Abstract
Objectives
The EPIWATCH artificial intelligence (AI) system scans open-source data using automated technology and can be used to detect early warnings of infectious disease outbreaks. In May 2022, a multicountry outbreak of Mpox in non-endemic countries was confirmed by the World Health Organization. This study aimed to identify signals of fever and rash-like illness using EPIWATCH and, if detected, determine if they represented potential Mpox outbreaks.
Study design
The EPIWATCH AI system was used to detect global signals for syndromes of rash and fever that may have represented a missed diagnosis of Mpox from 1 month prior to the initial case confirmation in the United Kingdom (7 May 2022) to 2 months following.
Methods
Articles were extracted from EPIWATCH and underwent review. A descriptive epidemiologic analysis was conducted to identify reports pertaining to each rash-like illness, locations of each outbreak and report publication dates for the entries from 2022, with 2021 as a control surveillance period.
Results
Reports of rash-like illnesses in 2022 between 1 April and 11 July (n = 656 reports) were higher than in the same period in 2021 (n = 75 reports). The data showed an increase in reports from July 2021 to July 2022, and the Mann–Kendall trend test showed a significant upward trend (P = 0.015). The most frequently reported illness was hand-foot-and-mouth disease, and the country with the most reports was India.
Conclusions
Vast open-source data can be parsed using AI in systems such as EPIWATCH to assist in the early detection of disease outbreaks and monitor global trends.
Keywords: Mpox, Communicable diseases, Emerging, Artificial intelligence, Public health surveillance, Orthopoxvirus
Introduction
Techniques such as social media mining and news media scanning using open-source data have been utilized in public health surveillance for the early detection of new or emerging infectious disease outbreaks.1 , 2 This can be useful in countries with low diagnostic capacity or where censorship (for political reasons, cultural stigma or for fear of impacting tourism) may result in a lack of formal reporting.1 , 2 The EPIWATCH system uses artificial intelligence (AI) to harness open-source data, such as media reports, press releases, official reports and social media, for early epidemic signals and can provide an early warning for emerging infectious disease outbreaks.1, 2, 3 It scans vast, open-source data for diseases and clinical syndromes using two AI subsystems.4
On 7 May 2022, a case of Mpox was confirmed in England by the United Kingdom Health Security Agency (UKHSA) in a person with recent travel history to Nigeria.5 On 21 May 2022, the World Health Organization confirmed a multicountry outbreak of Mpox in 12 non-endemic countries, mostly in Europe, with no established travel links to endemic areas in the African continent, suggesting local transmission.5 As of 29 November 2022, there were more than 81,000 cases with 56 deaths globally in this outbreak, peaking in June 2022, with the majority of cases reported from Europe and the United States (USA).6 As of 29 November 2022, Mpox had spread to 110 countries, of which 103 had not previously reported Mpox.6
Human Mpox was first detected in 1970 in the Democratic Republic of the Congo (DRC), and there have been subsequent epidemics in Central and West Africa, with a significant resurgence of cases in Nigeria and the DRC since 2017.7 The increasing number of infections in previously endemic and non-endemic countries has in part been attributed to the growing number of people without orthopoxvirus immunity due to both the accumulation of unvaccinated people since the smallpox vaccination ceased following eradication in 1980 and waning of immunity from smallpox vaccines, which protect against Mpox.8 , 9
In the 2022 outbreak, the epidemiological situation was further complicated by the atypical presentation of Mpox symptoms compared with previous outbreaks.10 The main feature of Mpox is a vesicular-pustular rash characterized by multiple lesions on the face, hands and feet.9 In a study of more than 500 cases in the current epidemic, while a rash was reported in 97% of cases, 64% of cases had less than 10 lesions, with 10% having only a single lesion.10 The most common sites of the rash were the anogenital region, followed by the trunk, extremities and face.9 , 10 Other presenting features of Mpox include a prodrome of fever, lethargy, headache and lymphadenopathy, which can differentiate Mpox from chickenpox.9 , 10 These clinical features are shared with more common viruses such as varicella, measles, herpes simplex, secondary syphilis and hand-foot-and-mouth disease.11
