Abstract
One-third of students experience a mental health condition associated with decreased academic functioning and increased risk of dropping out. While mental health difficulties are lower among male students, they are twice as likely to die by suicide. Although the importance of gender-sensitive interventions for male students has been emphasized, feasible and effective approaches are unexplored. This investigation conducted three gender-sensitive feasibility interventions for male students to evaluate acceptability, changes to help-seeking and mental health outcomes. Three interventions were delivered to 24 male students. The interventions included the following: Intervention 1—a formal intervention targeting male students, Intervention 2—a formal intervention that adopted gender-sensitive language and promoted positive masculine traits, and Intervention 3—an informal drop-in offering a social space providing health information. These were evaluated for acceptability, attitudes to help-seeking, and mental health outcomes. All interventions were equally acceptable. The informal drop-in was more acceptable, having better engagement from male students who have greater conformity to maladaptive masculine traits, more negative attitudes to help-seeking, higher levels of self-stigma, who were less likely to have used mental health support before and belonged to an ethnic minority. These findings indicate differences in acceptability, particularly uptake, for hard-to-engage male students. Informal strategies help reach male students who would otherwise not engage with mental health support, familiarize them with help-seeking, and connect them with pre-existing mental health interventions. More work needs to be carried out using larger samples to investigate the efficacy of informal interventions to engage male students.
Keywords: help-seeking, interventions, service uptake, feasibility, mental health
Mental health disorders are commonly reported among university students with prevalence rates ranging from 20% to 30% (Bruffaerts et al., 2018; McManus & Gunnell, 2020). Common mental health disorders such as depression and anxiety often contribute to greater drop-out rates and reduced academic functioning (Auerbach et al., 2016; Bruffaerts et al., 2018; Eisenberg et al., 2007; Hjorth et al., 2016). Depression and anxiety occur more frequently among female students (Liu et al., 2019; McManus & Gunnell, 2020), yet male students are more than twice as likely to die by suicide (Gunnell et al., 2020). Indeed, higher suicide rates among male students has been observed since 2000 (Gunnell et al., 2020) and is consistent with older adults, where men are 2.35 times more likely to take their own life compared to women worldwide (Chang et al., 2019).
Higher suicide in male students may be attributable to them engaging with more lethal means to take their own life, reducing the opportunity for both prevention and intervention (Callanan & Davis, 2012; Mergl et al., 2015). This challenge is compounded further as higher suicide rates in male students can be further explained by lower engagement with mental health services compared to female students (Cadigan et al., 2019; Eisenberg et al., 2007; Pedrelli et al., 2016)—reducing the opportunity to provide suitable treatment or support. Gender is a significant predictor for receiving treatment, with male students being 2.32 and 2.52 times less likely to receive treatment compared to women or students who identify as a gender other than male or female, respectively (Seehuus et al., 2021). A meta-analysis of 27 studies by Schnyder et al. (2017) reports negative attitudes to help-seeking significantly reduce the likelihood of seeking help (OR = .80), with help-seeking attitudes consistently being reported lower in men and male students (Brenner et al., 2018; Clough et al., 2019; Wendt & Shafer, 2016). Indeed, this helps explain why suicide is higher in men despite them being less likely to have thoughts of taking their own life or presenting to hospitals for self-harm (Mental Health Foundation, 2016).
This disparity in service use is a complex process with a multitude of barriers negatively influencing mental health service engagement (Sagar-Ouriaghli, Godfrey, et al., 2020). Common barriers include, male students holding more negative attitudes to help-seeking (Clough et al., 2019; Nam et al., 2010), having greater conformity to traditional masculine norms (Ramaeker & Petrie, 2019; Seidler et al., 2016), reporting both higher public- and self-stigma (Levant et al., 2014; Wu et al., 2017), and poorer mental health literacy relative to their female counterparts (Clough et al., 2019; Haavik et al., 2017).
As conformity to masculine norms negatively influences help-seeking attitudes and behaviors among male students, it might act as a potential target area to elicit behavior change and improve help-seeking (Ramaeker & Petrie, 2019; Seidler et al., 2016; Vogel et al., 2011; Wimer & Levant, 2011). Research on positive masculinity suggests that general conformity to masculine norms may not be entirely detrimental. Conformity to specific traits such as emotional control, self-reliance, dominance, masculine toughness, and anti-femininity may well explain help-seeking reluctance (Gorski, 2010; Heath et al., 2017; Sileo & Kershaw, 2020; Wimer & Levant, 2011). Masculine traits such as winning, masculine status, and in some instances, risk-taking can also be protective factors, helping to reduce the likelihood of mental health problems, as well as improving the chances of help-seeking when needed (Heath et al., 2017; Iwamoto et al., 2018; Wong et al., 2017).
Published work between 2019 and 2022 emphasize the importance of gender-sensitive interventions for male students (Mackenzie et al., 2019; Ratnayake & Hyde, 2019; Sagar-Ouriaghli, Brown, et al., 2020; Schoen et al., 2019; Sileo & Kershaw, 2020). Certain interventions have been developed and tested. For example, “It’s a Goal!” targeted young men to promote positive mental health and prevent the development of serious mental health problems—demonstrating significant improvements in mental health measures (Spandler et al., 2013). HeadsUpGuys hosted a website with a range of psychoeducation, coping strategies and preventive advice for men with depression (HeadsUpGuys, n.d.). This intervention was not evaluated, but more than 65,000 men completed a depression self-assessment (Ogrondniczuk et al., 2018). ManTherapy is another website targeting men at risk of suicide and reluctant to seek help, leading to 59,894 mental health screenings and 19,586 people accessing crisis information (Man Therapy, n.d.; Spencer-Thomas et al., 2014). Help Out a Mate was tailored toward adolescent males aged 12 to 18, using a sports-based mental health literacy program to increase help-seeking intentions (Liddle et al., 2021). Those completing this intervention responded positively and saw improvements in mental health literacy, help-seeking attitudes and intentions to provide help (Liddle et al., 2021). Finally, the Real Men Real Depression was a national public campaign in the United States seeking to educate the public about depression in men from 2003 to 2005 (National Institute of Mental Health, n.d.). More than 14 million people were reached in this campaign, generating more than 5,000 emails and calls to information hotlines (Rochlen et al., 2005).
Indeed, male students may benefit from techniques and approaches that have been effective at improving help-seeking and mental health difficulties among older males. These include the delivery of psychoeducation materials, reframing help-seeking to align with masculine norms, and the use of male role models to convey information (Sagar-Ouriaghli et al., 2019). Other techniques reported in male-specific interventions include solution-focused approaches, sensitively sign-posting services, and the use of lay language and humor (American Psychological Association, Boys and Men Guidelines Group, 2018; Brown et al., 2019; Erentzen et al., 2018; Liddon et al., 2019; Patrick & Robertson, 2016; Sagar-Ouriaghli, Brown, et al., 2020; Sagar-Ouriaghli et al., 2019; Seidler et al., 2018; Yousaf et al., 2015).
As the recommendations for male-specific adaptations/approaches continue to grow, it is imperative that such recommendations are tested in the context of their feasibility. Here, a feasibility study can help investigators and future research prepare for a full-scale investigation (Bowen et al., 2009). Feasibility studies are relied on to produce a set of findings that inform whether an intervention should be investigated for efficacy testing (Bowen et al., 2009). They assess the feasibility of the steps needed to take place as part of a main study. Processes such as recruitment rates, retention rates, resources required, and insight into the management of a full trial can be tested (Thabane et al., 2010; Van Teijlingen & Hundley, 2001). Feasibility testing enables researchers to assess whether their ideas and approaches are acceptable, relevant, and sustainable to the population of interest. It is encouraged that feasibility studies are reported and published as they inform wider research in the same or similar field (Thabane et al., 2010). This helps with producing large-scale interventions that hold more external relevance, generalizability to a real-world setting, and thus, dissemination (Bowen et al., 2009; Van Teijlingen & Hundley, 2001).
Thus, this study aims to assess the feasibility of gender-sensitive interventions for male university students. By developing and testing the feasibility of interventions that are more gender-sensitive for the needs of male students, we can begin to clarify which approaches should be investigated further for efficacy testing. Here, we assess the feasibility by aiming to explore differences in male engagement and uptake to mental health initiatives. In turn, this may help to improve mental health outcomes for male students and subsequently reduce their elevated risk for suicide. The current investigation sought to assess three gender-sensitive mental health pilot interventions for male students by evaluating their differences in acceptability and feasibility. The aims were as follow:
To assess the overall acceptability and feasibility of the three interventions.
To assess differences in acceptability scores between the three interventions.
To examine the types of male students who engage with the three interventions, regarding their help-seeking attitudes, self-stigma, conformity to masculine norms, mental health status, ethnicity, previous help-seeking, age, level of study, and degree faculty.
To assess the interventions’ potential effectiveness for improving help-seeking attitudes, behaviors, and mental health status at post, 2-week, and 4-week follow-up for all three interventions to power future studies.
Method
Design
Descriptive statistics pertaining to self-stigma, conformity to masculine norms, mental health status, ethnicity, level of study, degree faculty, age, and previous help-seeking were used to analyze the types of students who engaged with the interventions. Feasibility was analyzed to explore whether a particular intervention was more or less acceptable to male students. Finally, a pre–post design was implemented to analyze changes in help-seeking attitudes, behaviors, and mental health status.
Measures
The measures within this investigation assessed the acceptability (including uptake) of each intervention to determine overall feasibility. In addition, conformity to masculine norms, self-stigma, mental health status, and help-seeking attitudes and behaviors were measured to explore any descriptive differences of the participants engaging with each gender-sensitive intervention.
Theoretical Framework of Acceptability Questionnaire
The Theoretical Framework of Acceptability Questionnaire (TFAQ) was used to evaluate the acceptability and feasibility of the interventions (Sekhon et al., 2018). The TFAQ contains nine items evaluating eight distinct domains that relate to acceptability including; general acceptability, affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness, and self-efficacy (Sekhon et al., 2017). Each domain includes one item except for perceived effectiveness where two items are included to capture the perceived effectiveness for help-seeking and mental health outcomes. All of the items are rated on a Likert-type scale ranging from 1 to 5, where higher scores indicate better acceptability. One item also provides a textbox allowing for participants to provide qualitative feedback. Items 3 and 8 (burden and opportunity costs) are reversed coded, where lower scores represent greater acceptability.
As intervention 3 (Man Cave) was an informal drop-in, the uptake, total number of students attending, and the number of students consenting was recorded to further evaluate acceptability.
