Abstract
Objectives
The effect of social media on COVID-19 vaccination behavior is sub-Saharan Africa is unclear. We conducted a study to determine social media use among a random nationally representative sample of adults in Uganda and assessed the association between recent social media use and COVID-19 vaccination uptake.
Methods
We used data from the 2020 general population survey in Uganda, the Population-based HIV Impact Assessment Survey, to identify a probability sample for a mobile phone survey and included nonphone owners in the phone survey by asking phone owners to pass the phone.
Results
In March 2022, of the 1022 survey participants, 213 (20%) did not own a mobile phone, 842 (80%) owned a mobile phone, of whom 199 (24%) indicated social media use, and 643 (76%) of whom did not use social media. Among all participants, the most frequent source of COVID-19 vaccine information was radio. Overall, 62% reported receiving the COVID-19 vaccination. The multivariable logistic regression model found that social media use was not associated with vaccination status.
Conclusion
Social media users in this population sample from Uganda—who were mainly young, urban residents with higher educational attainment—continue to utilize TV, radio and health care workers for public health messages, thus the Government of Uganda should continue to conduct public health communication through these mediums.
Keywords: COVID-19, vaccine, social media, Africa, Uganda, cell phone survey
Background
Social media and the internet have played an important role in motivating vaccine hesitancy worldwide due to the rapid pace information travels on the internet, difficulty assessing the accuracy of online information, and reluctance of social media companies to tackle misinformation and disinformation. 1 Even minimal exposure—5–10 min—to vaccine-critical content has been noted to increase one's perceptions of vaccination risks and decreases perceptions of the consequences of vaccine omission and intentions to vaccinate. 2 This has fueled concern about the role of social media on COVID-19 vaccine hesitancy, a demand-side barrier defined as “the reluctance or refusal to vaccinate despite the availability of vaccines,” an issue listed as a top 10 threat to global health in 2019 by the World Health Organization. 3
The concerns regarding social media and vaccine attitudes and uptake extend to sub-Saharan Africa (SSA), where mobile phone usage has grown rapidly over the past 15 years, and social media use has increased, albeit at a slower rate compared to other regions of the world. 4 There was concern about increasing vaccine hesitancy in SSA prior to COVID-19 pandemic. 5 For example, a trend was noted among persons in the wealthiest quintiles refusing vaccination for their children in a study conducted early 2020 in 86 low- and middle-income countries. 6 Less is known about vaccine hesitancy for adult vaccines in SSA, and information on COVID-19 vaccine hesitancy was mainly conducted prior to the availability of such vaccines in SSA, creating estimates of anticipated instead of actual behavior.7–9 Recognizing the importance of combating misinformation circulating via social media, in 2020 the World Health Organization launched The Africa Infodemic Response Alliance to combat misinformation about COVID-19. 10
In Uganda, a country with a population of 44 million, 56% of the population owned a mobile phone in 2018, 11 with an estimated 16% owning a smartphone. 12 COVID-19 vaccination campaigns began in March 2021 for specific subsets of the populations. The vaccine was made available to the general population in August 2021 and as of September 2022, 82% of adults (18+ years) have received one dose, and 58% are fully vaccinated. Two phone studies at the end of 2020 found a high willingness (over 80%) to be vaccinated for COVID-19 among participants in Uganda.13,14 In a survey conducted by Africa CDC, 24% of Ugandans surveyed said they trusted online sources for COVID-19-related information, 13 but the effect of social media on COVID-19-related behaviors has not been studied in-depth.
The purpose of this study is to describe social media use among mobile phone owners in Uganda and assess the association between recent social media use and vaccination uptake. We also describe sociodemographic and health information source differences between mobile phone owners who use social media, those who do not, and nonmobile phone owners within a nationally representative sample of the population in Uganda.
