Abstract
The posterior cruciate ligament (PCL) is the largest and strongest ligament of the knee, with a tremendous role as the primary posterior stabilizer of the knee. Surgical management of PCL injuries is very demanding, due to the fact that the PCL tear usually is a part of multiligamentous knee injury. Moreover, PCL anatomy, especially its course and attachment points to femur and tibia, makes reconstruction of the PCL technically challenging. The main pitfall is the sharp angle between created during reconstruction surgery bony tunnels, which forms so called “killer turn”. The authors present a technique of the remnant-preserving PCL arthroscopic reconstruction that simplifies the procedure and uses the method of reverse passage of the PCL graft to overcome the killer turn.
Technique Video
Arthroscopic remnant preserving PCL reconstruction with reverse passage of the graft. The left knee is being operated on. In the beginning, PCL injury is confirmed. Autograft is prepared from semitendinosus and gracilis tendon, which are quadrupled, and is strengthened using Hi-Fi Tape. Suture disc is implemented on the femoral end of the graft. With the knee in 90° flexion and visualization through anteromedial portal, the femoral PCL insertion point is dissected until the footprint is exposed. The guide pin introduced through anterolateral portal is drilled with a free-hand technique through the center of the footprint, and an incision is made above its exit point of the medial femoral condyle (MFC). The tunnel in medial femoral condyle is drilled using drill size matched to the obtained graft diameter. The posteromedial portal is created under visualization through the anterolateral portal. The arthroscopic cannula is used to facilitate tools maneuvering. The PCL tibial insertion site is located and dissected using a radiofrequency probe until the PCL footprint is being exposed. With an eyelet pin, the looped surgical thread is passed between anterolateral portal and the exit point of the medial femoral condyle tunnel. The tibial tunnel drill-guide is inserted through anteromedial portal and passed between the thread inserted previously through the femoral tunnel. The arthroscope is switched to the posteromedial portal and the tibial tunnel drill-guide is placed on the center of the natural tibial PCL footprint. The tibial tunnel is drilled with a drill matched to the graft size. The next step is passing the suture loop through tibial and femoral tunnels. To facilitate suture passing, the metal wire with the suture loop attached to it is inserted through created tibial tunnel and hooked onto the drill guide. The drill guide is withdrawn, passing the suture loop through the thread inserted previously between anterolateral portal and femoral tunnel. Subsequently, the looped thread passed between anterolateral portal and femoral tunnel is retrieved through femoral tunnel exit on the medial side of the thigh, passing the suture loop through the femoral tunnel. The next step is passing the graft. Another Hi-Fi Tape is passed around the tibial end of the graft. The Hi-Fi Tape is then tied to suture loop, on the femoral end and passed through both femoral and tibial tunnels, by retrieving suture loop through tibial tunnel. Under arthroscopic visualization, the autograft is introduced into the femoral tunnel and then into the tibial tunnel. Hi-Fi Tape is then knotted on the Suture Disc, sealing the exit of the tibial tunnel. Proper graft tension is achieved using the Tensioner. Here, you can see a postoperative radiograph, with visible suture discs on the tibial and femoral side.
Introduction
The posterior cruciate ligament (PCL) plays an important role in stabilization of the knee joint in various planes. It is the largest and strongest ligament of the knee, and its main role is to limit posterior tibial translation and tibial external rotation.1,2 The PCL tears are rare, with estimated prevalence of 3% of all knee injuries. However, up to 95% of cases of the PCL tears involve multiligamentous injuries, usually caused by vehicle or sports accidents.3,4 The necessity of a multifactorial approach make the PCL tears challenging to treat and always require an individual approach. When the decision about surgery is made, one should remember that the PCL reconstruction itself is a technically demanding procedure. The main troublesome factor is the ligament’s complicated anatomy. Tibial attachment of the PCL is located ∼1 cm distal to the joint surface, resulting in a sharp angle, where the graft for the tibial tunnel exists, commonly known as “killer turn”.5, 6, 7 Another disadvantage is the requirement of creating additional arthroscopic approaches, including trans-septal portal, which can cause difficulties for inexperienced surgeons. The authors present a surgical technique for arthroscopic remnant preserving 3-portal PCL reconstruction, with opposite to commonly described graft passage direction, which overcomes difficulties associated with the killer turn. Preserving PCL remnant can alternate healing and saves native mechanoreceptors of the PCL.7
Diagnosis
The diagnosis of the PCL tear is made based on history of trauma, clinical examination, radiographs and magnetic resonance imaging (MRI). MRI is also used to assess any concomitant intra-articular lesions. As PCL tears commonly occur in high-energy trauma, any other lesions and neurovascular injuries ought to be excluded.
