Abstract
Patellofemoral pain and instability are common indications for imaging that are encountered in everyday practice. The authors comprehensively review key aspects of patellofemoral instability pertinent to radiologists that can be seen before the onset of osteoarthritis, highlighting the anatomy, clinical evaluation, diagnostic imaging, and treatment. Regarding the anatomy, the medial patellofemoral ligament (MPFL) is the primary static soft-tissue restraint to lateral patellar displacement and is commonly reconstructed surgically in patients with MPFL dysfunction and patellar instability. Osteoarticular abnormalities that predispose individuals to patellar instability include patellar malalignment, trochlear dysplasia, and tibial tubercle lateralization. Clinically, patients with patellar instability may be divided into two broad groups with imaging findings that sometimes overlap: patients with a history of overt patellar instability after a traumatic event (eg, dislocation, subluxation) and patients without such a history. In terms of imaging, radiography is generally the initial examination of choice, and MRI is the most common cross-sectional examination performed preoperatively. For all imaging techniques, there has been a proliferation of published radiologic measurement methods. The authors summarize the most common validated measurements for patellar malalignment, trochlear dysplasia, and tibial tubercle lateralization. Given that static imaging is inherently limited in the evaluation of patellar motion, dynamic imaging with US, CT, or MRI may be requested by some surgeons. The primary treatment strategy for patellofemoral pain is conservative. Surgical treatment options include MPFL reconstruction with or without osseous corrections such as trochleoplasty and tibial tubercle osteotomy. Postoperative complications evaluated at imaging include patellar fracture, graft failure, graft malposition, and medial patellar subluxation.
©RSNA, 2023
Quiz questions for this article are available in the supplemental material.
Introduction
The patella is widely known for three attributes: (a) It is the largest sesamoid bone in the body, (b) it normally has the thickest articular cartilage in the body, and (c) it is associated with pain and premature osteoarthritis when it does not track normally in the trochlear groove of the femur. These features of the patella are immutable, but our understanding of patellar disorders continues to evolve dramatically.
In the past century, some experts regarded the knee cap, or tibial sesamoid, as a morphologic remnant with no important function (1). Experts now believe that the patella evolved in mammals to help resist gravity by providing an enhanced lever system for lower extremity ambulation (2). Indeed, as an anatomic “pulley” that centralizes the divergent forces from the four quadriceps muscles, the patella markedly improves mechanical advantage and allows increased torque by at least 24% (3). The patella also functions as a “spacer” to protect the extensor tendons and dynamically dissipate patellofemoral forces that can be many times an individual’s body weight (eg, more than three times body weight during stair climbing, more than seven times body weight while squatting, more than 20 times body weight with jumping) (4).
Normal mobility of the patella is integral to its function. Although patellofemoral forces are substantial, normal patellar tracking occurs when there is an appropriate dynamic equilibrium between osteoarticular and soft-tissue structures. However, when anatomic structures are dysfunctional and there is a force imbalance, patellar maltracking may occur—often in association with a traumatic event or biomechanical overload that causes pain and decreased quality of life.
Patellofemoral pain is highly prevalent, affecting one in five individuals in the general population annually (5). Historically, more than 100 surgeries have been described for pain associated with patellar tracking abnormalities and patellar instability (6), and treatment decisions have been based on findings of static nonphysiologic imaging. However, like the patella itself, research on patellofemoral disorders has been “on the move.” Within the past 5 years, more than 570 articles on patellar instability have been listed in PubMed, with these scholarly works emphasizing new insights into patellofemoral anatomy, clinical assessment, diagnostic imaging, and specific treatments. However, as noted in a recent consensus statement from orthopedic subspecialty organizations, there is still a need for refinements in diagnostic imaging, including refinements in assessing the use of dynamic imaging for patellar instability (7).
In this article, we review key aspects of patellofemoral disorders that can occur before the onset of osteoarthritis and describe recently reported anatomic insights, highlights in clinical evaluation, evolving imaging techniques, and consensus standards of treatment.
Anatomy
Having knowledge of the patellofemoral anatomy is a fundamental first step to confidently distinguishing normal from abnormal imaging findings. In addition to evaluating relevant anatomic structures, analyzing the alignment of these structures may be helpful for understanding the clinical significance of imaging findings. Indeed, given that reconstruction of the patellofemoral anatomy and normalization of patellofemoral alignment are primary goals of surgical interventions, awareness of the osteoarticular and soft-tissue structures that provide stability is essential to image interpretation in the preoperative and postoperative settings.
Osteoarticular Structures
Key osseous structures that affect the patellofemoral alignment are the patella, trochlea, and tibial tubercle (Fig 1). The patella is tethered proximally by the quadriceps tendon and distally by the patellar tendon. Posteriorly, the patella articulates with the trochlea, a sulcus in the distal femur, forming the patellofemoral articulation. Distally, the tibial tubercle serves as the insertion site for the patellar tendon; therefore, the location of this tubercle can influence patellar alignment. Patella alta, trochlear dysplasia, and lateralization of the tibial tubercle are important risk factors for patellar maltracking and instability. Other risk factors include genu valgum and rotational malalignment in the lower extremity.
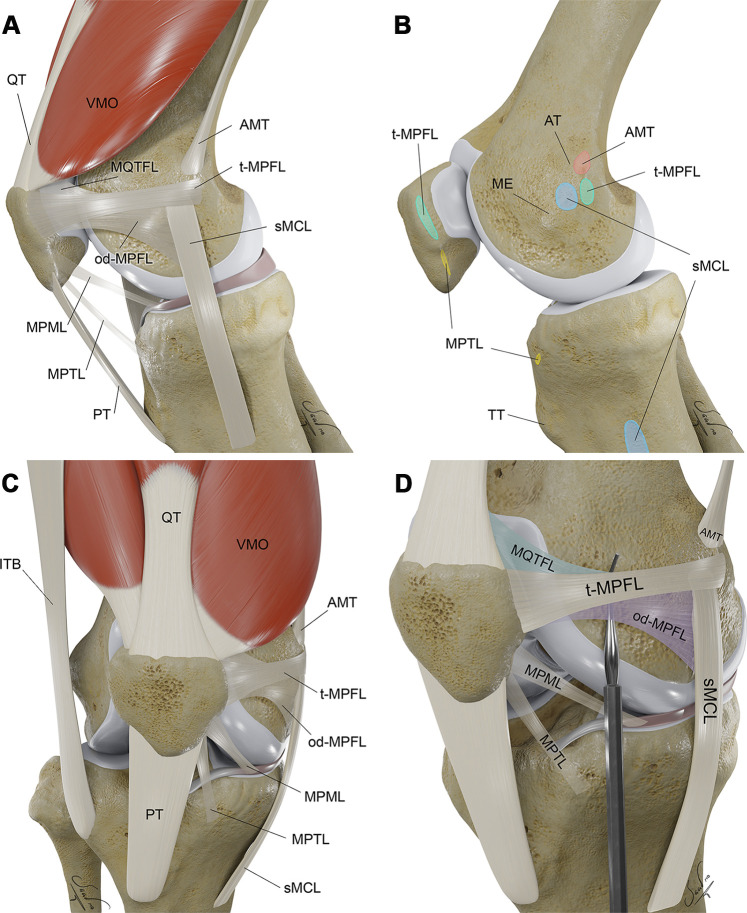
Figure 1.
Three-dimensional (3D) illustrations show key osseous and soft-tissue structures of extensor mechanism in the lateral (A, B), anterior (C), and external oblique (D) perspectives, with respective osseous attachment areas. Structures of the medial patellofemoral ligament (MPFL) complex are exaggerated by the probe (in D). AMT = adductor magnus tendon, AT = adductor tubercle, ITB = iliotibial band, ME = medial epicondyle, od-MPFL = MPFL with oblique decussation component, t-MPFL = MPFL with transverse oblique decussation component, MPML = medial patellomeniscal ligament, MPTL = medial patellotibial ligament, MQTFL = medial quadriceps tendon femoral ligament, PT = patellar tendon, QT = quadriceps tendon, sMCL = superficial medial collateral ligament, TT = tibial tubercle, VMO = vastus medialis obliquus muscle.
During childhood, the shape of the patella and trochlea change concurrently, suggesting a dynamic interplay between these two structures during development (8). More than two-thirds of primary patellar dislocations occur in individuals between the ages of 10 and 19 years, and these dislocations particularly affect females, who tend to have a shallower trochlear groove with a wider sulcus angle (9).
Soft-Tissue Structures
In addition to the quadriceps and patellar tendons, several other soft-tissue retinacular structures influence patellar motion relative to the trochlea. The term retinaculum (Latin, meaning “to retain”) refers to fibrous bands or ligaments that help hold a structure, such as the patella, in appropriate alignment.
Medial and lateral retinacular structures are increasingly being recognized as a complex of patellar restraints with extensions both proximal and distal to the knee joint line. The medial patellar retinacular structures, also referred to as the medial patellofemoral ligament (MPFL) complex, function to limit lateral patellar translation (10). Recent anatomic literature and our imaging experience indicate that there is variability in the size and visibility of the individual structures of the MPFL complex, as well as some diversity in specific osseous and soft-tissue attachment sites. Anatomic descriptions also may vary with various knee positions and dissection methods (eg, outside-in vs inside-out) (11).
The most important component of the MPFL complex is the MPFL, although there is increasing interest in three secondary medial stabilizers: the medial quadriceps tendon femoral ligament (MQTFL), medial patellomeniscal ligament (MPML), and medial patellotibial ligament (MPTL). In our experience, secondary stabilizers are inconsistently visualized with diagnostic imaging (12), and there is a paucity of original MRI research beyond cadaveric investigations (13). We find that knowledge of these secondary stabilizers is particularly helpful when interpreting MRI findings after these stabilizers have been reconstructed.
Proximal Medial Patellar Restraints: MPFL and MQTFL.—The MPFL is the primary static soft-tissue restraint to lateral patellar displacement and is commonly reconstructed surgically in patients with MPFL dysfunction and patellar instability. The MPFL is generally described as a horizontally oriented, ribbonlike ligament that spans from the medial patella (proximal two-thirds) to the adjacent medial femur (most commonly near the physeal scar, at a sulcus between the medial femoral epicondyle and the adductor tubercle) (Fig 2) (13–16). On a true lateral radiograph, the midpoint of the MPFL femoral attachment is termed the Schöttle point and is an important landmark for determining the correct femoral tunnel position for MPFL reconstruction (Fig 3). This landmark is relevant for radiologists interpreting postoperative imaging findings because femoral tunnel malposition (>10 mm from the Schöttle point) results in worse patient-reported outcomes, including higher rates of recurrent patellar dislocation (17).
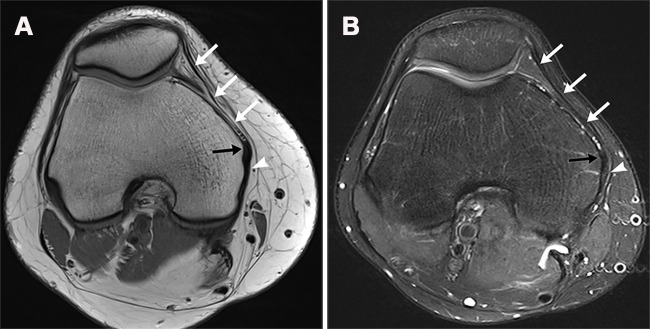
Figure 2.
MPFL. Axial proton-density–weighted (A) and T2-weighted fat-suppressed (B) MR images show a normal MPFL (white arrows). The MPFL is a horizontally oriented ribbonlike ligament that spans from the medial patella to the adjacent medial femur. The MPFL merges with the fibers of the medial collateral ligament (black arrow) at the epicondyle and inserts immediately posterior onto the femur (arrowhead).
Figure 3.
