Abstract
Background
Therapeutic replacement of pancreatic endocrine β-cells is key to improving hyperglycaemia caused by insulin-dependent diabetes . Whilst the pool of ductal progenitors, which give rise to the endocrine cells, are active during development, neogenesis of islets is repressed in the human adult. Recent human donor studies have demonstrated the role of EZH2 inhibition in surgically isolated exocrine cells showing reactivation of insulin expression and the influence on the H3K27me3 barrier to β-cell regeneration. However, those studies fall short on defining the cell type active in transcriptional reactivation events. This study examines the role of the regenerative capacity of human pancreatic ductal cells when stimulated with pharmacological inhibitors of the EZH2 methyltransferase.
Results
Human pancreatic ductal epithelial cells were stimulated with the EZH2 inhibitors GSK-126, EPZ6438, and triptolide using a 2- and 7-day protocol to determine their influence on the expression of core endocrine development marker NGN3, as well as β-cell markers insulin, MAFA, and PDX1. Chromatin immunoprecipitation studies show a close correspondence of pharmacological EZH2 inhibition with reduced H3K27me3 content of the core genes, NGN3, MAFA and PDX1. Consistent with the reduction of H3K27me3 by pharmacological inhibition of EZH2, we observe measurable immunofluorescence staining of insulin protein and glucose-sensitive insulin response.
Conclusion
The results of this study serve as a proof of concept for a probable source of β-cell induction from pancreatic ductal cells that are capable of influencing insulin expression. Whilst pharmacological inhibition of EZH2 can stimulate secretion of detectable insulin from ductal progenitor cells, further studies are required to address mechanism and the identity of ductal progenitor cell targets to improve likely methods designed to reduce the burden of insulin-dependent diabetes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13148-023-01491-z.
Keywords: Islet, Pancreas, Ductal cells, Regenerative capacity, Histone modification, EZH2
Introduction
Among the top 10 leading causes of deaths worldwide, treatment of diabetes remains problematic due to a lack of curative therapeutics, with vigorous vigilance required to maintain normoglycaemia in patients. Whilst transplantation of whole pancreas or purified islets is effective at restoring the glucose index in Type 1 diabetics [1] with the condition, this is severely limited by the numbers of donors worldwide. Given the projected increase in prevalence of diabetes [2], replacement of the insulin-producing β-cells remains an unmet medical need.
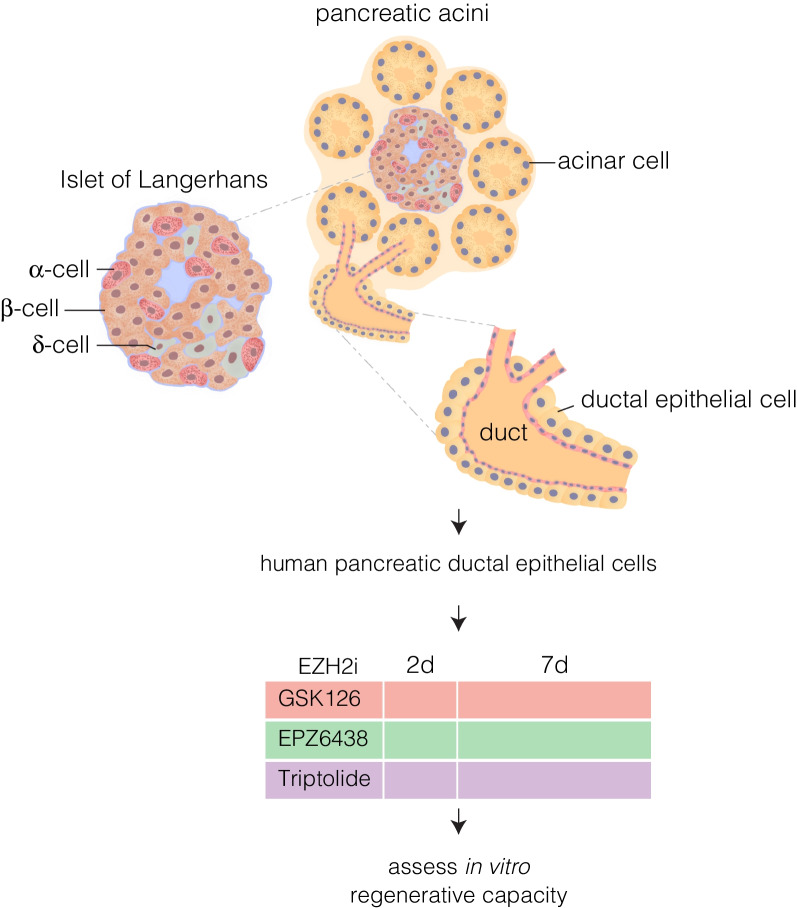
Pancreas organogenesis is tightly regulated by the stepwise expression of transcription factors (TFs) that generates both the exocrine (consisting of the acinar and ductal cells), and endocrine (Islets of Langerhans) compartments (Fig. 1) [3–10]. The existence of stem cells within the pancreatic ducts has been widely debated with observational studies depicting the aggregation of islets adjacent to the ductal epithelium suggestive of their ductal origin [11–14]. Further pancreatic injury models, ranging from pancreatic ductal ligation to partial and 90% pancreatomies, offered support for the hypothesis that stem cells were present within the ductal niche [15] and could give rise to endocrine cells of the islet upon NGN3 expression, similar to embryonic development [16]. More recent studies have demonstrated the existence of ductal NGN3+ cells with the ability to differentiate and give rise to adult β-cells [17]. The results of that study were correlated by single cell RNA sequencing experiments of the ductal progenitor niche [18] and reconfirms evidence from a prior study which demonstrate the presence of ductal progenitors capable of differentiating into α-cells, followed by development into β-cells upon overexpression of Pax4, or inhibition of Arx [19, 20]. Lineage tracing studies of this process clearly demonstrate the existence of ductal NGN3+ cells that have differentiated into insulin-producing β-cells. Although highly active during development, the mechanism of de novo generation of the endocrine compartment by ductal progenitor cells is suppressed in the adult [21, 22], whereas the exocrine compartment is thought to be considerably more plastic. This raises questions to the mechanisms by which this repression is achieved, as well as how it may be reactivated to restore the β-cell mass.
Fig. 1.
Schematic organization of the exocrine and endocrine compartments in the human pancreas featuring the ductal epithelial cells which are hypothesized to contain progenitor cells capable of regeneration upon exposure to EZH2 inhibitors (EZH2i)
A recent study provided evidence for the role of epigenetics in the repression of pancreatic progenitors with the presence of epigenetic modifications differing between ductal progenitors capable of differentiating into β-cells via transgenic overexpression of PAX4 or inhibition of ARX, and the latent progenitor population of wild-type controls [23]. The inhibition of NGN3-positive progenitors is associated with the alteration of histone modifications that are responsible for functionally repressing genes. Differential EZH2 expression during embryogenesis plays an important role on influencing the generation of endocrine progenitors [24]. Furthermore, EZH2 has been shown to regulate the differentiation of pancreatic endocrine progenitors in the embryonic stage [25] along with playing key roles in other models of disease [26, 27]. Therefore, it may have a function in the repression of ductal progenitors in the adult, with inhibition of the EZH2 protein allowing for activation of the adult ductal progenitors. Indeed, further studies show EZH2 inhibition in a mixed exocrine milieu isolated from human donors, stimulated the production of insulin transcripts, resulting in a change in the expression profile [28]. Given the results of previous studies, we had proposed that the increase in insulin as a result of EZH2 inhibition could originate from the ductal progenitors within the mixed exocrine fraction [28]. To investigate this, human pancreatic ductal epithelial cells were stimulated with EZH2 inhibitors (Fig. 1).
