Abstract
Purpose: The capacity to recover motor function with pathology or age-related decline is termed physical resilience. It is unknown what outcome domains are captured with existing measurement instruments. Thus, this scoping review aimed to identify measurement instruments for physical resilience, identify research gaps, and make recommendations for future research. Methods: Articles were included from the search when their subject matter included the term resilience in relation to the physical health of older adults. Data on physical resilience measurement instruments were extracted using the outcome domains: body function or structure, activity and participation, and societal impact. Results: The majority of the 33 included articles involved older adults with fractures, cardiac conditions, and cancer. Many measurement instruments quantified body function or structure, and some instruments captured activity and participation, and societal impact of physical resilience. Measurement instruments were pooled into 4 categories: psychological, physiological, motor function, and psychosocial scales. No studies combined all areas of measurement. Conclusions: A potential gap of a measurement instrument capturing social aspects of physical resilience was identified. Comprehensive measurement could identify which outcome domains could be targeted to foster resilience. This knowledge might be useful across many health disciplines and contribute to therapeutic decision-making and rehabilitation strategies.
Key words: motor skills, physical functional performance, physiology, sociology, walking
Abstract
Objectif : la résilience physique désigne la capacité de recouvrer sa fonction motrice malgré le déclin lié à une pathologie ou à l’âge. On ne sait pas quels domaines de résultats cliniques les instruments de mesure actuels saisissent. Ainsi, la présente étude de portée visait à déterminer les instruments pour mesurer la résilience physique, repérer les lacunes de la recherche et faire des recommandations en vue des futures recherches. Méthodologie : les articles de la recherche étaient conservés lorsque leur sujet incluait le terme resilience à l’égard de la santé physique des personnes âgées. Les chercheurs ont extrait les données sur les instruments de mesure de la résilience physique au moyen des domaines de résultats suivants : fonction ou structure corporelle, l’activité et la participation et les répercussions sociétales. Résultats : la majorité des 33 articles inclus portaient sur des personnes âgées ayant des fractures, des affections cardiaques et un cancer. De nombreux instruments de mesure quantifiaient la fonction ou la structure corporelle et certains saisissaient l’activité, la participation et les répercussions sociétales de la résilience physique. Les chercheurs ont regroupé les instruments de mesure en quatre catégories : échelles psychologique, physiologique, de la fonction motrice et psychosociale. Aucune étude ne combinait tous les domaines de mesure. Conclusions : les chercheurs ont repéré une lacune potentielle d’un instrument qui saisit les aspects sociaux de la résilience physique. Une mesure exhaustive pourrait déterminer les domaines de résultat à cibler pour favoriser la résilience. Ces connaissances pourraient être utiles dans de nombreuses disciplines et contribuer aux décisions thérapeutiques et aux stratégies de réadaptation.
Mots-clés : : marche, motricité, performance fonctionnelle physique, physiologie, sociologie
Frequently, research involving ageing concentrates on illness or the pathogenic aspects of disease,1 but interest is growing in a more positive aspect of ageing, namely resilience,2–4 the capacity to recover or resist the adverse effects of a stressor.5–7 Not simply the absence of pathology or disease, resilience is a dynamic, adaptive process.8 It is a multifaceted concept that entails psychological features, social relationships, environment, genetics, and biology.9 Although understudied compared with research on illnesses or diseases that impact older adults, resilience is associated with more positive trajectories of ageing.2,10–12
Considering multiple trajectories of recovery are observed and not fully explained by biological factors,13–15 a budding construct stemming from this work is physical resilience. This term is relatively recent, with a lack of consensus on its definition or measurement. A description may include “resilience for physical functioning” consider that aspects of resilience may include psychological or social in nature. A recent review of the physical resilience construct found that only 38% of articles sufficiently defined resilience.6 Further, some definitions include an aspect of “robustness” while others do not.16 This lack of definition consensus may contribute to incomplete or inconsistent measurement. For the purposes of this article, physical resilience is defined as the ability to recover/optimize function amongst disease- or age-related physical losses.6,17 Physical resilience, as it relates to older adults, is conceptualized “at the whole person level: a characteristic which determines one’s ability to resist or recover from functional decline following health stressor(s).”6 The likelihood of experiencing comorbidities and physical impairments that affect one’s ability to be mobile and independent in the community increases with age, such as a decline in motor functions like walking ability and speed after a stroke or hip fracture.18,19 Given that it is difficult to preserve motor function with ageing,20,21 high levels of physical resilience may provide individuals with lower risks of injury and mortality as well as increase the number of years of independent mobility.
Outside of age-related alterations to motor function, physiological factors can also influence levels of physical resilience. Heart rate, blood pressure, and postural sway are examples of physiological responses to physical stressors, and considered to be measures of resilience as acute changes in these parameters can be associated with longer-term trajectories of health; for example, recovery of physical function after bedrest requires regaining muscle strength and cardiorespiratory status to baseline levels.5 Moreover, physically resilient individuals can be identified by genetic or neuroendocrine variations related to resilient trajectories.8 Critically, little research examines links between motor function and physiological measures in the context of physical resilience. According to the lifecourse model of multimorbidity resilience, resilience can arise from multiple factors that together contribute to coping and recovery from illness.22 The individual, social, and environmental resources that need to be mobilized to achieve recovery or a state of multimorbidity wellness are complex.22,23 Comprehensive measurements of physical resilience may contribute to, for example, therapeutic decision-making, pre-habilitation strategies, and quicker detection of complications;5 however, a broad review of the literature pooling these measurement instruments is lacking.
