Abstract
Background
Ankylosing spondylitis–related cervical spine fracture with neurologic impairment (ASCF-NI) is a rare but often lethal injury. Factors independently associated with survival after treatment remain poorly defined, and identifying patients who are likely to survive the injury remains challenging.
Questions/purposes
(1) What factors are independently associated with survival after treatment among patients with ASCF-NI? (2) Can a nomogram be developed that is sufficiently simple for clinicians to use that can identify patients who are the most likely to survive after injury?
Methods
This retrospective study was conducted based on a multi-institutional group of patients admitted and treated at one of 29 tertiary hospitals in China between March 1, 2003, and July 31, 2019. A total of 363 patients with a mean age of 53 ± 12 years were eventually included, 343 of whom were male. According to the National Household Registration Management System, 17% (61 of 363) died within 5 years of injury. Patients were treated using nonsurgical treatment or surgery, including procedures using the anterior approach, posterior approach, or combined anterior and posterior approaches. Indications for surgery included three-column injury, unstable fracture displacement, neurologic impairment or continuous progress, and intervertebral disc incarceration. By contrast, patients generally received nonsurgical treatment when they had a relatively stable fracture or medical conditions that did not tolerate surgery. Demographic, clinical, and treatment data were collected. The primary study goal was to identify which factors are independently associated with death within 5 years of injury, and the secondary goal was the development of a clinically applicable nomogram. We developed a multivariable Cox hazards regression model, and independent risk factors were defined by backward stepwise selection with the Akaike information criterion. We used these factors to create a nomogram using a multivariate Cox proportional hazards regression analysis.
Results
After controlling for potentially confounding variables, we found the following factors were independently associated with a lower likelihood of survival after injury: lower fracture site, more-severe peri-injury complications, poorer American Spinal Injury Association (ASIA) Impairment Scale, and treatment methods. We found that a C5 to C7 or T1 fracture (ref: C1 to C4 and 5; hazard ratio 1.7 [95% confidence interval 0.9 to 3.5]; p = 0.12), moderate peri-injury complications (ref: absence of or mild complications; HR 6.0 [95% CI 2.3 to 16.0]; p < 0.001), severe peri-injury complications (ref: absence of or mild complications; HR 30.0 [95% CI 11.5 to 78.3]; p < 0.001), ASIA Grade A (ref: ASIA Grade D; HR 2.8 [95% CI 1.1 to 7.0]; p = 0.03), anterior approach (ref: nonsurgical treatment; HR 0.5 [95% CI 0.2 to 1.0]; p = 0.04), posterior approach (ref: nonsurgical treatment; HR 0.4 [95% CI 0.2 to 0.8]; p = 0.006), and combined anterior and posterior approach (ref: nonsurgical treatment; HR 0.4 [95% CI 0.2 to 0.9]; p = 0.02) were associated with survival. Based on these factors, a nomogram was developed to predict the survival of patients with ASCF-NI after treatment. Tests revealed that the developed nomogram had good performance (C statistic of 0.91).
Conclusion
The nomogram developed in this study will allow us to classify patients with different mortality risk levels into groups. This, coupled with the factors we identified, was independently associated with survival, and can be used to guide more appropriate treatment and care strategies for patients with ASCF-NI.
Level of Evidence
Level III, therapeutic study
Introduction
Ankylosing spondylitis (AS) is chronic inflammatory arthritis associated with multilevel spinal bone fusion [1]. Bone fusion involves the disc space anteriorly and the facet joints posteriorly. As the disease progresses, pathologic changes lead to excessive stiffness of the entire spine (often referred to as “bamboo spine”) and kyphosis [33]. Epidemiologic evidence suggests that the spines of patients with AS are more susceptible to fracture; this risk has been estimated to be approximately 3.3 times more severe than in a healthy spine [27]. Cervical spine fractures occur more commonly than thoracic or lumbar fractures in patients with AS [38]. Clinically, AS-related cervical fractures (ASCF) often involve all three columns of the spine, making them generally unstable fractures, all the more so because these patients often have longer lever arms and greater torque associated with multilevel ankyloses [28, 38]. As a result, patients with ASCF are at high risk of neurologic impairment after fracture [37]. ASCF with neurologic impairment (ASCF-NI) is life threatening and results in a much higher risk of death than more common fractures in the cervical spine [40]. Thus, the treatment of patients with ASCF-NI is more complicated and challenging. Current treatment strategies mainly include nonsurgical and surgical treatment. Surgical approaches include the anterior approach, posterior approach, and combined anterior and posterior approach [13, 18, 21, 32]. Knowing which patients are likely to survive their injuries can help clinicians decide which treatment approaches are the most sensible. Until recently, there were no treatment guidelines on the topic, and the 2015 guideline on the topic focused on surgery [19] but did not provide details about other factors that might be associated with an increased or decreased likelihood that a patient might survive this serious injury. Relatively little information is available on which factors might be associated with survival [35], and to our knowledge, there is no clinically useful, easy-to-use treatment nomogram that might help inform a clinician’s decision-making process in this high-stakes setting.
We therefore asked: (1) What factors are independently associated with survival after treatment among patients with ASCF-NI? (2) Can a nomogram be developed that is sufficiently simple for clinicians to use that can identify patients who are the most likely to survive after injury?
Patients and Methods
Study Design and Setting
This was a retrospective study drawn from a multi-institutional database maintained in the spine departments of 29 tertiary-care hospitals in China. These hospitals are in urban areas.
Patient Population and Data Collection
Patients were identified from a retrospective, multi-institutional database consisting of 509 patients who sustained ASCFs and were admitted by spine specialists between March 1, 2003, and July 31, 2019, at 29 tertiary hospitals in China. Patients were included if they met the following criteria: diagnosis of AS based on the New York Diagnostic Criteria revised in 1984, at least one cervical fracture (C1 to C7 or T1) confirmed by imaging examination, fracture combined with neurologic impairment (American Spinal Injury Association [ASIA] neurologic function classification A to D), and no history of cervical spine surgery. Exclusion criteria included death within 24 hours after injury (the patient died before receiving effective treatment and evaluation), history of tumors or space-occupying lesions in the cervical spinal canal, and missing vital records (ID number, initial consultation records, or surgical records). After applying these inclusion and exclusion criteria, we included 363 patients in the analyzed cohort (Fig. 1). Given the retrospective nature of this study, no additional patient informed consent was needed. A group of three surgeons reviewed the accuracy of the included data each time the data were included.
