Abstract
Background
Orthopaedic surgery is the surgical specialty with the lowest proportion of women. Conflicting evidence regarding the potential challenges of pregnancy and parenthood in orthopaedics, such as the implications of delayed childbearing, may be a barrier to recruitment and retainment of women in orthopaedic surgery. A summary of studies is needed to ensure that women who have or wish to have children during their career in orthopaedic surgery are equipped with the relevant information to make informed decisions.
Questions/purposes
In this systematic review, we asked: What are the key gender-related barriers pertaining to (1) family planning, (2) pregnancy, and (3) parenthood that women in orthopaedic surgery face?
Methods
Embase, MEDLINE, and PsychINFO were searched on June 7, 2021, for studies related to pregnancy or parenthood as a woman in orthopaedic surgery. Inclusion criteria were studies in the English language and studies describing the perceptions or experiences of attending surgeons, trainees, or program directors. Studies that sampled surgical populations without specific reference to orthopaedics were excluded. Quantitative and qualitative analyses were performed to identify important themes. Seventeen articles including surveys (13 studies), selective reviews (three studies), and an environmental scan (one study) met the inclusion criteria. The population sampled included 1691 attending surgeons, 864 trainees, and 391 program directors in the United States and United Kingdom. The Risk of Bias Instrument for Cross-Sectional Surveys of Attitudes and Practices tool was used to evaluate the risk of bias in survey studies. A total of 2502 women and 560 men were sampled in 13 surveys addressing various topics related to pregnancy, parenthood, and family planning during an orthopaedic career. Three selective reviews provided information on occupational hazards in the orthopaedic work environment during pregnancy, while one environmental scan outlined the accessibility of parental leave policies at 160 residency programs. Many of the survey studies did not report formal clarity, validity, or reliability assessments, therefore increasing their risk of bias. However, our analysis of the provided instruments as well as the consistency of identified themes across multiple survey studies suggests the evidence we aggregated was sufficiently robust to answer the research questions posed in the current systematic review.
Results
These data revealed that many women have witnessed or experienced discrimination related to pregnancy and parenthood, at times resulting in a decision to delay family planning. In one study, childbearing was reportedly delayed by 67% of respondents (304 of 452) because of their career choice in orthopaedics. Orthopaedic surgeons were more likely to experience pregnancy complications (range 24% to 31%) than the national mean in the United States (range 13% to 17%). Lastly, despite these challenging conditions, there was often limited support for women who had or wished to start a family during their orthopaedic surgery career. Maternity and parental leave policies varied across training institutions, and only 55% (56 of 102) of training programs in the United States offered parental leave beyond standard vacation time.
Conclusion
The potential negative effects of these challenges on the orthopaedic gender gap can be mitigated by increasing the availability and accessibility of information related to family planning, parental leave, and return to clinical duties while working as a woman in orthopaedic surgery. Future research could seek to provide a more global perspective and specifically explore regional variation in the environment faced by pregnancy or parenting women in orthopaedic surgery.
Level of Evidence
Level III, prognostic study.
Introduction
Although approximately 50% of medical school graduates are women, fewer than 15% of orthopaedic surgeons are women [12, 35]. Several studies have explored causes for this discrepancy with one common theme: Women in orthopaedics have and continue to experience gender-based discrimination in the workplace [1, 10, 31]. Gender-based discrimination is particularly prevalent for women who are, or wish to become, parents while pursuing a career in orthopaedic surgery. For example, women are asked inappropriate questions regarding their family status more frequently than men during orthopaedic interviews [2, 21]. Women are subject to discriminatory comments from colleagues and attendings regarding potential pregnancies, and they are told there are detrimental repercussions of pregnancy on a women’s career [19]. Furthermore, women who wish to become pregnant while working or training as an orthopaedic surgeon will need to navigate potential exposures to ionization radiation and toxic chemicals, long and physically demanding operative procedures, and unpredictable work schedules [7, 8, 28, 31].
The challenges surrounding family planning, pregnancy, and parenthood as a woman in orthopaedics may be perceived as a barrier to entering the field and could influence a woman’s specialty choice [14]. A survey revealed that 30% of women who had children during surgical residency would advise a woman medical student against pursuing a career in surgery [25]. Thus, prospective applicants may also be negatively influenced by the experiences of a limited number of peers. However, women who are seeking guidance from the available published evidence to help inform their decision-making about pregnancy and parenthood during a career in orthopaedic surgery will find conflicting recommendations. Specifically, there are varied reports regarding the risks associated with occupational exposure to radiation and toxic chemicals, as well as the correlation between a career in orthopaedic surgery and an increased risk of pregnancy-related complications [15, 23, 24]. A synthesis of the available evidence is needed to ensure that women who have or wish to have children during their career in orthopaedic surgery can identify and prepare for the challenges they might face.
Therefore, in this systematic review, we asked: What are the key gender-related barriers pertaining to (1) family planning, (2) pregnancy, and (3) parenthood that women in orthopaedic surgery face?