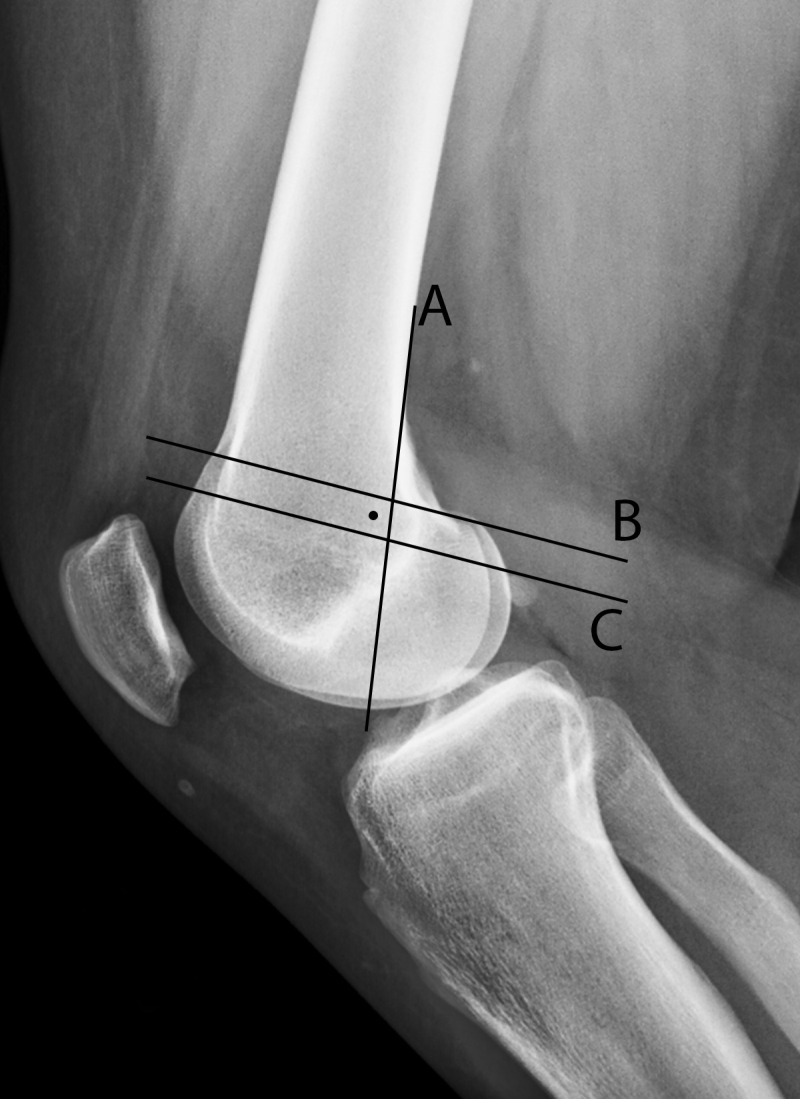
Radiographic landmarks for MPFL reconstruction. The Schöttle point (dot) is the midpoint of the MPFL attachment on the femur and the target for MPFL reconstruction tunnel placement (16). Lateral radiograph shows that the Schöttle point is 1 mm anterior to the posterior cortex extension line (A), distal to a line drawn between the anterior and posterior origins of the medial femoral condyle (B), and proximal to the level of the posterior point of the Blumensaat line (C).
In addition to the main horizontally oriented transverse component of the MPFL, an additional “oblique decussation component” of the MPFL, which attaches to the proximal fibers of the superficial medial collateral ligament, has been described in recent studies (18,19). As a consequence of this intimate anatomic decussation, MRI shows abnormal edema signal intensity with most medial collateral ligament injuries, even though the patients do not have a clinically relevant MPFL injury (19).
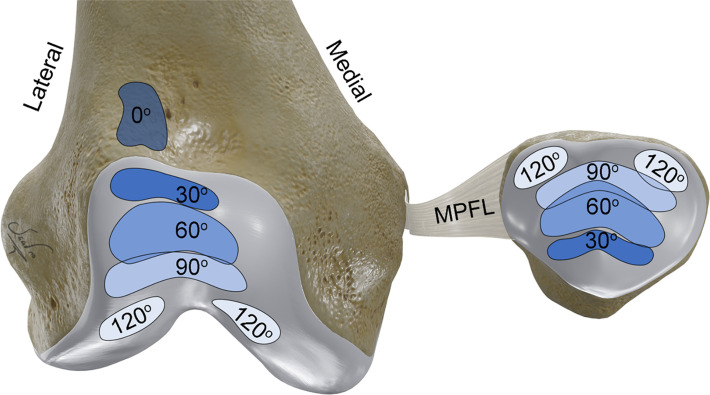
Proximal to the MPFL and patella, oblique ligament fibers extending to insert into the distal quadriceps, termed the MQTFL, have been described in recent studies. While the MPFL is primarily responsible for resisting lateral patellar translation from 0° to 90° of knee flexion, the MQTFL may contribute to stability, particularly in full extension (20). Surgical techniques may now be used to reconstruct the MPFL, the MQTFL, or both of these proximal medial patellar restraints (21–23).
Distal Medial Patellar Restraints: MPML and MPTL.—The MPML and MPTL extend from the inferomedial patella to the medial meniscus and anteromedial tibia, respectively (Fig S1) (24,25). Although the MPML and MPTL are considered secondary stabilizers, the contributions of these distal medial patellar restraints against lateral patellar translation, tilt, and rotation in some positions (up to 48%, 71%, and 92%, respectively, during knee flexion) can be substantial (26). As a result, MPFL reconstructions now may be combined with MPTL reconstruction in some patients with patellar instability (27).
Lateral Retinacular Structures.—The lateral patellofemoral ligament complex, like its medial counterpart, has both osseous and soft-tissue attachments (28). The primary component of the lateral patellofemoral complex is the lateral patellofemoral ligament that extends from the lateral patella and adjacent patellar tendon to the femur (distal-anterior to the lateral femoral epicondyle). Smaller-caliber secondary stabilizers spanning from the inferolateral patella to the lateral meniscus anterior horn (lateral patellomeniscal ligament) and the adjacent tibia near the Gerdy tubercle (lateral patellotibial ligament) also have been described (28).
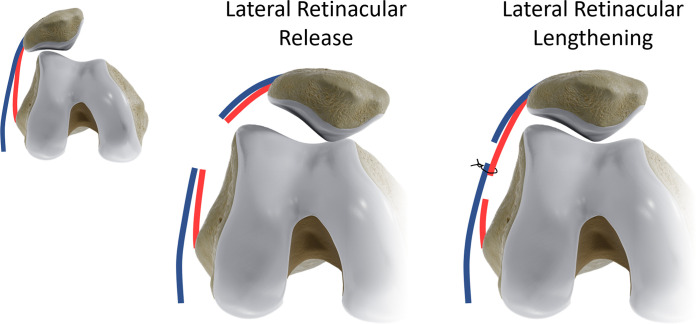
It is important to note that the lateral patellofemoral complex can play a key role in both lateral and medial patellar displacement (29). Although lateral retinacular structures are occasionally injured in the setting of trauma, these structures most commonly are clinically relevant when they are associated with fibrosis (decreased elasticity) or iatrogenic injury (eg, after aggressive lateral retinacular release or surgical overcorrection in patients with lateral patellar instability) (29). Medial patellar displacement and instability are rare in the absence of iatrogenic injury (30). Indeed, because of concern for iatrogenic medial patellar instability, many surgeons now address tight lateral retinacular tissues with a controlled retinacular “lengthening” rather than a traditional lateral “release” procedure (31). There is now a general consensus among patellofemoral surgeons that an isolated lateral release procedure is never appropriate for the treatment of patellar instability (7).
Clinical Evaluation
Anterior knee pain has an extensive differential diagnosis (32) that includes acute and chronic disorders of the articular cartilage, extensor tendons, adjacent soft tissues (eg, infrapatellar fat pad), and patella tracking. Patients with patellofemoral pain related to patellar malalignment are more commonly female and tend to present with this pain in their second and third decades of life. In general, patients with patellar malalignment can be divided into two broad groups with distinct kinematic profiles and sometimes different imaging findings: patients with a history of overt patellar instability after a traumatic event (eg, dislocation, subluxation) and patients without such a history (33).
Patellar Dislocation
Patient History.—Patellar dislocations occur most commonly during quadriceps muscle contraction when a valgus force is applied to a nearly extended knee while the foot is fixed on the ground and the tibia is externally rotated (34). Although such noncontact “twisting” injuries are most frequent, a direct blow to the knee or deeper knee flexion also may be associated with patellar dislocation.
Patients commonly describe having pain acutely, with the knee giving way, a “pop,” and often spontaneous reduction of the dislocated patella. They also may describe a sensation of the kneecap feeling unstable. Frank patellar dislocation, especially when there are recurrent episodes, is generally much easier to diagnose clinically than subtle intermittent subluxation.
Physical Examination.—In the acute setting, a transient lateral patellar dislocation event may be confused clinically with cruciate or collateral ligament injuries, especially anterior cruciate ligament rupture. Patients with these types of injuries may have nonspecific hemarthrosis, soft-tissue swelling, arthrogenic muscle inhibition (degraded quadriceps muscle contraction) (35), and guarding during physical examination maneuvers. In the nonacute setting, clinical evaluation for localized tenderness, patellar malalignment, and patellar instability is generally easier and may be more similar to clinical evaluation of patients who have a history of chronic patellar maltracking without a history of dislocation.
Patellar Maltracking
Patient History.—Patellar maltracking may be defined as dynamic malalignment of the patella relative to the trochlear groove during knee motion. Although patellar maltracking can certainly occur in patients after a dislocation event, recent research highlights the finding that atraumatic patellofemoral pain (sometimes referred to as patellofemoral pain syndrome) can have a distinct kinematic profile during active quadriceps muscle contraction (33). Affected patients often report having pain behind the patella that is aggravated by activities that involve weight bearing on a flexed knee, such as that during squatting (sensitivity, 92%) (Movie 1) (36).
Movie 1:
Patellar motion, both normal and abnormal, can be evaluated during physical examination with squatting. Dynamic imaging techniques strive to replicate patellar motion during physiologic stress, such as during knee extension-flexion or quadriceps contraction.
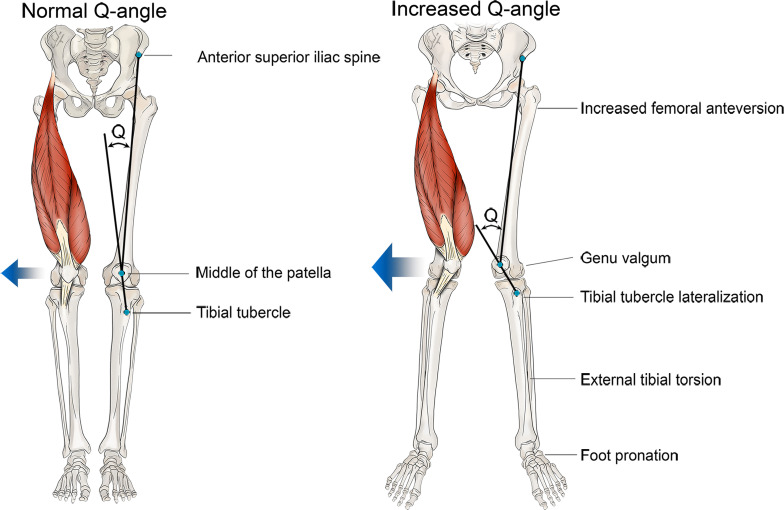
Physical Examination.—Alignment and tracking of the patella can be analyzed at physical examination, as well as during diagnostic imaging. Overall alignment of the lower extremity in the coronal plane is commonly assessed by using the quadriceps, or Q, angle. The Q angle helps quantify tibial tubercle lateralization on the basis of the relationships of the tibial tubercle with the patella and the anterior superior iliac spine (Fig 4). A larger Q angle and genu valgum are associated with an increased lateral quadriceps vector that promotes lateral patellar maltracking and are risk factors for lateral patellar dislocation and patellofemoral osteoarthritis (37).
Figure 4.
Quadriceps angle, or Q angle. This angle is formed by the intersection of lines drawn from the anterior superior iliac spine to the center of the patella, and from the center of the patella to the tibial tubercle. An increased Q angle is associated with an increased magnitude of laterally directed forces on the patella (blue arrows) and thus increases the risk of lateral patellar maltracking and dislocation. Femoral anteversion, genu valgum, tibial tubercle lateralization, external tibial torsion, and foot pronation can contribute to an increased Q angle.
