Abstract
Background
National Institutes of Health (NIH) funding is a key driver of orthopaedic research, but it has become increasingly difficult to obtain in recent years. An understanding of the types of grants that are commonly funded, how productive they are, and the factors associated with obtaining funding may help orthopaedic surgeons better understand how to earn grants.
Questions/purposes
In this study, we sought to determine (1) the proportion of current academic orthopaedic surgeons who have obtained NIH grant funding, (2) the productivity of these grants by calculating grant productivity metrics, and (3) the factors (such as gender, subspecialty, and additional degrees) that are associated with obtaining grant funding.
Methods
Current academic orthopaedic surgeons at the top 140 NIH-funded institutions were identified via faculty webpages; 3829 surgeons were identified. Demographic information including gender (men constituted 88% of the group [3364 of 3829]), academic rank (full professors constituted 22% [856 of 3829]), additional degrees (those with MD-PhD degrees constituted 3% [121 of 3829]), leadership positions, and orthopaedic subspecialty was collected. Funding histories from 1985 through 2021 were collected using the NIH Research Portfolio Online Reporting Tools Expenditures and Results. Grant type, funding, publications, and citations of each article were collected. A previously used grant impact metric (total citations per USD 0.1 million) was calculated to assess grant productivity. Multivariable binomial logistic regression was used to evaluate factors associated with obtaining funding.
Results
Four percent (150 of 3829) of academic orthopaedic surgeons obtained USD 338.3 million in funding across 301 grants, resulting in 2887 publications over the entire study period. The R01 was the most commonly awarded grant in terms of the total number awarded, at 36% (108 of 301), as well as by funding, publications, and citations, although other grant types including T32, F32, R03, R13, and R21 had higher mean grant impact metrics. There was no difference between men and women in the by-gender percentage of academic orthopaedic surgeons who obtained funding (4% [135 of 3229] versus 3% [15 of 450]; odds ratio 0.9 [95% confidence interval 0.5 to 1.7]; p = 0.80). A department having a single funded PhD researcher may be associated with surgeon-scientists obtaining grant funding, but with the numbers available, we could not demonstrate this was the case (OR 1.4 [95% CI 0.9 to 2.2]; p = 0.12).
Conclusion
Fewer than one in 20 academic orthopaedic surgeons have received NIH funding. R01s are the most commonly awarded grant, although others demonstrate increased productivity metrics. Future studies should investigate the role of co–principal investigators on productivity and the role of different funding sources.
Clinical Relevance
Individuals should pursue both R01 and non-R01 grants, and departments should consider cultivating relationships with funded PhDs. The specific research infrastructure and departmental policies of the most productive institutions and grants should be surveyed and emulated.
Introduction
National Institutes of Health (NIH) funding helps drive the advancement of all fields of biomedical research in the United States. In orthopaedic surgery, major advances in our understanding of the natural history and treatment of osteoarthritis, strategies for ligamentous repair, pain management techniques, implant design, and countless other fields would not have been possible without the basic, translational, and clinical research that NIH funding has supported [7-9, 20, 21]. However, obtaining NIH funding has become increasingly difficult for physician-scientists, particularly surgeon-scientists, who must balance busy operative schedules with performing research [12, 26]. There has been an increase in the number of NIH grant applications with a decline in the number of funded grants, career development awards, and funding to surgeon-scientists [14, 26, 36].
Evaluating the state of NIH funding to orthopaedic surgeons would indicate how much funding is available as well as individual and departmental characteristics that are associated with successfully obtaining funding. Furthermore, it would outline the areas that are commonly funded and the specific grant mechanisms that are most available. It would also demonstrate which grant mechanisms are the most productive. This information may help surgeons and their departments better understand how to obtain grants and the specific grant types and areas to pursue. It may also specifically demonstrate to the NIH the continued need for grant funding to orthopaedic surgery and the types of grants and areas of research to fund. This is particularly relevant given the anticipated growth of the field [19, 35]. Despite this, the evidence is fairly limited regarding NIH funding in orthopaedic surgery. Prior studies have commented on K-awardees in orthopaedic surgery and funding among hand surgeons [32-34], but the last NIH funding analysis for the field was performed with data from 2005 to 2014, notably with scientists comprising most of the study population instead of surgeons-scientists.
