Abstract
With an increased appreciation of the importance an intact meniscus has on normal knee kinematics and function, more meniscal tears are being treated with a repair rather than partial meniscectomy. There are several techniques for repairing torn meniscal tissue, including the outside-in, inside-out, and all-inside repairs. Each technique comes with its advantages and drawbacks. The inside-out and outside-in techniques allow for greater control of the repair using knots outside the joint capsule; however, they pose a risk for neurovascular injury and require additional incisions. Arthroscopic all-inside repairs have seen increasing popularity, but with current techniques, fixation is achieved either with intra-articular knots or extra-articular implants, leading to variable outcomes and the potential for postoperative complications. This technical note describes the use of SuperBall, an all-inside meniscus repair device that provides an all-arthroscopic approach, no intraarticular knots or implants, and surgeon-guided tensioning of the meniscus repair.
Technique Video
Tear of the right lateral meniscus posterior horn repaired with the SuperBall repair device. Right leg is placed in figure-four position, and tear is visualized with an arthroscope via the lateral portal. The Superball depth limiter is adjusted to 16 mm and inserted into medial portal. Red safety button depressed and delivery needle are lowered to desired depth. The first suture bundle is deployed at desired location using the system trigger. Needle is repositioned to the second location for suture bundle, and trigger is pressed until hard stop is felt. Device is then repeatedly triggered until sufficient tension is achieved, and meniscal tear is reduced. Red suture cutting button is depressed, and the blue Superball pusher is retracted to rear position and pushed back down to initial position to deploy Superball suture tail on the peripheral side of the meniscus. The green actuating suture is gently pulled to secure repair, the device is removed, and the suture is cut flush with meniscus. The 2nd SuperBall device is used a few millimeters posterior to the first.
Introduction
In recent years, evidence has accumulated that meniscus repair may be a superior option to full or partial meniscectomy in the treatment of symptomatic meniscal tears, primarily because of the preservation of native tissue and a decreased risk of early-onset osteoarthritis.1, 2, 3 This is of particular importance in younger patient populations for whom the prevention of progressive arthrosis is essential, and meniscus repair has been associated with favorable clinical outcomes.4 Furthermore, although controversy remains as to whether meniscal tears in the red-white zone are better suited to repair versus excision, several long-term outcome studies have demonstrated satisfactory results of meniscus repair in the red-white zone comparable to repairs of the red-red zone.3,5,6 Thus, meniscus repair may have broader applicability in the treatment of meniscal pathology than was previously indicated.
Despite these apparent benefits, a major drawback of meniscus repair compared to partial meniscectomy is its higher rate of reoperations. Reoperation rates for partial meniscectomies range from 1.4 to 3.9%, while rates for isolated meniscal repairs range from 16.5 to 20.7%.3 In fact, one meta-analysis found that 64% of repairs failed within 2 years of the index surgery.7 Aside from the location of repair (medial vs lateral meniscus) (Fig 1) and concomitant anterior cruciate ligament reconstruction (ACLR), repair technique is also a significant predictive factor for repair failure.8 Westermann et al. found that in the setting of ACLR and concomitant meniscal repairs, all-inside techniques had a significantly higher failure rate than inside-out techniques; most of these were secondary to device migration or implant irritation.8,9 These findings highlight the need for novel instruments and approaches for performing meniscus repair to help curb reoperation rates and improve long-term outcomes.
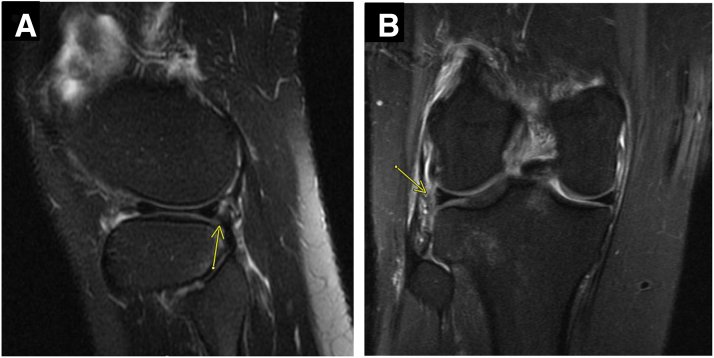
Fig 1.