Methods
Study design and participants
The 2020 Uganda Population-based HIV Impact Assessment Survey (UPHIA2020) served as the parent study for this phone survey. UPHIA2020 was a nationally representative household survey among adults 15 and older, conducted from February 2020 through March 2021 that focused on HIV-related outcomes. 15 The two-stage cluster design included 313 primary sampling units from 11 political regions, enrolling 95.7% (American Association for Public Opinion Research [AAPOR] Response Rate [RR] 4) 16 of eligible households (N = 10,527), from which 26,071 adults participated in an individual interview (94.2% AAPOR RR 4). All UPHIA2020 participants who completed the survey were asked if they agree to be contacted for future research. UPHIA2020 methods were aligned with previous PHIA survey approaches. 17
We included households on the sample frame that had at least one participant over 18 who completed the UPHIA2020 survey, consented to being contacted for future research, reported phone ownership, and spoke one of the seven survey languages [Ateso, English, Luganda, Lugbara, Luo, Runyankole-Rukiga, or Runyoro-Rutoro]. During the phone interview, for weighing purposes, the respondent had to report living in the same enumeration area where they participated in UPHIA2020.
We sampled the households using proportional allocation with the number of households per enumeration area as the measure of size. For enumeration areas with less than five households, we kept all the households in the sample.
The sampling approach was designed to address coverage error (difference between target population and sample frame)—in this case the difference between mobile phone owners and nonmobile phone owners.18,19 Specifically, UPHIA2020 participants who were phone owners were considered ‘primary respondents’. From among the selected households, one primary respondent was sampled. Next, in each sampled household, one ‘secondary respondent’ was randomly selected among all nonmobile phone owners listed during UPHIA2020. If there were no nonphone owners listed in the household, we asked the phone owner during the phone survey if there was anyone who did not own a mobile phone who slept in their household the past night who was the interviewer could approach about participating. Consenting secondary respondents participated after the primary respondent completed the survey and passed the phone to them. Anticipating noncontact, and refusals, we sampled twice the number (N = 1609) of primary respondents required for the survey.
Procedures
The questionnaire was adapted from other vaccine hesitancy 20 and social media engagement questionnaires. UPHIA2020 interviewers were recruited to administer the survey, working from both a central office and their homes, from March 7–27, 2022. Calls were placed throughout the day, with multiple calls placed within one day to a participant who did not answer the call, but a participant was rarely called on multiple days. To participate, respondents provided verbal consent and in return were offered $1 compensation for their time.
Measures
A current social media user was defined as a phone-owning participant who reported using any of the following social media sites in the past week, during the phone survey: Instagram, Facebook, Twitter, WhatsApp, or YouTube.
The outcome of interest, COVID-19 vaccination status, was measured via three questions during the phone survey. Anyone who reported receiving one dose of a single-dose vaccine or two doses of any other vaccine was considered fully vaccinated. For each dose reported, we asked for a date of vaccination.
We controlled for four variables. The first was location (urban or rural); as recorded during UPHIA2020. For the following three variables, sex (male or female); education (no formal education; primary; secondary; tertiary; and above); and age (18–24; 25–34; 35–44; and 45 and older), UPHIA2020 data were used for all primary and some secondary respondents. For secondary respondents not linked to UPHIA2020, we only used the phone survey data. For the multivariable logistic regression, we dichotomized education attainment as secondary education and higher and primary education and less.
Analyses
All primary and secondary respondents who completed the survey were included in the analytic sample. We describe the characteristics of all participants and characteristics of mobile phone owners who do not use social media, mobile phone owners who use social media, and nonmobile phone owners. COVID-19 knowledge is described among the aforementioned groups. The multivariable logistic regression model assessed the odds of being vaccinated between social media users and nonusers, adjusting for covariates noted above, comparing social media users with nonsocial media users (the latter group including mobile phone owners who do not use social media and people who do not own mobile phones).
All results include a 95% confidence interval using Taylor series linearization method weighting. Some sampled UPHIA2020 households did not meet the criteria for inclusion in the phone survey sample frame, that is, did not have any phone owners or did not have at least one phone owner that consented to follow-up. To account for these ineligible households, we treated their absence from the phone survey sample frame as an under-coverage issue, and we accounted for this using a nonresponse type of adjustment. A chi-square automatic interaction detection algorithm was used to adjust between the phone survey sample frame and UPHIA2020 population. The final adjusted household weights from UPHIA2020 were used to weight the data and new household weights for the phone survey were added to compensate for household unknown eligibility and nonresponse, along with adjustments for selection probability, nonresponse and post-stratification weights for both primary and secondary respondents. Analyses were conducted in STATA 15 and we determined statistical significance using an alpha of less than 0.05.