We therefore sought to determine (1) the proportion of current academic orthopaedic surgeons who have obtained NIH grant funding, (2) the productivity of these grants by calculating grant productivity metrics, and (3) the factors (such as gender, subspecialty, and additional degrees) that are associated with obtaining grant funding.
Materials and Methods
Study Design and Setting
This study was a retrospective query of the NIH funding histories of orthopaedic surgeons employed at the 140 highest NIH-funded academic institutions in 2020 [2]. Current attending orthopaedic surgeons as of July 1, 2021 were identified via faculty webpages. Their funding histories were then queried using the NIH’s Research Portfolio Online Reporting Tools Expenditures and Results (NIH RePORTER) [27], an online database of prior grants and their resulting publications. We used faculty webpages for surgeon listings because they are the most complete publicly available listings of orthopaedic surgeons and their demographics. NIH RePORTER was used for collecting grant data because it is maintained by the NIH and is comprehensive, accurate, and searchable.
Surgeon Demographics
We identified 3829 orthopaedic surgeons (Table 1). Orthopaedic surgeons who were men comprised 88% (3364 of 3829) of the study population. Current academic ranks included 42% (1621 of 3829) assistant professors, 22% (856 of 3829) associate professors, and 22% (856 of 3829) full professors. Three percent (121 of 3829) had a PhD degree, while 3% (115 of 3829) had an MS degree. The only physicians included in this study were those who completed a residency in orthopaedic surgery, except for plastic surgeons who completed additional fellowship training in hand and upper extremity surgery.
Table 1.
Demographics of the study population
| Characteristic | NIH-funded (n = 150) | No NIH funding (n = 3679) |
| Gender, men | 90 (135) | 88 (3229) |
| Graduate degree (non-MD) | 34 | 202 |
| PhD | 61 (25) | 27 (96) |
| MS | 22 (9) | 30 (106) |
| Division | 150 | 3679 |
| Adult reconstruction | 15 (23) | 14 (510) |
| Foot and ankle | 3 (4) | 7 (245) |
| Hand and upper extremity | 13 (20) | 13 (490) |
| Orthopaedic oncology | 12 (18) | 3 (118) |
| Pediatric orthopaedics | 11 (16) | 12 (433) |
| Spine | 10 (15) | 12 (427) |
| Sports medicine | 17 (25) | 21 (781) |
| Trauma | 8 (12) | 10 (379) |
| General orthopaedics | 5 (8) | 4 (130) |
| Multiple | 6 (9) | 5 (166) |
| Professorship | 150 | 3679 |
| Assistant | 11 (17) | 44 (1604) |
| Associate | 19 (29) | 23 (827) |
| Full | 63 (95) | 21 (761) |
| Emeritus | 3 (5) | 1 (32) |
| Unknown | 3 (4) | 12 (455) |
| Leadership | 60 | 836 |
| Chair or Vice Chair | 37 (22) | 19 (157) |
| Division chief | 50 (30) | 53 (442) |
| PD or APD | 13 (8) | 28 (237) |
Data presented as % (n). Chair or Vice Chair represents department of orthopaedic surgery lead, whereas division chief represents subspecialty lead. PhD = Doctor of Philosophy; MS = Master of Science; PD = residency program director; APD = associate residency program director.
Grant Data Collection
Grant history for each orthopaedic surgeon was collected, including grants awarded from January 1, 1985, to July 1, 2021. We used a Python script to assemble the following for each grant from NIH RePORTER: grant number and type, grant title, principal investigator, institution of work, grant start and end dates, total grant funding, NIH institution, NIH study section, number of publications, and PubMed Central reference number of each publication. Grants were categorized as F32 or similar (F30, F31, F32), K-award (K02, K08, K11, K23, K24, K76), R01, R03, R13, R21, other R award (R00, R25, R29, R34, R44, R56, or ), T32, and other grants (DP1, P30, P50, S10, S15, U13, U54, UG1, UH3, or UM1). The total number of grants, funding, publications, citations, total grant impact metric (explained below), and mean grant impact metric were then calculated for each grant category. The renewal status of any R01 grant eligible for renewal was recorded, as was the number of K-Award (Mentored Research Career Development Awards) to R01 (Research Project Awards) transitions, defined as a surgeon receiving both a K-Award and R01 grant in their career.