Three main methodologies for resilience measurement are psychometric, definition-driven, and data-driven approaches;24 however, these measurement methodologies are not specific to physical resilience, and so physical resilience quantification may use an assortment of measurement instruments. To understand how physical resilience is currently measured, and to capture the individual and psychosocial aspects that support recovery or maintenance of motor function with ageing, we must examine a range of literature25,26 Complex interactions among sociological, psychological, and biological factors are likely to account for why some individuals may exhibit physical resilience, and therefore can recover independent levels of mobility in the face of an illness. Some aspects of physical resilience have been studied, but physiology and motor function factors have not been examined concurrently in one scoping review.5,6 A wide search strategy allows for the possibility to discover connections among physiological and motor function factors (along with psychological and psychosocial factors), and to map potential elements that may foster physical resilience. To better understand the current state of the evidence and to identify gaps, we used a scoping review framework to comprehensively examine the literature on how physical resilience in older adults is quantified or measured. The objectives of this scoping review were to: (1) identify outcome domains, subdomains, and measurement instruments for physical resilience based on Boers and colleagues (2014);27 (2) map the key concepts of physical resilience as represented in measurement instruments for it; and (3) identify methodological gaps and make recommendations for future research. Outcome domains and subdomains were considered to be the underlying constructs that the measurement instruments assessed (i.e., domains/subdomains are what is being measured), while measurement instruments themselves are how physical resilience was measured.
Methods
Study design
The scoping review methods employed in support of this research have been reported in detail,26 are briefly described below, and were conducted according to the framework proposed by Arksey and O’Malley,28 among others.29–31
Stage 1: Identify the research objective
This scoping review aimed to: (1) identify outcome domains, subdomains, and measurement instruments for physical resilience based on Boers and colleagues;27 (2) map the key physical resilience concepts as represented in the identified measurement instruments; and (3) identify gaps and make recommendations for future research. To facilitate the scoping review objectives, older adults were defined as ≥ 65 years of age, and the use of physical resilience required that the resilience be applied in relation to the physical health of older adults.
Stage 2: Identify relevant studies
Relevant articles were identified in Scopus, Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE, Web of Science, PsycInfo, and AgeLine through a search conducted from inception through to March 14, 2018, and the search was updated on October 31, 2019, to identify any additional citations. These databases were chosen to ensure comprehensive coverage of ageing and rehabilitation publications. The key concepts of resilience and older adults were searched with both Medical Subject Headings (MeSH) and keyword searches. Based on the search terms employed in previous resilience reviews,24,32 the MeSH terms resilience, psychological, aging, and aged were used, and supplemented with keyword searches of terms such as resilience, aging, ageing, elderly, and older adult. The search strategies for all databases are provided in the protocol paper.26 The search results were uploaded into EndNote (version 6.0.2) and duplicates were removed prior to screening. Overall, over 16,000 unique citations were identified (Figure 1, online Appendix 1).
Figure 1 .
PRISMA flow diagram.
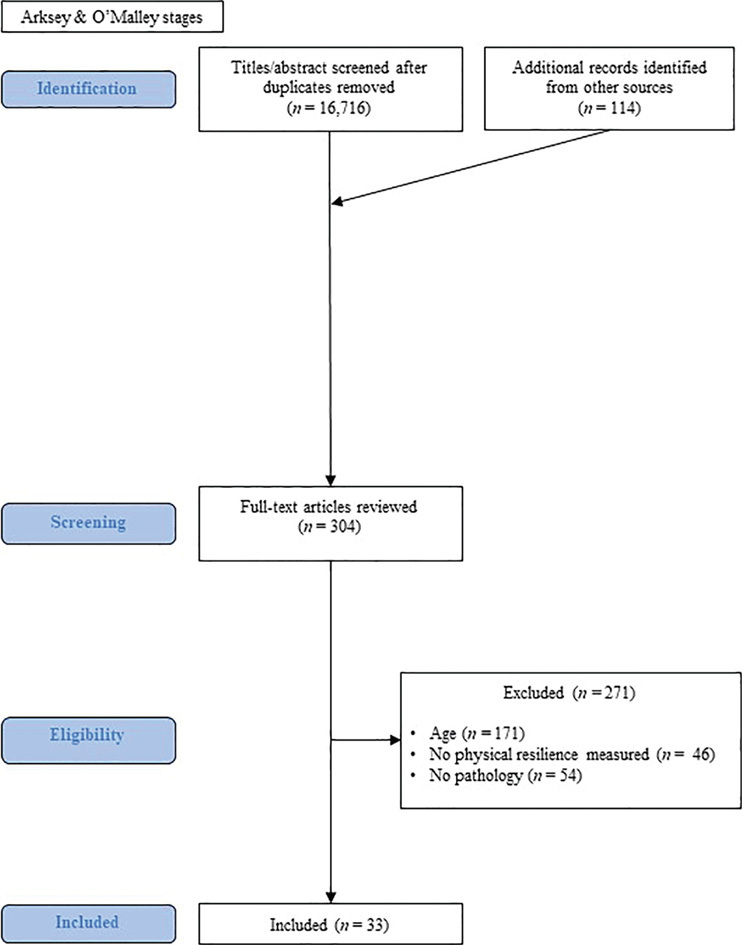
Note: Arksey and O’Malley stages are shaded, with boxes describing actions at each stage of the scoping review.