(A) Sagittal view of magnetic resonance image showing a vertical tear of the peripheral right posterior horn lateral meniscus (yellow arrow) (B) Coronal view of MRI showing the peripheral vertical right lateral meniscus tear (yellow arrow).
Arthroscopic meniscal repair can be achieved using the inside-out, outside-in, or the all-inside technique.10 Each technique has its advantages and disadvantages (Table 1). Historically, inside-out repair with vertical mattress sutures was considered the gold-standard technique for managing meniscal tears in the red-red and red-white zones.11 Inside-out repairs are typically considered versatile for many tear patterns and allow the surgeon to secure the repair sutures via knots tied under direct visualization with greater tension control.12 However, as new devices have been introduced, allowing for an all-arthroscopic repair without the need for additional surgical incisions, the inside-out technique using zone-specific cannulas has become less commonly used.
Table 1.
Advantages and Disadvantages of the Technique
| Advantages | Disadvantages |
|---|---|
| Lack of intra-articular components lowers risk of cartilage damage or knot loosening | Deployment of suture cutting button, pusher, and actuating suture is difficult to achieve without assistance |
| Able to achieve secure reduction without buttons in extracapsular space | |
| Arthroscopic tensioning avoids risk of injury to neurovascular structures by limiting additional incisions |
Outside-in techniques are less commonly used and often reserved for mid-body or anterior third meniscal tears. This technique involves introducing two spinal needles through the capsule and into the joint to shuttle sutures across the site of the meniscal tear. A small skin incision is made, and the sutures are tied to the capsule to secure the repair of the meniscus. This technique has been favorable in treating meniscal tears due to the small incisions, low risk of neurovascular injuries, and high success rates.13
All-inside devices have used arrows, anchors, intra-articular knots, and buttons to achieve fixation of the repair.14 All-inside repairs are faster, less technically demanding, and minimally invasive with a lower risk of injury to the posterior neurovascular structures.15 Despite these advantages, intra-articular knots can loosen, and extracapsular anchors can cause irritation and synovitis or end up in the intra-articular space. This technical note presents a technique for meniscal repair using the SuperBall Meniscal Repair System (Arcuro Medical, Naples, FL) that provides an arthroscopic all-inside repair without the use of intra-articular knots and the ability to tension the suture as desired to achieve a stable, anatomic reduction.
Surgical Technique (Lateral Meniscus Repair)
Positioning, Diagnostic Arthroscopy, and Lesion Preparation
The patient is positioned supine on a standard operating room table with the leg in a leg holder and the foot of the bed dropped. A diagnostic arthroscopy is always performed using standard inferolateral and inferomedial arthroscopic portals. The arthroscope is inserted into the joint, and the suprapatellar space is visualized. The arthroscope is then directed to visualize the articular surfaces of the patella and the trochlea, followed by the lateral gutter and medial gutter, looking for intra-articular loose bodies. The arthroscope is then directed toward the lateral compartment, where the peripheral tear of the posterior horn of the lateral meniscus was visualized. The tear was examined using an arthroscopic probe and found to be unstable. A meniscal rasp and arthroscopic motorized shaver were introduced through the inferomedial portal and used to prepare the lesion site, creating a bleeding bed for tissue repair and healing.