All grant data were attributed solely to the listed orthopaedic surgeon and no coinvestigators. M01 (22 grants) and UL1 (1 grant) funding was excluded because these are large, multidisciplinary grants typically awarded to multiple principal investigators. When analyzing grants by productivity metrics, we excluded 18% (55 of 301) because of absent funding data.
Calculation of Grant Impact Metric
Using the PubMed Central reference numbers of each grant, we used the NIH database iCite to assemble total citations of each paper [15]. The grant impact metric was then calculated as follows:
This previously used metric is therefore an evaluation of citation-based productivity [5, 25].
Primary and Secondary Study Outcomes
Our primary study goal was to determine the number of orthopaedic surgeons who receive NIH funding. To achieve this, we queried the funding histories of each orthopaedic surgeon using NIH RePORTER.
Our secondary study goals were to calculate grant productivity metrics for NIH-funded orthopaedic surgeons and determine which factors were associated with an increased likelihood of obtaining NIH funding. Grant productivity metrics included the number of articles, grant impact metric, R01 renewal proportion, and K to R01 transition proportion. To evaluate which factors were associated with obtaining NIH funding, we performed binomial logistic regression using surgeon demographics including gender, current academic rank, graduate degree other than MD or equivalent, subspecialty, leadership position, and whether a funded PhD was associated with a department.
Ethical Approval
Ethical approval was not sought for the present study because only publicly available databases were queried and analyzed.
Statistical Analysis
Descriptive statistics were used to address the primarily exploratory first and second research purposes, which evaluate the proportion of orthopaedic surgeons who have obtained NIH funding and grant productivity metrics, respectively. To address the third research purpose evaluating the factors associated with obtaining grant funding, an exploratory, univariable analysis was first performed to assess the association of the following factors with funding proportion: gender, orthopaedic subspecialty, leadership position, professorship rank, additional degree, institutional NIH funding rank, and whether a department had a funded PhD investigator. Factors were then advanced to a multivariable binomial logistic regression analysis if p was < 0.10. All factors met the advancement criteria, except for gender. However, gender was advanced given the expected considerable overlap between this factor and others including professorship rank and leadership position. The resulting multivariable model had an area under the receiver operating characteristic curve of 0.85.
All statistical analyses were performed using SPSS Statistics, version 28.0.1.0 (IBM Corp). Alpha was set at 0.05 to evaluate statistical significance in the multivariable analysis.
Results
Percentage of Orthopaedic Surgeons Who Obtained NIH Grants
Four percent (150 of 3829) of academic orthopaedic surgeons obtained USD 338.3 million in funding across 301 grants between 1985 and 2021. The largest grant type both in terms of number awarded and funding was the R01 (36% of grants [108 of 301] with 63% of funding [USD 213.5 million of USD 338.3 million]). Most funding awarded over the study period was from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (66% of funding [USD 223.4 million of USD 338.3 million]) (Fig. 1).
Fig. 1.
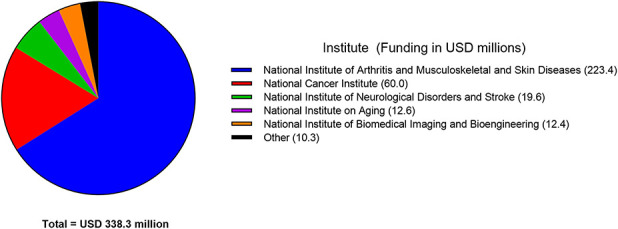
This pie chart shows the total grant awards in millions by NIH Institute. The National Institute of Arthritis and Musculoskeletal and Skin Diseases provided the most grant funding (USD 223.4 million; 66% of total funding). Other funding institutes included the National Eye Institute; the National Center for Research Resources; the Agency for Healthcare Research and Quality; the National Institute of Diabetes and Digestive and Kidney Diseases; the National Library of Medicine; the National Institute of Dental and Craniofacial Research; the National Institute of Arthritis, Diabetes, Digestive, and Kidney Diseases; the National Institute of Environmental Health Sciences; Office of the Director, National Institutes of Health; the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Institute of Nursing Research; the National Institute of General Medical Sciences; and the National Heart, Lung, and Blood Institute. A color image accompanies the online version of this article.
