Abstract
Microsurgery is technically challenging, typically requiring a primary surgeon and an assistant to complete several key operative steps. These may include manipulation of fine structures, such as nerves or vessels in preparation for anastomosis; stabilization of the structures; and needle driving. Even seemingly mundane tasks of suture cutting and knot tying require fine coordination between the primary surgeon and assistant in the microsurgical environment. Although prior literature discusses the implementation of microsurgical training centers at academic institutions and residency programs, there is a paucity of work describing the role of the assistant surgeon in a microsurgery operation. In this surgical technique article, the authors discuss the role of the assisting surgeon in microsurgery, with recommendations for trainees and attendings alike.
Key words: Assistant, Assisting in surgery, Hand surgery, Microsurgery, Plastic surgery, Reconstructive surgery
The first microsurgical procedure was performed by Carl Olof Nylén, a Swedish otorhinolaryngologist, who also developed the first surgical microscope.1 In the subsequent century, microsurgical techniques became mainstay practice for several surgical specialties, including plastic surgery, orthopedic surgery, and otolaryngology. Microsurgery requires the use of an operating microscope (or surgical loupes) and microsurgical instruments to anastomose vessels and coapt nerves often smaller than a few millimeters in diameter. It is a technically challenging surgical discipline, often requiring years of training to develop proficiency.2 Within hand surgery, microsurgical techniques enable the anastomosis of vessels and coaptation of nerves for complex reconstructions and free tissue transfers.
Assistant surgeons can aid with several key steps, including manipulation of fine structures, such as nerves or vessels, in preparation for anastomosis; stabilization of the structures; and needle driving, thereby increasing surgical efficiency and reducing operative time. Seemingly mundane tasks of suture cutting and knot tying require coordination between the primary surgeon and assistant in the microsurgical environment. Often, trainees are expected to fulfill the assistant position in a microsurgical setting before extensive exposure to microsurgery, to the detriment of the trainee’ experience.
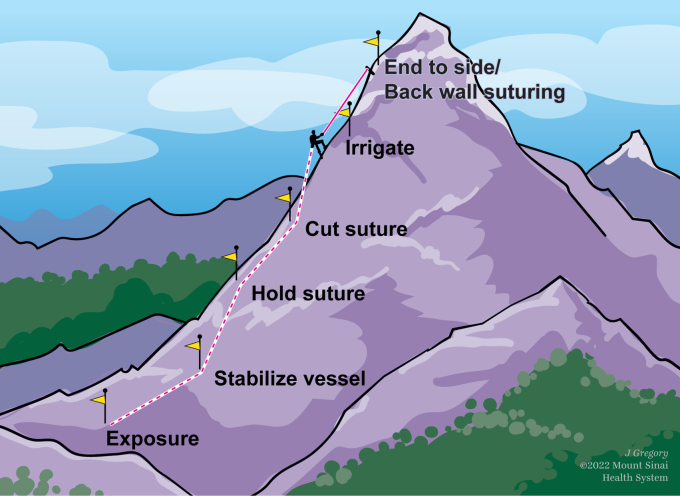
Most published literature on microsurgical education focuses on the skill set of the primary surgeon or the development of microsurgical curricula; however, less has been discussed regarding the optimal role of the assistant surgeon, which can be critical for successful surgical and clinical outcomes (Fig. 1).3, 4, 5 In this article, the authors aim to describe the role of a proficient assistant surgeon in microsurgical procedures and provide an overview for trainees with limited microsurgical exposure and the senior educators training these surgeons. Although the techniques described are used at the authors’ medical center, the reader should consider variability between individual surgeons and institutions.
Figure 1.
A number of key steps are critical for the microsurgeon and microsurgical assistant for successful surgical outcomes.