Conformity to Masculine Norms Inventory and Self-Stigma of Seeking-Help Scale
The Conformity to Masculine Norms Inventory (CMNI-46) (Mahalik et al., 2003) and the Self-Stigma of Seeking-Help scale (SSOSH) (Vogel et al., 2006) were completed at baseline because conformity to masculine norms and self-stigma are barriers to help-seeking for male students (Levant et al., 2014; O’Brein et al., 2005; Ramaeker & Petrie, 2019; Seidler et al., 2016; Vogel et al., 2011; Wimer & Levant, 2011; Wu et al., 2017).
The CMNI-46 contains 46 items measuring the degree of conformity to nine traditional masculine norms, including winning, emotional control, primacy of work, risk-taking, violence, heterosexual self-presentation, playboy, self-reliance, and power over women (Mahalik et al., 2003; Parent & Moradi, 2011). Items are rated on a 4-point Likert-type scale from strongly disagree (0) to strongly agree (3), and a score for each domain can be calculated by taking the mean score of the respective items. A mean score across all items is used to generate a total conformity to masculine norms score, whereby higher scores represent greater conformity to masculine norms (Mahalik et al., 2003; Parent & Moradi, 2011). The CMNI-46 has good internal consistency (α = .78–.89) (Parent & Moradi, 2011).
The SSOSH scale includes 10 items rated on a 6-point Likert-type scale ranging from strongly disagree (0) to strongly agree (5). A total self-stigma score is obtained where higher scores indicate greater concern that seeking mental health support would negatively affect one’s satisfaction with oneself, self-confidence, and overall self-worth. The SSOSH scale has strong internal consistency (α = .86–.90) and moderate test–retest reliability (0.72) (Vogel et al., 2006).
Attitudes Seeking Professional Psychological Help Scale and the Actual Help-Seeking Questionnaire
To evaluate help-seeking attitudes and behaviors, the Attitudes Toward Seeking Professional Psychological Help Scale—Short Form (ATSPPH-SF) (Fischer & Farina, 1995) and the Actual Help-Seeking Questionnaire (AHSQ) (Rickwood et al., 2005; Wilson et al., 2005) were used. The ATSPPH-SF contains 10 items rated on a 4-point Likert-type scale ranging from disagree (0) to agree (3). A total score for mental health help-seeking attitudes is obtained, whereby higher scores represent more favorable help-seeking attitudes. The ATSPPH-SF has moderate internal consistency (α = .77–.84) and good test–retest reliability (0.80) (Elahi et al., 2008; Fischer & Farina, 1995). The AHSQ contains 10 items measuring behavioral help-seeking (e.g., presenting to a service or speaking to friends and family) in the past 2-weeks. The AHSQ has moderate internal consistency (α = .70–.85) and good test–retest reliability (.86–.92) (Wilson et al., 2005).
Warwick-Edinburgh Mental Well-Being Scale
Mental health status was measured via the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS), a 14-item questionnaire containing positively phrased items measuring positive affect, psychological functioning, and personal relationships. Items are rated on a 5-point Likert-type scale ranging from none of the time (0) to all of the time (5). Scores are summed with higher scores representing greater overall well-being (Tennant et al., 2007). The WEMWBS has been extensively validated in a student population (1,749, 44% male), demonstrating good internal consistency (α = .89) and test–retest reliability (0.83) (Tennant et al., 2007). The WEMWBS was chosen as traditional mental health scales such as the Beck Depression Inventory (BDI), Kessler’s Psychological Distress Scale (K10), and Patient Health Questionnaire (PHQ-9) have been reported to produce lower scores for men (Baillie, 2005; Kendel et al., 2010; Salokangas et al., 2002; Slade et al., 2011). Men often present with “male depressive symptoms,” including more somatic and atypical symptoms of depression, greater risk taking and excessive substance misuse which are not detected in traditional scales (Martin et al., 2013; Seidler et al., 2016).
The WEMWBS also places greater emphasis on positive mental health utilizing less medical terminology, that is, “I’ve been feeling good about myself” (Tennant et al., 2007). Indeed, much of the male help-seeking literature emphasizes the importance of using lay and informal language as it is deemed more acceptable by men (Men’s Health Forum, 2015; Patrick & Robertson, 2016; Pollard, 2016; River, 2018; Robertson et al., 2015; Seaton et al., 2019).
The ATSPPH-SF, AHSQ, and WEMWBS were completed at baseline for all interventions, postintervention for interventions 1 and 2, and at both 2-week and 4-week follow-up for all three interventions. Postintervention data for intervention 3 (Man Cave) was not collected due to the informal, drop-in nature of the intervention.
Interventions
Ethical approval was granted for each intervention by the King’s College London’s (study approval number: LRS-18/19-13460 and RESCM-19/20-13460) local Research Ethics Office with each participant providing written informed consent to participate. The content included within the three interventions was identified from a systematic review and focus groups conducted with male students (Sagar-Ouriaghli, Brown, et al., 2020; Sagar-Ouriaghli et al., 2019). A theoretical framework specifically tailored toward male students outlines the development of the interventions (Sagar-Ouriaghli, Godfrey, et al., 2020). Each intervention’s content was operationalised through the use of Behaviour Change Techniques (BCTs) (Michie et al., 2016, 2018). These BCTs are listed within a taxonomy (BCTTv1) outlining the active ingredients that promote behavior change, that is, help-seeking (Michie et al., 2013). Table 1 summarizes the intervention content, BCTs used, and practical application. By describing the development and active ingredients (i.e., BCTs) of each intervention, it enables other researchers or health care/education providers to replicate or build on the current findings. To further aid replication, a framework for developing interventions specifically for male students (Sagar-Ouriaghli, Godfrey, et al., 2020), the Template for Intervention Description and Replication (TIDieR) checklist (see supplementary appendix file 1) and the Consolidated Standards of Reporting Trials (CONSORT) extension statement for reporting pilot or feasibility trials (see supplementary appendix file 2) have been followed (Eldridge et al., 2016; Hoffman et al., 2014; Lancaster & Thabane, 2019).
Table 1.
Summary of the Intervention Content, BCTs, and the Delivery Method Across the Three Gender-Sensitive Interventions
| Intervention content | BCT(s) embedded within the intervention | Delivery method |
|---|---|---|
| Delivery of mental health information regarding depression, anxiety and alcohol misuse | 5.1. Information about health consequences 5.3. Information about social and environmental consequences 5.6. Information about emotional consequences |
Group presentation for interventions 1 and 2 outlining what mental health is, stressors at university, symptoms associated with excessive low mood, excessive worry, and excessive alcohol use. Highlighting how many symptoms and when their duration is cause for concern. Case study examples/vignette’s where students have to identify the symptoms. Intervention 3 included a leaflet about mental health symptoms, what they look like and when their duration is cause for concern. |
| Information on available mental health services, the treatment structure and its effectiveness | 3.2. Social support (practical) 5.1. Information about health consequences 5.3. Information about social and environmental consequences |
Listing different types of support in both interventions 1 and 2 including: friends and family, online support, university services, and professional services in the NHS. Emphasizing that they have the choice to engage with any service they feel is appropriate. Presentation of a “road map” regarding how long referrals, assessments, treatment duration, and the effectiveness of medication and cognitive behavioral therapy (CBT). Same information provided within a leaflet in intervention 3. |
| Use of videos and photos of male celebrities who have experienced mental health help-seeking | 6.2. Social comparison 9.1. Credible source |
Group discussion on photographs of male celebrities from a range of professions who have openly discussed issues relating to mental health (e.g., Prince William and UK rapper Stormzy) and a short video from YouTube where male celebrities talk about their mental health struggles (Interventions 1 and 2 only). |
| Emphasis placed on taking responsibility for your mental health | 3.2. Social support (practical) 13.2 Framing/Re-framing |
Interventions 1 and 2 included a presentation highlighting that taking responsibility and finding appropriate support is positive. Support can extend to friends, family, and professional support. Group discussion on why men find it difficult to ask for help. Intervention 2 and 3 labeled as “improving psychological strength for men” and “Man Cave” to align with male stereotypes. |
| Delivering a male-only space whilst facilitating social support | 3.1. Social support (unspecified) | Group based interventions specifically for male-students. Games console activity after interventions 1 and 2 as part of the honorarium given. Intervention 3 provided an informal drop in space to meet other male students by providing a series of social activities (games console, board games, arts and crafts, and table tennis). |
| Highlighting active problem-solving/self-help techniques such as problem-solving, mindfulness, time management and action planning | 1.2. Problem-solving 1.4. Action planning 11.2. Reduce negative emotions |
Interventions 1 and 2 includes information and practice activities for relaxation techniques (5-minute YouTube activity on mindfulness), solving a novel problem (e.g., how to make £1million in 6 months), time management (a case study/vignette on how to improve a student’s poor time management), and action planning where student’s identify 3 key problems and three potential solutions that can be completed in the next month. Intervention 2 had additional information about behavioral activation, how to identify negative cycles and patterns of behavior and how to change them as well as setting and monitoring goals. |
| Mental health self-assessment as part of a “self-check” to evaluate one’s current difficulties | 2.1 Monitoring of behavior by others without feedback 2.2. Feedback on behavior 2.3. Self-monitoring of behavior |
Completion of the Warwick-Edinburgh Menta Well-Being Scale (WEMWBS) as a “self-check” exercise for interventions 1 and 2. Repeated again in session 2, with the addition of calculating total scores and what “healthy” or average scores (i.e., 50) look like—if substantially lower participants were reminded of the content addressed such as finding support and self-help techniques. Intervention 3 included the WEMWBS as a “self-check” within a leaflet. |
Note. CBT = cognitive behavioral therapy; WEMWBS = Warwick-Edinburgh Mental Well-Being Scale.
In addition, focus group recommendations on how best to promote the interventions included: not to label them as a “mental health” intervention, to provide an incentive for attending, to promote through student-led societies, and to deliver such initiatives during orientation week and exams (Sagar-Ouriaghli, Brown, et al., 2020).
Recruitment for each intervention lasted a duration of 4 weeks. All three interventions were delivered face-to-face by a PhD student (ISO, male) with the support of a medical student (VT, male).
Intervention 1: Men-Tality
Intervention 1 was promoted during orientation week at the university welcome fair where university societies can show-case extra-curricular activities (Sagar-Ouriaghli, Brown, et al., 2020). In addition, posters and the fortnightly university e-mail circular were used to promote the intervention.