Grant Productivity Metrics
These grants resulted in 2887 articles, 103,307 PubMed citations, and an overall mean grant impact metric of 53 ± 173. The R01 was the most productive in terms of total publications and citations, although other grant types demonstrated a higher mean grant impact metric (Table 2). Orthopaedic oncology received the highest funding while producing the most publications and citations (Table 3). Approximately one-third of R01 grants eligible for competitive renewal were successfully renewed throughout the study period (38% of eligible grants [31 of 82]). Additionally, approximately one-half of K-awardees could complete a K to R01 transition (46% of awardees [12 of 26]).
Table 2.
NIH grant data and productivity metrics by grant type
| Grant type | Number of grants | Funding, in millions of USD | Publications | Citations | Total grant impact metric | Mean grant impact metric |
| F32 or similar | 4 | 0.4 | 10 | 387 | 312 | 78 ± 74 |
| K award | 26 | 15.8 | 295 | 7708 | 1221 | 47 ± 62 |
| R01 | 108 | 213.5 | 1765 | 69,429 | 3152 | 29 ± 48 |
| R03 | 25 | 4.7 | 109 | 2873 | 1338 | 54 ± 69 |
| R13 | 21 | 0.4 | 16 | 594 | 2352 | 112 ± 333 |
| R21 | 29 | 9.6 | 104 | 3577 | 1042 | 36 ± 70 |
| Other R | 13 | 13.1 | 54 | 1532 | 135 | 10 ± 17 |
| T32 | 6 | 7.2 | 169 | 5987 | 398 | 66 ± 44 |
| Other grants | 14 | 73.6 | 365 | 11,220 | 3184 | 227 ± 546 |
Publications are defined as PubMed-indexed published articles. Citations are per the NIH database iCite, which tracks PubMed citations. The total grant impact metric is defined as the summation of all individual grant impact metrics for a given grant type, whereas the mean grant impact metric is the mean of the individual grant impact metrics for a given grant type. Mean impact data are presented as mean ± standard deviation. F32 or similar = F30, F31, F32.
Table 3.
NIH grant data and productivity metrics by subspecialty
| Subspecialty | Number of grants | Funding, in millions of USD | Publications | Citations | Total grant impact metric | Mean grant impact metric |
| Adult reconstruction | 31 | 32.1 | 217 | 10,163 | 1001 | 32 ± 59 |
| Foot and ankle | 6 | 3.6 | 30 | 804 | 93 | 15 ± 15 |
| Hand and upper extremity | 37 | 52.3 | 463 | 12,499 | 976 | 26 ± 54 |
| Orthopaedic oncology | 36 | 82.6 | 586 | 19,468 | 1681 | 47 ± 88 |
| Pediatric orthopaedics | 30 | 23.0 | 148 | 6182 | 771 | 26 ± 46 |
| Spine | 31 | 39.7 | 323 | 9156 | 813 | 26 ± 37 |
| Sports medicine | 21 | 28.0 | 428 | 17,577 | 4976 | 237 ± 521 |
| Trauma | 18 | 14.0 | 104 | 4030 | 491 | 27 ± 49 |
| General orthopaedics | 24 | 41.9 | 392 | 16,505 | 1821 | 76 ± 129 |
| Multiple | 12 | 21.1 | 196 | 6923 | 511 | 43 ± 61 |
Mean impact data are presented as mean ± standard deviation. Funding includes all NIH grants received over the study period after excluding M01 and UL1 grants. Publications are defined as PubMed-indexed published articles. Citations are per the NIH database iCite, which tracks PubMed citations. The total grant impact metric is defined as the summation of all individual grant impact metrics for a given grant type, whereas the mean grant impact metric is the mean of the individual grant impact metrics for a given grant type.
Factors Associated With Grant Funding
After controlling for potentially confounding variables, we found that a PhD degree (compared with no additional degree; odds ratio 6 [95% confidence interval 4 to 11]; p < 0.001), MS degree (compared with no additional degree; OR 3 [95% CI 1.2 to 6]; p = 0.02), associate professor rank (compared with assistant professor; OR 3 [95% CI 2 to 6]; p < 0.001), professor status (compared with assistant professor; OR 9 [95% CI 5 to 15]; p < 0.001), chair or vice chair (compared with no leadership position; OR 2 [95% CI 1.2 to 4]; p = 0.009), and higher institutional funding rank (OR 0.98 [95% CI 0.97 to 0.99]; p < 0.001) were associated with an increased odds of receiving grant funding (Table 4).