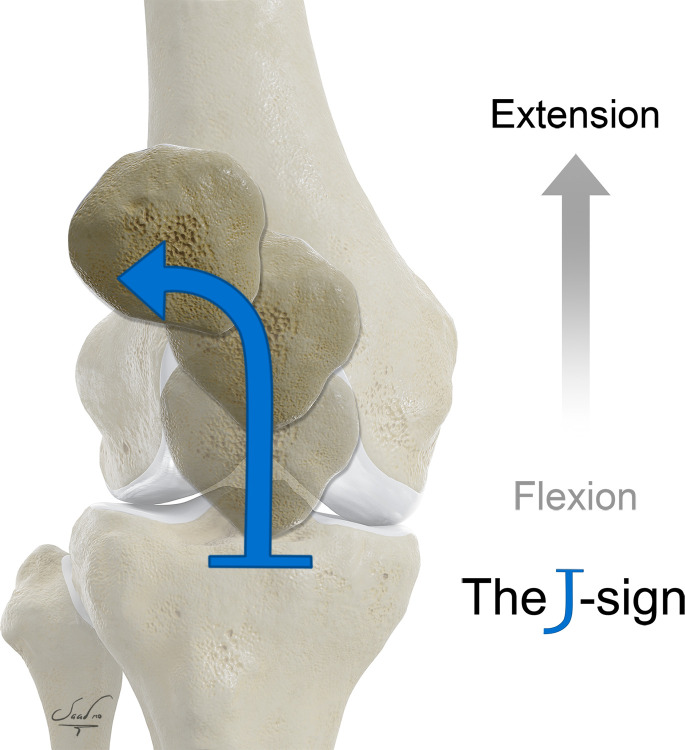
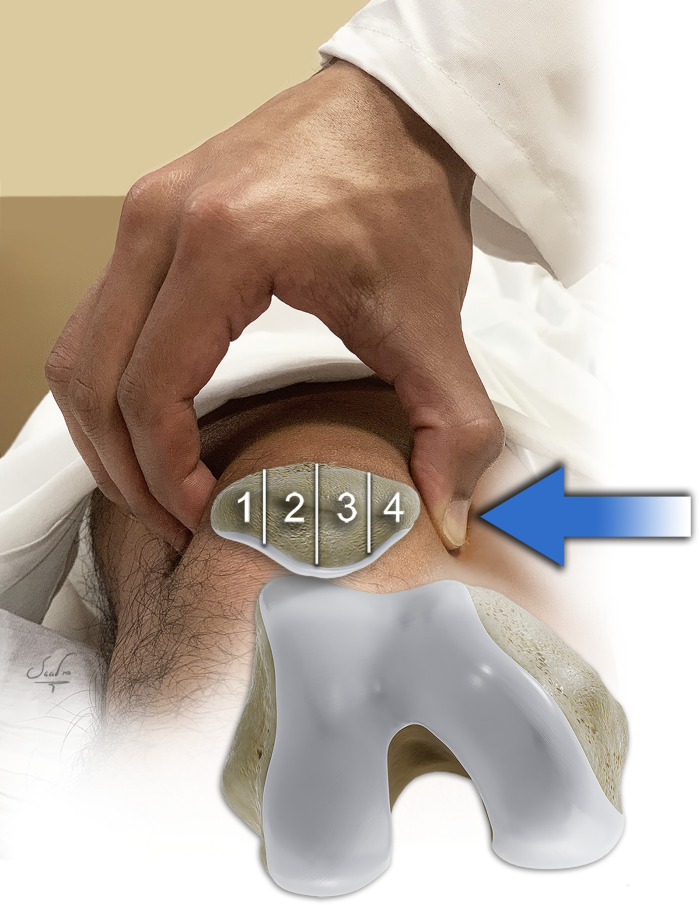
Patellar maltracking can be diagnosed during quadriceps muscle contraction with physical examination, or with dynamic imaging, when a positive “J” sign (ie, lateral deviation of the patella defined as two or more quadrants during terminal knee extension) is present (Fig 5) (38,39). Although the J sign is one of the most common physical examination techniques used to diagnose patellar maltracking, the inter- and intraobserver reliability of this sign is poor, even among subspecialty patellofemoral experts, which reinforces the importance of objective measurements with imaging (eg, four-dimensional CT) (37). Other classic diagnostic maneuvers include the patellar glide test (assessment of hyperlaxity, a risk factor of patellar instability) (Fig 6), the patellar apprehension test (subjective evaluation for patient apprehension and/or sensation of instability while the examiner displaces the patella laterally), and the medial patellar tilt test (assessment of lateral retinacular tightness and reducibility of lateral patellar tilt) (7,39).
Figure 5.
The J sign. This sign is a clinical finding that is indicative of patellar maltracking and is associated with patellofemoral pain syndrome. The J sign refers to an abnormal inverted J path that the patella takes with active knee extension from flexion in patients with patellar hypermobility.
Figure 6.
Patellar glide test. This test is used to evaluate passive patellar mobility, with the knee in full extension and in 30° flexion caused by the examiner pushing the patella medially and laterally. The examiner can palpate the projecting posterior surface of the patella and estimate the degree of patellar movement. The mobility is expressed in numbers of patellar quadrants (1–4) displaced from the starting position.
Imaging Evaluation
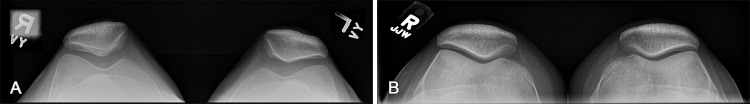
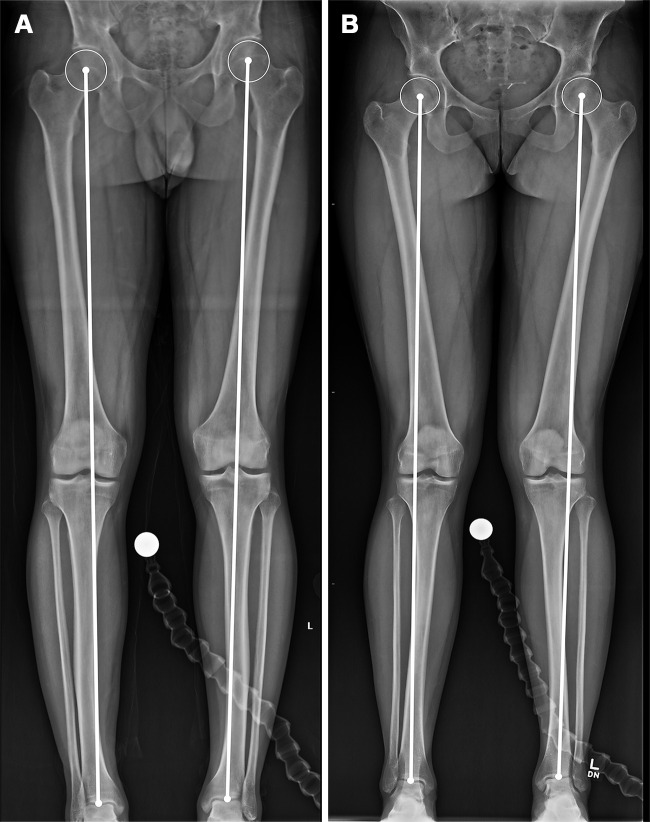
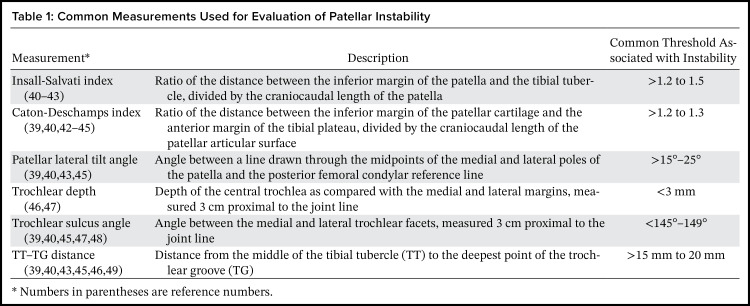
For patients with a first-time patellar dislocation, the initial management generally includes imaging evaluation with knee radiography (eg, with lateral, bilateral Merchant, and bilateral anteroposterior weight-bearing hip-to-ankle views) (Figs 7, 8) and MRI. With both radiography and MRI, images are evaluated most importantly for intra-articular osteochondral fragments, as well as for patellofemoral alignment, including patellar height, patellar position and tilt, trochlear morphology, and tibial tubercle lateralization (Table 1 [39–49], Figs S2–S8). The detection of intra-articular osteochondral fragments, if present, is particularly important as an indication for surgical intervention (7,31,39). Lower extremity imaging to assess for genu valgum and rotational malalignment (particularly excessive femoral anteversion and excessive external tibial rotation) also may be important in influencing management.
Figure 7.
Imaging evaluation of patellar dislocation. (A) Merchant-view radiographs, which are obtained with the patient supine, the knee flexed to 45° at the table edge, and the tube angled downward 30°, typically with both knees in the field of view, enable evaluation of patellar alignment and symmetry. (B) Sunrise-view radiographs may be obtained with the patient prone (shown here) or supine, but for prone radiographs, they are obtained with the knee flexed to 115° and the tube angle 15° cephalad. The sunrise view is not as sensitive for assessment of patellar maltracking, but it allows better visualization of the inferior patellofemoral joint.
Figure 8.
Evaluation of the mechanical axis on radiographs in a 27-year-old man with a normal mechanical axis (A) and a 31-year-old woman with bilateral genu valgum (B). The mechanical axis is evaluated on standing full-length lower extremity radiographs. A line is drawn from the center of the femoral head to the center of the talar dome. A normal mechanical axis is defined by a line passing through the knee between the medial and lateral margins of the tibial spine.
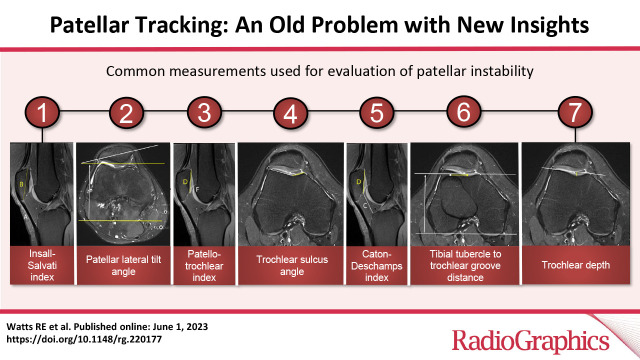
Table 1:
Common Measurements Used for Evaluation of Patellar Instability
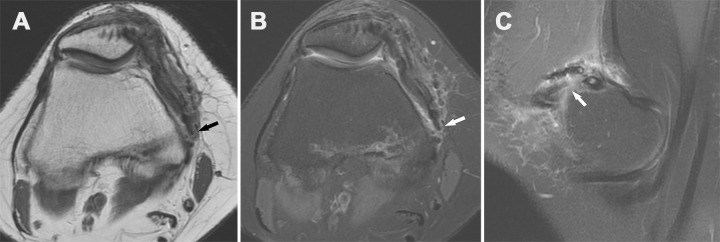
After a lateral patellar dislocation, MRI commonly shows additional characteristic injuries to osteoarticular structures and adjacent soft tissues. Typical osteoarticular derangements include bone contusions and osteochondral fractures, often at the patella (medial aspect) and lateral femoral condyle (anterolateral aspect) (Figs 9, 10, S9), as well as intra-articular osteochondral bodies and joint effusion in the acute setting (Fig 11). The most salient soft-tissue injury to detect is rupture of the MPFL. Normally, the MPFL and other patellar retinacular structures (eg, the MPML) are most conspicuous on proton-density–weighted MR images, on which they are seen as thin low–signal-intensity structures (Movie 2). However, when injured, these retinacular structures are seen with increased signal intensity, disrupting the normal ligament morphology, and with low signal intensity on fat-suppressed fluid-sensitive MR images (Fig 12). The MPFL is injured in almost all (~95%) patellar dislocations, although the location of the injury is variable (37% at the patellar attachment, 37% at the femoral attachment, 16% midsubstance, and the remainder at a combination of sites) (50). Patient age affects the site of MPFL injuries, with femoral attachment injuries relatively more common (in 47% of cases) in patients older than 16 years (50).
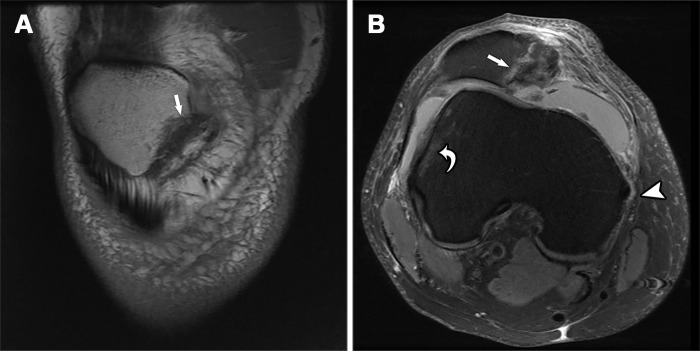
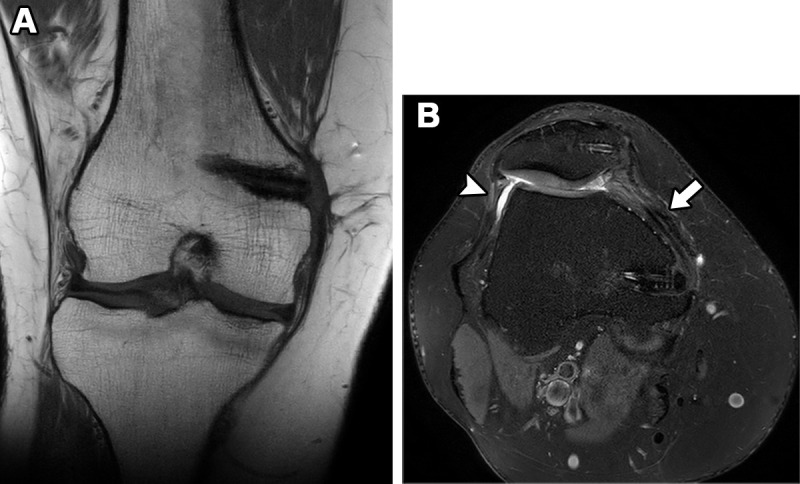
Figure 9.