Materials and Methods
Study Design, Information Sources, and Search Strategy
We conducted the study in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [22]. A systematic search was conducted on June 7, 2021, in consultation with a medical librarian. Embase, MEDLINE, and PsychINFO were searched using a combination of the following terms and their synonyms: pregnancy OR (parental OR maternal OR parenting OR parenthood) AND orthopaedic surgery.
Selection Process
We included articles if they identified perceptions or experiences related to women in orthopaedic surgery who were pregnant or parents. Additional inclusion criteria required that the article be accessible in English; however, no limitations were made for timing of publication or region of publication. We excluded articles addressing medical students’ experiences, because this study sought to identify the perceptions and experiences of or about women actively practicing orthopaedic surgery. Actively practicing women were defined as residents, fellows, and attending surgeons. We included articles that included direct perceptions of actively practicing women by colleagues or attendings (such as program directors). Articles that collected aggregate data on women surgeons but did not provide orthopaedics-specific results were excluded. Conference abstracts were excluded because the aim of the analysis was to generate rich descriptions in keeping with a qualitative approach. Although not typical for a systematic review, review articles that summarized qualitative information that would otherwise not be captured in source publications (such as reviews summarizing practice guidelines or occupational standards for radiation exposure) were included. Review articles of primary research were excluded.
We used Covidence.org to organize the screening process. Two reviewers (LJM and AGA) screened all abstracts retrieved from the search strategy, after removal of duplicates. Disputes were resolved by consensus discussion with a third reviewer (ZM). After full-text review, the included studies were uploaded into NVivo 12 (QSR International) qualitative data software for analysis.
Data Collection Process and Data Items
We used a primarily qualitative approach to analyzing the full-text articles. The focus was on understanding the perceptions and experiences of pregnancy and parenthood in orthopaedic surgery. A thematic analysis, as described by Braun and Clarke [3], was used to analyze the included articles. Coding was performed using NVivo qualitative data software. Codes were generated inductively from the data and deductively using themes identified in previous work [29].
Study characteristics, including year of publication, location of study, study design and perspective, and the number and career stage of research participants, were extracted into a prepopulated chart. Where available, we collected quantitative data on pregnancies, including the number of pregnancies, mean age at first pregnancy, complications per attempted pregnancy, infertility per 1 year of attempted reproduction, and whether pregnancy was delayed because of career planning.
Risk of Bias Assessment
The Risk of Bias Instrument for Cross-Sectional Surveys of Attitudes and Practices tool was used to evaluate the risk of bias in survey studies (Supplemental Table 1; http://links.lww.com/CORR/B24). Most studies scored low or medium for the risk of bias with respect to the population sampled and response rate; however, many studies scored high on risk of bias with respect to managing missing data (such as nonresponders) and reporting of a clarity, validity, or reliability assessment. Although nonresponders were not evaluated in many studies, our analysis of the population sampled in the included studies reveals there was adequate representation of our population of interest (attending surgeons, residents, and trainees as well as commentary from men and women). However, our analysis of the provided instruments as well as the consistency of identified themes across multiple survey studies suggests the evidence we aggregated here was sufficiently robust to answer the research questions posed in the current systematic review.
Summary of Current Evidence
Twenty-three full-text articles were assessed for possible inclusion, with 17 meeting the eligibility criteria (Fig. 1). The included studies were conducted in the United States (15 studies) or the United Kingdom (two studies) in 2006 or later. Most studies used a survey design (13 studies), and the population sampled included 864 trainees, 1691 attending orthopaedic surgeons, and 391 program directors (Table 1). Three selective reviews and one environmental scan of 160 residency program websites were also included.
Fig. 1.
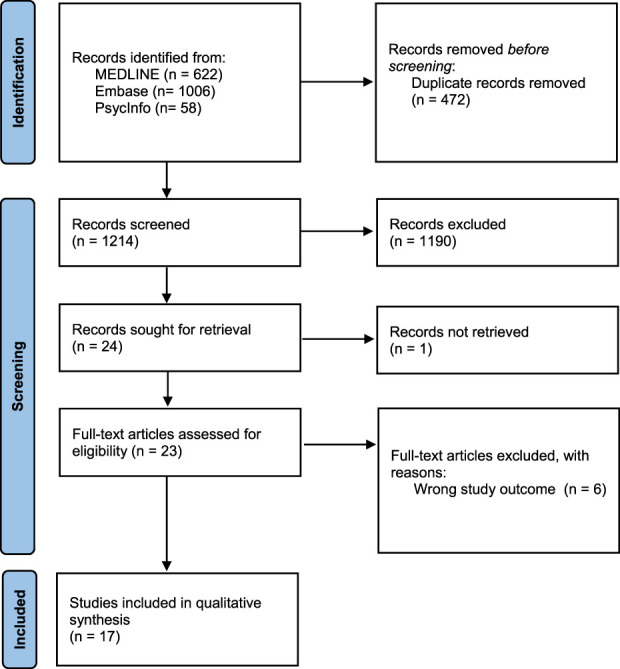
This PRISMA flow diagram shows the included studies.
Table 1.
