Abstract
Background
Radiofrequency (RF) devices are being increasingly used for cosmetic dermatology applications. Recent studies have reported an apparent dualistic nature of RF devices for hair, causing either removal or growth depending on the modality of RF.
Materials and Methods
PubMed/MEDLINE and Web of Science searches were conducted in July 2022 according to PRISMA guidelines for studies discussing RF technology in hair applications (n = 19).
Results
The majority of studies describe the utility of RF devices in removal of unwanted hair (n = 15). Bipolar RF has been used in combination with intense pulsed light for effective long-term removal of body and facial hair. The chromophore-independent method of energy delivery in RF makes it a viable add-on therapy for treating lighter colored hair and darker Fitzpatrick skin types. Monopolar RF is used for eyelash removal in patients with trichiasis. In contrast, fractional RF has been used to stimulate hair growth in patients with alopecia areata and androgenetic alopecia.
Conclusions
Preliminary evidence supports the use of bipolar and monopolar RF devices for hair removal, while fractional RF appears to be an emerging technology for hair growth. Additional studies are needed to investigate the efficacy, mechanisms, and parameters of radiofrequency devices for various hair applications.
Keywords: Radiofrequency, Alopecia, Hair
Introduction
With the recent rise in hair loss conditions, there is a newly heightened attention to the need for better therapies, including novel devices. With significant advances in technology, the use of radiofrequency (RF) devices has expanded into the field of dermatology for an array of skin conditions including rhytides, cellulite, and hypertrophic scars [1]. The role of RF devices in the hair science arena is not as clear: while studies report increased use of RF devices for hair removal, there are also recent reports of RF devices used for hair growth [2, 3]. This apparent dual nature in hair applications makes RF an intriguing modality with a potential therapeutic role in a spectrum of hair conditions.
RF systems work by producing a high-frequency, alternating electric field that induces current through charged molecules. When applied to tissue, polar molecules such as water align within the field and oscillate rapidly, producing thermal energy that heats the surrounding tissue − a process known as resistive heating [4]. Unlike lasers that require a chromophore such as melanin for energy transfer, RF depends on the intrinsic impedance of the targeted tissue, making it a safer option to be used across all skin types [5].
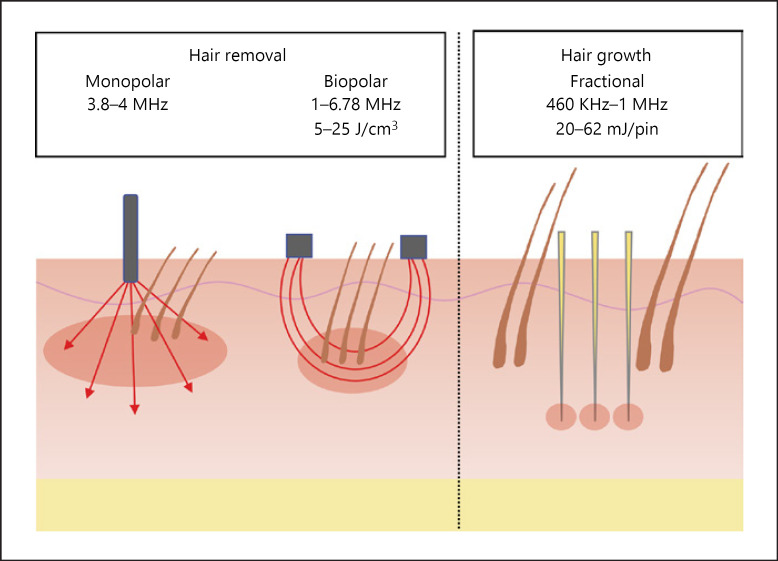
The distribution of the RF current, and thus the mode of energy delivery, is contingent on the configuration of the system's electrodes [6]. Monopolar RF (mRF) consists of a single active electrode and a large grounding electrode placed on the patient. The mRF electrode concentrates energy at the point of contact with tissue but dissipates rapidly with distance as current is conducted toward the grounding pad. Bipolar RF (biRF) consists of two electrodes at a fixed distance between which current is conducted. In this configuration, current is limited to only the tissue placed directly between the electrodes, thus enabling a more controlled distribution of current [7]. Fractional RF consists of multiple electrodes in an array of pins or needles that deliver energy at controlled depths with minimal superficial involvement [5]. These distinct modalities allow for delivery of different degrees of thermal energy to variable depths of skin (Fig. 1).
Fig. 1.
Three RF modalities: monopolar, bipolar and fractional.
In our search for novel hair loss therapeutic modalities, a better insight into the role of RF technologies in hair applications is warranted. With that goal, we reviewed and assessed the literature to provide an overview of the RF modalities used for therapeutic hair applications, their respective efficacies, side effects, and strength of evidence.