Meniscal Repair
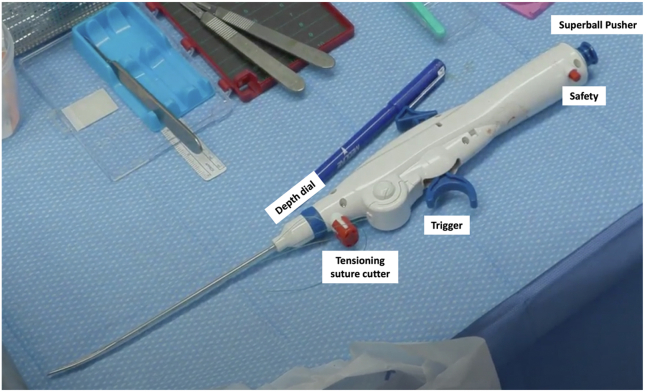
After preparing the tear site and identifying the pattern and extent of the meniscal tear (Fig 2), the Superball device’s depth limiter is adjusted by rotating the blue dial on the device and aligning the desired depth with the arrow on the superior aspect of the device. In this case, a depth of 16 mm was used (Figs 3 and 4).
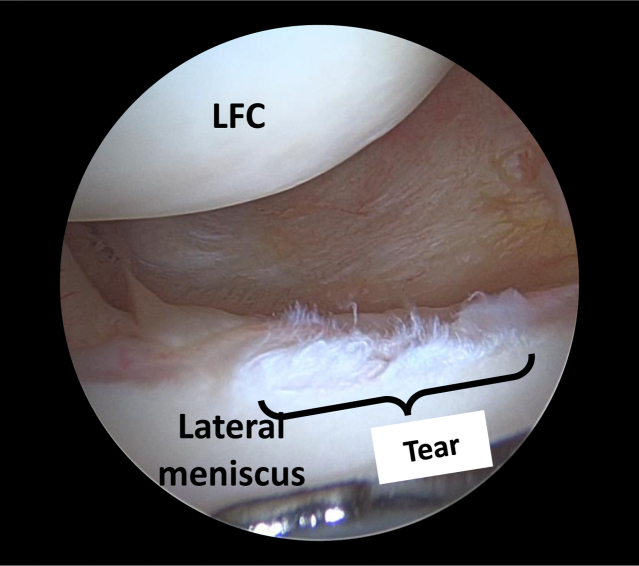
Fig 2.
Arthroscopic view of the patient’s right lateral meniscus inferiorly and lateral femoral condyle superiorly, with the arthroscope in the lateral portal and the arthroscopic probe in the medial portal. The right knee is kept in the figure of four position to visualize the tear. LFC, lateral femoral condyle.
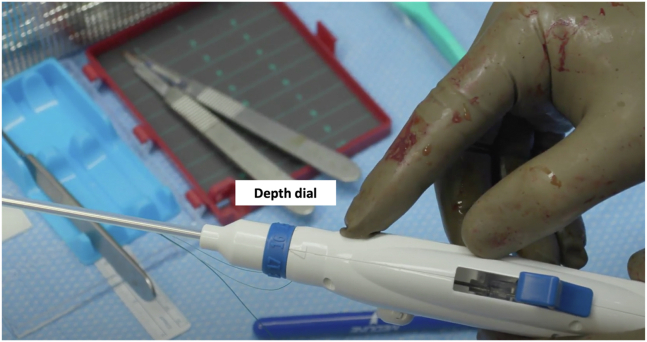
Fig 3.
Image showing Superball device set to the predetermined depth of 16 mm.
Fig 4.
Superball device.
