Abstract
Background: Although use of complementary and alternative medicine (CAM) is rising among older adults, many do not discuss these healthcare practices with their primary care practitioners (PCPs). This study sought to determine the prevalence of CAM use and to identify factors associated with CAM disclosure among patients ages 65 and older. Methods: Participants completed an anonymous survey, which evaluated their CAM use over the past year and disclosure of CAM to a PCP. Additional questions queried demographics, patient health, and relationships with one’s PCP. Analyses included descriptive statistics, chi-square tests and logistic regression. Results: One hundred seventy-three participants answered surveys. Sixty percent reported use of at least one form of CAM in the past year. Among those using CAM, 64.4% disclosed use to their PCP. Patients disclosed supplements/herbal products and naturopathy/homeopathy/acupuncture at a higher rate than body work techniques and mind-body practices (71.9% and 66.7% vs. 48% and 50%). The only factor significantly associated with disclosure was trust in one’s PCP (odds ratio = 2.97; confidence interval = 1.01–8.73). Conclusions: Clinicians may improve CAM disclosure rates in older adults by inquiring about all types of CAM and continuing to invest in their patient relationships, specifically by building trust.
Keywords: complementary medicine, alternative therapies, disclosure, professional-patient relations
Introduction
Over the past several decades, there has been a steady increase in the prevalence of Complementary and Alternative Medicine (CAM) use in the United States along with a surge of published literature demonstrating the safety, efficacy, and acceptance of CAM (Frass et al., 2012; Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public, 2005; Phutrakool & Pongpirul, 2022) Defined as “a group of diverse medical and healthcare practices and products that are not presently considered part of conventional medicine” (National Library of Medicine. Bethesda (MD): National Library of Medicine (US), 2019), CAM encompasses modalities such as mind-body practices, acupuncture, and massage therapy, among others. Ample evidence supports the use of CAM as a non-pharmacological adjunct to mainstream medicine or as an alternative for an array of conditions, including rheumatic diseases, orthopedic and musculoskeletal pain, cancer symptoms, and psychiatric conditions (Kogan, 2018; Rakel, 2017). Recently, the National Academies released their report endorsing a CAM approach to healthcare for veterans and the nation known as Whole Health (National Academies of Sciences, Engineering, and Medicine, 2023). This growing trend of CAM use may be of particular importance in older patients given the prevalence of chronic illness and polypharmacy in this population (Kim & Parish, 2017; National Council on Aging, 2018).
Among patients 60 years and older the prevalence of CAM use is higher compared to the U.S. general adult population (41-63% vs. 36-38%, respectively) (Harris et al., 2012). Numerous studies have demonstrated the utility of CAM in treating conditions specific to older patients such as osteoporosis and falls (Kogan, 2018), and CAM has been associated with healthy aging (Mackenzie & Rakel, 2006). However, while a significant proportion of patients report using CAM, few discuss these practices with their primary care practitioners (PCPs). The 2012 National Health Interview Survey found that 42.3% of CAM users in the general U.S. population did not disclose their CAM use to their PCP (Jou & Johnson, 2016). Few studies to date have examined disclosure rates in older patients, specifically. One national survey found that only half (50.9%) of patients over age 65 disclosed their use of herbal supplements (Bruno & Ellis, 2005), and studies examining forms of CAM other than herbal medicinal products found disclosure rates ranging from 38% to 59% (Arcury et al., 2013; Cheung et al., 2007; Najm et al., 2003).
Nondisclosure of CAM use to PCPs has serious implications, especially among older patients. Interactions between conventional medicine and CAM may produce severe adverse effects. For example, in patients 65 and older, concurrent use of prescription drugs with herbal medicinal products has been associated with bleeding disorders, alterations in blood glucose, and inhibition of cytochrome P450 3A4 substrates (Agbabiaka et al., 2017). Even CAM modalities that are generally considered safe such as yoga and acupuncture have potential risks (Chung et al., 2003; Johnson et al., 2004). For these reasons, it is essential that all clinicians be aware of their patients’ CAM use to provide the most effective and safe treatments, as well as to build a foundation of trust and collaboration with those they serve. In the general population, several factors have been identified to explain a patient’s decision not to discuss CAM with a PCP. These include a lack of inquiry about CAM from clinicians, fear of clinician disapproval, perception of disclosure as unimportant, and belief that the clinician lacks knowledge about CAM (Foley et al., 2019).