Results
Increase in β-cell markers following inhibition of EZH2
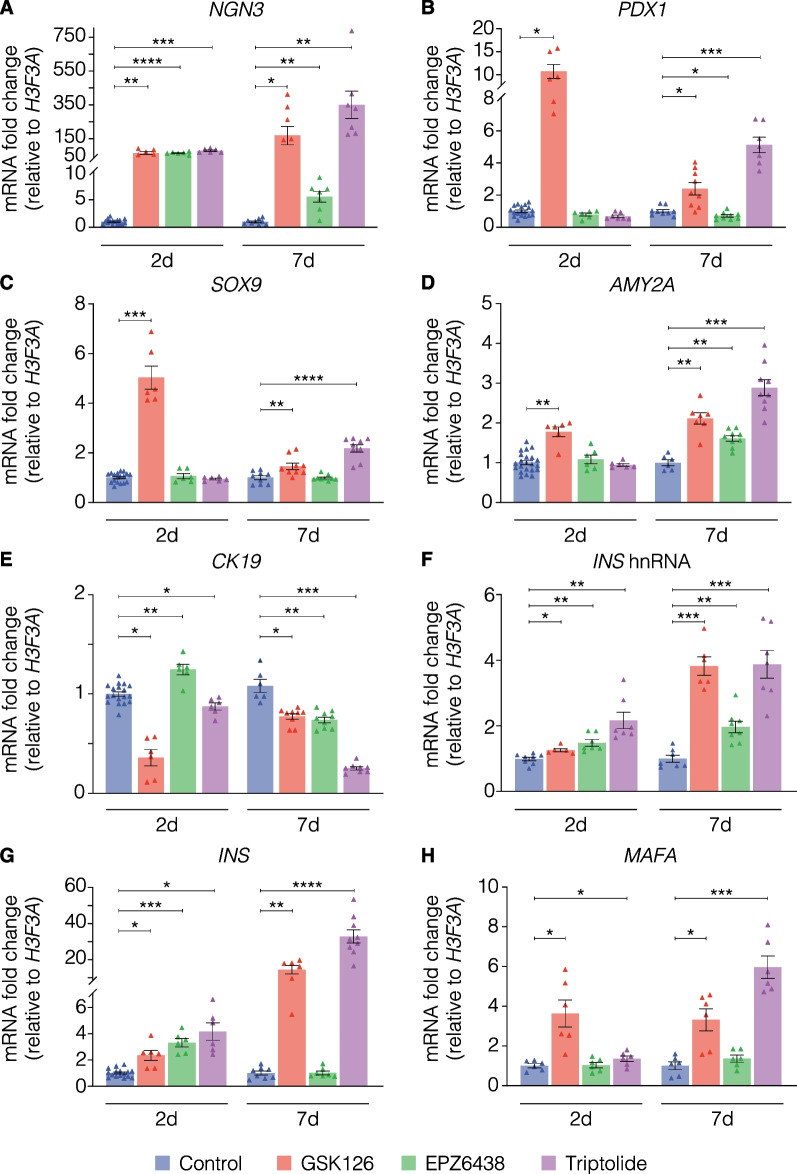
To examine whether pharmacological EZH2 inhibition could influence the terminal differentiated status, adult human pancreatic ductal epithelial cells were stimulated with GSK-126, EPZ6438 and triptolide over 2 and 7 days (Fig. 2). Genes investigated included those important during endocrine development, as well as the expression of genes involved in retention of identity post-development for both ductal and β-cells. Culture of pancreatic ductal cells with GSK-126, EPZ6438 and triptolide for 2 days significantly elevated NGN3 mRNA levels (Fig. 2A). Further increases were observed at 7 days with GSK-126 and triptolide. In contrast, only GSK-126 demonstrated a statistically significant increase in PDX1 expression at 2 days and triptolide demonstrating increase at 7 days (Fig. 2B). A similar observation was seen with SOX9 expression (Fig. 2C). Alpha-amylase (AMY2A) transcripts were increased significantly following 2 days of GSK-126 stimulation, while all EZH2 inhibitors significantly elevated AMY2A mRNA levels (Fig. 2D). There was a decrease in the cytoplasmic CK19 following 2 days of treatment (Fig. 2E) showing statistically significant decreases upon stimulation with GSK-126 and triptolide. Although EPZ-6438 demonstrated an increase at the 2-day time point, by day 7 CK19 expression levels had decreased significantly to match the reduction seen with the other compounds (Fig. 2E).
Fig. 2.
Key markers of endocrine development, epithelial-to-mesenchymal transition, pancreatic ducts, and islets are altered in human pancreatic ductal cells following stimulation with EZH2 inhibitors. Variation in mRNA transcripts of A Neurogenin3 [NGN3], B Pancreatic duodenal homeobox factor 1 [PDX1], C SRY-box transcription factor 9 [SOX9], D Alpha amylase [AMY2A], E Cytokeratin 19 [CK19], F Insulin heterogeneous nuclear RNA [INS hnRNA], G Insulin [INS] and H V-maf musculoaponeurotic fibrosarcoma oncogene homolog A [MAFA], following 2- and 7-day stimulation with GSK-126 at 10 µM, EPZ6438 at 1 µM, and triptolide at 20 nM. Data are displayed as mean of fold change ± S.E.M. of 3 replicates, calculated by normalizing drug values to DMSO (vehicle-treated) controls. Statistically significant change in expression was determined using Student’s t test to compare control values to each drug, *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001
Inhibition of EZH2 in pancreatic ductal cells stimulated a statistically significant increase in insulin transcripts of both the unprocessed heterogeneous nuclear form (Fig. 2F) and the mature mRNA (Fig. 2G). The increase in gene expression was maintained at 7 days with even further increases for triptolide, as well as GSK-126. V-maf musculoaponeurotic fibrosarcoma oncogene homolog A, or MAFA mRNA levels increased in a statistically significant manner at the 2-day point only upon treatment with GSK-126 and triptolide (Fig. 2H). Whilst the fold change compared to vehicle treatment was stable for GSK-126 treatment at 7 days, EPZ-6438 similarly began to induce a statistically significant increase in MAFA transcript.
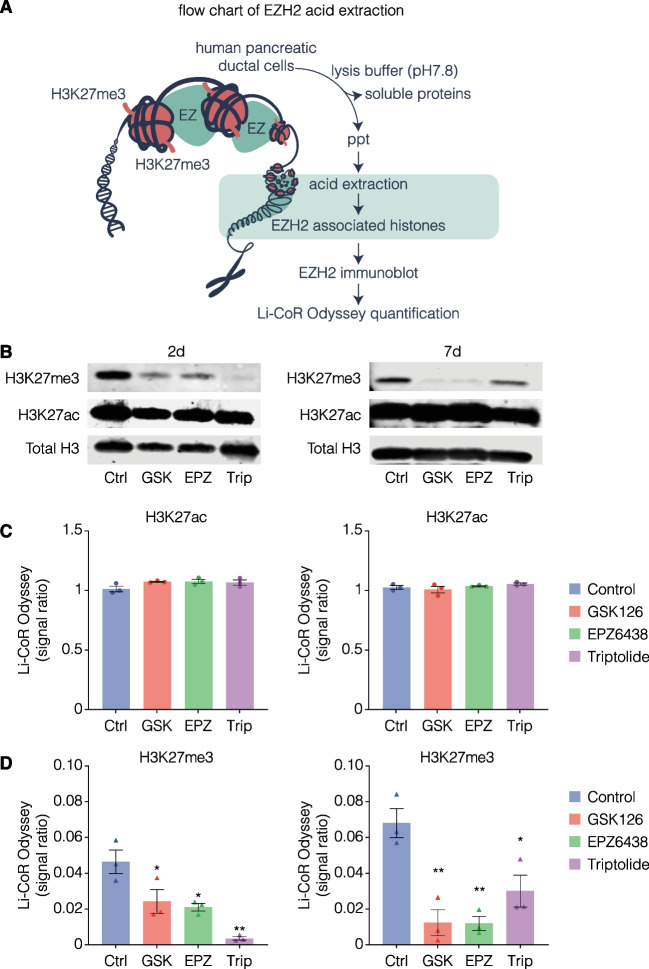
H3K27me3 content is reduced in endocrine genes following EZH2 inhibition
To confirm that the EZH2 inhibitors were working to reduce EZH2 activity within the nuclear chromatin, histone proteins were isolated by acid-extraction from pancreatic ductal cells and analysed for H3K27me3 and H3K27ac content relative to total H3 extracted (Fig. 3A). There was a lack of change in H3K27ac between EZH2i treatments and controls (Fig. 3 B, C). In contrast, following 2 days, the drugs significantly reduced H3K27me3 in the pancreatic ductal cells when compared to the vehicle-treated controls (Fig. 3B, D). Prolonged stimulation over 7 days further decreased H3K27me3 with GSK126 and EPZ6438, which was not noted with triptolide (Fig. 3D).