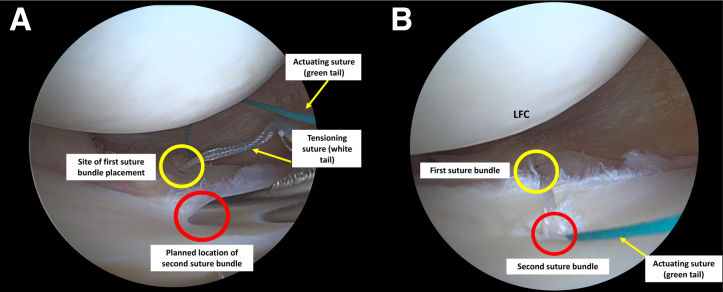
With the arthroscope in the inferolateral portal and a valgus force applied to the knee, the SuperBall device is inserted into the inferomedial portal protected by a skid. The red safety button on the back of the device is then depressed, making it ready for use. Once the stitch configuration is determined, the device’s tip is brought to the desired site on the meniscus/capsule and penetrated to the predetermined depth. Pulling back on the trigger deploys the first suture bundle behind the posterior capsule. The device is then brought out of the tissue and inserted into the second desired location. Pulling the trigger again deploys the second suture bundle. In horizontal mattress repair configurations, the bundle closest to the arthroscope should be deployed first; in vertical mattress configurations, the superior bundle should be deployed first. Once the second suture bundle is deployed, the stitch can be tensioned by activating the trigger back and forth, typically 3-4 times (Figs 4 and 5) (Video 1).
Fig 5.
Arthroscopic view of the right knee placed in figure of four positioning (A) Arthroscopic view from the lateral portal of the SuperBall device (inserted in the medial portal) and the deployed first suture bundle behind the posterior capsule (yellow circle). SuperBall device tip is placed at the location where the second suture bundle will be deployed (red circle). (B) Arthroscopic view (from the lateral portal) of the actuating suture (green tail in panel B) after the second suture bundle has been placed and tensioning (white tail in panel A) suture has been cut.
Once ideal tension is achieved, the tensioning suture can be cut and retracted by pressing the red tension suture cutter button (Fig 4). Although maintaining the device in the same position, the needle can be retracted into the delivery system, and the Superball tail is deployed using the SuperBall pusher. This step can be completed with the help of an assistant. The actuating suture (green tail) is then gently pulled to create the SuperBall and secure the stitch (Fig 5). At this point, the device can be safely removed from the joint space. Using a suture cutter, the surgeon can cut the actuating suture flush with the meniscus to complete the repair. Depending on the tear pattern and size, further additional SuperBall implants can be placed in multiple configurations on both the superior and inferior surfaces of the meniscus to achieve a balanced repair and stable fixation. In the setting of an isolated meniscus repair, microfracture awls are used in the intercondylar notch for marrow venting.16
Rehabilitation
Following arthroscopic meniscus repair, patients are made non-weightbearing for the first postoperative week with the impacted knee in a hinged knee brace locked in full extension. At their initial postoperative office visit, the hinged knee brace is unlocked from 0 to 90°, and their weightbearing is advanced. Patients will begin formal physical therapy working on their knee range of motion and quadriceps strength. At the 4-week postoperative office visit, the hinged knee brace is completely unlocked. The brace is discontinued at 6 weeks postoperatively, and patients begin to use the stationary bicycle and elliptical. Patients will continue with their formal physical therapy with the goal of full, symmetric knee range of motion by 8-10 weeks postoperatively. Return to athletic activity is permitted between 4 and 6 months postoperatively if full knee range of motion and adequate quadriceps and hamstring strength have returned (90% of the contralateral side). The surgeon discusses with the patient whether a functional unloader brace should be used during high-intensity contact athletics to protect the repair site.
Discussion
There are various methods for repairing meniscal tears, including inside-out, outside-in, and all-inside techniques. The main advantage of inside-out repair is the ability to tie extracapsular knots and tension the repair, as desired; however, this technique can be time-consuming, requires additional incisions, and poses a risk of neurovascular injury.17,18 All-inside repairs are faster and minimally invasive, but the different fixation methods come with unique risks.19,20
Early all-inside meniscal repair devices relied heavily upon arrows, screws, and staples to achieve fixation of the meniscus to the articular capsule. However, these devices had high rates of complications like synovitis and chondral injury and were quickly replaced by all-suture devices with intraarticular knots. While these intracapsular repairs led to less irritation and chondral injury, they have been found to be prone to migration and repair loosening.21 Meanwhile, extracapsular anchors and buttons are thought to cause synovial irritation and pain in addition to the potential that they become intra-articular.21 Some all-inside devices have been found to cause larger meniscal microtears than inside-out devices.22 Despite the risks posed by each repair technique, no differences have been found in failure rates or patient-reported outcomes between all-inside and inside-out techniques.23 Surgeons may use either technique depending on the tear’s size, location, and etiology.24 Many prefer all-inside repair for posterior horn tears to avoid damaging the neurovascular structures in the posterior aspect of the knee. In contrast, others prefer inside-out repairs for large, displaced bucket handle tears to achieve a more secure reduction of the meniscal fragment.