Intervention 1 was a psycho-educational intervention designed to improve knowledge of mental health problems, self-help techniques, and available help/support. It was delivered in a room located in the student union and was divided into two 2-hour group sessions. In session 1, information on mental health symptoms (depression, anxiety, and alcohol misuse) and how to recognize them, available mental health services, treatment structure, treatment effectiveness, videos/photos of male celebrities who have experienced mental health difficulties to frame help-seeking within a masculine narrative, and greater emphasis placed on taking responsibility for your mental health were addressed (Table 1). The following week, in session 2, a video of male celebrities discussing mental health difficulties and help-seeking was viewed before exploring a range of skills including problem-solving, mindfulness, time management, and action planning. Finally, a mental health self-assessment (i.e., WEMWBS) was completed individually for students to do a “self-check” within the session. Responses were used to privately evaluate one’s current difficulties and participants were reminded of the available services and self-management techniques that were addressed in sessions 1 and 2 (Table 1).
Intervention 2: Psychological Strength for Men
Intervention 2 was titled “Improving Psychological Strength for Men” to provide a more “positive masculine” image, enabling male students to engage with a mental health intervention. The aim and content embedded within intervention 2 focused more on problem-solving and solution focused techniques—discussing them in the first session, while placing greater emphasis on positive masculine stereotypes (e.g., responsibility and psychological strength) (Table 1). As before, mental health labels were deliberately avoided to help engage more male students (Sagar-Ouriaghli, Brown, et al., 2020). The phrasing of “psychological” was chosen to avoid mental health–related terms, and information relating to depression, anxiety, and alcohol misuse were labeled as “low mood,” “worries/stress,” and “excessive drinking,” respectively. Posters and the fortnightly e-mail circular were used to promote the intervention.
Intervention 2 was also divided into two 2-hour group sessions. Session 1 focused on skills such as behavioral-activation, action planning, mindfulness, goal setting and monitoring, problem-solving, and time management techniques. The following week, session 2 emphasized one’s responsibility to look after their mental health before providing information around available mental health services, identifying mental health symptoms, treatment structure, and treatment effectiveness (Table 1). Finally, mental health self-assessments (i.e., WEMBWS) were completed to obtain personal feedback about their current mental health status (Table 1).
Intervention 3: Man Cave
Intervention 3 was informal and offered a group drop-in for male students. It was based on previous focus group results, indicating that male students have a preference for informal and fun settings (Sagar-Ouriaghli, Brown, et al., 2020). Intervention 3 was titled “Man Cave” to emphasize a male-only group and was hosted on the ground floor within the student union in close proximity to the student café. This ensured a more opportunistic setting, unlike interventions 1 and 2 where pre-registration/sign-up was required. As before, intervention 3 was advertised via posters and across the fortnightly e-mail circular.
Intervention content was delivered through leaflets distributed within the room, which could be discretely collected. Two researchers (ISO and VT) were available to answer questions. Specially adapted leaflets containing information about available mental health services, mental health symptoms, and a self-assessment scale (i.e., WEMBWS) were provided. Additional leaflets addressing physical health, local doctor’s surgeries, smoking cessation, and university gyms were provided (Table 1). Various social activities such as board games, video gaming, table tennis, and snacks were stationed around the room to shift the focus away from mental health with the intention to be more inviting (Table 1). Drop-in sessions ran weekly for 4 hours over 4 weeks. Students were free to attend for any time period and attend as many sessions as they liked.
Results
Participants
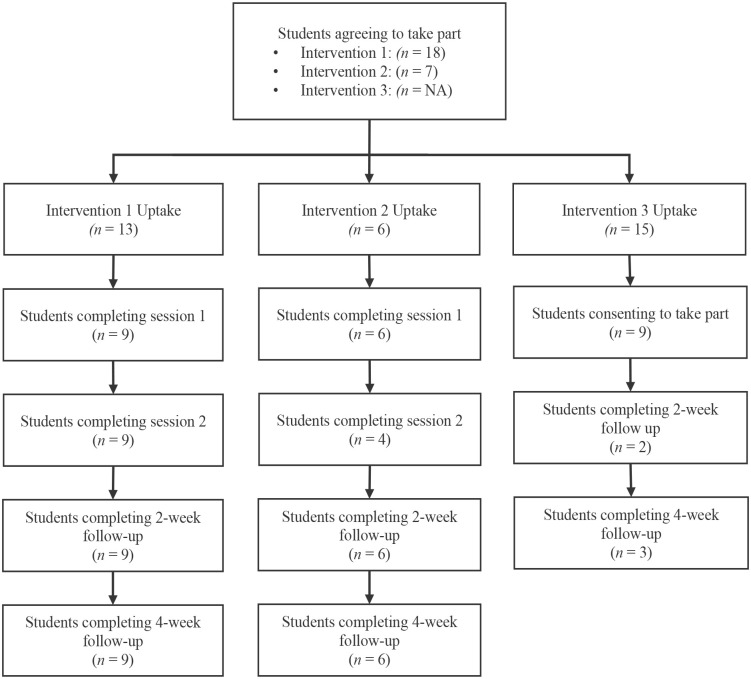
Across the three pilot interventions, 24 male students were recruited. For participants to be eligible to participate, they had to identify as male as well as be a student (undergraduate or postgraduate). A total of 126 students expressed interest in intervention 1 (Men-Tality) and provided contact details to a member of the research team at the welcome fair. An additional 23 students responded to the poster/e-mail invitation. Of the 149 male students expressing interest in intervention 1, nine students attended and completed the intervention. Owing to logistical restrictions and to prevent students from engaging in both interventions simultaneously, interventions 2 (Psychological Strength) and 3 (Man Cave) were promoted later within the academic year and were not advertised during welcome fair. Twenty-two students expressed interest in intervention 2, with six attending the intervention where all completed 4-week follow. For intervention 3, 15 students expressed interest, with nine consenting to take part and 3 completing 4-week follow-up. Within intervention 3, only one student completed both 2-week and 4-week follow-up. A summary of students agreeing to take part, uptake, and completion rates is depicted in Figure 1. Demographic information of the 24 participants split by each intervention is outlined in Table 2.
Figure 1.
Recruitment Flow Chart Across All Three Pilot Interventions
Table 2.
Summary of Participants Demographics Split by Intervention
| Demographic | Intervention 1 (Men-Tality) | Intervention 2 (Psych strength) | Intervention 3 (Man Cave) | Total |
|---|---|---|---|---|
| n (% male) | 9 (100%) | 6 (100%) | 9 (100%) | 24 (100%) |
| Mean age in years (SD) | 25.44 (8.71) | 25.50 (4.51) | 22.11 (4.81) | 24.21 (6.45) |
| Ethnicity | ||||
| Other White background | 4 (44%) | 4 (66%) | 0 (0%) | 8 (34%) |
| Pakistani | 0 (0%) | 1 (17%) | 4 (44%) | 5 (22%) |
| Black African | 0 (0%) | 0 (0%) | 2 (22%) | 2 (8%) |
| White British | 1 (11%) | 0 (0%) | 1 (11%) | 2 (8%) |
| Chinese | 1 (11%) | 0 (0%) | 0 (0%) | 1 (4%) |
| Indian | 1 (11%) | 0 (0%) | 0 (0%) | 1 (4%) |
| Bangladeshi | 0 (0%) | 0 (0%) | 1 (11%) | 1 (4%) |
| Mixed White and Black Caribbean | 0 (0%) | 1 (17%) | 0 (0%) | 1 (4%) |
| Other Asian Background | 1 (11%) | 0 (0%) | 0 (0%) | 1 (4%) |
| Any other background | 1 (11%) | 0 (0%) | 1 (11%) | 2 (8%) |
| Degree faculty | ||||
| Natural and mathematical sciences | 3 (33%) | 2 (33%) | 8 (89%) | 13 (55%) |
| Social sciences and public policy | 2 (22%) | 2 (33%) | 0 (0%) | 4 (16%) |
| Arts and humanities | 1 (11%) | 1 (17%) | 1 (11%) | 3 (13%) |
| Psychiatry, psychology, and neuroscience | 2 (22%) | 0 (0%) | 0 (0%) | 2 (8%) |
| Life science and medicine | 0 (0%) | 1 (17%) | 0 (0%) | 1 (4%) |
| School of law | 1 (11%) | 0 (0%) | 0 (0%) | 1 (4%) |
| Level of study | ||||
| Undergraduate | 4 (44%) | 1 (17%) | 7 (78%) | 12 (50%) |
| Postgraduate (Masters or PhD) | 5 (56%) | 5 (83%) | 2 (22%) | 12 (50%) |
| Has previously sought help for mental health | ||||
| Yes | 4 (44%) | 5 (83%) | 2 (22%) | 11 (46%) |
| No | 4 (44%) | 0 (0%) | 6 (67%) | 10 (41%) |
| Prefer not to say | 1 (11%) | 1 (17%) | 1 (11%) | 3 (13%) |
Aim 1: To Assess the Overall Acceptability and Feasibility for All Three Interventions
Mean (SD) scores for all acceptability domains (general acceptability, affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness, and self-efficacy) are summarized in Table 4. All three interventions were rated favorably regarding their overall acceptability with 76% (n = 13) rating the intervention as “acceptable” and 24% (n = 4) rating the intervention as “completely acceptable.” Similarly, 82% (n = 14) of participants either “liked” or “strongly liked” their respective intervention, while only 18% (n = 3) had “no opinion.” When asked how much the intervention aligned with their beliefs about mental health and help-seeking (ethicality), 88% (n = 15) were in “agreement” or “strong agreement,” 6% (n = 1) had “no opinion,” while 6% (n = 1) “disagreed.” Participants were asked whether the intervention improved their overall mental health/well-being and their attitudes toward seeking help (perceived effectiveness). For overall mental health/well-being, 47% (n = 8) “agreed,” 35% (n = 6) had “no opinion” and 18% (n = 3) “disagreed.” For attitudes toward seeking help, 65% (n = 11) either “agreed” or “strongly agreed,” while 35% (n = 6) had “no opinion.” When asked whether it was clear how engaging in the intervention helped to manage their mental health (intervention coherence), 76% (n = 13) “agreed” or “strongly agreed” that it was clear and 24% (n = 4) had “no opinion.” In addition, two negatively phrased items sought to identify how much effort it took to engage (burden) and how much engaging interfered with other priorities (opportunity costs). 65% (n = 11) felt engaging took “very little effort” or “no effort at all,” 18% (n = 3) had “no opinion,” 12% (n = 2) took “a lot of effort” and 6% (n = 1) required a “huge effort.” When asked whether the intervention interfered with their other priorities, 76% (n = 13) “disagreed” or “strongly disagreed” and 24% (n = 4) had “no opinion.” Finally, participants were asked how confident they would feel about engaging with the intervention again (self-efficacy), 71% (n = 12) felt “confident” or “very confident” about engaging again, while 29% (n = 5) had “no opinion.” The final question included within the TFAQ captures general feedback obtained through a written text box. Twelve of the 17 participants completing the TFAQ provided qualitative feedback (Table 3).