Table 4.
Multivariable binomial logistic regression analysis factors
| Characteristic | OR (95% CI) | p value |
| Gender, men | 0.9 (0.5 to 1.7) | 0.80 |
| Graduate degree (non-MD) | ||
| PhD | 6 (4 to 11) | < 0.001 |
| MS | 3 (1.2 to 6) | 0.02 |
| Division | ||
| Adult reconstruction | 0.7 (0.3 to 1.8) | 0.46 |
| Foot and ankle | 0.4 (0.1 to 1.4) | 0.14 |
| Hand and upper extremity | 0.8 (0.3 to 2.2) | 0.74 |
| Orthopaedic oncology | 2 (0.7 to 5) | 0.17 |
| Pediatric orthopaedics | 0.6 (0.2 to 1.6) | 0.34 |
| Spine | 0.6 (0.2 to 1.5) | 0.24 |
| Sports medicine | 0.7 (0.3 to 1.8) | 0.46 |
| Trauma | 0.6 (0.2 to 1.5) | 0.26 |
| Multiple | 0.7 (0.2 to 2.1) | 0.51 |
| Professorship | ||
| Associate | 3 (2 to 6) | < 0.001 |
| Full | 9 (5 to 15) | < 0.001 |
| Leadership | ||
| Chair or Vice Chair | 2 (1.2 to 4) | 0.009 |
| Division chief | 1.1 (0.7 to 1.8) | 0.59 |
| PD or APD | 0.6 (0.2 to 1.5) | 0.28 |
| Rank | 0.98 (0.97 to 0.99) | < 0.001 |
| Funded PhD | 1.4 (0.9 to 2.2) | 0.12 |
The PhD and MS degrees, associate and full professorship, Chair or Vice Chair leadership positions, and higher institutional NIH funding rank were associated with increased proportions of NIH funding. Comparator groups: graduate degree: no additional degree, division: general orthopaedics, professorship: assistant, leadership: no leadership position. Chair or Vice Chair represents department of orthopaedic surgery lead, whereas division chief represents subspecialty lead. PhD = Doctor of Philosophy; MS = Master of Science; PD = residency program director; APD = associate residency program director.
We found orthopaedic surgeons who were men (compared with orthopaedic surgeons who were women; OR 0.9 [95% CI 0.5 to 1.7]; p = 0.80) were not associated with an increased or decreased odds of receiving grant funding. Additionally, no orthopaedic subspecialty (compared with comparator group general orthopaedics) was associated with an increased or decreased odds of receiving grant funding. A department having a single funded PhD researcher may be associated with surgeon-scientists obtaining grant funding, but with the numbers available, we could not demonstrate this is the case (OR 1.4 [95% CI 0.9 to 2.2]; p = 0.12).
Discussion
NIH grant funding has helped to drive major diagnostic and therapeutic advancements in orthopaedic surgery [7-9, 20, 21]. However, this funding has become increasingly difficult for surgeon-scientists to obtain because of increasing grant competition and clinical demands [12, 14, 26, 36]. In this study, we sought to determine which grants are commonly awarded, establish which grants are the most productive, and understand which factors are associated with obtaining grant funding. In doing so, we better outlined how individuals and departments can be competitive for grants, as well as which grants to pursue. Although the most-awarded grant to orthopaedic surgeons is the R01, other less competitive grants are productive and should be pursued, including the R03, R13, R21, T32, and F32 grants. Additionally, having even one funded scientist in a department may be associated with surgeon-scientist funding. Departments should consider hiring and building relationships with such individuals.
Limitations
We only evaluated current orthopaedic surgeons at academic medical centers. Retired surgeons and those who have transitioned to private practice were not included. Although this limits our ability to comment on any longitudinal trends in grant funding, our findings on grant productivity metrics and the factors associated with obtaining grants are unlikely to be affected by the lack of inclusion of these surgeons. We did not evaluate co–principal investigators, which in recent years have been allowed by the NIH. An available co–principal investigator may be a factor associated with obtaining grant funding, but we are unable to comment on this. We also included recent grants that have not yet completed their duration of funding. Without adequate time to fully use grant resources, some grant productivity metrics may be underestimated. Additionally, other funding sources such as Orthopaedic Research and Education Foundation grants and private entities were outside the scope of this work [3, 16, 22]. Nonetheless, NIH grants are a mainstay of extramural funding, and an understanding of their status in orthopaedic surgery is valuable. Surgeon demographic data were limited to those available on faculty webpages. However, these are the most complete publicly available sources for this information and are generally well maintained by institutions. Furthermore, we only analyzed articles listed in NIH RePORTER, as well as articles associated with a specific NIH grant. Because NIH RePORTER is maintained by the NIH, it is the most comprehensive and accurate source for this information.
