disease Control and Prevention, Agency for Toxic Substances and Disease Registry. 2022. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
- 11.Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm
- 12.Pollard K, Jacobsen LA.The Appalachian Region: a data overview from the 2016–2020 American Community Survey. 2022. https://www.arc.gov/report/the-appalachian-region-a-data-overview-from-the-2016-2020-american-community-survey