To the Editor: In March 2020, New York City (NYC) experienced a surge of coronavirus infections, becoming the epicenter of the global pandemic. Low-income, communities of color were the hardest hit, with morbidity and mortality far outweighing that of more affluent white areas.1 Our dermatology departments operate out of 2 safety net hospitals in Brooklyn and Manhattan serving racially diverse neighborhoods that experienced some of the highest death rates in NYC.2 Beginning in July, we began to notice an abrupt uptick in cases of hair shedding in our clinics. The timeframe, approximately 3 to 4 months after the shelter in place directive in NYC, correlates with the expected onset of telogen effluvium (TE).
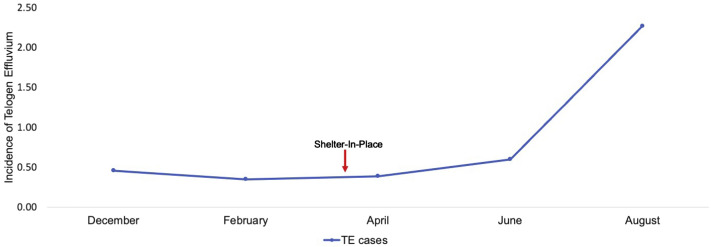
To quantify the incidence of TE, a retrospective analysis was performed whereby all patients diagnosed with the condition were extracted from among the total patients evaluated by dermatology (SlicerDicer; EPIC, Verona, WI). Between November 1, 2019 and February 29, 2020, an average of 7.5 cases of TE were identified every 2 months—an incidence of 0.4% (Fig 1 ). This rate remained stable through June 2020 with an incidence of 0.5%. However, in July and August, 43 patients with TE were identified, corresponding to an incidence of 2.3%—a >400% increase in incidence (Fig 1). The entirety of this increase was caused by the presence of this condition in persons of color, most notably Hispanic/Latinx, in line with the disproportionately high mortality rate of this subset of the population caused by COVID-19 in NYC.3
Fig 1.
Incidence of telogen effluvium from two safety-net hospitals in New York City, before and during the COVID-19 pandemic (November 1, 2019 to August 31st 2020). Bimonthly averages are presented. New York State's shelter-in-place directive is highlighted with an arrow, March 20, 2020.
Despite the considerable rise in cases of TE in other nonwhite populations, no substantial increase in this disorder was noted in Blacks/African Americans, a demographic also severely affected by COVID-19 (Table I ). As reflected in the prepandemic numbers, Blacks/African Americans were overall less likely to be diagnosed with TE compared with other groups. Further research is needed to explore this discrepancy. Of note, in the year before the arrival of COVID-19 we had not recorded a single case of TE in a man. However, during the pandemic, 5 cases were identified in men in our clinics.
Table I.
Telogen effluvium cases and patient demographics prepandemic and during the pandemic∗
| Prepandemic (September 1, 2019-February 29, 2020) | During the pandemic (March 1, 2020-August 31, 2020) | P value | |
|---|---|---|---|
| Total TE cases | 18 | 50 | |
| Total patients seen by dermatology | 3761 | 3006 | |
| Incidence of TE | 0.5 | 1.7 | <.001 |
| Demographics of TE cases, n (%) | |||
| White | 5 (27.8) | 5 (10) | .72 |
| Hispanic/Latinx | 12 (66.7) | 32 (64) | <.001 |
| Black/African American | 0 (0) | 1 (2) | — |
| Other | 1 (5.5) | 12 (24) | <.001 |
| Gender of TE cases, n (%) | |||
| Female | 18 (100) | 45 (90) | <.001 |
| Male | 0 (0) | 5 (10) | — |
| Age of TE cases, n (%) | |||
| ≤30 | 4 (22.2) | 9 (18) | .72 |
| 31-60 | 12 (66.7) | 34 (68) | <.001 |
| ≥61 | 2 (11.1) | 7 (14) | .93 |
| Average monthly patients ± SD | 1066.2 ± 106.4 | 814.5 ± 154.8 | |
| Demographics (all patients seen by dermatology), % ± SD | |||
| White | 5.0 ± 0.4 | 10.9 ± 0.7 | <.001 |
| Hispanic/Latinx | 50.8 ± 1.3 | 47.6 ± 1.8 | .43 |
| Black/African American | 12.9 ± 1.3 | 14.4 ± 0.6 | .61 |
| Other | 31.3 ± 0.9 | 27.1 ± 1.6 | .15 |
| Gender (all patients seen by dermatology), % ± SD | |||
| Female | 58.8 ± 1.2 | 60.1 ± 2.3 | .66 |
| Male | 41.2 ± 1.2 | 39.9 ± 2.3 | .76 |
SD, Standard deviation; TE, telogen effluvium.
Locations include Metropolitan Hospital, New York, and Coney Island Hospital, Brooklyn, New York.
The etiology of TE is multifactorial. As such, it is unclear if the surge in cases is more closely related to stress associated with the pandemic or the physiological toll of infection. Due to a shortage of reagents at the time, only 2 patients had been tested for COVID-19 (both negative). Importantly, hair loss is one of the most reported complaints of people with persistent symptoms after infection with COVID-19.4 Thus, the possibility exists that some degree of underlying inflammation may be a factor in a subset of patients.5 To that end, it is advisable to assess for systemic symptoms and monitor for resolution. The management of TE consists primarily of removal or treatment of the underlying cause and reassurance.
Limitations of this study include the possibility of coding errors and potential for bias because of public knowledge of the association of hair loss with COVID-19. Nonetheless, dermatologists may well see an influx of TE in communities significantly impacted by COVID-19.
Conflicts of interest
None disclosed.
Footnotes
Drs Cline and Kazemi contributed equally to this work.
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.New York City Department of Health website COVID-19: data. Latest data. https://www1.nyc.gov/site/doh/covid/covid-19-data.page Available at:
- 2.Brooklyn ZIP code has NYC's highest death rate. The New York Times. https://www.nytimes.com/2020/05/18/nyregion/coronavirus-new-york-update.html#:∼:text=Brooklyn%20area%20has%20N.Y.C.'s%20highest%20death%20rate%20by%20ZIP%20code.,-The%20Brooklyn%20ZIP&text=10469%2C%20the%20East%20Bronx%3A%20307,deaths%20(one%20in%20240) Available at:
- 3.Dwyer C. New York City's Latinx residents hit hardest by coronavirus deaths. NPR. https://www.npr.org/2020/04/08/829726964/new-york-citys-latinx-residents-hit-hardest-by-coronavirus-deaths Available at:
- 4.Lambert N.J., Survivor Corps . Indiana University School of Medicine; 2020. COVID-19 “long hauler” symptoms survey report. [Google Scholar]
- 5.Puntmann V.O., Carerj M.L., Wieters I., et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]