Abstract
Gastrointestinal histoplasmosis remains an inconspicuous clinicopathologic entity. It is predominantly considered a protean manifestation of disseminated disease. We hereby delineate a unique case of biopsy-proven isolated colonic histoplasmosis in a patient undergoing methotrexate therapy. Furthermore, we present the first systematic review of the MEDLINE, Google Scholar, Embase, and Scopus databases regarding isolated colonic histoplasmosis in adult patients receiving immunomodulator therapy (IMT). A total of 13 case reports (level of clinical evidence: IV) were identified. The mean age was 55.6 ± 11.1 years, with 9 (69.2%) cases reported in women. Patients with subclinical disease (5, 38.5%) were often incidentally diagnosed by screening colonoscopy. Symptomatic individuals predominantly presented with diarrhea (4, 30.8%), weight loss (3, 23.1%), and/or abdominal pain (3, 23.1%). IMT was mainly administered for liver transplant (4, 30.8%), renal transplant (4, 30.8%), and ulcerative colitis (2, 15.4%). Common colonoscopy features included colonic ulcerations (7, 53.8%), polyps or pseudopolyps (3, 23.1%), and/or mass-like lesions (3, 23.1%). Diagnosis was made by histology of colonic biopsy in 11 (84.6%) and resected specimens in 2 (15.4%) patients. Treatment consisted of a combination of amphotericin B with oral itraconazole in 6 (46.2%), oral itraconazole alone in 5 (38.5%), and amphotericin B alone in 2 (15.4%) patients. Complete clinical recovery was achieved in all patients. This article illustrates that isolated colonic involvement can be the only clinical presentation of histoplasmosis. It may masquerade as other bowel disorders, presenting diagnostic and therapeutic conundrums. Gastroenterologists should rule out colonic histoplasmosis in IMT recipients who develop unexplained colitis symptoms.
Keywords: gastrointestinal histoplasmosis, isolated colonic involvement, colonoscopy, inflammatory bowel disease, immunomodulator therapy, immunosuppression
Introduction
The fungal infection with Histoplasma capsulatum often occurs in endemic areas worldwide. 1 The incidence in individuals aged 65 and older in the United States has been estimated to be 3.4 cases per 100 000 people. 2 It has predominantly been encountered in Ohio and Mississippi and in the southeastern states. 3 Histoplasma capsulatum, a dimorphic fungus, causes a self-limiting respiratory illness in immunocompetent patients. The T cells activate macrophages to engulf and clear the fungi, showing mild or no symptoms. 4 However, immunocompromised patients can present with disseminated and life-threatening infection. In these patients, T cells are unable to activate macrophages. 4 This allows fungus to remain engorged within the macrophages and spread through the blood and lymphatics to other parts of the body. 4 Disseminated disease may cause severe morbidity and mortality. Therefore, a multidisciplinary team approach is important for rapid detection and treatment.
Gastrointestinal histoplasmosis is a well-described albeit uncommon clinicopathologic entity. 5 The clinical symptomatology is frequently nonspecific, with a majority of patients experiencing nausea, vomiting, or diarrhea.5,6 Endoscopic evaluation may reveal mucosal ulcers and tumor-like polyps. 6 Significant clinical associations include human immunodeficiency virus (HIV) syndrome, organ transplantation, and autoimmune disorders.5-7 Isolated gastrointestinal histoplasmosis may mimic inflammatory bowel disease (IBD) due to similar clinical and endoscopic features. 8 However, patients who have histoplasmosis but are misdiagnosed with IBD may experience worse clinical outcomes from immunosuppressive therapy, including mortality. 9 Therefore, excluding histoplasmosis before starting treatment can be crucial in cases of suspected overlap with IBD.
We chronicle here an interesting case of biopsy-proven isolated colonic histoplasmosis with unique clinical and colonoscopy findings in a patient undergoing immunomodulator therapy (IMT). Prompt detection facilitated early treatment, resulting in an excellent clinical response. Furthermore, to our knowledge, this report represents the first systematic review discussing isolated colonic histoplasmosis in adult patients undergoing IMT. This article aims to increase community awareness of colonic histoplasmosis given the clinical importance of early diagnosis. Clinicians should remain cognizant of this differential to avoid morbidity and mortality in suspected patients with overlapping clinical features.
Illustrative Case
Presentation
A 65-year-old Caucasian female from Osseo, Wisconsin, presented to the Marshfield Medical Center Emergency Department with mild subacute diarrhea. She reported a 2-week history of 3 to 4 episodes of loose, watery bowel movements per day that were free of mucus or blood. On further review, she endorsed occasional night sweats. She denied respiratory symptoms, abdominal pain, nausea, weight loss, chest pain, fever, chills, bruising, urinary problems, or vaginal discharge. Her medical background was significant for rheumatoid arthritis on methotrexate treatment, varicose veins, a total hysterectomy for fibroids, and a bilateral mastectomy for BRCA gene mutations. She denied the use of any over-the-counter medications or herbal supplements. Her family history was remarkable for BRCA gene mutations and breast and ovarian cancers in her mother and sisters. She denied smoking, alcohol consumption, or substance use. The patient is a retired teacher. Her recent travel history included frequent visits to her daughter in Little Falls, Minnesota, near the Mississippi River. Her vital signs revealed the following: 98.5°F temperature, 92/60 mm Hg blood pressure, 24 breaths/minute respiratory rate, 74 beats/minute heart rate, and 97% oxygen saturation on room air. The abdominal examination was negative for hepatosplenomegaly. The bowel sounds were intact, with no rebound tenderness or abdominal wall rigidity.