Results
Between March 7 and 27, 2022, 1055 participants enrolled, of whom 842 (79.8%) reported owning a mobile phone (primary respondents) and 213 (20.2%) reported not owning a phone (secondary respondents). Of 842 who owned a phone, 643 (76.4%) did not report any social media use in the past week, and 199 (23.6%) used social media in the past week. The response rate (AAPOR #2) among primary respondents was 62.7% and among secondary respondents was 55.0%. Mobile phone survey respondents were similar to all UPHIA2020 survey respondents in sex, education, and residence but were younger (18–24 overrepresented; 45 and older underrepresented).
Population characteristics are presented in Table 1. The median age was 32 years (interquartile range [IQR] 24–44), 53.3% were female, and 61.8% lived in rural settings. With regard to educational attainment, 7.1% had no formal education, 47.1% had primary, and 46.8% had secondary education or higher. Nonmobile phone owners were mainly female (68.2%), were on average younger (median age 24 years, IQR 20–33), were majority rural residents (91.6%), and only 4.9% reported tertiary education or higher. Compared to the population, mobile phone owners who did not report social media use were more likely to be older (36 years, IQR 27–48), rural residents (69.7%), and had similar education attainment. Social media users had a median age of 28 years (IQR 23–35), were 52.7% female, were majority urban residents (64.3%), and had higher educational attainment (39.4% tertiary education).
Table 1.
Characteristics of participants.
| Attribute | All respondents N (%) |
Nonmobile phone owners N (%) |
Mobile phone owner doesn’t use social media N (%) |
Mobile phone owner uses social media N (%) |
|---|---|---|---|---|
| N = 1.055 | N = 213 | N = 643 | N = 199 | |
| Age | ||||
| Median (IQR) | 32 (24, 44) | 24 (20, 32) | 36 (27, 48) | 28 (23, 35) |
| 18–24 | 303 (26.3) | 80 (50.0) | 75 (17.1) | 47 (32.9) |
| 25–34 | 334 (30.3) | 65 (26.7) | 195 (28.9) | 84 (38.0) |
| 35–44 | 233 (18.9) | 35 (11.0) | 161 (22.4) | 37 (15.2) |
| 45+ | 276 (24.5) | 33 (12.3) | 212 (31.6) | 31 (13.9) |
| Sex | ||||
| Male | 496 (46.8) | 64 (31.8) | 331 (50.6) | 102 (46.8) |
| Female | 559 (53.3) | 149 (68.2) | 312 (49.4) | 98 (52.2) |
| Education | ||||
| No formal education | 70 (7.1) | 18 (5.8) | 56 (8.2) | 3 (1.4) |
| Primary | 432 (47.1) | 105 (47.9) | 366 (56.4) | 38 (17.6) |
| Secondary | 271 (31.2) | 74 (41.4) | 172 (27.9) | 83 (41.0) |
| Tertiary | 124 (14.6) | 15 (4.9) | 49 (7.5) | 75 (40.0) |
| Geography | ||||
| Rural | 564 (61.8) | 152 (71.4) | 445 (68.2) | 68 (35.1) |
| Urban | 334 (38.2) | 61 (28.6) | 198 (31.8) | 131 (64.9) |
N is unweighted, % is weighted.