Despite the risks, few studies have explored factors linked to CAM disclosure in older adults. Our search yielded only one quantitative study examining variables associated with CAM disclosure in patients 65 and older, specifically. This study found three factors associated with CAM disclosure: age (younger than 70 vs. older), doctor opinion of CAM, and having fewer health concerns (Halpin et al., 2020). Another study in the general population found that non-Latino white, married, and female patients are more likely to disclose CAM (Chao et al., 2008).
Our study sought to build upon this existing knowledge base by quantitatively examining factors associated with CAM disclosure in older adults (>64 years). These factors included previously investigated variables such as demographics and self-rated health status. Other analyzed factors (i.e., degree held by PCP, patient trust in PCP, patient confidence in PCP, patient satisfaction with PCP, and patient understanding of PCP explanations) have been explored in previous research and associated with CAM use, but they have yet to be investigated in the context of disclosure (Astin, 1998). Additionally, our study aimed to broaden the literature on how disclosure varies by CAM type (e.g., body work, naturopathy).
Given the prevalence of CAM use among older patients and associated risks with non-disclosure, it is essential to understand what contributes to patients’ decisions to discuss these practices with their PCPs. Ultimately, results from our study will inform and guide clinician-patient conversations about CAM, leading to optimal health and well-being.
Method
Participants
We conducted a cross-sectional survey study of older Connecticut residents from November 2021 to September 2022. The study was approved by the UConn Health Institutional Review Board. This was a convenience sample recruited by the Recruitment and Community Engagement Core of the University of Connecticut Center on Aging from their research volunteer registry. Patients who were 65 years old and older who could read and write in English were eligible, and they received the survey and consent by postal mail. Those who chose to participate had the option to respond via postal mail or online. Additional participants were recruited using a University-wide email system that posted a weekly, online survey invitation. Collected data were entered into REDCap 13.1.7. Participation was voluntary and anonymous, and participants did not receive compensation. We calculated that the analyses required a minimum of 150 participants to achieve an 8% margin of error with a 95% confidence level.
Measures
The survey (see Supplemental Material) was a compilation of 22 questions adapted from previous, similar studies. To assess the outcome variable (i.e., patient disclosure of CAM to a PCP), we asked participants about their use of four different CAM modalities over the prior year, employing a similar format used by the 2011 National Center for Complementary and Alternative Medicine (NCCAM) Survey. The four categories of CAM included: (1) herbal products/dietary supplements (e.g., ginkgo biloba or St. John’s wort), (2) body work (e.g., massage, chiropractic manipulation), (3) mind-body practices (e.g., meditation, yoga, tai chi), and (4) naturopathy/acupuncture/homeopathy. For each of these four categories, patients who answered “yes” to using one or more of these types of CAM in the past year were asked if they had informed their PCP about their CAM use. We next categorized participants as “disclosers” if they had informed their PCP about using one or more types of CAM. This provided a dichotomized outcome variable, that is, disclosure of CAM: yes or no.
Survey questions regarding the predictor variables were also drawn from previous studies. A series of questions exploring satisfaction, trust, confidence and understanding were adapted from a prior study (Astin, 1998). For this series of questions, participants provided answers using a Likert-type scale. These variables were dichotomized in analyses such that scores on these Likert-type scales of 4 or 5 (e.g., “a lot,” “completely”) were compared to scores of 3, 2, or 1 (e.g., “somewhat,” “only a little,” “not at all”). Self-rated health was assessed using the WHO’s single item measure, and the responses “very good” and “good” health were compared to “moderate,” “bad,” and “very bad” health (World Health Organization, 2002). Demographic variables included age, self-identified gender, race/ethnicity, education and marital status. Participants were also asked to identify the degree (e.g., medical doctor (M.D.)), doctor of osteopathy, physician assistant) of his or her PCP. This clinician variable was dichotomized in analyses as M.D. versus all other clinician degrees. The survey also included questions from the NCCAM questionnaire relating to reasons for non-disclosure of CAM and patient interest in discussing CAM with a PCP (National Center for Complementary and Alternative Medicine, The American Association of Retired Persons, 2011). The principal investigator (M.P.G.) of this study is a medical doctor of family medicine.