Methods and Materials
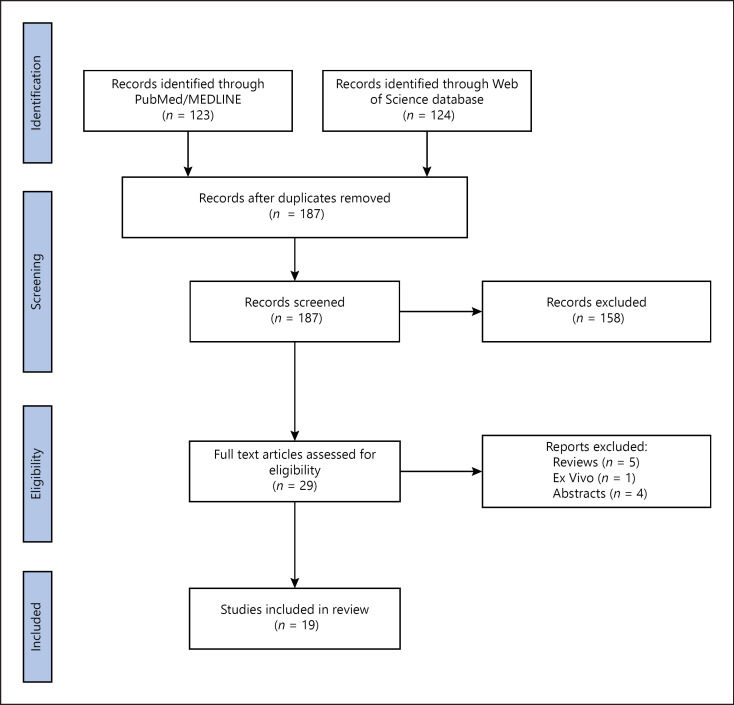
A primary literature search was conducted in July 2022 using the PubMed/MEDLINE and Web of Science databases with the search terms “(radiofrequency OR “radio frequency”) AND (alopecia OR hair OR trichiasis)” according to PRISMA reporting guidelines for systematic reviews (Fig. 2). Only full-text articles that directly evaluated the use of RF in human hair growth or reduction were included. Case reports, case series, case-control, cohort, cross-sectional, and randomized controlled trials were all included. Studies written in languages other than English, abstracts, animal studies, ex vivo or in vitro studies, review articles, or studies not specific to hair were excluded.
Fig. 2.
PRISMA flow diagram for the literature review of RF in hair.
Results
One hundred eighty-seven articles were found using the search terms above. Of these, 19 records were included for review after search criteria were applied: four randomized controlled trials, three multi-center cohort studies, nine single-center cohort studies, one retrospective study, one case series, and one case report. Fifteen studies described the utility of RF in hair reduction and four in hair growth (Tables 1, 2).
Table 1.
Summary of studies using RF for hair removal
| Hair removal | ||||||||
|---|---|---|---|---|---|---|---|---|
| Source | Type of study (evidence level) | Target | System/settings | RF modality | Adjunct | Patients | Treatment plan | Results/findings |
| Yaghmai et al. (2004) | Prospective multicenter study (II) | Facial/body hair | IPL + RF system Aurora DS (Syneron Medical Ltd., Yokneam, Israel) RF: 1 MHz, 10–20 J/cm3, 200 ms pulse Optical energy: 680–980 nm, 14–30 J/cm2, 25 ms pulse |
Bipolar | IPL | 60 F, 9 (age range: 18–64 year/o) Skin type: I–VI |
IPL + RF: 1 tx | 90 days post-tx Average hair count reduction from baseline: 46% AEs: transient hyperpigmentation, hypopigmentation, erythema, perifollicular edema, crusting |
| Garden et al. (2020) | Prospective multicenter study (II) | Facial/body hair | Combined IPL and RF me system (Syneron Medical Ltd., Yokneam, Israel) RF: 6.78 MHz, 2 W, 2 s pulse Optical energy: 550–100 nm, 2–4 J/cm2, 6 ms pulse |
Bipolar | IPL | Study 1:50 F and 8 M (age range: 18–58) Study 2:19 F (age range: 20–59) Skin type: I–VI |
Study 1 (body hair): IPL+ RF (7 weekly tx) → non-maintenance versus maintenance (monthly tx for 6–12 month) Study 2 (facial hair): IPL + RF (4 tx over 2–5 days → 2 weekly tx → 6 biweekly tx) |
Study 1 Mean hair reduction, 6 month post-tx Maintenance: 56% Non-maintenance: 47% Mean hair reduction, 12 month post-tx Maintenance: 52% Non-maintenance: 37% Study 2 Mean hair reduction Post-tx: 45% 12 month post-tx: 42% AEs: mild pain, transient erythema |
| Erkiert-Polguj et al. (2021) | Prospective single-center study (II) | Axillary hair | IPL + RF system (Mimari, Poland) Optical energy: 420–630 nm, 7 mm depth, 28 J/cm2−34 J/cm2, 2× passes RF: 7 mm depth |
Bipolar | IPL | 33 F with dark hair (age range: 21–47) Skin type: II–III | IPL (one axilla) (4 total tx, 4 week intervals) IPL + RF (other axilla) (4 total tx, 4 week intervals) |
3 month post-tx Mean hair reduction IPL: 33.4% IPL + RF: 38.82% AEs: mild burning and stinging sensation during tx |
| Sadick et al. (2004) | Prospective single-center study (II) | Facial hair | IPL + RF system RF: 20 J/cm3, up to 120 ms pulse, 4 mm depth Optical energy: 680–980 nm, 24–30 J/cm2, short pulse profile mode |
Bipolar | IPL | 36 F with white and blonde facial hair (age range: 38–83 year/o) Skin type: I–V | IPL + RF (4 total tx over 9–12-mo period) | 6 month post-tx Average hair clearance of 48% Slightly increased clearance rate for blonde hair (52%) versus white hair (44%) AEs: transient hyperpigmentation and mild persistent erythema |
| Sadick et al. (2004) | Prospective single-center study (II) | Facial/body hair | IPL + RF system Aurora DS (Syneron Medical, Yokneam, Israel) RF: 10–20 J/cm3, up to 120 ms pulse, 4 mm depth Optical energy: 680–980 nm, 15–26 J/cm2, up to 120 ms pulse |
Bipolar | IPL | 40 adults (age range: 18–46 year/o) Skin type: II–V |
IPL + RF (4 total tx over 9–12-mo period, at 8–12-wk intervals) | 6 month post-tx Average hair clearance of 75% observed in all body locations. No significant dependence on skin type AEs: transient erythema |