Fig. 1.
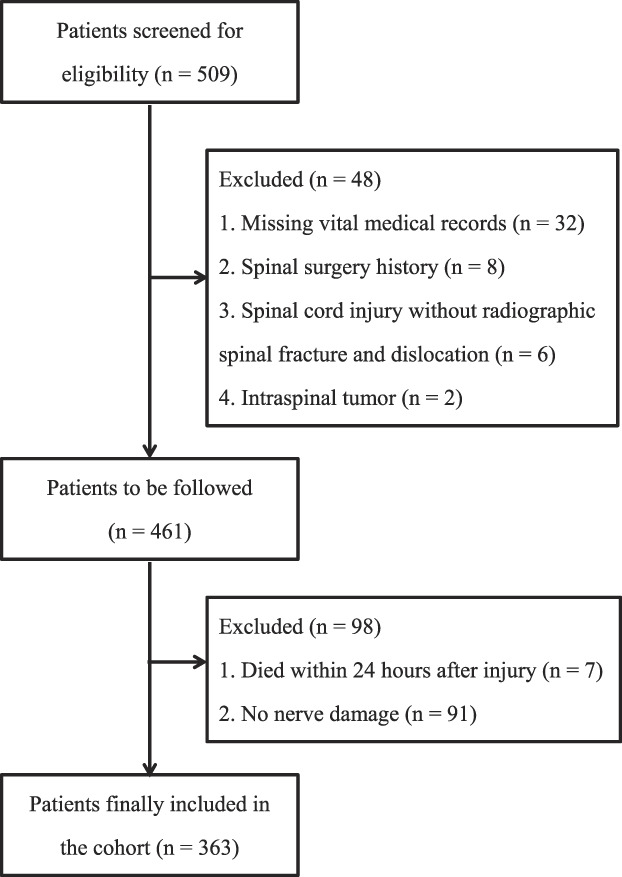
This flow diagram shows the process of patient inclusion and exclusion.
Patients’ Baseline Data and Study Variables
We obtained the demographic and clinical characteristics of patients by consulting our hospital database, including age, gender, hospital stay, time from injury to admission, injury type (multiple injuries or single injury), mechanism of injury (high-energy or low-energy injury), fracture site (C1 to C4 or 5 or C5 to C7 or T1), ASIA classification (ASIA Class A to D), underlying diseases (present or absent), Charlson comorbidity index score (0, 1, or 2 or more), and peri-injury complications (absent, mild, moderate, or severe). Treatment details included methods (nonsurgical or surgical), and if the method was surgical, we noted the surgical approaches (anterior approach, posterior approach, and combined anterior and posterior approach), as well as time from injury to surgery, operation time, and intraoperative bleeding. During the period in question, patients generally received nonsurgical treatment when they had a relatively stable fracture or medical conditions that did not tolerate surgery. By contrast, patients received surgical treatment when they had a three-column injury, unstable fracture displacement, neurologic impairment or continuous progression, and intervertebral disc incarceration. Patients with anterior spinal cord compression were usually treated with an anterior approach, and those with posterior joint locking were generally treated with a posterior approach. Patients with poor bone quality usually received the combined anterior and posterior approach. In this study, the definition of multiple injuries was the presence of injuries to more than one body area or system. High-energy injuries included motor vehicle collisions, motorcycle collisions, direct crush injuries, and falls from higher than 4 feet. Low-energy injuries included injuries caused by athletic activity, ground-level twisting injuries, or falls from less than 4 feet [25]. Peri-injury complications referred to complications that occurred within 14 days after injury. In this study, peri-injury complications were divided into three levels according to their severity: severe (complications including respiratory and circulatory system dysfunction and septic shock), moderate (complications including respiratory infection, deep vein thrombosis, and internal fixation loosening), and absence of or mild complications (no complications or complications including decubitus ulcer, urinary tract infection, electrolyte disturbance, peptic ulcer, and subarachnoid or epidural hematoma) (Supplemental Table 1; http://links.lww.com/CORR/B6).
The mean age of the patients was 53 ± 12 years. Among all patients, 94% (343 of 363) were male, 78% (283 of 363) of patients agreed to undergo surgery, 33% (118 of 363) had underlying medical conditions, and 58% (209 of 363) had peri-injury complications (Table 1). The median follow-up time in this study was 38 months (interquartile range 13 to 66 months), and 17% (61 of 363) of the patients had died within 5 years of injury. The 6-month, 1-year, and 5-year mortality rates were 14% (95% confidence interval 14% to 15%), 15% (95% CI 14% to 15%), and 18% (95% CI 16% to 21%), respectively.
Table 1.
Patient and clinical characteristics
| Characteristic | Total (n = 363) |
| Age in years, mean ± SD | 53 ± 12 |
| Gender, men, % (n) | 94 (343) |
| Length of hospital stay in days, median (IQR) | 13 (9-22) |
| Time from injury to admission in hours, median (IQR) | 7 (4-12) |
| Time from injury to surgery in days, median (IQR) | 9 (5-17) |
| Operation time in minutes, mean ± SD | 263 ± 119 |
| Intraoperative bleeding in mL, mean ± SD | 469 ± 466 |
| Injury type, % (n) | |
| Single injury | 77 (281) |
| Multiple injuries | 23 (82) |
| Injury mechanism, % (n) | |
| High-energy | 36 (132) |
| Low-energy | 64 (231) |
| Fracture site, % (n) | |
| C1 to C4/5 | 28 (100) |
| C5 to C7/T1 | 72 (263) |
| Neurologic classification (ASIA) | |
| A | 22 (78) |
| B | 10 (37) |
| C | 20 (72) |
| D | 49 (176) |
| Treatment method, % (n) | |
| Nonsurgical treatment | 22 (80) |
| Anterior approach | 23 (85) |
| Posterior approach | 34 (124) |
| Combined anterior and posterior approach | 20 (74) |
| Presence of underlying disease, % (n) | |
| Presence | 33 (118) |
| Absence | 68 (245) |
| Charlson comorbidity index, % (n) | |
| 0 | 67 (242) |
| 1 | 18 (66) |
| ≥ 2 | 15 (55) |
| Levels of peri-injury complications, % (n) | |
| Severe | 16 (57) |
| Moderate | 20 (73) |
| Absence or mild | 64 (233) |
ASIA = American Spinal Cord Injury Association.