Data analysis: The first step of the analysis examined demographic characteristics using descriptive statistics in the sample as a whole, including CAM users and non-users. We next created cross-tabulation (e.g., 2 × 2) tables and performed χ² tests to assess the association between the disclosure status (i.e., disclosure vs. non-disclosure) and the predictor variables (e.g., demographics, self-rated health, etc.). For this set of analyses we only included participants who had used one or more forms of CAM in the past year. Predictor variables that were significant (i.e., p < .05) in the χ² tests were then included in a logistic regression model, which examined the likelihood of disclosure regressed against the predictor variable and demographics. Additionally, we examined frequency of disclosure by CAM type and used McNemar’s test to compare disclosure status between the four different types of CAM. Some participants did not answer all questions in the survey. No question is missing more than 4% of the data. Analyses used listwise deletion of missing data. We performed analyses in SPSS 29.0 (© SPSS/IBM) and SAS 9.4 (© SAS Institute).
Results
One hundred seventy-three total participants (N = 173) completed the survey (response rate = 23%; 750 surveys mailed). Ninety-nine participants responded by USPS mail, and 74 completed the online survey. The sample as a whole was 82% female, 92.4% white non-Hispanic, and mean age 76.7 years (standard deviation = 7.8 years; range = 65–98 years).
Of the 173 total participants, 104 participants (60.1%) had used at least 1 form of CAM in the past 12 months. Among those 104 participants, 59 (34.1%) had used one form of CAM, 27 (15.6%) had used two forms, 10 (5.7%) had used three forms, and 8 (4.6%) had used four forms. The most commonly used form of CAM was herbal products/dietary supplements with 64 (37.0%) of the sample as a whole taking these in the past 12 months. Fifty (28.9%) had used mind-body practices, 46 (26.6%) had used body work techniques, and 15 (8.7%) had used naturopathy/acupuncture/homeopathy.
Among the 104 participants using CAM, 67 (64.4%) had disclosed one or more forms of CAM to their PCP. Fifty (74.6%) of those participants had disclosed all forms of CAM to their PCP while 17 (25.3%) had disclosed some but not all forms of CAM. When broken down by type of CAM, 46 of 64 participants (71.9%) using herbal products/dietary supplements disclosed this use to their PCP, 24 of 50 participants (48.0%) using mind-body practices disclosed this use to their PCP, 23 of 46 participants (50.0%) using body work techniques disclosed this use to their PCP, and 10 of 15 participants (66.7%) using naturopathy/acupuncture/homeopathy disclosed this use to their PCP (see Figure 1). Based on McNemar’s test, significantly more participants disclosed use of herbal products/dietary supplements compared to both mind-body practices and body work (p < .01). There was no significant difference between disclosure status of herbal products/dietary supplements and naturopathy/acupuncture/homeopathy. The top two reasons for non-disclosure among participants in the non-discloser group were: (1) never thinking to tell one’s PCP (50%), and (2) the PCP never asked (42%).
Figure 1.
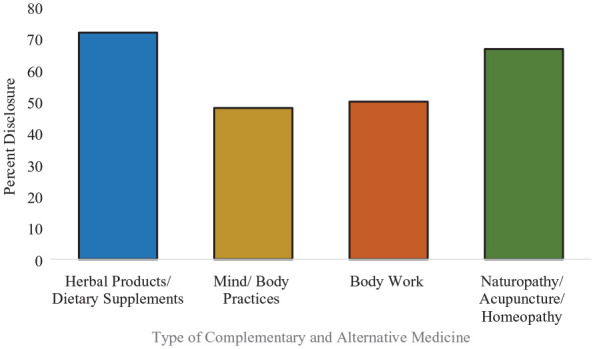
Disclosure rate by type of complementary and alternative medicine.
Results of the χ² tests assessing the association between disclosure status (i.e., disclosure vs. non-disclosure) and the predictor variables, are displayed in Table 1. Participants using CAM were 84.5% female, 92.2% white non-Hispanic, 59.4% married, and 77.2% with 4-year college degrees or postgraduate degrees. Mean age was 75.6 (standard deviation = 7.2). There were no statistically significant differences between disclosers and non-disclosers in any of these demographic categories or in patient self-reported health.
Table 1.