Study characteristics
| Study | Country | Study design | Population sampled, n | Gender of respondents, n | Survey response percentage, % (n) |
| Bohl et al. [2] | USA | Survey | 488 (staff: 488) | Women: 488 | 49 (488) |
| Bucknall and Pynsent [5] | UK | Survey | 54 (staff: 54) | Women: 1 Men: 53 |
92 (54) |
| Clement et al. [6] | USA | Survey | 69 (PDs: 69) | NR | 45 (69) |
| Downes et al. [8] | USA | Selective review | |||
| Goss et al. [9] | USA | Survey | 337 (staff and trainees: 158, PDs: 179) | Women: 337 | 52 (337) |
| Hamilton et al. [11] | USA | Survey | 223 (staff: 223) | Women: 223 | 49 (223) |
| Jurenovich and Cannada [14] | USA | Survey | 252 (staff: 252) | Women: 252 | NR |
| Keene et al. [15] | USA | Selective review | |||
| Linehan and Gioe [17] | USA | Survey | 89 (staff: 89) | Women: 89 | 24 (89) |
| Mulcahey et al. [18] | USA | Survey | 190 (trainees: 190) | Women: 190 | 32 (190) |
| Nemeth et al. [19] | USA | Survey | 61 (PDs: 61) | Women: 12 Men: 49 |
40 (61) |
| Nguyen et al. [20]a | USA | Survey | 801 (staff: 585, trainees: 216) | Women: 801 | NR |
| Poon et al. [24]a | USA | Survey | 801 (staff: 585, trainees: 216) | Women: 801 | NR |
| Reid et al. [26] | USA | Survey | 495 (trainees: 458, PDs: 37) | Women: 109 Men: 458 |
NR |
| Siljander et al. [27] | USA | Environmental scan | 160 (residency programs 160) | ||
| Uzoigwe and Middleton [30] | UK | Selective review | |||
| Weiss and Teuscher [32] | USA | Survey | 45 (PDs: 45) | NR | 31 (45) |
These studies used the same dataset; however, they addressed different topics. PDs = program directors; NR = not recorded.
Results
Family Planning
Women considering starting a family have been discouraged from becoming parents by their colleagues and superiors, and they have delayed childbearing or adoption to preserve their professional reputation [11, 18, 24, 26]. In a survey of orthopaedic trainees, residents described receiving subtle remarks to discourage pregnancy; for instance, one resident recalled being told by an attending surgeon, “[I] couldn’t imagine what would happen if one of you girls got pregnant,” while another received “comments from an attending joking about requiring birth control for all female residents” [18]. Other residents reported more direct comments, “I had a conversation…with several male attendings that no resident should ever have kids during residency, especially females” [18]. Furthermore, 46% of program directors in one study believed pregnancy and parenthood had a negative effect on women’s scholarly activities [19]. In a survey of orthopaedic attendings, 21% of respondents believed their women colleagues’ family responsibilities should not be accommodated because many feared their own workload would grow consequently [5].
Many women in orthopaedics have delayed childbearing because of their career choice; however, some stated it had a limited influence [9, 11, 24]. In one study in the United States, the mean age of women orthopaedic surgeons at the time of delivery of their first child was “considerably older” than population norms (33.1 versus 24.6 years) (Table 2) [11]. When asked about reasons for delaying having children, in one study, women residents were more likely than men residents to report concerns regarding reputation (57.6% versus 0.8%; p < 0.001) and effects on career opportunities (42.4% versus 7.6%; p < 0.001) [26]. Women surgeons who were surveyed about having children reported they “would have preferred having children at an earlier time” (37% [83 of 222]) [11], but that childbearing was intentionally delayed because of their career choice as an orthopaedic surgeon (67% [304 of 452]) [24].
Table 2.
Pregnancy characteristics reported in survey studies
| Study | Respondents with at least one child, % (n) | Mean number of children | Mean age at time of first delivery in years | Delay in childbearing because of career, % (n) | Pregnancy complication, % (n) |
Miscarriage, % (n) | Infertility, % (n) | Fertility treatment, % (n) |
| Hamilton et al. [11] | 57.4 (128 of 223 surveyed) | 2.1 | 33.1 | NR | 31.2 (82 of 263 pregnancies) | 6.5 (17 of 263 surgeons) | 30.4 (45 of 148 attempted pregnancies) | 60 (27 of 45 with infertility) |
| Poon et al. [24] | 60.0 (452 of 801 surveyed) | 33.6 | 67.3 (304 of 452 respondents) | 24.4 (207 of 847 pregnancies) | 32.9 (160 of 484 attempted pregnancies) | 17% (73 of 437 surgeons sought infertility services for first pregnancy) | 12.4 (105 of 847 pregnancies) | |
| Reid et al. [26] | 39.5 (179 of 453 men and women residents) | 1.6 | NR | 56.7 (59 of 104 women residents) | NR | NR | NR | NR |
NR = not reported.