The Superball meniscus repair device provides an arthroscopic all-inside suture repair without intra-articular knots or extracapsular implants. The lack of intra-articular components eliminates the risk of knot loosening or cartilage damage. The suture bundles and SuperBall-locking mechanism are designed to deploy in the extracapsular space, which allows for a secure reduction without the need for buttons, which are known to cause irritation.
In contrast to other all-inside techniques, the SuperBall tensioning mechanism allows the surgeon to tension the stitch arthroscopically until reduction is achieved. This allows for greater control without additional incisions for needle retrieval and knot tying, which have been associated with an increased risk of injury to posterior neurovascular structures. As is the case with many novel devices, the usage of the SuperBall device can benefit from knowledge of pearls and pitfalls (Table 2). Noted below, optimal results can be achieved with specific surgical techniques involving suture placement, multiple utilizations of the triggers, and incorporation of assistance. Although the clinical data are limited, the SuperBall device promises the ease and minimally invasive benefits of all-inside repair, with the tension control of an inside-out repair.
Table 2.
Pearls and Pitfalls of the Technique
| Pearls |
| First place superior suture and follow with the inferior pass to allow for direct visualization of the repair suture and its tensioning to ensure the tear site is adequately reduced. |
| It will often take 3-5 utilizations of the trigger to get enough tension |
| Pitfalls |
| Low threshold to pie crust the MCL |
| Assistant needs to feel the click of buttons before releasing |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.J.S. reports royalties from Jaypee Publishing; consulting fees for Vericel, Subchondral Solutions, Smith & Nephew, Organogenesis, Joint Restoration Foundation, Flexion Therapeutics, Fidia, and Arthrex; speaker fees from Smith & Nephew, Arthrex, and Vericel; holds stocks or stock options in Better PT; research support from Cartiheal, Fidia, and Organogenesis; financial or material support from Jaypee Publishing Financial and Springer. He also reports committee membership in the AAOS, American Orthopaedic Association, and Arthroscopy Association of North America, and he serves on the editorial or governing board of Cartilage, Bulletin of the Hospital for Joint Diseases. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Tear of the right lateral meniscus posterior horn repaired with the SuperBall repair device. Right leg is placed in figure-four position, and tear is visualized with an arthroscope via the lateral portal. The Superball depth limiter is adjusted to 16 mm and inserted into medial portal. Red safety button depressed and delivery needle are lowered to desired depth. The first suture bundle is deployed at desired location using the system trigger. Needle is repositioned to the second location for suture bundle, and trigger is pressed until hard stop is felt. Device is then repeatedly triggered until sufficient tension is achieved, and meniscal tear is reduced. Red suture cutting button is depressed, and the blue Superball pusher is retracted to rear position and pushed back down to initial position to deploy Superball suture tail on the peripheral side of the meniscus. The green actuating suture is gently pulled to secure repair, the device is removed, and the suture is cut flush with meniscus. The 2nd SuperBall device is used a few millimeters posterior to the first.