Discussion of Key Findings
Over the long period of this study, fewer than one in 20 academic orthopaedic surgeons obtained an NIH grant, and the proportion of orthopaedic surgeons obtaining large grants (such as R01 and K-awards) was much smaller still. The funding proportion identified here among academic orthopaedic surgeons is an order of magnitude higher than the previously reported NIH funding proportion of 0.3% for all orthopaedic surgeons [6]. However, it is still below the reported percentages of other academic surgical specialties, including cardiac (18%) and thoracic (16%) surgery [24, 25]. This logically leads to the question of why this may be the case. Orthopaedic surgeons do have access to other avenues of extramural funding including private industry and Orthopaedic Research and Education Foundation grants, as well as training programs such as the American Academy of Orthopaedic Surgeons Clinician Scholar Development Program and the Orthopaedic Research Society Grant Writing Program, but the interplay of these funding sources and training programs with NIH funding is not known [3, 13, 16, 22]. Also unknown is the impact of the underrepresentation of MD-PhD candidates who pursue orthopaedic surgery or the reduced availability of residency research tracks in orthopaedic surgery compared with other fields [23, 29, 37]. Future studies might evaluate which funding sources orthopaedic surgeons most commonly choose to pursue and why. Different award mechanisms may be warranted by the NIH to achieve better funding parity between fields.
Approximately one-half of K-awardees could complete a K to R01 transition, and approximately one-third of eligible R01 grants were competitively renewed throughout the study period. These percentages do not differ meaningfully from the overall percentages of K to R01 transitions (43%) and R01 competitive renewal percentages (36%) reported elsewhere [17, 28], which implies productive use of these grants and argues in favor of continued NIH funding. However, although R01 grants were the largest category in terms of the total number awarded, funding, publications, and citations, other grants including T32, F32, R03, R13, and R21 remain productive with regard to the mean grant impact metric. Surgeon-scientists may elect to pursue these grants because they demonstrate productivity potential but are generally less competitive than R01 grants [28]. The NIH may consider increasing funding to these grants specifically as well, and department chairs might consider allocating additional research time to surgeon-scientists who pursue and earn these less common grants. Future studies might directly survey highly productive institutions and their individual grants to better characterize the specific research infrastructure and departmental policies that are associated with grant funding and productivity. These policies can then be emulated by other institutions.
Although the baseline number of women obtaining funding in orthopaedic surgery is lower than that of men and should be increased, there does not appear to be inequity in terms of the funding proportion by gender. This is particularly important given the less than favorable findings reported for other surgical fields [10, 30, 31]. Other factors associated with obtaining grant funding such as higher academic rank, additional degree training, and select department leadership positions are similar to those reported in published work [11, 18, 24, 25]. Additionally, having a single funded PhD researcher in an orthopaedic department may be associated with increased odds of surgeon-scientists obtaining funding, after controlling for confounding variables, although with the numbers available, we could not demonstrate this to be true. Therefore, departments might consider hiring nonsurgeon researchers to complement surgeon-scientists. Doing so would likely encourage collaboration and facilitate the sharing of ideas and resources, and in doing so, increase funding percentages and grant productivity [1, 4]. This is particularly relevant given the allowance of co–principal investigators on NIH grants. Future studies should evaluate direct collaboration between these groups.
Conclusion
Fewer than one in 20 academic orthopaedic surgeons have received NIH funding. The NIH might consider increasing funding to orthopaedic surgeons to achieve better parity between fields. Furthermore, although R01 grants are the most commonly awarded NIH grant to orthopaedic surgeons, other NIH grants demonstrate increased productivity metrics and should be pursued. Additionally, institutions should recruit funded PhD researchers to their departments. Future studies should investigate the role of co–principal investigators and their influence on NIH funding and productivity. They should also evaluate different sources of funding to orthopaedic surgery and specifically examine which funding avenues are most commonly pursued and why. Finally, highly productive institutions and their grants should be directly surveyed to outline the specific research infrastructure and departmental policies that are associated with grant funding and productivity.