Table 4.
Summary of Means, SD and One-Way ANOVA for All Interventions Scores for Acceptability
| TFAQ domain | M (SD) | One-way ANOVA between the three pilot interventions | |||||
|---|---|---|---|---|---|---|---|
| Intervention 1 (Men-Tality) | Intervention 2 (Psych strength) | Intervention 3 (Man Cave) | F | df | Error | p | |
| Acceptability | 4.78 (0.44) | 4.75 (0.50) | 4.75 (0.50) | .01 | 2 | 14 | .993 |
| Affective attitude | 4.11 (0.78) | 4.50 (0.58) | 4.25 (0.96) | .34 | 2 | 14 | .717 |
| Burden a | 2.11 (1.17) | 2.25 (0.96) | 3.25 (0.96) | 1.59 | 2 | 14 | .238 |
| Ethicality | 4.33 (0.71) | 4.25 (0.50) | 3.50 (1.00) | 1.82 | 2 | 14 | .198 |
| Intervention coherence (help-seeking) | 4.22 (0.67) | 3.75 (0.50) | 3.75 (0.96) | .94 | 2 | 14 | .415 |
| Opportunity costs a | 2.00 (0.71) | 1.75 (0.96) | 1.75 (0.96) | .20 | 2 | 14 | .825 |
| Perceived effectiveness (help-seeking) | 4.00 (0.71) | 4.00 (0.82) | 3.25 (0.50) | 1.78 | 2 | 14 | .204 |
| Perceived effectiveness (mental health) | 3.44 (0.73) | 3.00 (1.15) | 3.25 (0.50) | .44 | 2 | 14 | .656 |
| Self-efficacy | 3.89 (0.60) | 3.75 (0.96) | 4.00 (0.82) | .12 | 2 | 14 | .892 |
Note. TFAQ = Theoretical Framework of Acceptability Questionnaire.
Items are reverse coded, and lower scores indicate better acceptability.
Table 3.
Qualitative Feedback Obtained From the TFAQ
| Intervention | Comment |
|---|---|
| Intervention 1: Men-Tality | “I only hope that more people would participate in this, as mental well-being is often neglected” |
| “Good overview of mental health issues and ways to cope and where to get help” | |
| “I found it enjoyable, FIFA is a great way to get people together” | |
| “Although I can see how some of the strategies discussed may help some people, in my case they seem unlikely to work” | |
| “Was useful, learnt new techniques, forced me to reflect more on my own wellbeing” | |
| “Would have been useful to go through ways of ‘nudging’ us to do beneficial activities for mental health so they become a habit” | |
| “To take care of yourself is taking care of your mental health. This is the first and most important step to begin with if you want to improve” | |
| Intervention 2: Psychological strength for men | “Not sure that 2x2 hour workshop brings big changes, but the atmosphere was good” |
| “Very good overall” | |
| Intervention 3: Man Cave | “I had only come for one session, so perhaps I most likely wasn’t able to benefit too much as far as mental health is concerned but I certainly did leave happier after my session” |
| “I didn’t know how I could have engaged more beyond my lengthy discussion with one of the organisers, apart from that I was too tentative to get involved” | |
| “I have no strong opinions. I feel it may be useful for some more vulnerable guys, but I believe men should be able to deal with their problems themselves and these kinds of things don’t appeal to most men” |
Note. TFAQ = Theoretical Framework of Acceptability Questionnaire.
Aim 2: To Assess Differences in Acceptability Scores Between the Interventions
As indicated by a series of one-way analyses of variance (ANOVAs), no significant differences were observed for all the domains on the TFAQ (overall acceptability, affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness, and self-efficacy) (Table 4).
Aim 3: To Examine the Types of Male Students Who Engage With the Interventions Regarding Their Help-Seeking Attitudes, Self-Stigma, Conformity to Masculine Norms, Mental Health Status, Ethnicity, Previous Help-Seeking, Age, Level of Study, and Degree Faculty
Baseline Help-Seeking Attitudes
Across the three interventions, help-seeking attitudes (ATSPPH-SF) were significantly different at baseline (Table 5). A Bonferroni post hoc test revealed that help-seeking attitudes were significantly lower for intervention 3 when compared to intervention 1, t(16) = 7.22, p = .006, 95% confidence interval (CI): (1.09–12.55). No significant differences were observed between interventions 1 and 2, t(13) = 2.44, p = .892, 95% CI (–3.51 to 8.40), or between intervention 2 and 3, t(13) = 4.78, p = .147, 95% CI (–1.17 to 10.73).
Table 5.
Summary of Means, SD and One-Way ANOVA for All Intervention’s Baseline Scores for Help-Seeking Attitudes, Mental Health Status, Self-Stigma, and Conformity to Masculine Norms
| Scale | M (SD) | One-way ANOVA between the three pilot interventions | ||||||
|---|---|---|---|---|---|---|---|---|
| Intervention 1 (Men-Tality) | Intervention 2 (Psych strength) | Intervention 3 (Man Cave) | Male student norms | F | df | Error | p | |
| Baseline help-seeking attitudes (ATSPPH-SF) | 21.44 (4.25) | 19.00 (3.29) | 14.22 (5.29) | 15.90 (5.44) | 6.39 | 2 | 21 | .007* |
| Baseline mental health status (WEMWBS) | 50.44 (7.68) | 43.00 (13.31) | 46.89 (13.07) | 49.14 (7.87) | .83 | 2 | 21 | .451 |
| Baseline self-stigma (SSOSH) | 22.56 (5.03) | 20.33 (6.44) | 26.00 (8.96) | 27.10 (7.70) | 1.26 | 2 | 20 | .306 |
| Baseline conformity to masculine norms (CMNI-46) | ||||||||
| Total | 1.11 (0.23) | 1.36 (0.34) | 1.42 (0.44) | 1.51 (0.25) | 2.07 | 2 | 21 | .152 |
| Emotional control | 1.15 (0.60) | 0.97 (0.87) | 1.46 (0.66) | 1.45 (0.54) | 1.01 | 2 | 21 | .381 |
| Winning | 1.37 (0.43) | 2.14 (0.62) | 1.54 (0.38) | 1.66 (0.45) | 5.33 | 2 | 21 | .013* |
| Playboy | 1.08 (0.43) | 1.29 (0.75) | 1.44 (0.68) | 1.28 (0.65) | .78 | 2 | 21 | .470 |
| Violence | 1.43 (0.55) | 1.61 (0.64) | 1.41 (0.80) | 1.84 (0.49) | .20 | 2 | 21 | .823 |
| Self-reliance | 1.04 (0.44) | 1.43 (0.94) | 1.37 (0.88) | 1.33 (0.49) | .65 | 2 | 21 | .532 |
| Risk taking | 1.36 (0.53) | 1.27 (0.84) | 1.49 (0.41) | 1.45 (0.46) | .28 | 2 | 21 | .761 |
| Power over women | 0.42 (0.41) | 0.63 (0.44) | 0.89 (1.11) | 1.07 (0.57) | .75 | 2 | 21 | .486 |
| Primacy of work | 1.22 (0.67) | 1.63 (0.74) | 1.20 (0.36) | 1.36 (0.54) | 1.08 | 2 | 21 | .357 |
| Heterosexual self-preservation | 0.74 (0.50) | 1.06 (0.62) | 1.76 (0.88) | 1.80 (0.66) | 4.79 | 2 | 21 | .007* |
Note. ATSPPH-SF = Attitudes Toward Seeking Professional Psychological Help Scale—Short Form; WEMWBS = Warwick-Edinburgh Mental Well-Being Scale; CMNI-46 = Conformity to Masculine Norms Inventory; SSOSH = Self-Stigma of Seeking-Help scale.
p < .05.
When comparing help-seeking attitudes at baseline to male student norms in previous research (Elahi et al., 2008), participants in intervention 1 had significantly more positive help-seeking attitudes, t(8) = 3.917, p = .004, 95% CI (2.28–8.81), d = 1.13. No significant differences for help-seeking attitudes were observed for intervention 2, t(5) = 2.311, p = .069, 95% CI (–.35 to 6.55), d = .69, or intervention 3, t(8) = 1.013, p = .341, 95% CI (–5.05 to 2.14), d = .31, when compared to male student norms (Elahi et al., 2008).
Baseline Self-Stigma
Upon visual inspection, baseline self-stigma appeared lower for both interventions 1 and 2 when compared to intervention 3. However, this difference was not significant (Table 5). When compared to male student norms outlined in previous research, a one-sample t-test showed that baseline self-stigma for intervention 1 was significantly lower than male student norms (Vogel et al., 2006), t(8) = 2.71, p = .027, 95% CI (–8.41 to –.68), d = .70. This was also apparent for intervention 2 when compared to male student norms, t(5) = 2.57, p = .050, 95% CI (–13.52 to –.01), d = .95. However, for intervention 3, baseline self-stigma was not significantly different to the male student norms, t(7) = .37, p = .726, 95% CI (–8.24 to 6.04), d = .13.
Baseline Conformity to Masculine Norms
Across the three interventions, only the domains of winning and heterosexual self-preservation revealed significant differences (Table 5). Employing the Bonferroni post hoc test, winning was significantly higher for intervention 2 when compared to intervention 1, t(13) = .769, p = .013, 95% CI (–1.40 to –.43). However, there were no significant differences for winning between interventions 1 and 3, t(16) = .175, p = 1.00, 95% CI (–.74 to .39), or between intervention 2 and 3, t(13) = .59, p = .067, 95% CI (–.03 to 1.22).
Similarly, the Bonferroni post hoc test for heterosexual self-preservation revealed this to be significantly higher for intervention 3 when compared to intervention 1, t(16) = 1.02, p = .019, 95% CI (–1.90 to –.15). There were no significant differences for heterosexual self-preservation between interventions 1 and 2, t(13) = .32, p = 1.00, 95% CI (–1.30 to –.66), or between interventions 2 and 3, t(13) = .71, p = .223, 95% CI (–1.69 to .27).
When comparing conformity to masculine norms with male student norms as highlighted in previous research (Parent & Moradi, 2011), those attending intervention 1 scored significantly lower on total conformity to masculine norms, t(8) = 5.102, p = .001, 95% CI (–.581 to –.219), d = 1.67, power over women, t(8) = 4.728, p = .001, 95% CI (–.972 to –.335), d = 1.31, and heterosexual self-preservation t(8) = 6.340, p < .001, 95% CI (–1.445 to –.674), d = 1.81. No significant differences were observed for emotional control, winning, playboy, violence, self-reliance, risk taking, and primacy of work when comparing intervention 1 to male student norms.