Equipment
The microsurgical assistant should be familiar and facile with the components of the operating microscope and various microsurgical instruments. The operating microscope consists of a base and a suspension arm. The power switch of the microscope is generally located on the base. Once brought into the operative field, the base should be locked to avoid unwanted motion. The position of the objective lens can then be adjusted by unlocking and locking the suspension arm using the handles. Once the microscope is positioned, dials on the handles allow for zoom and focus. Directly above the eyepiece is a knob that allows adjustment of the interpupillary distance. The operating microscope can be sterilely draped to include the suspension arm or the handles alone, depending on surgeon preference (Fig. 2).
Figure 2.
Image demonstrating proper sterile draping of the operative microscope using sterile gloves to drape the handles alone.
There are a variety of microsurgical instruments that should be within the assistant’s vernacular. These include the micro needle holder, micro forceps, straight micro scissors, curved micro scissor, vessel dilator, single micro clamp, and double approximator micro clamps (Fig. 3).
Figure 3.
Image depicting (from left to right) the micro forceps, micro needle holder, curved micro scissor, straight micro scissors, and Acland single and double approximator micro vessel clamps. The micro forceps are used for grasping and manipulating tissues and sutures. The micro needle holder is used to drive the needle. Micro scissors are used for micro tissue dissection and suture cutting. The Acland micro vessel clamps are used to occlude and approximate vessels for anastomoses.
Setup and Positioning
Before handling microsurgical instruments and assisting with the procedure, the assistant’s environment should be carefully considered from an ergonomic standpoint. The assistant should be positioned comfortably from head to toe. The commonly used sitting posture is created by shifting forward on the seat while maintaining straight posture of the back and neck, stretching upward toward the eye pieces. In this posture, the hips and knees are at right angles and some weight is shifted onto the feet. Chair height is adjusted to allow positioning of the elbows at approximately 90° with the forearms supported on the table to minimize tremor. Towels or a folded surgical gown placed under the wrists or forearms help position the hands optimally in the microsurgical field, preventing fatigue and, again, minimizing tremor (Fig. 4). The next step is focusing the microscope to allow both the primary surgeon and the assistant to remain in focus as the microscope head is repositioned and the magnification is adjusted throughout the procedure. This so-called parfocal view is achieved by increasing the magnification to the highest setting, focusing on a defined point in the center of the field, then decreasing the magnification to the lowest setting, and then focusing each eye separately using the eye pieces. This is followed by setting the interpupillary distance. This is a simple adjustment of the binocular tubes so that the dual images emerging from the eye pieces align with the surgeon’s pupils. If done correctly, the result is a sharp three-dimensional picture.
Figure 4.
Example of optimal posture and positioning of the microsurgical assistant.
Microsurgical Tasks
Several operative tasks that are best performed by two surgeons offer an opportunity for meaningful contribution by the assistant microsurgeon. Such microsurgical tasks include vessel manipulation for anastomosis, nerve manipulation and handling, and suture management. These steps are discussed in detail further in the article, and intraoperative images with corresponding renderings are provided to depict the techniques. Techniques specific to certain maneuvers or operative steps are discussed first, followed by general principles that should be considered throughout the duration of the surgery.
Vessel manipulation
Careful vessel manipulation is critical for successful anastomosis and microsurgical outcomes. The assistant surgeon should aid in manipulating vessel ends in preparation for anastomosis and needle driving. Care should be taken during dissection to avoid any damage to the perforating vessels.
Vessels are optimally manipulated using rotation and tension to facilitate suturing by the primary surgeon. Coordination of such tasks requires careful teamwork and communication. In the placement of two 180° or three 120° stay sutures, the assistant can provide value in the placement of the second and third sutures. For example, the assistant can gently grasp the adventitia with forceps in each hand, rotating and dilating the vessel to demonstrate subsequent suture placement. This surface should directly face the primary suture.
After placement of stay sutures, the assistant should aid the primary surgeon in visualization of the intraluminal space for suture placement. This can be achieved by rotating the vessel using the long suture end of a “stay stitch.” The assistant’s second forceps can gently grasp the adventitia near the location of the next suture to pull the cut edge away from the contralateral vessel. This allows the primary surgeon to safely dilate the vessel with forceps or pass the suture with complete visualization.