Investigations and Diagnosis
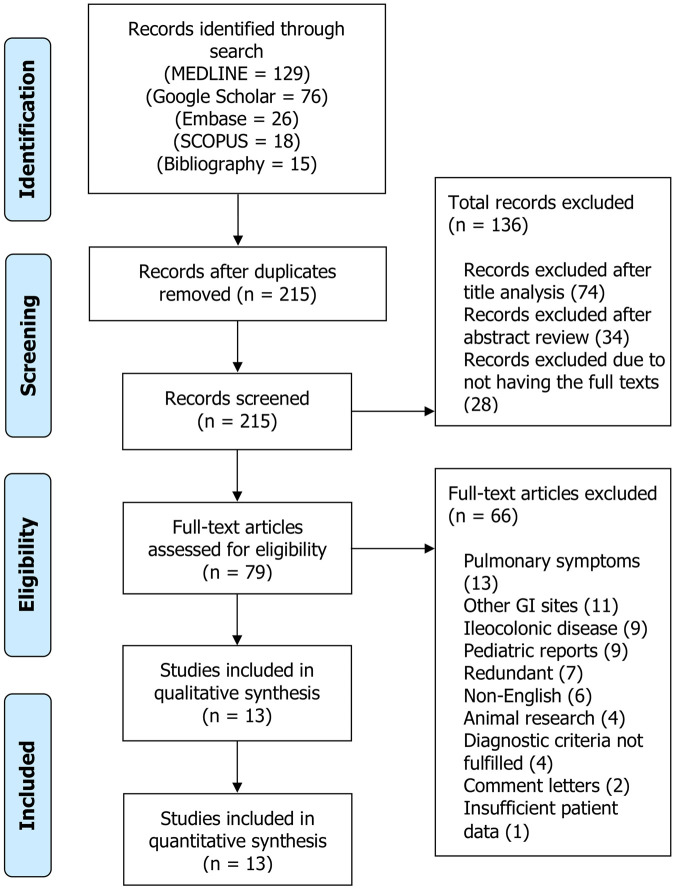
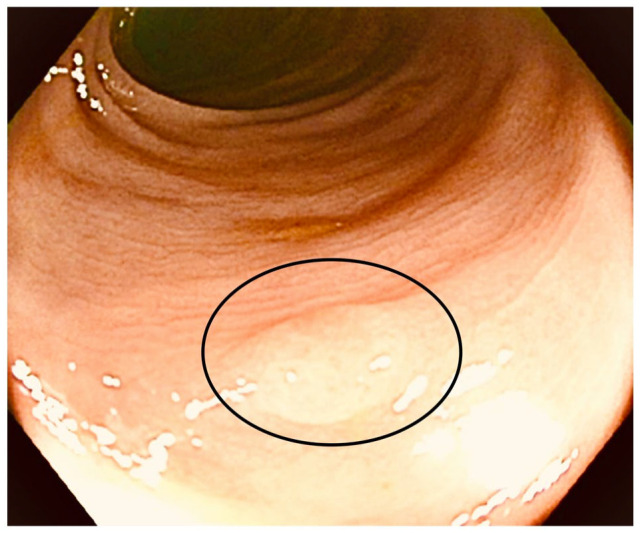
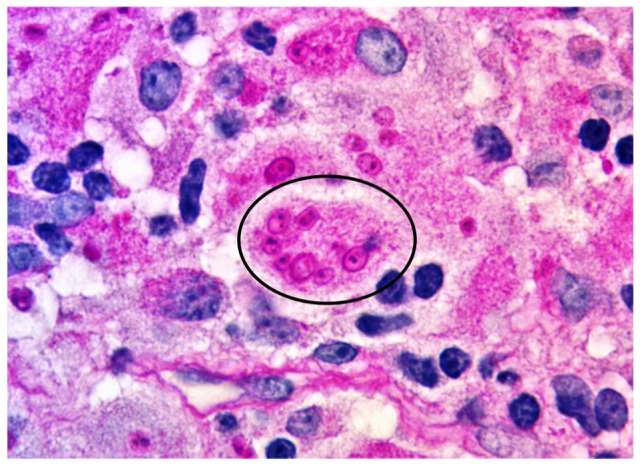
On admission, the patient underwent extensive diagnostic testing (Table 1). Colonoscopy was macroscopically normal, except for finding one small sessile polyp in the descending colon (Figure 1). There was no evidence of ischemia, ulcerations, or other mucosal abnormalities. The terminal ileum also appeared normal on up to 10 cm of endoscopic examination. Cold snare polypectomy resulted in complete en bloc endoscopic removal of the polyp. The histologic analysis of the polypectomy specimen revealed polypoid mucosa with increased foamy histiocytes without dysplasia or malignancy. The periodic acid-Schiff (PAS) stain showed intracellular yeast forms of Histoplasma (Figure 2). The intracellular presence of fungi occasionally appeared as grape-like clusters (Figure 3). Grocott-Gomori’s methenamine silver (GMS) stain showed multiple tiny yeast-like organisms, consistent with H. capsulatum (Figure 4). Random colonic biopsies were negative for microscopic colitis.
Table 1.
Laboratory Data of the Patient at the Initial Presentation.
| Laboratory parameter | Patient value | Reference range |
|---|---|---|
| Serum procalcitonin | 1.84 | <0.1 ng/mL |
| Blood osmolality | 263 | 275-295 mmol/kg |
| C-reactive protein | 4.5 | <3 mg/L |
| White cell count | 3.4 | 4.5-11.0 × 109/L |
| Platelet count | 53 × 109 | 150-450 × 109/L |
| Hemoglobin | 11.7 | 12.0-15.5 g/dL |
| Alanine aminotransferase | 20 | 0-34 IU/L |
| Aspartate aminotransferase | 21 | 15-46 IU/L |
| Alkaline phosphatase | 178 | 45-140 mg/dL |
| Total bilirubin | 1.2 | <1.2 mg/dL |
| Total protein | 6.4 | 6.3-8.5 mg/dL |
| Serum albumin | 3.9 | 3.5-5.5 mg/dL |
| Anion gap | 9 | 3-11 mmol/L |
| Blood urea nitrogen | 15 | 9-18 mg/dL |
| Serum creatinine | 1.1 | 0.6-1.3 mg/dL |
| Random blood glucose | 113 | 40-139 mg/dL |
| Thyroid-stimulating hormone | 1.85 | 0.4-4.0 mIU/L |
| Corrected serum calcium | 8.9 | 8.5-10.3 mg/dL |
| Serum magnesium | 1.7 | 0.85-1.10 mmol/L |
| Serum sodium | 132 | 136-145 mmol/L |
| Serum potassium | 3.4 | 3.5-5.1 mmol/L |
| Serum chloride | 101 | 98-107 mmol/L |
| Serum CO2 | 22 | 21-32 mmol/L |
Figure 1.
Colonoscopy showing a sessile polyp in the descending colon (circle). No other mucosal abnormalities such as ulceration, erosion, hemorrhage, edema, or punctate lesions were noted.
Figure 2.
Histologic appearance of the polypectomy specimen. The periodic acid-Schiff staining shows intracellular fungi, indicating Histoplasma capsulatum (circle). No dysplastic or malignant changes were noted.
Figure 3.
Periodic acid-Schiff stain showing intracellular yeast forms appearing as grape-like clusters of Histoplasma (circle).
Figure 4.