Many physicians in non-endemic countries have minimal or no experience with Mpox and may misdiagnose it as another rash and fever illness. In a 2022 study of Italian medical professionals, it was shown that there were significant knowledge gaps on all aspects of Mpox infections, including systemic complications, rash distribution and use of vaccination as a preventative measure.12 Another study of university medical students reported that of 11 Mpox knowledge items, only three were correctly identified by more than 70% of respondents and only 26.2% knew that vaccination against Mpox was available.13 Clinical diagnostic errors may also cause misdiagnosis of Mpox cases for other rash-like diseases such as varicella. In Central Africa, Mpox was misdiagnosed as varicella in up to 50% of the confirmed cases.14 Reasons identified for the misdiagnoses include clinician difficulty differentiating between Mpox and other rash-like illnesses, poor laboratory testing capacities especially in low-resource settings, low rates of health seeking behaviour, and test refusal due to social stigma in certain communities.15, 16, 17
International case definitions have primarily focused on people who identify as gay, bisexual or men who have sex with men (MSM), collectively GBMSM, or has had one or more sexual partners in the preceding 21 days.18 Mpox infection can occur in anyone following close physical contact with a person with Mpox, or even clothing and bedding items that have been in contact with lesions.9 , 18 In the 2022 epidemic, there were documented cases in women and children, with at least 83 cases in children recorded in the USA as of 24 September 2022, including 28 children aged 0–12 years.18, 19, 20 Restrictive case definitions may lead to restricted testing and, therefore, under-ascertainment of the extent of the early stages of the 2022 epidemic.18 , 21
Due to the possibility that Mpox may be misdiagnosed as other illnesses with rash and fever and that countries with weak surveillance systems may not have complete ascertainment of Mpox, in this study we aimed to monitor trends in rash-like illnesses using EPIWATCH during the time period prior to, and coinciding with, the MPX outbreak.
Methods
This study involves three parts 1) search of the EPIWATCH early warning system, 2) data extraction and screening and 3) descriptive analysis and time series analysis of the rash-like illnesses reported prior to and during the 2022 Mpox epidemic, which began on 7 May 2022.
The EPIWATCH system
EPIWATCH is a curated open-source, AI-based outbreak observatory that searches vast quantities of media reports, press releases, official reports and social media for early detection of outbreaks of infectious diseases.4 The collected data undergoes human review, with a trained analyst screening the article for outbreak information including disease, syndrome or symptoms of human or zoonotic disease, case numbers, location and date.1 , 2 If outbreak information is validated, a ‘report’ is entered onto the EPIWATCH database.1 , 2 This removes irrelevant articles. EPIWATCH can be used to detect early reports of potential outbreaks through publicly available sources in settings with inadequate or absent disease surveillance.1, 2, 3 The system has been used to collect outbreak data since 2016 and has been further enhanced by AI and machine learning.1 , 2 , 4 Searches can be tailored for specific languages or regions as well as for specific infectious disease syndromes. The EPIWATCH observatory was developed at University of New South Wales Sydney (UNSW) and is managed by staff at the Biosecurity Program, The Kirby Institute, UNSW.4
Search strategy
In consultation with the EPIWATCH team, we considered potential candidates for misdiagnosis of Mpox, namely diseases and syndromes with clinical features of rash-like illness, and used the EPIWATCH system to identify possible trends in the month leading to the first case identified in the United Kingdom and during the ongoing outbreak. Symptom-related terms such as ‘acute fever and rash’, ‘fever of unknown origin’ and a list of differential diagnosis for Mpox inclusive of ‘hand, food and mouth disease (HFMD)’, ‘varicella’, ‘herpes simplex’, ‘measles’, ‘syphilis’, and ‘tomato flu/fever’ were searched. ‘Tomato Flu/Fever’, a term used in India for a rash and fever illness, was also included in this analysis due to lack of case definition at the time and the characteristics of mucocutaneous blisters.22 Table S1 presents the list of the illnesses and their characteristics in the supplementary material. The searches were conducted for the period of 1 April 2022 to 11 July 2022, to capture the period 1 month prior to and 2 months following the first identified case in the United Kingdom of this outbreak.
Data were collected for comparison to the same period in the previous year (1 April 2021 to 11 July 2021) as a comparator. Monthly total reports for rash-like illnesses from the EPIWATCH system were collected for the 43 months from January 2019 to July 2022 for a time-series analysis.
Data extraction and screening process
All articles in non-English languages are autotranslated to English in the EPIWATCH system. These were extracted into a Microsoft Excel spreadsheet and reviewed. There were a total of 2187 reports in the initial search for the 2019–2022 surveillance period. From title screening for relevance, 57 duplicate entries were removed. Articles related to diseases not in the search list were also removed (n = 73).