Study Outcomes
The primary study goal was to identify which factors are independently associated with death within 5 years of injury. Survival data included whether the patient had died, and if they had died, the date of their death. This information was identified through the National Household Registration Management System and based on the patients’ ID numbers. This national system records the dates of birth and death of Chinese citizens. No data were missing from this part of our study; that is, we knew the dead or alive status of all patients. The secondary goal was to develop and test a clinically applicable nomogram. The final censoring date was November 1, 2020.
Ethical Approval
Ethical approval for this study was obtained from the Medical Ethics Committee of the First Affiliated Hospital of the Chinese People's Liberation Army Military Medical University (ethics committee approval number: KY20212199-F-1).
Statistical Analysis
Categorical variables are reported as percentages and whole numbers, and continuous variables are reported as either mean with standard deviations or medians with IQRs, unless indicated otherwise. A Kaplan–Meier curve was drawn to show specific survival (Supplemental Fig. 1; http://links.lww.com/CORR/B7). This study also plotted a hazard function curve, which demonstrated that patients had the highest risk of death within 6 months of injury (Supplemental Fig. 2; http://links.lww.com/CORR/B8).
To assign a value to each variable in creating a model, we created categories for the continuous variables in the model. This study converted continuous variables, specifically age, into categorical variables using cubic spline analysis. Sensitivity analyses revealed a maximization of Wald chi-square with 4 knots (chi-square = 24.05). We noted the effect of age on the hazard ratio of mortality was linear above a threshold of approximately 54 years and constant below the same threshold (Supplemental Fig. 3; http://links.lww.com/CORR/B9). Therefore, age was divided into two categories (< 54 years and ≥ 54 years).
To ensure good performance of the model, we first calculated the maximum number of parameters that can be included in the model. For 363 patients and 61 events, the calculation was performed according to the method mentioned in the study by Riley et al [26]. The results showed that the model can incorporate up to 13 parameters (shrinkage factor = 0.909). Therefore, seven variables (12 parameters) were considered as candidate variables based on previous studies and clinical practice needs. These variables included age (two categories) [28, 30], injury type (two categories) [10, 24], underlying disease (two categories) [22], fracture site (two categories) [8, 17], peri-injury complications (three categories) [15, 36], neurologic function (four categories) [11, 15], and treatment methods (four categories) [31].
Subsequently, we used a multivariable Cox proportional hazards regression model to define the independent factors associated with survival. All candidate variables were entered into the multivariable Cox proportional hazards regression model. Independent risk factors were then defined using backward stepwise selection with the Akaike information criterion. We used a correlation matrix to evaluate all explanatory variables for collinearity, and plausible interaction terms were tested. No significant interactions were found. Therefore, no interaction term was included in the multivariable analysis. We formulated a nomogram based on the results of the multivariable Cox regression analysis.
We evaluated the nomogram’s performance according to discrimination (predictive accuracy for individual outcomes) and calibration (accuracy of point estimates of the survival function). We evaluated the discrimination of the nomogram using Harrell C statistic, which is equivalent to the area under the receiver operating characteristic (ROC) curve and is used to estimate the probability of concordance between predicted and observed outcomes. A C statistic of 0.5 indicates the absence of discrimination, whereas a C statistic of 1.0 indicates perfect separation of patients with different outcomes [9]. A C statistic of 0.50 to 0.70 has low accuracy, between 0.71 and 0.90 has medium accuracy, and higher than 0.90 has high accuracy [16]. A time-dependent ROC analysis for the proposed prognostic model was also conducted. To further assess the discriminative ability of the model, we then plotted Kaplan-Meier curves stratified by the tertile of the estimated probability that was calculated from the nomogram. Calibration was assessed by dividing the risk scores into tertiles for patients and plotting observed versus predicted survival. A calibration plot is a graphic representation of the relationship between the observed outcome frequencies and the predicted probabilities. The closer the line formed by the predicted survival and the observed survival is to a 45° diagonal line, the better the calibration of the nomogram [4]. Validation was performed using 1000 bootstrap samples to quantify overfitting of our modeling strategy and predict the future performance of the model.
In all analyses, we used p < 0.05 to indicate statistical significance. All statistical analyses were performed using Stata 10.0 (StataCorp), SPSS version 17.0 (IBM Corp), and R 4.0.4 (R Foundation for Statistical Computing) with packages Hmisc, survminer, survival, grid, lattice, Formula, ggpubr, ggplot2, rms, and pec. The data analysis was conducted from December 1, 2021, to May 1, 2022.
Results
Factors Independently Associated With Survival
After controlling for potentially confounding variables, we found the following factors were independently associated with a lower likelihood of survival after injury: lower fracture site, high-energy injury, more-severe peri-injury complications, poorer ASIA classification, and treatment methods (namely, nonsurgical treatment and anterior approach). Specifically, C5 to C7 or T1 fracture (ref: C1 to C4 or 5; HR 1.7 [95% CI 0.9 to 3.5]; p = 0.12), moderate peri-injury complications (ref: absence of or mild complications; HR 6.0 [95% CI 2.3 to 16.0]; p < 0.001), severe peri-injury complications (ref: absence of or mild complications; HR 30.0 [95% CI 11.5 to 78.3]; p < 0.001), ASIA Grade A (ref: ASIA Grade D; HR 2.8 [95% CI 1.1 to 7.0]; p = 0.03), anterior approach (ref: nonsurgical treatment; HR 0.5 [95% CI 0.2 to 1.0]; p = 0.04), posterior approach (ref: nonsurgical treatment; HR 0.4 [95% CI 0.2 to 0.8]; p = 0.006), and combined anterior and posterior approach (ref: nonsurgical treatment; HR 0.4 [95% CI 0.2 to 0.9]; p = 0.02) were associated with survival (Table 2).