Pregnancy
Women who became pregnant during their orthopaedic surgery career faced potentially hazardous work conditions. Identified hazards to pregnancy included exposure to chemicals, radiation, and bloodborne pathogens in the operating room, as well as the physical demand of performing surgery (Table 3) [8, 11, 15, 17, 30]. Despite evidence that mitigation of these physical risks is possible, in one study, surgeons who were pregnant reported ongoing social barriers such as being excluded from cases, not being permitted to perform certain parts of procedures, and experiencing negative attitudes from colleagues [18]. Orthopaedic surgeons also were more likely to experience pregnancy-related complications (such as preterm labor or gestational diabetes) and infertility than women in the general population (Table 2). Specifically, orthopaedic surgeons were more likely to experience pregnancy complications (24% to 31%) than the national mean in the United States (13% to 17%) and the age-adjusted proportion for advanced maternal age between 35 to 39 years (20.6%). The proportion of women reporting infertility (17% [24] and 30% [11]) was found to be higher than the United States national mean (9%), but not different from that of age-matched cohorts [24].
Table 3.
Hazards of the orthopaedic work environment
| Hazard | Risk | Evidence | Mitigation Strategies |
| Exposure to radiation | Potential effects on the fetus include [15]: - Prenatal death - Growth restriction - Microsomia - Severe mental retardation - Organ malformation - Childhood cancer |
Conflicting evidence on radiation exposure when wearing standard (0.25-mm) lead aprons: - Measurable radiation exposure under a standard apron, varied by procedure [30] - No exposure during fluoroscopic procedures [8] |
- Standard lead apron [8,15] - Fetal lead apron [15] - Personal dosimeter at collar height [8] and over abdomen [15] - Increasing distance from radiation source [15] - Abstaining from participation in fluoroscopic procedures [30] |
| Exposure to MMA | Potential effects on the fetus include [15]: - Gross and skeletal fetal abnormalities - Reduction in fetal weight |
- MMA not a serious hazard when PPE used [8] - MMA levels were not elevated in orthopaedic surgeons’ breast milk postarthroplasty [17] |
- Use of vacuum mixer [8,15] - Use of personal hood [8,15] - Room air exchange [15] - Local surgical field suction [15] - Scrubbing out during cement phase of surgery [17] |
| Exposure to anesthetic gases | At high doses, anesthetic gases have fetotoxic effects [15] | - Waste levels of anesthesia gases had minimal risk to pregnant surgeons [8] - Fetotoxic effects not found at doses used for general anesthetic [15] |
- None provided |
| Exposure to bloodborne pathogens | Potential effects on the fetus include [15]: - Prenatal death - Vertical transmission HIV postexposure prophylaxis (AZT) may be mutagenic [15] |
- Transmission risks from percutaneous exposure vary from 0.3% (HIV) to 30% (hepatitis B) [8] - Maternofetal transmission risks well documented, risk up to 90% for hepatitis B infection in third trimester [8] |
- Personal protective equipment, including glove liners and full-facial coverage [8] - Postexposure prophylaxis - Discontinue breast feeding if taking AZT [15] |
| High physical demands | Potential effects on the fetus include [8]: - Preterm labour - Preeclampsia - IUGR |
- 20% to 30% maximum aerobic capacity during surgery, risks due to strenuous activity low [8] - No correlation between time in the operating room and rate of pregnancy complication, despite physical demand [14] |
- None provided |
| Extended duty hours | - Decreased water intake, lack of time for pumping when lactating can lead to mastitis and blocked ducts [17] | - Orthopaedic surgeons found to have increased risk of complications if working > 60 hours per week [14] | - None provided |
MMA = methyl methacrylate; AZT = azidothymidine; IUGR = intrauterine growth restriction.
Parenthood
Support for parenting women throughout their career in orthopaedics is lacking, with attendings experiencing a unique limitation compared with trainees [20]. Peer mentors, transparency in policy, and financial support were identified as areas requiring improvement in both groups. The overall paucity of women in orthopaedics made it difficult for women to easily access peer support; one survey respondent reported there were “no female attendings” at her institution [18]. There was variability in the awareness of and adherence to policies related to maternity leave (Table 4) as well as the provision of additional support such as lactation or breastfeeding space, childcare, and flexible scheduling (Table 5) [32]. Maternity and parental leave policies varied across training institutions, and only 55% (56 of 102) of training programs in the United States offered parental leave beyond standard vacation time [6, 27]. The mean maternity leave taken was 6.3 ± 5.0 weeks for residents and 9.6 ± 8.5 weeks for practicing surgeons (p < 0.001) [20]. We found no studies detailing the existence of or adherence to parental leave policies for attending surgeons. Although lactation policies were in place in some training programs, 43% (26 of 61) of residency program directors believed women should not be allowed to scrub out of a case to breastfeed [19].
Table 4.