Acknowledgment
We thank Wendy M. Novicoff PhD for assistance with the methods and statistical analyses that are presented in this work.
Footnotes
The institution of one or more of the authors (AKN) has received, during the study period, funding from the National Institutes of Health (F30 CA236370). The study was partially funded by the University of Virginia Engineering in Medicine Research Fund and Orthopaedic Research Fund.
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval was not sought for the present study.
Contributor Information
Anirudha S. Chandrabhatla, Email: ac2fp@uvahealth.org.
Jose R. Perdomo Trejo, Email: jrp7be@uvahealth.org.
Simon W. White, Email: sww4nmu@uvahealth.org.
Adishesh K. Narahari, Email: akn4uq@uvahealth.org.
A. Bobby Chhabra, Email: ac2h@hscmail.mcc.virginia.edu.
Quanjun Cui, Email: QC4Q@hscmail.mcc.virginia.edu.
References
- 1.Bell TM, Valsangkar N, Joshi M, et al. The role of PhD faculty in advancing research in departments of surgery. Ann Surg. 2017;265:111-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blue Ridge Institute for Medical Research. Table 2. Total NIH awards to each medical school in 2020 including percentage of direct and indirect costs. Available at: http://www.brimr.org/NIH_Awards/2020/default.htm. Accessed December 1, 2021.
- 3.Boddapati V, Sachdev R, Fu MC, Camp CL, Marx RG, Dines JS. Increasing industry support is associated with higher research productivity in orthopaedic surgery. J Bone Joint Surg Am. 2018;100:e36. [DOI] [PubMed] [Google Scholar]
- 4.Chinoy MR, Moskowitz J, Wilmore DW, Souba WW. Basic science faculty in surgical departments: advantages, disadvantages and opportunities. J Surg Res. 2005;123:1-2. [DOI] [PubMed] [Google Scholar]
- 5.Danthi N, Wu CO, Shi P, Lauer M. Percentile ranking and citation impact of a large cohort of National Heart, Lung, and Blood Institute-funded cardiovascular R01 grants. Circ Res. 2014;114:600-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demblowski LA, Busse B, Santangelo G, et al. NIH funding for surgeon-scientists in the US: what is the current status? J Am Coll Surg. 2021;232:265-274.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dudli S, Ballatori A, Bay-Jensen AC, et al. Serum biomarkers for connective tissue and basement membrane remodeling are associated with vertebral endplate bone marrow lesions as seen on MRI (Modic changes). Int J Mol Sci. 2020;21:3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunlop DD, Semanik P, Song J, et al. Moving to maintain function in knee osteoarthritis: evidence from the osteoarthritis initiative (OAI): a review and lessons learned 10 years after start of enrollment. Arch Phys Med Rehabil. 2010;91:714-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eckstein F, Kwoh CK, Link TM; OAI investigators. Imaging research results from the Osteoarthritis Initiative (OAI): a review and lessons learned 10 years after start of enrolment. Ann Rheum Dis. 2014;73:1289-1300. [DOI] [PubMed] [Google Scholar]
- 10.Eloy JA, Svider PF, Kovalerchik O, Baredes S, Kalyoussef E, Chandrasekhar SS. Gender differences in successful NIH grant funding in otolaryngology. Otolaryngol Head Neck Surg. 2013;149:77-83. [DOI] [PubMed] [Google Scholar]
- 11.Ence AK, Cope SR, Holliday EB, Somerson JS. Publication productivity and experience: factors associated with academic rank among orthopaedic surgery faculty in the United States. J Bone Joint Surg Am. 2016;98:e41. [DOI] [PubMed] [Google Scholar]
- 12.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: continuing challenges in the 21st century. FASEB J. 2014;28:1049-1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hegde V, Johansen D, Park HY, Zoller SD, Hamad C, Bernthal NM. The relationship between OREF grants and future NIH funding success. J Bone Joint Surg Am. 2017;99:e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu Y, Edwards BL, Brooks KD, Newhook TE, Slingluff CL, Jr. Recent trends in National Institutes of Health funding for surgery: 2003 to 2013. Am J Surg. 2015;209:1083-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutchins BI, Baker KL, Davis MT, et al. The NIH Open Citation Collection: a public access, broad coverage resource. PLoS Biol. 2019;17:e3000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iyer S, Derman P, Sandhu HS. Orthopaedics and the Physician Payments Sunshine Act: an examination of payments to U.S. orthopaedic surgeons in the Open Payments Database. J Bone Joint Surg Am. 2016;98:e18. [DOI] [PubMed] [Google Scholar]
