1. Introduction
Challenges of receiving follow-up care with healthcare providers (HCP) existed before the onset of the COVID-19 pandemic due to time constraints, appointments during working hours, commuting distances, patient physical limitations, costs, and transportation. Telemedicine was initiated before this pandemic to serve patients with chronic illnesses facing constraints that influence healthcare follow-up. [[1], [2], [3]] Telemedicine delivers health and health-related services via telecommunications and digital communication technologies. Telemedicine technologies commonly used are live video conferencing, mobile health apps, “store and forward” electronic transmission, and remote patient monitoring. [4]
Caring for older adults with cancer is often complicated [5] and has become more so with the onset of COVID-19. [1] In May 2022, there were 522 million confirmed cases and over six million deaths globally due to COVID-19 [6]. Older adults with cancer who acquire COVID-19 have a higher risk of death from the disease. [7] This has generated a challenge for safe healthcare delivery among older adults, who historically have been a marginalized group. [8,9] Since the start of the pandemic crisis, telemedicine has been used as an essential tool to meet the needs and challenges of safely delivering health care services remotely, at lower non-medical costs, with the hope of equivalent quality as in-person visits. [10,11] However, the experiences of providers caring for older adults with cancer using telemedicine are unknown. Here, we present the results from two survey-based studies, spring of 2020 and summer of 2021 conducted, to explore this gap.
2. Methods
In April 2020, members of the Advocacy Committee of the Cancer and Aging Research Group (CARG) and the Association of Community Cancer Centers (ACCC) developed a Qualtrics survey to gather data from direct care providers focused on caring for older adults with cancer during the COVID-19 pandemic. In the summer of 2021, a similar survey was launched by the same research team. The 2020 survey contained 20-items, including three open-ended questions, and the 2021 survey contained 25 items, four of which were open-ended questions. Qualitative and quantitative data from both surveys have already been published [[11], [12], [13], [14], [15]]. The current paper reports findings related to telemedicine from both surveys.
Questions specific to telemedicine (video only) on both surveys covered perceived barriers to the use of telemedicine in older adults with cancer. In the most recent survey, additional items were added, focusing on benefits associated with telemedicine use, changes in volume from before to during the pandemic, and the availability of guidelines to select patients for telemedicine vs. face-to-face appointments. Information about the provider's professional history (years in providing care to patients with cancer, percentage of older patients, medical profession/specialty, cancer program classification, setting, and state, if in the US, or country of residence, if outside the US) was collected.
Potential participants were recruited by emails sent through professional organizations' listservs and email blasts (CARG, ACCC, Association of Oncology Social Work, Social Work Hospice and Palliative Care Network, International Society of Geriatric Oncology, European Cancer Organisation, Advanced Practitioner Society for Hematology and Oncology, Academy of Oncology Nurse & Patient Navigators, Geriatric Society of America, American College of Rehab Medicine, American Physical Therapy Association, and Los Angeles Oncology Nursing Society Chapter) as well as social media messaging (e.g., Facebook, Twitter). Individuals were eligible to participate if they: (1) provided care for people with cancer, (2) participated in the study voluntarily, and (3) understood that the results might be reported in multiple publications.
The online survey for 2020 was available from April 10 to May 1, 2020, and the 2021 online survey was open from June 15 to September 2, 2021. The University of Cincinnati Institutional Review Board (IRB) approved both studies, and the University of Louisville IRB also approved the 2021 survey. The data were analyzed using descriptive statistics (frequencies, percentages) and chi-squares with IBM SPSS Statistics version 28.0.
3. Results
3.1. Participant Characteristics Spring 2020
Of the 495 online surveys that were opened, 274 (55.4%) respondents s met the eligibility criteria and completed the initial survey. Most respondents were social workers (42.7%), followed by physicians (24.6%), oncology nurses/navigators (8.8%), and advance practice providers (APPs; 4.0%). Just over 68% of the respondents reported that over 50% of their patients were aged over 65. The distribution by years of post-training practice was evenly split between 1 to over 20 years. The groups ranged from one to four years (20.5%) to over 20 years (28.9%). The vast majority were based in the US (92%). Thirty six percent reported working in a National Cancer Institute (NCI) affiliated academic setting, followed by 29% who practiced in community cancer programs. (Table 1 ).