Types of social media used
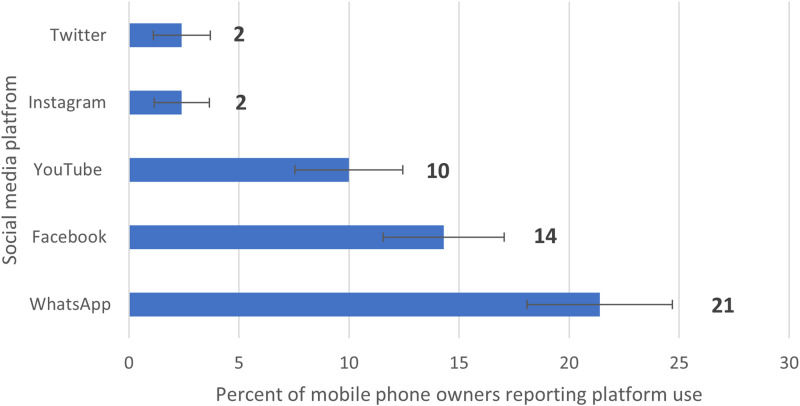
Among phone owners, 21.4% (95% confidence interval [CI] 18.3–24.9) reported using WhatsApp in the past week, 14.3% (95% CI 11.7–17.2%) used Facebook, and 10% (95% CI 7.9–12.8%) used YouTube. Less than 5% reported using Instagram or Twitter (see Figure 1).
Figure 1.
Percent of mobile phone owners using each social media site in the past week.
Among those who used social media in the past week, WhatsApp was used most frequently: 44.7% (95% CI 36.6–53.0%) reported daily use, 46.6% (95% CI 38.4–54.9%) a few days a week, and 8.7% (95% CI 5.0–14.8%) less than weekly (Table 2). Most Facebook users accessed the site only a few days during a week (66.6%, 95% CI 57.1–74.9%). YouTube, Instagram, and Twitter were also used most frequently only a few days during a week.
Table 2.
Frequency of social media use among those reporting social media use in the past week.
| Source | Using everyday N (%; 95% CI) |
Some days N (%; 95% CI) |
Once a week or less N (%; 95% CI) |
|---|---|---|---|
| 97 (44.7; 36.6–53.1) | 97 (46.6; 38.4–54.9) | 19 (8.74; 5.0–14.8) | |
| 37 (21.2; 14.7–29.7) | 84 (66.6; 57.2–74.9) | 15 (11.7; 6.8–19.3) | |
| YouTube | 32 (31.4; 21.1–43.8) | 57 (55.4; 43.3–66.7) | 12 (13.3; 6.6–25.1) |
N is unweighted, % is weighted.
The majority of (78.8%; 95% CI 71.1–84.9) social media users reported seeing mostly positive information (positive being defined by the respondent) about COVID-19 on any social media platform; 21.1% (95% CI 15.1–28.9) saw mostly negative (self-defined) information. There were no differences by sex, place of residence, or educational attainment with regard to seeing positive or negative information. Forty-three percent (95% CI 37.1–51.7) of social media users reported ever sharing positive or encouraging information about the COVID-19 vaccine on any platform, with more women (53.0%; 95% CI 42.8–62.9%) than men (34.8%; 95% CI 25.0–46.1%, p = 0.02) and more urban (48.6%; 95% CI 39.3–57.9%) than rural (32.0%; 95% CI 20.6–46.1%, p = 0.05) posting positive information. Only 14.2% (95% CI 9.4–20.8%) of social media users reported having ever posted negative or discouraging information about COVID-19 vaccine on any social media platform.
Sources and type of COVID-19 vaccine information
Among all participants, the most frequent source of COVID-19 vaccine information was radio (50.6%; 95% CI 46.6–54.7%), but whereas 55.3% (46.5–63.8%) of nonmobile phone owners and 55.9% (51.2–60.6%) of nonsocial media users cited radio, only 29.8% (22.6–38.3%) of social media users used radio as their main source (data not shown). Although television was the second most used source of COVID-19 vaccine information, more social media users reported television as a main source of information (27.5%, 95% CI 19.8–36.8%) compared to the other groups.
Overall, 60.8% (95% CI 57.02–64.5%) of participants had “ever seen or heard anything bad” in the community about COVID-19 vaccines (Table 3). Family (33.0%; 95% CI 29.4–37.0%), religious spaces (church or mosque, 17.4%; 14.4–21.0%), and social media (15.7%; 13.1–18.9%) were infrequent sources of negative COVID-19 vaccine information.
Table 3.