| Sochor et al. (2011) | Randomized controlled trial (I) | Leg hair | IPL + RF system Aurora DS (Syneron Medical Ltd., Yokneam, Israel) RF: 1 MHz, 5–20 J/cm3 Optical energy: 680–980 nm, 30 J/cm2 Diode Laser MeDioStar XT (Asclepion, Germany) 810 nm, 32 J/cm2 pulse |
Bipolar | IPL | 40 F with varying hair color (age range: 20–53 year/o) Skin type: II–III |
IPL (2 total tx, 4–6-wk intervals) versus IPL + RF (2 total tx, 4–6-wk intervals) versus diode laser (2 total tx, 4–6-wk intervals) | 8 month post-tx Mean hair count reduction IPL: 39.16% IPL + RF:47.15% Diode laser: 49.90% IPL + RF and Diode both > IPL alone IPL + RF comparable to diode lasers AEs: Tx-associated pain, mild erythema, perifollicular edema, and transient hyperpigmentation |
| Garden et al. (2014) | Prospective multicenter study (II) | Facial/body hair | Combined IPL and RF device Bipolar me system (Syneron Medical Ltd., Yokneam, Israel) RF: 6.78 MHz, 2 W, 6 ms pulse Optical: 550–1200 nm, 2–4 J/ cm2 |
Bipolar | IPL | 89 F, 9 M with brown/ black hair (age range: 23–60 year/o) Skin type: I–VI |
IPL + RF Study 1 (n = 94) 7 total tx, at 1-wk intervals followed by 3 additional tx at 4-wk intervals (maintenance side) versus zero additional tx (no maintenance side) Study 2 (n = 37) 3 total tx at 2–4-d intervals |
Study 1 1 month post-tx 55% reduction in hair count bilaterally 3 month post-tx maintenance = 58% reduction no maintenance = 43% reduction Study 2 2 month post-tx 44% hair reduction AEs: transient erythema, edema, itching. One subject with blistering in axilla |
| Schroeter et al. (2006) | Prospective single-center study (II) | Not specificed | IPL + RF system Aurora DS Bipolar (Syneron Medical Ltd., Yokneam Israel) Mean energy used per patient RF: 18.6 J/cm3 IPL: 23.2 J/cm2 |
Bipolar | IPL | 17 F with blond hair (age range: 45–66 year/o) Skin type: I–II |
IPL + RF 4–12 total tx, 30–798-day duration |
Mean of 8.45 tx 54.7% mean hair reduction Correlation found between hair removal and the number of tx (Pearson correlation coefficient: −0.15) No serious AEs observed |
| Goldberg et al. (2005) | Prospective single-center study (II) | Facial hair | IPL + RF system Aurora DS Bipolar (Syneron Medical Ltd., Yokneam Israel) RF: 20 J/cm3, 4 mm depth Optical energy: 680–950 nm, 24–30 J/cm2, short pulse profile mode |
Bipolar | IPL, 5-ALA | 15 F with non-pigmented facial hair (age range: 45–65 year/o) Skin type: II–IV |
IPL + RF (2 total tx, 4–6 week intervals) + Topical aminolevulinic acid versus IPL + RF (2 total tx, 4–6 week intervals) |
6 month post-tx Mean terminal white hair removal ILP + RF: 35% ILP + RF + topical ALA: 48% 0/5 patients with vellus hair responded to tx AEs: transient post-tx erythema |
| Karsai et al. (2009) | Retrospective study (II) | Facial hair | IPL + RF system Aurora DS Bipolar (Syneron Medical Ltd., Yokneam, Israel) RF: 1 MHz, 20 J/cm3 Optical energy: 680–980 nm, 30 J/cm2 Mean fluence used per patient IPL: 23.7 J/cm2 RF: 17.6 J/cm3 |
Bipolar | IPL | 24 F (age range: 12–76 year/o) Skin type: II–II |
IPL + RF (3 total tx at 4–6 week intervals followed by additional tx at 3-mo intervals) | Mean of 5.2 treatments 3.2 month mean follow-up: no/poor clearance: 22.2% moderate: 28.9% good: 46.7% excellent: 2.2% AEs: erythema, swelling, and hyperpigmentation |
| Farshi et al. (2012) | Double-blind, randomized, placebo-controlled study (I) | Facial hair | IPL + RF Aurora/ELOS system Bipolar (Syneron Medical Ltd., Yokneam, Israel) RF: 18–25 J/cm3 Optical energy: 18–26 J/cm2 |
Bipolar | IPL, finasteride | 75 F with facial hirsutism (age range: 21–52 year/o) Skin type: III–IV |
IPL + RF (3 total tx at 4-wk intervals, additional 1tx at 6 month f/u) + finasteride (2×/daily) versus IPL + RF (3tx q4wk, 1 tx at 6 month F/U) + placebo (2×/daily) | 6 month post-tx mean hair density (IPL + RF) + finasteride: 19.7 → 8 5(IPL + RF) + placebo: 19.1 → 9 Finasteride treatment with IPL + RF is significantly more effective than monotherapy AEs: mild discomfort and transient erythema |
| Salour et al. (2011) | Double-blind, randomized clinical trial (I) | Trichiasis | RF Ellman Surgitron (Cynosure Monopolar LLC., Westford, MA, USA) RF: 4-MHz, (power = 2), 2–3 mm depth, cut-coag mode Green argon laser continuous mode 930-nm argon coherent device, 50-µm diameter, 760-mW |