Table 2.
Factors independently associated with survival after treatment for an ankylosing spondylitis cervical fracture with neurologic impairment
| Predictive variable | Regression coefficient | HR (95% CI) | p value |
| Fracture site | 0.12 | ||
| C1-C4/5 | Reference | NA | |
| C5-C7/T1 | 0.5 | 1.7 (0.9 to 3.5) | 0.12 |
| Peri-injury complications | < 0.001 | ||
| Absence or mild | Reference | NA | |
| Moderate | 1.8 | 6.0 (2.3 to 16.0) | < 0.001 |
| Severe | 3.4 | 30.0 (11.5 to 78.3) | < 0.001 |
| Treatment method | 0.01 | ||
| Nonsurgical treatment | Reference | NA | |
| Anterior approach | -0.8 | 0.5 (0.2 to 1.0) | 0.04 |
| Posterior approach | -0.9 | 0.4 (0.2 to 0.8) | 0.006 |
| Combined approach | -0.9 | 0.4 (0.2 to 0.9) | 0.02 |
| ASIA neurologic classification | 0.07 | ||
| ASIA D | Reference | NA | |
| ASIA C | 0.3 | 1.4 (0.5 to 3.9) | 0.6 |
| ASIA B | 0.4 | 1.5 (0.5 to 4.7) | 0.4 |
| ASIA A | 1.0 | 2.8 (1.1 to 7.0) | 0.03 |
ASIA = American Spinal Injury Association.
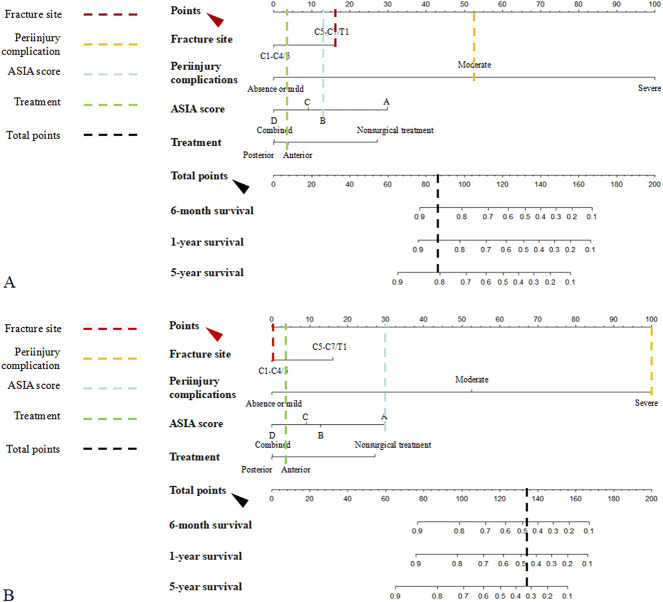
Nomogram for Clinicians
We created a nomogram that was designed to be simple enough to use in clinical practice based on findings from our multivariable model (Fig. 2). The nomogram demonstrated good accuracy in estimating the risk of death, with a Harrel C statistic of 0.91 (95% CI 0.92 to 0.89). In the bootstrap resampling, the C statistic was 0.88, suggesting the nomogram was a good model for predicting outcomes. The areas under the time-dependent ROC curve were higher than 0.88 (Fig. 3). To further assess the discrimination of the model, we plotted Kaplan-Meier curves stratified by tertiles of the probability of survival calculated from the nomograms (Fig. 4). The survival of each tertile was significantly different (log-rank, p < 0.001). The calibration plot graphically showed the nomogram resulted in good agreement regarding the risk of death (Fig. 5). Patients with the lowest predicted survival (tertile 1) had a substantially worse survival than patients in tertiles 2 and 3. The observed mean survival proportions were 57% in tertile 1, 91% in tertile 2, and 98% in tertile 3.
Fig. 2.
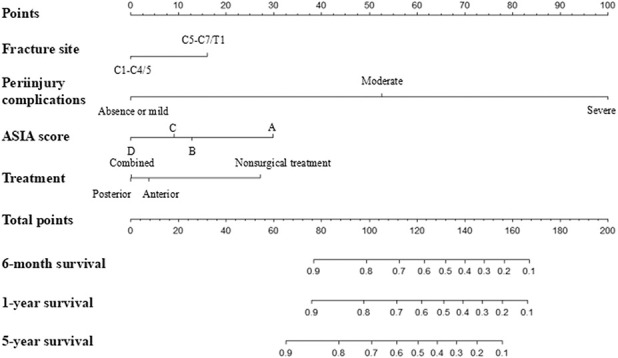
This figure shows the nomogram predicting survival in patients with ASCF-NI after treatment. To use the nomogram, find the position of each variable on the corresponding axis, draw a vertical line to the points axis for the number of points, and add the points from all the variables. Finally, draw a line from the total points axis to determine survival at the lower line of the nomogram. ASIA = American Spinal Injury Association.
Fig. 3.
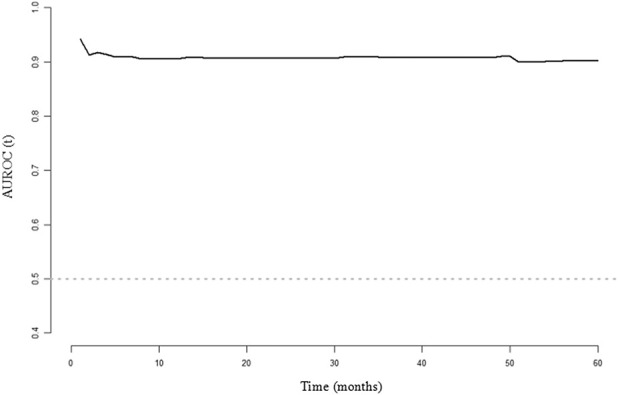
This figure shows a time-dependent ROC analysis for the proposed prognostic model. From 1 to 60 months after injury, AUROCs were higher than 0.88. This showed the nomogram had an excellent discriminatory ability. ROC = receiver operating characteristic; AUROC = area under the receiver operating characteristic curve.