- 17.Jagsi R, Motomura AR, Griffith KA, Rangarajan S, Ubel PA. Sex differences in attainment of independent funding by career development awardees. Ann Intern Med. 2009;151:804-811. [DOI] [PubMed] [Google Scholar]
- 18.Kron IL. Getting promoted. J Thorac Cardiovasc Surg. 2001;121:S17-S18. [DOI] [PubMed] [Google Scholar]
- 19.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 20.Ma PX. Biomimetic materials for tissue engineering. Adv Drug Deliv Rev. 2008;60:184-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29:1948-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marshall DC, Jackson ME, Hattangadi-Gluth JA. Disclosure of industry payments to physicians: an epidemiologic analysis of early data from the Open Payments Program. Mayo Clin Proc. 2016;91:84-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mittwede PN, Morales-Restrepo A, Fourman MS, et al. Research-track residency programs in orthopaedic surgery: a survey of program directors and recent graduates. J Bone Joint Surg Am. 2019;101:1420-1427. [DOI] [PubMed] [Google Scholar]
- 24.Narahari AK, Cook IO, Mehaffey JH, et al. Comprehensive National Institutes of Health funding analysis of academic cardiac surgeons. J Thorac Cardiovasc Surg. 2020;159:2326-2335.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Narahari AK, Mehaffey JH, Chandrabhatla AS, et al. Longitudinal analysis of National Institutes of Health funding for academic thoracic surgeons. J Thorac Cardiovasc Surg. 2022;163:872-879.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Narahari AK, Mehaffey JH, Hawkins RB, et al. Surgeon scientists are disproportionately affected by declining NIH funding rates. J Am Coll Surg. 2018;226:474-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institutes of Health. Research portfolio online reporting tools. Available at: https://projectreporter.nih.gov/reporter.cfm. Accessed December 1, 2021.
- 28.NIH Report. Success rates. Available at: https://report.nih.gov/funding/nih-budget-and-spending-data-past-fiscal-years/success-rates. Accessed November 1, 2022.
- 29.Robertson CM, Klingensmith ME, Coopersmith CM. Prevalence and cost of full-time research fellowships during general surgery residency: a national survey. Ann Surg. 2009;249:155-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roubinov D, Haack LM, Folk JB, et al. Gender differences in National Institutes of Health grant submissions before and during the COVID-19 pandemic. J Womens Health (Larchmt). 2022;31:1241-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silva NA, Cerasiello SY, Herendeen JS, et al. Gender differences in NIH grant funding in neurological surgery. J Clin Neurosci. 2020;80:43-49. [DOI] [PubMed] [Google Scholar]
- 32.Silvestre J, Ahn J, Levin LS. National Institutes of Health funding to departments of orthopaedic surgery at U.S. medical schools. J Bone Joint Surg Am. 2017;99:e5. [DOI] [PubMed] [Google Scholar]
- 33.Silvestre J, Hines SM, Chang B, Ahn J. Transition to independent research funding among National Institutes of Health K grant awardees at departments of orthopaedic surgery. J Bone Joint Surg Am. 2021;103:e90. [DOI] [PubMed] [Google Scholar]
- 34.Silvestre J, Ruan QZ, Chang B. Analysis of National Institutes of Health funding in hand surgery. Hand (N Y). 2019;14:560-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455-1460. [DOI] [PubMed] [Google Scholar]
- 36.Smithson M, McLeod MC, Chu DI, et al. NIH funding of researchers in surgery: decreased career development awards over time. J Surg Res. 2021;266:6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.von Kaeppler EP, Akabas MH, Brass LF, Amanatullah DF. MD-PhD graduates remain underrepresented in orthopaedic surgery: National MD-PhD Program Outcome Survey update. J Orthop Res. 2020;38:2181-2188. [DOI] [PubMed] [Google Scholar]