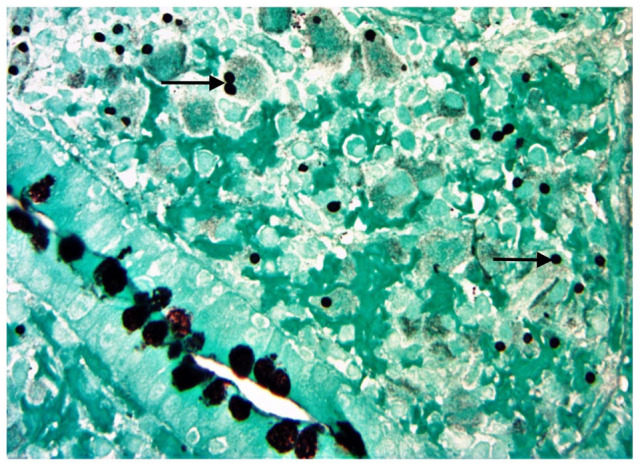
The colonic specimen stained by Grocott-Gomori’s methenamine silver showing individual and dividing Histoplasma yeast forms (arrows).
The Histoplasma urine antigen testing yielded a confirmatory result of 18.64 ng/mL (reference range: 0.20-20.00 ng/mL) (MiraVista Diagnostics, Indianapolis, Indiana). A specimen for blood culture was then obtained in a regular blood culture bottle. It came back positive for the growth of H. capsulatum after 4 weeks. The positive fungal blood culture was not sent for susceptibility testing as the patient had already started receiving an empirical antifungal treatment. Contrast-enhanced computed tomography (CT) scan of the brain, chest, and abdomen ruled out involvement of other organ systems. The testing for serum interleukin-6, amyloid A, alpha-fetoprotein, carcinoembryonic antigen, cancer antigen 19-9, and cancer antigen 125 was negative for abnormalities. None of the additional diagnostic workups identified concurrent viral, bacterial, or fungal etiologies (Table 2). The evaluation for other autoimmune diseases was also negative. Based on the workup findings and the exclusion of probable etiologies, a presumed diagnosis of isolated colonic histoplasmosis was established.
Table 2.
Diagnostic Workup for Concomitant Probable Etiologies.
| Test | Specimen source | Patient result | Reference range |
|---|---|---|---|
| Interleukin-6 | Serum | 3.4 | <6.4 pg/mL |
| Amyloid A | Serum | 11 | 10-25 mg/L |
| Alpha-fetoprotein | Serum | 2.7 | 0-9.0 ng/mL |
| Carcinoembryonic antigen | Serum | 0.03 | 0-2.5 ng/ml |
| Cancer antigen 19-9 | Serum | 7 | 0-26 ng/ml |
| Cancer antigen 125 | Serum | 19 | 0-35 U/ml |
| IgM anti-HAV antibody | Serum | Negative | Negative |
| HBsAg | Serum | 0.07 | <0.90 S/Co |
| Anti-HCV antibody | Serum | 0.04 | <0.90 S/Co |
| Cytomegalovirus DNA | Serum | Not detected | <200 copies/mL |
| HIV-1/HIV-2 antigen/antibody immunoassay | Serum | Negative | Negative |
| Mycoplasma pneumoniae IgG and IgM antibodies | Serum | Negative | Negative |
| Cryptococcus antigen | Serum | Negative | Negative |
| SARS-CoV-2 NP | Nasopharyngeal swab | Negative | Negative |
| RSV (NAT) | Nasal swab | Negative | Negative |
| Influenza A and B molecular assays | Nasal swab | Negative | Negative |
| MRSA PCR | Nasal swab | Negative | Negative |
| Blastomyces antigen | Urine | 1.7 | 0.2-14.7 ng/mL |
| Legionella antigen | Urine | Negative | Negative |
| Streptococcus pneumoniae antigen | Urine | Negative | Negative |
| Interferon gamma release assay | Whole blood | Negative | Negative |
| Sputum culture | Sputum | No growth | Negative |
| Fungal smear KOH test sputum | Sputum | Few small budding yeasts or pseudo hyphae | Negative |
Abbreviations: HAV, hepatitis A virus; HbsAg, hepatitis B surface antigen; HIV, human immunodeficiency virus; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; NP, nucleocapsid protein; RSV NAT, respiratory syncytial virus nucleic acid test; MRSA, methicillin resistant Staphylococcus aureus; PCR, polymerase chain reaction; KOH, potassium hydroxide.
Treatment and Clinical Outcome
After consultation with the infectious disease team, the patient was initiated on intravenous liposomal amphotericin B at a dose of 5 mg/kg/day. She tolerated the treatment well, with a good clinical response. After 14 days, she was switched to oral itraconazole 200 mg twice a day for 12 months. No immunosuppressant therapy was recommended for the next 1 year. Her rheumatologist prescribed naproxen 750 mg oral extended-release tablet once a day. She was advised to avoid disease-modifying antirheumatic drugs (DMARDs) due to the risk of immunosuppression. After 1 month of treatment, urine Histoplasma antigen testing revealed a level of 0.7 ng/dL. After 6 months, a follow-up appointment at the infectious disease clinic confirmed the complete clinical resolution of her symptoms. Her anemia and thrombocytopenia had also resolved, with a hemoglobin level of 12.7 g/dL and a platelet count of 154 × 109/L. The follow-up colonoscopy was unremarkable for polyps or mucosal abnormalities after 1 year of antifungal treatment. The patient reported no recurrent symptoms or signs thereafter.
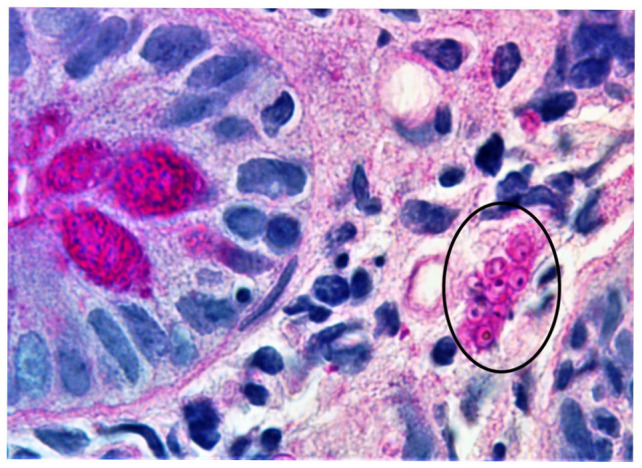
Methods
Search Strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed for this systematic review. 10 The authors performed a systematic literature search for isolated colonic histoplasmosis in the setting of IMT. The target databases included MEDLINE, Google Scholar, Embase, and Scopus. The latest search date was June 20, 2022. Specific search terms were used. The terms related to infection and drug-associated immunosuppression, such as “histoplasmosis,” “Histoplasma,” “Histoplasma capsulatum,” “fungal infection,” “immunomodulator therapy,” “IMT,” and “immunocompromised,” were combined using the Boolean operators “AND” and “OR” with the following keywords: “colon,” “colonic,” “large intestine,” “ascending colon,” “transverse colon,” and “descending colon,” with all associated permutations.