Monopolar | none | 56 F, 44 M with trichiasis (age range: 14–98 year/o) | Single tx RF (n = 48) versus argon laser (n = 52) |
3 month post-tx Treatment success 82.4% RF group 62.9% in laser group Recurrence 17.6% RF group 37.1% laser group RF is significantly more effective than argon laser therapy for treating trichiasis AEs: notching observed in 4 patients (3 RF, 1 argon laser) |
| Kim et al. (2014) | Prospective single-center study (II) | Trichiasis | Ellman Surgitron (RF) (Cynosure LLC., Westford, MA, USA) 3.8-MHz, 2–3 mm depth, cut and coag mode, power = 3 | Monopolar | Mitomycin C |
14 F, 7 M with trichiasis (age range: 40–76 year/o) | Single tx Group 1 (9 F, 5 M) RF ablation + injection of 0.02% mitomycin C Group 2 (5 F, 2 M) RF ablation (monotherapy) |
6 month post-tx Recurrence 16.4% RF + mitomycin C 60.7% RF (monotherapy) 0.02% mitomycin C in conjunction with RF ablation significantly improves success rate of RF ablation treatment in trichiasis patients AEs: eyelid notching reported in two patients in group 2 |
| Kezirian et al. (1993) | Prospective single-center study (II) | Trichiasis | Ellman Surgitron FFPF (Cynosure LLC., Westford, MA, USA) 3.8-MHz, power: 2.5, 2–3 mm deep |
Monopolar | None | 16 F, 10 M with trichiasis (age range: 67–90 year/o) | Single RF tx | 6 month post-tx success rate: 67% AEs: eyelid notching (n = 2), granuloma (n = 1), and persistent erythema and tenderness post 1 month (n = 1) |
| Mehta et al. (2022) | Case report (IV) | Axillary hair | maXium (KLS Martin Group, Freiburg, Germany) RF: 5–10 W, applied to 0.25-mm acupuncture needles |
Monopolar | None | 1 patient with hidradenitis suppurativa | Single RF tx of axillary hair | Hair density decreased from 23/cm2 to 4/ cm2 (83% reduction) Hidradenitis suppurativa lesions healed a month after procedure but recurred 4 months later AEs: mild hyperpigmentation |
Table 2.
Summary of studies using RF for hair growth
| Hair growth | ||||||||
|---|---|---|---|---|---|---|---|---|
| First author | Type of study (evidence level) | Condition | System/settings | RF modality | Adjunct | Patients | Treatment plan | Results/findings |
| Tan et al. (2019) | Prospective placebo-controlled trial (II) | AGA | Novel Device (Innogen, Tel Aviv, Israel) RF: 460 KHz 12 W, 62 mJ/pin |
Fractional | None | 24 M with AGA (avg age of 29.5) | RF treatment (n = 19) versus sham (n = 5) 4 total tx at 3-wk intervals |
Average increase in hair counts RF = 22.8% versus sham = 9.6% (p = 0.08) No AEs observed |
| Verner et al. (2018) | Prospective single-center study (II) | AGA | HairLux (Innogen Technologies Ltd., Yokneam, Israel) RF: 460 KHz 20 mJ/pin |
Fractional | None | 18 F, 7 M with AGA (age range: 19–73 year/o) | 10 total tx, 2-wk intervals | 2 month post-tx Hair density: 31.6% average increase Hair shaft thickness: 18% average increase No serious AEs observed |
| Yu et al. (2018) | Randomized controlled split-scalp trial (I) | AGA | BodyTite (Derma Optic & Electronic Ltd., Chongqing, China) RF: 1 MHz 12 W, 1.5 mm depth, 300 ms |
Fractional (microneedle) | Minoxidil | 19 M with AGA (age range: 23–45 year/o) | Split-scalp treatment 5% minoxidil 2×/daily (monotherapy) versus RF (5 total tx, 4-wk intervals) + 5% minoxidil 2×/daily | 5 month post-tx Minoxidil Mean hair count: 46.22 +/− 18.77 → 63.21+/− 63.21 Mean hair thickness: 52 +/− 16 → 66 +/− 14 µm Minoxidil + RF Mean hair count: 44.12 +/− 21.58 → 73.14 +/− 25.45 Mean hair thickness: 53 +/− 13 → 71 +/− 15 µm Combined treatment with RF is significantly better than monotherapy of minoxidil alone AES: tx-related pain, transient pinpoint bleeding, and mild erythema |
| Issa et al. (2015) | Case series (IV) | AA | RF: 45 W CO2 laser: 60 W, 60 mJ/pixel | Fractional | Triamcinolone | 4 F, 1 M with AA (age range: 18–47 year/o) | CO2 laser versus RF (1–6 treatments, 3-wk intervals) + Topical Triamcinolone + Acoustic pressure wave US | Fractional RF + triamcinolone + US complete response in patient 1 and 2 after 3 tx and 6 tx, respectively Fractional CO2 laser + triamcinolone + US complete response in patients 3, 4, and 5 after 1 tx each. Results sustained at 12 month F/U AEs: mild burning sensation during tx |
RF, radiofrequency; AGA, androgenic alopecia; AA, alopecia areata; IPL, intense pulsed light; AE, adverse event; Tx, treatment; Pt, patient; F/U, follow-up; US, ultrasound.