References
- 1.Lee W.Q., Gan J.Z., Lie D.T.T. Save the meniscus—Clinical outcomes of meniscectomy versus meniscal repair. J Orthop Surg (Hong Kong) 2019;27 doi: 10.1177/2309499019849813. [DOI] [PubMed] [Google Scholar]
- 2.Lutz C., Dalmay F., Ehkirch F.P., et al. Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res. 2015;101:S327–S331. doi: 10.1016/j.otsr.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Paxton E.S., Stock M.V., Brophy R.H. Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 4.Yang B.W., Liotta E.S., Paschos N. Outcomes of meniscus repair in children and adolescents. Curr Rev Musculoskel Med. 2019;12:233–238. doi: 10.1007/s12178-019-09554-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaufils P., Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103:S237–S244. doi: 10.1016/j.otsr.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Weber J., Koch M., Angele P., Zellner J. The role of meniscal repair for prevention of early onset of osteoarthritis. J Exp Orthop. 2018;5:10. doi: 10.1186/s40634-018-0122-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schweizer C., Hanreich C., Tscholl P.M., et al. Nineteen percent of meniscus repairs are being revised and failures frequently occur after the second postoperative year: A systematic review and meta-analysis with a minimum follow-up of 5 years. Knee Surg Sports Traumatol Arthrosc. 2022;30:2267–2276. doi: 10.1007/s00167-021-06770-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westermann R.W., Duchman K.R., Amendola A., Glass N., Wolf B.R. All-inside versus inside-out meniscal repair with concurrent anterior cruciate ligament reconstruction: A meta-regression analysis. Am J Sports Med. 2017;45:719–724. doi: 10.1177/0363546516642220. [DOI] [PubMed] [Google Scholar]
- 9.Wilmes P., Lorbach O., Brogard P., Seil R. [Complications with all-inside devices used in reconstructive meniscal surgery] Orthopade. 2008;37:1088–1089. doi: 10.1007/s00132-008-1307-4. 1091-1085, 1097-1088. [DOI] [PubMed] [Google Scholar]
- 10.Marigi E.M., Till S.E., Wasserburger J.N., Reinholz A.K., Krych A.J., Stuart M.J. Inside-out approach to meniscus repair: Still the gold standard? Curr Rev Musculoskel Med. 2022;15:244–251. doi: 10.1007/s12178-022-09764-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marigi E.M., Kennon J.C., Dholakia R., et al. Cost analysis and complication rate comparing open, mini-open, and all arthroscopic rotator cuff repair. JSES Rev Rep Tech. 2021;1:84–89. doi: 10.1016/j.xrrt.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Youn G.M., Van Gogh A.M.R., Mirvish A.B., Chakrabarti M.O., McGahan P.J., Chen J.L. Inside-out bucket-handle meniscus repair with a single-handed self-advancing zone-specific meniscus repair device. Arthrosc Tech. 2019;9:e117–e121. doi: 10.1016/j.eats.2019.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chahla J., Gannon J., Moatshe G., LaPrade R.F. In: The menisci: A comprehensive review of their anatomy, biomechanical function and surgical treatment. LaPrade R.F., Arendt E.A., Getgood A., Faucett S.C., editors. Springer; Berlin, Germany: 2017. Outside-in meniscal repair: Technique and outcomes; pp. 129–135. [Google Scholar]
- 14.Malinowski K., Góralczyk A., Hermanowicz K., LaPrade R.F. Tips and pearls for all-inside medial meniscus repair. Arthrosc Tech. 2019;8:e131–e139. doi: 10.1016/j.eats.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golz A.G., Mandelbaum B., Pace J.L. All-inside meniscus repair. Curr Rev Musculoskelet Med. 2022;15:252–258. doi: 10.1007/s12178-022-09766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freedman K.B., Nho S.J., Cole B.J. Marrow stimulating technique to augment meniscus repair. Arthroscopy. 2003;19:794–798. doi: 10.1016/s0749-8063(03)00695-9. [DOI] [PubMed] [Google Scholar]
- 17.Cuéllar A., Cuéllar R., Díaz Heredia J., Cuéllar A., García-Alonso I., Ruiz-Ibán M.A. The all-inside meniscal repair technique has less risk of injury to the lateral geniculate artery than the inside-out repair technique when suturing the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2018;26:793–798. doi: 10.1007/s00167-017-4490-1. [DOI] [PubMed] [Google Scholar]