Inclusion and Exclusion Criteria
The inclusion criteria consisted of articles describing biopsy-proven isolated colonic histoplasmosis involving adult patients (≥18 years) undergoing IMT and published before June 20, 2022. The articles must report ≥5 of the following data points: patient age, sex, comorbid conditions, clinical presentations, diagnostic methods, management, and clinical outcome. The studies with no full texts available, involving pediatric patients, describing individuals with pulmonary or other symptoms, or those with endoscopic evidence of gastrointestinal involvement other than the colon or in addition to the colon, were excluded.
Eligibility and Inclusion in Analysis
Three authors independently reviewed search results to determine eligibility. The relevant full-text articles and conference papers were retrieved. Furthermore, the bibliography lists of the search results were also screened. We systematically excluded duplicate and redundant results, non-English articles, and reports with insufficient patient data. The English-language articles containing the necessary patient details were shortlisted. The disputes over inclusion were rectified by mutual consensus. The senior author granted final approval to include a study in our analysis. The initial search yielded a total of 264 articles for isolated colonic histoplasmosis in adult patients undergoing IMT. Of these, 13 studies fulfilled the inclusion criteria and were included in the case analysis. The PRISMA flow diagram outlines the methodology used for our systematic search (Figure 5).
Figure 5.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram showing the search methodology for data synthesis regarding isolated colonic histoplasmosis in adult patients receiving immunomodulator therapy.
Abbreviation: GI, gastrointestinal.
Data Collection and Statistical Analysis
Two authors independently reevaluated the full-text versions of the included papers and verified the retrieved data. The information on the patient demographics, presentation, patterns comorbidities and IMT, diagnostic workup, treatment, and clinical outcomes was thoroughly examined and documented in Microsoft Excel sheets. Descriptive statistics were used, and the data were presented as mean ± standard deviation, range, or percentage, as applicable.
Results
Patient Demographics and Comorbidities
A total of 13 case reports (clinical evidence level: IV) dating from 2007 to 2021 were identified.11-23 The mean age was 55.6 ± 11.1 years (range: 34-68 years), and 10 (76.9%) patients were above 50 years of age. A female gender predilection was noted, as 9 (69.2%) cases were reported in women. A fixed geographical distribution was not evident. However, most cases were reported from the United States 10 (76.9%), followed by France 1 (7.7%), India 1 (7.7%), and Brazil 1 (7.7%). Patients were undergoing IMT for orthotopic liver transplant (4, 30.8%), renal transplant (4, 30.8%), ulcerative colitis (2, 15.4%), psoriatic arthritis (1, 7.7%), rheumatoid arthritis (1, 7.7%), and systemic lupus erythematosus (1, 7.7%). The IMT regimens consisted of varying combinations of different agents, including tacrolimus in 7 (53.8%), mycophenolate mofetil in 6 (46.2%), prednisone in 4 (30.8%), infliximab in 3 (23.1%), methotrexate in 2 (15.4%), and/or sirolimus in 1 (7.6%) patient.
Clinical Presentations and Imaging Findings
Subclinical disease was found in 5 (38.5%) patients. As they were asymptomatic, histoplasmosis was incidentally detected during the screening colonoscopy. In symptomatic individuals, major clinical presentations were related to intermittent diarrhea in 4 (30.8%), weight loss in 3 (23.1%), abdominal pain in 3 (23.1%), fever in 3 (23.1%), and/or hematochezia in 3 (23.1%) cases. Colonoscopy findings included solitary or multiple mucosal ulcerations in 7 (53.8%), polyps or pseudopolyps in 3 (23.1%), mass-like lesions in 3 (23.1%), mucosal edema in 2 (15.4%), hemorrhagic changes in 1 (7.7%), and/or diffuse colitis in 1 (7.7%) patient. The disease involved the ascending colon in 6 (46.2%), the transverse colon in 4 (30.8%), and/or the entire colon in 3 (23.1%) patients. The descending and sigmoid segments were affected in 2 (15.4%) patients each. The CT findings were reported in 4 (30.8%) cases. The bowel wall thickening (2, 50%), colonic mass (1, 25%), and enlarged mesenteric lymph nodes (1, 25%) were among the major radiographic findings.
Diagnosis
In terms of blood workup, patients occasionally revealed low hemoglobin, low white cell count, thrombocytopenia, and deranged liver function tests. Serum or urine Histoplasma antigen testing was performed in 6 (46.2%) patients. Three (50%) of these individuals had histoplasmosis confirmed by antigen testing, whereas 3 (50%) had negative results. Pertinently, 11 (84.6%) patients were diagnosed based on the histopathologic examination of the colonic biopsy specimens. Unfortunately, 2 (15.4%) patients had to undergo extensive gastrointestinal surgeries before precise etiology establishment. In these cases, the diagnosis was confirmed by pathologic analysis of the resected colonic specimens. The diagnostic workup for concurrent viral, bacterial, and fungal infections systematically excluded other plausible differentials.
Treatment and Clinical Outcomes
The treatment consisted of various antifungal regimens: a combination of amphotericin B with oral itraconazole in 6 (46.2%), oral itraconazole alone in 5 (38.5%), and amphotericin B alone in 2 (15.4%) patients. Surgical interventions, such as a right hemicolectomy (1, 7.7%) and a total abdominal colectomy with partial proctectomy (1, 7.7%), were also reported. Clinical response to antifungal therapy was promising, achieving complete recovery in all patients. We noted case-to-case variations in the method and time interval used to assess the treatment response. In this regard, colonoscopies were reported in 6 (46.2%) patients. The follow-up duration was documented in 8 (61.5%) patients. The mean length of follow-up was 4.9 ± 4.7 months, ranging from 7 days to 12 months (Table 3).
Table 3.