Fig. 3.
Stimulation with EZH2 inhibitors reduces H3K27me3 content in human pancreatic ductal epithelial cells. A Histone proteins were isolated from pancreatic ductal cells stimulated with EZH2 inhibitors and control cells using 5 M of sulfuric acid. Acid-precipitated (ppt) histone proteins were separated on Nu-Page gel followed by immunoblotting to quantify the total H3 and H2K27me3 levels using Li-CoR Odyssey. B Representative western blots of H3K27me3 and H3K27ac relative to total H3 following 2-day and 7-day stimulation with GSK126 at 10 µM, EPZ6438 at 1 µM, triptolide at 20 nM compared with vehicle control DMSO. C Quantitative analysis of H3K27ac and D H3K27me3 relative to total H3 following 2-day and 7-day stimulation with GSK126 at 10 µM, EPZ6438 at 1 µM, triptolide at 20 nM compared with vehicle control DMSO. Data are displayed as mean signal ratio of H3K27ac or H3K27me3 to total H3 ± SEM of 3 replicates with representative blots above. Each dot plot represents signal ratio of H3K27ac from one independent replicate. Each triangle plot represents signal ratio of H3K27ac or H3K27me3 from one independent replicate. Statistically significant differences were determined using Student’s t-tests against control. *P < 0.05, **P < 0.01
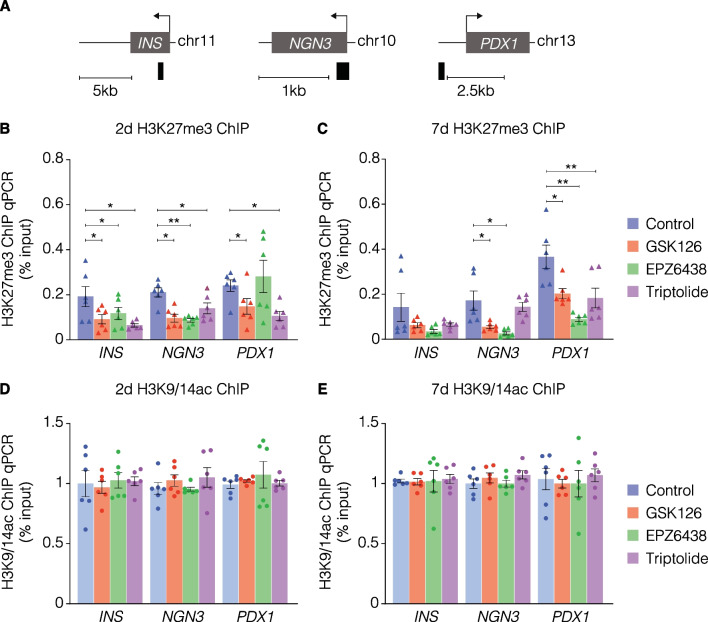
Given that EZH2 is involved in writing H3K27me3 which is associated with gene repression, we next assessed whether gene expression as a result of treatment with EZH2 inhibitors could influence H3K27me3 content of related genes. H3K27me3-associated chromatin was immunopurified (ChIP) from pancreatic ductal cells. qPCR was used to assess H3K27me3 content using primers specifically designed to detect the promoter regions of INS, endocrine master regulator NGN3, and β-cell marker PDX1 (Fig. 4A). Consistent with previous results [28], ChIP revealed GSK-126 significantly reduced the H3K27me3 content of chromatin associated with the INS promoter domain, as well as NGN3 and PDX1 (Fig. 4B). Additionally, these results were also demonstrated with triptolide. EPZ-6438 reduced H3K27me3 content of PDX1 at 7 days (Fig. 4C). Furthermore, a lack of change in the H3K9/14 acetylation (H3K9/14ac) demonstrates the specificity of the EZH2i in modulating the trimethylation signal of human pancreatic ductal epithelial cells (Fig. 4D, E), which is further correlated with a lack of change as assessed by western blots (Additional file 1: Figure S1).
Fig. 4.
Reduction of H3K27me3 content associated with the chromatin of DNA in the INS-IGF2, NGN3, and PDX1 promoter regions following inhibition of EZH2. A H3K27me3 content was assessed by using amplifiers (black bars against DNA regions corresponding to the promoters of INS, NGN3 and PDX1). Quantitative PCR analysis of H3K27me3 associated DNA using ChIP following B 2-day and C 7-day stimulation of human pancreatic ductal epithelial cells compared to vehicle control. Data are displayed as the mean input signal against H3K27me3 abundance ± S.E.M of 3 replicates. Each triangle plot represents one technical replicate. Statistically significant differences were determined using Student’s t-tests against control. *P < 0.05, **P < 0.01, ***P < 0.001. Quantitative PCR analysis of H3K9/14ac associated DNA using ChIP following D 2-day and E 7-day stimulation of human pancreatic ductal epithelial cells compared to vehicle control. Data are displayed as the mean input signal against H3K9/14ac abundance ± S.E.M of 3 replicates. Each dot plot represents one technical replicate. Statistically significant differences were determined using Student’s t-tests against control
EZH2 inhibition stimulates insulin expression in human pancreatic ductal epithelial cells
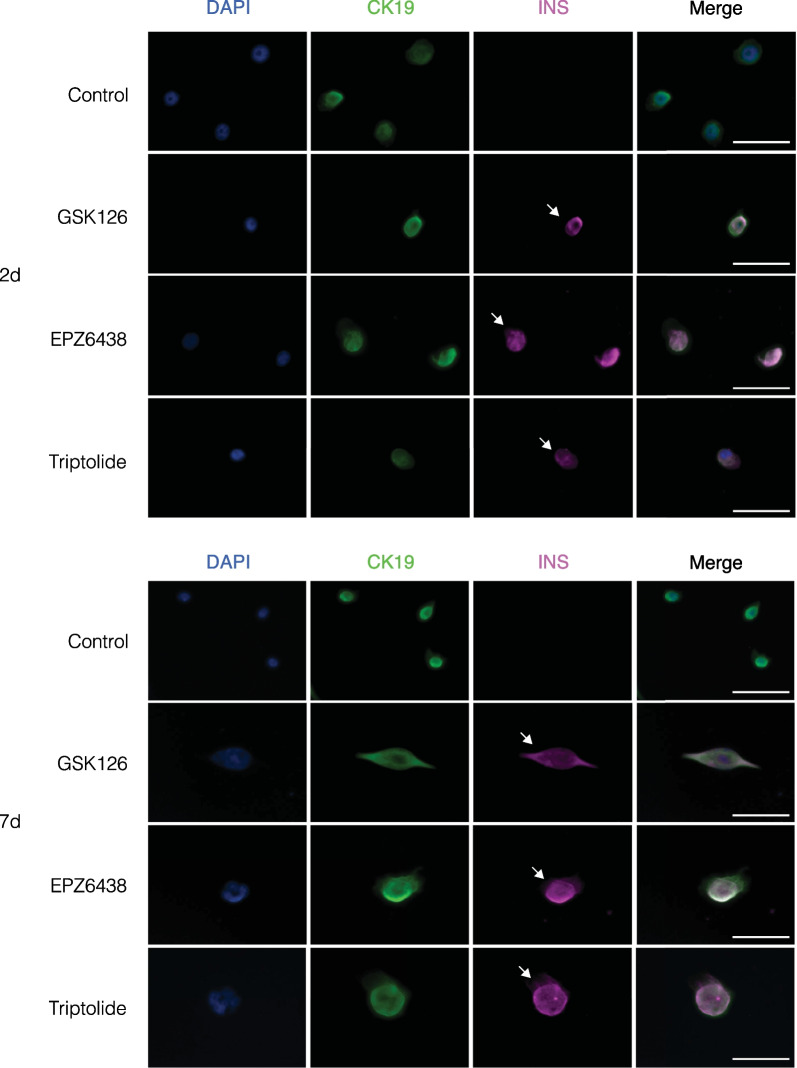
To determine whether increased INS and CK19 gene expression were indicative of a functional synthesis of the protein, cells stimulated with EZH2 inhibitors for 2 and 7 days were stained using immunofluorescence for INS and CK19 with DAPI serving as a control nuclear stain (Fig. 5A). All cells stained were positive for CK19 indicating their ductal cell identity. Importantly, a population of pancreatic ductal cells were positive for insulin, which were not present in the DMSO controls. An average of 3 in 20,000 cells were observed. Following 7 days, there was an overall increase in the numbers of insulin-positive cells, averaging 7 in 20,000 cells per treatment (Fig. 5B).