Data analysis
A descriptive epidemiologic analysis was conducted using Microsoft Excel to identify the number of reports pertaining to each rash-like illness, the locations of each outbreak and time of publication of the reports for the entries from the 2021 (n = 75) and 2022 (n = 656) surveillance periods. The locations were ranked according to the number of associated reports in 2022, and the top eight were selected for further analysis. If the information was available, additional information such as Mpox case numbers, diagnostic capabilities and smallpox vaccination coverage was also included and is presented in Table S2 in the supplementary material.
The percentage increase in the number of reports across the years 2021 and 2022 was compared. A time-series analysis using the Mann–Kendall test using XLSTAT software23 was used to detect the changes in trend from reports of rash-like illnesses from January 2019 to July 2022. IBM SPSS Statistics, Version 22, was used,24 and to identify if the change was significant, a P-value of 0.05 was applied.
Results
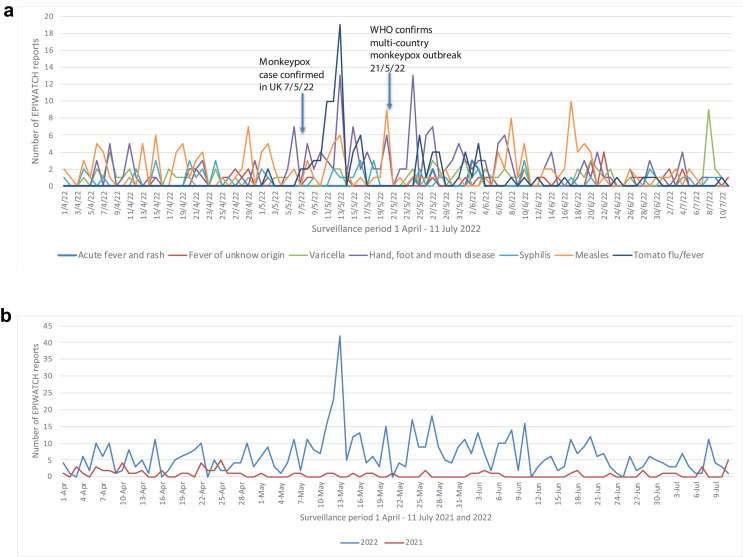
There were 656 reports of rash and fever illness made between the dates 1 April 2022 and 11 July 2022, which were included in the analysis. Results from the surveillance period are shown in Fig. 1 a, with Fig. 1b comparing the total number of reports with the previous year (2021) over the same time period for comparison (n = 75).
Fig. 1.
a. Global reports of a rash-like illness over the 2022 surveillance time period (1 April to 11 July 2022). b. Comparison of global reports of a rash-like illnesses over the surveillance time period (1 April to 11 July 2022 and 2021).
For each search term, the number of reports were as follows: HFMD (n = 191), varicella (n = 84), herpes simplex (n = 0), measles (n = 175), syphilis (n = 56), acute rash and fever (n = 8), fever of unknown origin (n = 47) and tomato flu/fever (n = 96).
The number of reports per country for the 2022 surveillance period and per search term for the 2021 and 2022 surveillance period are included in Tables S3–5 in the supplementary material. The geographical distribution of reports made during the surveillance period is demonstrated in Fig. 2 . Table 1 summarises information related to the Mpox outbreak status of the top eight countries ranked by report.
Fig. 2.
Geographical distribution of reports during the surveillance period (1 April to 11 July 2022). Note – circles denote regional clusters, blue pins are single locations/cases. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article).
Table 1.
Top eight countries (by number of EPIWATCH reports collected during surveillance period) and confirmed Mpox cases as of 30 November 2022.
| Country | EPIWATCH reports 1/4–11/7/22 | MPX confirmed cases 30/11 |
|---|---|---|
| India | 181 | 17 |
| Malaysia | 135 | 0 |
| USA | 31 | 29,325 |
| Japan | 30 | 7 |
| Brazil | 26 | 9905 |
| Afghanistan | 23 | 0 |
| Indonesia | 16 | 1 |
| Ukraine | 16 | 5 |
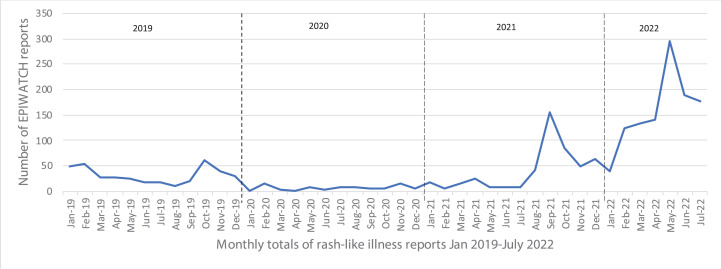
Reports were analysed from the EPIWATCH system from January 2019 to July 2022. Fig. 3 presents the variation in reports per month for rash-like illnesses over this time period. The data showed an increase in reports from July 2021 to July 2022, and the Mann–Kendall trend test showed a significant upward trend (P = 0.015).
