Abstract
One of the most common osseous abnormalities associated with patellar instability and patellofemoral osteochondral disease is patella alta, characterized by an Insall–Salvati ratio ≥1.2 or a Caton–Deschamps Index ≥1.2. Despite being the most common surgical treatment option for patella alta, tibial tubercle osteotomy with distalization raises concerns due to the complete detachment of the tubercle, which may lead to damage of local vascularity from periosteal detachment and increased mechanical stress at the attachment site. These factors are related to greater risk of complications, such as fractures, loss of fixation, delayed union, or nonunion of the tuberosity. We describe a technique for tibial tubercle osteotomy with distalization that aims to minimize these complications through care with the osteotomy, stabilization, bone cut thickness, and local periosteum.
Technique Video
This video shows the steps of the tibial tubercle osteotomy with distalization procedure performed on a cadaveric specimen of a left knee.
Patellar instability is a condition caused by soft-tissue abnormalities, limb malalignment, or osseous abnormalities.1,2 One of the most common osseous abnormalities associated with patellar instability is patella alta, characterized by an Insall–Salvati ratio (the ratio of the patellar tendon length to the maximum length of the patella) ≥1.2 or a Caton–Deschamps Index (CDI) ≥1.2.3,4 The CDI is the ratio of the length between the anterior angle of the tibial plateau to the most inferior aspect of the patellar articular surface to the length of the patellar articular surface.4 Patella alta is a form of patellofemoral malalignment that alters knee extensor mechanics, elevating the stress on the patellofemoral joint, and is associated with increased articular cartilage degeneration.5,6
There is a lack of consensus in the surgical management of patients with recurrent patellar instability or patellofemoral cartilage lesions associated with patella alta. Various proximal and distal procedures have been used, for example, medial patellofemoral ligament reconstruction, patellar tendon imbrication, and tibial tubercle osteotomy (TTO) with distalization.7 TTO with distalization is the most common surgical treatment option for patella alta.8, 9, 10 Despite evidence that suggests TTO with distalization leads to good radiographic, clinical, and functional outcomes, concerns about the risk of osseous complications with procedures involving complete detachment of the distal tuberosity remain, including fractures of the proximal tibia, loss of tibial tuberosity fixation, and delayed union or nonunion of the tuberosity.8, 9, 10, 11, 12, 13, 14, 15 We propose a distalizating TTO technique for the correction of patella alta that aims to minimize these complications through the creation of a V-shaped osteotomy, tubercle stabilization, and periosteum repair.
Surgical Technique (With Video Illustration)
The patient is placed in the supine position. A 5-cm anterolateral incision is made from the lateral aspect of the patellar tendon distally. A bovie is used to release the periosteum lateral and medial to the tubercle. The patellar tendon insertion is elevated to locate the proximal aspect of the tubercle. The periosteum is cut 4 cm distally to the patellar tendon insertion (Figs 1 and 2), and a periosteal elevator is used to peel the periosteum distally to 6 cm (Fig 3). A V-cut is made both medially and laterally at 45°, creating a 6-cm bone fragment. In the sagittal plane, the cut is inclined around 20° to 30° anteriorly from proximal to distal (Fig 4). A transverse cut is then performed in the proximal part of the tubercle (Fig 5). The cuts are first made using an oscillating saw, then completed with an osteotome. A V-shaped wedge is withdrawn from the distal portion of the osteotomized bone after cuts at 5 and 6 cm (Fig 6A). The tibial tubercle shingle is moved distally and a 8- to 10-mm allograft Evans wedge (MTF Biologics, Edison, NJ) is cut to fit into the proximal aspect of the osteotomy (Fig 6B) and tamped into the proximal aspect of the osteotomy, creating a bony buttress (Fig 7). The amount of distalization is determined by the CDI, with the goal of 1.0 to 1.1. In most cases, this means the tubercle is moved 8 to 10 mm and the size of the Evans wedge is defined accordingly.
Fig 1.
Shown is an anterior view of the left knee. The tibial tubercle is measured distal to the patellar tendon insertion.
Fig 2.
Shown is an anterior view of the left knee. The tibial tubercle is marked at 4 cm distally to patellar tendon insertion.
Fig 3.
Shown is an anterior view of the left knee. The periosteum is peeled back from 4 to 6 cm using a scalpel and periosteal elevator.