Fig. 5.
Stimulation of human pancreatic ductal cells with EZH2 inhibitors GSK-126 at 10 µM, EPZ6438 at 1 µM and triptolide at 20 nM influences the expression of insulin (INS) following A 2-day and B 7-day stimulation. Images were captured using ThermoFisher EVOS at 40×magnification and processed on ImageJ. Images are representative of 3 replicates. Scale bar represents 50 µM. White arrows indicate INS expressing CK19-positive cells
Human pancreatic ductal epithelial cells are capable of releasing insulin
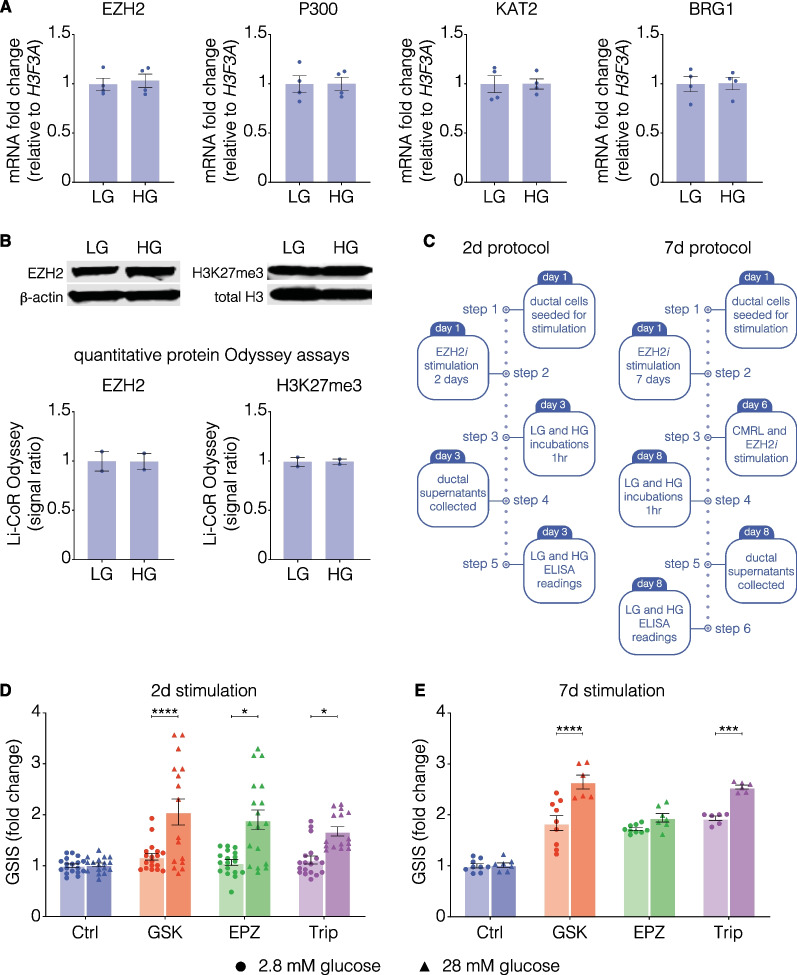
Since insulin was detected by pharmacological EZH2 inhibition, we assessed glucose-stimulated insulin secretion (GSIS). To confirm the specificity of the assay, basal and stimulating levels of EZH2 and H3K27me3 were established by qRT-PCR (Fig. 6A), as well as western blot (Fig. 6B). Additionally, mRNA levels of the histone acetyltransferases P300, KAT2, and chromatin remodeler BRG1 were unchanged following 1 h of incubation in high glucose. There was no change in EZH2 expression, or protein levels as demonstrated by the lack of change in trimethylation following exposure to high glucose, thus confirming that any subsequent alterations in insulin concentration were due to EZH2i stimulation. The GSIS assay was performed following EZH2i stimulation using a 2 or 7 day protocol (Fig. 6C) to examine whether those insulin-producing pancreatic ductal cells were functional in their capacity to produce insulin under 1 h of incubation in basal (2.8 mM glucose) or stimulating (28 mM glucose) conditions. Following incubation in high-glucose media, we observed increased release of insulin from human pancreatic ductal epithelial cells stimulated with GSK-126, EPZ6438 and triptolide (Fig. 6D), which was not observed in the control DMSO-treated cells. Release of insulin was also maintained at 7 days with GSK126 and triptolide (Fig. 6E). Taken together these results suggest there is a population of cells capable of releasing insulin following pharmacological EZH2 inhibition.
Fig. 6.
EZH2 inhibitors influence glucose-sensitive insulin secretion in human pancreatic ductal cells. A Gene expression of chromatin modulators EZH2, P300, KAT2 and BRG1 are unchanged in non-inhibitor-treated cells following exposure to high glucose (HG) compared to non-exposed (LG) cells. Data are presented as mean of fold change ± S.E.M. of 2 replicates, calculated by normalizing high glucose values to low glucose (unexposed) controls. Statistically significant change in expression was determined using Student’s t-test. B Representative western blots and quantitative analysis of EZH2 and H3K27me3 following exposure to high glucose (HG) compared to low glucose (LG). Data are displayed as mean signal ratio of EZH2 to β-actin or H3K27me3 to total H3 ± SEM of 2 replicates with representative blots above. Each dot plot represents signal ratio of one independent replicate. Statistically significant differences were determined using Student’s t-tests against control. C 2- and 7-day protocols for assessment of glucose-stimulated insulin secretion from EZH2 inhibitor (EZH2i) treated human pancreatic ductal epithelial cells. Both protocols were initiated with seeding of cells to establish cultures. Two-day EZH2i stimulation was performed in CMRL to resolve background insulin, whilst for 7-day stimulations, the initial EZH2i doses were delivered in normal growth media, followed by switching to CMRL on day 6. On the final day of the protocol, cells were incubated for 1 h in low glucose followed by 1 h in high glucose. The supernatant was collected for quantification of insulin secretion in ELISAs. ELISA quantified D 2- and E 7-day secretion of insulin from human pancreatic ductal epithelial cells following 1 h of incubation in low (2.8 mM) and high (28 mM) concentrations of glucose. Insulin concentrations were normalized to control 2.8 mM concentrations to calculate fold change. Data are presented as mean of fold change ± S.E.M. of 3 replicates. Dots represent one technical replicate of 2.8 mM glucose supernatant. Triangles represent one technical replicate of 28 mM glucose supernatant. Student’s t-tests were used to assess whether variation in insulin secretion was statistically significant, *P < 0.05, **P < 0.01, ****P < 0.0001
Discussion
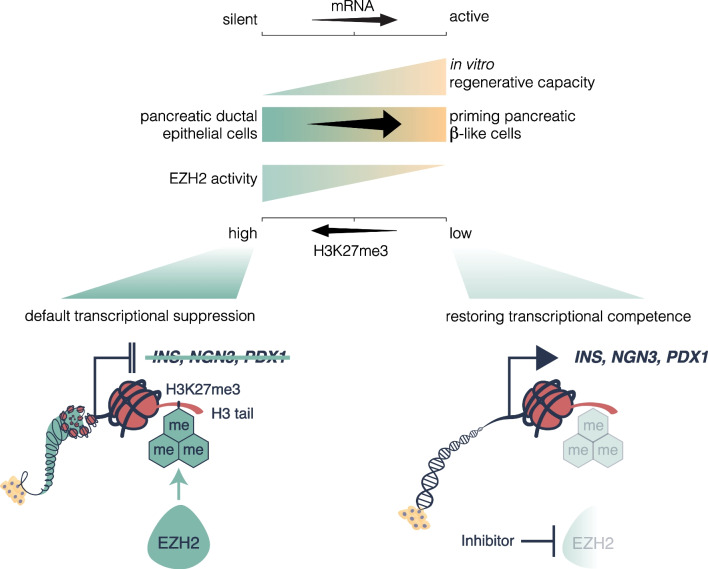
While the default regenerative state of ductal cells is thought to lie dormant in the adult pancreas, the experimental observations of these studies indicate that adult pancreatic ductal progenitor cells can be influenced and re-activated upon stimulation by EZH2 inhibition (Fig. 7).