Additionally, the assistant should ensure that the primary surgeon avoids inadvertently catching the back wall of the vessel with the suture, catching adventitia, or crossing the intraluminal aspects of sutures. For both arterial and venous anastomoses, the assistant surgeon should appreciate any intraluminal blood obscuring operative visualization. If intraluminal blood does preclude visualization, the assistant can flush the field with heparinized saline and clear any fluid with a cellulose eye spear. When a venous coupler is being used, the assistant should ensure that the coupler device is not placing any undue tension on veins.
When performing end-to-side vessel anastomoses, the microsurgical assistant can help the primary surgeon by pulling and rotating the suture line so that the primary surgeon works on a flat surface. An experienced assistant may place sutures from the assistant’s side when the line of vision for the primary surgeon is obscured.
Nerve manipulation
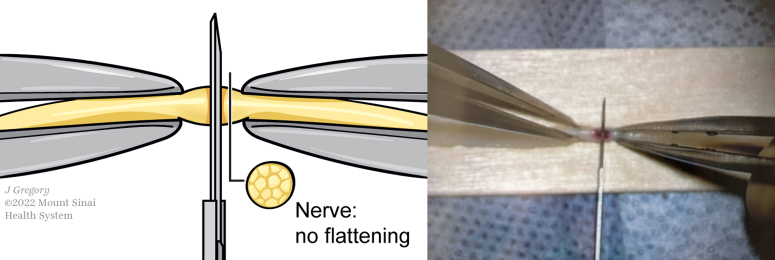
The microsurgical assistant plays an important role in manipulating neural structures for cutting and reconstruction. In preparation for cutting, the nerve should be supported circumferentially to keep the nerve tubular and avoid compression or flattening (Fig. 5). The aim of the assistant should be to provide appropriate stabilization and visualization to facilitate a clean cut by the primary surgeon. This can best be achieved by creating appropriate tension using two forceps positioned around the desired cutting point, with the nerve positioned over a clean background for optimal contrast and visualization.
Figure 5.
Schematic and clinical image depicting nerve transection under the microscope with circumferential support to keep the nerve tubular, avoiding compression or flattening.
Suture manipulation
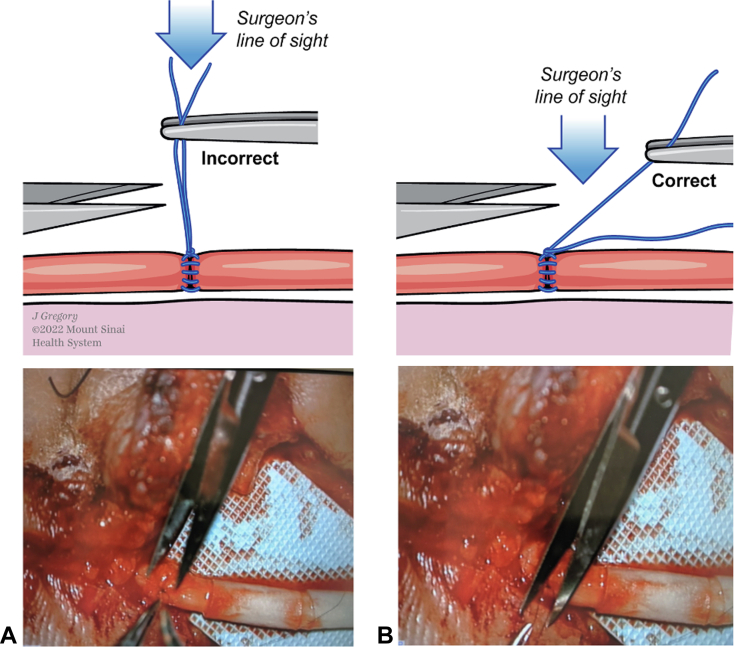
Suture manipulation and management during microsurgery are important to ensure effective anastomosis completion and mitigate iatrogenic intraoperative complications during suture cutting and knot tying. In preparation for suture cutting, the assistant should hold the suture perpendicular to the optical path, providing maximal visualization for the primary surgeon (Fig. 6). Additionally, the assistant should present the sutures individually to the primary surgeon for cutting, providing appropriate tension. The assistant should avoid holding the suture in line with the optical path, which reduces visualization for the primary surgeon and increases the risk of operative complications. Suture tails should be cut to a length at which they do not interfere with passage of the next suture and do not become entrapped in the next knot.