For those attending intervention 2, scores for heterosexual self-preservation were significantly lower compared to male student norms, t(5) = 2.933, p = .033, 95% CI (–1.395 to –.092), d = 1.16. All other domains of, total conformity to masculine norms, emotional control, winning, playboy, violence, self-reliance, risk-taking, power over women, and primacy of work did not differ significantly to male student norms. Finally, participants attending intervention 3 did not have any significant differences across all domains when compared to male student norms.
Baseline Mental Health Status
Mental health status (WEMWBS) did not differ significantly at baseline between the three interventions (Table 5). Mental health status at baseline for intervention 1 did not differ significantly from male student’s norms as highlighted in previous research (Tennant et al., 2007), t(8) = .509, p = .624, 95% CI (–4.60 to 7.21), d = .17. This was also observed for intervention 2, t(5) = 1.130, p = .310, 95% CI (–20.11 to 7.83), d = .56, and intervention 3, t(8) = .551, p = .597, 95% CI (–11.67 to 7.17), d = .21.
Ethnicity, Previous Help-Seeking, Age, Level of Study, and Degree Faculty at Baseline
Of the participants engaging within the three interventions, significant differences were observed for ethnicity, whereby intervention 3 engaged more ethnic minorities: Fisher’s Exact, p = .021, Cramer’s V = .707 and for those who have previously sought help for mental health compared to those who have not: Fisher’s Exact, p = .038, Cramer’s V = .58. No significant differences were observed for age as confirmed by a one-way ANOVA: F(2, 21) = .745, p = .487. Finally, Fisher’s exact test revealed no significant differences between the interventions for level of study (p = .089) or degree faculty (p = .106).
Aim 4: To Assess the Interventions’ Potential Effectiveness for Improving Help-Seeking Attitudes, Behaviors, and Mental Health Status at Post, 2-Week, and 4-Week Follow-Up for All Three Interventions to Power Future Studies
Postintervention Changes to Help-Seeking Attitudes & Behaviours
Certainly, the primary aim for feasibility studies should be to assess feasibility and acceptability (Thabane et al., 2010). Nonetheless, despite the small sample sizes, an exploratory analysis was conducted to examine changes to help-seeking attitudes and behaviors at follow-up. For interventions 1 and 2, no significant changes in help-seeking attitudes were observed at postintervention, 2-week follow-up, or 4-week follow-up when compared to baseline (Table 7). Similarly, no significant changes to help-seeking attitudes were observed in intervention 3 for 2-week follow-up or 4-week follow-up when compared to baseline (Table 7).
Table 7.
Summary of Means (SD) and Test for Significance (t-tests) for Post-, 2-Week, and 4-Week Follow-Up Change in Scores for Help-Seeking Attitudes and Mental Health Status
| Intervention | M (SD) | |||
|---|---|---|---|---|
| Baseline | Post | 2-week follow-up | 4-week follow-up | |
| Help-seeking attitudes (ATSPPH-SF) | ||||
| Intervention 1 (Men-Tality) | 21.44 (4.25) | 22.11 (3.95) | 21.11 (4.17) | 22.44 (3.81) |
| Intervention 2 (Psych strength) | 19.00 (3.29) | 19.33 (5.69) | 20.83 (4.62) | 20.67 (5.20) |
| Intervention 3 (Man Cave) | 14.22 (5.29) | — | 20.00 (8.49) | 14.67 (12.66) |
| Mental health status (WEMWBS) | ||||
| Intervention 1 (Men-Tality) | 50.44 (7.68) | 49.67 (7.78) | 48.67 (7.86) | 49.89 (9.78) |
| Intervention 2 (Psych strength) | 43.00 (13.31) | 32.67 (7.37) | 44.67 (8.19) | 44.33 (9.35) |
| Intervention 3 (Man Cave) | 46.89 (13.07) | — | 46.00 (22.63) | 53.67 (12.90) |
Note. All comparisons are made with Baseline as the reference group. ATSPPH-SF = Attitudes Toward Seeking Professional Psychological Help Scale—Short Form; WEMWBS = Warwick-Edinburgh Mental Well-Being Scale.
With regards to help-seeking behaviors occurring in the past 2 weeks captured by the AHSQ, more than half (50%) of participants completing the questionnaire sought help at any time point (i.e., baseline, postintervention, 2-week follow-up, 4-week follow-up) from at least 1 source (Table 6). Only a positive increase in students seeking help in the past 2 weeks was observed for intervention 1 at post follow-up (+11%) (Table 6).
Table 6.
Frequency and Percentages of Where Participants Sought Help in the Last 2 Weeks at Baseline, Post, 2-Week Follow-Up and 4-Week Follow-Up for All Interventions
| Intervention 1 (Men-Tality) | Intervention 2 (Psych strength) | Intervention 3 (Man Cave) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Timepoint | Baseline | Post | 2WFU | 4WFU | Baseline | Post | 2WFU | 4WFU | Baseline | Post | 2WFU | 4WFU |
| n total | 9 | 9 | 9 | 9 | 6 | 3 | 6 | 6 | 9 | 0 | 2 | 3 |
| Partner | 22% (2) | 22% (2) | 22% (2) | 11% (1) | 50% (3) | 33% (1) | 67% (4) | 67% (4) | 11% (1) | — | 0% (0) | 0% (0) |
| Friend | 44% (4) | 67% (6) | 67% (6) | 44% (4) | 100% (6) | 67% (2) | 83% (5) | 83% (5) | 33% (1) | — | 100% (2) | 67% (2) |
| Parent | 22% (2) | 22% (2) | 33% (3) | 22% (2) | 67% (4) | 33% (1) | 50% (3) | 67% (4) | 44% (4) | — | 100% (2) | 0% (0) |
| Other relative | 11% (1) | 11% (1) | 11% (1) | 11% (1) | 33% (2) | 0% (0) | 67% (4) | 33% (2) | 0% (0) | — | 0% (0) | 33% (1) |
| Mental health professional | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 17% (1) | 33% (1) | 0% (0) | 33% (2) | 11% (1) | — | 0% (0) | 0% (0) |
| Phone help line | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | — | 0% (0) | 0% (0) |
| Doctor/GP | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 0% (0) | 33% (1) | 0% (0) | 0% (0) | 11% (1) | — | 0% (0) | 0% (0) |
| Teacher | 33% (3) | 33% (3) | 11% (1) | 0% (0) | 17% (1) | 0% (0) | 33% (2) | 17% (1) | 22% (2) | — | 0% (0) | 0% (0) |
| Other | 0 (0) | 0% (0) | 0% (0) | 11% (1) | 17% (1) | 33% (1) | 0% (0) | 17% (1) | 11% (1) | — | 50% (1) | 0% (0) |
| Not sought help | 11% (1) | 0% (0) | 22% (2) | 44% (4) | 0% (0) | 33% (1) | 0% (0) | 17% (1) | 33% (3) | — | 0% (0) | 33% (1) |
| % Seeking help* | 89% (8) | 100% (9) | 78% (7) | 56% (5) | 100% (6) | 67% (2) | 100% (6) | 83% (5) | 67% (6) | — | 100% (5) | 67% (2) |
Note. numbers in parentheses is the number of individual responses (n). AHSQ = Actual Help-Seeking Questionnaire; GP = general practitioner.
percentages are calculated from total number of participants completing the AHSQ at the respective time point.
Postintervention Changes to Mental Health Status
As outlined previously, the primary aim of feasibility studies are to assess their feasibility and acceptability (Thabane et al., 2010). As with help-seeking, exploratory analysis was conducted to examine any changes to mental health status at follow-up. Indeed, these findings should be interpretated tentatively due to small sample sizes and differences in drop-out rates between the interventions. Interventions 1 and 2 did not yield any significant improvement to mental health status at post-, 2-week, or 4-week follow-up when compared to baseline (Table 7). Similarly, no significant changes to mental health status were observed in intervention 3 at 2-week or 4-week follow-up when compared to baseline (Table 7).
Discussion
All three interventions were rated positively regarding their overall acceptability, affective attitude, ethicality, self-efficacy, intervention coherence for help-seeking, and perceived effectiveness for help-seeking and well-being (aim 1). All interventions were rated equally acceptable (aim 2), indicating that the BCTs embedded across these interventions are acceptable strategies to engage male students. Regarding our third aim, only intervention 3 (Man Cave) was significantly better at engaging male students; as they were less likely to have sought help before, held more negative help-seeking attitudes, and who endorsed self-stigmatizing beliefs and conformity to masculine norms similar to that of male student norms. Intervention 1 (Men-Tality) was significantly better at engaging male students who endorsed less self-stigmatizing beliefs, less conformity to masculine norms (particularly heterosexual self-preservation and power over women), and more positive help-seeking attitudes than expected for this population group. Intervention 2 (Psychological Strength) was also significantly better at engaging male students who endorsed less self-stigmatizing beliefs compared to male student norms. Students attending intervention 2 exhibited similar help-seeking attitudes as expected for this population group, however appeared to score significantly higher for the masculine trait of winning, and lower for heterosexual self-preservation.
Self-stigma was only lower for interventions 1 and 2 when compared to male student norms suggesting that intervention 3 engaged a more representative sample of male students with high self-stigma. Most participants attending intervention 3 had not previously sought help for mental health difficulties which may be due to higher self-stigma. This is an important consideration when designing future male-sensitive interventions, as self-stigma is a key barrier to engaging with mental health support (Levant et al., 2014; Wu et al., 2017). Informal approaches are likely to be more acceptable to male students with high self-stigma, particularly if they have not engaged with mental health support previously.
Participants attending interventions 1 and 2 had significantly lower total conformity to masculine norms, power over women, and heterosexual self-preservation than expected for this population group. Indeed, these maladaptive masculine traits are barriers to help-seeking as total conformity to masculine norms negatively influence help-seeking attitudes (Ramaeker & Petrie, 2019; Seidler et al., 2016; Vogel et al., 2011; Wimer & Levant, 2011), power over women contributes to worse mental health outcomes (Wong et al., 2017), and greater heterosexual self-preservation can be seen as a dimension of antifemininity contributing to greater help-seeking reluctance (Sileo & Kershaw, 2020). In addition, winning was significantly higher for participants in intervention 2 which can be considered as an adaptive trait as it has been reported to encourage help-seeking and act as a protective factor from mental health difficulties (Iwamoto et al., 2018). These findings indicate that those attending interventions 1 and 2 represent an atypical subgroup of male students who may be more amenable to therapy as they experience less barriers (and more facilitators) when seeking help for mental health. This was not observed for intervention 3. The informal approaches and strategies seen in intervention 3 were more acceptable at engaging male students whose conformity to masculine norms are representative of the wider male student population.
