Key Teaching Points.
-
•
Cardioneuroablation can be considered as an alternative to pacing in selected patients with swallow syncope that are refractory to conservative management.
-
•
The sites and extent of ablation depend on the type of cardioinhibitory response (asystole vs atrioventricular block), although a complete vagal denervation involving both atria probably offers the best chances of clinical success.
-
•
Zero-fluoroscopy is a feasible approach for cardioneuroablation that minimizes the effects of radiation exposure for patients and health care staff.
Introduction
Swallow syncope is a rare type of reflex syncope.1,2 Its pathophysiology is probably related to the stimulation of neural pathways that cause vagal hyperactivation generating syncope secondary to a combination of severe bradyarrhythmias and hypotension.2 Diet modifications and pacemaker implant (when conservative management fails) have been the cornerstones of swallow syncope treatment.
In recent years, cardioneuroablation (CNA) has emerged as a novel therapeutic strategy for several forms of functional bradyarrhythmias.3, 4, 5, 6 We present a case of confirmed swallow-induced syncope that was successfully treated with CNA as an alternative to permanent pacing.
Case report
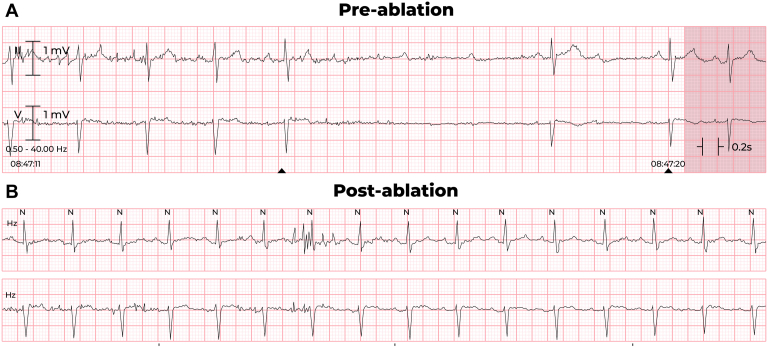
A 61-year-old female patient without known cardiac comorbidities presented with a >5-year history of dizzy spells and facial flushing provoked by swallowing solid foods. The symptoms were initially attributed to menopause; however, they did not subside over time, and despite modification of her eating habits and diet, she developed recurrent episodes of syncope. A Holter monitor was requested and evidenced multiple episodes of high-degree atrioventricular (AV) block, with pauses lasting up to 7 seconds (Figure 1), all related to eating. The episodes were not associated with change in the sinus rate or significant PR prolongation preceding the AV block (Figure 2A). The patient was admitted to the hospital for cardiac workup and monitoring. Her resting electrocardiogram was normal, a transthoracic echocardiogram showed no structural abnormalities, and cardiac magnetic resonance imaging ruled out infiltrative diseases. Full-body contrast computed tomography and gastrointestinal endoscopic studies were also unremarkable. While she was in the hospital, her symptoms and conduction abnormalities were easily reproducible by ingestion of bread or other solid foods (Figure 2A).
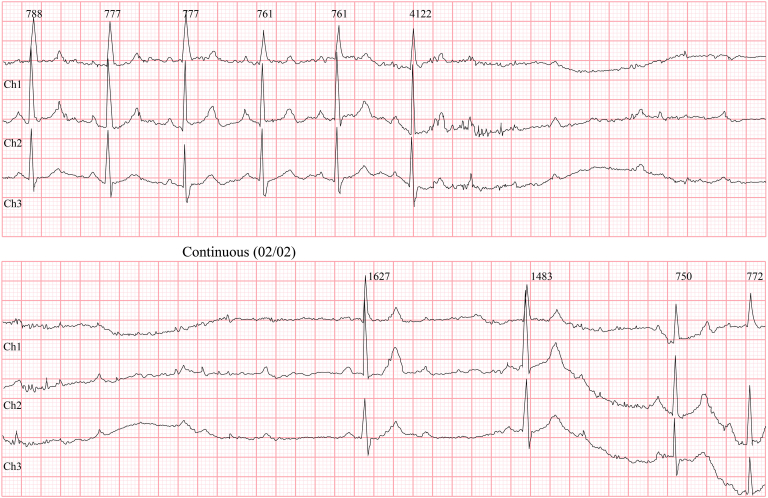
Figure 1.