Figure 6.
Schematic and clinical image depicting suture cutting under the microscope. (A) holding the suture straight up makes it difficult for the assistant to assess where the suture should be cut. (B) The surgeon optimizes visualization by holding the suture at an angle to the optical path, allowing the assistant to gauge where to place the cut.
The assistant surgeon should assist with knot tying because handling the ends of a micro suture is difficult when the suture becomes adherent to surrounding raw tissue surfaces or is placed in ergonomically suboptimal positions. During knot tying, the free end of the suture should be placed in air and at a convenient location for easy grasping (Fig. 7). The assistant should hold the short end close to the emergence point so that the primary surgeon can grasp closer to the free end of the suture, which prevents looping the short end of the suture in the knot. The assistant surgeon should also hold the adjacent suture as a way to open the lumen and minimize the risk of catching the back wall of the vessel with the needle.
Figure 7.
Schematic and clinical image depicting the use of long suture ends to rotate and position vessel ends for suture passing. During suture knot tying, the free end of the suture should be kept in air and at a convenient location for easy grasping.
Other operative principles
An important principle of assisting in microsurgery is providing appropriate retraction to facilitate exposure and optimize visualization. As discussed earlier, providing retraction is important at several points throughout the operation, including vessel positioning for anastomosis, needle driving, nerve cutting, and suture cutting. In scenarios in which the assistant microsurgeon cannot visualize the anatomy of interest through the microscope during retraction, he or she may consider using loupes during these steps to improve visualization.
The assistant microsurgeon may also play an important role in mitigating tremor-related movement and variability of the primary surgeon. This has been specifically described in replantation surgery of amputated parts.6 In the absence of an assistant, other techniques to reduce intraoperative tremor include the use of a microsurgical tray and silicone finger mat to atraumatically hold amputated parts during replantation.7
The assisting microsurgeon should be conscious of other seemingly simple surgical principles, including anticipation and communication. Throughout the procedure, the assistant should anticipate next steps in providing tension and maximizing visualization.8 The assistant should aim to improve in anticipating surgical needs throughout the course of the operation and in subsequent cases. The primary surgeon and assisting surgeon should strive for effective communication throughout the operation, especially during steps requiring high degrees of coordination, such as vessel anastomosis.9 Positive outcomes of such steps require well-articulated, closed-loop communication from both the primary surgeon and assistant.
Future Directions
Studies focusing on training microsurgeons have been primarily limited to microsurgical educational curricula. One study implementing an online microsurgical residency training curriculum found an increase in precurriculum and postcurriculum test scores and faster anastomosis times compared with those with controls.10 Another systematic review of five randomized controlled trials on microsurgical education found strong evidence for the effectiveness of training on low-fidelity models to improve skills on higher-fidelity human cadavers.11 This study also highlighted the relative paucity of research on microsurgical education—of >2,000 original citations queried, only five studies were ultimately included.11
Research on the role and impact of surgical assistants in microsurgery and other surgical fields is limited. Because microsurgical cases are performed daily at most institutions, additional research should be performed on this important aspect of patient care. Future directions may include consideration of the utility of paired training and whether paired training may be superior to individual training.