Demographic, Patient and Clinician Factors by CAM Disclosure Status.
| All CAM Users (n = 104) |
Disclosers (n = 67) |
Non-Disclosers (n = 37) |
Pearson Chi-Square or 2-sided t value | |
|---|---|---|---|---|
| Factors | n (%) | n (%) | n (%) | |
| Demographics | ||||
| Age (years) | Mean = 75.6 (SD = 7.2) | Mean = 75.4 (SD = 7.2) | Mean = 75.8 (SD = 7.4) | t = 0.23 |
| Female gender | 87 (84.5%) | 58 (86.6%) | 29 (80.6%) | 0.65 |
| White non-Hispanic | 94 (92.2%) | 62 (92.5%) | 32 (91.4%) | 0.04 |
| Married | 60 (59.4%) | 40 (59.7%) | 20 (58.8%) | 0.01 |
| Education (4-year college or post-graduate degree) | 78 (77.2%) | 50 (76.9%) | 28 (77.8%) | 0.01 |
| Patient Factor | ||||
| Self-reported health (good or very good) | 82 (80.4%) | 54 (81.8%) | 28 (77.8%) | 0.24 |
| Clinician Factors | ||||
| PCP is MD | 72 (71.3%) | 47 (73.4%) | 25 (67.6%) | 0.40 |
| Satisfaction with PCP | 58 (56.9%) | 42 (63.6%) | 16 (44.4%) | 3.50* |
| Trust in PCP | 79 (78.2%) | 56 (84.8%) | 23 (65.7%) | 4.92** |
| Confidence in PCP | 77 (76.2%) | 51 (77.3%) | 26 (74.3%) | 0.11 |
| Understanding of PCP answers to medical questions | 82 (82.0%) | 56 (84.8%) | 26 (76.5%) | 1.07 |
Note. CAM = Complementary and Alternative Medicine; SD = Standard Deviation; PCP = Primary Care Practitioner.
p < .1. **p < .05.
Among clinician factors related to disclosure status, only patient trust in PCP was significantly (p = .03) associated with disclosure, with more disclosers (84.8%) acknowledging a high degree of trust in their PCPs compared to non-disclosers (65.7%). Additionally, 63.6% of disclosers expressed satisfaction with their PCPs compared to 44.4% of non-disclosers (p = .06). Other clinician-related factors (i.e., clinician degree, confidence in PCP, understanding of PCP answers) were not associated with disclosure status (p > .30).
The only predictor variable entered into the logistic regression was trust in PCP. Three demographic variables (age, gender, race) were entered in as controls. Logistic regression (Table 2) revealed that patients disclosing CAM use were about three times more likely to acknowledge a high degree of trust in their PCPs than non-disclosers (odds ratio = 2.97; confidence interval = 1.01–8.73).
Table 2.
Regression Model of Factors Related to Disclosure of CAM a .
| Factors | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Trust in PCP | 2.97 | [1.01, 8.73]* |
Note. CAM = Complementary and Alternative Medicine; PCP = Primary Care Practitioner.
model includes demographic variables (age, gender, race).
p < .05.
Discussion
A majority of the participants (60.1%) in our study had used one or more forms of CAM in the past 12 months, a finding that is consistent with data from two prior national polls (Maciasz et al., 2022; National Center for Complementary and Alternative Medicine, The American Association of Retired Persons, 2011), which found CAM rates ranging from 63-66% in patients over age 50, and 54% in patients aged 65 and older. The rates of different CAM types in our study were also consistent with past research. The 2011 NCCAM survey found that the most frequently used type of CAM over a 12-month period was herbal products/dietary supplements (37%) followed by body work (22%). Similarly, our study found herbal products/dietary supplements to be the most frequently used (37%) followed by body work (26.6%).
Unlike the 2011 NCCAM study, however, the current study found a higher rate of mind-body practice (28.9% vs. 9%). Our findings align with the more recent National Poll on Healthy Aging (Maciasz et al., 2022), which found 24% of participants aged 50 to 80 had used yoga, and 27% had used meditation and mindfulness. These trends likely reflect the rising national popularity of mind-body practices. Data from the National Health Interview Surveys showed an increase from 9.5% to 14.3% in yoga practice and a three-fold increase (4.1% to 14.2%) in the use of meditation among U.S. adults between 2012 and 2017 (Clarke et al., 2018). Results from our study suggest that this rise might be even more pronounced in the older population.