Table 1.
Participant demographics.
| 2020 |
2021 |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Profession | ||||
| Physician | 67 | 24.6 | 40 | 35.7 |
| Advanced Practice Provider | 11 | 4.0 | 14 | 12.5 |
| Social Work | 117 | 42.7 | 33 | 29.5 |
| Oncology nurse/navigator | 24 | 8.8 | 12 | 10.7 |
| Administrator | 21 | 7.7 | – | – |
| Mixed | 17 | 6.3 | 5 | 4.5 |
| Othera | 11 | 5.5 | 8 | 7.1 |
| Type of Program | ||||
| Comprehensive Cancer Program, Tertiary Referral Center, Specialist Care Center | 100 | 36.8 | 64 | 58.2 |
| Community Cancer Program | 83 | 30.5 | 29 | 26.4 |
| Hospital | 49 | 18.0 | 5 | 4.5 |
| Integrated | 19 | 7.0 | – | – |
| Physician-Owned Oncology Practice | 12 | 4.4 | 3 | 2.7 |
| Other | 9 | 3.3 | 9 | 8.2 |
| Percent of patients over 65 years of age | ||||
| Less than or equal to 10% | 2 | 0.7 | 2 | 1.5 |
| 11 to 25% | 12 | 4.4 | 8 | 6.0 |
| 26 to 50% | 72 | 26.4 | 27 | 20.1 |
| 51 to 75% | 156 | 57.1 | 72 | 53.7 |
| Over 75% | 31 | 11.4 | 25 | 18.7 |
| Years in Practice | ||||
| 1 to 4 | 56 | 20.5 | 25 | 22.7 |
| 5 to 10 | 66 | 24.2 | 32 | 29.1 |
| 11 to 20 | 79 | 28.9 | 26 | 23.6 |
| Over 20 | 73 | 26.4 | 27 | 24.5 |
| Country | ||||
| USA | 253 | 92.3 | 89 | 65.0 |
| International | 20 | 7.3 | 18 | 13.1 |
administration, physical therapist, dietitian, pharmacist, pulmonologist, medical assistant, case manager.
3.2. Participant Characteristics Summer 2021
Two hundred and thirty-five respondents started the survey, with 137 (58.3%) meeting the inclusion criteria and completing the survey. Most respondents were physicians (35.7%), followed by social workers (29.5%), APPs (12.5%), and oncology nurses/navigators (10.7%). The majority were affiliated with NCI-affiliated academic settings (58.2%), followed by community cancer programs (26.4%). Seventy-two percent of the respondents reported that over 50% of their patients were over 65. The length of professional practice (post-training years) working with individuals with cancer was evenly distributed between 1 and over 20 years, with groups ranging from one to four years (22.7%) to over 20 years (24.5%). Most respondents (65%) were based in the US. (Table 1).
3.3. Telemedicine Use
Almost 29% of study participants reported using telemedicine to meet with patients before COVID. This rose to 80.6% during COVID. Of those who reported using telemedicine during COVID, 18.4% had a lower volume than before COVID, with 32.7% reporting the volume was the same, 22.4% reporting a slightly higher volume, and 26.5% reporting a significant increase in volume. Only 33.1% reported having institutional guidelines for when to use telemedicine with a patient; 41.8% reported having no such guidelines and 24.6% reported not knowing if there were guidelines.
The most commonly reported benefits of telemedicine use were less need for transportation (82.5%), patient safety (79.6%), availability of caregivers to attend appointments (68.6%), and healthcare worker safety (67.2%). The remaining benefits were the ease of scheduling (46.0%), healthcare provider convenience (39.4%), and increased patient confidence in using telemedicine (29.2%).