Surgical Technique
Indications
Posterior instability of the knee caused by PCL tear grade II and III.
Contraindications
Contraindications include open knee injury, concomitant fractures of the knee, neurovascular injury, skin injuries or infection in region of planned cuts, an unstable patient condition, and finally, patient noncompliance with the strict rehabilitation protocol.
Patients Positioning
The patient is positioned supine with a nonsterile thigh tourniquet applied. The operated limb is placed on a leg holder and prepared in a sterile fashion.
Diagnostic Arthroscopy and Graft Preparation
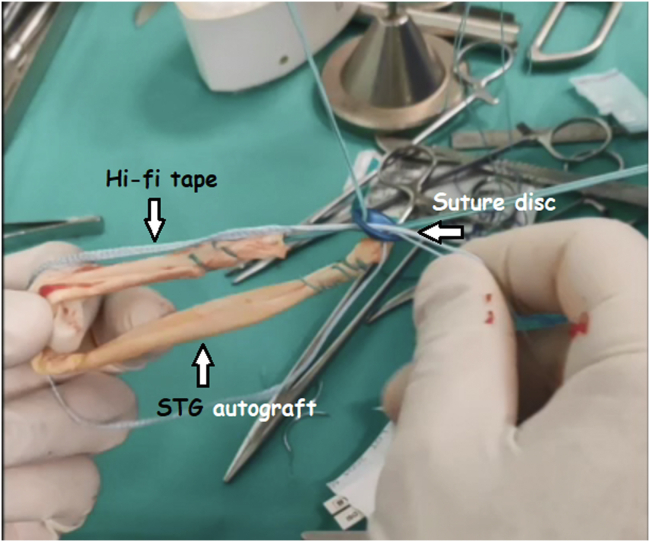
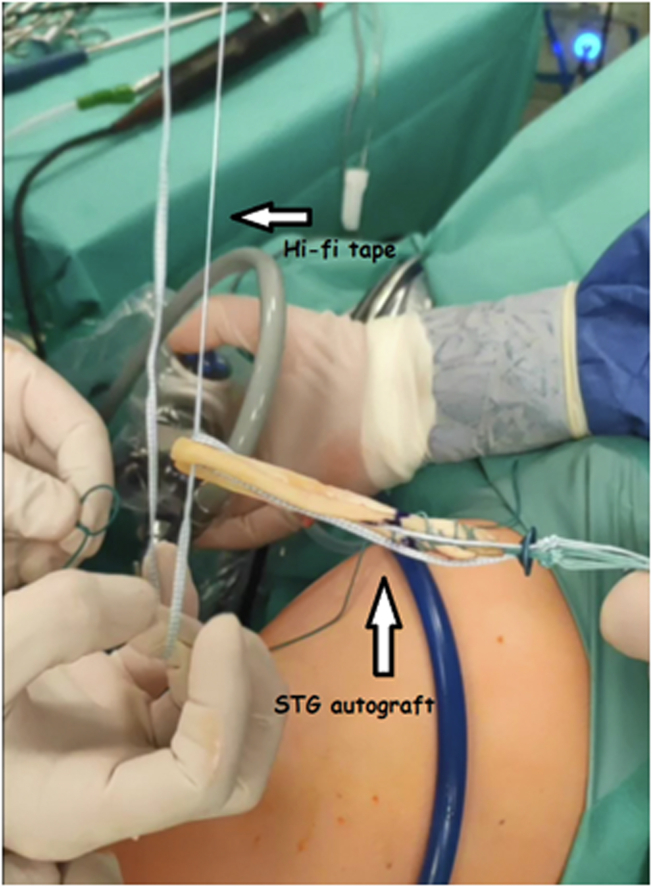
The diagnostic arthroscopy is performed through standard anterolateral and anteromedial portals using 30° arthroscope (Arthrex, Munich, Germany). At the beginning, the diagnosis of the PCL tear is confirmed. Before addressing the PCL, any concomitant lesions are excluded. Autografts used in this procedure are prepared from semitendinosus tendon and gracilis tendon, harvested from ipsilateral side, which are quadrupled, and strengthen using Hi-Fi Tape (Conmed, Largo, FL). The autograft diameter usually varies between 8 to 9 mm, and its length is approximately 100 mm. Suture disc (Medgal Sp., Księżyno, Poland) is implemented on the femoral end of the graft (Fig 1). Marking on the graft is created, indicating measured femoral tunnel length, which is usually ∼40 mm long.