Fig. 7.
The default transcriptional state of pancreatic ductal progenitors is hypothesized by high EZH2 activity suppressing the expression of endocrine genes such as INS, NGN3 and PDX1. Inhibition of EZH2 restores the progenitor capacity in ductal cells, reducing the H3K27me3 mark and allowing for transcription of genes that influence differentiation into β-like cells
EZH2 is a known epigenetic regulator capable of binding to the master controller of pancreatic endocrine cells NGN3 and considered an important regulator of endocrine fate during development [29]. Consistent with previous studies demonstrating the ability of ductal cells to transdifferentiate from α-cells into insulin-producing cells [19, 20], we observe that the transcriptional expression index of human pancreatic ductal epithelial cells stimulated by pharmacological EZH2 inhibitors can be recapitulated in terminally differentiated adult cells, with increased expression in NGN3 indicating a transition in cell identity resulting from exposure to GSK-126, EPZ-6438, and triptolide. This result closely corresponds with the reduced H3K27me3 chromatin content associated with the NGN3 gene, implying a function for EZH2 in supressing the progenitor population found in the adult pancreatic ductal niche. Indeed, the loss of the repressive H3K27me3 mark plays a role in allowing for the activation of developmental regulators in a number of systems including pancreatic and endocrine formation [30–32]. These developmental regulators, including PDX1, are known to be bivalently primed, possessing both the repressive H3K27me3 and activating H3K4me3 mark, with EZH2 as part of the PcG group playing an important role in maintaining repression in non-endocrine cell types, as well as in endocrine progenitors. SOX9 is considered the master regulator of epithelial-to-mesenchymal transition in a number of developmental processes [5, 7] responsible for regulating downstream genes involved in proliferation and differentiation. The increase in SOX9 gene expression probably reflects the developmental recapitulation of epithelial-to-mesenchymal transition following NGN3 expression as the ductal pancreatic progenitors aggregate to form the endocrine islets, a process that is essential for islet cells to maintain their function by defining their structure [33]. Decreased CK19 expression further reflect this transition, by indicating a subtle yet functionally important loss of ductal cell identity.
Despite elevated NGN3 expression following 2 days, only GSK-126 resulted in a significant tenfold increase of PDX1 transcripts, with longer periods required to stimulate similar increases in PDX1 by other compounds. These results may indicate a greater efficacy of GSK-126 over an identical time period, with more delayed effects demonstrated by the other drugs due to structural variations affecting binding efficacy. Although responsible for inducing pancreatic formation during embryogenesis [34] PDX1 expression in the adult is confined to the β-cell and is critically involved in regulating insulin production in the mature β-cell. Strikingly, 2 days of stimulation was sufficient to demonstrate increased insulin gene expression, as well as protein, albeit in a select number of cells. Interestingly, the elevation of INS hnRNA implies a functional de novo transcription of the insulin gene, which closely correlates with the expression pattern of the mature INS mRNA, [35] further corroborating evidence of the increase in insulin gene expression. In addition, although CK19 gene expression was reduced when treated with GSK-126 at 2 days, with EPZ-6438 and triptolide reducing expression at 7 days, immunofluorescent staining demonstrated no overt reduction in the protein level, possibly indicating a retention of ductal phenotype and representing a more transitionary immature β-cell albeit increased expression of MAFA, which is restricted to mature β-cells in adults similar to PDX1 [36]. Indeed, previous studies have further noted heterogeneity among juvenile and transitionary β-cells, which may reflect the co-staining of insulin and CK19 in this cell population [37]. Importantly, MAFA is critically involved in regulating the ability of β-cells to respond to glucose [38], which may explain the sensitivity to glucose variability. Furthermore, the results of the GSIS assay highlight an important feature of epigenetically reprogrammed insulin-producing cells, namely their ability to reflect mature β-cells by responding to changes in glucose levels by secreting insulin. It is important to note, however, that the increase in the concentration of insulin is at a picomolar level, with mature β-cells demonstrating variations with much larger increases of concentration [39]. Indeed, although staining of 7-day cells displayed a consistent CK19 signal, the increase in insulin positive cell size was more indicative of a progression of the differentiation process, with elevated basal insulin secretion more accurately reflecting physiological conditions displayed by β-cells [39].
As potential therapeutics, GSK-126, and triptolide appear to exert pharmacological effects on transcriptional indices associated with β-cell neogenesis and identity, with GSK-126 showing a greater efficacy at day 2 and triptolide at day 7, displaying an over 300-fold increase in gene transcription in the case of NGN3. This disparity in the transcriptional expression index may lie in the differing modes of action for GSK-126 [40], which is a synthetically designed competitive inhibitor of EZH2, whilst triptolide —a naturally derived EZH2 inhibitor that has been shown to reduce EZH2 at the protein level by inhibiting EZH2 gene transcription [41]. Whilst GSK-126 usage has been primarily trialled as a cancer therapeutic, triptolide has been tested as a treatment for inflammatory conditions [42]. However, there was no measurable difference between the three EZH2 inhibitors on insulin secretion, correlating with their similar effect on the nuclear H3K27me3 content of adult pancreatic ductal cells. Additionally, although GSK-126 and EPZ6438 are both S-adenosyl-l-methionine (SAM) competitive inhibitors of EZH2, they display varied effects on differential gene expression. This might be due to the aforementioned variation in binding capacity, with GSK-126 demonstrating greater specificity to EZH2 relative to EZH1 when compared to EPZ6438 [43]. The specific effects of EZH2 inhibition will need to be explored in subsequent knockdown or silencing experiments to conclusively determine the differential expression profile induced by inhibition of EZH2 unobscured by any off-target effects arising due to the lack of drug clearance in vitro.
This work, albeit important as a proof-of-concept study but also recognizing its limitations, will require evaluation in a suitable diabetic animal model to determine whether the functional response to glucose by inhibiting pancreatic EZH2 is capable of ameliorating hyperglycaemia through a duct-to-β-cell regenerative pathway. The results bear weight given that, although limited in their ability to model normal physiology, the ductal cell line use reflects human epigenetic modifications, which are not always recapitulated in murine models with noted variations between species extending from genetic and cellular regulation to tissue structure as well as overall function [39, 44, 45].
Importantly, based on the results of immunofluorescent staining for insulin, not all ductal cells are capable of responding to EZH2 inhibitor stimulation, highlighting the as-of-yet undefined pool of ductal progenitors that can express NGN3 and differentiate into insulin-producing cells. The differential cellular response reflects the diminutive numbers of progenitor cells, which have been noted previously, as well as reports of heterogeneity in pancreatic cell populations both at the embryonic and the adult stage using single cell analysis [18, 46, 47]. Possible approaches to better characterize these progenitor populations may involve single-cell sequencing to examine which genes or markers can be used to define cells capable of undergoing differentiation into β-like cells. Furthermore, whilst insulin protein expression was detected in our studies, additional experiments need to be conducted to confirm the cellular presence of the other endocrine markers to determine whether these ductal progenitors are able to generate other islet cell types. Likewise, although the inhibition of EZH2 is shown to reduce the H3K27me3 mark, allowing for NGN3 transcription, the specific genes that are differentially regulated downstream of this process and responsible for this transition are yet to be explored.