Stage 3: Study selection
After training and calibration with a small subset of titles/abstracts, all were independently screened by the principal author and one of two co-authors (SP, and GS or JL) with citations selected for full text review according to the following criteria: (1) participants recruited for the study had to have an identified pathology (e.g., frailty, hip fracture, cardiac event); (2) participants’ mean age had to be + 1 standard deviation > 65 years old so that the majority of the sample was older than 65; and (3) the term resilience had to be clearly applied to the physical health of the participants (Figure 1). Citations were excluded if they did not meet the inclusion criteria, were non-English, or were non–peer reviewed (e.g., editorials, newspaper articles, unpublished literature). Eligibility was further assessed with full-text screening by the same three independent reviewers (SP and one of GS or JL). The initial electronic search was supplemented by hand searching the reference lists from included studies to identify any missing studies. Additionally, the reference lists of resilience review articles were searched to determine whether eligible studies were missed. No additional studies met the inclusion criteria for data extraction and charting from this stage of the review (Figure 1). Online supplementary Table 1 presents the 33 research articles that met the inclusion criteria, and the measurement instruments as defined by the relevant studies. Moreover, the authors of the included research articles determined what the measurement instruments were; these were not censored to fit any additional criteria. For example, if the authors used a psychological resilience measure to gauge physical resilience, we report it as the measurement instrument in this scoping review.
Stage 4: Charting the data
The three reviewers (SP and one of GS or JL) independently extracted data from the identified articles and charted in duplicate using a pilot-tested data extraction form. Data extracted included author(s), year, country of origin, study population including sample size and pathology, study design (e.g., longitudinal), primary measurement instrument for physical resilience as defined by the authors, related outcome domain, and subdomain,27,33 as well as secondary measurement instruments. In each included paper, the primary measurement instrument for physical resilience was categorized by the authors of this manuscript using the International Classification of Functioning, Disability and Health (ICF)33 under one of the following domains: (1) body function or structure; (2) activity and participation; and (3) societal impact of the pathology.27 Body function or structure is the physiological function of body systems or anatomical parts of the body such as organs or limbs; activity and participation are the execution of an action by an individual or the involvement in a life situation; societal impact is the environment in which people live and conduct their lives.33 Subdomains, also under the ICF model, were (1) death, (2) life, (3) resource use or economic impact, and 4) pathophysiologic manifestations.27 Names of secondary measurement instruments were extracted, summarized, and categorized as potential measures for further study; however, no categorization for domain or subdomain was conducted. After extraction, data were compared between the reviewers and any discrepancies resolved by discussion and consensus.
Results
Stage 5: Collating, summarizing, and reporting the results
The results were compiled according to the protocol for this scoping review.26 The 33 articles that were included in this review had the following study designs: longitudinal (16 studies),34–47 cohort (7 studies),48–54 cross-sectional (6 studies),25,55–61 clinical trials (3 studies),62–64 and experimental in design (1 study)65 (online supplementary Table 1). Two studies were published in 1999, with the remaining 31 published between 2008 and 2020. Thirteen studies were completed in the US and 10 in Europe, with a further 4 in Australia, 3 in Canada, 1 in Singapore, 1 in Taiwan, and 1 in Brazil. Sample sizes of individual studies varied from n = 29 to n = 6,771. Clinical populations studied involved older adults with fractures (10 studies), cardiovascular conditions (4 studies), cancer (3 studies), pain (3 studies), a history of falling (2 studies), frailty (2 studies), multimorbidity (2 studies), chronic obstructive pulmonary disease (1 study), orthopedic surgery (1 study), stroke (1 study), and visual impairment (1 study) (online supplementary Table 1). Three studies involved older adults with unspecified pathologies; however, these papers met our inclusion criteria as participants were selected based on moderate levels of physical disability on the Short Performance Physical Battery (SPPB),43 or presented with a high enough level of disability requiring admission to inpatient rehabilitation35,39 (online supplementary Table 1).