By mobile phone ownership and social media use, sources of vaccine information, sources of negative information and sources used to clarify COVID-19 vaccine information.
| Total population (all phone survey respondents) | Nonmobile phone owners | Mobile phone owner doesn't use social media | Mobile phone owner uses social medial | Weighted Pearson chi-square statistic** p-value for differential distribution of sources between nonphone owners, phone owners without social media use and social media users | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | p-value | |
| Percent using source for vaccine information | |||||
| TV | 430 (42.7) | 71 (35.2) | 224 (36.6) | 135 (68.6) | <0.001 |
| Newspaper | 205 (18.5) | 28 (12.9) | 115 (17.1) | 62 (28.3) | 0.00 |
| Radio | 905 (85.0) | 191 (90.1) | 546 (84.6) | 168 (81.7) | 0.13 |
| Internet | 181 (17.6) | 21 (10.2) | 38 (5.7) | 122 (61.4) | <0.001 |
| Social media | 221 (20.9) | 25 (11.2) | 46 (6.9) | 150 (73.3) | <0.001 |
| Friends or family | 783 (73.1) | 152 (71.5) | 483 (74.1) | 149 (71.5) | 0.73 |
| District task force | 566 (52.3) | 119 (51.6) | 354 (54.9) | 93 (44.9) | 0.09 |
| Traditional leader | 553 (51.8) | 107 (49.4) | 344 (52.5) | 102 (51.8) | 0.78 |
| Politicians | 800 (75.9) | 156 (72.8) | 517 (80.7) | 127 (63.7) | <0.001 |
| Health authorities | 901 (85.3) | 190 (86.8) | 559 (87.7) | 152 (76.3) | 0.01 |
| Percent who had seen or heard anything bad about COVID-19 from each source | |||||
| Social media | 158 (15.7) | 19 (9.5) | 34 (4.7) | 105 (55.8) | <0.001 |
| Church or mosque | 174 (17.4) | 21 (10.3) | 109 (17.8) | 44 (22.7) | 0.02 |
| Family | 336 (33.1) | 72 (37.2) | 188 (29.9) | 76 (39.0) | 0.06 |
| Community at large | 625 (60.8) | 126 (62.8) | 361 (57.0) | 138 (70.8) | 0.01 |
| Percent using each source to clarify unsure COVID-19 vaccine information | |||||
| Social media | 137 (13.4) | 17 (7.1) | 36 (5.6) | 115 (43.6) | <0.001 |
| Internet | 149 (13.8) | 22 (9.3) | 40 (5.8) | 87 (42.9) | <0.001 |
| Health worker | 923 (87.0) | 186 (86.6) | 566 (88.4) | 171 (82.9) | 0.22 |
| Family | 633 (67.9) | 139 (61.1) | 382 (59.9) | 112 (62.1) | 0.24 |
| Friends | 623 (60.0) | 126 (62.5) | 381 (60.2) | 116 (57.2) | 0.63 |
N is unweighted, % is weighted.
**Due to complex survey design, chi-2 tests were adjusted with Rao and Scott's first-order correction method.
Among all participants, health workers were most frequently cited (86.9% 95% CI 84.2–89.3%) as a source to access “when you hear information about the COVID-19 vaccine that you are not sure about.” Family and friends (62.1%; (95% CI 58.1–65.8%) and 60.0%; (56.3–63.6%)) were also commonly used sources of clarification. Among social media users, the frequency of use of health workers, family, and friends to clarify unclear information was the same as the overall population, but web-based platforms were an added source: 43.5% (36.7–51.2%) cited social media and 43.6% (36.4–51.1%) cited internet as sources to clarify COVID-19 vaccine information.
Association between social media use and COVID-19 vaccination
Overall, 62.0% (95% CI 58.4–65.5%) of participants reported being fully vaccinated against COVID-19 with no differences by mobile phone ownership or social media use associated with vaccination uptake. After adjusting for co-covariates, results from the multivariable logistic regression model indicated that social media use was not associated with self-reported COVID-19 vaccination status (odds ratio 1.05; 95% CI 0.67–1.63) (Table 4).
