Abstract
Key Clinical Message
It may be possible to extend the use of the robotic arm to pelvic and acetabular surgery leading to safe, repeatable screw placement, and less radiation exposure for patients, surgeons and OR staff.
Abstract
In this case, a novel, robotic‐assisted technique was used to place a sacroiliac screw in a patient with unstable injuries of the pelvic ring. Intraoperative and postoperative fluoroscopic, radiographic, and CT imaging demonstrated a safely positioned 6.5 mm cannulated screw without unplanned cortical violation or impingement on neurovascular structures. To our knowledge, this is the first such reported case using a robot widely available in the Americas or Europe.
Keywords: fracture, pelvis, robot‐assisted, robotic, robotic arm, sacroiliac

1. INTRODUCTION
The use of robotic technology has long been known to be effective in many industries such as manufacturing and automotive industries. The first surgical application of industrial robotic technology was described when an industrial robotic arm was modified to perform a stereotactic brain biopsy with 0.05 mm accuracy. 1 The use of robotic‐assisted technology in surgical applications has expanded since then and has been used successfully in neurologic, cardiac, gynecologic, urologic, and more recently orthopedic surgery. 2 , 3 , 4 , 5 , 6 Robotic‐assisted surgery in the spine has been shown to be effective and safe. 7 Robotic‐assisted surgery in the treatment of traumatic pelvic and acetabular injuries draws parallels to pedicle fixation in that pelvic and acetabular implants are also placed in narrow bony corridors where there is the potential for devastating neurovascular injury. This has traditionally made percutaneous fixation of the pelvis a procedure that requires significant expertise and precise imaging protocols intraoperatively. In some situations, surgery is postponed due to obstruction of imaging by bladder contrast or bowel gas. With the use of robotic‐assisted technology, these issues could be circumvented, and intraoperative robotic arm assistance and real‐time data availability on implant position and trajectory could allow for precise and accurate placement of pelvic fixation. Robotic‐assisted placement of screws into the pelvis has been reported before using the TiRobot (TINAVI Medical Technologies, Beijing, China). 8 To our knowledge, we report the first such case to be performed outside of China using a robotic system and instruments widely available in the Americas and Europe.
2. CASE REPORT
After demonstrating that the ExcelsiusGPS robotic arm (Globus Medical) could be used to place 6.5 mm cannulated screws into the pelvis using cadaveric specimens, a patient was selected for robotic‐assisted percutaneous pelvic fixation. Informed consent was obtained. The patient presented to our Level 1 trauma center in October 2021 with multiple traumatic injuries.
A 57‐year‐old patient sustained a pelvic ring injury with right SI widening and fractures of the ipsilateral right superior and inferior rami and left inferior ramus extending into the left pubis (Figures 1 and 2). Informed consent for robotic‐assisted surgery was obtained.
FIGURE 1.

Preoperative imaging including (A) anteroposterior (B) outlet and (C) inlet radiographs of the pelvis.
FIGURE 2.

Intraoperative CT showing right SI widening the axial (A) and coronal (B) planes.
3. SURGICAL TECHNIQUE
We utilized a “scan and plan” workflow, where the patient was prepared and draped in usual sterile fashion prior to any screw planning with the robot. The post for the patient reference tracking array (called the “dynamic reference base” or DRB) was first anchored to the operative hemipelvis in the iliac crest starting about 5 cm posterior to the anterior superior iliac spine and perpendicular to the floor to allow for visualization of the array by the robotic camera, which was placed at the head of the bed. The surveillance marker was placed in similar fashion on the contralateral hemipelvis. The purpose of the surveillance marker is to guard against loss of robotic registration if the DRB was disturbed (bumped or otherwise moved) inadvertently by an assistant during the case. The “scan and plan” reference array (called the intraoperative CT marker or “ICT”) was then attached to the post for the DRB (Figure 3). The O‐Arm was then positioned around the patient, and AP and lateral fluoroscopy views confirmed that all necessary markers from the arrays would be contained within the spin. Note that an O‐Arm with the capability to perform a 40 cm spin is required for this technique. An O‐Arm spin was then performed, and that data were transferred to the robot. A right‐sided SI screw was planned using a 6.5 mm pedicle screw (Figure 4). The robotic instruments were registered, and robotic registration was confirmed by using a navigated probe placed against bony landmarks.
FIGURE 3.

Clinical setup for robotic screw placement. Reference array (DRB and pin for DRB) on the operative hemipelvis. ICT attached to that array. Surveillance marker on the contralateral hemipelvis to guard against loss of registration.
FIGURE 4.
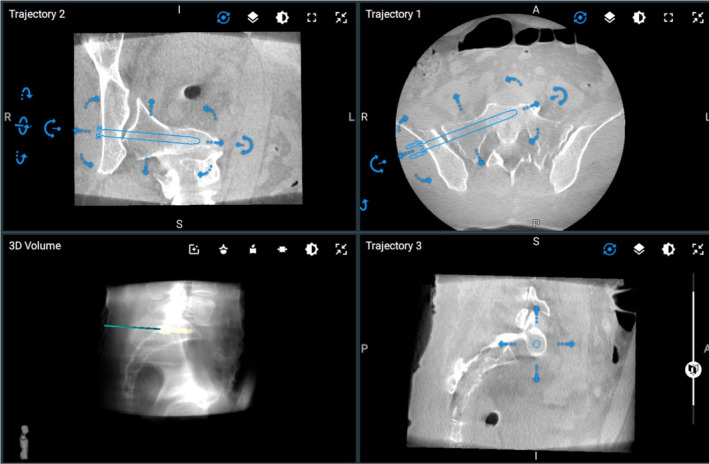
Robotic plan for the SI screw.
The robot was draped in sterile fashion and brought near the surgical field. The surgical arm was brought into position in line with the planned screw trajectory. Robotic instruments were used to incise the skin. Blunt dissection was carried to bone. The robotic burr was used to open the outer cortex of the ilium. A 5.5 mm robotic tap was then placed to the limits of its depth. The tap was removed, and a robotic awl was placed against the bone. The central trocar from the awl was removed, and a 0.9 mm nitinol wire was placed through the awl into the path created by the tap. The wire position was maintained, and the awl as well as the end‐effector from the robot were removed. Using the nitinol wire as a feeler probe bone could be felt circumferentially through the entire course of the tapped bone. The robot was moved away from the surgical field. C‐arm was brought in, and the position of the wire in the bone was confirmed to be as planned. A 6.5 mm partially threaded screw was then placed over the wire under fluoroscopic control, and the wire withdrawn. Post‐procedure CT scan demonstrated placement of the screw exactly as planned (Figure 5).
FIGURE 5.