A majority of participants (64.4%) in our sample disclosed use of one or more forms of CAM to their PCP – a finding consistent with the 2012 National Health Interview Survey (Jou & Johnson, 2016), which found a non-disclosure rate of 42.3% (disclosure rate = 57.7%). Disclosure rate varied by CAM type. Participants in the current sample were most likely to disclose herbal products/dietary supplements (71.9%) and naturopathy/acupuncture/homeopathy (66.7%) compared to mind-body practices (48.0%) or body work (50.0%). The National Health Interview Survey (Jou & Johnson, 2016) also found the highest rates of disclosure when discussing herbs/supplements (75.1%) and acupuncture (64.5%) and the lowest rates when disclosing massage (42.2%), yoga/tai chi/qi gong (35.3%), and meditation/mindfulness (36.0%). These data suggest there may be greater acceptance for discussing supplements and acupuncture versus body work and mind-body practices. Our study thus reveals an opportunity for clinicians to fill a care gap and initiate discussions with their older patients about mind-body practices and body work, specifically.
The current study sought to identify factors associated with older patients’ disclosure of CAM. Our literature review found only one prior study (Halpin et al., 2020) having quantitatively examined factors associated with disclosure in patients 65 years and older. This prior study found several factors (younger patient age, doctor’s opinion of CAM, and having fewer health concerns) associated with disclosure. In comparison, our study did not find significant associations for any demographic or patient-related variables. The previous study was performed in a similar demographic sample (i.e., highly educated, majority white), but only examined ingestible forms of CAM in the regressions, which may account for the difference in findings. Given the paucity of research on this topic, further studies are needed to identify which demographic and patient factors, if any, are associated with CAM disclosure to PCPs.
The one variable significantly associated with disclosure of CAM in our analyses was trust in one’s PCP, with disclosers being nearly three times more likely to acknowledge a high degree of trust in their PCPs than non-disclosers. Although lack of trust in and dissatisfaction with conventional physicians have been previously associated with use of alternative medicine (Astin, 1998), trust has not been quantitatively examined in the context of disclosure. Interestingly, previous qualitative studies demonstrate that the clinician-patient relationship does impact disclosure. One study of older adults found that one of the primary themes contributing to a patient’s decision to disclose complementary medicine use was having a supportive physician (Arcury et al., 2013). Another qualitative study described the association between doctors’ interpersonal skills (e.g., attentive listening, respect, being involved) and patients’ willingness to disclose complementary medicine (Kelak et al., 2018).
Our findings highlight the impact of the doctor-patient connection on patient health outcomes and reinforce the explicit importance of cultivating trusting relationships with one’s patients. Indeed, the top reasons for non-disclosure in our study were (1) not thinking to tell one’s PCP (50%), and (2) never having a PCP ask about CAM (42%), further suggesting that a breakdown in communication contributes to non-disclosure. Previous studies have also cited both of these as leading reasons for non-disclosure (Jou & Johnson, 2016; National Center for Complementary and Alternative Medicine, The American Association of Retired Persons, 2011). Various strategies have been proposed to assist practitioners in initiating open communication about CAM. Some of these strategies include: (1) adding a standardized question about CAM to medical forms, (2) asking for a complete list of therapies including prescription, over-the-counter, herbal therapies and other CAM practices, (3) remaining curious, asking, “How does CAM help with this symptom?,” and (4) acknowledging the patient’s autonomy and efforts toward self-care in choosing CAMs (National Institutes of Health, 2008; Stubbe, 2018). These strategies normalize CAM conversations, conveying to patients that these topics are valid and enabling practitioners to provide comprehensive care.
Clinical Implications for Health Managers and Policymakers
The topic of CAM is at the forefront of policymaking as evidenced in the National Academies’ recently published report, recommending the scaling and spreading of Whole Health Care, which “. . .integrates evidence-based conventional medical care with complementary and integrative health. . .” nationwide across all health systems and the lifespan (National Academies of Sciences, Engineering, and Medicine, 2023). As such, understanding our patients’ current CAM use and factors associated with disclosure will be essential to implementing the report’s call for healthcare transformation. For instance, healthcare leaders might develop strategies to educate and empower practitioners to initiate clinical conversations about CAM and to do so in a way that builds patient trust and engagement.
Limitations
The current study offers a foundation for future research, expanding knowledge on an important topic that has received little attention in the medical literature. Our study does contain the following methodological limitations: 1) the sample size was relatively small. Although the descriptive results aligned well with past research, a larger sample may yield more nuanced results in the analyses on disclosure. For instance, a larger sample would have allowed us to perform regressions by CAM type instead of grouping all of the types of CAM together; 2) the sample was majority white non-Hispanic and highly educated, which limits the generalizability of the results. This is of particular importance since past studies have found racial/ethnic differences in CAM disclosure in the general population (Chao et al., 2008); 3) this study may have been subject to selection bias since participants chose whether or not to participate. Although a significant number of participants (39.9%) reported no use of CAM in the past year, it is possible that more potential participants declined to complete the survey due to a lack of interest in the topic; 4) as with all survey studies, we were unable to ensure that participants were independent in their responses, completing the survey on their own without assistance.