Fig. 4.
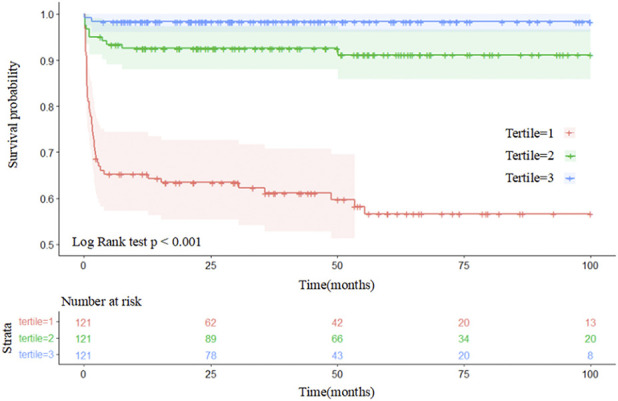
These Kaplan-Meier curves demonstrate survival in patients with ASCF-NI after treatment according to tertiles of predicted survival. Patients with the lowest predicted survival (tertile 1) had substantially poorer survival compared with patients in tertiles 2 and 3. The observed mean survival of patients were 57% in tertile 1, 91% in tertile 2, and 98% in tertile 3.
Fig. 5.
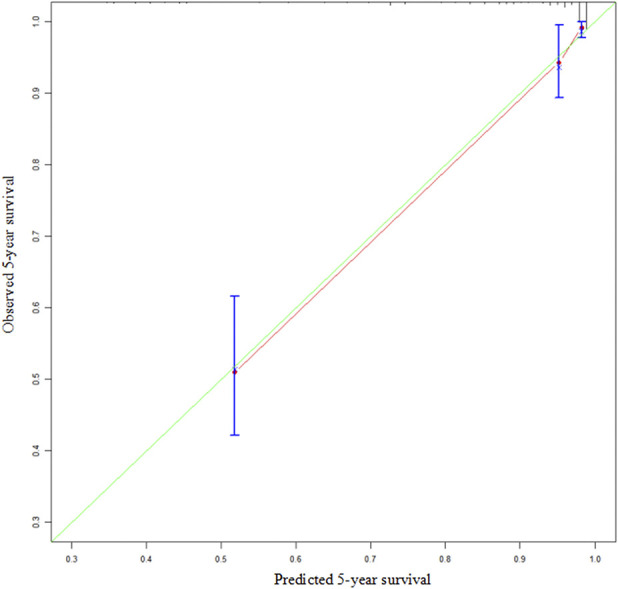
This figure is a calibration plot comparing predicted and observed survival at 5 years of follow-up. The green line represents the ideal fit, and the red line represents the agreement between the predicted and observed survival.
Nomogram Use
An example of the specific use of this nonogram is as follows: A patient with a C6 fracture who sustained an ASCF has a moderate peri-injury complication and an ASIA grade of B and is scheduled for anterior surgery. Based on these characteristics, surgeons can draw vertical lines on the corresponding nodes of each factorial axis according to the patient information. The four colored lines represent the four independent factors associated with survival. The intersection of each vertical line with the points axis represents the score for the factors (Fig. 6A). Therefore, fracture site has a score of 16, peri-injury complications has a score of 53, ASIA grade has a score of 13, and treatment has a score of 4. The patient’s total score is 16 + 53 + 13 + 4 = 86. Then, draw a vertical line at 86 on the total points axis. The intersection of this vertical line and the three survival lines represents the individual survival rate at the corresponding timepoint. Specifically, the 6-month, 1-year, and 5-year survival rates of the patient were 86%, 86%, and 80%, respectively.
Fig. 6.
(A) In this figure, the four colored lines represent the four independent factors associated with survival. To use the nomogram, the user would draw vertical lines on the corresponding points of each factorial axis according to the patient’s information. The intersection of each vertical line with the points axis (red arrow) represents the score for that factor. This patient would have 86 total points (16 points for fracture site, 53 points for periinjury complications, 13 points for ASIA score, and 4 points for treatment methods). Then, the user would draw a vertical line at 84 on the total points axis (black arrow). The intersection of this vertical line and the three survival lines represents the individual survival rate of the patient at the corresponding timepoint. The 6-month, 1-year, and 5-year survival rates of the patient were 86%, 86%, and 80%, respectively. (B) The second sample should be evaluated in the same way. The patients would have 134 total points (0 points for fracture site, 100 points for periinjury complications, 30 points for ASIA score, and 4 points for treatment methods), for predicted 6-month, 1-year, and 5-year survival rates of 48%, 46%, and 32%, respectively. ASIA = American Spinal Injury Association.
In another example, a patient with a C3 fracture, severe peri-injury complications, and an ASIA Grade A neurologic function who was treated with anterior surgery would have 134 total points (0 points for fracture site, 100 points for peri-injury complications, 30 points for ASIA score, and 4 points for treatment methods), for predicted 6-month, 1-year, and 5-year survival rates of 48%, 46%, and 32%, respectively (Fig. 6B).
Discussion
ASCF-NI is a complex and high-risk spinal injury [20]. The complexity of the disease makes it difficult to predict the survival of patients with ASCF-NI after treatment [14, 30]. Based on a multicenter, nationwide cohort comprising 363 patients with ASCF-NI, we found several key factors were independently associated with poorer survival after injury, including lower fracture site, more-severe complications, a poorer ASIA score, and the treatment selected (with patients who received nonsurgical treatment being less likely to survive than those who received surgery). We then developed and validated a clinically useful nomogram that can help surgeons anticipate a patient’s likelihood of survival after treatment for ASCF-NI.
Limitations
First, baseline comparisons were not performed at the time of patient exclusion because of missing vital records. Vital records mainly included ID number, initial consultation records, or surgical record. The absence of such data made it difficult to perform baseline comparisons. The absence of the ID number in turn made it hard to obtain the outcome variable. Therefore, we needed to exclude these patients. Although the reasons for missing data are not clearly related to model variables or outcomes, this may lead to selection bias, to some extent.