Chi-square tests were used to explore differences in identified benefits by percent of patients over 65 (50% or fewer vs. over 50%), years in practice (1–10 years vs. over 10 years), and type of program (comprehensive vs. other). There was no significant finding by percent of patients over 65 or by years of practice. There were associations found with more benefits identified by those who work at comprehensive cancer settings as compared to other types of programs for benefits related to patient safety (χ2 = 9.040, p < .01), patient transportation (χ2 = 7.830, p < .01), caregiver ability to attend virtual appointments (χ2 = 16.739, p < .001), and ease of scheduling (χ2 = 8.669, p < .01).
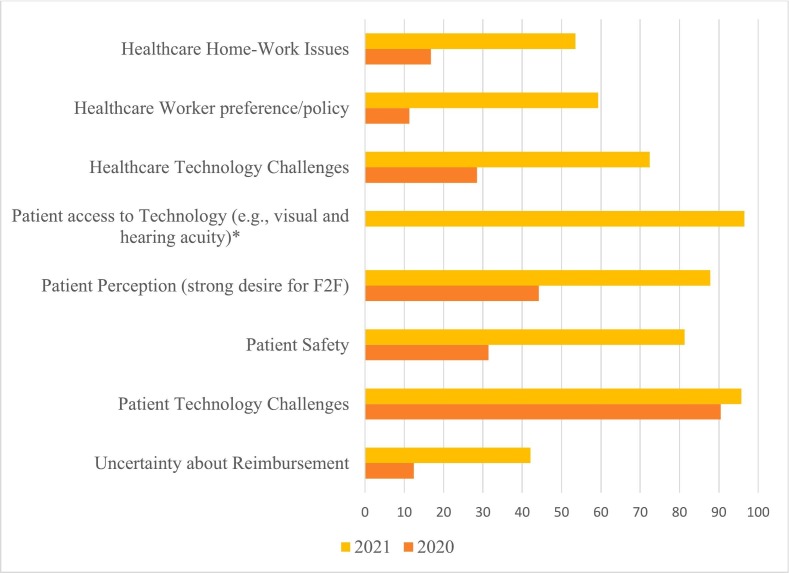
The 2020 survey's top reported barriers to telemedicine use were patient access to needed technology, patient technology challenges, patients' strong desire for face-to-face appointments, institutional infrastructure, healthcare worker technology challenges, and patient safety. The top barriers reported in the 2021 survey were accessibility issues (e.g., visual and auditory acuity) for patients, patient technology challenges, patient access to the needed technology, patients' strong desire for face-to-face appointments, patient safety, healthcare worker technology challenges, healthcare worker preference/policy, healthcare worker home-work issues, and uncertainty about reimbursement (Fig. 1 ). In the 2020 survey, 1.8% of respondents endorsed no barriers; this increased to 26.1% in the 2021 survey.
Fig. 1.
Barriers to Telemedicine in 2020 and 2021.
*Only asked in 2021; F2F = face-to-face.
Chi-square analysis was used to explore differences in identified barriers by percent of patients aged over 65 (50% or fewer vs. over 50%), years of practice (1–10 years vs. over 10), and type of program (NCI-affiliated vs. other). There were no associations in the barriers by years in practice or type of program. There were statistically significant associations related to barriers to patient access to needed technology in both 2020 and 2021. Those respondents with over 50% of their patients aged over 65 reported patient access to necessary technology as a barrier more often than those with 50% or fewer patients over 65 in both surveys (2020, χ2 = 6.264, p < .05: 2021, χ2 = 7.085, p < .01). In 2021 more barriers were identified related to visual and hearing acuity (not asked in 2020) among those with over 50% of patients aged over 65 (χ2 = 7.085, p < .05).