Measurement instruments, by pathology
We identified 22 unique measurement instruments for physical resilience. For older adults with fractures, measurement instruments for physical resilience included psychological measures of depression,36,45 psychological resilience measures like the Connor-Davidson Resilience Scale,40,51,52 blood measures like neopterin, which is an inflammatory biomarker that may predict non-survival after hip fracture,42 and motor function measures like the Physical Resilience Scale.36,63 Additionally, scores compiled of multiple outcome measures were used.46 For older adults with cardiovascular conditions, measurement instruments included psychological resilience measures like the Connor-Davidson Resilience Scale,38,55 and combined psychosocial and physical health scores.38,41 For older adults with cancer, 2 papers employed psychological measures such as the 11-item Resilience Scale,34 and combined psychosocial (e.g., European Organization for Research and Treatment of Cancer Quality of Life Questionnaire [EORTC]) and physical measures.34,37 One paper defined physical resilience in individuals with breast cancer as a return to within 10 points of the pre-chemotherapy EORTC Questionnaire 12 months later.64 For older adults with a history of falling, cognitive48 and blood pressure49 measures were used. For individuals who were frail, the 2 identified papers used psychological measurement instruments50,62 and psychological scales.62 For older adults with multimorbidity, 2 papers developed a multimorbidity resilience index that included additive scores from motor function, psychological, and social scales.25,61
So that all content areas were included based on the protocol paper’s description for the amalgamation of results, measurement instruments of physical resilience were pooled into 4 broad categories: (1) psychological or cognitive measures, (2) physiological measures, (3) motor function scales, and (4) psychosocial scales.26 Amalgamation of results was an iterative process whereby reviewers ensured all of the content areas were included into categories. No studies pooled physiological measures with psychosocial or motor function scales, and no studies combined all of these 4 areas of measurement. Two studies combined psychosocial with motor function into a composite measure.25,61
In 2014, Boers and colleagues developed a framework of what is measurable within patient-centred research. This framework included the core areas of 1) death, 2) life impact, 3) resource use or economic impact, and 4) pathophysiology, with the ICF providing the framework for broader domains. The core areas were used to classify measurement instruments into domains and subdomains in online supplementary Table 1. Regarding the ICF outcome domains of: (1) body function or structure, (2) activity and participation, and (3) societal impact of the pathology, all measurement instruments quantified an aspect of body function or structure, with some instruments capturing activity and participation (online supplementary Table 1). One measurement instrument, a multimorbidity resilience index, examined societal impact of the pathologies together with body function or structure and activity and participation in the context of physical resilience (online supplementary Table 1). For the ICF subdomains of (1) death, (2) life, (3) resource use or economic impact, and (4) pathophysiologic manifestations, all measurement instruments examined pathophysiological features, with some also capturing aspects of life, and resource use/economic impact (online supplementary Table 1). No measurement instrument examined death.
Research gaps
We determined the priority level for research gaps and focus for future research by giving areas with the least research the highest priority for future research.27 The largest gap, and thus the highest priority, is the need for a measurement instrument that quantifies all aspects of physical resilience, namely psychosocial, physiological, motor function, and psychology. In particular, two measurement instruments (Multidimensional Health Locus of Control scale and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire) ask one or two survey questions of psychosocial aspects of physical resilience regarding a pathology’s impact on participation in social events or family life. However, these instruments were not designed to examine physical resilience, and are missing physiological and psychological measurement. Two studies did form a composite measure and combined psychosocial with motor function, but did not include physiological measurement. While one measurement instrument is explicitly endeavouring to quantify physical resilience (the Physical Resilience Scale), the scale does not include physiological measurements or the societal impact of the pathology.56,63 The second-highest priority for future research is studies that combine psychosocial or motor function measures with physiological measurements. Additional gaps include a lack of studies within Africa, and only 1 study each explicitly examining physical resilience within older adults with neurological impairment and lung conditions.
Discussion
This scoping review is the first to identify outcome domains and measurement instruments of physical resilience in older adults; these measurement instruments quantify features of physical resilience and this information is essential to mapping how physical resilience is currently measured. We identified a large gap regarding the need for a measurement instrument that captures all aspects of physical resilience – psychosocial, physiological, motor function, and psychology – including all domains and subdomains of the International Classification of Functioning, Disability and Health.33 Thus, the interaction of all aspects of resilience is not currently quantified in one comprehensive measure. Considering the heterogeneity of the studies identified by this scoping review, we are unable to recommend a meta-analysis at this point in time. The number of studies of physical resilience in older adults is low (n = 33 identified studies). Distribution of the studies lack breadth in the countries involved as well as the pathologies studied (online supplementary Table 1). Physical resilience may differ depending on the pathology, as a given pathology may impact biopsychosocial aspects of life uniquely. A comprehensive instrument that assesses all aspects of physical resilience for a given pathology (e.g., cardiovascular disease), or a cluster of diseases that often occur together (e.g., cardiovascular disease, diabetes, stroke), could identify which factors and interactions among outcome domains can be targeted to foster or maximize resilience. In particular, potential interactions between physiological and motor function parameters would be identified if such a measure could be generated.
Some current measurement instruments miss aspects of physical resilience (online supplementary Table 1)
Investigating the negative response to a stressor, for example, the way that depression rating scales do, may not be a comprehensive method of measuring physical resilience. Resilience measures like the Connor-Davidson Resilience Scale were designed to capture psychological aspects of resilience at a broad level. Self-reported measures, like the Global Rating of Change scale, provide a method to obtain information on patients’ self-perception of whether their condition is improving or deteriorating over time.66 A drawback of self-reported measurement instruments is that they rely on an individual’s recall or memory, which can lead to over- or underestimation of change. While physical resilience may involve psychological elements (or perceptions of overall resilience), current physical resilience measurement instruments do not quantify the social and biological aspects inherent in physical resilience. Blood samples and physiological measures may seem like obvious techniques to measure resilience as they are physical in nature; however, when used, these measures miss potential interactions of the biological with the social and psychological.67,68
Some quality-of-life measures capture physical function, psychological health, and the impact of the pathology on social interactions. Again, what is overlooked is direct physiological measurement and sociological aspects such as culture and socioeconomic status. Moreover, quality-of-life measurement instruments may focus on negative aspects of a pathology’s impact on life, as opposed to measuring the positive adaptive aspects of resilience. Considering that a defining feature of resilience is the adaption or maintenance of physical function after a stressor, these types of measurement instruments may miss important dimensions and processes of physical resilience.