Parental leave characteristics
| Study | Parental leave offered | Parental leave taken |
| Clement et al. [6] | - 55% of residency programs reported parental leave benefits - Maternity leave ranged from 1 to 8 weeks - 11% of residency programs stated they provide paid leave |
|
| Hamilton et al. [11] | - 74% of respondents took < 8 weeks (mean = 7.8 weeks); 5% took > 12 weeks - 46% of respondents dissatisfied with duration of leave - Less maternity leave during training than during clinical practice (mean = 4 weeks during training versus 7 weeks during practice) |
|
| Goss et al. [9] | - Orthopaedic residents ranked “attitudes toward maternity leave” among the least important factors influencing their program selection | |
| Mulcahey et al. [18] | - 23% of respondents stated their program had a formal maternity leave policy; 45.8% did not know whether a policy existed - 1% indicated that their program had a formal leave policy for adoptive parents or parents of children born via surrogacy - 6.3% indicated that their programs provided extended leave for complications related to pregnancy and childbirth |
- Of 22 maternity leaves reported by 19 women who had children during training: 59.1% took 5 to 8 weeks of maternity leave, 40.9% took 0 to 4 weeks, and all took < 8 weeks |
| Nguyen et al. [20] | - Mean paid leave offered was 4.6 ± 4.2 weeks for the first child and 4.5 ± 4.6 weeks for the second child - No difference in leave time offered between trainees and practicing physicians |
- Mean leave taken was 8.2 ± 7.4 weeks for the first child and 8.4 ± 6.3 weeks for the second child - Practicing surgeons took more leave than did residents (9.6 ± 8.5 weeks vs 6.3 ± 5.0 weeks; p < 0.001) - Mean cost of maternity leave was greater for staff surgeons than residents (USD 45,350.08 versus USD 153.85; p < 0.001) |
| Reid et al. [26] | - 49.9% of residents unsure whether their program had a formal parental leave policy; 19.1% noted that there was no formal parental leave policy - 31.1% reported a known formal leave policy; 43.4% of these residents described the policy as inadequate - 78.4% of PDs reported that their program had a policy - PDs reported a mean maximum allotted time of 3.9 weeks (95% CI 2.2-5.5 weeks) for paternity leave and 7.1 weeks (95% CI 5.6-8.5 weeks) for maternity leave |
- Residents who were men who had children during residency reported taking less parental leave than residents who were women (0.8 vs 4.6 weeks; p < .001) |
| Siljander et al. [27] | - 84% of programs had transparent, accessible parental leave information on their websites: 3% on their program website, 81% on the institution website - 21% of programs offered paid parental leave |
|
| Weiss and Teuscher [32] | - 80% of programs had a formal maternity leave policy; 49% of programs had a formal paternity leave policy - 18% of programs had an adoption leave policy; 18% of programs had no formal policy - For programs that had parental leave policies: 60% allowed 4 to 6 weeks off; 19% allowed 6 weeks off, and 9% allowed 4 weeks off - In 38% of policies, parental leave was allocated as vacation - 46% of programs required makeup time; 16% of programs listed makeup time as an option |
- 61% of programs reported no utilization of leave by trainees - 85% of programs reported utilization by 3 or fewer residents - Reasons for leave included maternity (61%), paternity (31%), and adoption (8%) |
PD = program director.
Table 5.
Characteristics of lactation/breastfeeding and childcare practices and policies
| Study | Lactation or breastfeeding | Childcare |
| Hamilton et al. [11] | - 90% of women breastfed for > 1 month and 71% continued for > 4 months - Most women who discontinued breastfeeding before 6 months reported problems with accessibility or time for breastfeeding after their return to work - Mean duration of breastfeeding was shorter during training than clinical practice (4.7 versus 8.3 months; p = 0.003) - Reported dissatisfaction with length of breastfeeding was higher among women in training than in clinical practice |
|
| Mulcahey et al. [18] | - 22% of respondents indicated their program provided facilities for production and storage of breast milk; 48% did not know whether such facilities existed - 9% responded that their program allowed residents to scrub out of a procedure to pump breast milk; 76% did not know whether such a policy existed |
- 7% of respondents stated their program provided on-site childcare; 66% said it was not available; 26% did not know |
| Reid et al. [26] | - 4% of residents reported that they had access to discounted childcare; no residents reported free childcare - 74% of residents with children reported that childcare was unaffordable |
Other Relevant Findings
Although many of the challenges faced by trainees and practicing surgeons were universal throughout family planning, pregnancy, and parenthood, there were also important differences between these two cohorts. For example, the financial implications of parental leave were greater for attending surgeons than for trainees (Fig. 2).
Fig. 2.
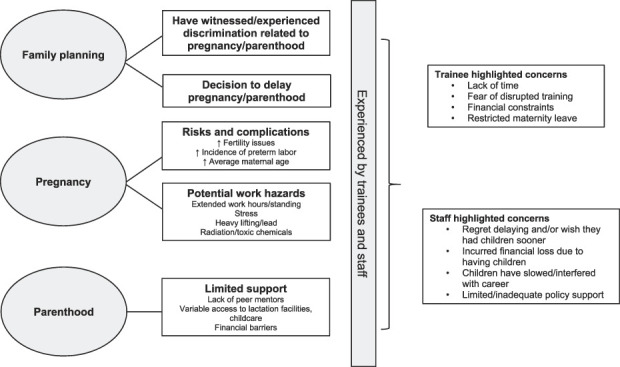
This thematic map demonstrates three stages during which women who have or wish to have a family experience gender-based discrimination, barriers, and challenges in orthopaedics.