Recurrent patellar dislocation in a 34-year-old man after a fall while walking. Coronal T1-weighted (A) and axial proton-density–weighted fat-suppressed (B) MR images show an inferomedial patellar fracture (straight arrow) associated with bone marrow edema-like signal intensity. An MPFL tear (arrowhead in B) at the femoral attachment and a characteristic bone contusion (curved arrow in B) at the lateral aspect of the lateral femoral condyle also are present.
Figure 10.
Recurrent patellar dislocation in a 34-year-old man after a fall. Coronal T1-weighted (A) and proton-density–weighted fat-suppressed (B) MR images show bone marrow edema-like signal intensity associated with an impaction fracture (arrow) of the lateral femoral condyle.
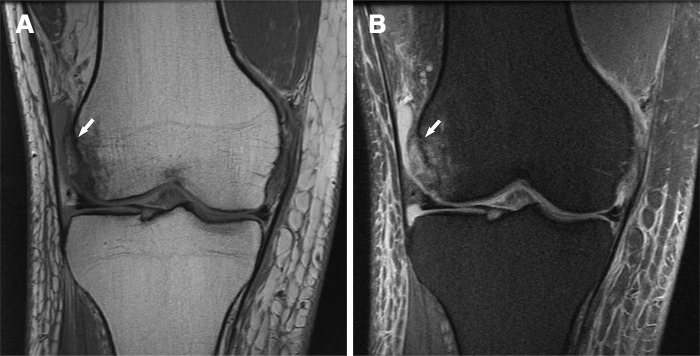
Figure 11.
Osteochondral injury of the inferior medial aspect of the patella in a 19-year-old woman after an acute patellar dislocation. (A) Axial proton-density–weighted fat-suppressed MR image shows tearing of the MPFL at the patellar and femoral attachments (arrowheads). An additional sheared intra-articular osteochondral fragment composed of a slab of articular cartilage (black arrow) and a sliver of subchondral bone plate (white arrow) is seen. (B) The presence of an osseous component makes the fragment (arrow) visible on a sunrise-view radiograph.
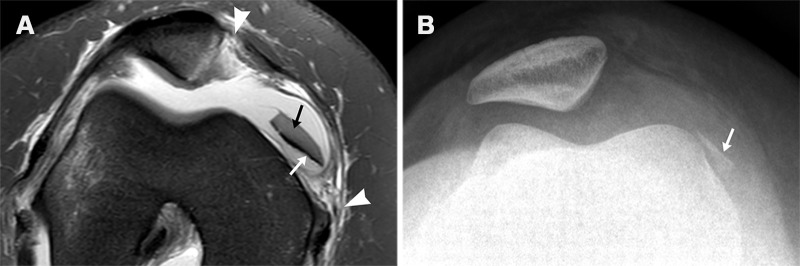
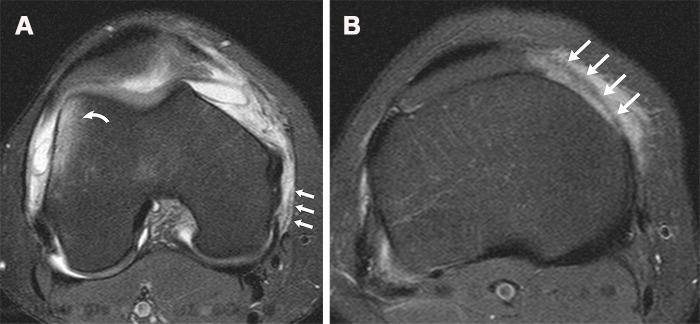
Figure 12.
Acute lateral patellar dislocation in a 20-year-old woman. (A) Axial T2-weighted fat-suppressed MR image shows tearing of the posterior fibers of the MPFL (straight arrows) and a characteristic bone contusion (curved arrow) at the lateral aspect of the lateral femoral condyle. (B) Axial T2-weighted fat-suppressed MR image obtained further distally shows tearing of the MPML and MPTL (arrows).
Movie 2.
MPML seen at MRI. Coronal and sagittal proton-density–weighted MR images demonstrate the MPML extending from the inferomedial aspect of the patella to the medial meniscus anterior horn.
Imaging enables both qualitative and quantitative evaluation of patellofemoral disorders. While qualitative assessment is generally the foundation for diagnostic imaging interpretations, quantitative imaging may help in objectively describing the severity of a derangement to improve documentation, clarify communication, and monitor therapy response. Given that manual measurements require significantly more time than qualitative interpretations, algorithms to automate measurements and populate structured reports are being used (51). As with any qualitative or quantitative imaging evaluation that influences treatment, the clinical context is crucial.
Radiologic measurements related to patellar maltracking have proliferated for many decades, with methodologic variability across the literature encumbering physician understanding, communication, reliability, and efficiency. For example, in a relatively recent systematic review (40), 106 unique measurements were evaluated and included 11 measurements of patellar height, 38 measurements of trochlear morphology, and 39 measurements of patellar tracking.
The spirited debate regarding patellofemoral measurement methodologies and normal values is not settled here. Rather, this section highlights recent observations in the literature to consider for general guidance when discussing this controversial area. To that end, we cite systematic reviews that summarize hallmarks of interreader reliability and diagnostic validity. These evidence-based findings have influenced our imaging evaluations of patellar malalignment, trochlear dysplasia, tibial tubercle lateralization, and rotational deformity.
Patellar Malalignment
Patella Alta.—With both radiography and MRI, two patellar height metrics have consistently demonstrated moderate to good interreader reliability: the Insall-Salvati index and the Caton-Deschamps index (Fig 13) (44,46,52). The Insall-Salvati index may demonstrate superior reproducibility compared with the Caton-Deschamps index (40,46). Both of these indexes (41,42) have been validated in children and adults. The Insall-Salvati index may be spuriously affected by morphologic variations in the patella and tibial tubercle (eg, due to developmental osseous prominence, traction apophysitis, or history of trauma). The Caton-Deschamps index is artifactually low when it is measured with the knee in hyperextension.
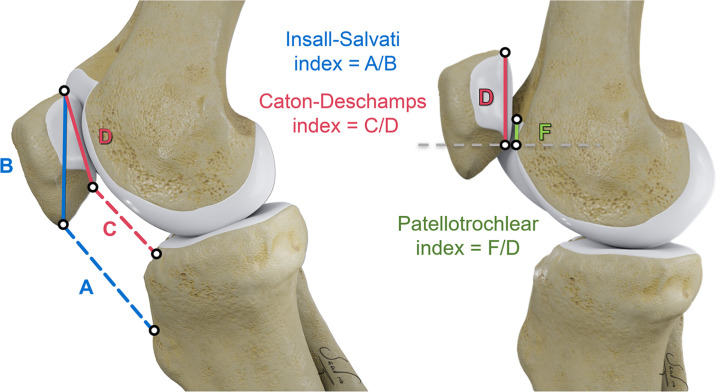
Figure 13.
Measurements for patellar height. The patellar tendon length at its inner aspect (A), greatest diagonal length of the patella (B), distance between the inferior margin of the patellar articular surface and anterior lip of the tibial plateau (C), greatest length of the patellar articular surface (D), and length of trochlear cartilage overlapping the patella (F) are depicted.
The Insall-Salvati and Caton-Deschamps indexes are frequently reported by using radiography and MRI (40), although recent works suggest that the Insall-Salvati index has better reliability and agreement with use of these two modalities (42). Furthermore, with both radiography and MRI, these two patellar height indexes demonstrate statistically significant discrimination validity (defined as the ability of a metric to distinguish patients with versus those without a history of patellar instability) (47,52).
Although patellar height indexes were initially applied to radiographs showing variable knee flexion, the use of MRI with the knee consistently positioned in nearly full extension has gained greater acceptance. This is, in part, because instability events tend to occur at nearly full extension, and MRI studies have demonstrated increased patellar height in patients with patellar maltracking, as compared with in control subjects (43).
On MR images, the patellotrochlear index (PTI) is increasingly being used as a measure of patellar height based on true patellotrochlear cartilage congruence. The PTI, defined as the ratio of the length of trochlear cartilage overlapping the patella to the length of patellar cartilage on a midsagittal MR image, has good interreader and intrareader reliability at MRI (Fig 13) (42,53).
All three of these patellar height metrics (Insall-Salvati index, Caton-Deschamps index, and PTI) vary substantially with variations in knee extension and flexion (Fig 14). Indeed, the Insall-Salvati and Caton-Deschamps indexes tend to have substantially increased values with knee extension (43,52). Patellotrochlear cartilage overlap also increases with knee flexion (Fig 15), but any measurement of the PTI obtained with the knee in flexion can be corrected to 0° of flexion by using a simple mathematical formula: PTIc = PTIm− (1.3 × FAk) (53), where PTIc is the corrected PTI, PTIm is the measured PTI, and FAk is the knee flexion angle.
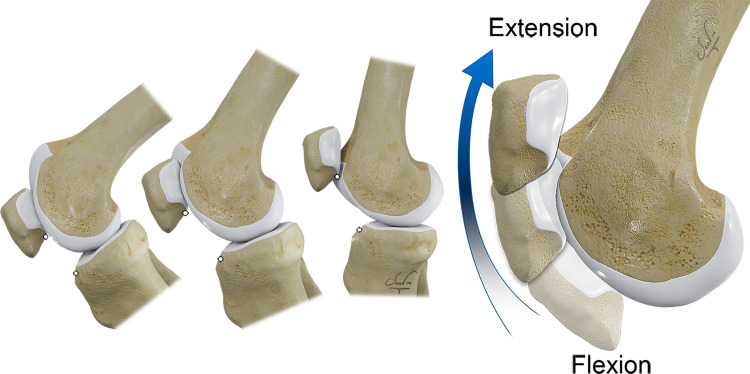
Figure 14.
Normal patellofemoral kinematics. As the knee flexes and extends, the patella tilts, rotates, and shifts with respect to the trochlea, incorporating six degrees of freedom of patellar movement. Measurements of patellar height vary at different degrees of knee flexion and can confound evaluation of the patella alta. Standard lateral radiographs used to define the normal range of patellar height are obtained at 30° of flexion. Standard CT and MR images are obtained with the knee in extension; therefore, the patella is normally positioned more proximally relative to the trochlea.
Figure 15.
Patellofemoral contact areas. Normal contact areas between the patella and femoral trochlea vary at different angles of knee flexion. This results in variable contact force at the patellofemoral articulation in different degrees of flexion. In general, the contact pressure increases with increasing flexion angle degree.
On MR images, the thresholds for diagnosing patella alta vary, with surgical correction considered more seriously when values are substantially beyond the reported cutoff points (eg, >1.2 to 1.5 for the Insall-Salvati index, >1.2 to 1.3 for the Caton-Deschamps index, <13% to 28% for the PTI) (43). When patients who have patellar instability are compared with control subjects, there is a difference in mean MRI Insall-Salvati index values (1.3 [95% CI: 1.21, 1.41] vs 1.1 [95% CI: 1.05, 1.23], respectively) and mean Caton-Deschamps index values (1.2 [95% CI: 1.05, 1.26] vs 1.0 [95% CI: 0.90, 1.14], respectively) (40).
Patellar Tilt and Translation.—With imaging in the axial plane, there are at least 11 distinct methods for measuring lateral patellar tilt and at least 22 methods for measuring lateral patellar translation relative to the femur (33). Although distinct methods for measuring maltracking continue to emerge and may have merit, standardized metrics that are simple and practical are valued in daily clinical practice.