Table 4.
Adjusted odds of COVID-19 vaccination by key sociodemographic characteristics.
| Covariate | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Social media use | |||
| Yes vs No | 1.05 | 0.67–1.63 | 0.83 |
| Age group (18–24 reference) | |||
| 25–34 | 1.30 | 0.86–1.9 | 0.216 |
| 35–44 | 1.63 | 1.07–2.50 | 0.025 |
| 45+ | 1.75 | 1.1–2.7 | 0.015 |
| Location | |||
| Urban vs Rural | 0.63 | 0.45–0.88 | 0.008 |
| Education | |||
| Secondary & Above vs Primary and below | 1.64 | 1.15–2.34 | 0.006 |
| Gender | |||
| Male vs Female | 0.99 | 0.74–1.3 | 0.94 |
Discussion
This phone survey about social media use and COVID-19 vaccination among a randomly sampled nationally representative group in Uganda showed that despite a difference in sociodemographic profile and more frequently obtaining COVID-19 vaccination information from television and social media platforms, social media users had similar vaccination rates compared to nonusers. Social media users, of whom 73% cited social media platforms as a source of COVID-19 vaccine information, were younger, more educated and more urban than nonusers. However, social media users maintained person-based sources of information (such as health care workers and politicians) and continued to ask friends, family and health care workers to clarify unclear information.
WhatsApp was the most frequently used social media platform, with most users accessing it at least a few times a week or more. Social media users most frequently saw positive COVID-19 vaccine information online, and just under half had ever posted positive information about the COVID-19 vaccine themselves. Very few (14%) reported ever posting negative information.
Our findings that most of the population used radio and health authorities to obtain health information matches previous studies, including an Africa CDC survey about COVID-19 information sources conducted in 2021. 13 The finding that rural respondents were more likely to be vaccinated than urban respondents is not consistent with COVID-19 vaccination data available through nationals program in Uganda but is consistent with the pattern of childhood immunization uptake in Uganda, where rates are higher among rural populations.
The 2016–17 Uganda Demographic and Health Survey (DHS) found that overall, 9% of women and 23% of men aged 15–49 had used the Internet in the past 12 months. We estimate social media use (more specific than internet) among phone owners, and within the past week, and did not find a sex gap in utilization. This may be because the major barrier to social media and internet use is phone ownership, or it could be caused by differing time frame and denominator (i.e., comparing use between the population, as done by the DHS versus our estimate, only mobile phone owners).
In terms of the effect of social media on vaccine behavior in SSA, as previously mentioned, most existent research found social media had a deleterious impact on anticipated vaccine behavior.7–9 In Addis Ababa, in January 2021, social media, when cited as the primary source of information, was associated with vaccine hesitancy among a face-to-face sample, 7 and among youth in Nairobi, social media was the major source of information contributing to hesitancy. 9 A study of six countries in SSA that examined current masking behavior is one of the few articles that asked about current behavior in relation to social media use. The article noted that respondents using social media as their main source of information on COVID-19 had slightly greater odds of perceiving face masks as being effective in preventing COVID-19. 21
Our study is among the first to create population-based estimates of social media use in SSA and to link social media use to COVID-19 vaccination behavior. Existent research on social media's impact on health behavior intent has taken place in neighboring countries (Ethiopia, Kenya) but not in Uganda.
We also contribute to understanding which and how frequently social media platforms are used, information that is not readily available. The description of phone owners and those who use social media weekly can be used by public health practitioners to know who they may be able to reach through social media–based communication and interventions.
The study has several strengths such as using a probability sample from a known general population sampling frame. By sampling from a recent face-to-face general population survey in Uganda, we had access to over 200 questions about respondents to carefully examine for any error or bias and to create robust weights for analysis. Including nonphone owners (secondary respondents) is strength of our study, as it allows for the inclusion of nonphone owners making the survey more representative of the whole population. In contrast, previous studies have primarily been conducted via internet surveys. Sampling via the internet includes only those who have internet access, and as our results show, are a very different demographic group than noninternet users. We were able to compare three groups: phone owners who use social media, phone owners who do not use social media, and nonphone owners. Most existent articles do not have a nonsocial media use comparison group thus modeled the impact of social media differently. Finally, drawing conclusions about social media use among phone owners is a good fit between research question and sample population as internet is mainly accessed via mobile in SSA.