Second, the variables we used to construct the model were limited to those available in the multi-institutional database. We believed that AS severity–related variables, such as joint mobility disorders or joint swelling, should be included in the analysis. These reflect the stiffness of the spine, which is closely related to fracture severity. Including age in the multivariate analysis partially reduced model damage caused by the absence of AS severity–related variables. However, if these factors could be considered, the performance of the model would probably be more robust.
Third, the choice of treatment may have been influenced by selection bias. However, the indications we presented earlier were generally shared, and were adhered to across the participating sites. Nonetheless, accepted guidelines are still not available, and there may have been some variability among surgeons and institutions, although we do not believe there was much variability. To try to address this concern, we compared patient characteristics that reflect the severity of the condition (ASIA score and peri-injury complications) across treatment groups and found no difference (Supplemental Table 2; http://links.lww.com/CORR/B10). Therefore, it is reasonable to assume that differences in surgical indications are not likely to harm the usability of the model.
Discussion of Key Findings
Because this is the first prediction nomogram that has been developed for patients with ASCF-NI, it is difficult to corroborate these findings with those of previous work. However, our proposed nomogram demonstrated excellent discriminative ability, with a C statistic of 0.91 [16]. The tertiles’ Kaplan-Meier curves further supported the idea that the model demonstrated good discrimination (Fig. 4). In addition, to evaluate the model’s calibration, a calibration plot was drawn. The line formed by the predicted survival and the observed survival was close to the 45° diagonal line, which indicated good agreement about the presence of estimation by the nomogram and observed survival [4] (Fig. 5). Altogether, these results strongly suggest the proposed nomogram provides patient-specific information regarding the survival risk for patients with ASCF-NI. Bootstrap validation of the model revealed minimal evidence of model overfit [34] (Supplemental Table 3; http://links.lww.com/CORR/B11). In the bootstrap resampling cohort, the C statistic was 0.88, which suggests good discrimination.
We found that lower fracture site, more-severe peri-injury complications, a poorer ASIA classification, and treatment methods (namely, nonsurgical treatment and anterior approach) were independently associated with poorer survival after injury. Patients with fractures at C5 to C7 and T1 have a higher risk of death. This may be related to the anatomic properties of this site, which lies at the junction of the relatively flexible cervical vertebrae and the relatively inflexible thoracic vertebrae [39]. This site is more likely to have severe displacement and spinal cord injury after trauma. In addition, fractures at C5 to T1 in patients with AS are easily missed because of osteoporosis, kyphotic deformity, minor trauma, and overlap of the shoulders [8]. In our nomogram, peri-injury complications were identified as the factor most strongly associated with a higher risk of death. Similarly, Khuri et al. [15] reported that the occurrence of a 30-day postoperative complication was more important than preoperative patient risk and intraoperative factors in determining survival after major surgery. Therefore, peri-injury complications must be considered when assessing treatment prognosis.
Similar to previous studies [5, 18, 40], this study confirmed that patients with severe neurologic impairment have a lower survival rate than patients with less severe impairment. The risk of death of patients with ASIA Grade A was much higher that of patients with ASIA Grade D. There may be many reasons for this. For example, patients with severe spinal cord injuries are often treated with longer periods of bedrest, and so are more likely to experience complications associated with recumbency. Additionally, severe activity restriction increases patients’ psychologic stress, which will adversely affect the treatment effect and progress of rehabilitation [12].
Treatment methods also influence the survival of patients with ASCF-NI, and much research has been done to demonstrate the association of such methods with survival [7, 19]. The current mainstream opinion is that surgery is recommended [6, 18, 23]. The main reasons are as follows: a fracture in a patient with AS usually extends across all anterior and posterior elements and is extremely unstable [29], nonsurgical treatment cannot satisfactorily reduce or stabilize the cervical spine because of the stiffness of the spine and the irreducible surrounding soft tissues [13], and surgery can stabilize a vulnerable spine immediately and offer direct decompression [19]. This current study reached a similar conclusion, with the nomogram showing that patients who underwent surgery had higher survival than patients who accepted nonsurgical treatment. Patients who underwent the anterior approach were less likely to survive than those who underwent the posterior approach and combined approach. Some previous studies hold the same view [2, 3]. The authors of one of these studies believed that anterior approach stabilization alone is not adequate, because instability of the posterior column may go undetected [2]. In addition, evidence showed that the anterior approach has a higher implant failure rate [3].
The current study also showed that most of the deaths occurred very early during the follow-up period. Patients have highest risk of death within 6 months of injury (Supplemental Fig. 2; http://links.lww.com/CORR/B8). No studies reported similar phenomena until now. This may be related to peri-injury complications [36]. Although the reasons remain unclear, the results of this study are sufficient to demonstrate that patients with ASCF-NI should be given a major focus in the first 6 months after injury.
Conclusion
Using a large multicenter dataset of patients with ASCF-NI, low fracture site, more-severe peri-injury complications, poorer ASIA classification, and treatment methods (namely, nonsurgical treatment and anterior approach) were independently associated with poorer survival after injury. A nomogram was developed, which performed well on internal validation. This nomogram will allow surgeons to classify patients with different mortality risk levels into groups. This, coupled with well-defined independent factors related to survival, can be used to guide more appropriate treatment and care strategies for patients with ASCF-NI.