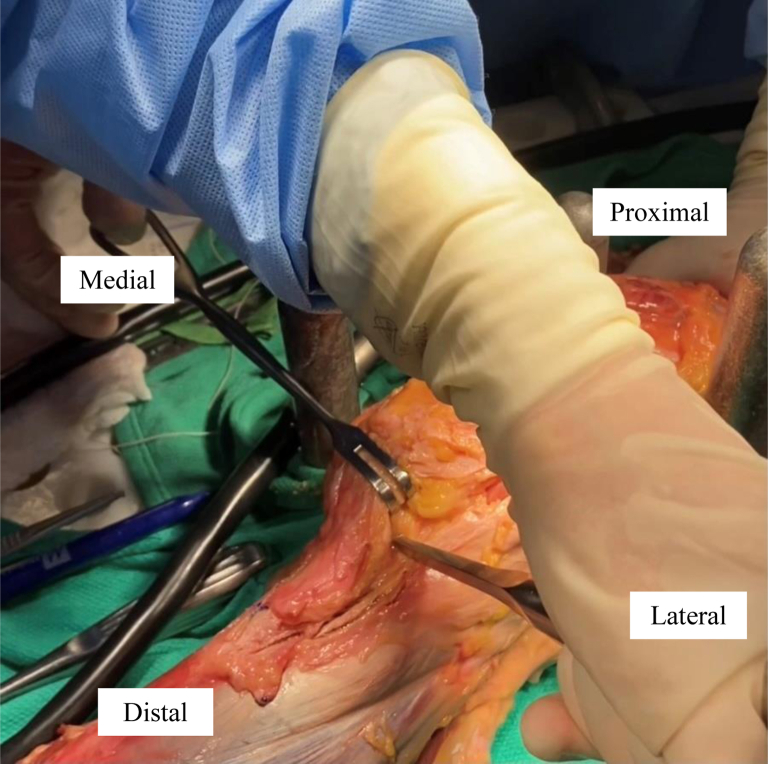
Fig 4.
Shown is an anterior view of the left knee. A 45° V-shaped cut is performed with an oscillating saw blade both medially and laterally. In the sagittal plane, the cut is inclined around 20° to 30° anteriorly from proximal to distal.
Fig 5.
Shown is an anterior view of the left knee. The patellar tendon insertion is retracted. A transverse cut is made proximal to the patellar tendon insertion using an osteotome after the initial cut is made with a saw blade.
Fig 6.
(A) Shown is a V-shaped wedge, which is the result of the chevron osteotomy after making cuts at 5 and 6 cm. (B) Shown is a 10-mm Evans wedge, which is marked to match the proximal aspect of the shingle and fit into the defect.
Fig 7.
Shown is an anterior view of the left knee. An Evans wedge is placed into the proximal aspect of the osteotomy.
The tibial tubercle is reduced in a good fit to the distal region of the cut (Fig 8) and secured with two 4.5-mm self-tapping cortical bone screws (DePuy Synthes, Warsaw, IN) using a lag technique aiming distally through the tibial tubercle (Fig 9). Fluoroscopy is used to confirm the screw length. The periosteum is repaired with VICRYL (Ethicon, Somerville, NJ) sutures covering the distal part of the wedge (Fig 10). The incision is then closed in a layered fashion. The skin is closed deeply with absorbable sutures, followed by a running MONOCRYL stitch (Ethicon) and Steri-Strips (3M, St. Paul, MN) (Fig 11 and Video 1).
Fig 8.
Shown is a medial view of the left knee. The distal aspect of the shingle is fit to the distal region of the cut.
Fig 9.
Shown is an anterior view of the left knee. The tubercle is fixated with two 4.5-mm cortical lag screws aiming distally.
Fig 10.
Shown is ananterior view of the left knee. The periosteum is brought back across to be repaired with VICRYL sutures, covering the distal portion of the tubercle.
Fig 11.
Shown are lateral radiographs of the right knee from a 19-year-old female patient with patella alta and patellar instability who was indicated for tibial tubercle osteotomy with distalization. (A) Shown is a lateral view of the right knee preoperatively, highlighting a Caton–Deschamps Index of 1.32. (B) Shown is a lateral view of the right knee 3 months’ postoperatively. The Caton–Deschamps Index has decreased to 0.91. The screws and the Evans wedge are well-positioned providing stabilization for the distalized tubercle. (C) Shown is a lateral view of the right knee 8 months’ postoperatively after screw removal showing full osseous integration. The Caton–Deschamps index remains 0.91.