Hair Reduction
A total of 15 studies have reported using RF-equipped devices to reduce unwanted hair growth, either as monotherapy or as an adjunctive treatment (Table 1). Interestingly, the use of mRF devices to remove eyelashes in patients with trichiasis has been documented in three separate clinical studies (total n = 147 patients). The first use was reported by Kezirian et al. [6] who demonstrated successful improvement of trichiasis in 67% of patients 6 months after a single mRF treatment. In further studies, the efficacy of mRF was compared to that of an argon laser and was found to significantly reduce trichiasis recurrence rates 3 months after a single treatment (mRF 17.6% vs. 37.1% argon laser; p < 0.001) [8]. To further improve mRF results in trichiasis patients, Kim et al. studied the effect of combining mitomycin C with RF treatment compared to RF monotherapy. They found that combination therapy had greater success with only a 16.4% recurrence rate compared to 60.7% with monotherapy 6 months after a single treatment (p < 0.01) [9].
The question of combining biRF in combination with intense pulsed light laser (IPL) to remove unwanted hair was the most frequently published topic, being reported in eleven studies. Superiority in hair removal of the IPL and biRF combination therapy compared to IPL alone was demonstrated in a blinded, controlled trial that reported a significantly greater reduction in mean hair count after two treatments (47.2% IPL/biRF vs. 39.2% IPL monotherapy; p = 0.004) [10]. A similar improvement in hair reduction with combination therapy after four weekly treatments was later reported in a split axillae study (38.8% IPL/biRF vs. 33.4 IPL monotherapy; p = 0.02) [11]. A double-blind, placebo-controlled trial of 77 patients with hirsutism sought to further increase the efficacy of combination IPL/biRF by adding topical finasteride. Their results demonstrated a significant decrease in hair density 6 months posttreatment on both the topical finasteride and placebo sides compared to their respective baseline (p < 0.0001) and a significant decrease in hair density in the topical finasteride group compared to placebo (1/cm2 lower; p = 0.04) [12].
Efficacy of IPL and biRF combination systems has varied across studies. After a single treatment, hair count in 69 patients was reduced by an average of 46% compared to baseline at 90 days posttreatment (p < 0.05) [13]. Another study reported an average hair clearance of 75% after 4 treatments in 40 patients at 18-month follow-up [3]. One study noted a positive correlation with treatment number and hair clearance, reporting >50% clearance in nearly half of patients after an average of 5.2 IPL/biRF treatments [3, 14]. A similar positive correlation was further described by Schroeter et al. [15] who reported a mean hair reduction of 54.7% in blonde-haired patients after an average of 8.5 treatments.
Hair clearance with IPL/biRF was sustained through maintenance treatment sessions. After a 55% average hair count reduction was achieved in 94 patients with seven IPL/biRF treatments, patients who continued with maintenance sessions had a significantly greater reduction in hair compared to patients who stopped treatment (58% maintenance vs. 43% non-maintenance; p < 0.01) [16]. In a similar study of 58 patients using a home-use device, those who continued monthly maintenance treatments demonstrated significantly higher long-term hair reduction at 6 and 12 months post-treatment (56% and 52%, respectively) compared to non-maintenance groups (47% and 37%, respectively) (p < 0.0001 for all comparisons) [17].
Long-term hair reduction with IPL/biRF has been demonstrated across all hair colors, including lighter colored hairs which have typically been challenging to treat with laser-based therapies. Mean hair removal after a single treatment in one study was 60% in blonde-haired patients and 40% in white-haired patients, although removal of black and brown hair was more efficacious (85% and 80%, respectively) [3]. Similar results were reported in a study of 87 patients which showed mean hair reductions of 43% for black hair, 49% for brown hair, and 35% for blonde hair (p < 0.05 all groups) [13]. Conversely, one study demonstrated no significant difference in hair clearance efficacy between fair- and dark-colored hair (p = 0.872) [14]. Sadick et al. [18] specifically studied lighter colored hair removal and reported greater efficacy of blonde facial hair removal compared to white facial hair (52% vs. 44%) after four treatments in 36 patients. A split-face trial of 15 patients showed that the efficacy of IPL/biRF in removing white facial hair could be improved by pretreating patients with aminolevulinic acid, a photosensitizing agent (48% pretreatment vs. 36% no pretreatment after two sessions) [19]. However, non-pigmented vellus hair did not respond to either treatment protocol in this trial. Finally, a study in 17 patients with blonde hair reported a mean hair reduction of 54.7% after an average of 8.5 treatments [15].
RF appeared to be well tolerated by patients of all Fitzpatrick skin types in the hair removal studies, with no serious adverse events being reported. The most commonly reported adverse events were minor, including transient erythema, edema, hyperpigmentation, and mild treatment-associated pain [10, 13, 14, 17, 18]. A total of 7 patients treated with mRF across the three trichiasis studies developed eyelid notching [6, 8, 9].