Acknowledgments
We thank the following hospitals for their outstanding contributions to this research: Xian Red Cross Hospital, Shang’xi; Zhengzhou Orthopedics Hospital, He’nan; Affiliated Hospital of Qingdao University, Shangdong; The Third Hospital of Hebei Medical University, Hebei; The Second Xiangya Hospital of Central South University, Hu’nan; West China Hospital Huaxi Hospital, Sichuan; The Xijing Hospital of Air Force Medical University, Shangxi; Shanghai Changzheng Hospital, Shanghai; The Second Affiliated Hospital of Wenzhou Medical University, Zhejiang; General Hospital of Shenyang Military, Liaoning; Shandong Provincial Hospital, Shangdong; General Hospital of Ningxia Medical University, Ningxia; Qilu Hospital of Shandong University, Shangdong; Daping Hospital of Third Military Medical University, Chongqing; Anhui Provincial Hospital, Anhui; Jiangsu Province Hospital, Jiangsu; The First Affiliated Hospital of Anhui Medical University, Anhui; Shanghai Changhai Hospital of Naval Military Medical University, Shanghai; The First Affiliated Hospital of Sun Yat-sen University, Guangdong; Tangdu Hospital of Air Force Medical University, Shangxi; Guangzhou Military Region General Hospital, Guangdong; Traditional Chinese Medicine Hospital of Guangdong Province, Guangdong; The Third Xiangya Hospital of Central South University, Hu’nan; General Hospital of Lanzhou Military Region, Gansu; Shanghai Ninth People's Hospital of Shanghai Jiao Tong University School of Medicine, Shanghai; Fuyang People's Hospital, Anhui; Jinan Military General Hospital, Shangdong; Langfang Edburg Hospital, Hebei; Zhengda Shaoyang Orthopedics Hospital, Hu’nan.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from the Medical Ethics Committee of the First Affiliated Hospital of the Chinese People's Liberation Army Military Medical University (ethics committee approval number: KY20212199-F-1).
This work was performed at the First Affiliated Hospital of Air Force Military Medical Univeristy, Xi'an, Shaanxi Province, PR China.
Contributor Information
Hao Bai, Email: fmmubai@126.com.
Yaobin Li, Email: 690174198@qq.com.
Xinyi Huang, Email: 1043218781@qq.com.
Quanchang Tan, Email: sci_research@126.com.
Xuexiao Ma, Email: mxxqdfy@163.com.
Qingde Wang, Email: 15093483697@163.com.
Linfeng Wang, Email: jzwlf1899@163.com.
Xiongsheng Chen, Email: cxspine@smmu.edu.cn.
Bing Wang, Email: xywb801@csu.edu.cn.
Liangbi Xiang, Email: xiangliangbi_lxb@163.com.
Hao Liu, Email: dr.liuhao6304@hotmail.com.
Xiaomin Ma, Email: maxiaomin2008@126.com.
Xinyu Liu, Email: newyuliu@163.com.
Zhensong Jiang, Email: jiangzhensong1975@163.com.
Aimin Wu, Email: aiminwu@wmu.edu.cn.
Weidong Cai, Email: caiwhspine@sina.com.
Peng Liu, Email: liupengd@163.com.
Ningfang Mao, Email: maonf@163.com.
Ming Lu, Email: tcluming1@163.com.
Yong Wan, Email: yongwan65@163.com.
Xiaofang Zang, Email: xy3zxf@yeah.net.
Songkai Li, Email: lisongkai@gmail.com.
Bo Liao, Email: liaobo@fmmu.edu.cn.
Shuai Zhao, Email: zhaoshuai1996@163.com.
Suochao Fu, Email: fusuochao@163.com.
Youzhuan Xie, Email: drxie_miss@163.com.
Haiyang Yu, Email: fy.yhy@163.com.
Ruoxian Song, Email: ruoxiansong@sina.com.
Zhensheng Ma, Email: mazhensheng@yahoo.com.
Ming Yan, Email: spineyanming@163.com.
Jianjun Chu, Email: 8017050@zju.edu.cn.
Jiangbo Sun, Email: 2242342752@qq.com.
Xiang Liu, Email: zggklx2013@163.com.
Yafei Feng, Email: fengyafei2005@163.com.
Yuan Dong, Email: bainana_dy@163.com.
Dingjun Hao, Email: honghuispine@163.com.
Wei Lei, Email: leiwei@fmmu.edu.cn.
References
- 1.Bae J, Theologis AA, Jang J-S, Lee S-H, Deviren V. Impact of fatigue on maintenance of upright posture: dynamic assessment of sagittal spinal deformity parameters after walking 10 minutes. Spine (Phila Pa 1976). 2017;42:733-739. [DOI] [PubMed] [Google Scholar]
- 2.Cornefjord M, Alemany M, Olerud C. Posterior fixation of subaxial cervical spine fractures in patients with ankylosing spondylitis. Eur Spine J. 2005;14:401-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Einsiedel T, Schmelz A, Arand M, et al. Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine. 2006;5:33-45. [DOI] [PubMed] [Google Scholar]
- 4.Fenlon C, O'Grady L, Doherty ML, Dunnion J. A discussion of calibration techniques for evaluating binary and categorical predictive models. Prev Vet Med. 2018;149:107-114. [DOI] [PubMed] [Google Scholar]
- 5.Gao Q, Zhang Z, Shao T, et al. Predictor of surgical outcomes in ankylosing spondylitis cervical spinal fracture: an at least 2 years follow-up retrospective study. Spine (Phila Pa 1976). 2021;46:E31-E36. [DOI] [PubMed] [Google Scholar]
- 6.Gilard V, Curey S, Derrey S, Perez A, Proust F. Cervical spine fractures in patients with ankylosing spondylitis: importance of early management. Neurochirurgie. 2014;60:239-243. [DOI] [PubMed] [Google Scholar]
- 7.Govindarajan V, Bryant J-P, Perez-Roman RJ, Wang MY. The role of an anterior approach in the treatment of ankylosing spondylitis-associated cervical fractures: a systematic review and meta-analysis. Neurosurg Focus. 2021;51:E9. [DOI] [PubMed] [Google Scholar]
- 8.Guo Q, Cui Y, Wang L, Lu X, Ni B. Single anterior approach for cervical spine fractures at C5-T1 complicating ankylosing spondylitis. Clin Neurol Neurosurg. 2016;147:1-5. [DOI] [PubMed] [Google Scholar]
- 9.Harrell FE, Jr, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982;247:2543-2546. [PubMed] [Google Scholar]
- 10.Harris MB, Sethi RK. The initial assessment and management of the multiple-trauma patient with an associated spine injury. Spine (Phila Pa 1976). 2006;31:S9-S15. [DOI] [PubMed] [Google Scholar]