In summary, while novel therapies that restore β-cell mass are required to effectively ameliorate deficiencies associated with insulin-dependent diabetes, our study serves as a proof of concept that EZH2 inhibition could influence reprogramming of adult human pancreatic ductal cells towards insulin expressing and glucose responsive β-like transitioning cells following 48 h of exposure to inhibitors. Whilst extensively covered during development [25, 30], this is the first paper to determine a role for EZH2 in endocrine cell determination, as well as maintenance of pancreatic ductal progenitors in the adult. Our experimental observations suggest the possibility that reprogrammed cells were capable of producing insulin and functionally elevated insulin secretion in response to glucose stimulation. While the study was limited to in vitro demonstration of EZH2 inhibition, future studies will need to account for heterogeneity in cell populations, as well as investigating the ability to reverse hyperglycaemia in pre-clinical models whilst further characterizing the responsive-regenerative cells. In conclusion, this study provides some evidence that there exists a niche of pancreatic ductal cells that are capable of becoming β-like cells and therefore representing a viable alternative source for cell replacement therapy.
Methods
Cell culture and EZH2 inhibitor stimulation
Human pancreatic ductal epithelial cells were purchased from AddexBio and cultured according to the recommended protocols. Cells were cultured in complete Keratinocyte Serum-Free Media (supplemented with human recombinant EGF, Bovine Pituitary Extract and Antibiotic–Antimycotic [Gibco]). All cell cultures were grown and maintained in a 37 °C, 5% CO2 environment using a tissue culture incubator. Once cells reached 70–80% confluency, passaging was performed using 0.05% Trypsin EDTA (Sigma).
EZH2 inhibitors investigated in this study included the synthetically designed GSK-126 (S7061, SelleckChem), and EPZ-6438 (S7128, SelleckChem), as well as the naturally occurring compound, triptolide (S3604, SelleckChem), which is known to display EZH2 inhibitor activity. Vehicle control was DMSO. Cells were treated over 2 main timepoints, with harvests occurring following 2 and 7 days.
For the 2-day time point, cells were seeded and left to adhere in plates for 24 h. Treatment was initiated with the first dose made up in complete K-SFM. The second dose was delivered 24 h later following a media change. For the longer period of 7 days, cells were initially seeded in 10-cm plates, with doses delivered on alternate days following the initial period of 24 h. When the plate reached 90% confluency, cells were passaged using 0.05% trypsin EDTA (Sigma) and re-seeded at a 1:2 dilution. 3 days prior to harvest, cells were passaged and seeded into cell culture plates depending on the application, with the final addition occurring like the 2-day treatment over 2 periods of 24 h.
RNA extraction and quantitative RT-PCR
TRIzol was used to extract total RNA from 5 × 105 cells seeded in 12-well plates, which were untreated (vehicle control DMSO) or incubated with EZH2 inhibitors for 2 and 7 days. RNA was isolated using the RNeasy Kit according to the manufacturer’s directions. Following measurement of RNA concentration using a QIAxpert System, 1 ug of RNA was used for cDNA synthesis by a high-capacity cDNA Reverse Transcription Kit (Applied Biosystems). The resulting cDNA reaction mix was diluted 1:6 to make up the final template cDNA used subsequently.
Quantitative real-time PCR (qRT-PCR) was performed to examine differential gene expression using the following reaction mix: 5 µL Brilliant II SYBR® Green QPCR Master Mix (600,903, Agilent Technologies), 2 µL nuclease-free water, 2 µL of template cDNA, and 0.5 µL of forward and reverse primer from OligoPerfect designer (Thermo Fisher Scientific), detailed in Table 1. qRT-PCR cycles were carried out using Applied Biosystems 7500 Fast Real-Time PCR System, with each reaction consisting of a 3-min hot start at 95 °C, followed by 40 cycles of 5 s at 95 °C, and 15 s at 60 °C. Ct values of experimental genes were normalized to housekeeping gene H3F3A. Fold change of mRNA abundance was calculated by normalizing drug treated values to vehicular controls.
Table 1.
Human primers for qRT-PCR
| Gene | Primer | Sequence |
|---|---|---|
| H3F3A | Human cDNA forward | ACAAAAGCCGCTCGCAAGAGTG |
| Human cDNA reverse | TTTCTCGCACCAGACGCTGGAA | |
| INS | Human cDNA forward | GCAGCCTTTGTGAACCAACAC |
| Human cDNA reverse | CCCCGCACACTAGGTAGAGA | |
| NGN3 | Human cDNA forward | CTAAGAGCGAGTTGGCACTGA |
| Human cDNA reverse | GAGGTTGTGCATTCGATTGCG | |
| PDX1 | Human cDNA forward | GAAGTCTACCAAAGCTCACGCG |
| Human cDNA reverse | GGAACTCCTTCTCCAGCTCTAG | |
| SOX9 | Human cDNA forward | AGGAAGCTCGCGGACCAGTAC |
| Human cDNA reverse | GGTGGTCCTTCTTGTGCTGCAC | |
| CK19 | Human cDNA forward | AGCTAGAGGTGAAGATCCGCGA |
| Human cDNA reverse | GCAGGACAA TCCTGGAGTTCTC | |
| AMY2A | Human cDNA forward | GATAATGGGAGCAACCAAGTGGC |
| Human cDNA reverse | CAGTATGTGCCAGCAGGAAGAC | |
| MAFA | Human cDNA forward | GCTTCAGCAAGGAGGAGGTCAT |
| Human cDNA reverse | TCTGGAGTTGGCACTTCTCGCT | |
| INS hnRNA | Human cDNA forward | GAGATGGGGAAGATGCTGGG |
| Human cDNA reverse | GGAGGACACAGTCAGGGAGA | |
| EZH2 | Human cDNA forward | TCCTTTTCATGCAACACCCAACACT |
| Human cDNA reverse | TCCAAATGCTGGTAACACTGTGGTC | |
| EP300 | Human cDNA forward | GCAGTGTGCCAAACCAGATG |
| Human cDNA reverse | GGGTTTGCCGGGGTACAATA | |
| KAT2 | Human cDNA forward | ATTCTGCAGGGGCCGAGCCT |
| Human cDNA reverse | ATCACACGGAGCCGCTTGGC | |
| BRG1 | Human cDNA forward | GCTCATGGCTGAAGATGAGG/ |
| Human cDNA reverse | CAGGCGCTTGTCCTTCTTC |
Quantitative PCR Chromatin immunoprecipitation (q-PCR ChIP)
Approximately 5 × 106 cells were fixed in 1% formaldehyde for 10 min, with a further 10-min incubation in 0.125 M glycine to quench the cross-linking reaction. The fixed cell pellet was lysed following resuspension and homogenization in sodium dodecyl (lauryl) sulphate (SDS) lysis buffer (1% SDS, 10 mM EDTA, 50 mM Tris–HCl pH 8.1) with a protease inhibitor cocktail (Roche Diagnostics GmBH, Mannheim, Germany) included. Samples were incubated on ice for 5 min following which sonication was performed to shear chromatin between 200 and 600 bp. Sonicated chromatin was resuspended in ChIP Dilution Buffer (0.01% SDS, 1.1% Triton X-100, 1.2 mM EDTA, 16.7 mM Tris–HCl pH 8.0 and 167 mM NaCl). 20 μL of Dynabeads® Protein A (Invitrogen, Carlsbad, CA, USA) was added to each sample and pre-cleared. Overnight incubation at 4 °C with H3K27me3 or H3K9/14ac antibody was used for immunoprecipitation of chromatin, as previously described. Immunoprecipitates were collected by magnetic isolation and washed sequentially with low-salt and high-salt buffers. Immunoprecipitated DNA was then eluted from solution with 0.1 M NaHCO3 containing 1% SDS. Protein-DNA cross-links were reversed by incubation of samples in Proteinase K (Sigma, St. Louis, MO, USA) for 2 h at 62 °C. DNA was purified using a Qiagen MinElute column (Qiagen Inc., Valencia, CA, USA). H3K27me3 or H3K9/14ac content at the promoters of the INS-IGF2, NGN3 and PDX1 genes was assessed by qPCR using primers designed from the integrative ENCODE resource. ChIP primers are shown in Table 2.