Fig. 3.
A time series analysis of total monthly reports for rash-like illness extracted from the EPIWATCH system January 2019–July 2022.
Discussion
The number of reports about rash-like illnesses in 2022 between 1 April and 11 July (n = 656 reports) was much higher (775% increase) than the same time period in 2021 (n = 75 reports). The observed peak in reports of rash-like illnesses in 2022 occurred between 6 May and 13 May 2022 coinciding with the early reports of cases of Mpox in the United Kingdom in the current outbreak. HFMD was the most frequently reported diagnosis, of which there were multiple ongoing outbreaks in Malaysia at the time, with 32 times more cases reported compared to the same period the previous year.25 India had the most reports, ranging from ‘tomato flu/fever’, a colloquial term for the rash associated with dengue, HFMD or other illnesses with fever and rash,22 a varicella outbreak, and reports of ‘fever of unknown origin’. The majority of reports collected in the EPIWATCH system for rash-like illnesses were in Asia (India = 181, Malaysia = 135), and not in the countries of Europe and North America (USA = 31) where there was documented widespread transmission of Mpox. Subsequent reporting of Mpox cases in India total 17 as 29 November 2022.6 However, diagnostic capability is higher in the USA and Europe, and it is possible in low- and middle-income countries that Mpox was misdiagnosed.
Inadequate diagnostic capability in low resource settings has been identified as a factor which may lead to underreporting or misdiagnosis,21 , 26 and testing capacity was low in several of the countries in our analysis (see Table S3). However, there has also been a lack of testing in high-income countries, potentially due to restricted case definitions, lack of knowledge by primary health care providers leading to misdiagnosis, and stigma around the disease.26 The majority of Mpox cases in the current outbreak have been identified in MSM.18 , 21 International case definitions have defined a probable Mpox case as anyone with an unexplained rash or lesion(s) and has either a recent epidemiological link to a probable case of Mpox, or identifies as a MSM, or has had one or more new sexual partners in the 21 days before symptom onset.18 , 27 This case definition may exclude women and children who had no travel history or contact with confirmed infection, and may lead to misdiagnosis.18 , 19
The 2022 Mpox epidemic peaked in the middle of 2022 and has since waned.
While the signals for rash-like illnesses did not correspond to the countries experiencing the highest burden of the Mpox epidemic, we were looking for signals in low-income countries where surveillance may not be as complete and timely as in the high-income countries that were affected by Mpox in 2022. Clinicians may be unfamiliar with symptoms of orthopoxvirus infections; therefore, the signal we demonstrated can be used to prompt a formal investigation for Mpox and other rash and fever illnesses.
Advances in synthetic biology make it possible that orthopoxviruses could be used as bioweapons.28 , 29 A system like EPIWATCH can be used to monitor for a sudden increase in rash and fever presentations, or any other clinical syndrome, as an early warning of an outbreak and a trigger for timely investigation.
This study includes several limitations. The EPIWATCH system is designed to observe an early-warning signal of a potential infectious disease outbreak through the use of syndromic surveillance; therefore, the data that are collected do not represent case numbers or an epidemic curve but report about a syndrome or disease. There is almost certainly reporting bias due to increasing media awareness leading to increased reports rather than actual increase in disease occurrence. Open-source data are not validated and are not intended to replace traditional diagnostics or surveillance but to be a trigger for more timely investigation of potential epidemics. Early identification of epidemics results in a more feasible prospect of containment. A strength of our methodology is that open-source intelligence can overcome weak surveillance systems. The EPIWATCH system uses AI to scan vast quantities of open-source data continuously for diseases and syndromes in 52 languages, which could not be processed manually due to the volume of data. Outbreak signals are reviewed and collated in a weekly digest by a group of trained analysts. The online dashboard is publicly available and updated in real time.
Conclusion
Considering the overlapping clinical characteristics within the case definitions of Mpox, hand-foot-and-mouth disease and varicella, it is possible that Mpox and other orthopoxviruses may be misdiagnosed as another viral illness, particularly in countries with low diagnostic capacities in poor resource settings. Open-source intelligence can be used to monitor for outbreaks of fever and rash-like illnesses, especially in countries without widespread testing capacity. The utility of open-source data from syndromic surveillance systems such as EPIWATCH could be used in early warning of emerging outbreaks and to inform international public health responses, such as increasing testing capacities and directing resources and investigations to resource-poor settings to curb the spread of infectious diseases with epidemic potential.