Discussion
Although medical school graduating classes are represented by near-equal proportions of women and men, gender representation in orthopaedic surgery remains disparate (more than 85% men in most countries worldwide) [33]. This raises the question: Why are women not choosing orthopaedic surgery as a career? One of the suggested causes is the perceived incompatibility between being an orthopaedic surgeon and having a family. This study sought to elucidate this potential barrier with a systematic review focused on the perceptions and experiences of pregnant and parenting women in orthopaedic surgery in three distinct stages: family planning, pregnancy, and parenthood (Fig. 2). We found that many women have witnessed or experienced discrimination related to pregnancy and parenthood, resulting in a decision to delay pregnancy. In turn, women faced increased risks of complications in pregnancy, partly because of advanced maternal age but compounded by the potential hazards of the orthopaedic work environment. Lastly, despite these challenging conditions, there was often limited support for women who have or wish to start a family during their orthopaedic career. A concerted effort at the undergraduate, graduate, administrative, and international levels is needed to shift the culture to embrace the possibility of pregnancy and parenthood for women in orthopaedics (Table 6).
Table 6.
Suggestions to decrease barriers related to pregnancy and parenthood in orthopaedic surgery
| Level | Suggestions |
| Undergraduate | - Provide education on family planning to students (policies, financial considerations) - Connect prospective students with women mentors where possible (in person or virtual) or a cross-gender ally |
| Postgraduate | - Provide education on family planning to trainees (policies, financial considerations) - Promote resident–medical student mentorship - Outline clear maternity leave, lactation, and childcare policies - Plan for the possibility of pregnant residents - Support new parents in their transition back to training |
| Hospital or hiring organizations | - Provide education on family planning to staff (policies, financial considerations) - Recruit women surgeons with children to academic settings and positions of leadership - Promote staff–trainee and staff–staff mentorship - Plan for the possibility of pregnant staff - Establish clear policies for maternity leave, lactation - Explore supporting or providing childcare |
| International orthopaedic community | - Investigate local barriers to the recruitment and retainment of woman surgeons who have or wish to start a family; consider using qualitative methods for an in-depth understanding of local issues - Investigate factors influencing fertility and pregnancy complications and their mitigating strategies; consider using experimental research methods |
Limitations
This systematic review has several limitations, including the quality of included studies, the regional distribution of data, and the conflation of concepts related to sex and gender in the available studies. Most publications used a survey design that has the advantage of reaching a large sample size but may lack nuance in the quality of data received. The included surveys were assessed to have a high risk of bias because the used instruments lacked validity. Despite this, we believe the data we obtained were relevant and sufficient to provide an understanding of the subject matter. Additionally, many of the included studies had a large sample size with moderate to high response proportions ranging from 24% to 92%. We believe we had a sufficiently representative sample of the population of interest (women in orthopaedics) but the results are best interpreted in the context of women’s experiences in the United States, because most data were collected in the United States. Regions with diverse licensing requirements, maternity leave policies, and cultural norms may have different experiences that should be explored. The concepts of sex and gender were not differentiated in the studies we found, with all studies characterizing participants by sex. In fact, many should have characterized by gender, because many concepts that were addressed referred to social roles rather than biological function (with the exception of fertility and pregnancy complications). This could underrepresent or misrepresent individuals with diverse gender identities. Because of the underrepresentation of women in orthopaedics, we focused on the gender-based experiences of women; however, exploring the parental experiences of men and other gender identities in orthopaedics is another important avenue of study. Furthermore, few studies discussed policy or experiences related to adoptive parenting, surrogate pregnancy, or miscarriage.
Family Planning
Consistent findings in our review were pressures (real and perceived) on women to delay starting families [24]; perhaps because of this, women orthopaedic surgeons were much older at the time of their first delivery than population norms [10]. This could reflect a perception of discussing family planning in orthopaedics as “taboo.” To combat negative perceptions, trainees and attending surgeons should be formally educated on program policies related to pregnancy and parenthood. Individuals who need more support could be provided with the opportunity to connect with a suitable mentor, whether that be in person or through an online network (such as Women in Orthopaedics Worldwide or the Ruth Jackson Orthopaedic Society). Increasing the visibility of women in academic settings and positions of leadership who choose to have children may also be a primary strategy to help normalize the idea of parenting during an orthopaedic career. Given the current proportion of men in orthopaedics, allyship and cross-gender mentorship is also critical [13, 16]. Men should also be encouraged to support women who wish to have families in orthopaedics and speak out against gender-related discrimination.
Pregnancy
Women in orthopaedics are more likely to report infertility and pregnancy complications than women in the general population are, which may be associated with physical hazards in the operating room [15, 24]. Infertility and complications have been shown to be more common depending on conditions of the orthopaedic work environment such as long hours, physical labor, and psychologic stress [24]. However, it is still unknown to what extent the impact of delayed pregnancy and advanced maternal age contributes to fertility and pregnancy complications compared with the orthopaedic work environment itself. Embracing the possibility of pregnancy in orthopaedic training may reduce the pressure women experience to delay starting a family. Training programs and hospital administration should anticipate that both men and women surgeons may become parents and have strategies in place to accommodate modified work duties and have plans for maintaining adequate call coverage during their pregnancy and parental leave. Furthermore, pregnant women should be supported to make informed decisions regarding operating room participation, because the current evidence suggests that strategies for limiting exposure to physical hazards such as radiation and toxic chemicals are effective [8, 15, 24].