- 18.Malinowski K., Ebisz M., Góralczyk A., LaPrade R.F., Hermanowicz K. You can repair more tears than you think—Tricks for all-inside lateral meniscal repair with nonabsorbable sutures. Arthrosc Tech. 2020;9:e979–e986. doi: 10.1016/j.eats.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bogunovic L., Kruse L.M., Haas A.K., Huston L.J., Wright R.W. Outcome of all-inside second-generation meniscal repair: Minimum five-year follow-up. J Bone Joint Surg Am. 2014;96:1303–1307. doi: 10.2106/JBJS.M.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grant J.A., Wilde J., Miller B.S., Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40:459–468. doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 21.Tachibana Y., Sakaguchi K., Goto T., Oda H., Yamazaki K., Iida S. Repair integrity evaluated by second-look arthroscopy after arthroscopic meniscal repair with the FasT-Fix during anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38:965–971. doi: 10.1177/0363546509356977. [DOI] [PubMed] [Google Scholar]
- 22.Dibartola A., Calafiore D., Everhart J., Kaeding C., Magnussen R., Flanigan D. Implant associated meniscus micro-tears: imaging human cadaveric menisci. Arthroscopy. 2021;37:e5. [Google Scholar]
- 23.Fillingham Y.A., Riboh J.C., Erickson B.J., Bach B.R., Jr., Yanke A.B. Inside-out versus all-inside repair of isolated meniscal tears: An updated systematic review. Am J Sports Med. 2017;45:234–242. doi: 10.1177/0363546516632504. [DOI] [PubMed] [Google Scholar]
- 24.Pace J.L., Inclan P.M., Matava M.J. Inside-out medial meniscal repair: Improved surgical exposure with a sub-semimembranosus aproach. Arthrosc Tech. 2021;10:e507–e517. doi: 10.1016/j.eats.2020.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tear of the right lateral meniscus posterior horn repaired with the SuperBall repair device. Right leg is placed in figure-four position, and tear is visualized with an arthroscope via the lateral portal. The Superball depth limiter is adjusted to 16 mm and inserted into medial portal. Red safety button depressed and delivery needle are lowered to desired depth. The first suture bundle is deployed at desired location using the system trigger. Needle is repositioned to the second location for suture bundle, and trigger is pressed until hard stop is felt. Device is then repeatedly triggered until sufficient tension is achieved, and meniscal tear is reduced. Red suture cutting button is depressed, and the blue Superball pusher is retracted to rear position and pushed back down to initial position to deploy Superball suture tail on the peripheral side of the meniscus. The green actuating suture is gently pulled to secure repair, the device is removed, and the suture is cut flush with meniscus. The 2nd SuperBall device is used a few millimeters posterior to the first.
Tear of the right lateral meniscus posterior horn repaired with the SuperBall repair device. Right leg is placed in figure-four position, and tear is visualized with an arthroscope via the lateral portal. The Superball depth limiter is adjusted to 16 mm and inserted into medial portal. Red safety button depressed and delivery needle are lowered to desired depth. The first suture bundle is deployed at desired location using the system trigger. Needle is repositioned to the second location for suture bundle, and trigger is pressed until hard stop is felt. Device is then repeatedly triggered until sufficient tension is achieved, and meniscal tear is reduced. Red suture cutting button is depressed, and the blue Superball pusher is retracted to rear position and pushed back down to initial position to deploy Superball suture tail on the peripheral side of the meniscus. The green actuating suture is gently pulled to secure repair, the device is removed, and the suture is cut flush with meniscus. The 2nd SuperBall device is used a few millimeters posterior to the first.