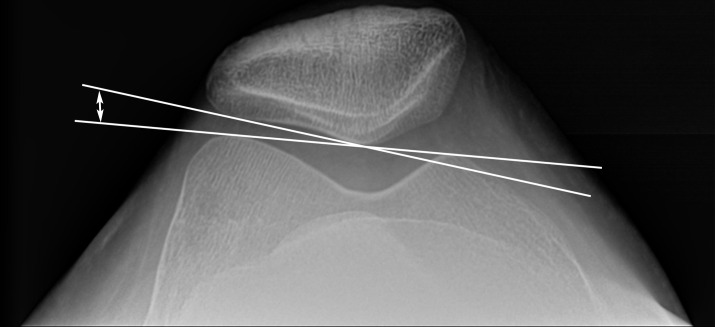
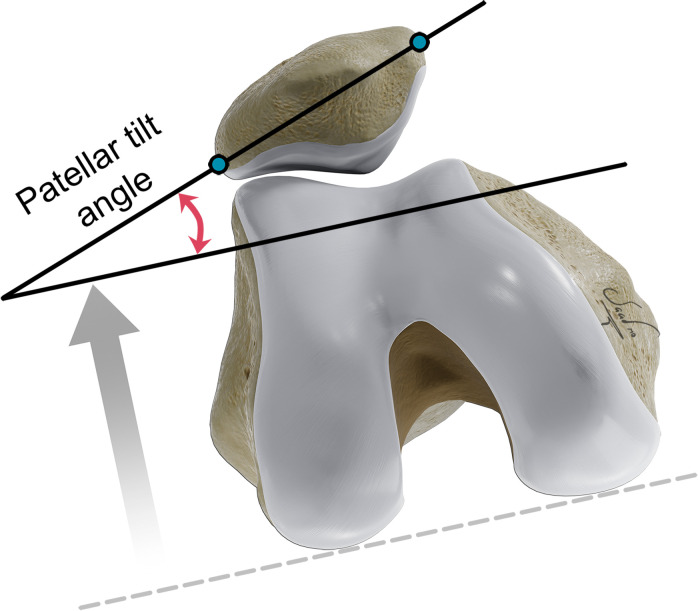
The techniques for measuring the patellar position on axial radiographs are often different from those used to measure this position on axial CT and MR images, because axial radiographs do not show the posterior aspect of the femoral condyles. To measure patellar tilt on axial radiographs, the lateral patellofemoral angle is constructed with one line drawn along the lateral patellar facet and a second line drawn to determine the trochlear axis (from the medial to lateral margins of the trochlea) (Fig 16) (40,47). To measure patellar tilt on axial CT and MR images, we use the patellar tilt angle (Fig 17), which is defined by the line crossing the maximal width of the patella (on a midpatellar image) and the bicondylar line tangent to the femoral posterior condyles (on an image showing the greatest posterior extent of the femoral condyles).
Figure 16.
Lateral patellofemoral angle. The lateral patellofemoral angle (double-headed arrow) is measured between the line drawn along the lateral patellar facet and the line from the medial to lateral margins of the trochlea.
Figure 17.
Patellar tilt angle. The patellar tilt angle is measured between the line through the medial and lateral patella at the greatest patellar width (blue dots) and a line parallel to the reference line tangent to the posterior borders of the femoral condyles (dashed line).
For lateral patellar displacement, the medial-lateral distance is measured from the deepest portion of the trochlear groove to the patellar median ridge (parallel to the trochlear axis line on an axial radiograph or to the bicondylar line at cross-sectional imaging) (Fig S10) (33,54).
Trochlear Dysplasia
Trochlear dysplasia is defined as an abnormal shape of the trochlea, which is often seen as a shallow or short groove. Although the classification system of Dejour (45), involving the use of lateral radiographs, has been described extensively in publications, it has not been proven to be reliable (47,55).
With MRI, three quantitative measures of trochlear dysplasia have generally good inter- and intrareader reliability and discrimination validity: trochlear depth, sulcus angle, and lateral trochlear inclination (46). In addition, an easy-to-use MRI grading system can be used to qualitatively classify the proximal trochlea as normal, slightly shallow (mild dysplasia), flat (moderate dysplasia), or convex (severe dysplasia). This grading system is used to guide management and has excellent inter- and intrareader reliability (48).
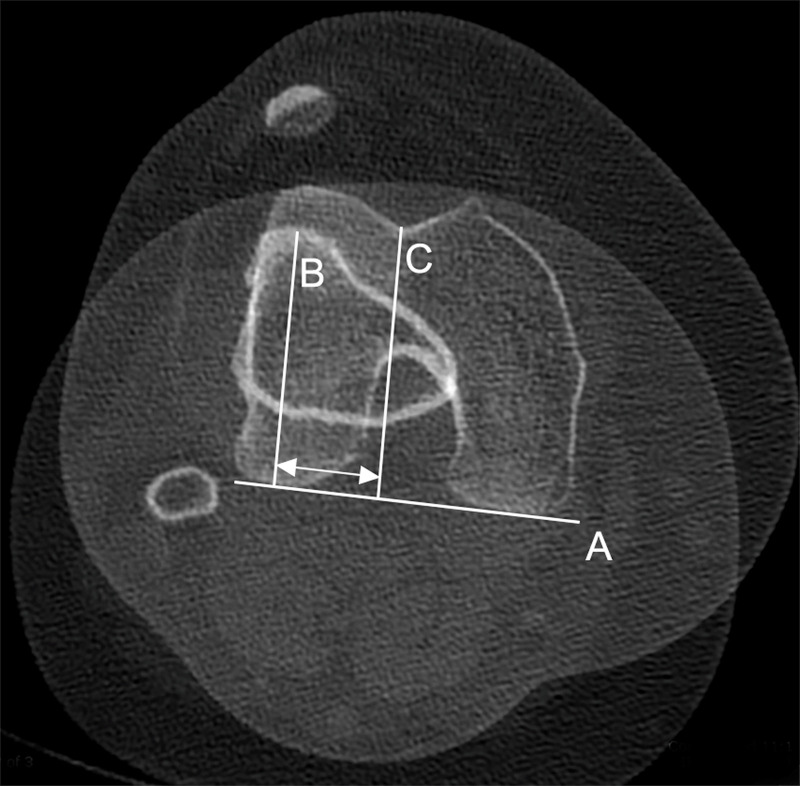
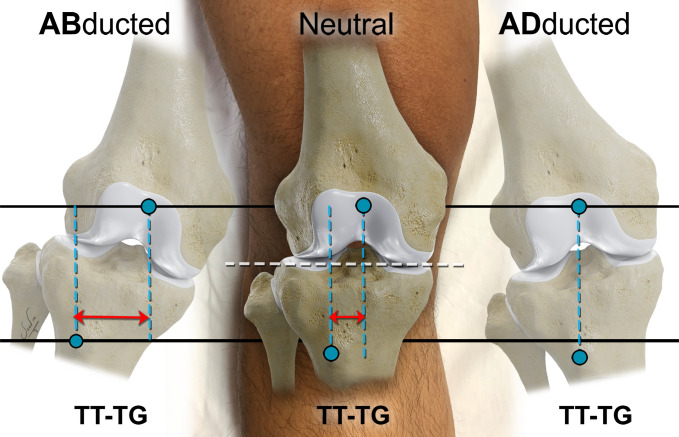
Tibial Tubercle Lateralization
Excessive lateralization of the tibial tubercle contributes to a lateral vector force on the patella and is a risk factor for patellar maltracking. To quantify the amount of tibial tubercle lateralization, two metrics are reliable: the medial-lateral distance from the tibial tubercle to the trochlear groove (TT-TG) (Fig 18, Movie 3) and the medial-lateral distance from the tibial tubercle to the posterior cruciate ligament (TT–PCL) (40,46,47). For TT-TG and TT-PCL metrics, abnormal values (>20 mm and >21–24 mm, respectively) as a potential indication for surgical correction have been reported (40).
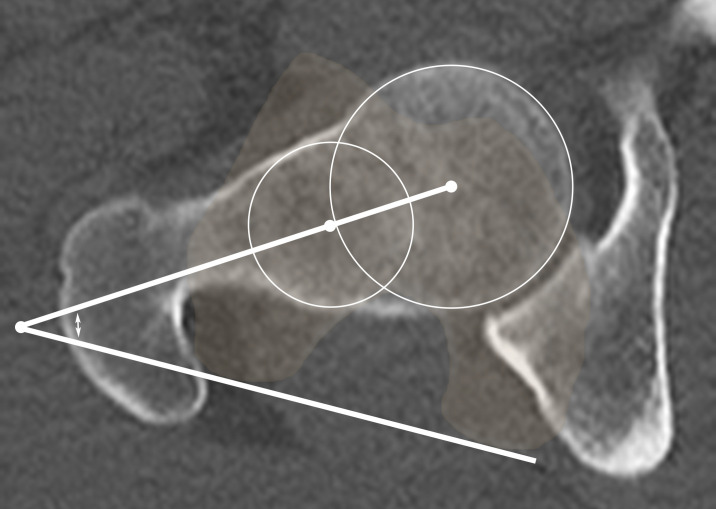
Figure 18.
Measurement of tibial tubercle lateralization. Postreconstruction analysis can be used to make a more accurate determination of the TT-TG (arrows). Superimposing an axial CT section through the tibial tubercle (B) on top of a section at the posterior femoral condylar reference line (A) and the deepest point of the trochlear groove (C) allows a more reliable calculation of the TT-TG.
Movie 3.
Practical TT-TG measurement obtained on an axial CT image. In most cases, the TT-TG can be measured without the assistance of additional reconstructions on a true axial image. This video shows the steps in creating the reference line, identifying the midpoint of the tibial tubercle, and then drawing the TT-TG.
The TT-TG is the most commonly reported metric (40) and is often considered to be superior to the TT-PCL measurement for differentiating patients with patellofemoral instability from their stable counterparts (49). In fact, recent research (56) has questioned the prevailing dogma that the TT-PCL metric reflects true lateralization of the tibial tubercle, independent of femoral rotation and knee flexion.
Similar to other metrics, the TT-TG can be influenced by several factors, including imaging modality, knee flexion, and lower extremity alignment in the coronal plane. For example, knee flexion results in unlocking of the screw-home mechanism that mildly decreases tibial tubercle lateralization (averaging 1 mm at 15° of flexion and 2 mm at 30° of flexion) (57). Screw-home mechanism refers to the external rotation of the tibia, relative to the femur, that occurs during the last 20° of knee extension. It is more important that the TT-TG distance can be highly sensitive to lower extremity positioning in slight abduction or adduction when axial images are not adjusted to the anatomic transverse plane (Fig 19) (58). Indeed, only 5° of abduction is associated with a spurious 3.4-mm increase (38%) in the measured TT-TG (58).
Figure 19.
Effect of axial image orientation on the TT-TG measurement. The TT-TG (double-headed arrows) is sensitive to small changes in knee position and should be interpreted with caution if the orientation of the axial image acquisition is not standardized. For neutral orientation and accurate measurement, the axial imaging plane (black lines) is prescribed along the anatomic axial plane parallel to the knee joint (white dashed line). Abduction results in a significant increase in TT−TG, while adduction leads to a spurious decrease in TT−TG.
The most recent promising parameter associated with recurrent patellar instability is used to evaluate the transverse offset from the tibial tubercle to the lateral trochlear ridge (Fig S11) (59). By scrolling proximally to distally on axial MR images, the reader can assess whether the tibial tubercle is substantially medial to the lateral trochlear ridge (normal, on track) or lateral to this ridge (abnormal, off track).
Rotational Deformity
Excessive lower extremity twisting, or torsion, is increasingly being recognized as a risk factor for patellar instability that can be diagnosed with imaging and treated with derotational osteotomy of the femur or tibia (60,61). For the femur, increased anteversion (internal rotation) results in medialization of the trochlea and effectively a lateral vector force on the patella. For the tibia, increased external torsion (external rotation) is associated with external rotation of the foot and subsequent knee valgus that also results in a lateral vector force on the patella (60).
For imaging evaluation, preoperative planning and postoperative follow-up may be performed with low-dose biplanar radiography (eg, EOS System; EOS Imaging), ultra–low-dose CT, or MRI (62). With use of CT or MRI, the degree of femoral anteversion and tibial torsion can be determined by measuring angles with reference axes at the proximal and distal ends of each bone (eg, femoral neck axis vs femoral bicondylar axis, tibial transcondylar axis vs tibial bimalleolar axis) at axial imaging (Fig 20). Wide ranges of normal values for femoral anteversion and external tibial torsion have been published, but measurements of greater than 30° are a potential indication for surgery in adults (60,61).
Figure 20.
Measurement of femoral version. Axial CT image shows the femoral neck angle (double-headed arrow) measurement obtained by using 3D best-fit circles at the femoral head and femoral neck. The femoral version is determined by combining this measurement with the femoral bicondylar axis at the knee. Using 3D techniques for measurements can limit inter- and intraobserver error and improve accuracy.
Dynamic Topics
The imaging techniques being actively researched and showing promise for more widespread clinical use include US, three-dimensional (3D) CT and MRI, and dynamic CT and MRI.