Axial CT slices of the screw demonstrating appropriate positioning of the right SI screw.
4. DISCUSSION
Robotic‐assisted surgery has been demonstrated to be a safe and effective technique in spine surgery where instrumentation is placed in narrow corridors in close proximity to neurovascular structures. 7 The authors found robotic‐assisted percutaneous fixation appealing in traumatic pelvic injuries where fixation is also placed in narrow corridors of bone while avoiding damage to neurovascular structures such the sacral and L5 nerves and nearby vascular structures such as the superior gluteal artery and its branches. Percutaneous fixation in the pelvis requires detailed knowledge of complex, three‐dimensional pelvic anatomy and its variations and the ability to correlate this 3D anatomy to 2D fluoroscopic imaging. 9 The sacrum is known to have varying anatomy with sacral dysmorphia reported in 44% of patients. 10 These variations in anatomy underscore the importance of accurate and consistent imaging. Quality of c‐arm imaging is affected by several factors outside surgeon control such as the presence of bowel gas, bladder contrast, availability of a skilled c‐arm technician, and large patient body habitus. The use of robotic‐assisted surgery may mitigate some or all of these issues, as intraoperative CT imaging is not constrained by the presence of many of these factors.
Robotic‐assisted surgery for percutaneous fixation of traumatic pelvic injuries is a novel technique that allowed for safe and accurate screw placement in this case. To our knowledge, this is the first reported case in the Americas and Europe of robotic‐assisted surgery for treatment of traumatic pelvic injuries. The patient was in the supine position, which is standard for most surgeons treating these injuries utilizing standard techniques. Further research is needed to demonstrate accuracy of implant placement relative to the preoperative plan.
AUTHOR CONTRIBUTIONS
Austin F Smith: Writing – original draft; writing – review and editing. Jon b Carlson: Conceptualization; methodology; project administration; supervision; writing – review and editing.
FUNDING INFORMATION
None.
CONFLICTS OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
None.
Smith AF, Carlson JB. Robotic‐assisted percutaneous pelvis fixation: A case report. Clin Case Rep. 2023;11:e7527. doi: 10.1002/ccr3.7527
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- 1. Hockstein NG, Gourin CG, Faust RA, Terris DJ. A history of robots: from science fiction to surgical robotics. J Robot Surg. 2007;1(2):113‐118. doi: 10.1007/s11701-007-0021-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zelhart M, Kaiser AM. Robotic versus laparoscopic versus open colorectal surgery: towards defining criteria to the right choice. Surg Endosc. 2018;32(1):24‐38. doi: 10.1007/s00464-017-5796-2 [DOI] [PubMed] [Google Scholar]
- 3. Matthews CA. New developments in robotics and single‐site gynecologic surgery. Clin Obstet Gynecol. 2017;60(2):296‐311. doi: 10.1097/GRF.0000000000000274 [DOI] [PubMed] [Google Scholar]
- 4. Domb BG, Chen JW, Lall AC, Perets I, Maldonado DR. Minimum 5‐year outcomes of robotic‐assisted primary Total hip arthroplasty with a nested comparison against manual primary Total hip arthroplasty: a propensity score‐matched study. J Am Acad Orthop Surg. 2020;28(20):847‐856. doi: 10.5435/JAAOS-D-19-00328 [DOI] [PubMed] [Google Scholar]
- 5. Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic‐arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig‐based total knee arthroplasty: a prospective cohort study. Bone Jt J. 2018;100‐B(7):930‐937. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Smith AF, Eccles CJ, Bhimani SJ, et al. Improved patient satisfaction following robotic‐assisted Total knee arthroplasty. J Knee Surg. 2021;34(7):730‐738. doi: 10.1055/s-0039-1700837 [DOI] [PubMed] [Google Scholar]
- 7. Lieberman IH, Kisinde S, Hesselbacher S. Robotic‐assisted pedicle screw placement during spine surgery. JBJS Essent Surg Tech. 2020;10(2):e0020. doi: 10.2106/JBJS.ST.19.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu HS, Duan SJ, Xin FZ, Zhang Z, Wang XG, Liu SD. Robot‐assisted minimally‐invasive internal fixation of pelvic ring injuries: a single‐center experience. Orthop Surg. 2019;11(1):42‐51. doi: 10.1111/os.12423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miller AN, Routt MLC. Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg. 2012;20(1):8‐16. doi: 10.5435/JAAOS-20-01-008 [DOI] [PubMed] [Google Scholar]
- 10. Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML. Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma. 2010;24(10):622‐629. doi: 10.1097/BOT.0b013e3181cf0404 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.