Comparative Analysis of the Reported Cases of Isolated Colonic Histoplasmosis in Patients Undergoing Immunomodulator Therapy.
| Authors | Age/gender/country | Clinical presentation | Comorbid conditions and IMT | Workup | Colonoscopy findings | Histological diagnosis confirmation | Treatment | Clinical outcome, follow-up |
|---|---|---|---|---|---|---|---|---|
| Ghassemi et al 11 | 42/F/USA | Watery diarrhea, intermittent fever, and weight loss | Renal transplant 3 years prior on tacrolimus and MMF | Normal WBC count, hemoglobin 10 g/dL, stool negative for pathogens | Multiple scattered ulcers (1-3 cm in diameter) throughout the colon | Biopsy | Amphotericin B; oral itraconazole | Symptoms resolved within 1 wk |
| Ordonez et al 12 | 68/F/USA | Screening colonoscopy | Psoriatic arthritis treated with methotrexate and infliximab | Colonoscopy 7 y prior was normal | Ulceration, pathology reported benign findings | Biopsy of resected specimen | Pathology of RHC specimen confirmed histoplasmosis; itraconazole | Colonoscopy 2 mo postop revealed normal mucosa |
| Mavrogenis et al 13 | 55/M/France | Rectal bleeding, abdominal pain, and weight loss | Renal transplant 2 y prior on prednisone, tacrolimus, MMF | CT: a 5-cm thickened, stenotic segment of the right colon and enlarged mesenteric lymph nodes | A 5-cm right colonic ulcer and multiple ulcerated and nonulcerated pseudopolyps | Biopsy | Amphotericin B; oral itraconazole | Colonoscopy and CT scan were normal after 4 mo |
| Soape et al 14 | 59/M/USA | Abdominal pain, diarrhea, and weight loss | Rheumatoid arthritis on infliximab and methotrexate, truck driver | CT: diffuse omental caking with transverse colon masses | A near-obstructing, cancer-like colonic mass | Biopsy | Loop ileostomy for possible obstruction; amphotericin B for 2 wk and itraconazole for 6 wk |
Recovered; ileostomy was later reversed |
| Garg et al 15 | 51/F/USA | Routine screening colonoscopy | SLE (chronic steroids and MMF), ESRD on hemodialysis | CT: focal area of thickening in distal ascending colon. Urine Histoplasma antigen (–) | A submucosal-appearing ulcerated 3-cm mass in the distal ascending colon | Biopsy | Itraconazole once daily for 6 mo | Repeat colonoscopy 6 mo later was normal |
| Sharma et al 16 | 68/F/India | Loose stools, anorexia, and weakness | OLT for hepatitis C-related CLD 5 y prior | CT: ileal thickening with pancreatic cystic attenuation | Multiple small linear ulcer with normal intervening mucosa in transverse colon | Biopsy | Amphotericin B | Recovered, 3 mo |
| Henke et al 17 | 43/M/USA | Progressive abdominal pain and distention | Ulcerative colitis for 12 y | Serum and urine Histoplasma antigens were “weakly (+), but below the level of quantification” | Single 2-cm discrete ulcer with heaped-up edges in the distal ascending colon | Biopsy | Amphotericin for 2 wk, itraconazole for 12 mo | Recovered |
| Krishna et al 18 | 34/F/USA | Fever, hypotension, AMS, hematochezia, and refractory anemia requiring blood transfusions | Ulcerative pancolitis on infliximab complicated by recurrent CDI requiring FMT | ALP 1009, ALT 120, AST 293 U/L, CMV PCR and urine Histoplasma (+), Histoplasma (+) but CMV (–) on sigmoidoscopy and colectomy pathology | Sigmoidoscopy with biopsies demonstrating diffuse colitis | Biopsy and resected specimen | Ganciclovir and amphotericin B, TAC and PP, amphotericin B; itraconazole | Recovered |
| Higley et al 19 | 68/F/USA | Hematochezia | Renal transplant on immunosuppressives | Hemoglobin 5.3 g/dL, Histoplasma galactomannan urinary antigen (+) | Nodular mucosa, focal blanching, and hemorrhagic appearance in the entire colon | Biopsy | Amphotericin B for 2 wk; itraconazole | Recovered |
| Zalkin et al 20 | 67/M/USA | Asymptomatic, screening colonoscopy | Renal transplant on tacrolimus, MMF, and prednisone | Urine Histoplasma antigen (–) | Sub-centimeter ulcerations in the descending and transverse colons, all upon a pale, raised granular area | Biopsy | Itraconazole | Recovered |
| Ferreira et al 21 | 60/F/Brazil | Colon cancer screening | OLT for alcoholic cirrhosis on tacrolimus, MMF, and prednisone, UGIB | Hemoglobin 9.3 g/dL, thrombocytopenia 138,000 platelets/µL, INR 1.5, albumin 2.8 g/dL | Eight colonic polyps: cecum 1, ascending colon 2, transverse colon 4, and sigmoid colon 1 of 12 mm | Biopsy | Itraconazole for 12 mo | After 1 y of treatment, colonoscopy showed normal mucosa |
| Spallone et al 22 | 51/F/USA | Intermittent diarrhea | CKD and AIH status post OLT 12 y prior on MMF and sirolimus | Tests for AFB, fungal organisms, and routine bacterial cultures and CMV and HH1 were (–) | Ulcerated, friable mass suspicious for malignancy in the ascending colon | Biopsy | Itraconazole not tolerated; amphotericin B for 2 wk | Colonoscopy after 1 mo showed normal mucosa |
| Cui et al 23 | 57/M/USA | Asymptomatic, surveillance colonoscopy | OLT for chronic HCV cirrhosis and HCC, on tacrolimus, adenomatous colon polyps | Histoplasma urine antigen 0.51 ng/mL | Numerous sessile, partially ulcerated, colonic polyps throughout the colon | Biopsy | Itraconazole for 12 mo | Recovered, 12 mo |
Abbreviations: IMT, immunomodulator therapy; MMF, mycophenolate mofetil; WBC, white blood cell; RHC, right hemicolectomy; CT, computed tomography; SLE, systemic lupus erythematosus; ESRD, end-stage renal disease; OLT, orthotopic liver transplantation; CLD, chronic liver disease; AMS, altered mental status; CDI, Clostridium difficile infection; FMT, fecal microbiota transplantation; ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate aminotransferase; CMV, cytomegalovirus; TAC, total abdominal colectomy; PP, partial proctectomy; UGIB, upper gastrointestinal bleeding; INR, international normalized ratio; CKD, chronic kidney disease; AIH, autoimmune hepatitis; HH1, human herpesviruse 1; HCV, hepatitis C virus.
Discussion
To our knowledge, this article is the first systematic review evaluating diagnostic and therapeutic trends of isolated colonic histoplasmosis in adult patients undergoing IMT.