Parenthood
Parental leave policies in orthopaedic programs are inconsistent and often unsupportive of people who wish to start families; for example, nearly half of orthopaedic training programs in one survey offered surgical learners no parental leave beyond standard vacation time [6]. Although most training programs have a maternity leave policy, residents continue to face barriers in accessing and using such policies. A call to action has been made by Worthington et al. [34] to introduce standard, paid parental leave for all residents, citing benefits such as supporting parent and child health, promoting residency wellness, and reducing gender disparities. Therefore, governing bodies should work with all relevant stakeholders, including women who are pregnant and those who are parents, to determine what constitutes an adequate maternity leave with respect to length, pay, and considerations for assisting return to work such as lactation space and access to childcare. This is currently unknown in the orthopaedic context.
Other Relevant Findings
Finally, attending surgeons faced unique challenges with respect to family planning, pregnancy, and maternity leave, because the guidelines, policies, and support for attendings are even less explicit than for trainees. For example, the mean cost of maternity leave for an attending surgeon was dramatically greater than that of a trainee (USD 153.85 versus USD 45,350.08) [20]. None of the studies commented on how women surgeons are supported in their return to clinical work after leave. Examples of supportive transition include providing a mentor, providing a period of modified duties, and offering supervision [4]. Given the positive impact of attending–student mentorship, considerations to encourage and support practicing orthopaedic surgeons who wish to start a family during their career could have downstream effects on the recruitment of women medical students.
Conclusion
Orthopaedic surgery has the lowest proportion of women of all surgical specialties. We found that women may experience gender-based discrimination related to pregnancy and parenthood, either directly or indirectly. Discriminatory experiences combined with the demands of an orthopaedic career may influence women to delay childbearing, which is associated with increased maternal risks. Women may also face potential challenges related to the physical, psychologic, and financial implications of becoming pregnant during their training or career. Acknowledgment and action are needed from the orthopaedic community to normalize, encourage, and support family planning, pregnancy, and parenthood for women in orthopaedic surgery.
Acknowledgment
We thank Diane Lorenzetti MLS, PhD, who provided guidance for our systematic search.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
The work was performed at the University of Calgary in Calgary, AB, Canada.
Contributor Information
Annalise G. Abbott, Email: Annalise.abbott@ucalgary.ca.
Zoe Mack, Email: zoe.mack@ucalgary.ca.
Prism Schneider, Email: prism.schneider@ahs.ca.
Laurie A. Hiemstra, Email: hiemstra@banffsportmed.ca.
References
- 1.Ahmed M, Hamilton LC. Current challenges for women in orthopaedics. Bone Jt Open. 2021;2:893-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bohl DD, Iantorno SE, Kogan M. Inappropriate questions asked of female orthopaedic surgery applicants from 1971 to 2015: a cross-sectional study. J Am Acad Orthop Surg. 2019;27:519-526. [DOI] [PubMed] [Google Scholar]
- 3.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77-101. [Google Scholar]
- 4.British Orthopaedic Association. Return to work. Available at: https://www.boa.ac.uk/careers-in-t-o/parenthood-orthopaedics/return-to-work.html. Accessed March 8, 2022.
- 5.Bucknall V, Pynsent PB. Sex and the orthopaedic surgeon: a survey of patient, medical student and male orthopaedic surgeon attitudes towards female orthopaedic surgeons. Surgeon. 2009;7:89-95. [DOI] [PubMed] [Google Scholar]
- 6.Clement RC, Olsson E, Katti P, Esther RJ. Fringe benefits among us orthopedic residency programs vary considerably: a national survey. HSS J. 2016;12:158-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CMA. 2019. Canadian Medical Association physician workforce survey results. Available at: https://www.cma.ca/2019-cma-physician-workforce-survey-results. Accsssed December 21, 2022.
