Abstract
The patient's financial experience is often complex and confusing.
Recent regulations support bringing more transparency to healthcare billing processes.
A patient journey map illustrates the patient experience in a healthcare process helping to identify improvement opportunities to better support patient-centered care.
Price transparency can be increased by communicating the patient's financial responsibility early in the care process as well as simplifying patient communications.
Digital health applications can help improve the patient financial experience and ultimately engagement in the payment process.
Greater clarity and improved processes may occur if the patient's journey is visualized.
Keywords: patient financial experience, patient journey map, price transparency, digital health, digital health applications, healthcare billing
Introduction to the Issue
Billing for healthcare services is complex and involves many different stakeholders, often with conflicting views, resulting in processes too complicated for patients to understand. After patients seek healthcare services and receive treatment, healthcare providers request payment from the patient's insurance company and/or the patient, depending on coverage. Insurance coverage is determined by service, medical necessity, deductibles, and coinsurance percentages, among other factors. Patients are usually sent a billing statement requesting payment; however, understanding a healthcare bill for medical services can be challenging for them. 1 This often leaves patients confused and frustrated with the experience.
An important part of the patient experience is to provide clear expectations regarding the payment process and the patient's financial responsibility which can help facilitate patient engagement in those processes. That is, if patients understand what to expect about their financial responsibility, they can more actively engage in taking action on their portion of healthcare bills. Being more engaged in their healthcare by taking on the role of a consumer also helps patients reduce overall treatment expenses, an especially important factor given rising healthcare costs. As patients shift to the role of consumers, their expectations for healthcare processes shift to mirror retail processes that provide fast, easy, convenient service.2,3
Further, industry best practices specify that healthcare financial communications should be easy to understand. 4 First, bills should clearly communicate the patient's financial responsibility, and second, administrative processes should be patient-friendly. 4 In reality, healthcare billing practices frequently do not meet these standards. 5
Additionally, healthcare bills often contain unexpected charges. In fact, in 2021, 87% of consumers were surprised by a medical bill they received. 1 In recent years, Congress has taken action to address healthcare billing practices to reduce the number of unexpected bills patients receive. The No Surprises Act (passed in 2020; effective January 2022) sought to eliminate surprise bills that patients, with private insurance, may receive for services from out-of-network providers. While insurers may make payments for out-of-network services, in the past, providers could bill patients for the balance of their charges not paid by insurers. 6 This Surprises Act limits patient costs for out-of-network providers to in-network copays and coinsurance and sets limits for deductibles and maximum out-of-pocket payments in these situations. 6 This Act specified that providers could no longer send bills to patients for the remaining balance or increase the bill.
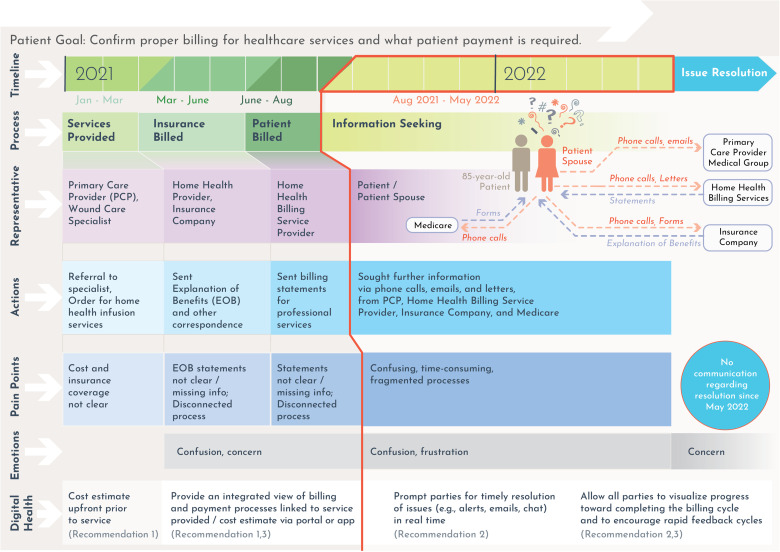
To better understand the patient experience, a patient journey map can be drafted. A patient journey map visually illustrates the patient experience as the patient moves through healthcare processes, while also providing insight into areas that may need improvement to support patient-centered care 7 as well as digital technologies that may support the patient's journey. 8 Below, one patient's journey is described to show how the patient sought to resolve a healthcare bill as well as key factors that affected the patient’s experience.
Key Factors for Consideration Based on the Patient's Journey
An 85-year-old male received a series of 6 home infusion services (a Medicare Part B service) to treat a hip wound infection. These services were provided from January to March 2021 by a large integrated health system's home health division. The patient received Statements for Professional Services (eg, bills) for these services. Notably, these bills provided no indication whatsoever as to whether the services had been billed to primary and secondary insurance. Further, only charge dates were listed without indicating service dates.
The patient also received monthly Explanation of Benefits (EOBs) from his insurance provider that listed the primary infusion service as “INFUS SPL NOT USED W/EXT INFUS PUMP CASSETTE/BAG” and a billing code of A4223. The EOBs also contained notes stating the patient's financial responsibility was 20% of the total amount for services from a “Network Provider.” A date range of a week was provided but no specific service dates. The total amount due for the 6 infusion services was US$1973.93, as indicated on a statement received in August 2021. This stated patient responsibility was a surprise (the patient did not expect it) and a financial burden as the patient was on a fixed income. Because it was not clear on the Statements for Professional Services whether insurance had been billed properly, the patient's spouse sought more information before making any payments.