A further consideration is to determine whether the measurement instruments identified by this review are evaluating the whole construct of physical resilience or just a part of it. If the construct of physical resilience can be understood in its entirety, interventions can be developed and evaluated in order to identify those that foster physical resilience in the rehabilitation of pathologies affecting older adults.
Social impacts of physical resilience
No measurement instrument thoroughly examines the social impact of physical resilience, beyond a cursory level. Social and psychological circumstances can impact morbidity and mortality through physiological processes and behaviour through several potential pathways, one being the mediating role of physiology; another potential pathway is through a moderating role of physiological resilience, which can foster social and psychological resilience, or through reciprocal or bidirectional associations.68 If an illness or disease affects the ability of older adults to move about their environment, the pathology likely affects all aspects of life, such as social networks, social support, and health-enhancing behaviours. Furthermore, the physical resilience of older adults with low or high socioeconomic status may differ in important and unidentified ways, outside of known benefits of lower disease rates for socioeconomically advantaged people.67 Beyond the individual, the lack of measurement of sociological aspects of physical resilience, including economic impacts like medical/resource use, reduces our understanding of the manifestation of and techniques that may foster physical resilience. Performing research in countries that lack resilience studies may give insight into how physical resilience could be fostered given differing cultural, sociological, demographic, and life-course events, where an alteration in any of these factors may foster physical resilience differently than in the US or Europe. Thus, for a complete understanding of physical resilience, the measurement of social (individual level), societal (beyond individual level), and global impacts is required.
An inherent limitation of scoping reviews is that they provide breadth and not depth on a topic.28,31 As physical resilience is a concept with emerging evidence, a scoping review is the best approach to ensure the broadest possible data are extracted and analyzed. The current review provides a broad view of the measurement of physical resilience in older adults, but is unable to describe the effectiveness of these measurement instruments on specific outcomes. However, providing a breadth of knowledge via a scoping review may be useful to people across many health disciplines, such as rehabilitation health professionals, researchers, policy-makers, and administrators, and may contribute to therapeutic decision making, prehabilitation strategies, and quicker detection of complications.69 While this scoping review aimed to identify measurement instruments, it did not address the validity or timing for use of these measurement instruments.16 Another potential limitation is that most of the current research was completed in the US or Europe, so conclusions drawn are likely more reflective of individuals in the developed world versus developing nations. Along these lines, the included papers were limited to studies published in English. A future review including all languages may identify other useful measurement instruments.
Conclusion
Understanding how potential biopsychosocial factors contribute to pathology and recovery may outline ways that physical resiliency could be fostered in the rehabilitation process. Fostering physical resilience may improve prehabilitation and/or preventative strategies to promote recovery, could improve acute to chronic care management, compress morbidity, and ultimately improve quality of life during the ageing process.
Key Messages
What is already known on this topic
Resilience is the capacity to recover or resist the adverse effects of a stressor and is a multifaceted concept that entails psychological features, social relationships, environment, genetics, and biology.
What this study adds
We identified 22 unique measurement instruments for physical resilience. No single measurement instrument quantifies all aspects of physical resilience. Greater knowledge of physical resilience may help identify protective factors and approaches that promote healthy ageing.
Supplementary Material
References
- 1.Fontana L, Kennedy BK, Longo VD, et al. Medical research: treat ageing. Nature. 2014;511(7510):405–7. 10.1038/511405a. Medline:25056047 [DOI] [PubMed] [Google Scholar]
- 2.Silverman AM, Molton IR, Alschuler KN, et al. Resilience predicts functional outcomes in people aging with disability: a longitudinal investigation. Arch Phys Med Rehabil. 2015;96(7):1262–8. 10.1016/j.apmr.2015.02.023. Medline:25757790 [DOI] [PubMed] [Google Scholar]
- 3.Ezeamama AE, Elkins J, Simpson C, et al. Indicators of resilience and healthcare outcomes: findings from the 2010 health and retirement survey. Qual Life Res. 2016;25(4):1007–15. 10.1007/s11136-015-1144-y. Medline:26475139 [DOI] [PubMed] [Google Scholar]
- 4.Rybarczyk B, Emery E, Guequierre L, et al. The role of resilience in chronic illness and disability in older adults. In: Hayslip B, Smith G, editors. Annual review of gerontology and geriatrics. New York: Springer; 2012. p. 173–88. [Google Scholar]
- 5.Hadley EC, Kuchel GA, Newman AB. Report: NIA workshop on measures of physiologic resiliencies in human aging. J Gerontol A Biol Sci Med Sci. 2017;72(7):980–90. 10.1093/gerona/glx015. Medline:28475732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whitson HE, Duan-Porter W, Schmader KE, et al. Physical resilience in older adults: systematic review and development of an emerging construct. J Gerontol A Biol Sci Med Sci. 2016;71(4):489–95. 10.1093/gerona/glv202. Medline:26718984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagnild G, Young HM. Resilience among older women. Image J Nurs Sch. 1990;22(4):252–5. 10.1111/j.1547-5069.1990.tb00224.x. Medline:2292448 [DOI] [PubMed] [Google Scholar]