Symptomatic gastrointestinal histoplasmosis is encountered in only 3% to 12% of patients. 24 Contrarily, an autopsy series revealed that up to 70% of the individuals with disseminated disease had gastrointestinal involvement. 25 This finding suggests that subclinical gastrointestinal histoplasmosis is more common than previously thought, making it an under-recognized condition. In immunocompetent hosts, gastrointestinal histoplasmosis is reported in only 0.05% of cases but has higher odds of affecting immunocompromised patients.26-28 It can be attributed to the increased probability of disseminated disease among immunocompromised hosts. Several risk factors have been implicated in the dissemination to other organs, including advanced age, organ transplantation, HIV syndrome, blood cancers, and IMT.26-29 Histoplasmosis may affect any segment of the gastrointestinal tract, mainly due to the lymph node seeding from hematogenous spread.6,30 However, the most frequently involved sites are the terminal ileum and the colon.5,6,30 Surprisingly, there is still a dearth of published data on isolated colonic histoplasmosis in the setting of IMT.
In patients with gastrointestinal histoplasmosis, 4 common pathological forms have been described: (1) subclinical and microscopic cluster formation, consisting of macrophages in the lamina propria; (2) plaques and pseudopolyps caused by fungi-containing macrophages; (3) tissue necrosis and ulceration resulting in abdominal pain, diarrhea, and hemorrhage; and (4) localized thickening and inflammation of the bowel wall.5,31,32 As a result, focal or multiple mucosal ulcers, polyps, strictures, and obstructing mass lesions are often found in gastrointestinal histoplasmosis. 32 In our review, the colonoscopic features of isolated colonic disease were in line with the aforementioned observations. Imaging features can be related to intestinal wall thickening or mass-like lesions obstructing the lumen. 32 As gastrointestinal histoplasmosis is typically indicative of disseminated disease, its detection can be further aided by imaging studies. Abdominal ultrasound and CT may reveal liver or spleen enlargement, deep adenopathies, adrenal masses, or ascites.33,34
Histoplasmosis can frequently mimic other disorders such as IBD, lymphoma, tuberculosis, certain infections, or cancer due to the nonspecific colonoscopic findings.29,35-40 The overlapping presentation patterns, similar gastrointestinal site involvement, and inflammatory changes associated with both conditions may contribute to its misdiagnosis as IBD.9,41 Immunosuppressive therapy after a misdiagnosis may lead to disastrous clinical outcomes in hosts with already compromised immune systems.9,41 Therefore, gastroenterologists and endoscopists should maintain a low diagnostic threshold for gastrointestinal histoplasmosis in suspected patients. Before starting IBD treatment, a meticulous exclusion of such infectious etiologies should be performed. Strict protocols should be developed for histoplasmosis screening. The overlapping clinical presentations, travel history, and possible exposure are important factors in this regard. Moreover, an effective multidisciplinary clinical approach should be adopted, particularly in the communication between gastroenterologists and pathologists.
Serum or urine Histoplasma antigen testing can often aid detection. 42 Several biochemical tests are used in this regard. The urinary antigen was positive in approximately 95% of immunosuppressed patients with disseminated disease. 43 Newer techniques such as quantitative enzyme immunoassay, lateral flow assay, and detection of Histoplasma galactomannan can be used for an early presumptive diagnosis of histoplasmosis.44,45 For antibodies, it takes 4 to 8 weeks to become detectable after an acute infection. 46 Three common ways to test for Histoplasma antibodies include enzyme immunoassay, immunodiffusion, and complement fixation. 46 The most sensitive serological test is complement fixation testing using yeast antigen. 46 Immunodiffusion is the most specific serological test. 46 In our patient, the Histoplasma urine antigen testing yielded a confirmatory result of 18.64 ng/mL. This finding tailored our diagnostic approach, resulting in subsequent diagnosis of colonic histoplasmosis.
In our review, Histoplasma antigen testing was reported in only 6 (42.6%) cases. Of these, it showed positive results in 3 (50%) patients. Nonetheless, the diagnostic confirmation was obtained from the histological examination of the biopsies or resected colonic specimens. Ekeng et al 47 conducted a descriptive review of gastrointestinal histoplasmosis from 2001 to 2021. Of the included 123 cases, 109 (88.6%) were diagnosed by histopathology. 47 It shows that histological analysis can play a vital role in detecting this serious infection early in the course of the disease, especially in immunocompromised patients. Therefore, the use of specific fungal stains on biopsy specimens from the colon should be considered in suspected patients to prevent misdiagnosis, even in nonendemic areas. On histological examination, the presence of granuloma is not required to confirm the diagnosis. 48 In a case series of 6 patients with gastrointestinal histoplasmosis from North India, none of the patients had granuloma on histological analysis. 48 The PAS staining revealed the presence of multiple intracellular and extracellular organisms with eccentrically placed nuclei and a peripheral halo, suggestive of histoplasmosis. 48 Therefore, special stains such as GMS and PAS often help in the characterization of the fungal cell wall, leading to the identification of Histoplasma.
The Infectious Diseases Society of America recommends treatment of moderate and moderate-to-severe disseminated histoplasmosis with initial amphotericin B for 1 to 2 weeks followed by itraconazole administration for 12 months. 49 Wheat et al 50 showed that liposomal amphotericin B results in more rapid clearance of fungal burden compared with itraconazole. The findings of this clinical trial further support the initial amphotericin B use for moderately severe or severe histoplasmosis. 50 Itraconazole is a preferred maintenance treatment unless the patient is on proton-pump inhibitors. Lahner et al 51 showed in their systematic review that co-administration of proton-pump inhibitors may impair absorption of itraconazole. In the case series reported from India, all 6 patients with gastrointestinal histoplasmosis were successfully treated with injectable amphotericin B for 2 weeks, followed by twice-daily 200 mg oral itraconazole. 48 At the 4-week follow-up, endoscopy was performed in 4 patients, which showed healing of esophageal and ileo-colonic mucosal lesions. 48
In our systematic review, transplant recipients constituted the largest group affected by isolated colonic histoplasmosis in the setting of IMT. With regard to histoplasmosis treatment, no difference exists between transplant recipients and the general population. 52 The discontinuation of antifungal therapy after 12 months has been considered safe. 52 In patients with gastrointestinal histoplasmosis, early treatment is imperative to avoid the serious sequelae, including intestinal perforation and hemorrhage. No specific follow-up guidelines are available. However, patients may be evaluated for persistent mucosal abnormalities with repeat colonoscopies and biopsies.