Hair Growth
In contrast, fractional RF devices have been reportedly used in four reports to help stimulate hair growth in patients with androgenetic alopecia (AGA) and alopecia areata (AA) (Table 2). Fractional RF has successfully been used as an adjunct treatment for transepidermal assisted drug delivery. One study used fractional RF treatments in combination with topical triamcinolone in two patients with AA, resulting in complete regrowth of patches after 3–6 treatments at 12 months [20]. Another split-scalp study compared hair growth with topical minoxidil, with or without fractional RF treatment (5x), in 19 patients with AGA. Mean hair counts were significantly higher with combination fractional RF therapy compared to minoxidil only (66% vs. 37% increase; p = 0.01). There was also a significant increase in hair thickness in the combination therapy group (34% vs. 27% increase; p = 0.02) [21].
The use of fractional non-ablative RF devices as monotherapy to stimulate hair growth has been evaluated in 2 studies thus far. One such device was used to treat 25 patients with AGA and demonstrated a 31.6% increase in hair density and 18% increase in hair shaft thickness after 10 treatments [22]. A similar device was used in a blinded, sham device-controlled trial in 24 patients with AGA which showed a significant increase in hair count in the RF group (22.8% RF group vs. 9.6% sham group; p = 0.08) [23].
The fractional RF devices used for hair growth were all well tolerated. No serious adverse events were reported in any of the studies. Several tolerable side effects were reported, including transient pinpoint bleeding, mild erythema, and burning or tingling sensation during treatment [20, 21].
Discussion
Depending on the modality and adjunctive treatments used, RF can either be utilized to achieve hair growth or hair removal. Currently, the existing evidence of RF in hair applications most strongly supports its use in unwanted hair removal. Of the studies that utilized RF for hair removal, the majority combined biRF energy with IPL. These devices, often referred to as electro-optical systems, consist of a biRF generator and a flashlamp that delivers pulsed light at wavelengths between 580 and 980 nm [24, 25]. The idea behind this combination therapy is that the two energy sources act synergistically to heat and destroy hair follicles at a lower optical fluence energy than would be required by IPL alone [24].
The most intriguing finding from this review is that the addition of RF is used to overcome some of the challenges that light hair and dark skin pose to laser and light-based hair removal treatments. These latter treatments rely on melanin within hair follicles to act as a chromophore that will transfer light energy into thermal energy, subsequently damaging the hair follicles [26]. However, in darker skin types where more melanin is concentrated in the epidermis, there is potential for more off-target epidermal damage, leading to blistering and dyschromia [27]. Conversely, lightly pigmented hairs cannot be treated with light-based techniques as effectively since they do not contain high concentrations of melanin [28].
Because the RF systems are dependent on tissue impedance rather than pigment chromophores, their delivery of energy is independent of hair color or skin type. The addition of biRF to IPL therapy for hair removal has been shown to be more effective than IPL alone and has been successfully used for hair removal across all skin types and most hair colors [3, 10, 11]. One notable exception is vellus hair which remains difficult to treat even with the addition of RF energy. Goldberg et al. [19], noting that biRF alone has never been reported for hair removal, speculated that IPL and biRF likely act synergistically and thus require a nonzero concentration of melanin in hair follicles to achieve follicle destruction. Sadick et al. [3] theorized that this synergy is due to the heating of hair follicles by optical energy which subsequently lowers surrounding tissue's impendence. Because current seeks the path of least resistance, RF current can more effectively concentrate in these preheated regions and assist in destroying the follicular unit. This model might explain why IPL and RF combination systems are still more effective at removing darker pigmented hair than lighter colors, as is also the case with IPL monotherapy [3]. The success of hair removal with these systems has been variable, but it appears to be dependent on the number and frequency of treatment sessions as well as the adjunctive topical treatments used.
Unlike biRF, monopolar has been used for hair removal as monotherapy and independent of other energy sources [6, 8]. The most commonly reported application of mRF is for treating trichiasis. Since first being reported for this purpose in 1993, it has grown in use due to its efficacy, relative ease of use, and cost-effectiveness [6, 8]. The devices used in these studies consist of a handpiece, a disposable electrode tip, and an RF generator that operates in the 3.8–4 MHz range. The electrode tips are inserted directly into individual eyelash follicles which are then ablated. A variation on this technique was reported by Mehta et al. [29] who applied a mRF device to acupuncture needles inserted into axillary hair follicles in a patient with hidradenitis suppurativa. In this case, the acupuncture needles acted as a conductor of RF current, theoretically reducing wear and tear of the electrode tip.
Our quest to identify novel hair growth-stimulating therapies concluded that RF devices can be utilized to achieve hair growth in certain conditions when a fractional modality is used, either alone or in conjunction with topical treatments. This modality has been used to enhance delivery of local steroids and minoxidil which are considered mainstays of AA and AGA, respectively. Fractional RF, which creates micro-perforations in the epidermis, facilitates a more efficient delivery of drugs to deeper levels of the skin through channels, thus helping overcome limitations in achieving a homogenous dermal distribution with topical treatments alone. This treatment strategy, known as transepidermal drug delivery, has previously been used for a variety of dermatologic treatments. Yu et al. [21] utilized this technique to deliver minoxidil in patients with AGA, resulting in increased hair growth compared to minoxidil alone. However, the authors speculated that the resulting wounds of fractional RF might have also contributed to this result. Indeed, hair growth has been reported following fractional RF treatments alone [2]. Potential mechanisms for fractional RF wound-induced hair growth include anagen phase maintenance by insulin-like growth factor-1 upregulation, increased local tissue perfusion via VEGF induction, or new hair follicle formation resulting from Wnt signaling stimulation [22]. Thus, fractional RF, which induces targeted dermal injury using an array of pins or microneedles, appears to be an emerging technology for stimulating hair growth in conditions such as AGA even when used as monotherapy [22, 23]. However, the number of studies to date on RF for hair growth is limited, and larger studies are needed to further evaluate the technology's efficacy in restoring hair.