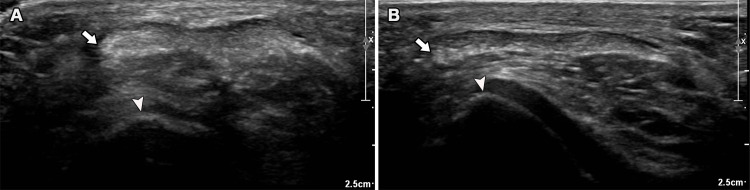
US Imaging.—In addition to enabling direct assessment of soft-tissue structures such as the MPFL complex, US allows dynamic assessment of medial-lateral translation of the patella during flexion and extension or during the application of stress at transverse imaging. For example, when comparing knees with a disrupted versus intact MPFL complex, the medial patellofemoral distance (from the margin of the patella to the medial rim of the trochlea) can increase approximately 30% at 20° of knee flexion (averaging 4 mm without stress and increasing to 6 mm when laterally directed forces are applied on the patella to simulate the patellar glide test) (63). We have also used an anterior-lateral sonographic window to show lateral tracking of the patellar tendon by measuring the interval between the patellar tendon and the lateral trochlear rim at transverse US (Fig 21, Movie 4); these findings can mimic findings seen at MRI (Figs 22, S12). However, there is currently a dearth of data on the reliability and validity of sonographic patellar instability metrics (46).
Figure 21.
Sonographic assessment of patellar instability. Transverse US images of the patellar tendon can be used to quantify lateral translation at various degrees of flexion without (A) and with (B) quadriceps contraction. The distance from the lateral edge of the patellar tendon (arrow) in relation to the lateral margin of the trochlea (arrowhead) can be readily measured and indicates an increase in patellar tendon overriding with quadriceps contraction that is characteristic of maltracking.
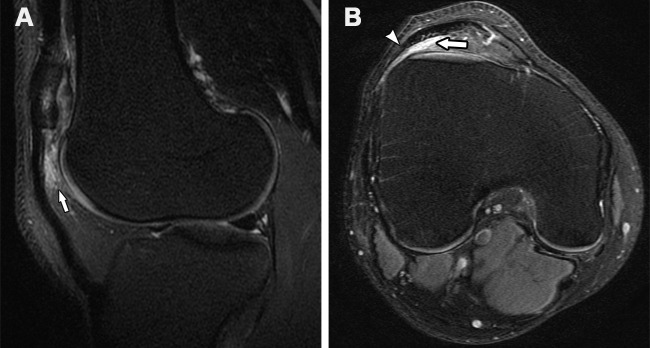
Figure 22.
Anterior knee pain and instability in a 21-year-old man. Sagittal T2-weighted (A) and axial proton-density–weighted (B) fat-suppressed MR images show lateral maltracking of the patella and patellar tendon, with the lateral aspect of the patellar tendon (arrowhead in B) extending laterally to the lateral trochlear ridge. There is also subjacent ill-defined edema (arrow) within the superolateral aspect of the infrapatellar fat pad, consistent with fat pad impingement.
Movie 4.
Dynamic US of the patellar tendon. The patient is placed in a supine position, and transverse images of the patellar tendon are obtained at rest and with full (submaximal) contraction of the quadriceps muscle. Lateral translation of the patellar tendon is assessed in relation to the lateral margin of the trochlea. In this asymptomatic subject, the patellar tendon does not move lateral to the lateral margin of the trochlea.
3D CT and MRI.—Conventional two-dimensional anatomic planes may not show the 3D morphologic features that are important for diagnosis and treatment planning. For example, a single axial image at the proximal trochlea shows a cross-sectional profile, but it does not show various 3D morphologic variations or reduced trochlear volume, which may be useful to a surgeon selecting a trochleoplasty technique (eg, arthroscopic mini-trochleoplasty, sulcus-deepening trochleoplasty, lateral facet-elevation trochleoplasty, or recession wedge trochleoplasty) (Fig 23). 3D imaging data may also be useful for preoperative planning with 3D printing and for finite element models to computationally simulate the biomechanical outcomes of various surgical interventions. However, 3D postprocessing is currently considered time consuming and labor intensive; therefore, refinements in automation and standardization would be helpful (64).
Figure 23.

Trochlear dysplasia. 3D CT reconstruction of the distal femur shows a flat trochlea (arrow) with an anterior prominence in relation to the distal femur.
Dynamic CT and MRI.—Cross-sectional imaging during active joint loading and motion has been evaluated in a growing number of studies. CT and MRI studies performed with the patient in upright weight-bearing positions will probably remain of academic interest only (43), but dynamic acquisitions during motion or muscle contraction are currently in limited clinical use.
With four-dimensional CT (3D CT examinations that capture motion occurring in the time dimension), high–spatial-resolution and high–temporal-resolution images can show standard patellofemoral imaging metrics and a positive J sign during active knee extension (Fig 24) that correlate with instability symptoms (65). However, four-dimensional CT scans are more technically challenging to acquire and interpret. Other drawbacks of four-dimensional CT include radiation exposure and limited ability to show internal derangements and soft-tissue injuries.
Figure 24.
CT assessment for the J sign. Axial CT images at the level of the mid patella show the dynamic relationship of the patella with the trochlea in 30° of flexion (A), 0° of flexion (B), and slight hyperextension (C). Obtaining images at different positions from flexion to extension allows characterization of trochlear engagement and quantitative evaluation of the superior and lateral translations of the patella in extension.
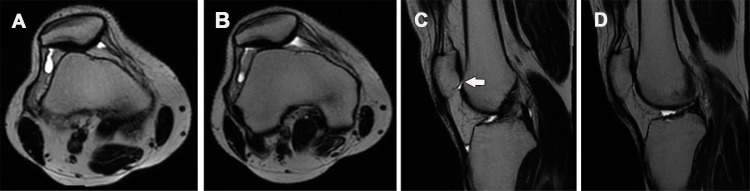
For dynamic MRI, one protocol involves placing two ring surface coils and then acquiring axial and sagittal multisection gradient-echo images while performing two cycles of motion from flexion (40°) to full extension in a custom-made device within 30 seconds (66). An alternative pragmatic dynamic MRI protocol allows the patient’s knee to remain in the dedicated knee coil while a submaximal quadriceps muscle contraction is performed during a 10-second acquisition of axial and sagittal images (Fig 25). With both of these MRI protocols, routine imaging parameters can be evaluated qualitatively or quantitatively. It should be noted that MR images acquired with short acquisition times and high temporal resolution have relatively low spatial resolution; therefore, dynamic images are always acquired as supplements to routine high–spatial-resolution MR images.
Figure 25.
Patellar maltracking seen in a 39-year-old man at physical examination. Axial (A, B) and sagittal (C, D) T2-weighted single-shot fast spin-echo MR images were obtained with quadriceps contraction (A, C) and without quadriceps contraction during a routine static acquisition at rest (B, D). The images obtained with quadriceps contraction (A, C) show increased patellar height and increased lateral tilt, with loss of patellotrochlear cartilage overlap (arrow in C).
Treatment
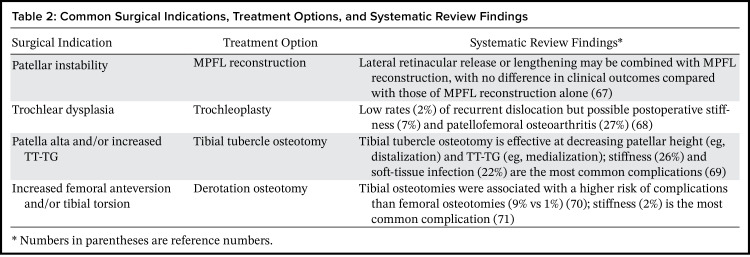
Conservative management is generally the initial imaging-based treatment strategy for patellofemoral pain. Physical therapy, along with other nonsurgical management with taping and bracing, is a primary focus. In patients with recurrent dislocation or in whom conservative management is unsuccessful, treatment options include MPFL reconstruction with or without additional osseous corrections such as trochleoplasty, tibial tubercle osteotomy, and derotational osteotomy (Table 2) (67–71).
Table 2:
Common Surgical Indications, Treatment Options, and Systematic Review Findings
MPFL Reconstruction
MPFL reconstruction is the mainstay of treatment for recurrent patellar dislocations. Lateral retinacular lengthening or release may be combined with MPFL reconstruction (Fig 26), although a relatively recent systematic review revealed no difference in clinical outcomes between this combination procedure and MPFL reconstruction alone (67).
Figure 26.
Lateral patellar retinacular release versus lengthening. Superficial (blue) and deep (red) layers of the lateral patellar retinaculum are schematically depicted. In the retinacular release procedure, which is frequently performed arthroscopically, both layers are transected in one plane. Full lateral release may cause iatrogenic medial patellar subluxation and instability. In retinacular lengthening, deep and superficial layers are isolated during an open surgery and transected at different levels to allow the patella to reduce and then are reapproximated to achieve appropriate tension and maintain integrity of the lateral retinaculum.
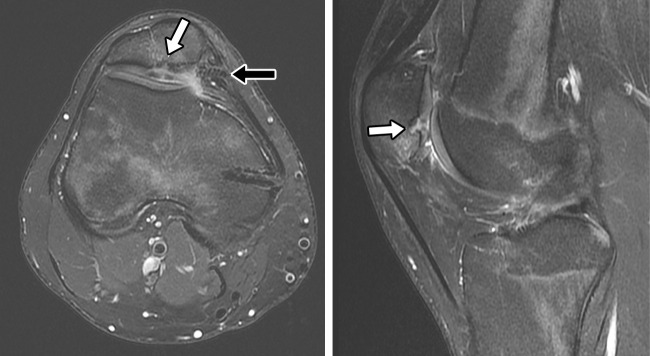
MPFL reconstruction can be difficult to evaluate with MRI. Grafts are often low-signal-intensity tissue with postoperative fibrotic changes (Fig 27). Complications can include graft failure, graft malposition, medial patellar subluxation, and patellar fracture. Closely scrutinizing grafts for the presence of a fluid-filled defect is important in detecting graft tears (Fig 28). Hardware failure may also be encountered (Fig 29). In patients with skeletal immaturity, the close proximity of the physis to the MPFL femoral attachment results in a risk of premature physeal closure.
Figure 27.
Postoperative findings in a 25-year-old woman after MPFL reconstruction and lateral release. Coronal T1-weighted (A) and axial proton-density-weighted fat-suppressed (B) MR images show the expected finding of an intact MPFL reconstruction with a semitendinosus allograft (arrow in B) and bioabsorbable screw tracts at the medial patella and near the medial femoral epicondyle. Expected postprocedural changes, with attenuation of the lateral retinaculum from a prior lateral release (arrowhead in B), also are seen.
Figure 28.
Recurrent patellar dislocation in a 29-year-old woman 3 years after she underwent MPFL reconstruction. Axial proton-density–weighted (A) and T2-weighted (B) fat-suppressed MR images and sagittal T2-weighted fat-suppressed MR image (C) show tearing of the femoral attachment site of the reconstructed MPFL (arrow), near the femoral interference screw.
Figure 29.
Hardware failure in a 17-year-old adolescent boy with mechanical symptoms and anterior knee pain 6 months after MPFL reconstruction. Axial (A) and sagittal (B) T2-weighted fat-suppressed MR images show a displaced screw (black arrow in A) at the posterior-medial aspect of the patella. There is deep chondral fissuring (white arrow) with underlying bone marrow edema-like signal intensity adjacent to the inferior drill tract that extends into the articular cortex of the medial patellar facet.
Trochleoplasty
Trochleoplasty is a general term used to describe surgical techniques performed in an attempt to limit patellar instability events by moving or deepening the native trochlea (72). Patients with severe trochlear dysplasia in the setting of patellar instability may benefit from trochleoplasty in conjunction with MPFL reconstruction. Studies report generally good patient satisfaction with trochleoplasty and an overall associated complication rate of 13% (consisting of increased patellofemoral pain [66%], decreased range of motion [27%], and recurrent dislocation [7%]) (73). Postoperatively, there may be scarring or altered patellar tracking with increased contact pressures that vary from normal patterns (Fig 15). This may in part explain the postoperative stiffness (7%) and high rates of patellofemoral osteoarthritis (27%) reported in a recent meta-analysis of 1000 trochleoplasties (68).
Tibial Tubercle Osteotomy
Tibial tubercle osteotomy involves moving the tibial tubercle to a more favorable location (eg, more distally for patella alta, more medially for abnormal TT-TG medialization, and/or more anteriorly in the setting of patellofemoral chondrosis). This procedure can be used to correct patella alta and lateral translation of the patella. Patella alta is associated with greater lateral displacement, greater lateral tilt, and a decreased contact area (increased contact pressure) compared with the patellar profiles in control subjects (74). Combined with MPFL reconstruction, tibial tubercle distalization leads to normalization of the patellar height in 87% of patients and patellar stabilization in 96% of patients (75). Reported clinical outcomes are generally positive (in 79% of cases), with an average complication rate of 10% (most commonly infection and stiffness) (69). It is important to note that tibial tubercle osteotomies are contraindicated in young children because of the proximity of the physis.