4. Discussion
Our study focuses on the evolution in telemedicine (with video only) related to the COVID pandemic at two points in time, and how telemedicine experiences changed from the beginning of the pandemic to more than one and a half years into the pandemic. Most literature on telemedicine use in older adults with cancer focuses on the patient, family caregiver, and HCP level of satisfaction since the onset of COVID. [16,17] Our study is unique because it explored benefits and barriers to telemedicine from HCPs who were using this modality with people diagnosed with cancer. Further, by examining HCP perceived use, benefits, barriers, and changes to telehealth over time, this study helps to clarify what next steps are needed and the ways to support and improve telehealth use for both providers and their patients.
Differences in the identification of benefits of using telehealth with older adults with cancer were found by HCPs more often by those who worked at comprehensive cancer centers (i.e., NCI designated, tertiary referral, and specialist cancer centers) as compared to those who worked in other cancer care settings. Differences were found between those HCP who reported more than 50% of their patients being aged over 65 as compared to those having 50% or fewer patients aged over 65 related to patients having access to necessary technology or visual and hearing acuity. Neither of these findings have been reported previously.
Arem et al. [17] explored experiences of HCPs and adult patients using telemedicine during COVID-19 in a cross-sectional study. They similarly reported technology challenges faced by HCPs and patients. In their study, HCPs and patients reported reimbursement and access issues. These were captured in our second survey but not the first. Similar to our study, Arem et al. found that the benefits of telemedicine included both patient and HCP safety and having family caregivers present during the appointments. A concern for both providers and patients was that the provider would “miss something,” which validated patient safety as a top challenge for HCPs during COVID in our study. [17] Limitations of our studies include the small sample size, most of the respondents being from the USA, respondents possibly being different between survey years, and a potential selection bias which limits generalizability of findings to all providers' experiences.
In conclusion, the COVID-19 pandemic provided a unique opportunity for millions of patients, caregivers, and HCPs to experience telemedicine. Our study showed that HCPs acknowledge both benefits of having telemedicine as a method of healthcare delivery and barriers to telemedicine-based patient care. Future studies need to address these multifaceted barriers, such as no access to proper internet connectivity, difficulty using technology because of aging-related issues, and infrequent institutional guidelines on the proper context of delivering care via telemedicine. Furthermore, the equivalency of in-person and telemedicine visits should be tested. Only by effectively addressing barriers toward telemedicine can this platform remain a vital part of the healthcare system for older adults with cancer.
Author Contributions
Study concepts: AS, JLKS, LCC, MP, BC, NMLB, JLKS, KB, EP, LMB.
Study design: AS, KB, JLKS, EP, LMB.
Data acquisition: EP, LMB.
Quality control of data and algorithms: KB.
Data analysis and interpretation: KB, MAVM, JLKS, LCC, MP, AK.
Statistical analysis: KB.
Manuscript preparation: MAVM, KB,
Manuscript editing: All authors.
Manuscript review: All authors.
Declaration of Competing Interest
NMLB and LMB reported relevant activities outside the submitted work: NMLB has served on advisory boards for Pfizer, Abbot, and Sanofi; received travel grants from Exact Sciences, Pfizer, and Lilly; and received speaker fees from Pfizer and AbbVie. LMB has served as a consultant for Pfizer, AstraZeneca, EMD Serono, and Merck.
References
- 1.Turner-Lee N., Karsten J., Roberts J. Bookings Institution; Jhon Locke Foundation May: 2020. Removing regulatory barriers to telehealth before and after COVID-19. [Google Scholar]
- 2.Kaiser Permanente Why telehealth - Benefits & Barriers to adoption. 2020. https://business.kaiserpermanente.org/insights/telehealth/why-benefits-barriers Accessed April 27, 2020.
