INTRODUCTION
The number of people receiving facial filler injections for aesthetic purpose has been increasing in recent years. Simultaneously, the number of patients dissolving fillers due to unsatisfactory outcomes or adverse effects, such as granuloma and allergy, is also increasing. Hyaluronidase has various uses, including dissolving hyaluronic acid fillers and treating granulomatous foreign body reactions and necrosis associated with filler injections.1 Here, I will discuss why ultrasonography should be performed before a filler dissolving injection and why the filler should be dissolved while viewing ultrasonographic images.2 Hyaluronidase is an endoglycosidase that breaks down hyaluronic acid into monosaccharides by cleaving its glycosidic bonds.3,4
Safe performance of this method requires sufficient understanding of the anatomy of the face, because of the heavy distribution of vital blood vessels, nerves, retaining ligaments, and muscles.5
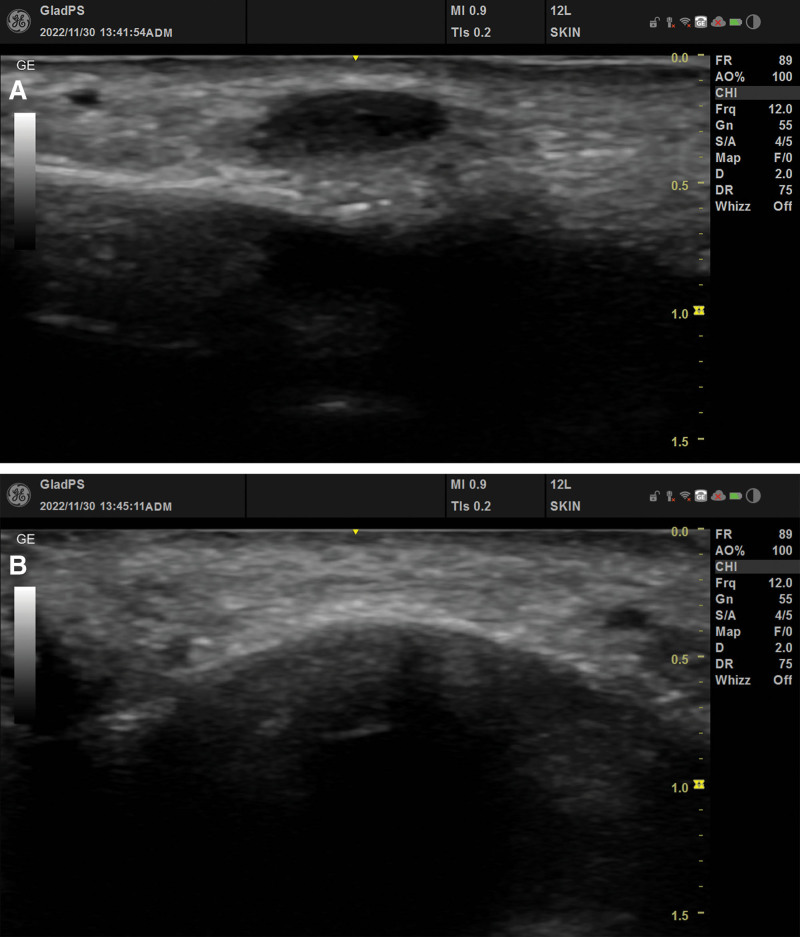
The author performed filler removal using ultrasonography on more than 500 patients. First, palpation was performed, and after confirming the exact location and depth with ultrasound, it was marked with a pen. The filler was removed by injection of hyaluronidase. Some people had swelling and heat due to allergy to hyaluronidase, but they improved within 2–3 days and did not experience any other side effects (Fig. 1). This ultrasonography-guided hyaluronidase injection technique offers several advantages, as follows:
Fig 1.
Pre- and post-procedure ultrasonic images. A, Filler in the anterior cheek shown before hyaluronidase injection. B, Anterior cheek after the filler has been completely dissolved.
Ultrasonography is rapid and simple, with no risk of radiation exposure.
This technique involves no additional discomfort for patients and can be more comfortable.
This method does not require injection into a wide area around the injected filler, indicating that a smaller amount of hyaluronidase can be used.
Vital blood vessels and nerves can be avoided using ultrasonographic images.
When catastrophic adverse effects (such as blindness or necrosis) occur, exacerbation of such adverse effects can be quickly and accurately prevented.
This method can effectively dissolve the filler, as the target is accurately set beforehand.
In cases wherein undissolved fillers are still present despite several dissolution procedures, ultrasonography-guided hyaluronidase injection before removing the filler by incision is a feasible approach for both the patient and the physician. A limitation is that it is very difficult to completely remove granuloma or filler if it remains in a very small size, or if the filler is broken into very small sizes by melting it. In addition, there are cases in which the filler cannot be confirmed by ultrasound. The use of more precise ultrasound is necessary.
This study is a conceptual thought and represents the author’s opinion based on experience, and a more scientific study with 500 patients will be conducted in the future.
DISCLOSURE
The author has no financial interest to declare in relation to the content of this article.
Footnotes
Published online 13 June 2023.
REFERENCES
- 1.Jung HH. An overview of its properties, applications, and side effects. Arch Plast Surg. 2020;47:297–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim MS, Youn S, Na CH, et al. Allergic reaction to hyaluronidase use after hyaluronic acid filler injection. J Cosmet Laser Ther. 2015;17:283–285. [DOI] [PubMed] [Google Scholar]
- 3.DeLorenzi C. New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J. 2017;37:814–825. [DOI] [PubMed] [Google Scholar]
- 4.Bailey SH, Fagien S, Rohrich RJ. Changing role of hyaluronidase in plastic surgery. Plast Reconstr Surg. 2014;133:127e127–127132e. [DOI] [PubMed] [Google Scholar]
- 5.DeLorenzi C. Transarterial degradation of hyaluronic acid filler by hyaluronidase. Dermatol Surg. 2014;40:832–841. [DOI] [PubMed] [Google Scholar]