Derotational Osteotomy
While derotational osteotomies to correct tibial torsion have been described with patellar instability, supracondylar osteotomies of the distal femur are more typically performed. The supracondylar osteotomy procedure typically involves anatomic correction with a horizontal osteotomy with screw and plate fixation of the femur (76). Derotational osteotomies may be combined with additional procedures, most commonly MPFL reconstruction, and are generally associated with improved knee function, decreased pain, decreased patellar instability events, and good patient satisfaction (70,71). Stiffness (limited knee flexion) is the most common reported complication (2%) (71), and loss of fixation is potentially the most concerning (70). Realignment surgery for deformity in the coronal plane (usually genu valgum) also can be performed to address an important risk factor for recurrent patellar instability.
Conclusion
Patellofemoral pain and instability are common indications for imaging that are encountered in everyday practice. A strong understanding of patellofemoral anatomy, various clinical presentations, typical imaging findings, and personalized treatment options enables radiologists to provide maximal value to patients and referring providers with high-quality preoperative and postoperative imaging.
Funding.—A.S.C. supported by the National Institutes of Health (grants R01 AR077604 and R01 EB002524); a Precision Health and Integrated Diagnostics Seed Grant from Stanford University; GE Healthcare; and Philips.
Presented as an education exhibit at the 2021 RSNA Annual Meeting.
Disclosures of conflicts of interest.—: T.G. Editorial board member of RadioGraphics. A.S.C. Consulting fees from Subtle Medical, Chondrometric, Image Analysis Group, Edge Analytics, Innovative Cure in Medicine, and Culvert Engineering; member of scientific advisory boards of Chondrometrics and BrainKey; shareholder in Subtle Medical, LVIS, and BrainKey. S.L.S. American Orthopaedic Society for Sports Medicine grant for motion analysis study; royalties from ConMed and Donjoy Orthopedic; consulting fees from Active Implants, Allosource, Association of Osteosynthesis, Arcuro, Arthrex, Bioventus, ConMed, Depuy Johnson & Johnson, Donjoy Orthopedic, Flexion, JRF Ortho, Kinamed, LifeNet, NewClip, Reparel, Sarcio, Smith & Nephew, Sparta Biomedical, Vericel, and Vivorte; committee member of Arthroscopy Association of North America, Anterior Cruciate Ligament Study Group, American Orthopaedic Society for Sports Medicine, and Biologic Alliance; committee chair of American Academy of Orthopaedic Surgeons; editorial board member of Arthroscopy Journal, Current Reviews in Musculoskeletal Medicine, and Video Journal of Sports Medicine; committee member and general board member of International Cartilage Regeneration & Joint Preservation Society; committee deputy chair of International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine; course chair of International Sports Medicine Fellows; online course chair of Patellofemoral Foundation; owns stock in Vivorte, Sarcio, Reparel, and Epic Bio. R.D.B. President-elect of the Society of Academic Bone Radiologists.
Abbreviations:
- MPFL
- medial patellofemoral ligament
- MPML
- medial patellomeniscal ligament
- MPTL
- medial patellotibial ligament
- MQTFL
- medial quadriceps tendon femoral ligament
- 3D
- three dimensional
- TT-TG
- medial-lateral distance from the tibial tubercle to the trochlear groove
References
- 1. Brooke R . The treatment of fractured patella by excision. A study of morphology and function . Br J Surg 1937. ; 24 ( 96 ): 733 – 747 . [Google Scholar]
- 2. Samuels ME , Regnault S , Hutchinson JR . Evolution of the patellar sesamoid bone in mammals . PeerJ 2017. ; 5 : e3103 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Neumann DA . Knee . In: Falk K , ed. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation . 2nd ed. St. Louis, Mo: : Mosby/Elsevier; , 2010. ; 557 . [Google Scholar]
- 4. Aglietti P , Menchetti P . Biomechanics of the patellofemoral joint . In: Scuderi GR , ed. The Patella . New York, NY: : Springer; , 1995. ; 25 . [Google Scholar]
- 5. Smith BE , Selfe J , Thacker D , et al . Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis . PLoS One 2018. ; 13 ( 1 ): e0190892 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hughston JC . Subluxation of the patella . J Bone Joint Surg Am 1968. ; 50 ( 5 ): 1003 – 1026 . [PubMed] [Google Scholar]
- 7. Post WR , Fithian DC . Patellofemoral Instability: A Consensus Statement From the AOSSM/PFF Patellofemoral Instability Workshop . Orthop J Sports Med 2018. ; 6 ( 1 ): 2325967117750352 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Richmond CG , Shea KG , Burlile JF , et al . Patellar-Trochlear Morphology in Pediatric Patients From 2 to 11 Years of Age: A Descriptive Analysis Based on Computed Tomography Scanning . J Pediatr Orthop 2020. ; 40 ( 2 ): e96 – e102 . [DOI] [PubMed] [Google Scholar]
- 9. Choi W , Lee SJ , Oh J , et al . Magnetic Resonance Imaging of Patellofemoral Morphometry Reveals Age and Gender Variations in the Knees of Children and Adolescents . Diagnostics (Basel) 2021. ; 11 ( 11 ): 1985 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tanaka MJ , Chahla J , Farr J 2nd , et al . Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction . Knee Surg Sports Traumatol Arthrosc 2019. ; 27 ( 8 ): 2537 – 2550 . [Published correction appears in Knee Surg Sports Traumatol Arthrosc 2019;27(8):2551.] [DOI] [PubMed] [Google Scholar]
- 11. Ge Y , Chen S , Kato T , Zdanowicz U , Smigielski R . A polygon-shaped complex appearance of medial patellofemoral ligament with dynamic functional insertion based on an outside-in and inside-out dissection technique . Knee Surg Sports Traumatol Arthrosc 2018. ; 26 ( 12 ): 3754 – 3761 . [DOI] [PubMed] [Google Scholar]
- 12. Zandee van Rilland E , Payne S , Gorbachova T , et al . MRI of Patellar Stabilizers: Visibility of Primary and Secondary Ligament Anatomy . Presented at the Annual Meeting of the American Roentgen Ray Society , Honolulu, Hawaii , April 16–20 . [Google Scholar]
- 13. Dirim B , Haghighi P , Trudell D , Portes G , Resnick D . Medial patellofemoral ligament: cadaveric investigation of anatomy with MRI, MR arthrography, and histologic correlation . AJR Am J Roentgenol 2008. ; 191 ( 2 ): 490 – 498 . [DOI] [PubMed] [Google Scholar]
- 14. Sobhy MH . Editorial Commentary: Medial Patellofemoral Complex: Driving a Better Understanding of Medial Knee Anatomy . Arthroscopy 2019. ; 35 ( 4 ): 1147 – 1151 . [DOI] [PubMed] [Google Scholar]
- 15. Raoulis V , Fyllos A , Klontzas ME , et al . Surgical and Radiological Anatomy of the Medial Patellofemoral Ligament: A Magnetic Resonance Imaging and Cadaveric Study . Diagnostics (Basel) 2021. ; 11 ( 11 ): 2076 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen J , Xiong Y , Han K , et al . Computed Tomography Imaging Analysis of the MPFL Femoral Footprint Morphology and the Saddle Sulcus: Evaluation of 1094 Knees . Orthop J Sports Med 2022. ; 10 ( 2 ): 23259671211073608 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cregar WM , Huddleston HP , Wong SE , Farr J , Yanke AB . Inconsistencies in Reporting Risk Factors for Medial Patellofemoral Ligament Reconstruction Failure: A Systematic Review . Am J Sports Med 2022. ; 50 ( 3 ): 867 – 877 . [DOI] [PubMed] [Google Scholar]
- 18. Baldwin JL . The anatomy of the medial patellofemoral ligament . Am J Sports Med 2009. ; 37 ( 12 ): 2355 – 2361 . [DOI] [PubMed] [Google Scholar]
- 19. Collins MS , Tiegs-Heiden CA , Frick MA , Brandt MD . Medial patellofemoral ligament MRI abnormalities in the setting of MCL injuries: are they clinically relevant? Skeletal Radiol 2022. ; 51 ( 7 ): 1381 – 1389 . [DOI] [PubMed] [Google Scholar]
- 20. Christian DR , Redondo ML , Cancienne JM , et al . Differential Contributions of the Quadriceps and Patellar Attachments of the Proximal Medial Patellar Restraints to Resisting Lateral Patellar Translation . Arthroscopy 2020. ; 36 ( 6 ): 1670 – 1676 . [DOI] [PubMed] [Google Scholar]
- 21. Chahla J , Smigielski R , LaPrade RF , Fulkerson JP . An Updated Overview of the Anatomy and Function of the Proximal Medial Patellar Restraints (Medial Patellofemoral Ligament and the Medial Quadriceps Tendon Femoral Ligament) . Sports Med Arthrosc Rev 2019. ; 27 ( 4 ): 136 – 142 . [DOI] [PubMed] [Google Scholar]
- 22. Fulkerson JP . Editorial Commentary: The Best Medial Patellofemoral Reconstruction May Include Components of Both Quadriceps and Patellar Attachments . Arthroscopy 2020. ; 36 ( 6 ): 1677 – 1678 . [DOI] [PubMed] [Google Scholar]
- 23. Temponi EF , Saithna A , Gonçalves MBJ , Soares LFM , Carvalho RB , de Carvalho Júnior LH . Combined Reconstruction of the Medial Patellofemoral Ligament and Medial Quadriceps Tendon-Femoral Ligament . Arthrosc Tech 2021. ; 10 ( 1 ): e193 – e198 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hinckel BB , Lipinski L , Arendt EA . Concepts of the Distal Medial Patellar Restraints: Medial Patellotibial Ligament and Medial Patellomeniscal Ligament . Sports Med Arthrosc Rev 2019. ; 27 ( 4 ): 143 – 149 . [DOI] [PubMed] [Google Scholar]
- 25. Felli L , Alessio-Mazzola M , Lovisolo S , Capello AG , Formica M , Maffulli N . Anatomy and biomechanics of the medial patellotibial ligament: a systematic review . Surgeon 2021. ; 19 ( 5 ): e168 – e174 . [DOI] [PubMed] [Google Scholar]
- 26. Philippot R , Boyer B , Testa R , Farizon F , Moyen B . The role of the medial ligamentous structures on patellar tracking during knee flexion . Knee Surg Sports Traumatol Arthrosc 2012. ; 20 ( 2 ): 331 – 336 . [DOI] [PubMed] [Google Scholar]
- 27. Aicale R , Maffulli N . Combined medial patellofemoral and medial patellotibial reconstruction for patellar instability: a PRISMA systematic review . J Orthop Surg Res 2020. ; 15 ( 1 ): 529 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huddleston HP , Chahla J , Gursoy S , et al . A Comprehensive Description of the Lateral Patellofemoral Complex: Anatomy and Anisometry . Am J Sports Med 2022. ; 50 ( 4 ): 984 – 993 . [DOI] [PubMed] [Google Scholar]
- 29. Dandu N , Trasolini NA , DeFroda SF , Darwish RY , Yanke AB . The Lateral Side: When and How to Release, Lengthen, and Reconstruct . Clin Sports Med 2022. ; 41 ( 1 ): 171 – 183 . [DOI] [PubMed] [Google Scholar]
- 30. Loeb AE , Farr J , Parikh SN , Cosgarea AJ . Noniatrogenic Medial Patellar Dislocations: Case Series and International Patellofemoral Study Group Experience . Orthop J Sports Med 2021. ; 9 ( 2 ): 2325967120985530 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liu JN , Steinhaus ME , Kalbian IL , et al . Patellar Instability Management: A Survey of the International Patellofemoral Study Group . Am J Sports Med 2018. ; 46 ( 13 ): 3299 – 3306 . [DOI] [PubMed] [Google Scholar]
- 32. Sahota B , Howes M , Rio E , Docking S , Cook J . Association between knee pain location and abnormal imaging or arthroscopic findings: a systematic review . Ann Phys Rehabil Med 2022. ; 65 ( 4 ): 101638 . [DOI] [PubMed] [Google Scholar]