- 8.Russo SJ, Murrough JW, Han MH, et al. Neurobiology of resilience. Nat Neurosci. 2012;15(11):1475–84. 10.1038/nn.3234. Medline:23064380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rutter M. Annual research review: resilience – clinical implications. J Child Psychol Psychiatry. 2013;54(4):474–87. 10.1111/j.1469-7610.2012.02615.x. Medline:23017036 [DOI] [PubMed] [Google Scholar]
- 10.Jeste DV, Savla GN, Thompson WK, et al. Association between older age and more successful aging: critical role of resilience and depression. Am J Psychiatry. 2013;170(2):188–96. 10.1176/appi.ajp.2012.12030386. Medline:23223917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cosco TD, Prina AM, Perales J, et al. Lay perspectives of successful ageing: a systematic review and meta-ethnography. BMJ Open. 2013;3(6):e002710. 10.1136/bmjopen-2013-002710. Medline:23794575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byun J, Jung D.. The influence of daily stress and resilience on successful ageing. Int Nurs Rev. 2016;63(3):482–9. 10.1111/inr.12297. Medline:27305866 [DOI] [PubMed] [Google Scholar]
- 13.Iwashyna TJ. Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Respir Crit Care Med. 2012;186(4):302–4. 10.1164/rccm.201206-1138ed. Medline:22896591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harcombe H, Langley J, Davie G, et al. Functional status following injury: what recovery pathways do people follow? Injury. 2015;46(7):1275–80. 10.1016/j.injury.2015.04.004. Medline:25920372 [DOI] [PubMed] [Google Scholar]
- 15.Langley J, Davie G, Wilson S, et al. Difficulties in functioning 1 year after injury: the role of preinjury sociodemographic and health characteristics, health care and injury-related factors. Arch Phys Med Rehabil. 2013;94(7):1277–86. 10.1016/j.apmr.2013.02.012. Medline:23439409 [DOI] [PubMed] [Google Scholar]
- 16.Varadhan R, Walston JD, Bandeen-Roche K. Can a link be found between physical resilience and frailty in older adults by studying dynamical systems? J Am Geriatr Soc. 2018;66(8):1455–8. 10.1111/jgs.15409. Medline:29727469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Resnick B, Galik E, Dorsey S, et al. Reliability and validity testing of the physical resilience measure. Gerontologist. 2011;51(5):643–52. 10.1093/geront/gnr016. Medline:21402647 [DOI] [PubMed] [Google Scholar]
- 18.Kim MJ, Yabushita N, Tanaka K. Exploring effective items of physical function in slow walking speed and self-reported mobility limitation in community-dwelling older adults. Geriatr Gerontol Int. 2012;12(1):50–8. 10.1111/j.1447-0594.2011.00726.x. Medline:21729226 [DOI] [PubMed] [Google Scholar]
- 19.Asiri FY, Marchetti GF, Ellis JL, et al. Predictors of functional and gait outcomes for persons poststroke undergoing home-based rehabilitation. J Stroke Cerebrovasc Dis. 2014;23(7):1856–64. 10.1016/j.jstrokecerebrovasdis.2014.02.025. Medline:24809670 [DOI] [PubMed] [Google Scholar]
- 20.Hunter SK, Pereira HM, Keenan KG. The aging neuromuscular system and motor performance. J Appl Physiol (1985). 2016;121(4):982–95. 10.1152/japplphysiol.00475.2016. Medline:27516536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson RS, Segawa E, Buchman AS, et al. Terminal decline in motor function. Psychol Aging. 2012;27(4):998–1007. 10.1037/a0028182. Medline:22612603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wister AV, Coatta KL, Schuurman N, et al. A lifecourse model of multimorbidity resilience: theoretical and research developments. Int J Aging Hum Dev. 2016;82(4):290–313. 10.1177/0091415016641686. Medline:27076489 [DOI] [PubMed] [Google Scholar]
- 23.Connelly E, Allen C, Hatfield K, et al. Features of resilience. Environ Syst Decis. 2017;37(1):46–50. 10.1007/s10669-017-9634-9. [DOI] [Google Scholar]
- 24.Cosco TD, Kaushal A, Hardy R, et al. Operationalising resilience in longitudinal studies: a systematic review of methodological approaches. J Epidemiol Community Health. 2017;71(1):98–104. 10.1136/jech-2015-206980. Medline:27502781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wister A, Lear S, Schuurman N, et al. Development and validation of a multi-domain multimorbidity resilience index for an older population: results from the baseline Canadian Longitudinal Study on Aging. BMC Geriatr. 2018;18(1):170. 10.1186/s12877-018-0851-y. Medline:30053838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peters S, Cosco TD, Mackey DC, et al. Measurement instruments for quantifying physical resilience in aging: a scoping review protocol. Syst Rev. 2019;8(1):34. 10.1186/s13643-019-0950-7. Medline:30691527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boers M, Kirwan JR, Wells G, et al. Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. J Clin Epidemiol. 2014;67(7):745–53. 10.1016/j.jclinepi.2013.11.013. Medline:24582946 [DOI] [PubMed] [Google Scholar]
- 28.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Intl J Social Res Method. 2005;8(1):19–32. 10.1080/1364557032000119616. Medline:31705429 [DOI] [Google Scholar]
- 29.Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6. 10.1097/xeb.0000000000000050. Medline:26134548 [DOI] [PubMed] [Google Scholar]
- 30.Tricco AC, Lillie E, Zarin W, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15. 10.1186/s12874-016-0116-4. Medline:26857112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. 10.1186/1748-5908-5-69. Medline:20854677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cosco TD, Kaushal A, Richards M, et al. Resilience measurement in later life: a systematic review and psychometric analysis. Health Qual Life Outcomes. 2016;14(1):16. 10.1186/s12955-016-0418-6. Medline:26821587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.International classification of functioning . Disabil Health J (icf). 2001.