Table 2.
Human primers for q-PCR ChIP
| Gene | Primer | Sequence |
|---|---|---|
| INS-IGF2 | PromR1 forward | GGGAACATAGAGAAAGAGGTCTCA |
| PromR1 reverse | AATTAATCTCAGCTTCCCCCTAAC | |
| NGN3 | PromR1 forward | TTGCTCCTAGCCTATCTTTCCTTA |
| PromR1 reverse | CTTTAGAATTCCTGGACCCTTCTC | |
| PDX1 | PromR1 forward | ACGTTTCTGCAAAGCTGTCTAGTT |
| PromR1 reverse | GGCTTCAAACCATTCAGTAACTTC |
Protein blot
Histone proteins were extracted from 1 × 106 cells per sample. Acid extraction of nuclear proteins and immunoblotting was performed as previously described [26]. Protein content of samples was incubated using Bradford’s Reagent (Sigma), with standard concentrations of BSA used to determine concentration. 1 µg of protein per sample was run on a 4–12% gel (Nu-Page, Invitrogen) before transfer to a PVDF membrane. Membranes (Immobilon-FL; Millipore) were incubated in primary antibody against H3 (1B1B2, CST), H3K27ac (ab4729, Abcam), EZH2 (#4905, CST), β-actin (ab8226, Abcam) and H3K27me3 (07-229, Millipore) overnight (dilutions listed in Table 3). Membranes were incubated in secondary antibody and imaged using LiCoR Odyssey infrared system. Image studio was used to quantify the protein bands with total H3 or β-actin as a loading control.
Table 3.
Antibody dilutions for western blot and immunofluorescent staining of human pancreatic ductal epithelial cells
| Antibody | Dilution |
|---|---|
| Rabbit H3K27me3 | 1:2500 |
| Mouse total H3 | 1:1000 |
| Rabbit H3K27ac | 1:1000 |
| Mouse β-actin | 1: 10,000 |
| Rabbit EZH2 | 1:1000 |
| IRDye® 680CW goat anti-rabbit | 1:10,000 |
| IRDye® 800CW goat anti-mouse | 1:10,000 |
| Rabbit anti-CK19 | 1:200 |
| Guinea pig anti-insulin | 1:250 |
| Alexa fluor 488 donkey anti-rabbit | 1:1000 |
| IRDye® 680CW donkey anti-guinea pig | 1:1000 |
Immunofluorescence
20 × 104 cells were seeded on 15-mm coverslips in 24-well plates and treated with EZH2 inhibitors or vehicle control over 2 or 7 days. Cells were fixed in 4% PFA. 0.1% Triton X diluted in PBS was used to permeabilize cells for 10 min, followed by blocking in a solution of 0.2% gelatin, 2.5% bovine serum albumin made up in PBS (PBG). Primary antibodies against CK19 (HPA002465 Sigma-Aldrich) and INS (A0564, DAKO) were made up in PBG according to the dilutions listed in Table 3 and incubated overnight at 4 °C. Coverslips were washed and incubated with secondary antibodies against rabbit (Alexa Fluor 488), and guinea pig (IRDye® 680CW) (dilutions in Table 3) for 1 h at room temperature. Cells were then washed and incubated with 4′,6-diamidino-2-phenylindole (DAPI) as a nuclear counterstain (at a 1:100 dilution from a 10 μg/mL stock; D8417 Sigma-Aldrich) for 10 min prior to mounting using Prolong Gold Anti-Fade mountant with DAPI (ThermoFisher). Slides were viewed and images were obtained from EVOS (ThermoFisher) using the TagBFP, Cy5, and GFP filters. Images were processed using Image J.
Glucose-stimulated insulin secretion assay
5 × 105 cells were seeded in 12-well plates and allowed to adhere for 24 h. Given the relatively high concentration of insulin in KSFM, cells were washed and cultured with CMRL-complete (CMRL 1066 supplemented with Antibiotic–Antimycotic [Gibco], and Glutamax [Gibco]) to reduce the background insulin concentration of the ELISA. Cells stimulated with EZH2 inhibitors or vehicle control (DMSO) for 2 or 7 days, following which they were washed with 2.8 mM glucose Krebs Buffer Solution (25 mM HEPES, 115 mM sodium chloride, 24 mM sodium hydrogen carbonate, 5 mM potassium chloride, 1 mM magnesium chloride heptahydrate, 0.1% bovine serum albumin, and 2.5 mM calcium chloride dihydrate made up in deionized water) two times, and incubated for 1 h to obtain the low glucose (basal) insulin secretion. Next, cells were cultured in 28 mM (High) glucose Krebs Buffer solution and incubated for 1 h to obtain the glucose stimulated insulin secretion. Supernatant was collected and Ultrasensitive Insulin ELISA (Mercodia) was used to determine the concentration of insulin according to manufacturer’s instructions. Fold change of insulin secreted by cells were calculated by adjusting to cells stimulated with EZH2 inhibitors for insulin concentrations compared to control.
Supplementary Information
Additional file 1. Analysis of H3K9/14 acetylation content relative to total H3 shows no change following treatment with EZH2 inhibitors for 2- and 7-days.
Author contributions
SNM, KA-H, IK, HK, JO and SM performed the studies and data visualization. SNM, KA-H and AE-O wrote the manuscript and SNM, KA-H and AE-O prepared all figures. KA-H and AE-O were involved in conceptualization, supervision, project administration and funding acquisition. All authors read and approved the final manuscript.
Funding
Professor El-Osta is a National Health and Medical Research Council (NHMRC) Senior Research Fellow (1154650) and acknowledges grant support NHMRC Clinical Trials and Cohort Studies Grant (2014763). This work was supported by a research grant from the Danish Diabetes Academy to Professor El-Osta, which is funded by the Novo Nordisk Foundation, grant number NNF17SA0031406 and Juvenile Diabetes Research Foundation (JDRF) United States of America, 1-INO-2022-1123-A-N. This research was partly supported by Yvonne Butterfield research donation including anonymous donors.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Butler AE, Misselbrook D. Distinguishing between type 1 and type 2 diabetes. BMJ: Br Med J (Online) 2020;370:2998. doi: 10.1136/bmj.m2998. [DOI] [PubMed] [Google Scholar]
- 2.Cho NH, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 3.Ramond C, et al. Understanding human fetal pancreas development using subpopulation sorting, RNA sequencing and single-cell profiling. Development. 2018;145(16):dev165480. doi: 10.1242/dev.165480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Offield MF, et al. PDX-1 is required for pancreatic outgrowth and differentiation of the rostral duodenum. Development. 1996;122(3):983–995. doi: 10.1242/dev.122.3.983. [DOI] [PubMed] [Google Scholar]
- 5.Belo J, et al. The role of SOX9 transcription factor in pancreatic and duodenal development. Stem Cells Dev. 2013;22(22):2935–2943. doi: 10.1089/scd.2013.0106. [DOI] [PubMed] [Google Scholar]
- 6.Johansson KA, et al. Temporal control of neurogenin3 activity in pancreas progenitors reveals competence windows for the generation of different endocrine cell types. Dev Cell. 2007;12(3):457–465. doi: 10.1016/j.devcel.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Delous M, et al. Sox9b is a key regulator of pancreaticobiliary ductal system development. PLoS Genet. 2012;8(6):e1002754–e1002754. doi: 10.1371/journal.pgen.1002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishimura W, et al. A switch from MafB to MafA expression accompanies differentiation to pancreatic β-cells. Dev Biol. 2006;293(2):526–539. doi: 10.1016/j.ydbio.2006.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quilichini E, et al. Pancreatic ductal deletion of hnf1b disrupts exocrine homeostasis, leads to pancreatitis, and facilitates tumorigenesis. Cell Mol Gastroenterol Hepatol. 2019;8(3):487–511. doi: 10.1016/j.jcmgh.2019.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gouzi M, et al. Neurogenin3 initiates stepwise delamination of differentiating endocrine cells during pancreas development. Dev Dyn. 2011;240(3):589–604. doi: 10.1002/dvdy.22544. [DOI] [PubMed] [Google Scholar]
- 11.Bonner-Weir S, et al. Transdifferentiation of pancreatic ductal cells to endocrine β-cells. Biochem Soc Trans. 2008;36(3):353–356. doi: 10.1042/BST0360353. [DOI] [PubMed] [Google Scholar]
- 12.Inada A, et al. Carbonic anhydrase II-positive pancreatic cells are progenitors for both endocrine and exocrine pancreas after birth. Proc Natl Acad Sci. 2008;105(50):19915–19919. doi: 10.1073/pnas.0805803105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonner-Weir S, et al. The pancreatic ductal epithelium serves as a potential pool of progenitor cells. Pediatr Diabetes. 2004;5:16–22. doi: 10.1111/j.1399-543X.2004.00075.x. [DOI] [PubMed] [Google Scholar]