- 11.Inglis T, Banaszek D, Rivers CS, et al. In-hospital mortality for the elderly with acute traumatic spinal cord injury. J Neurotrauma. 2020;37:2332-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacoby SF, Shults J, Richmond TS. The effect of early psychological symptom severity on long-term functional recovery: a secondary analysis of data from a cohort study of minor injury patients. Int J Nurs Stud. 2017;65:54-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jo D-J, Kim S-M, Kim K-T, Seo E-M. Surgical experience of neglected lower cervical spine fracture in patient with ankylosing spondylitis. J Korean Neurosurg Soc. 2010;48:66-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanter AS, Wang MY, Mummaneni PV. A treatment algorithm for the management of cervical spine fractures and deformity in patients with ankylosing spondylitis. Neurosurg Focus. 2008;24:E11. [DOI] [PubMed] [Google Scholar]
- 15.Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y, Margonis GA, Prescott JD, et al. Nomograms to predict recurrence-free and overall survival after curative resection of adrenocortical carcinoma. JAMA Surg. 2016;151:365-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kouyoumdjian P, Guerin P, Schaelderle C, Asencio G, Gille O. Fracture of the lower cervical spine in patients with ankylosing spondylitis: retrospective study of 19 cases. Traumatol Surg Res. 2012;98:543-551. [DOI] [PubMed] [Google Scholar]
- 18.Lazennec JY, d'Astorg H, Rousseau MA. Cervical spine surgery in ankylosing spondylitis: review and current concept. Traumatol Surg Res. 2015;101:507-513. [DOI] [PubMed] [Google Scholar]
- 19.Longo UG, Loppini M, Petrillo S, Berton A, Maffulli N, Denaro V. Management of cervical fractures in ankylosing spondylitis: anterior, posterior or combined approach? Br Med Bull. 2015;115:57-66. [DOI] [PubMed] [Google Scholar]
- 20.Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal fracture in patients with ankylosing spondylitis: cohort definition, distribution of injuries, and hospital outcomes. Spine (Phila Pa 1976). 2016;41:191-196. [DOI] [PubMed] [Google Scholar]
- 21.Ma J, Wang C, Zhou X, Zhou S, Jia L. Surgical therapy of cervical spine fracture in patients with ankylosing spondylitis. Medicine. 2015;94:e1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinez-Laguna D, Nogues X, Abrahamsen B, et al. Excess of all-cause mortality after a fracture in type 2 diabetic patients: a population-based cohort study. Osteoporos Int. 2017;28:2573-2581. [DOI] [PubMed] [Google Scholar]
- 23.Mathews M, Bolesta MJ. Treatment of spinal fractures in ankylosing spondylitis. Orthopedics. 2013;36:e1203-1208. [DOI] [PubMed] [Google Scholar]
- 24.Oitment C, Thornley P, Jentzsch T, Pahuta M. Damage control orthopaedics in spinal trauma. J Am Acad Orthop Surg. 2021;29:e1291-e1302. [DOI] [PubMed] [Google Scholar]
- 25.Renninger CH, Cochran G, Tompane T, Bellamy J, Kuhn K. Injury characteristics of low-energy Lisfranc injuries compared with high-energy injuries. Foot Ankle Int. 2017;38:964-969. [DOI] [PubMed] [Google Scholar]
- 26.Riley RD, Snell KI, Ensor J, et al. Minimum sample size for developing a multivariable prediction model: PART II - binary and time-to-event outcomes. Stat Med. 2019;38:1276-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robinson Y, Sandén B, Olerud C. Increased occurrence of spinal fractures related to ankylosing spondylitis: a prospective 22-year cohort study in 17,764 patients from a national registry in Sweden. Patient Saf Surg. 2013;7:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rustagi T, Drazin D, Oner C, et al. Fractures in spinal ankylosing disorders: a narrative review of disease and injury types, treatment techniques, and outcomes. J Orthop Trauma. 2017;31:S57-S74. [DOI] [PubMed] [Google Scholar]
- 29.Sapkas G, Kateros K, Papadakis SA, et al. Surgical outcome after spinal fractures in patients with ankylosing spondylitis. BMC Musculoskelet Disord. 2009;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoenfeld AJ, Harris MB, McGuire KJ, Warholic N, Wood KB, Bono CM. Mortality in elderly patients with hyperostotic disease of the cervical spine after fracture: an age- and sex-matched study. Spine J. 2011;11:257-264. [DOI] [PubMed] [Google Scholar]
- 31.Schwendner M, Seule M, Meyer B, Krieg SM. Management of spine fractures in ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis: a challenge. Neurosurg Focus. 2021;51:E2. [DOI] [PubMed] [Google Scholar]
- 32.Shen FH, Samartzis D. Successful nonoperative treatment of a three-column thoracic fracture in a patient with ankylosing spondylitis: existence and clinical significance of the fourth column of the spine. Spine (Phila Pa 1976). 2007;32:E423-427. [DOI] [PubMed] [Google Scholar]
- 33.Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet. 2017;390:73-84. [DOI] [PubMed] [Google Scholar]
- 34.Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35:1925-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teunissen FR, Verbeek BM, Cha TD, Schwab JH. Spinal cord injury after traumatic spine fracture in patients with ankylosing spinal disorders. J Neurosurg Spine. 2017;27:709-716. [DOI] [PubMed] [Google Scholar]
- 36.Weinberg L, Ou Yang B, Cosic L, et al. Factors influencing early and long-term survival following hip fracture among nonagenarians. J Orthop Surg Res. 2021;16:653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Werner BC, Samartzis D, Shen FH. Spinal fractures in patients with ankylosing spondylitis: etiology, diagnosis, and management. J Am Acad Orthop Surg. 2016;24:241-249. [DOI] [PubMed] [Google Scholar]
- 38.Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18:145-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whang PG, Goldberg G, Lawrence JP, et al. The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. J Spinal Disord Tech. 2009;22:77-85. [DOI] [PubMed] [Google Scholar]
- 40.Wysham KD, Murray SG, Hills N, Yelin E, Gensler LS. Cervical spinal fracture and other diagnoses associated with mortality in hospitalized ankylosing spondylitis patients. Arthritis Care Res (Hoboken). 2017;69:271-277. [DOI] [PMC free article] [PubMed] [Google Scholar]