Fig 1.
Autograft used in the procedure of posterior cruciate ligament (PCL) reconstruction prepared from semitendinosus tendon and gracilis tendon, harvested from ipsilateral side, which are quadrupled, and strengthened using Hi-Fi Tape. Suture disc is implemented on the femoral end of the graft. STG, semitendinosus and gracilis autograft.
PCL Reconstruction
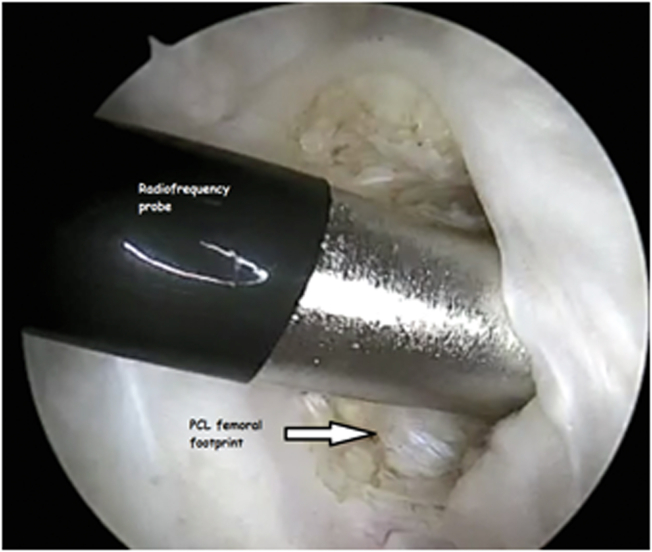
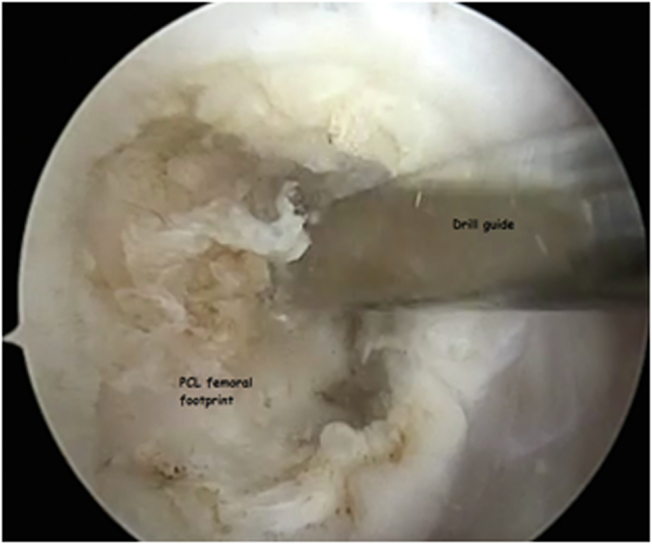
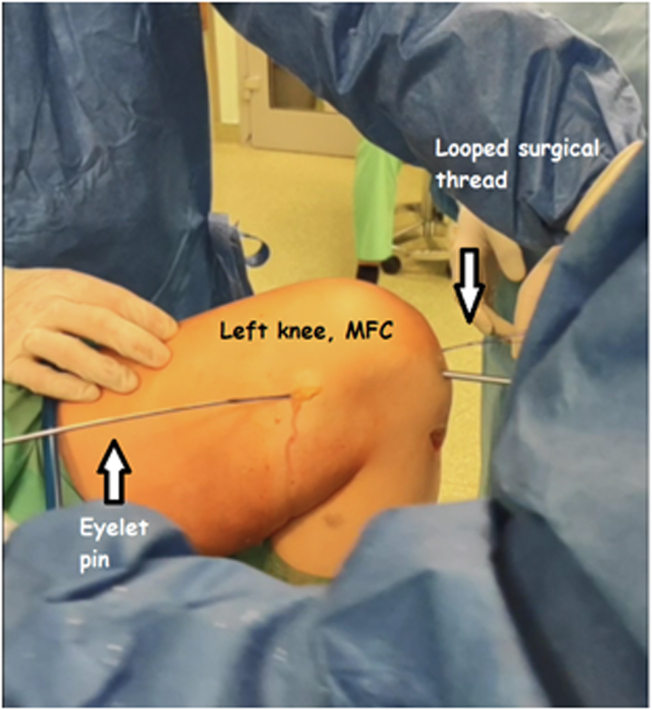
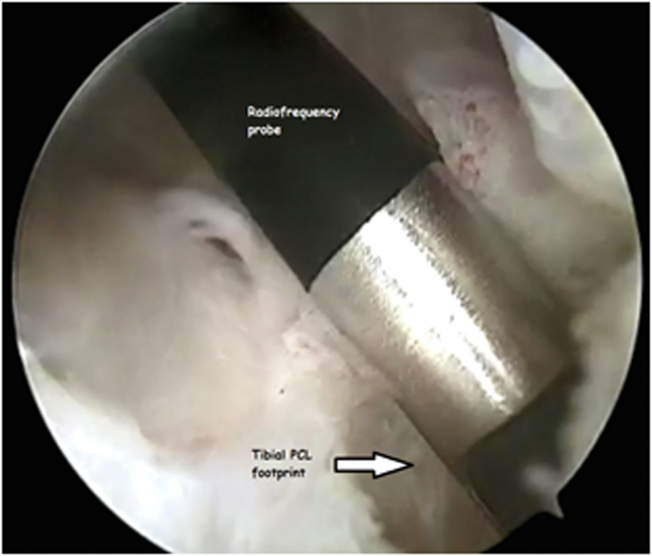
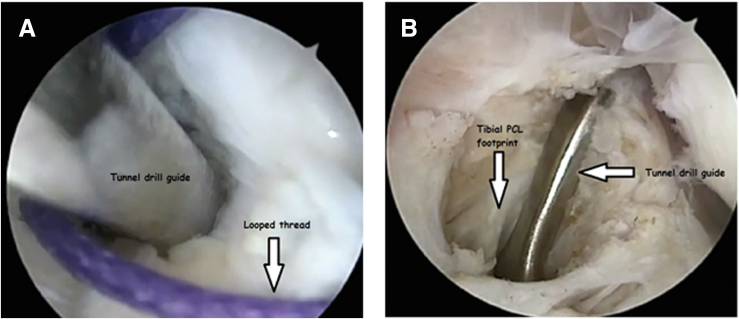
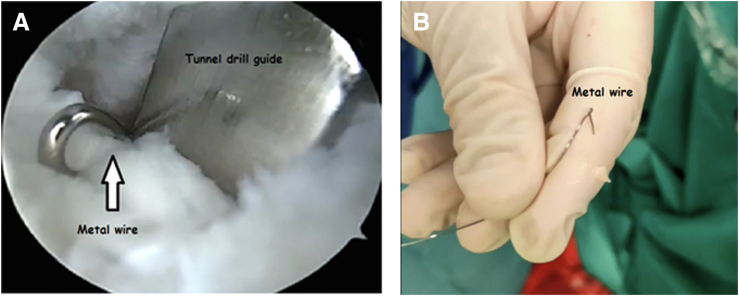
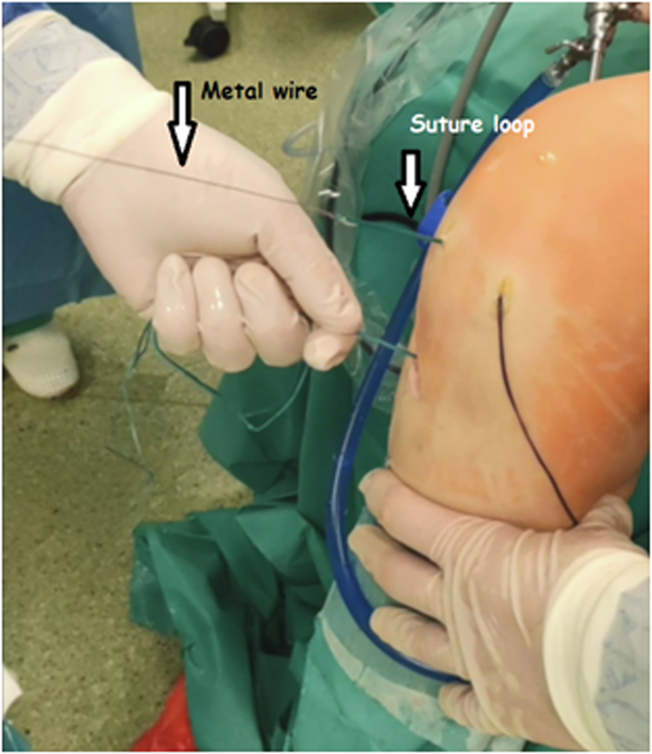
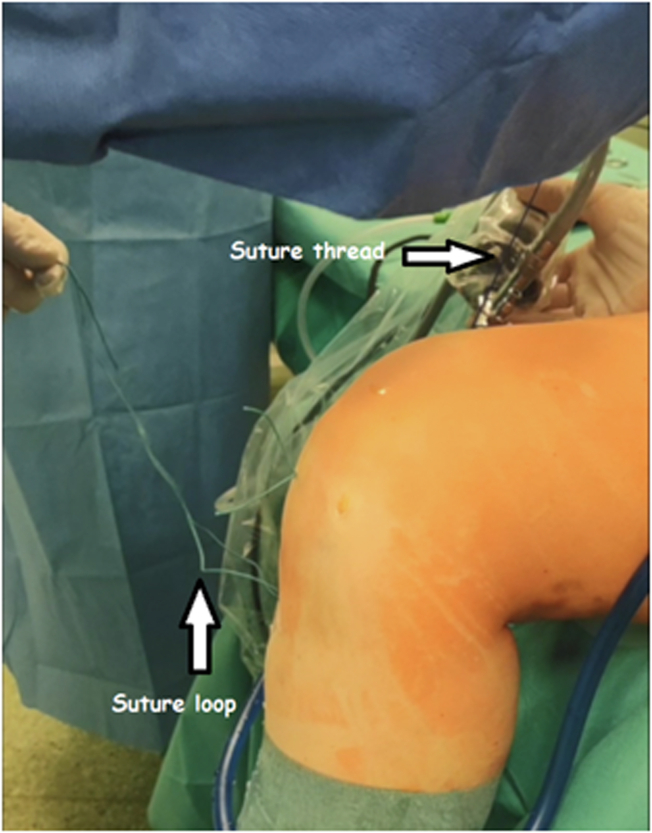
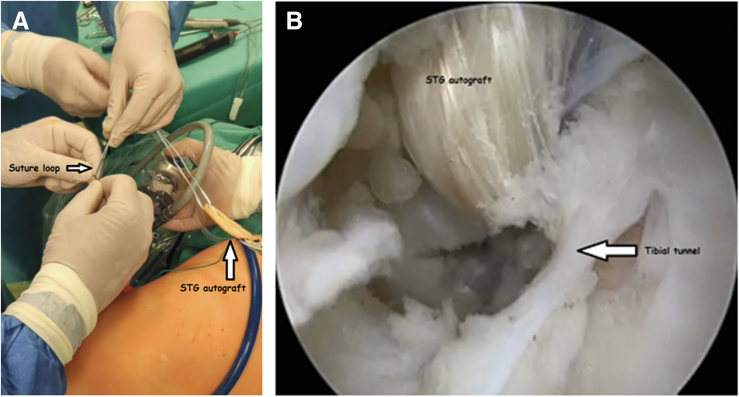
With the knee in 90° flexion and visualization through anteromedial portal, the femoral PCL insertion point is dissected until the footprint is exposed, using radiofrequency probe (Fig 2). The remnant of the PCL is left intact. The guide pin introduced through anterolateral portal is drilled with a free-hand technique through the center of the footprint, and an incision is made above its