Author statements
Ethical approval
Not applicable.
Funding
The study was supported by the Balvi Filantropic Fund. C. Raina MacIntyre is supported by a NHMRC Principal Research Fellowship, grant no. 1137582.
Competing interests
All authors declare that they have no conflicts of interest.
Author contributions
Danielle Hutchinson: writing – original draft, review & editing, conceptualization, methodology and formal analysis. Mohana Kunasekaran: methodology, formal analysis and writing - review & editing. Ashley Quigley: methodology and writing - review & editing. Aye Moa: formal analysis and writing - review & editing. C. Raina MacIntyre: supervision, writing - review & editing and conceptualization.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2023.05.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.MacIntyre C.R., Chen X., Kunasekaran M., Quigley A., Lim S., Stone H., et al. Artificial intelligence in public health: the potential of epidemic early warning systems. J Int Med Res. 2023;51(3) doi: 10.1177/03000605231159335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacIntyre C.R., Lim S., Quigley A. Preventing the next pandemic: use of artificial intelligence for epidemic monitoring and alerts. Cell Rep Med. 2022;3(12) doi: 10.1016/j.xcrm.2022.100867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puca C., Trent M. Using the surveillance tool EpiWATCH to rapidly detect global mumps outbreaks. Global Biosecurity. 2020;2(1) None. [Google Scholar]
- 4.EPIWATCH - About: EPIWATCH. 2022. https://www.epiwatch.org/ [updated 2022]. Available from: [Google Scholar]
- 5.Multi-country monkeypox outbreak in non-endemic countries: World Health Organization. 2022. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385 [updated 21 May 2022]. Available from: [Google Scholar]
- 6.2022 monkeypox outbreak global map: centers for disease control and prevention. 2022. https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html [updated 29 November 2022]. Available from: [Google Scholar]
- 7.Monkeypox - key facts: World health organization. 2022. https://www.who.int/news-room/fact-sheets/detail/monkeypox [updated 19 May 2022]. Available from: [Google Scholar]
- 8.Nguyen P.Y., Ajisegiri W.S., Costantino V., Chughtai A.A., MacIntyre C.R. Reemergence of human monkeypox and declining population immunity in the context of urbanization, Nigeria, 2017-2020. Emerg Infect Dis. 2021;27(4):1007–1014. doi: 10.3201/eid2704.203569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poland G.A., Kennedy R.B., Tosh P.K. Prevention of monkeypox with vaccines: a rapid review. Lancet Infect Dis. 2022;22(12):e349–e358. doi: 10.1016/S1473-3099(22)00574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thornhill J.P., Barkati S., Walmsley S., Rockstroh J., Antinori A., Harrison L.B., et al. Monkeypox virus infection in humans across 16 countries — April–June 2022. N Engl J Med. 2022;388:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 11.MacIntyre C.R. 2022. Monkeypox is not a global emergency for now, says WHO. 3 things we need to know next about how it's mutating and spreading: the Conversation.https://theconversation.com/monkeypox-is-not-a-global-emergency-for-now-says-who-3-things-we-need-to-know-next-about-how-its-mutating-and-spreading-185297 [updated 26 June 2022]. Available from: [Google Scholar]
- 12.Riccò M., Ferraro P., Camisa V., Satta E., Zaniboni A., Ranzieri S., et al. When a neglected tropical disease goes global: knowledge, attitudes and practices of Italian physicians towards monkeypox, preliminary results. Trop Med Infect Dis. 2022;7(7) doi: 10.3390/tropicalmed7070135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sallam M., Al-Mahzoum K., Dardas L., Al-Tammemi A., Al-Salahat K., Bakri F., et al. Updated: knowledge of human monkeypox and its relation to conspiracy beliefs among students in Jordanian health schools: filling the knowledge gap on emerging zoonotic viruses. Medicina (Kaunas, Lithuania) 2022;58:924. doi: 10.3390/medicina58070924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer H., Perrichot M., Stemmler M., Emmerich P., Schmitz H., Varaine F., et al. Outbreaks of disease suspected of being due to human monkeypox virus infection in the democratic Republic of Congo in 2001. J Clin Microbiol. 2002;40(8):2919–2921. doi: 10.1128/JCM.40.8.2919-2921.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lederman E.R., Reynolds M.G., Karem K., Braden Z., Learned-Orozco L.A., Wassa-Wassa D., et al. Prevalence of Antibodies against orthopoxviruses among residents of likouala region, republic of Congo: evidence for monkeypox virus exposure. Am J Trop Med Hyg. 2007;77(6):1150–1156. [PubMed] [Google Scholar]