- 34.Baier P, Ihorst G, Wolff-Vorbeck G, et al. Independence and health related quality of life in 200 onco-geriatric surgical patients within 6 months of follow-up: who is at risk to lose? Eur J Surg Oncol. 2016;42(12):1890–7. 10.1016/j.ejso.2016.07.013. Medline:27519617 [DOI] [PubMed] [Google Scholar]
- 35.Barma M, Goodbrand JA, Donnan PT, et al. Slower decline in C-reactive protein after an inflammatory insult is associated with longer survival in older hospitalised patients. PLoS One. 2016;11(7):e0159412. 10.1371/journal.pone.0159412. Medline:27467771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cristancho P, Lenze EJ, Avidan MS, et al. Trajectories of depressive symptoms after hip fracture. Psychol Med. 2016;46(7):1413–25. 10.1017/s0033291715002974. Medline:27032698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duan-Porter W, Cohen HJ, Demark-Wahnefried W, et al. Physical resilience of older cancer survivors: an emerging concept. J Geriatr Oncol. 2016;7(6):471–8. 10.1016/j.jgo.2016.07.009. Medline:27478133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Edward KL, Stephenson J, Giandinoto JA, et al. An Australian longitudinal pilot study examining health determinants of cardiac outcomes 12 months post percutaneous coronary intervention. BMC Cardiovasc Disord. 2016;16(1):31. 10.1186/s12872-016-0203-9. Medline:26841927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goodbrand JA, Hughes LD, Cochrane L, et al. Association between bisphosphonate therapy and outcomes from rehabilitation in older people. Arch Gerontol Geriatr. 2017;70:195–200. 10.1016/j.archger.2017.01.017. Medline:28214400 [DOI] [PubMed] [Google Scholar]
- 40.Kohler S, Loh SM.. Patient resilience in the fracture orthopaedic rehabilitation geriatric environment. Australas J Ageing. 2017;36(1):65–8. 10.1111/ajag.12362. Medline:27868331 [DOI] [PubMed] [Google Scholar]
- 41.Kotajarvi BR, Schafer MJ, Atkinson EJ, et al. The impact of frailty on patient-centered outcomes following aortic valve replacement. J Gerontol A Biol Sci Med Sci. 2017;72(7):917–21. 10.1093/gerona/glx038. Medline:28329140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Larsen M, Bayard C, Lepetitcorps H, et al. Elevated neopterin levels predict early death in older hip-fracture patients. EBioMedicine. 2017;26:157–64. 10.1016/j.ebiom.2017.11.003. Medline:29157836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehta M, Whyte E, Lenze E, et al. Depressive symptoms in late life: associations with apathy, resilience and disability vary between young-old and old-old. Int J Geriatr Psychiatry. 2008;23(3):238–43. 10.1002/gps.1868. Medline:17676651 [DOI] [PubMed] [Google Scholar]
- 44.Wahl HW, Schilling O, Oswald F, et al. Psychosocial consequences of age-related visual impairment: comparison with mobility-impaired older adults and long-term outcome. J Gerontol B Psychol Sci Soc Sci. 1999;54(5):P304–16. 10.1093/geronb/54b.5.p304. Medline:10542823 [DOI] [PubMed] [Google Scholar]
- 45.Zimmerman SI, Smith HD, Gruber-Baldini A, et al. Short-term persistent depression following hip fracture: a risk factor and target to increase resilience in elderly people. Soc Work Res. 1999;23(3):187–96. 10.1093/swr/23.3.187. [DOI] [Google Scholar]
- 46.Colon-Emeric C, Whitson HE, Pieper CF, et al. Resiliency groups following hip fracture in older adults. J Am Geriatr Soc. 2019;67(12):2519–27. 10.1111/jgs.16152. Medline:31469411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lim KK, Matchar DB, Tan CS, et al. The association between psychological resilience and physical function among older adults with hip fracture surgery. J Am Med Dir Assoc. 2019;21(2):260–6. 10.1016/j.jamda.2019.07.005. Medline:31522877 [DOI] [PubMed] [Google Scholar]
- 48.Best JR, Davis JC, Liu-Ambrose T.. Longitudinal analysis of physical performance, functional status, physical activity, and mood in relation to executive function in older adults who fall. J Am Geriatr Soc. 2015;63(6):1112–20. 10.1111/jgs.13444. Medline:26096385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lagro J, Schoon Y, Heerts I, et al. Impaired systolic blood pressure recovery directly after standing predicts mortality in older falls clinic patients. J Gerontol A Biol Sci Med Sci. 2014;69(4):471–8. 10.1093/gerona/glt111. Medline:23873962 [DOI] [PubMed] [Google Scholar]