Limitations of this review include the differences in RF delivery systems and settings, treatment number, frequency, and follow-up duration. Further difficulties arise in assessing clinical efficacy due to combinations with IPL, lasers, microneedling, and topical modalities, heterogeneous methods of measuring changes in hair density and hair count, and small sample sizes.
Conclusion
Review of the literature reveals preliminary evidence for the use of RF in either hair removal or hair growth, depending on the modality and adjunctive treatments used. The available data has focused on combined use of biRF and IPL in reduction of body hair, which may be less dependent on hair and skin pigmentation than classic laser modalities. mRF is an effective choice for the treatment of trichiasis. Both modalities have shown good safety profiles and long-term efficacy in hair removal. In contrast, fractional RF used for hair growth has been described both as monotherapy and as a means of assisting topical drug delivery. This research is in its nascent stages, and additional studies are needed to validate its efficacy and to investigate its mechanism of action.
Statement of Ethics
An ethics statement is not applicable because this review is based exclusively on published literature.
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
Funding Sources
The authors did not receive any funding to complete this research.
Author Contributions
Colin Kincaid was responsible for writing the manuscript, analyzing and extracting data, and figure illustration. Nadine Romdhane, Ella Csuka, and Ajay N. Sharma were responsible for conceptualizing this work and screening all abstracts and full-text articles. Margit Juhasz and Natasha Mesinkovska were responsible for critical revisions.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Funding Statement
The authors did not receive any funding to complete this research.
References
- 1.Belenky I, Margulis A, Elman M, Bar-Yosef U, Paun SD. Exploring channeling optimized radiofrequency energy a review of radiofrequency history and applications in esthetic fields. Adv Ther. 2012 Mar;29((3)):249–266. doi: 10.1007/s12325-012-0004-1. [DOI] [PubMed] [Google Scholar]
- 2.Wang S, Mi J, Li Q, Jin R, Dong J. Fractional microplasma radiofrequency technology for non-hypertrophic post-burn scars in Asians a prospective study of 95 patients. Lasers Surg Med. 2017 Aug;49((6)):563–569. doi: 10.1002/lsm.22640. [DOI] [PubMed] [Google Scholar]
- 3.Sadick NS, Shaoul J. Hair removal using a combination of conducted radiofrequency and optical energies--an 18-month follow-up. J Cosmet Laser Ther. 2004 May;6((1)):21–26. doi: 10.1080/14764170410029013. [DOI] [PubMed] [Google Scholar]
- 4.Kam J, Frost A, Bloom JD. Radiofrequency rejuvenation of the ‘tweener’ patient under, over, or through the skin. Facial Plast Surg. 2021 Apr;37((2)):240–248. doi: 10.1055/s-0041-1722890. [DOI] [PubMed] [Google Scholar]
- 5.Weiner SF. Radiofrequency microneedling overview of technology, advantages, differences in devices, studies, and indications. Facial Plast Surg Clin North Am. 2019 Aug;27((3)):291–303. doi: 10.1016/j.fsc.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Kezirian GM. Treatment of localized trichiasis with radiosurgery. Ophthalmic Plast Reconstr Surg. 1993 Dec;9((4)):260–266. doi: 10.1097/00002341-199312000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Sadick N, Sorhaindo L. The radiofrequency frontier a review of radiofrequency and combined radiofrequency pulsed-light technology in aesthetic medicine. Facial Plast Surg. 2005 May;21((2)):131–138. doi: 10.1055/s-2005-872414. [DOI] [PubMed] [Google Scholar]
- 8.Salour H, Rafati N, Falahi MR, Aletaha M. A comparison of argon laser and radiofrequency in trichiasis treatment. Ophthalmic Plast Reconstr Surg. 2011;27((5)):313–316. doi: 10.1097/IOP.0b013e31820e59f5. [DOI] [PubMed] [Google Scholar]
- 9.Kim G-N, Yoo WS, Kim SJ, Han YS, Chung IY, Park JM, et al. The effect of 0.02% mitomycin C injection into the hair follicle with radiofrequency ablation in trichiasis patients. Korean J Ophthalmol. 2014 Feb;28((1)):12–18. doi: 10.3341/kjo.2014.28.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sochor M, Curkova AK, Schwarczova Z, Sochorova R, Simaljakova M, Buchvald J. Comparison of hair reduction with three lasers and light sources prospective, blinded and controlled study. J Cosmet Laser Ther. 2011 Oct;13((5)):210–215. doi: 10.3109/14764172.2011.586422. [DOI] [PubMed] [Google Scholar]
- 11.Erkiert-Polguj A, Algiert-Zielinska B, Skubalski J, Rotsztejn H. Comparison of hair reduction by intensive pulsed light device and combined intense pulsed light with a bipolar radiofrequency. J Dermatolog Treat. 2021 Dec;32((8)):945–949. doi: 10.1080/09546634.2020.1722310. [DOI] [PubMed] [Google Scholar]