Holter monitor rhythm strips showing episodes of high-degree atrioventricular block while the patient was eating.
Figure 2.
“Sandwich test”: A: preablation; B: postablation.
Implantation of a dual-chamber pacemaker was considered; however, the possibility of CNA was also discussed as a novel off-label treatment and the patient opted for this strategy. The ablation procedure was performed under general anesthesia using a nonfluoroscopic approach, guided by electroanatomic mapping (EnSite X; Abbott, St Paul, MN) and intracardiac echocardiography. A fast anatomical map of the right and left atria was created using an Advisor HD Grid catheter (Abbott) and the location of the ganglionated plexi (GPs) was determined by anatomical reference and fractionation mapping.7 Using an ablation catheter with contact force capability (TactiCath; Abbott), radiofrequency energy (30 W) was applied at GP sites, with particular focus on the posteromedial left GP (PMLGP), which was targeted from the left atrium and the ostium of the coronary sinus on the right side (Figure 3). At the end of the ablation procedure, the patient’s heart rate was 88 beats/min (from 44 beats/min at baseline), the PR interval was 165 ms (from 175 ms at baseline), and the Wenckebach point was 390 ms (from 490 ms at baseline). In addition, no significant heart rate response was observed with the administration of intravenous atropine (2 mg), although no preablation atropine test was available for comparison.
Figure 3.
Fractionation maps and ablation lesions delivered in the different ganglionated plexi areas in the right and left atrium.
Postablation, the patient was monitored in hospital for 24 hours with no recurrence of bradyarrhythmias, and a “sandwich challenge test” was negative for symptoms or electrocardiographic changes (Figure 2B). She was discharged the next day with instructions to complete 1 month of oral anticoagulation. At the 3-month follow-up, the patient remained completely asymptomatic on a normal diet, and no episodes of AV block were registered on a 72-hour Holter.
Discussion
Swallow syncope has been described in 0.3% of patients with recurrent syncope.8,9 Up to one-third of patients with swallow syncope may exhibit concurrent extracardiac pathologies mainly affecting the gastrointestinal system, which need to be excluded. As illustrated in this case, patients usually have a lengthy period of symptoms, and their manifestations are often attributed to other conditions.10 Permanent pacing is used in 55% of cases with syncope and reduces the rate of recurrent syncope by 98%.10
CNA has emerged as an alternative therapeutic option to treat cardioinhibitory vasovagal syncope and functional (vagally mediated) forms of AV block, with experience from different groups reporting promising short- and long-term outcomes.3, 4, 5, 6 Different approaches have been used to guide CNA, including intracardiac or extracardiac high-frequency stimulation, spectral mapping, mapping of fractionated electrograms, or purely anatomical guidance. The selection of what GPs should be targeted during ablation depends on the clinical scenario and the specific type of cardioinhibitory response. Anatomical studies have shown that most of the parasympathetic input to the sinoatrial node depends mainly on postganglionic fibers originating from the superior right atrial GP, while the AV node is mainly supplied by fibers originating from the PMLGP and Marshall tract GP.11 Thus, the superior right atrial GP should be the primary target in sinus bradyarrhythmias and the PMLGP in case of functional AV block. In our case, syncope was associated with a selective cardioinhibitory effect on the AV node, without concomitant sinus bradycardia. Although this may cast doubts sometimes about the true functional nature of the AV block, the consistent relationship with food ingestion in this patient supported a reflex mechanism.
A previous case of swallow syncope successfully treated with CNA has been previously published.12 The main difference with our case is that the mechanism of syncope was sinus arrest instead of AV block, and ablation was limited to the right atrium, at its junction with the SVC. In our case, biatrial ablation was performed, considering that significant overlap exists between GPs and ablation of the PMLGP may not be sufficient to denervate the AV node completely in some patients. A meta-analysis by Vandenberk and colleagues13 demonstrated that ablation in both atria increases the time free of syncope in patients undergoing CNA for vasovagal syncope.