- 50.Rebagliati GA, Sciume L, Iannello P, et al. Frailty and resilience in an older population: the role of resilience during rehabilitation after orthopedic surgery in geriatric patients with multiple comorbidities. Funct Neurol. 2016;31:171–7. 10.11138/fneur/2016.31.3.171. Medline:27678211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Resnick B, Galik E, Boltz M, et al. Physical activity in the post-hip-fracture period. J Aging Phys Act. 2011;19(4):373–87. 10.1123/japa.19.4.373. Medline:21911877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Resnick B, Hebel JR, Gruber-Baldini AL, et al. The impact of body composition, pain and resilience on physical activity, physical function and physical performance at 2 months post hip fracture. Arch Gerontol Geriatr. 2018;76:34–40. 10.1016/j.archger.2018.01.010. Medline:29455057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Resnick B, Klinedinst NJ, Yerges-Armstrong L, et al. Genotype, resilience and function and physical activity post hip fracture. Int J Orthop Trauma Nurs. 2019;34:36–42. 10.1016/j.ijotn.2019.03.005. Medline:31257007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sciume L, Rebagliati GAA, Iannello P, et al. Rehabilitation after urgent or elective orthopedic surgery: the role of resilience in elderly patients. Rehabil Nurs. 2018;43(5):267–74. 10.1097/rnj.0000000000000038. Medline:30168809 [DOI] [PubMed] [Google Scholar]
- 55.Hagglund L, Boman K, Stenlund H, et al. Factors related to fatigue among older patients with heart failure in primary health care. Int J Older People Nurs. 2008;3(2):96–103. 10.1111/j.1748-3743.2007.00091.x. Medline:20925898 [DOI] [PubMed] [Google Scholar]
- 56.Resnick B, Galik E, Wells CL, et al. The impact of pain management with opioids among older adults post orthopedic trauma. Pain Manag Nurs. 2016;17(5):302–10. 10.1016/j.pmn.2016.05.005. Medline:27567095 [DOI] [PubMed] [Google Scholar]
- 57.Cannon DL, Sriram KB, Liew AW, et al. Resilience factors important in health-related quality of life of subjects with COPD. Respir Care. 2018;63(10):1281–92. 10.4187/respcare.05935. Medline:30065078 [DOI] [PubMed] [Google Scholar]
- 58.Lee SY, Tung HH, Peng LN, et al. Resilience among older cardiovascular disease patients with probable sarcopenia. Arch Gerontol Geriatr. 2020;86:103939. 10.1016/j.archger.2019.103939. Medline:31525556 [DOI] [PubMed] [Google Scholar]
- 59.Morete MC, Solano JPC, Boff MS, et al. Resilience, depression, and quality of life in elderly individuals with chronic pain followed up in an outpatient clinic in the city of São Paulo, Brazil. J Pain Res. 2018;11:2561–6. 10.2147/jpr.s166625. Medline:30464576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Musich S, Wang SS, Slindee L, et al. The association of pain locus of control with pain outcomes among older adults. Geriatr Nurs. 2019;41(5):521–9. 10.1016/j.gerinurse.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 61.Wister A, Cosco T, Mitchell B, et al. Health behaviors and multimorbidity resilience among older adults using the Canadian Longitudinal Study on Aging. Int Psychogeriatr. 2019;32(1):1–15. 10.1017/s1041610219000486. Medline:31088579 [DOI] [PubMed] [Google Scholar]
- 62.Milte CM, Luszcz MA, Ratcliffe J, et al. Influence of health locus of control on recovery of function in recently hospitalized frail older adults. Geriatr Gerontol Int. 2015;15(3):341–9. 10.1111/ggi.12281. Medline:24674154 [DOI] [PubMed] [Google Scholar]
- 63.Resnick B, Wells C, Galik E, et al. Feasibility and efficacy of function-focused care for orthopedic trauma patients. J Trauma Nurs. 2016;23(3):144–55. 10.1097/jtn.0000000000000203. Medline:27163222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hurria A, Soto-Perez-de-Celis E, Allred JB, et al. Functional decline and resilience in older women receiving adjuvant chemotherapy for breast cancer. J Am Geriatr Soc. 2019;67:920–7. 10.1111/jgs.15493. Medline:30146695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sadler E, Sarre S, Tinker A, et al. Developing a novel peer support intervention to promote resilience after stroke. Health Soc Care Community. 2017;25(5):1590–1600. 10.1111/hsc.12336. Medline:26939997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009;17(3):163–70. 10.1179/jmt.2009.17.3.163. Medline:20046623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4):1973–98. 10.1161/01.cir.88.4.1973. Medline:8403348 [DOI] [PubMed] [Google Scholar]
- 68.Institute of Medicine Committee on H, Behavior: Research P, Policy . The national academies collection: reports funded by national institutes of health. In: Health and behavior: the interplay of biological, behavioral, and societal influences. Washington (DC): National Academies Press; (US): National Academy of Sciences; 2001. [PubMed] [Google Scholar]
- 69.McArthur C, Gibbs JC, Patel R, et al. A scoping review of physical rehabilitation in long-term care: interventions, outcomes, tools. Can J Aging. 2017;36(4):435–52. 10.1017/s071498081700040x. Medline:29130428 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