Recommendations for Future Research
Considering the stated limitations of this study as well as the paucity of studies quantitatively examining this topic, further research is essential. In the pursuit of generalizability, this study should be repeated in a larger and more diverse sample. Furthermore, considering the associations between cultural/religious practices and CAM (Stubbe, 2018), researchers who do obtain a diverse sample might consider investigating cultural/religious factors and how they play into patient-practitioner discussions about CAM.
Conclusions
This cross-sectional survey study demonstrates that 60% of older adults in the sample used one or more forms of CAM in the prior 12 months, levels similar to national trends. More importantly, 35.6% of those older adults using CAM did not disclose such use to their PCPs, creating a care gap of potential risks and benefits. Most notable, trust was the one variable associated with increased disclosure of CAM to one’s PCP, with disclosers being nearly three times more likely to acknowledge a high degree of trust in their PCPs than non-disclosers (odds ratio = 2.97; confidence interval = 1.01–8.73). Clinicians caring for older adults may improve CAM disclosure rates by asking about all types of CAM use, specifically body work and mind-body practices, and by continuing to invest in their ongoing relationships with patients – building trust and optimizing health.
Supplemental Material
Supplemental material, sj-docx-1-ggm-10.1177_23337214231179839 for Disclosure of Complementary and Alternative Medicine Use Among Older Adults: A Cross-Sectional Study by Julia Golden, Lisa Kenyon-Pesce, Julie Robison, James Grady and Mary P. Guerrera in Gerontology and Geriatric Medicine
Acknowledgments
We thank Deborah Noujaim, M.P.H. and Alba Santiago, B.A. of the UConn Center on Aging for their assistance mailing surveys. We are grateful for their contributions.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: The study was assessed, positively evaluated and approved by a responsible ethics committee (UConn Health Institutional Review Board, IRB Number 21X-254-2) on September 10, 2021, prior to commencement of survey distribution.
ORCID iD: Julia Golden  https://orcid.org/0009-0007-7114-7084
https://orcid.org/0009-0007-7114-7084
Supplemental Material: Supplemental material for this article is available online.
References
- Agbabiaka T. B., Wider B., Watson L. K., Goodman C. (2017). Concurrent use of prescription drugs and herbal medicinal products in older adults: A systematic review. Drugs & Aging, 34(12), 891–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcury T. A., Bell R. A., Altizer K. P., Grzywacz J. G., Sandberg J. C., Quandt S. A. (2013). Attitudes of older adults regarding disclosure of complementary therapy use to physicians. Journal of Applied Gerontology, 32(5), 627–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astin J. A. (1998). Why patients use alternative medicine: Results of a national study. JAMA, 279(19), 1548–1553. [DOI] [PubMed] [Google Scholar]
- Bruno J. J., Ellis J. J. (2005). Herbal use among US elderly: 2002 national health interview survey. The Annals of Pharmacotherapy, 39(4), 643–648. [DOI] [PubMed] [Google Scholar]
- Chao M. T., Wade C., Kronenberg F. (2008). Disclosure of complementary and alternative medicine to conventional medical providers: Variation by race/ethnicity and type of CAM. Journal of the National Medical Association, 100(11), 1341–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung C. K., Wyman J. F., Halcon L. L. (2007). Use of complementary and alternative therapies in community-dwelling older adults. Journal of Alternative and Complementary Medicine, 13(9), 997–1006. [DOI] [PubMed] [Google Scholar]
- Chung A., Bui L., Mills E. (2003). Adverse effects of acupuncture. Which are clinically significant? Can Family Physician, 49, 985–989. [PMC free article] [PubMed] [Google Scholar]
- Clarke T. C., Barnes P. M., Black L. I., Stussman B. J., Nahin R. L. (2018). Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief, no 325. National Center for Health Statistics. [PubMed] [Google Scholar]
- Foley H., Steel A., Cramer H., Wardle J., Adams J. (2019). Disclosure of complementary medicine use to medical providers: A systematic review and meta-analysis. Scientific Reports, 9(1), 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frass M., Strassl R. P., Friehs H., Müllner M., Kundi M., Kaye A. D. (2012). Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. Ochsner Journal, 12(1), 45–56. [PMC free article] [PubMed] [Google Scholar]