- 33. Grant C , Fick CN , Welsh J , McConnell J , Sheehan FT . A Word of Caution for Future Studies in Patellofemoral Pain: A Systematic Review With Meta-analysis . Am J Sports Med 2021. ; 49 ( 2 ): 538 – 551 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dewan V , Webb MSL , Prakash D , Malik A , Gella S , Kipps C . When does the patella dislocate? A systematic review of biomechanical & kinematic studies . J Orthop 2019. ; 20 : 70 – 77 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sonnery-Cottet B , Hopper GP , Gousopoulos L , et al . Arthrogenic Muscle Inhibition Following Knee Injury or Surgery: Pathophysiology, Classification, and Treatment . Video J Sports Med 2022. ; 2 ( 3 ). [Google Scholar]
- 36. Nunes GS , Stapait EL , Kirsten MH , de Noronha M , Santos GM . Clinical test for diagnosis of patellofemoral pain syndrome: systematic review with meta-analysis . Phys Ther Sport 2013. ; 14 ( 1 ): 54 – 59 . [DOI] [PubMed] [Google Scholar]
- 37. Nagamine R , Miura H , Inoue Y , et al . Malposition of the tibial tubercle during flexion in knees with patellofemoral arthritis . Skeletal Radiol 1997. ; 26 ( 10 ): 597 – 601 . [DOI] [PubMed] [Google Scholar]
- 38. Best MJ , Tanaka MJ , Demehri S , Cosgarea AJ . Accuracy and Reliability of the Visual Assessment of Patellar Tracking . Am J Sports Med 2020. ; 48 ( 2 ): 370 – 375 . [DOI] [PubMed] [Google Scholar]
- 39. Rogers DL , Cosgarea AJ . Evaluating Patellofemoral Patients: Physical Examination, Radiographic Imaging, and Measurements . Clin Sports Med 2022. ; 41 ( 1 ): 1 – 13 . [DOI] [PubMed] [Google Scholar]
- 40. White AE , Otlans PT , Horan DP , et al . Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis . Orthop J Sports Med 2021. ; 9 ( 5 ): 2325967121993179 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kurowecki D , Shergill R , Cunningham KM , et al . A comparison of sagittal MRI and lateral radiography in determining the Insall-Salvati ratio and diagnosing patella alta in the pediatric knee . Pediatr Radiol 2022. ; 52 ( 3 ): 527 – 532 . [DOI] [PubMed] [Google Scholar]
- 42. Verhulst FV , van Sambeeck JDP , Olthuis GS , van der Ree J , Koëter S . Patellar height measurements: Insall-Salvati ratio is most reliable method . Knee Surg Sports Traumatol Arthrosc 2020. ; 28 ( 3 ): 869 – 875 . [DOI] [PubMed] [Google Scholar]
- 43. Becher C , Fleischer B , Rase M , et al . Effects of upright weight bearing and the knee flexion angle on patellofemoral indices using magnetic resonance imaging in patients with patellofemoral instability . Knee Surg Sports Traumatol Arthrosc 2017. ; 25 ( 8 ): 2405 – 2413 . [DOI] [PubMed] [Google Scholar]
- 44. Paul RW , Brutico JM , Wright ML , et al . Strong Agreement Between Magnetic Resonance Imaging and Radiographs for Caton-Deschamps Index in Patients With Patellofemoral Instability . Arthrosc Sports Med Rehabil 2021. ; 3 ( 6 ): e1621 – e1628 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dejour DH , Mesnard G , Giovannetti de Sanctis E . Updated treatment guidelines for patellar instability: “un menu à la carte” . J Exp Orthop 2021. ; 8 ( 1 ): 109 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Geraghty L , Humphries D , Fitzpatrick J . Assessment of the reliability and validity of imaging measurements for patellofemoral instability: an updated systematic review . Skeletal Radiol 2022. ; 51 ( 12 ): 2245 – 2256 . [DOI] [PubMed] [Google Scholar]
- 47. Fabricant PD , Heath MR , Mintz DN , et al . Many Radiographic and Magnetic Resonance Imaging Assessments for Surgical Decision Making in Pediatric Patellofemoral Instability Patients Demonstrate Poor Interrater Reliability . Arthroscopy 2022. ; 38 ( 9 ): 2702 – 2713 . [DOI] [PubMed] [Google Scholar]
- 48. Konrads C , Gonser C , Ahmad SS . Reliability of the Oswestry-Bristol Classification for Trochlear Dysplasia: Expanded Characteristics . Bone Jt Open 2020. ; 1 ( 7 ): 355 – 358 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brady JM , Rosencrans AS , Shubin Stein BE . Use of TT-PCL versus TT-TG . Curr Rev Musculoskelet Med 2018. ; 11 ( 2 ): 261 – 265 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kluczynski MA , Miranda L , Marzo JM . Prevalence and Site of Medial Patellofemoral Ligament Injuries in Patients With Acute Lateral Patellar Dislocations: A Systematic Review and Meta-analysis . Orthop J Sports Med 2020. ; 8 ( 12 ): 2325967120967338 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Larson N , Nguyen C , Do B , et al . Artificial Intelligence System for Automatic Quantitative Analysis and Radiology Reporting of Leg Length Radiographs . J Digit Imaging 2022. . 10.1007/s10278-022-00671-2. Published online July 6, 2022 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Smith TO , Davies L , Toms AP , Hing CB , Donell ST . The reliability and validity of radiological assessment for patellar instability: a systematic review and meta-analysis . Skeletal Radiol 2011. ; 40 ( 4 ): 399 – 414 . [DOI] [PubMed] [Google Scholar]
- 53. Ahmad M , Janardhan S , Amerasekera S , Nightingale P , Ashraf T , Choudhary S . Reliability of patellotrochlear index in patellar height assessment on MRI-correction for variation due to change in knee flexion . Skeletal Radiol 2019. ; 48 ( 3 ): 387 – 393 . [DOI] [PubMed] [Google Scholar]
- 54. Urch SE , Tritle BA , Shelbourne KD , Gray T . Axial linear patellar displacement: a new measurement of patellofemoral congruence . Am J Sports Med 2009. ; 37 ( 5 ): 970 – 973 . [DOI] [PubMed] [Google Scholar]
- 55. Rémy F , Chantelot C , Fontaine C , Demondion X , Migaud H , Gougeon F . Inter- and intraobserver reproducibility in radiographic diagnosis and classification of femoral trochlear dysplasia . Surg Radiol Anat 1998. ; 20 ( 4 ): 285 – 289 . [DOI] [PubMed] [Google Scholar]
- 56. Dong Z , Zhang X , Xu C , Ji G , Niu Y , Wang F . The tibial tubercle-posterior cruciate ligament (TT-PCL) distance does not truly reflect the lateralization of the tibial tubercle . Knee Surg Sports Traumatol Arthrosc 2022. ; 30 ( 10 ): 3470 – 3479 . [DOI] [PubMed] [Google Scholar]
- 57. Seitlinger G , Scheurecker G , Högler R , Labey L , Innocenti B , Hofmann S . The position of the tibia tubercle in 0°-90° flexion: comparing patients with patella dislocation to healthy volunteers . Knee Surg Sports Traumatol Arthrosc 2014. ; 22 ( 10 ): 2396 – 2400 . [DOI] [PubMed] [Google Scholar]
- 58. Yao L , Gai N , Boutin RD . Axial scan orientation and the tibial tubercle-trochlear groove distance: error analysis and correction . AJR Am J Roentgenol 2014. ; 202 ( 6 ): 1291 – 1296 . [DOI] [PubMed] [Google Scholar]
- 59. Weltsch D , Chan CT , Mistovich RJ , et al . Predicting Risk of Recurrent Patellofemoral Instability With Measurements of Extensor Mechanism Containment . Am J Sports Med 2021. ; 49 ( 3 ): 706 – 712 . [DOI] [PubMed] [Google Scholar]
- 60. Noonan B , Cooper T , Chau M , Albersheim M , Arendt EA , Tompkins M . Rotational Deformity: When and How to Address Femoral Anteversion and Tibial Torsion . Clin Sports Med 2022. ; 41 ( 1 ): 27 – 46 . [DOI] [PubMed] [Google Scholar]
- 61. Snow M . Tibial Torsion and Patellofemoral Pain and Instability in the Adult Population: Current Concept Review . Curr Rev Musculoskelet Med 2021. ; 14 ( 1 ): 67 – 75 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Waelti S , Fischer T , Griessinger J , et al . Ultra-low-dose computed tomography for torsion measurements of the lower extremities in children and adolescents . Insights Imaging 2022. ; 13 ( 1 ): 118 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bhimani R , Ashkani-Esfahani S , Mirochnik K , Lubberts B , DiGiovanni CW , Tanaka MJ . Utility of Diagnostic Ultrasound in the Assessment of Patellar Instability . Orthop J Sports Med 2022. ; 10 ( 5 ): 23259671221098748 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Pennock AT , Chang A , Doan J , Bomar JD , Edmonds EW . 3D Knee Trochlear Morphology Assessment by Magnetic Resonance Imaging in Patients With Normal and Dysplastic Trochleae . J Pediatr Orthop 2020. ; 40 ( 3 ): 114 – 119 . [DOI] [PubMed] [Google Scholar]
- 65. Tanaka MJ , Elias JJ , Williams AA , Demehri S , Cosgarea AJ . Characterization of patellar maltracking using dynamic kinematic CT imaging in patients with patellar instability . Knee Surg Sports Traumatol Arthrosc 2016. ; 24 ( 11 ): 3634 – 3641 . [DOI] [PubMed] [Google Scholar]
- 66. Frings J , Dust T , Krause M , et al . Dynamic Mediolateral Patellar Translation Is a Sex- and Size-Independent Parameter of Adult Proximal Patellar Tracking Using Dynamic 3 Tesla Magnetic Resonance Imaging . Arthroscopy 2022. ; 38 ( 5 ): 1571 – 1580 . [DOI] [PubMed] [Google Scholar]
- 67. Migliorini F , Maffulli N , Eschweiler J , Quack V , Tingart M , Driessen A . Lateral retinacular release combined with MPFL reconstruction for patellofemoral instability: a systematic review . Arch Orthop Trauma Surg 2021. ; 141 ( 2 ): 283 – 292 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Leclerc JT , Dartus J , Labreuche J , et al . Complications and outcomes of trochleoplasty for patellofemoral instability: a systematic review and meta-analysis of 1000 trochleoplasties . Orthop Traumatol Surg Res 2021. ; 107 ( 7 ): 103035 . [DOI] [PubMed] [Google Scholar]
- 69. Rosso F , Rossi R , Cottino U , Bonasia DE . Tibial tubercle osteotomy for patellofemoral malalignment and chondral disease provided good outcomes: a systematic review . J ISAKOS 2022. ; 7 ( 2 ): 78 – 86 . [DOI] [PubMed] [Google Scholar]
- 70. Sanchis-Alfonso V , Domenech-Fernandez J , Ferras-Tarrago J , Rosello-Añon A , Teitge RA . The incidence of complications after derotational femoral and/or tibial osteotomies in patellofemoral disorders in adolescents and active young patients: a systematic review with meta-analysis . Knee Surg Sports Traumatol Arthrosc 2022. ; 30 ( 10 ): 3515 – 3525 . [DOI] [PubMed] [Google Scholar]
- 71. Zhang Z , Cao Y , Song G , Li Y , Zheng T , Zhang H . Derotational Femoral Osteotomy for Treating Recurrent Patellar Dislocation in the Presence of Increased Femoral Anteversion: A Systematic Review . Orthop J Sports Med 2021. ; 9 ( 11 ): 23259671211057126 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Dejour DH , Deroche É . Trochleoplasty: indications in patellar dislocation with high-grade dysplasia—surgical technique . Orthop Traumatol Surg Res 2022. ; 108 ( 1S ): 103160 . [DOI] [PubMed] [Google Scholar]
- 73. Ferrua P , Compagnoni R , Calanna F , Randelli PS , Dejour D . Good patient satisfaction with low complications rate after trochleoplasty in patellofemoral instability . Knee Surg Sports Traumatol Arthrosc 2022. ; 30 ( 10 ): 3444 – 3450 . [DOI] [PubMed] [Google Scholar]
- 74. Ward SR , Terk MR , Powers CM . Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing . J Bone Joint Surg Am 2007. ; 89 ( 8 ): 1749 – 1755 . [DOI] [PubMed] [Google Scholar]
- 75. Schmiesing A , Engelking M , Agel J , Arendt EA . Distalization of the Tibial Tubercle for Patellar Stabilization Combined With Medial Patellofemoral Ligament Reconstruction: Length of Distalization or Residual Patella Alta and its Affect on Outcome . Am J Sports Med 2022. ; 50 ( 6 ): 1627 – 1634 . [DOI] [PubMed] [Google Scholar]
- 76. Biedert RM . Combined deepening trochleoplasty and supracondylar external rotation osteotomy for recurrent patellar instability in patients with trochlear dysplasia and increased femoral antetorsion . Knee 2020. ; 27 ( 4 ): 1158 – 1166 . [DOI] [PubMed] [Google Scholar]