Discussion
Without surgical intervention, recurrent patellar instability secondary to patella alta often results in degenerative changes of the articular cartilage, patellofemoral maltracking, and/or anterior knee pain. Thus, surgical intervention for patients with patella alta who experience instability and/or cartilage damage is recommended. A systematic review conducted by Tan et al.7 that evaluated outcomes between proximal, distal, and combined proximal/distal procedures for management of patellofemoral instability with patella alta determined that distal procedures alone allowed for better correction of patellar height in comparison with proximal procedures alone. However, complete detachment of the tibial tubercle during distalization TTOs poses a much greater risk of nonunion and tibial fracture compared with other TTO techniques, such as Elmslie–Trillat or Fulkerson.14 It has been suggested that this detachment of the tubercle may lead to damage of local vascularity due to periosteal detachment and increased mechanical stress at the attachment site of the transferred tubercle.14,16 Our technique aims to reduce these risks, improve the efficacy of distalization procedures in correcting patellar height, and minimize the risk of subsequent surgeries.
First, the creation of a V-shaped osteotomy promotes better bone healing as a result of the larger contact area created. Since the distal hinge of the osteotomy is violated to transfer the tubercle distally, care is taken to re-establish maximum distal contact. A V-shaped wedge is withdrawn from the distal portion of the osteotomized bone, allowing a good fit of the same to the distal region of the cut at the time of fixation. Periosteum is cautiously dissected from the tibia where the distal portion of the cut would be. This allows coverage of the distal portion of the transferred tubercle after fixation, recreating an environment of periosteal vascularization. Furthermore, stability of the bone fragment is critical for its consolidation. The use of 2 bicortical screws aiming distally achieves stabilization of the shingle to promote healing.17 Placing an Evans wedge between the fragment and the transverse proximal cut adds mechanical stability to the construct by preventing shifting of the transferred tubercle. To further reduce the risk of fracture, an oscillating saw is used in combination with an osteotome to make precise cuts and avoid unwanted extension of the osteotomy.14 In addition, the osteotomized fragment cannot be too thin, as this would increase the risk of fracture and decrease the amount of bone available for healing.18 In addition to distalization, some studies suggest that anteriorization of the tubercle unloads the patellofemoral joint, especially in cases of established cartilage lesions in patients with tibial tubercle positioned posteriorly in relation to trochlear groove.19, 20, 21 The anteriorly-inclined cut from proximal to distal in the sagittal plane is then performed to promote a slight anteriorization of the shingle as it is shifted distally. In addition, part of the removed wedge can be positioned posterior to the shingle to provide further anteriorization (Tables 1 and 2).
Table 1.
Advantages and Disadvantages of Tibial Tubercle Osteotomy With Distalization
| Advantages | Disadvantages |
|---|---|
| Correction of patellar height | Detachment of the distal hinge |
| Anteriorization of the tubercle | Risk of tubercle fracture |
| Periosteum repair promotes vascularity | Painful hardware |
| Additional stability through the Evans wedge | |
| Greater surface area created through the V-shaped cut |
Table 2.
Pearls and Pitfalls of Tibial Tubercle Osteotomy With Distalization
| Pearls | Pitfalls |
|---|---|
| Aim distally for optimal screw fixation | Distal screws can cut out laterally if you are not careful |
| Have both 4.5-mm and 3.5-mm fully threaded screws available as well as washers, as shingles may be small | Avoid debridement as fat pad scarring can occur |
| Avoid neurovascular bundle posteriorly |
Conclusions
The described technique for TTO with distalization is an effective treatment of patella alta and associated patellar instability and addresses the risk factors associated with TTO procedures.
Footnotes
A.G. reports other from Organogenesis, Bioventus, and Vericel, outside the submitted work. S.S. reports other from Smith & Nephew and Vericel, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows the steps of the tibial tubercle osteotomy with distalization procedure performed on a cadaveric specimen of a left knee.