- 12.Farshi S, Mansouri P, Rafie F. A randomized double blind vehicle controlled bilateral comparison study of the efficacy and safety of finasteride 0.5% solution in combination with intense pulsed light in the treatment of facial hirsutism. J Cosmet Laser Ther. 2012 Aug;14((4)):193–199. doi: 10.3109/14764172.2012.699680. [DOI] [PubMed] [Google Scholar]
- 13.Yaghmai D, Garden JM, Bakus AD, Spenceri EA, Hruza GJ, Kilmer SL. Hair removal using a combination radio-frequency and intense pulsed light source. J Cosmet Laser Ther. 2004 Dec;6((4)):201–207. doi: 10.1080/14764170410008133. [DOI] [PubMed] [Google Scholar]
- 14.Karsai S, Schmitt L, Raulin C, Hammes S. Combination of short- and long-pulsed mode of electro-optical synergy technology for photoepilation a retrospective study with short- and long-term follow-up. J Eur Acad Dermatol Venereol. 2009 Jan;23((1)):46–51. doi: 10.1111/j.1468-3083.2008.02944.x. [DOI] [PubMed] [Google Scholar]
- 15.Schroeter CA, Sharma S, Mbonu NC, Reineke T, Neumann HAM. Blond hair removal using ELOS systems. J Cosmet Laser Ther. 2006 Jun;8((2)):82–86. doi: 10.1080/14764170600660946. [DOI] [PubMed] [Google Scholar]
- 16.Garden JM, Zelickson B, Gold MH, Friedman D, Kutscher TD, Afsahi V. Home hair removal in all skin types with a combined radiofrequency and optical energy source device. Dermatol Surg. 2014 Feb;40((2)):142–151. doi: 10.1111/dsu.12407. [DOI] [PubMed] [Google Scholar]
- 17.Garden JM, Zelickson B, Friedman D, Kutscher TD, Rozen DM, Afsahi V. Long-term facial and body hair removal with a combined radiofrequency and optical home-use device for all skin types. J Drugs Dermatol. 2020 May;19((5)):498–503. [PubMed] [Google Scholar]
- 18.Sadick NS, Laughlin SA. Effective epilation of white and blond hair using combined radiofrequency and optical energy. J Cosmet Laser Ther. 2004 May;6((1)):27–31. doi: 10.1080/14764170410029022. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg DJ, Marmur ES, Hussain M. Treatment of terminal and vellus non-pigmented hairs with an optical/bipolar radiofrequency energy source-with and without pre-treatment using topical aminolevulinic acid. J Cosmet Laser Ther. 2005 Mar;7((1)):25–28. doi: 10.1080/147641700510037734. [DOI] [PubMed] [Google Scholar]
- 20.Issa MCA, Pires M, Silveira P, Xavier de Brito E, Sasajima C. Transepidermal drug delivery a new treatment option for areata alopecia? J Cosmet Laser Ther. 2015 Feb;17((1)):37–40. doi: 10.3109/14764172.2014.967778. [DOI] [PubMed] [Google Scholar]
- 21.Yu A-J, Luo YJ, Xu XG, Bao LL, Tian T, Li ZX, et al. A pilot split-scalp study of combined fractional radiofrequency microneedling and 5% topical minoxidil in treating male pattern hair loss. Clin Exp Dermatol. 2018 Oct;43((7)):775–781. doi: 10.1111/ced.13551. [DOI] [PubMed] [Google Scholar]
- 22.Verner I, Lotti T. Clinical evaluation of a novel fractional radiofrequency device for hair growth fractional radiofrequency for hair growth stimulation. Dermatol Ther. 2018 May;31((3)):e12590. doi: 10.1111/dth.12590. [DOI] [PubMed] [Google Scholar]
- 23.Tan Y, Wei L, Zhang Y, Goren A, McCoy J, Stanimirovic A, et al. Non-ablative radio frequency for the treatment of androgenetic alopecia. Acta Dermatovenerol Alp Pannonica Adriat. 2019 Dec;28((4)):169–171. [PubMed] [Google Scholar]
- 24.Sadick NS. Combination radiofrequency and light energies electro-optical synergy technology in esthetic medicine. Dermatol Surg. 2005;31((9 Pt 2)):1211–1217. doi: 10.1111/j.1524-4725.2005.31928. discussion 1217. [DOI] [PubMed] [Google Scholar]
- 25.Elsaie ML, Choudhary S, Leiva A, Nouri K. Nonablative radiofrequency for skin rejuvenation. Dermatol Surg. 2010 May;36((5)):577–589. doi: 10.1111/j.1524-4725.2010.01510.x. [DOI] [PubMed] [Google Scholar]
- 26.Lask G, Elman M, Slatkine M, Waldman A, Rozenberg Z. Laser-assisted hair removal by selective photothermolysis. Preliminary results. Dermatol Surg. 1997 Sep;23((9)):737–739. doi: 10.1111/j.1524-4725.1997.tb00406.x. [DOI] [PubMed] [Google Scholar]
- 27.Lorenz S, Brunnberg S, Landthaler M, Hohenleutner U. Hair removal with the long pulsed Nd YAG laser: a prospective study with one year follow-up. Lasers Surg Med. 2002 Feb;30((2)):127–134. doi: 10.1002/lsm.10032. [DOI] [PubMed] [Google Scholar]
- 28.Dierickx C. Laser-assisted hair removal state of the art. Dermatol Ther. 2000 Jan;13((1)):80–89. [Google Scholar]
- 29.Mehta N, Khan E, Gupta S. Radiofrequency epilation using acupuncture needles to decrease the disease burden in hidradenitis suppurativa. Dermatol Surg. 2022 Jul;48((7)):788–789. doi: 10.1097/DSS.0000000000003477. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.