The patient involved in this study represents a rare case of isolated colonic histoplasmosis in the setting of IMT. She belonged to a nonendemic region of the United States but reported a positive travel history to Mississippi in the past. The clinical presentation was unique in that it was only related to watery diarrhea, without any extraintestinal or pulmonary symptoms. Furthermore, her colonic mucosa was unrevealing of marked inflammatory changes, as only a sessile polyp was a positive finding. However, she became symptomatic and developed diarrhea. The histological examination of the polypectomy specimen confirmed histoplasmosis, and appropriate treatment resulted in a favorable clinical outcome. This case emphasizes the value of a careful endoscopic examination and the removal or biopsy of all colonic polypoid lesions. Furthermore, we presented a systematic review summarizing existing clinical evidence to increase community awareness about this unique clinicopathologic entity as it can pose diagnostic and therapeutic challenges in clinical practice.
Conclusion
Isolated colonic histoplasmosis in the setting of IMT remains a rare clinical entity. It can present as the only clinical sign of disseminated histoplasmosis. Due to its overlapping features with IBD, it may potentially expose patients to mistreatment with immunosuppressive agents. Therefore, it should be carefully excluded before treatment initiation, particularly in immunocompromised patients. Colonoscopy with biopsy can play a pivotal role in the detection. Gastroenterologists and endoscopists should remain vigilant for histoplasmosis in individuals on IMT presenting with compatible symptomatology or in asymptomatic cases during surveillance colonoscopy.
Footnotes
Authors’ Note: This paper was presented as an abstract at the Annual Scientific Meeting of the American College of Gastroenterology, October 21-26, 2022, in Charlotte, NC, USA.
ICMJE Author Contributions: FI and GN: study conception and design, systematic review of the medical databases, data tabulation, and drafting of the article. AA, MA, and MH: data acquisition and drafting of the work. MS, ZUH, and ST: data analysis and revisions of the manuscript. RI: data interpretation and study supervision by reviewing, revising, and improving the manuscript by suggesting critical modifications. All authors carefully assessed and edited the manuscript and gave their final approval of the version to be published. All authors are accountable for all aspects of the work.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Informed consent was obtained before publication. Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
Human Rights: All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
ORCID iD: Faisal Inayat  https://orcid.org/0000-0001-7576-7319
https://orcid.org/0000-0001-7576-7319
References
- 1.Conces DJ., Jr.Histoplasmosis. Semin Roentgenol. 1996;31:14-27. [DOI] [PubMed] [Google Scholar]
- 2.Baddley JW, Winthrop KL, Patkar NM, et al. Geographic distribution of endemic fungal infections among older persons, United States. Emerg Infect Dis. 2011;17:1664-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linder KA, Kauffman CA. Histoplasmosis: epidemiology, diagnosis, and clinical manifestations. Curr Fungal Infect Rep. 2019;13:120-128. [Google Scholar]
- 4.Mittal J, Ponce MG, Gendlina I, Nosanchuk JD. Histoplasma capsulatum: mechanisms for pathogenesis. Curr Top Microbiol Immunol. 2019;422:157-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamps LW, Molina CP, West AB, Haggitt RC, Scott MA. The pathologic spectrum of gastrointestinal and hepatic histoplasmosis. Am J Clin Pathol. 2000;113(1):64-72. [DOI] [PubMed] [Google Scholar]
- 6.Kahi CJ, Wheat LJ, Allen SD, et al. Gastrointestinal histoplasmosis. Am J Gastroenterol. 2005;100:220-231. [DOI] [PubMed] [Google Scholar]
- 7.Miller R, Assi M, AST Infectious Diseases Community of Practice. Endemic fungal infections in solid organ transplant recipients-Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13553. [DOI] [PubMed] [Google Scholar]
- 8.Dahiya D, Kichloo A, Singh J, et al. Histoplasmosis and inflammatory bowel disease: a case report. World J Gastrointest Endosc. 2021;13:24-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agrawal N, Jones DE, Dyson JK, et al. Fatal gastrointestinal histoplasmosis 15 years after orthotopic liver transplantation. World J Gastroenterol. 2017;23:7807-7812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghassemi KF, Wang RT, Muthusamy VR, et al. Colonic histoplasmosis. Gastroenterol Hepatol (N Y). 2007;3:459-460. [PMC free article] [PubMed] [Google Scholar]
- 12.Ordonez M, Fahy B, Sessoms S, et al. Colonic histoplasmosis mimicking malignant ulceration. Am J Gastroenterol. 2010;105:345.19888204 [Google Scholar]
- 13.Mavrogenis G, Coumaros D, Bazin D, Renard C, Moulin B, Bellocq JP. Giant colonic ulcer and pseudopolyps in an immunodepressed patient. Endoscopy. 2011;43(10):926-7; author reply 927. [DOI] [PubMed] [Google Scholar]
- 14.Soape M, Romano R, Thirumala S, et al. Disseminated histoplasmosis involving the colon and omentum: a rare presentation in the setting of IMT. Am J Gastroenterol. 2013;108:376.23358462 [Google Scholar]
- 15.Garg L, Purohit T, Lazarczyk D. There’s more than meets the eye: histoplasma mimicking colon neoplasm. Am J Gastroenterol. 2014;109:403. [Google Scholar]
- 16.Sharma R, Lipi L, Gajendra S, et al. Gastrointestinal histoplasmosis: a case series. Int J Surg Pathol. 2017;25:592-598. [DOI] [PubMed] [Google Scholar]
- 17.Henke J, Fathallah J, Hinthorn D, et al. Colonic histoplasmosis mimicking metastatic colon cancer in a patient with ulcerative colitis on infliximab. Am J Gastroenterol. 2019;114:59. [Google Scholar]
- 18.Krishna P, Muhammad H, Florence-Damilola O, et al. Primary colonic histoplasmosis secondary to fecal microbiota transplantation in a patient with ulcerative colitis on anti-TNF alpha. Am J Gastroenterol. 2019;114:59. [Google Scholar]
- 19.Higley C, Cherian N, Steinberg J, et al. Hematochezia? Think histoplasmosis. Am J Gastroenterol. 2019;114:1113-1115. [Google Scholar]
- 20.Zalkin D, Ho TH, Panarelli NC, et al. Histoplasmosis presenting as isolated colonic granulomas in an immunocompromised patient. Am J Gastroenterol. 2020;115:844. [Google Scholar]