The study also has several limitations. Due to sample size limitations, the number of covariates we could include in the multivariable model was few. Although secondary respondents associated with UPHIA2020 were also chosen using probability sampling, secondary respondents who were not linked via UPHIA2020 were randomly chosen by the primary respondent, who may have introduced bias. We asked the primary respondent to pass the phone to the most proximate nonphone owner but this approach could have introduced systematic differences in respondent profile. Furthermore, given that sociodemographic characteristics cluster within households, a more ideal approach to including nonphone owners would have been to recruit from households without any phone owners. The nonphone owners who live in households are likely systematically different from nonphone owners in households without any phone owners. Next, there may have been social desirability bias to report being vaccinated and to underreport negative posting online on social media. Uganda is a less social media–engaged country than neighboring countries in East Africa so results cannot be generalized to the region. 13 Those who use social media are an elite group (highly educated, urban). The impact of social media use on health outcomes may become more profound as the population that uses social media becomes more diverse, especially educationally.
Continuing with limitations, the percentage of the sample that reported being vaccinated for COVID-19 was almost twice the actual rate reported by the Ministry of Health at that time. The overestimate of key health behaviors continues to plague mobile phone surveys in SSA,22,23 where mobile phone ownership continues to be concentrated among the privileged who have better health outcomes. Although our study overestimated population vaccination status, our main finding that social media use does not impact vaccination should not be impacted by the overestimate. This is because it is likely that 60% of mobile phone owners and those living in houses with mobile phone are vaccinated. Those living in households without mobile phones, who were not included in our study, are likely vaccinated at a lower rate. We compare vaccination status among those living in a household with a mobile phone and given our independent variable (social media use) is contingent on mobile phone ownership (social media use in SSA is predominantly through mobile devices), those who were excluded (who are more likely to be unvaccinated) have very little social media exposure. If people in homes without mobile phones were included in our study, making our point estimate of vaccination status more accurate, they would also likely attenuate the already insignificant association between social media use and vaccination status.
Conclusion
In summary, we found that social media use is not associated with COVID-19 vaccination uptake as reported by participants in this study in Uganda. We also found that historical sources of COVID-19 vaccine information, for example, radio, television, health care provider, are highly relevant to phone owners and nonowners alike. This should encourage continued efforts to disseminate information regarding COVID-19 vaccination through health workers, and radio spots to reach the population with accurate information regarding COVID-19 vaccines.
Footnotes
Contributorship: ARG conducted the literature search. ARG, ACB, DA, SB, VM, and JJ designed the study. Data collection was led by DA, with support from ARG, SB, and VM. Data analysis was conducted by MH, QC, and ARG. The manuscript was drafted by ARG and ACB. All coauthors reviewed the manuscript and provided input.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data sharing: Requests for access to data used for this analysis can be made by contacting the corresponding author. Key deidentified individual participant data collected during the phone survey, along with a data dictionary, is available upon request to the corresponding author, after approval of a proposal by the study core investigators with a signed data access agreement.
Ethical approval: The Uganda Virus Research Institute, Uganda National Council for Science and Technology Ethics Committees, and Columbia University Institutional Review Board approved the study.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the Calderone Junior Faculty Award, Mailman School of Public Health, Columbia University. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Guarantor: ARG.
ORCID iD: Abigail R Greenleaf https://orcid.org/0000-0002-8261-7025
References
- 1.Stewart R, Madonsela A, Tshabalala N, et al. The importance of social media users’ responses in tackling digital COVID-19 misinformation in Africa. Digital Health 2022; 8: 20552076221085070. 2022/03/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Betsch C, Renkewitz F, Betsch T, et al. The influence of vaccine-critical websites on perceiving vaccination risks. J Health Psychol 2010; 15: 446–455. 2010/03/30. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Ten threats to Global Health in 2019, https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (2019, accessed 9 December 2020).