Similarly, interventions 1 and 2 had higher help-seeking attitudes at baseline, indicating that these students already held positive attitudes to help-seeking. Previous studies highlight that students who recently used mental health support score higher on the ATSPPH-SF compared to those who do not (Elahi et al., 2008). Significantly more negative help-seeking attitudes were seen in intervention 3 at baseline. These participants scored lower than what was expected for this population group, presenting with similar scores for those who do not use mental health support (Elahi et al., 2008). In addition, participants in intervention 3 were significantly less likely to have accessed mental health support in the past when compared to participants in interventions 1 and 2. Once again, these preliminary findings indicate that the informal drop-in intervention (intervention 3; Man Cave), was better at engaging male students who are likely to be representative of the wider male student population where they hold negative help-seeking attitudes and are less likely to have engaged with mental health support before.
For all three interventions, no significant changes to mental health status were observed at postintervention, 2-week, or 4-week follow-up when compared to baseline, possibly due to small sample sizes and loss of follow-up data. However, mental health status at baseline did not differ from male student norms. Across all three interventions, only five participants (20%) scored ≤40 on the WEMWBS at baseline which can be used to indicate major depression (Taggart et al., 2015). Therefore, the majority of participants would not fulfill diagnostic criteria for depression, and no significant changes to mental health status are likely to be due to a ceiling effect. Participants who scored equal to or below 40 on the WEMWBS were equally distributed across the three interventions.
No significant changes to help-seeking attitudes or behaviors at postintervention, 2-week, or 4-week follow-up were observed. No significant changes to help-seeking attitudes or mental health outcomes at follow-up were observed (aim 4), although such findings may be difficult to interpret due to small sample sizes and limited follow-up data.
Certainly, these interventions are likely to be underpowered to detect (or not detect) any significant changes, and such findings should be interpreted tentatively. Instead, more attention should be given to their feasibility.
Overall, the three interventions engaged different subgroups of male students. Interventions 1 and 2 engaged male students who held preexisting positive help-seeking attitudes, had lower self-stigma, who are more likely to have engaged with mental health support previously and had lower conformity to maladaptive masculine traits. Intervention 3 appeared better at engaging male students who had higher conformity to maladaptive masculine traits, higher self-stigma, negative perceptions of help-seeking, and who were less likely to have used mental health services before. As self-stigma, conformity to masculine norms, and negative help-seeking attitudes have been highlighted as key barriers to engaging with mental health support (Levant et al., 2014; Ramaeker & Petrie, 2019; Vogel et al., 2011; Wimer & Levant, 2011), participants engaging with intervention 3 are likely to be representative of the wider male student cohort who are a hard-to-reach group. Similarly, participants attending intervention 3 were more likely to be from an ethnic minority background which is also associated with reduced help-seeking behaviors for mental health difficulties (Guo et al., 2015; Parent et al., 2018; Twentyman & Frank, 2017). There may be cause for concern for this hard-to-reach group if they were to experience emotional distress at a later date. Having more barriers to navigate through may reduce their willingness to engage with support when needed. This is likely to reduce their opportunity for support, place them at greater risk of emotional distress and potentially suicide.
Considering all three interventions were rated equally acceptable, a one-size-fits-all approach to engage male students is not recommended. As both the formal and informal interventions were deemed equally acceptable, both these strategies may be required within a university setting to engage different types of male students. Informal drop-in interventions may or may not improve mental health outcomes, but instead may help engage hard-to-reach male students, provide a point of contact, and triage them to appropriate mental health support if needed. Certainly, informal spaces can assist with building rapport, trust, and familiarity with support which are often associated with future help-seeking (Gulliver et al., 2012; Liddon et al., 2019; Seidler et al., 2018).
Student mental health research tends to ignore gender and sex differences (Howard et al., 2017; Ryan et al., 2019). Such investigations do not position themselves to be gender-sensitive and instead adopt a gender-neutral approach to mental health research. Owing to this, it is likely that the male students who do take part are not representative of the wider male student population who are hard-to-reach (Howard et al., 2017; Ryan et al., 2019). Gender-neutral approaches may undermine the validity and efficiency of scientific findings, resulting in the inappropriate application of findings contributing to a detrimental impact for both male and female students (Howard et al., 2017). Future research is required to explore the overall effectiveness and acceptability of informal interventions such as drop-ins, social spaces, or student workshops for male students who are not primarily focused on mental health and well-being.
A strength of this investigation is that the components identified from our systematic review and qualitative work consisting of delivering mental health information, explaining how to identify mental health symptoms, incorporating active-problem-solving techniques to cope with distress, sign-posting mental health services, re-framing help-seeking to align with masculine values, avoiding labels of mental health; and to use both formal and informal approaches were acceptable for male students (Sagar-Ouriaghli, Brown, et al., 2020; Sagar-Ouriaghli et al., 2019; Sagar-Ouriaghli, Godfrey, et al., 2020). This article provides a detailed description of the intervention’s active ingredients through the use of BCTs to enable health care and education providers to replicate, implement, and refine the proposed interventions.
By obtaining scores for self-stigma, previous mental health support, and conformity to masculine norms, a richer picture of the types of male students who did engage is provided. This enhances the clinical applications of the current findings and provides more constructive evidence as to how to engage male students who are often hard to reach. This is also a different approach than that traditionally used in mental health services but may be more similar to the informal method used in the men’s sheds movement (Morgan et al., 2007; Wilson & Cordier, 2013).
Despite this, there are limitations. Although a sample size of 24 was obtained, this was split across three different interventions with smaller sample sizes. It is likely that these are underpowered to detect any significant changes (Krzywinski & Altman, 2013; Maxwell, 2004). Nonetheless, pilot interventions remain essential as they are informative about the research process and can indicate likely outcomes (Van Teijlingen & Hundley, 2001). Instead, pilot studies are the best way to assess feasibility, and attention should be given to the descriptive nature of each sample and the acceptability of the interventions (Thabane et al., 2010).
Intervention 3 was an informal drop-in whereby students could attend without preregistering, came in and out as they pleased, and attend as few sessions as they liked. As this was a formal investigation, informed consent and the completion of questionnaires was still required. This discouraged certain students from attending and was a barrier for six students who opted against consenting to take part. Of those who did consent, reassurance surrounding confidentiality and anonymity of the data collected was required. Indeed, this may align with this hard-to-reach group as they may be less familiar with mental health support—including research, less trusting of mental health professionals, and more fearful of how they will be perceived (i.e., stigma) (Yousaf et al., 2015). This is important to consider, as research processes can be a barrier when evaluating and engaging male students with mental health initiatives.
Owing to logistical difficulties and to prevent cross-contamination between the interventions, it was not possible to pilot all three interventions at the same time. This led to different recruitment approaches, with intervention 1 making use of the welcome fair at the start of the academic year when students have more time available and motivation to engage (Sagar-Ouriaghli, Brown, et al., 2020). Intervention 2 was delivered after the Christmas/winter-break. Students at this stage have different time resources available. They may have more time due to feeling more settled with their academic studies, or less time due to coursework, exams, and other deadlines. Similarly, greater emotional stress related to coursework and exam pressure may encourage them to access support or reduce their availability to seek help (Sagar-Ouriaghli, Brown, et al., 2020). Intervention 3 was delivered toward the end of the term (as opposed to the start as seen in interventions 1 and 2), causing other restrictions. The fourth week of delivering the drop-in coincided with student reading week—where students course content is solely delivered online and via textbooks. This meant there were less students using the café and reduced the opportunity for students to engage. These differences may have impacted the sample of students engaging, acceptability scores, and uptake.
Conclusion
This investigation provides insight into different strategies and approaches to designing gender-sensitive mental health interventions for male students. Although formal and structured mental health interventions that provide mental health information alongside self-help techniques and skills are acceptable to male students, more informal approaches such as drop-ins or social spaces are equally acceptable. These informal approaches may be more acceptable and have better uptake for hard-to-reach male students who hold stigmatizing beliefs, conform to maladaptive masculine traits, have pre-existing negative help-seeking attitudes, are of ethnic minority backgrounds, and who are less likely to have come in to contact with mental health services in the past—which is more representative of the male student cohort. Indeed, informal interventions may provide better uptake of male students and improve their engagement. Such approaches will help to facilitate help-seeking behaviors, increasing the opportunity to combat mental health difficulties, and possibly reduce the risk of suicide. Moving forward, fully powered future research examining the effectiveness and acceptability of informal mental health initiatives and how best to tailor them to male students is required as this remains a relatively unexplored therapeutic opportunity that has a lot of promise.
Supplemental Material
Supplemental material, sj-docx-1-jmh-10.1177_15579883231163728 for Improving Mental Health Help-Seeking Among Male University Students: A Series of Gender-Sensitive Mental Health Feasibility Interventions by Ilyas Sagar-Ouriaghli, Emma Godfrey, Vinay Tailor and June S. L. Brown in American Journal of Men’s Health
Footnotes
Author Credits and Full Details: I.S.O. contributed to formulating the research question, developing and designing the interventions, completing the ethics application, recruitment of participants, delivering the interventions, analysis and collection of data, and writing of the report. E.G. contributed to formulating the research question, providing supervision of the development and design of the interventions, guidance on conducting and interpreting feasibility studies, and assisting with the write up of the report. V.T, contributed with recruitment, co-facilitation and delivery of interventions, collecting data, and reviewing the finalized report.
J.S.L.B. contributed to formulating the research questions, developing and designing the interventions, assisting in interpreting data collected, advice about mental health help-seeking and access to care by men, and assisting with the write up of paper.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by the National Institute for Health Research (NIHR) Biomedical Research Center at South London and Maudsley NHS Foundation Trust and King’s College London. The funder had no role in study design, data collection, data analysis, data interpretation, or report writing. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
ORCID iD: Ilyas Sagar-Ouriaghli  https://orcid.org/0000-0002-3014-3104
https://orcid.org/0000-0002-3014-3104
Supplemental Material: Supplemental material for this article is available online.