- 21.Ferreira GSA, Watanabe ALC, Trevizoli NC, et al. Colonic infection by histoplasma capsulatum in a liver transplant patient: a case report. Transplant Proc. 2020;52(5):1413-1416. [DOI] [PubMed] [Google Scholar]
- 22.Spallone A, Dhal U, Woc-Colburn L, et al. Histoplasmosis in liver transplant recipients: case reports and a review of the literature. OBM Transplantation. 2020;4:103. [Google Scholar]
- 23.Cui M, Wong RCK, Gholam PM. Colonic histoplasmosis presenting as polyps in an asymptomatic patient with liver transplant. ACG Case Rep J. 2021;8(5):e00598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wheat LJ, Connolly-Stringfield PA, Baker RL, et al. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore). 1990;69(6):361-374. [DOI] [PubMed] [Google Scholar]
- 25.Goodwin RA, Jr, Shapiro JL, Thurman GH, Thurman SS, Des Prez RM. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine (Baltimore). 1980;59(1):1-33. [PubMed] [Google Scholar]
- 26.Psarros G, Kauffman CA. Colonic histoplasmosis: a difficult diagnostic problem. Gastroenterol Hepatol (N Y). 2007;3(6):461-463. [PMC free article] [PubMed] [Google Scholar]
- 27.Yang B, Lu L, Li D, et al. Colonic involvement in disseminated histoplasmosis of an immunocompetent adult: case report and literature review. BMC Infect Dis. 2013;13:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suh KN, Anekthananon T, Mariuz PR. Gastrointestinal histoplasmosis in patients with AIDS: case report and review. Clin Infect Dis. 2001;32:483-491. [DOI] [PubMed] [Google Scholar]
- 29.Zhu L, Zhang W, Yang L, et al. Disseminated histoplasmosis: intestinal multiple ulcers without gastrointestinal symptoms in an immune competent adult. J Cytol Histol. 2014;5:231. [Google Scholar]
- 30.Cappell MS, Mandell W, Grimes MM, et al. Gastrointestinal histoplasmosis. Dig Dis Sci. 1988;33:353-360. [DOI] [PubMed] [Google Scholar]
- 31.Panchabhai TS, Bais RK, Pyle RC, Mitchell CK, Arnold FW. An apple-core lesion in the colon: an infectious etiology. J Glob Infect Dis. 2011;3(2):195-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhu LL, Wang J, Wang ZJ, et al. Intestinal histoplasmosis in immunocompetent adults. World J Gastroenterol. 2016;22:4027-4033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radin DR. Disseminated histoplasmosis: abdominal CT findings in 16 patients. AJR Am J Roentgenol. 1991;157(5):955-958. [DOI] [PubMed] [Google Scholar]
- 34.Nacher M, Valdes A, Adenis A, et al. Gastrointestinal disseminated histoplasmosis in HIV-infected patients: a descriptive and comparative study. Plos Negl Trop Dis. 2021;15(1):e0009050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehmood A, Abdullah HMA, Inayat F, et al. Wolf in the sheep’s clothing: intestinal angioedema mimicking infectious colitis. BMJ Case Rep. 2018;11:e226682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inayat F, Hussain Q, Shafique K, et al. Cytomegalovirus colitis in immunocompetent patients. Cureus. 2016;8:e869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saleem S, Ishtiaq R, Inayat F, Aziz M, Bleibel W. Gastrointestinal and liver manifestations in COVID-19 population. Middle East J Dig Dis. 2021;13(4):281-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Inayat F, Jafar MS, Ali NS, Hussain Q, Hurairah A. Enigma of extrapulmonary tuberculosis: where do we stand? Cureus. 2017;9:e1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mehmood A, Ehsan A, Mukhtar M, et al. Acute mesenteric tuberculous lymphadenitis: a comparative analysis of twenty-one cases. Cureus. 2019;11:e4454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Inayat F, Hassan GU, Tayyab GUN, Saif MW. Post-transplantation lymphoproliferative disorder with gastrointestinal involvement. Ann Gastroenterol. 2018;31(2):248-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahmed A, Homsi N, Kapila R. Crohn’s disease or histoplasmosis? A case of severe disseminated histoplasmosis mimicking Crohn’s disease and literature review. Med Mycol Case Rep. 2020;30:8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guimarães AJ, Nosanchuk JD, Zancopé-Oliveira RM. Diagnosis of histoplasmosis. Braz J Microbiol. 2006;37:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hage CA, Ribes JA, Wengenack NL, et al. A multicenter evaluation of tests for diagnosis of histoplasmosis. Clin Infect Dis. 2011;53(5):448-454. [DOI] [PubMed] [Google Scholar]
- 44.Theel ES, Harring JA, Dababneh AS, Rollins LO, Bestrom JE, Jespersen DJ. Reevaluation of commercial reagents for detection of Histoplasma capsulatum antigen in urine. J Clin Microbiol. 2015;53(4):1198-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cáceres DH, Gómez BL, Tobón AM, Chiller TM, Lindsley MD. Evaluation of a Histoplasma antigen lateral flow assay for the rapid diagnosis of progressive disseminated histoplasmosis in Colombian patients with AIDS. Mycoses. 2020;63(2):139-144. [DOI] [PubMed] [Google Scholar]
- 46.Azar MM, Loyd JL, Relich RF, Wheat LJ, Hage CA. Current concepts in the epidemiology, diagnosis, and management of histoplasmosis syndromes. Semin Respir Crit Care Med. 2020;41(1):13-30. [DOI] [PubMed] [Google Scholar]
- 47.Ekeng BE, Itam-Eyo AE, Osaigbovo II, et al. Gastrointestinal histoplasmosis: a descriptive review, 2001-2021. Life (Basel). 2023;13:689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mandavdhare HS, Shah J, Prasad KK, et al. Gastrointestinal histoplasmosis: a case series from a non-endemic region in North India. Intest Res. 2019;17(1):149-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:807-825. [DOI] [PubMed] [Google Scholar]
- 50.Wheat LJ, Cloud G, Johnson PC, et al. Clearance of fungal burden during treatment of disseminated histoplasmosis with liposomal amphotericin B versus itraconazole. Antimicrob Agents Chemother. 2001;45(8):2354-2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lahner E, Annibale B, Delle Fave G. Systematic review: impaired drug absorption related to the co-administration of antisecretory therapy. Aliment Pharmacol Ther. 2009;29:1219-1229. [DOI] [PubMed] [Google Scholar]
- 52.Gajurel K, Dhakal R, Deresinski S. Diagnosis and treatment of histoplasmosis in solid organ transplant patients. Curr Opin Infect Dis. 2018;31(4):301-308. [DOI] [PubMed] [Google Scholar]