- 14.Bonner-Weir S, et al. A second pathway for regeneration of adult exocrine and endocrine pancreas: a possible recapitulation of embryonic development. Diabetes. 1993;42(12):1715–1720. doi: 10.2337/diab.42.12.1715. [DOI] [PubMed] [Google Scholar]
- 15.Li WC, et al. Activation of pancreatic-duct-derived progenitor cells during pancreas regeneration in adult rats. J Cell Sci. 2010;123(Pt 16):2792–2802. doi: 10.1242/jcs.065268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu X, et al. β cells can Be generated from endogenous progenitors in injured adult mouse pancreas. Cell. 2008;132(2):197–207. doi: 10.1016/j.cell.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 17.Gribben C, et al. Ductal Ngn3-expressing progenitors contribute to adult β cell neogenesis in the pancreas. Cell Stem Cell. 2021;28(11):2000–2008.e4. doi: 10.1016/j.stem.2021.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qadir MMF, et al. Single-cell resolution analysis of the human pancreatic ductal progenitor cell niche. Proc Natl Acad Sci. 2020;117(20):10876–10887. doi: 10.1073/pnas.1918314117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Hasani K, et al. Adult duct-lining cells can reprogram into β-like cells able to counter repeated cycles of toxin-induced diabetes. Dev Cell. 2013;26(1):86–100. doi: 10.1016/j.devcel.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 20.Ben-Othman N, et al. Long-term GABA administration induces alpha cell-mediated beta-like cell neogenesis. Cell. 2017;168(1):73–85.e11. doi: 10.1016/j.cell.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Kopp JL, et al. Sox9+ ductal cells are multipotent progenitors throughout development but do not produce new endocrine cells in the normal or injured adult pancreas. Development. 2011;138(4):653–665. doi: 10.1242/dev.056499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Solar M, et al. Pancreatic exocrine duct cells give rise to insulin-producing β cells during embryogenesis but not after birth. Dev Cell. 2009;17(6):849–860. doi: 10.1016/j.devcel.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Khurana I, et al. DNA methylation status correlates with adult β-cell regeneration capacity. NPJ Regen Med. 2021;6(1):1–5. doi: 10.1038/s41536-021-00119-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mallen-St Clair J, et al. EZH2 couples pancreatic regeneration to neoplastic progression. Genes Dev. 2012;26(5):439–444. doi: 10.1101/gad.181800.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu C-R, et al. Dynamics of genomic H3K27me3 domains and role of EZH2 during pancreatic endocrine specification. EMBO J. 2014;33(19):2157–2170. doi: 10.15252/embj.201488671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaipananickal H, et al. Targeting treatment refractory NET by EZH2 inhibition in postural tachycardia syndrome. Circ Res. 2020;126(8):1058–1060. doi: 10.1161/CIRCRESAHA.119.315654. [DOI] [PubMed] [Google Scholar]
- 27.Tang Y, et al. Inhibition of EZH2 primes the cardiac gene activation via removal of epigenetic repression during human direct cardiac reprogramming. Stem Cell Res. 2021;53:102365. doi: 10.1016/j.scr.2021.102365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Hasani K, et al. Inhibition of pancreatic EZH2 restores progenitor insulin in T1D donor. Sign Transduct Target Ther. 2022;7(1):248. doi: 10.1038/s41392-022-01034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jin C, et al. EZH2 deletion promotes spermatogonial differentiation and apoptosis. Reproduction. 2017;154(5):615–625. doi: 10.1530/REP-17-0302. [DOI] [PubMed] [Google Scholar]
- 30.Xie R, et al. Dynamic chromatin remodeling mediated by polycomb proteins orchestrates pancreatic differentiation of human embryonic stem cells. Cell Stem Cell. 2013;12(2):224–237. doi: 10.1016/j.stem.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pan G, et al. Whole-genome analysis of histone H3 Lysine 4 and lysine 27 methylation in human embryonic stem cells. Cell Stem Cell. 2007;1(3):299–312. doi: 10.1016/j.stem.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Bernstein BE, et al. A bivalent chromatin structure marks key developmental genes in embryonic stem cells. Cell. 2006;125(2):315–326. doi: 10.1016/j.cell.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 33.Zhou Q, et al. In vivo reprogramming of adult pancreatic exocrine cells to β-cells. Nature. 2008;455(7213):627–632. doi: 10.1038/nature07314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao T, et al. Pdx1 maintains β cell identity and function by repressing an α cell program. Cell Metab. 2014;19(2):259–271. doi: 10.1016/j.cmet.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wasserfall C, et al. Persistence of pancreatic insulin mRNA expression and proinsulin protein in type 1 diabetes pancreata. Cell Metab. 2017;26(3):568–575.e3. doi: 10.1016/j.cmet.2017.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olbrot M, et al. Identification of β-cell-specific insulin gene transcription factor RIPE3b1 as mammalian MafA. Proc Natl Acad Sci. 2002;99(10):6737–6742. doi: 10.1073/pnas.102168499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qiu W-L, et al. Deciphering pancreatic Islet β cell and α cell maturation pathways and characteristic features at the single-cell level. Cell Metab. 2017;25(5):1194–1205.e4. doi: 10.1016/j.cmet.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 38.Zhang C, et al. MafA is a key regulator of glucose-stimulated insulin secretion. Mol Cell Biol. 2005;25(12):4969–4976. doi: 10.1128/MCB.25.12.4969-4976.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dai C, et al. Islet-enriched gene expression and glucose-induced insulin secretion in human and mouse islets. Diabetologia. 2012;55(3):707–718. doi: 10.1007/s00125-011-2369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verma SK, et al. Identification of potent, selective, cell-active inhibitors of the histone lysine methyltransferase EZH2. ACS Med Chem Lett. 2012;3(12):1091–1096. doi: 10.1021/ml3003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao F, et al. Triptolide alters histone H3K9 and H3K27 methylation state and induces G0/G1 arrest and caspase-dependent apoptosis in multiple myeloma in vitro. Toxicology. 2010;267(1):70–79. doi: 10.1016/j.tox.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 42.Yuan K, et al. Application and mechanisms of triptolide in the treatment of inflammatory diseases: a review. Front Pharmacol. 2019;10:1469. doi: 10.3389/fphar.2019.01469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gulati N, Béguelin W, Giulino-Roth L. Enhancer of zeste homolog 2 (EZH2) inhibitors. Leuk Lymphoma. 2018;59(7):1574–1585. doi: 10.1080/10428194.2018.1430795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cyphert HA, et al. Examining how the MAFB transcription factor affects Islet β-cell function postnatally. Diabetes. 2019;68(2):337–348. doi: 10.2337/db18-0903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cabrera O, et al. The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. Proc Natl Acad Sci U S A. 2006;103(7):2334–2339. doi: 10.1073/pnas.0510790103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baron M, et al. A single-cell transcriptomic map of the human and mouse pancreas reveals inter- and intra-cell population structure. Cell Syst. 2016;3(4):346–360.e4. doi: 10.1016/j.cels.2016.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tosti L, et al. Single-nucleus and in situ RNA–sequencing reveal cell topographies in the human pancreas. Gastroenterology. 2021;160(4):1330–1344. doi: 10.1053/j.gastro.2020.11.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Analysis of H3K9/14 acetylation content relative to total H3 shows no change following treatment with EZH2 inhibitors for 2- and 7-days.