References
- 1.Tan S.H.S., Ibrahim M.M., Lee Z.J., Chee Y.K.M., Hui J.H. Patellar tracking should be taken into account when measuring radiographic parameters for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2018;26:3593–3600. doi: 10.1007/s00167-017-4795-0. [DOI] [PubMed] [Google Scholar]
- 2.Colvin A.C., West R.V. Patellar instability. J Bone Joint Surg Am. 2008;90:2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 3.Insall J., Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 4.Caton J. Method of measuring the height of the patella. Acta Orthop Belg. 1989;55:385–386. [PubMed] [Google Scholar]
- 5.Heino Brechter J., Powers C.M. Patellofemoral stress during walking in persons with and without patellofemoral pain. Med Sci Sports Exerc. 2002;34:1582–1593. doi: 10.1097/00005768-200210000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Ward S.R., Terk M.R., Powers C.M. Influence of patella alta on knee extensor mechanics. J Biomech. 2005;38:2415–2422. doi: 10.1016/j.jbiomech.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Tan S.H.S., Ngiam E.H.K., Lim J.Y., Lim A.K.S., Hui J.H. Surgical management of patella alta in patellofemoral instability: A systematic review and meta-analysis. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967121999642. 2325967121999642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caton J.H., Dejour D. Tibial tubercle osteotomy in patella–femoral instability and in patellar height abnormality. Int Orthop. 2010;34:305–309. doi: 10.1007/s00264-009-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knapik D.M., Kunze K.N., Azua E., Vadhera A., Yanke A.B., Chahla J. Radiographic and clinical outcomes after tibial tubercle osteotomy for the treatment of patella alta: A systematic review and meta-analysis. Am J Sports Med. 2022;50:2042–2051. doi: 10.1177/03635465211012371. [DOI] [PubMed] [Google Scholar]
- 10.Gardner E.C., Molho D.A., Fulkerson J.P. Coronal malalignment—when and how to perform a tibial tubercle osteotomy. Clin Sports Med. 2022;41:15–26. doi: 10.1016/j.csm.2021.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Leite C.B.G., Santos T.P., Giglio P.N., Pécora J.R., Camanho G.L., Gobbi R.G. Tibial tubercle osteotomy with distalization is a safe and effective procedure for patients with patella alta and patellar instability. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967120975101. 2325967120975101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mayer C., Magnussen R.A., Servien E., et al. Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta. Am J Sports Med. 2012;40:346–351. doi: 10.1177/0363546511427117. [DOI] [PubMed] [Google Scholar]
- 13.Harrison R.K., Magnussen R.A., Flanigan D.C. Avoiding complications in patellofemoral surgery. Sports Med Arthrosc Rev. 2013;21:121–128. doi: 10.1097/JSA.0b013e31828e88a2. [DOI] [PubMed] [Google Scholar]
- 14.Payne J., Rimmke N., Schmitt L.C., Flanigan D.C., Magnussen R.A. The incidence of complications of tibial tubercle osteotomy: A systematic review. Arthroscopy. 2015;31:1819–1825. doi: 10.1016/j.arthro.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 15.Johnson A.A., Wolfe E.L., Mintz D.N., Demehri S., Shubin Stein B.E., Cosgarea A.J. Complications after tibial tuberosity osteotomy: Association with screw size and concomitant distalization. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118803614. 2325967118803614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanamiya T., Naito M., Ikari N., Hara M. The effect of surgical dissections on blood flow to the tibial tubercle. J Orthop Res. 2001;19:113–116. doi: 10.1016/S0736-0266(00)00009-7. [DOI] [PubMed] [Google Scholar]
- 17.Tompkins M., Arendt E.A. Complications in patellofemoral surgery. Sports Med Arthrosc Rev. 2012;20:187–193. doi: 10.1097/JSA.0b013e31825c74cf. [DOI] [PubMed] [Google Scholar]
- 18.Servien E., Archbold P. In: Surgery of the knee. Neyret P., Demey G., editors. Springer; London: 2014. Episodic patellar dislocation; pp. 305–326. [Google Scholar]
- 19.Lansdown D.A., Christian D., Madden B., et al. The sagittal tibial tubercle-trochlear groove distance as a measurement of sagittal imbalance in patients with symptomatic patellofemoral chondral lesions. Cartilage. 2021;13:449S–455S. doi: 10.1177/1947603519900802. (1_suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Temperato J., Nuelle C.W. Tibial tubercle osteotomy with anteriorization and distalization for treatment of patellar instability with patella alta. Arthrosc Tech. 2022;11:e1045–e1051. doi: 10.1016/j.eats.2022.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koh J., Jones T., Elias J.J. Tibia tubercle distalization reduces contact pressures in patella alta and instability. Arthroscopy. 2021;37:82–83. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows the steps of the tibial tubercle osteotomy with distalization procedure performed on a cadaveric specimen of a left knee.
This video shows the steps of the tibial tubercle osteotomy with distalization procedure performed on a cadaveric specimen of a left knee.