- 16.Bragazzi N.L., Khamisy-Farah R., Tsigalou C., Mahroum N., Converti M. Attaching a stigma to the LGBTQI+ community should be avoided during the monkeypox epidemic. J Med Virol. 2022;95:e27913. doi: 10.1002/jmv.27913. [DOI] [PubMed] [Google Scholar]
- 17.Fleischauer A.T., Kile J.C., Davidson M., Fischer M., Karem K.L., Teclaw R., et al. Evaluation of human-to-human transmission of monkeypox from infected patients to health care workers. Clin Infect Dis. 2005;40(5):689–694. doi: 10.1086/427805. [DOI] [PubMed] [Google Scholar]
- 18.Thornhill J.P., Palich R., Ghosn J., Walmsley S., Moschese D., Cortes C.P., et al. Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series. Lancet. 2022;400(10367):1953–1965. doi: 10.1016/S0140-6736(22)02187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan D., Sze S., Nazareth J., Martin C.A., Al-Oraibi A., Baggaley R.F., et al. Monkeypox in the UK: arguments for a broader case definition. Lancet. 2022;399(10344):2345–2346. doi: 10.1016/S0140-6736(22)01101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hennessee I., Shelus V., McArdle C.E., Wolf M., Schatzman S., Carpenter A., et al. Epidemiologic and clinical features of children and Adolescents aged <18 Years with monkeypox - United States, May 17–September 24, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(44):1407–1411. doi: 10.15585/mmwr.mm7144a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joi P. Gavi - The Vaccine Alliance; 2022. What is behind the sudden international spread of monkeypox?https://www.gavi.org/vaccineswork/what-behind-sudden-international-spread-monkeypox?gclid=CjwKCAjwlqOXBhBqEiwA-hhitJpoT8G4QDDRLMCcv6x1-VxqODMT1MsASFo9Mt9yjzXSoTV9FzZJ3xoCIt4QAvD_BwE [updated 25 May 2022]. Available from: [Google Scholar]
- 22.Tomato flu: Narayana health. 2022. https://www.narayanahealth.org/blog/tomato-flu/#:∼:text=The%20blisters%20start%20as%20red,irritation%20and%20severe%20dehydration%20issues.&text=The%20symptoms%20of%20tomato%20flu%20are%20similar%20to%20chikungunya%20or%20dengue%20infection [updated 19 May 2022]. Available from: [Google Scholar]
- 23.XLSTAT 2018 . Addinsoft; Paris, France: 2017. Data analysis and statistical solution for Microsoft Excel. [Google Scholar]
- 24.IBM SPSS Statistics for windows, version 220. IBM Corp.; Armonk, NY: 2013. [Google Scholar]
- 25.Malaysia reports 32-fold increase in hand, foot and mouth disease in 2022. Outbreak News Today; 2022. http://outbreaknewstoday.com/malaysia-reports-32-fold-increase-in-hand-foot-and-mouth-disease-in-2022/ [updated 7 June 2022]. Available from: [Google Scholar]
- 26.Cohen E. 2022. Testing is crucial to getting monkeypox under control, but there's a 'shocking' lack of demand: CNN.https://edition.cnn.com/2022/07/28/health/monkeypox-testing-demand/index.html [updated 1 August 2022]. Available from: [Google Scholar]
- 27.Monkeypox: case definitions. UK Health Security Agency; 2022. https://www.gov.uk/guidance/monkeypox-case-definitions#:∼:text=A%20highly%20probable%20case%20is,remains%20the%20most%20likely%20diagnosis [updated 25 July 2022]. Available from: [Google Scholar]
- 28.Courtney-Guy S. The Metro; 2022. Russia ‘planned to use monkeypox as a bioweapon’, report warned.https://metro.co.uk/2022/05/20/russia-planned-to-use-monkeypox-as-a-bioweapon-report-warned-16680912/ [updated 20 May 2022]. Available from: [Google Scholar]
- 29.MacIntyre C.R. Reevaluating the risk of smallpox reemergence. Mil Med. 2020;185(7–8):e952–e957. doi: 10.1093/milmed/usaa084. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.