In conclusion, the assistant microsurgeon plays a critical role in the outcome of any microsurgical procedure, and a proficient assistant microsurgeon can help the primary surgeon navigate difficult tasks with ease. The assistant microsurgeon should be cognizant of operative steps, including vessel handling, nerve manipulation, and suture management. Other surgical principles of providing tension, reducing tremor-related or unintentional movement, anticipating next steps, and effective communication may be applied throughout the procedure to optimize outcomes while reducing operative time. Additional research and literature are warranted to better characterize the ideal education and role of newly assisting microsurgeons.
Acknowledgements
The authors thank Jill Gregory, CMI, a Medical Illustrator at the Icahn School of Medicine at Mount Sinai, for her illustrations included in this manuscript. This manuscript was supported by the Department of Surgery at NYC Health and Hospitals/Elmhurst.
Footnotes
Declaration of interests: D.F.V. is a fellow and consultant to Artis Ventures. No benefits in any form have been received or will be received by the other authors related directly to this article.
References
- 1.Dohlman G.F. Carl Olof Nylen and the birth of the otomicroscope and microsurgery. Arch Otolaryngol. 1969;90(6):813–817. doi: 10.1001/archotol.1969.00770030815025. [DOI] [PubMed] [Google Scholar]
- 2.Elliott R.M., Baldwin K.D., Foroohar A., Levin L.S. The impact of residency and fellowship training on the practice of microsurgery by members of the American Society for Surgery of the Hand. Ann Plast Surg. 2012;69(4):451–458. doi: 10.1097/SAP.0b013e318248036d. [DOI] [PubMed] [Google Scholar]
- 3.Niveditha M., Sharma R., Suri A. Microsurgical suturing assessment scores: a systematic review. Neurosurg Rev. 2022;45(1):119–124. doi: 10.1007/s10143-021-01569-3. [DOI] [PubMed] [Google Scholar]
- 4.Balasundaram I., Aggarwal R., Darzi L.A. Development of a training curriculum for microsurgery. Br J Oral Maxillofac Surg. 2010;48(8):598–606. doi: 10.1016/j.bjoms.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Chan W.Y., Matteucci P., Southern S.J. Validation of microsurgical models in microsurgery training and competence: a review. Microsurgery. 2007;27(5):494–499. doi: 10.1002/micr.20393. [DOI] [PubMed] [Google Scholar]
- 6.Venkatramani H., Sabapathy S.R. A simple technique for securing the amputated part during preparation in fingertip replantation. Br J Plast Surg. 2004;57(6):592–593. doi: 10.1016/j.bjps.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Blackburn A.V., Jemec B. The microsurgical instrument tray–a tremor-free assistant for stabilising amputated parts in replant surgery. J Plast Reconstr Aesthet Surg. 2007;60(8):961. doi: 10.1016/j.bjps.2007.01.063. [DOI] [PubMed] [Google Scholar]
- 8.Sexton K., Johnson A., Gotsch A., Hussein A.A., Cavuoto L., Guru K.A. Anticipation, teamwork and cognitive load: chasing efficiency during robot-assisted surgery. BMJ Qual Saf. 2018;27(2):148–154. doi: 10.1136/bmjqs-2017-006701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nagpal K., Vats A., Lamb B., et al. Information transfer and communication in surgery: a systematic review. Ann Surg. 2010;252(2):225–239. doi: 10.1097/SLA.0b013e3181e495c2. [DOI] [PubMed] [Google Scholar]
- 10.Satterwhite T., Son J., Carey J., et al. Microsurgery education in residency training: validating an online curriculum. Ann Plast Surg. 2012;68(4):410–414. doi: 10.1097/SAP.0b013e31823b6a1a. [DOI] [PubMed] [Google Scholar]
- 11.Ghanem A.M., Hachach-Haram N., Leung C.C.M., Myers S.R. A systematic review of evidence for education and training interventions in microsurgery. Arch Plast Surg. 2013;40(4):312–319. doi: 10.5999/aps.2013.40.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]