- 4.Okeleke K, Suardi S. The mobile economy sub-Saharan Africa 2021. London, UK: GSM Association, 2021. [Google Scholar]
- 5.Munoz-Cobos D, Monzon Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low- and middle-income countries: a systematic review. Int J Public Health 2015; 60: 767–780. [DOI] [PubMed] [Google Scholar]
- 6.Cata-Preta BO, Wehrmeister FC, Santos TM, et al. Patterns in wealth-related inequalities in 86 low- and middle-income countries: global evidence on the emergence of vaccine hesitancy. Am J Prev Med 2020. 2020/11/03. DOI: 10.1016/j.amepre.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dereje N, Tesfaye A, Tamene B, et al. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-method study. BMJ Open 2022; 12: e052432. 2022/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lamptey E, Senkyire EK, Dorcas S, et al. Exploring the myths surrounding the COVID-19 vaccines in Africa: the study to investigate their impacts on acceptance using online survey and social media. Clin Exp Vaccine Res 2022; 11: 193–208. 2022/07/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Osur JO, Chengo R, Muinga E, et al. Determinants of COVID-19 vaccine behaviour intentions among the youth in Kenya: a cross-sectional study. Arch Public Health 2022; 80: 159. 2022/06/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landmark alliance launches in Africa to fight COVID-19 misinformation, https://africacdc.org/news-item/landmark-alliance-launches-in-africa-to-fight-covid-19-misinformation/ (2020, accessed 10 December 2020).
- 11.Uganda Bureau of Statistics (UBOS) and ICF.. Uganda Demographic and Health Survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF, 2018.
- 12.Okeleke K. Uganda: driving inclusive socio-economic progress through mobile-enabled . GSMA, 2019.
- 13.Africa CDC. COVID 19 Vaccine Perceptions: a 15 country study , 2021.
- 14.Kanyanda S, Markhof Y, Wollburg P, et al. Acceptance of COVID-19 vaccines in sub-Saharan Africa: evidence from six national phone surveys. BMJ Open 2021; 11: e055159. 2021/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uganda Population-based HIV impact assessment UPHIA 2020- 2021 Summary Sheet. Kampala, Uganda, 2022.
- 16.The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes. Washington, DC: AAPOR, 2016. [Google Scholar]
- 17.Sachathep K, Radin E, Hladik W, et al. Population-based HIV impact assessments survey methods, response, and quality in Zimbabwe, Malawi, and Zambia. J Acquir Immune Defic Syndr 2021; 87: S6–S16. 2021/06/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ambel A, McGee K, Tsegay A. Reducing bias in phone survey samples: effectiveness of reweighting techniques using face-to-face surveys as frames in four African Countrie. Washington, DC: World Bank, 2021. [Google Scholar]
- 19.Brubaker J, Kilic T, Wollburg P.Representativeness of individual-level data in COVID-19 phone surveys: findings from sub-Saharan Africa. PLoS One 2021; 16: e0258877. 2021/11/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larson HJ, Jarrett C, Schulz WS, et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine 2015; 33: 4165–4175. 2015/04/22. [DOI] [PubMed] [Google Scholar]
- 21.Iyamu I, Apantaku G, Yesufu Z, et al. Is social media, as a main source of information on COVID-19, associated with perceived effectiveness of face mask use? Findings from six sub-Saharan African countries. Glob Health Promot 2022: 17579759211065489. 2022/01/28. DOI: 10.1177/17579759211065489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lau C, Cronberg A, Marks L, et al. In search of the optimal mode for Mobile phone surveys in developing countries. A comparison of IVR, SMS, and CATI in Nigeria. Surv Res Methods 2019; 13: 305–318. [Google Scholar]
- 23.Greenleaf AR, Gadiaga A, Guiella G, et al. Comparability of modern contraceptive use estimates between a face-to-face survey and a cellphone survey among women in Burkina Faso. PLoS One 2020; 15: e0231819. 2020/05/14. [DOI] [PMC free article] [PubMed] [Google Scholar]