- 3.Vahia I.V., Jeste D.V., Reynolds C.F. Older adults and the mental health effects of COVID-19. JAMA. 2020;324(22):2253–2254. doi: 10.1001/jama.2020.217535. NEJM Catalyst, Massachusetts Medical Society. What is Telehealth? February 1, 2018. [DOI] [PubMed] [Google Scholar]
- 4.NEJM Catalyst . February 1, 2018. Massachusetts medical society. What is Telehealth? [Google Scholar]
- 5.Shahrokni A., Kim S.J., Bosl G.J., Korc-Grodzicki B. How we Care for an Older Patient with Cancer. J Oncol Pract. 2017;13(2):95–102. doi: 10.1200/JOP.2016.017608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization Weekly epidemiological update on COVID-19: Overview, 15 May 2022. 2022. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---25-may-2022 Retrieved 2/24/2023 from.
- 7.Sharafeldin N., Bates B., Song Q., et al. Outcomes of COVID-19 in patients with cancer: report from the national COVID cohort collaborative (N3C) J Clin Oncol. July 10, 2021;39(20):2232–2246. doi: 10.1200/JCO.21.01074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farrell T.W., Francis L., Brown T., Ferrante L.E., et al. Rationing limited healthcare resources in the COVID-19 era and beyond: ethical considerations regarding older adults. J Am Geriatr Soc. June 2020;68(6):1143–1149. doi: 10.1111/jgs.16539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaynor T.S., Wilson M.E. Social Vulnerability and Equity: The Disproportionate Impact of COVID-19. Public Adm Rev. 2020 Jun 22 doi: 10.1111/puar.13264. Epub ahead of print. PMID: 32836465; PMCID: PMC7361760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sirintrapun S.J., Lopez A.M. American Society of Clinical Oncology Educational Book; 2018. Telemedicine in cancer care; pp. 540–545. [DOI] [PubMed] [Google Scholar]
- 11.Wehrle C.J., Lee S.W., Devarakonda A.K., Arora T.K. Patient and physician attitudes toward telemedicine in Cancer clinics following the COVID-19 pandemic. JCO Clin Cancer Inform. 2021 Apr;5:394–400. doi: 10.1200/CCI.20.00183. [PMID: 33822651] [DOI] [PubMed] [Google Scholar]
- 12.BrintzenhofeSzoc K., Krok-Schoen J.I., Pisegna J.L., et al. Survey of cancer care providers’ attitude toward care for older adults with cancer during the COVID-19 pandemic. J Geriat Oncol. March 2021;12(2):196–205. doi: 10.1016/j.jgo.2020.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krok-Schoen J.L., Pisegna J.L., BrintzenhofeSzoc K., MacKenzie A.R., Canin B., Plotkin E., et al. Experiences of healthcare providers of older adults with cancer during the COVID-19 pandemic. J Geriatr Oncol. 2021 Mar;12(2):190–195. doi: 10.1016/j.jgo.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pisegna J.L., BrintzenhofeSzoc K., Shahrokni A., Canin B., Plotkin E., Boehmer L.M., et al. Differences in urban and suburban/rural settings regarding care provision and barriers of cancer care for older adults during COVID-19. Support Care Cancer. 2023;31(1):1–9. doi: 10.1007/s00520-022-07544-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pergolotti M, Pisegna J, Cabrera Chien L, BrintzenhofeSzoc K, Kaur A, Battisti N, et al. (under review) healthcare providers’ experiences of continuing care for older adults with cancer during the COVID-19 pandemic. J Cancer Surviv. [DOI] [PMC free article] [PubMed]
- 16.Andrews E., Berghofer K., Long J., et al. Satisfaction with the use of telehealth during COVID-19: an integrative review. Intern J Nurs Stud Adv. November 2020;2 doi: 10.1016/j.ijnsa.2020.100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arem H., Moses J., Cisneros C., Blondeau B., Nekhlyudov L., Killackey M., et al. Cancer provider and survivor experiences with telehealth during the COVID-19 pandemic. JCO Oncol Pract. 2022;18(4):e452–e461. doi: 10.1200/OP.21.00401. [DOI] [PubMed] [Google Scholar]