Further studies involving more patients and longer follow-ups are necessary to adopt CNA as a standard therapy in this and other types of reflex syncope. Considering the promising evidence and obvious advantages over permanent pacing, it is likely that CNA may become a first-line therapy in the future.
Footnotes
Funding Sources: This research received no external funding.
Disclosures: All authors declare no conflict of interest.
References
- 1.Shen W.K., Sheldon R.S., Benditt D.G., et al. 2017 ACC/AHA/HRS Guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017;136:e60–e122. doi: 10.1161/CIR.0000000000000499. [DOI] [PubMed] [Google Scholar]
- 2.Dani M., Dirksen A., Taraborrelli P., et al. “be careful what you swallow”: a case series of swallow syncope. JACC Case Rep. 2021;3:469–473. doi: 10.1016/j.jaccas.2020.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aksu T., Golcuk E., Yalin K., Guler T.E., Erden I. Simplified cardioneuroablation in the treatment of reflex syncope, functional AV block, and sinus node dysfunction. Pacing Clin Electrophysiol. 2016;39:42–53. doi: 10.1111/pace.12756. [DOI] [PubMed] [Google Scholar]
- 4.Aksu T., Gopinathannair R., Bozyel S., Yalin K., Gupta D. Cardioneuroablation for treatment of atrioventricular block. Circ Arrhythm Electrophysiol. 2021;14 doi: 10.1161/CIRCEP.121.010018. [DOI] [PubMed] [Google Scholar]
- 5.Pachon J.C., Pachon E.I., Pachon J.C., et al. “Cardioneuroablation”--new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace. 2005;7:1–13. doi: 10.1016/j.eupc.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Yao Y., Shi R., Wong T., et al. Endocardial autonomic denervation of the left atrium to treat vasovagal syncope: an early experience in humans. Circ Arrhythm Electrophysiol. 2012;5:279–286. doi: 10.1161/CIRCEP.111.966465. [DOI] [PubMed] [Google Scholar]
- 7.Aksu T., Yalin K., Gopinathannair R. Fractionation mapping software to map ganglionated plexus sites during sinus rhythm. J Cardiovasc Electrophysiol. 2020;31:3326–3329. doi: 10.1111/jce.14753. [DOI] [PubMed] [Google Scholar]
- 8.Endean E.D., Cavatassi W., Hansler J., Sorial E. Deglutition syncope: a manifestation of vagal hyperactivity following carotid endarterectomy. J Vasc Surg. 2010;52:720–722. doi: 10.1016/j.jvs.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 9.Mathias C.J., Deguchi K., Schatz I. Observations on recurrent syncope and presyncope in 641 patients. Lancet. 2001;357:348–353. doi: 10.1016/S0140-6736(00)03642-4. [DOI] [PubMed] [Google Scholar]
- 10.Siew K.S.W., Tan M.P., Hilmi I.N., Loch A. Swallow syncope: a case report and review of literature. BMC Cardiovasc Disord. 2019;19:191. doi: 10.1186/s12872-019-1174-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aksu T., Yalin K., Bozyel S., Gopinathannair R., Gupta D. The anatomical basis behind the neuromodulation effects associated with pulmonary vein isolation. J Cardiovasc Electrophysiol. 2021;32:1733–1736. doi: 10.1111/jce.15038. [DOI] [PubMed] [Google Scholar]
- 12.Stiavnicky P., Wichterle D., Hrosova M., Kautzner J. Cardioneuroablation for the treatment of recurrent swallow syncope. Europace. 2020;22:1741. doi: 10.1093/europace/euaa060. [DOI] [PubMed] [Google Scholar]
- 13.Vandenberk B., Lei L.Y., Ballantyne B., et al. Cardioneuroablation for vasovagal syncope: A systematic review and meta-analysis. Heart Rhythm. 2022;S1547-5271(22):02088. doi: 10.1016/j.hrthm.2022.06.017. 4. [DOI] [PubMed] [Google Scholar]