As shown in Figure 1, the patient's journey to resolve the billing issue occurred over the next ten months. During this time, a variety of communications occurred—often containing conflicting information. For example, based on these communications, the patient’s financial responsibility varied from US$41 to US$362 per service. During this time, the home health service provider also changed its billing services vendor which resulted in staffing changes. Many messages were left for representatives as it was not possible to reach them directly.
Figure 1.
Patient journey to pay healthcare bill.
The patient's spouse contacted Medicare to verify that infusion services were covered service. She was informed that Medicare Part B does, indeed, cover external infusion pumps—if they are considered reasonable and necessary for treatment and if a doctor prescribes them for use in the patient's home. The Medicare agent also suggested sending a claim directly to Medicare as the home health billing provider had refused to do so. This claim was summarily denied because the home health provider was not a Medicare participating provider which was confusing as the health system, itself, was a Medicare provider.
The patient's wife also appealed the bill to the insurance company. As part of the appeal process, the insurance company representative informed them that payment should have been coordinated through the primary medical group (PMG) rather than being billed directly by the home health services provider, and a request was made to the PMG to address this issue. The status of the patient billing issue is unknown as there has been no communication since May 2022.
The patient's spouse described this overall experience as “fragmented, confusing, frustrating, and time-consuming.” She also was very concerned about what might happen if the bill was not paid while she was seeking more information and clarity. Key factors identified based on the patient journey included the following:
Too many conflicting communications. Each contact at the home health billing service and insurance company provided a different explanation of the billing situation which could not be reconciled. Written communications such as statements and EOBs were unclear and incomplete.
Long delays, with many cycles. The patient's spouse made multiple calls to gather information, and left messages requiring follow-up. In some cases, the follow-up required submitting a form. Then, there would be a lag till the next communication, and the cycle would start again.
Lack of focus on resolving the patient's concern. While many conversations took place with the various parties involved in this billing issue, no ownership was claimed by the various representatives involved in billing, given that there was no one point of contact for resolution.
Recommendations
The following are recommendations to address the patient journey pain points as noted in Figure 1.
Increase price transparency by communicating patient financial responsibility early in the care process as well as following industry best practices for patient communications. While 9 in 10 patients report that they would like to know their payment responsibility upfront, only 2 in 10 patients know what they will owe after an appointment. 1 Cost estimates help patients understand what they will owe; yet, few patients currently receive them. 2 At the same time, most healthcare organizations report having the capability to provide these cost estimates. 2 Due to recent regulations, under certain circumstances, healthcare providers and facilities are now required to provide a good faith estimate of expected charges. 9 Providing cost estimates and statements that clearly outline a patient's financial responsibility would undoubtedly reduce billing issues while increasing patient engagement and satisfaction.
Make patient billing processes more responsive and efficient by utilizing digital health technologies. Digital health applications transform processes through a combination of information, communication, and connectivity technologies. Examples include patient portals and mobile applications for asking questions and sharing information, as well as digital assistants with chat functionality. Access to digital technology tools through multiple channels can help encourage patients’ participation in their own healthcare and keep patients informed. 8 Use of digital technologies can also positively impact the quality of care by increasing responsiveness and improving administrative processes. 10
Make the patient journey visible to all parties to help streamline the billing cycle. Having one integrated view of the billing and payment process would undoubtedly make communications, status, and resolution timeline (eg, an issue that has been outstanding for 3 months without resolution) easier to follow. Digital health applications can support these efforts in real time and rapid feedback can be used to improve processes.
Conclusion
The patient's journey to pay a healthcare bill is often overly complex and confusing, due in no small part to the complicated processes used. Healthcare organizations need to be more proactive in improving and simplifying the patient's financial experience. The recommendations noted above can help improve these experiences in the future.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics and Patient Consent: The patient and the patient spouse agreed to share their patient experience from this perspective.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Melanie A. Meyer https://orcid.org/0000-0002-1850-8473
References
- 1.Instamed. Trends in healthcare payments. 2021. https://www.instamed.com/white-papers/trends-in-healthcare-payments-annual-report/.
- 2.Sanborn B. HIMSS Analytics survey shows patients want convenient payment options. 2018. updated June 8, 2018. https://www.healthcarefinancenews.com/news/himss-analytics-survey-shows-patients-want-convenient-payment-options.
- 3.Poucke A. Healthcare CEO Future Pulse: KPMG. 2021. https://home.kpmg/xx/en/home/insights/2021/06/healthcare-ceo-future-pulse.html.
- 4.Patient Friendly Billing Project: Healthcare Financial Management Association. 2019. https://www.hfma.org/patientfriendlybilling.
- 5.Asser J. Nearly 40% of patients find medical bills confusing: Health Leaders Media. 2022. https://www.healthleadersmedia.com/revenue-cycle/nearly-40-patients-find-medical-bills-confusing.
- 6.Hoadley J, Lucia K. The no surprises act: a bipartisan achievement to protect consumers from unexpected medical bills. J Health Polit Policy Law. 2022;47(1):93-109. [DOI] [PubMed] [Google Scholar]
- 7.Madathil C, Alfred L, eds. Patient journey mapping: a literature review. Proceedings of the 2020 IISE Annual Conference; 2020. [Google Scholar]
- 8.Borycki E, Kushniruk A, Wagner E, Kletke R. Patient journey mapping: integrating digital technologies into the journey. Knowl Manag E-Learn .2020;12(4):521-35. [Google Scholar]
- 9.Understanding costs in advance: Centers for Medicare & Medicaid Services. 2022. https://www.cms.gov/nosurprises/consumers/understanding-costs-in-advance.
- 10.Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC. Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res. 2021;123:557-67. [Google Scholar]