- 8.Downes J, Rauk PN, Vanheest AE. Occupational hazards for pregnant or lactating women in the orthopaedic operating room. J Am Acad Orthop Surg. 2014;22:326-332. [DOI] [PubMed] [Google Scholar]
- 9.Goss ML, McNutt SE, Hallan DR, Bible JE. Factors in orthopaedic residency decision-making for female applicants: a cross-sectional study. J Am Acad Orthop Surg. 2020;28:1055-1060. [DOI] [PubMed] [Google Scholar]
- 10.Halim UA, Elbayouk A, Javed S, Ali AM, Cullen CM. The prevalence and impact of gender bias and sexual discrimination in orthopaedics, and mitigating strategies. Bone Joint J. 2020;102:1446-1456. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton AR, Tyson MD, Braga JA, Lerner LB. Childbearing and pregnancy characteristics of female orthopaedic surgeons. J Bone Joint Surg Am. 2012;94:e77. [DOI] [PubMed] [Google Scholar]
- 12.Hiemstra LA, Wittman T, Mulpuri K, Vezina C, Kerslake S. Dissecting disparity: improvements towards gender parity in leadership and on the podium within the Canadian Orthopaedic Association. J ISAKOS. 2019;4:227-232. [Google Scholar]
- 13.Johnson WB, Smith DG. Athena Rising: How and Why Men Should Mentor Women. Bibliomotion; 2016. [Google Scholar]
- 14.Jurenovich KM, Cannada LK. Women in orthopedics and their fellowship choice: what influenced their specialty choice? Iowa Orthop J. 2020;40:13-17. [PMC free article] [PubMed] [Google Scholar]
- 15.Keene RR, Hillard-Sembell DC, Robinson BS, Saleh KJ, Novicoff WM. Occupational hazards to the pregnant orthopaedic surgeon. J Bone Joint Surg Am. 2011;93:e141. [DOI] [PubMed] [Google Scholar]
- 16.Leopold SS. Editorial: fears about #metoo are no excuse to deny mentorship to women in orthopaedic surgery. Clin Orthop Relat Res. 2019;477:473-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linehan CM, Gioe TJ. Serum and breast milk levels of methylmethacrylate following surgeon exposure during arthroplasty. J Bone Joint Surg Am. 2006;88:1957-1961. [DOI] [PubMed] [Google Scholar]
- 18.Mulcahey MK, Nemeth C, Trojan JD, O’Connor MI. The perception of pregnancy and parenthood among female orthopaedic surgery residents. J Am Acad Orthop Surg. 2019;27:527-532. [DOI] [PubMed] [Google Scholar]
- 19.Nemeth C, Roll E, Mulcahey MK. Program directors’ perception of pregnancy and parenthood in orthopedic surgery residency. Orthopedics. 2020;43:E109-E113. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen C V, Luong M, Weiss JM, Hardesty C, Karamitopoulos M, Poon S. The cost of maternity leave for the orthopaedic surgeon. J Am Acad Orthop Surg. 2020;28:e1001-e1005. [DOI] [PubMed] [Google Scholar]
- 21.O’Connor MI. Medical school experiences shape women students’ interest in orthopaedic surgery. Clin Orthop Relat Res. 2016;474:1967-1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phillips EA, Nimeh T, Lerner LB, Braga J. Does a surgical career affect a woman’s childbearing and fertility? A report on pregnancy and fertility trends among female surgeons. J Am Coll Surg. 2014;219:944-950. [DOI] [PubMed] [Google Scholar]
- 24.Poon S, Luong M, Hargett D, et al. Does a career in orthopaedic surgery affect a woman’s fertility? J Am Acad Orthop Surg. 2021;29:e243-e250. [DOI] [PubMed] [Google Scholar]
- 25.Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surg. 2018;153:644-652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reid DBC, Shah KN, Lama CJ, Kosinski LR, Daniels AH, Eberson CP. Parenthood among orthopedic surgery residents: assessment of resident and program director perceptions on training. Orthopedics. 2021;44:98-104. [DOI] [PubMed] [Google Scholar]
- 27.Siljander BR, Van Heest AE, Van Nortwick SS, Flakne JC, Bohn DC. What proportion of orthopaedic surgery residency programs have accessible parental leave policies, and how generous are they? Clin Orthop Relat Res. 2020;478:1506-1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sudarshan M, Hanna WC, Jamal MH, Nguyen LHP, Fraser SA. Are Canadian general surgery residents ready for the 80-hour work week? A nationwide survey. Can J Surg. 2012;55:53-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Todd AR, Cawthorn TR, Temple-Oberle C. Pregnancy and parenthood remain challenging during surgical residency: a systematic review. Acad Med. 2020;95:1607-1615. [DOI] [PubMed] [Google Scholar]
- 30.Uzoigwe CE, Middleton RG. Occupational radiation exposure and pregnancy in orthopaedics. J Bone Joint Surg Br. 2012;94:23-27. [DOI] [PubMed] [Google Scholar]
- 31.VanHeest A. Gender diversity in orthopedic surgery: we all know it’s lacking, but why? Iowa Orthop J. 2020;40:1-4. [PMC free article] [PubMed] [Google Scholar]
- 32.Weiss J, Teuscher D. What provisions do orthopaedic programs make for maternity, paternity, and adoption leave? Clin Orthop Relat Res. 2016;474:1945-1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Women in Orthopaedics Worldwide. Women in ortho per country. Available at: https://wowortho.org/. Accessed March 22, 2022.
- 34.Worthington RO, Feld LD, Volerman A. Supporting new physicians and new parents: a call to create a standard parental leave policy for residents. Acad Med. 2019;94:1654-1657. [DOI] [PubMed] [Google Scholar]
- 35.Yue T, Khosa F. Academic gender disparity in orthopedic surgery in canadian universities. Cureus. 2020;12:e7205. [DOI] [PMC free article] [PubMed] [Google Scholar]