References
- American Psychological Association, Boys and Men Guidelines Group. (2018). APA guidelines for psychological practice with boys and men. http://www.apa.org/about/policy/psychological-practice-boys-men-guidelines.pdf
- Auerbach R. P., Alonso J., Axinn W. G., Cuijpers P., Ebert D. D., Green J. G., Hwang I., Kessler R. C., Liu H., Mortier P., Nock M. K., Pinder-Amaker S., Sampson N. A., Aguilar-Gaxiola S., Al-Hamzawi A., Andrade L. H., Benjet C., Caldas-de-Almeida J. M., Demyttenaere K., . . .Bruffaerts R. (2016). Mental disorders among college students in the WHO world mental health surverys. Psychological Medicine, 46(14), 2955–2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baillie A. J. (2005). Predictive gender and education bias in Kessler’s psychological distress scale (K10). Social Psychiatry and Psychiatric Epidemiology, 40(9), 743–748. [DOI] [PubMed] [Google Scholar]
- Bowen D. J., Kreuter M., Spring B., Cofta-Woerpel L., Linnan L., Weiner D., Bakken S., Kaplan C. P., Squires L., Fabrizio C., Fernandez M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner R. E., Engel K. E., Vogel D. L., Tucker J. R., Yamawaki N., Lannin D. G. (2018). Intersecting cultural identities and help-seeking attitudes: The role of religious commitment, gender, and self-stigma of seeking help. Mental Health, Religion & Culture, 21(6), 578–587. [Google Scholar]
- Brown J. S., Sagar-Ouriaghli I., Sullivan L. (2019). Help-seeking among men for mental health problems. In Barry J. A., Kingerlee R., Seager M., Sullivan L. (Eds.), The Palgrave handbook of male psychology and mental health (pp. 397–415). Palgrave Macmillan. [Google Scholar]
- Bruffaerts R., Mortier P., Kiekens G., Auerbach R. P., Cuijpers P., Demyttenaere K., Green J. G., Knock M. K., Kessler R. C. (2018). Mental health problems in college freshmen: Prevalence and academic functioning. Journal of Affective Disorders, 225, 97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadigan J. M., Lee C. M., Larimer M. E. (2019). Young adult mental health: A prospective examination of service utilization, perceived unmet service needs, attitudes, and barriers to service use. Prevention Science, 20(3), 366–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callanan V. J., Davis M. S. (2012). Gender differences in suicide methods. Social Psychiatry and Psychiatric Epidemiology, 47(6), 857–869. [DOI] [PubMed] [Google Scholar]
- Chang Q., Yip P. S., Chen Y. (2019). Gender inequality and suicide gender rations in the world. Journal of Affective Disorders, 243, 297–304. [DOI] [PubMed] [Google Scholar]
- Clough B. A., Nazareth S. M., Day J. J., Casey L. M. (2019). A comparison of mental health literacy, attitudes, and help-seeking intentions among domestic and international teritary students. British Journal of Guidance & Counselling, 47(1), 123–135. [Google Scholar]
- Eisenberg D., Golberstein E., Gollust S. E. (2007). Help-seeking and access to mental health care in a university student population. Medical Care, 45(7), 594–601. [DOI] [PubMed] [Google Scholar]
- Elahi J. D., Schweinle W., Anderson S. M. (2008). Reliability and validity of the attitudes toward seeking professional psychological help scale-short form. Psychiatry Research, 159(3), 320–329. [DOI] [PubMed] [Google Scholar]
- Eldridge S. M., Chan C. L., Campbell M. J., Bond C. M., Hopewell S., Thabane L., Lancaster G. A. (2016). CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. British Medical Journal, 355, i5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erentzen C., Quinlan J. A., Mar R. A. (2018). Sometimes you need more than a wingman: Masculinity, femininity, and the role of humor in men’s mental health help-seeking campaigns. Journal of Social and Clinical Psychology, 37(2), 128–157. [Google Scholar]
- Fischer E. H., Farina A. (1995). Attitudes toward seeking professional psychological help: A shortened form and considerations for research. Journal of College Student Development, 36(4), 368–373. [Google Scholar]
- Gorski E. (2010). Stoic, stubborn, or sensitive: How masculinity affects men’s help-seeking and help-referring behaviors. UW-L Journal of Undergraduate Research, 13, 1–6. [Google Scholar]
- Gulliver A., Griffiths K. M., Christensen H. (2012). Barriers and facilitators to mental health help-seeking for young elite athletes: A qualitative study. BMC Psychiatry, 12, 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Caul S., Appleby L., John A., Hawton K. (2020). The incidence of suicide in University students in England and Wales 2000/2001 - 2016/2017: Record linkage study. Journal of Affective Disorders, 261, 113–120. [DOI] [PubMed] [Google Scholar]
- Guo S., Nguyen H., Weiss B., Ngo V., Lau A. S. (2015). Linkages between mental health need and help-seeking behavior among adolescents: Moderating role of ethnicity and cultural values. Journal of Counseling Psychology, 62(4), 682–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haavik L., Joa I., Hatloy K., Stain H. J., Langeveld J. (2017). Help seeking for mental health problems in an adolescent population: The effect of gender. Journal of Mental Health, 28(5), 467–474. [DOI] [PubMed] [Google Scholar]
- HeadsUpGuys. (n.d.). https://headsupguys.org/
- Heath P. J., Brenner R. E., Vogel D. L., Lannin D. G., Strass H. A. (2017). Masculinity and barriers to seeking counselling: The buffering role of self-compassion. Journal of Counseling Psychology, 64(1), 94–103. [DOI] [PubMed] [Google Scholar]
- Hjorth C. F., Bilgrav L., Frandsen L. S., Overgaard C., Torp-Pedersen C., Nielsen B., Bøggild H. (2016). Mental health and school dropout across educational levels and genders: A 4.8-year follow-up study. BMC Public Health, 16(1), 976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman T. C., Glasziou P. P., Boutron I., Milne R., Perera R., Moher D., Altman D. G., Barbour V., Macdonald H., Johnston M., Lamb S. E., Dixon-Woods M., McCulloch P., Wyatt J. C., Chan A., Michie S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. British Medical Journal, 348, g1687. [DOI] [PubMed] [Google Scholar]
- Howard L. M., Ehrlich A. M., Gamlen F., Oram S. (2017). Gender-neutral mental health research is sex and gender biased. The Lancet Psychiatry, 4(1), 9–11. [DOI] [PubMed] [Google Scholar]
- Iwamoto D. K., Brady J., Kaya A., Park A. (2018). Masculinity and depression: A longitudinal investigation of multidimensional masculine norms among college men. American Journal of Men’s Health, 12(6), 1873–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendel F., Wirtz M., Dunkel A., Lehmkuhl E., Hetzer R., Regitz-Zagrosek V. (2010). Screening for depression: Rasch analysis of the dimensional structure of the PHQ-9 and the HADS-D. Journal of Affective Disorders, 122(3), 241–246. [DOI] [PubMed] [Google Scholar]
- Krzywinski M., Altman N. (2013). Points of significance: Power and sample size. Nature Methods, 10(12), 1139–1140. [Google Scholar]
- Lancaster G. A., Thabane L. (2019). Guidelines for reporting non-randomised pilot and feasibilty trials. Pilot and Feasibilty Studies, 5(114), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levant K., Kamaradova D., Prasko J. (2014). Perspectives on percieved stigma and self-stigma in adult male patients with depression. Neuropsychiatric Disease and Treatment, 10, 1399–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle S. K., Deane F. P., Batterham M., Vella S. A. (2021). A brief sports-based mental health literacy program for adolescent males: A cluster-randomized controlled trial. Journal of Applied Sport Psychology, 33(1), 20–44. [Google Scholar]
- Liddon L., Kingerlee R., Seager M., Barry J. A. (2019). What are the factors that make a male-friendly therapy?. In Barry J. A., Kingerlee R., Seager M., Sullivan L. (Eds.), The Palgrave handbook of male psychology and mental health (pp. 671–694). Palgrave Macmillan. [Google Scholar]
- Liu C. H., Stevens C., Wong S. H., Yasui M., Chen J. A. (2019). The prevelance and predictors of mental health diagnoses and suicide among US college students: Implications for addressing disparities in service use. Depression and Anxiety, 36(1), 8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie C. S., Visperas A., Ogrondniczuk J. S., Oliffe J. L., Nurmi M. A. (2019). Age and sex differences in self-stigma and public stigma concerning depression and suicide in men. Stigma and Health, 4(2), 233–241. [Google Scholar]
- Mahalik J. R., Locke B. D., Ludlow L., Diemer M. A. (2003). Development of the conformity to masculine norms inventory. Psychology of Men & Masculinity, 4(1), 3–25. [Google Scholar]
- Man Therapy. (n.d.). https://www.mantherapy.org/
- Martin L. A., Neighbors H. W., Griffith D. M. (2013). The experience of symptoms of depression in men vs women analysis of the national comorbidity survey replication. JAMA Psychiatry, 70(10), 1100–1106. [DOI] [PubMed] [Google Scholar]
- Maxwell S. E. (2004). The persistence of underpowered studies in psychological research: Causes, consequences and remedies. Psychological Methods, 9(2), 147–163. [DOI] [PubMed] [Google Scholar]
- McManus S., Gunnell D. (2020). Trends in mental health, non-suicidal self-harm and suicide attempts in 16-24 year old students and non-students in England, 2000-2014. Social Psychiatry and Psychiatric Epidemiology, 55(1), 125–128. [DOI] [PubMed] [Google Scholar]
- Men’s Health Forum. (2015). How to make mental health services work for men. Men’s Health Forum. [Google Scholar]
- Mental Health Foundation. (2016). Fundamental facts about mental health 2016. Mental Health Foundation. [Google Scholar]
- Mergl R., Koburger N., Heinrichs K., Székely A., Tóth M. D., Coyne J., Quinatão S., Arensman E., Coffey C., Maxwell M., Vãrnick A., van Audenhove C., McDaid D., Sarchiapone M., Schmidtke A., Genz A., Gusmão R., Hegerl U. (2015). What are reasons for the large gender differences in the lethality of suicidal acts? An epidemiological analysis in four European Countries. PLOS ONE, 10(7), Article e0129062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Johnston M., Carey R. (2016). Behaviour change techniques. In Gellman M., Turner J. (Eds.), Encyclopedia of behavioral medicine (pp. 1–8). Springer. [Google Scholar]
- Michie S., Richardson M., Johnston M., Abraham C., Francis J., Hardeman W., Eccles M. P., Cane J., Wood C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. [DOI] [PubMed] [Google Scholar]
- Michie S., West R., Sheals K., Godinho C. A. (2018). Evaluating the effectiveness of behavior change techniques in health-related behavior: A scoping review of methods used. Translational Behavioral Medicine, 8(2), 212–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan M., Hayes R., Williamson M., Ford C. (2007). Men’s sheds: A community approach to promoting mental health and well-being. International Journal of Mental Health Promotion, 9(3), 48–52. [Google Scholar]