- Halpin S. N., Potapragada N. R., Bergquist S. H., Jarrett T. (2020). Use and factors associated with non-disclosure of complementary and alternative medicine among older adults. Educational Gerontology, 46(1), 18–25. [Google Scholar]
- Harris P. E., Cooper K. L., Relton C., Thomas K. J. (2012). Prevalence of complementary and alternative medicine (CAM) use by the general population: a systematic review and update. International Journal of Clinical Practice, 66(10), 924–939. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public. (2005). Complementary and Alternative Medicine in the United States. National Academies Press (US). 5, State of Emerging Evidence on CAM. https://www.ncbi.nlm.nih.gov/books/NBK83790/ [PubMed] [Google Scholar]
- Johnson D. B., Tierney M. J., Sadighi P. J. (2004). Kapalabhati pranayama: Breath of fire or cause of pneumothorax? A case report. Chest, 125(5), 1951–1952. [DOI] [PubMed] [Google Scholar]
- Jou J., Johnson P. J. (2016). Nondisclosure of complementary and alternative medicine use to primary care physicians: Findings from the 2012 National Health Interview Survey. JAMA Internal Medicine, 176(4), 545–546. [DOI] [PubMed] [Google Scholar]
- Kelak J. A., Cheah W. L., Safii R. (2018). Patient’s decision to disclose the use of traditional and complementary medicine to medical doctor: A descriptive phenomenology study (p. 2018). Evidence-Based Complementary and Alternative Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Parish A. L. (2017). Polypharmacy and medication management in older adults. Nursing Clinics, 52(3), 457–468. [DOI] [PubMed] [Google Scholar]
- Kogan M. (2018). Integrative geriatric medicine. Oxford University Press. [Google Scholar]
- Maciasz R., Kullgren J., Singer D., Solway E., Kirch M., Smith E., Malani P. (2022). Use of and interest in integrative medicine strategies. University of Michigan National Poll on Healthy Aging. 10.7302/4879 [DOI] [Google Scholar]
- Mackenzie E. R., Rakel B. (2006). Complementary and alternative medicine for older adults: A guide to holistic approaches to healthy aging. Springer Publishing Company. [Google Scholar]
- Najm W., Reinsch S., Hoehler F., Tobis J. (2003). Use of complementary and alternative medicine among the ethnic elderly. Alternative Therapies in Health and Medicine, 9(3), 50–57. [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2023). Achieving whole health: A new approach for veterans and the nation. The National Academies Press. 10.17226/26854 [DOI] [PubMed] [Google Scholar]
- National Center for Complementary and Alternative Medicine, The American Association of Retired Persons. (2011). Complementary and alternative medicine: What people aged 50 and older discuss with their health care providers. Consumer Survey Report; April13, 2010. [Google Scholar]
- National Council on Aging. (2018, June12). Healthy Aging Facts. Retrieved February 9, 2023, from https://www.ncoa.org/article/get-the-facts-on-healthy-aging
- National Institutes of Health. (2008). Time to talk about CAM: Health care providers and patients need to ask and tell. National Institutes of Health. Retrieved April 24, 2023 from https://www.nih.gov/news-events/news-releases/time-talk-about-cam
- National Library of Medicine. Bethesda (MD): National Library of Medicine (US). (2019). Complementary and Alternative Medicine. [Updated 2018 Mar 26]. https://www.ncbi.nlm.nih.gov/books/NBK518811/
- Phutrakool P., Pongpirul K. (2022). Acceptance and use of complementary and alternative medicine among medical specialists: A 15-year systematic review and data synthesis. Systematic Reviews, 11(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakel D. (2017). Integrative medicine (4th ed.). Elsevier Health Science. [Google Scholar]
- Stubbe D. E. (2018). Complementary and alternative medicine: If you don’t ask, they won’t tell. Focus, 16(1), 60–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2002). World Health Organization Health and Performance Questionnaire: Clinical Trials Baseline Version. https://www.hcp.med.harvard.edu/hpq/ftpdir/survey_clinical_7day.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ggm-10.1177_23337214231179839 for Disclosure of Complementary and Alternative Medicine Use Among Older Adults: A Cross-Sectional Study by Julia Golden, Lisa Kenyon-Pesce, Julie Robison, James Grady and Mary P. Guerrera in Gerontology and Geriatric Medicine