- Nam S. K., Chu H. J., Lee M. K., Lee H. J., Kim N., Lee S. M. (2010). A meta-analysis of gender differences in attitudes toward seeking professional psychological help. Journal of American College Health, 59(2), 110–116. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (n.d.). NIMH’s “real men. real depression” campaign. https://www.nimh.nih.gov/health/topics/men-and-mental-health/men-and-depression/nimhs-real-men-real-depression-campaign
- O’Brein R., Hunt K., Hart G. (2005). “It’s caveman stuff, but that is to a certain extent how guys still operate”: Men’s accounts of masculinity and help seeking. Social Science & Medicine, 61(3), 503–516. [DOI] [PubMed] [Google Scholar]
- Ogrondniczuk J., Oliffe J., Beharry J. (2018). HeadsUpGuys: Canadian online resource for men with depression. Canadian Family Physician, 64(2), 93–94. [PMC free article] [PubMed] [Google Scholar]
- Parent M. C., Hammer J. H., Bradstreet T. C., Schwartz E. N., Jobe T. (2018). Men’s mental health help-seeking behaviors: An intersectional analysis. American Journal of Men’s Health, 12(1), 64–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parent M. C., Moradi B. (2011). An abbreviated tool for assessing conformity to masculine norms: Psychometric properties of the conformity to masculine norms inventory-46. Psychology of Men & Masculinity, 12(4), 339–353. [Google Scholar]
- Patrick S., Robertson S. (2016). Mental health and wellbeing: Focus on men’s health. British Journal of Nursing, 25(21), 1163–1169. [DOI] [PubMed] [Google Scholar]
- Pedrelli P., Borsari B., Lipson S. K., Heinze J. E., Eisenberg D. (2016). Gender differences in the relationship among major depressive disorder, heavy alcohol use, and mental health treatment engagement among college students. Journal of Studies on Alcohol and Drugs, 77(4), 620–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard J. (2016). Early and effective intervention in male mental health. Perspectives in Public Health, 136(6), 337–338. [DOI] [PubMed] [Google Scholar]
- Ramaeker J., Petrie T. A. (2019). “Man up!”: Exploring intersections of sport participation, masculinity, psychological distress, and help-seeking attitudes and intentions. Psychology of Men & Masculinities, 20(4), 515–527. [Google Scholar]
- Ratnayake P., Hyde C. (2019). Mental health literacy, help-seeking behaviour and wellbeing in young people: Implications for practice. The Educational and Development Psychologist, 36(1), 16–21. [Google Scholar]
- Rickwood D., Deane F. P., Wilson C. J., Ciarrochi J. V. (2005). Young people’s help-seeking for mental health problems. Australian E-Journal for the Advancement of Mental Health, 4(3), 218–251. [Google Scholar]
- River J. (2018). Diverse and dynamic interactions: A model of suicidal men’s help seeking as it relates to health services. American Journal of Men’s Health, 12(1), 150–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson S., Bagnall A., Walker M. (2015). Evidence for a gender-based approach to mental health programmes: Identifying the key considerations associated with “being male.”Movember Foundation. [Google Scholar]
- Rochlen A. B., Whilde M. R., Hoyer W. D. (2005). The real men. Real depression campaign: Overview, theoretical implications, and research contributions. Psychology of Men & Masculinity, 6(3), 186–194. [Google Scholar]
- Ryan J., Lopian L., Le B., Edney S., Van Kessel G., Plotnikoff R., Vandelanotte C., Olds T., Maher C. (2019). It’s not raining men: A mixed-methods study investigating methods of improving male recruitment to health behaviour research. BMC Public Health, 19(1), 814–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagar-Ouriaghli I., Brown J. S., Tailor V., Godfrey E. (2020). Engaging male students with mental health support: A qualitative focus group study. BMC Public Health, 20(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagar-Ouriaghli I., Godfrey E., Bridge L., Meade L., Brown J. S. (2019). Improving mental health service utilization among men: A systematic review and synthesis of behavior change techniques within interventions targeting help-seeking. American Journal of Men’s Health, 13(3), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagar-Ouriaghli I., Godfrey E., Graham S., Brown J. S. (2020). Improving mental health help-seeking behaviours for male students: A framework for developing a complex intervention. International Journal of Environmental Research and Public Health, 17(14), 4965–4990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salokangas R. K., Vaahtera K., Pacriev S., Sohlman B., Lehtinen V. (2002). Gender differences in depressive symptoms. An artefact caused by measurement instruments? Journal of Affective Disorders, 68(2–3), 215–220. [DOI] [PubMed] [Google Scholar]
- Schnyder N., Panczak R., Groth N., Schultze-Lutter F. (2017). Association between mental health-related stigma and active help-seeking: Systematic review and meta-analysis. The British Journal of Psychiatry, 210(4), 261–268. [DOI] [PubMed] [Google Scholar]
- Schoen E., Brock R., Hannon J. (2019). Gender bias, other specified and unspecified feeding and eating disorders, and college students: A vignette study. Eating Disorders, 27(3), 291–304. [DOI] [PubMed] [Google Scholar]
- Seaton C. L., Bottorff J. L., Oliffe J. L., Medhurst K., DeLeenheer D. (2019). Mental health promotion in male-dominated workplaces: Perspectives of male employees and workplace representatives. Psychology of Men & Masculinities, 20(4), 541–552. [Google Scholar]
- Seehuus M., Moeller R. W., Peisch V. (2021). Gender effects on mental health symptoms and treatment in college students. Journal of American College Health, 69(1), 95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler Z. E., Dawes A. J., Rice S. M., Oliffe J. L., Dhillon H. M. (2016). The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review, 49, 106–118. [DOI] [PubMed] [Google Scholar]
- Seidler Z. E., Rice S. M., Ogrodniczuk J. S., Oliffe J. L., Dhillon H. M. (2018). Engaging men in psychological treatment: A scoping review. American Journal of Men’s Health, 12(6), 1882–1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekhon M., Cartwright M., Francis J. J. (2017). Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Services Research, 17(1), 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekhon M., Cartwright M., Francis J. J. (2018). Development of a theory-informed questionnaire to assess the acceptability of healthcare interventions: Application of pre-validation methods. UK Society of Behavioural Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sileo K. M., Kershaw T. S. (2020). Dimensions of masculine norms, depression, and mental health service utilization: Results from a prospective cohort study among emerging adult men in the United States. American Journal of Men’s Health, 14(1), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T., Grove R., Burgess P. (2011). Kessler psychological distress scale: Normative data from the 2007 Australian National Survey of Mental Health and Wellbeing. Australian & New Zealand Journal of Psychiatry, 45(4), 308–316. [DOI] [PubMed] [Google Scholar]
- Spandler H., McKewon M., Roy A., Hurley M. (2013). Football metaphor and mental well-being: An evaluation of the It’s A Goal! Programme. Journal of Mental Health, 22(6), 544–554. [DOI] [PubMed] [Google Scholar]
- Spencer-Thomas S., Hindman J., Conrad J. (2014). Man therapy: Outreach and impact on men’s mental health program 18 months after launch. http://mantherapy.org/pdf/White-Paper-Man-Therapy.pdf
- Taggart F., Stewart-Brown S., Parkinson J. (2015). Warwick-Edinburgh Mental Well-being Scale (WEMWBS) User Guide—Version 2. NHS Health Scotland. [Google Scholar]
- Tennant R., Hiller L., Fishwick R., Platt S., Joseph S., Weich S., Parkinson J., Secker J., Stewart-Brown S. (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health and Quality Life Outcomes, 5(1), 63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thabane L., Ma J., Chu R., Cheng J., Ismaila A., Rios L. P., Robson R., Thabane M., Giangreggorio L., Goldsmith C. H. (2010). A tutorial on pilot studies: The what, why and how. BMC Medical Research Methodology, 10(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twentyman J., Frank M. (2017). Effects of race and ethnicity on mental health and help-seeking amongst undergraduate university students. Journal of Undergraduate Ethnic Minority Psychology, 3(6), 2332–9300. [Google Scholar]
- Van Teijlingen E. R., Hundley V. (2001). The importance of pilot studies. Social Research UPDATE, 35, 1–4. [Google Scholar]
- Vogel D. L., Heimerdinger-Edwards S. R., Hammer J. H., Hubbard A. (2011). “Boys don’t cry”: Examination of the links between endorsement of masculine norms, self-stigma, and help-seeking attitudes for men from diverse backgrounds. Journal of Counseling Psychology, 58(3), 368–382. [DOI] [PubMed] [Google Scholar]
- Vogel D. L., Wade N. G., Haake S. (2006). Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology, 53(3), 325–337. [Google Scholar]
- Wendt D., Shafer K. (2016). Gender and attitudes about mental health help seeking: Results from national data. Health & Social Work, 41(1), 20–28. [Google Scholar]
- Wilson C. J., Deane F. P., Ciarrochi J. V., Rickwood D. (2005). Measuring help seeking intentions: Properties of the general help seeking questionnaire. Canadian Journal of Counselling, 39(1), 15–28. [Google Scholar]
- Wilson N. J., Cordier R. (2013). A narrative review of men’s sheds literature: Reducing social isolation and promoting men’s health and well-being. Health and Social Care in the Community, 21(5), 451–463. [DOI] [PubMed] [Google Scholar]
- Wimer D. J., Levant R. F. (2011). The relation of masculinity and help-seeking style with the academic help-seeking behavior of college men. The Journal of Men’s Studies, 19(3), 256–274. [Google Scholar]
- Wong Y. J., Ho M. R., Wang S. Y., Miller I. S. (2017). Meta-analyses of the relationship between conformity to masculine norms and mental health-related outcomes. Journal of Counseling Psychology, 64(1), 80–93. [DOI] [PubMed] [Google Scholar]
- Wu I. H., Bathje G. J., Kalibatseva Z., Sung D., Leong F. T., Collins-Eaglin J. (2017). Stigma, mental health, and counseling service use: A person-centred approach to mental health stigma profiles. Psychological Services, 14(4), 490–501. [DOI] [PubMed] [Google Scholar]
- Yousaf O., Grunfeld E. A., Hunter M. S. (2015). A systematic review of the factors associated with delays in medical and psychological help-seeking among men. Health Psychology Review, 9(2), 264–276. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jmh-10.1177_15579883231163728 for Improving Mental Health Help-Seeking Among Male University Students: A Series of Gender-Sensitive Mental Health Feasibility Interventions by Ilyas Sagar-Ouriaghli, Emma Godfrey, Vinay Tailor and June S. L. Brown in American Journal of Men’s Health