exit point of the medial femoral condyle (MFC) (Fig 3). The tunnel in MFC is drilled using drill size matched to the obtained graft diameter. With an eyelet pin, the looped surgical thread is passed between anterolateral portal and exit point of MFC (Fig 4, Video 1). The next step is to create posteromedial portal under visualization through anterolateral portal. The arthroscopic cannula is used to facilitate tools maneuvering. The PCL tibial insertion site is located and dissected using a radiofrequency probe until the PCL footprint is exposed (Fig 5). The tibial tunnel drill-guide (B. Braun Melsungen AG, Melsungen, Germany) is inserted through anteromedial portal and passed between the thread inserted previously through the femoral tunnel (Fig 6A). The arthroscope is switched to posteromedial portal and the tibial tunnel drill-guide is placed on the center of natural tibial PCL footprint (Fig 6B). The tibial tunnel is drilled with a drill matched to the graft size. The next step is passing the suture loop through the tibial and femoral tunnels. To facilitate suture passing, the metal wire with the suture loop attached to it is inserted through the created tibial tunnel and hooked onto the drill guide (Fig 7, A and B, Video 1). The drill guide is withdrawn, passing the suture loop through thread inserted previously between anterolateral portal and femoral tunnel (Fig 8).
Fig 2.
Arthroscopic view from the anterolateral portal in the left knee in 90° of flexion. The femoral PCL insertion point is dissected until the footprint is exposed, using a radiofrequency probe. Patient is positioned supine, while the left knee is being operated on. PCL, posterior cruciate ligament.
Fig 3.
Arthroscopic view from the anteromedial portal in the left knee in 90° of flexion. The remnant of the PCL is left intact. The guide pin introduced through the anterolateral portal is drilled through the center of the footprint. PCL, posterior cruciate ligament.
Fig 4.
With an eyelet pin, the looped surgical thread is passed between anterolateral portal and exit point of medial femoral condyle tunnel. Patient is positioned supine, while the left knee is being operated on. MFC, medial femoral condyle.
Fig 5.
Arthroscopic view from anterolateral portal into the posteromedial recess in the left knee flexed to 90°. The radiofrequency probe is introduced through the posteromedial portal. The PCL tibial insertion site is located and dissected using the radiofrequency device until the PCL footprint is exposed. PCL, posterior cruciate ligament.
Fig 6.
(A) The tibial tunnel drill-guide is inserted through the anteromedial portal and passed between the thread inserted previous through femoral tunnel. Patient is positioned supine, while left knee is being operated on; visualization is obtained through the anterolateral portal. (B) The tibial tunnel drill-guide is placed on the center of tibial PCL footprint. PC, posterior cruciate ligament.
Fig 7.
(A) Passing the suture loop through tibial and femoral tunnels. To use suture passing, the metal wire with suture loop attached to it is inserted through created tibial tunnel and hooked on the drill guide. Patient is positioned supine, while the left knee is being operated on. (B) The metal wire is used for suture passing in PCL reconstruction technique.
Fig 8.
The drill guide is withdrawn, passing the suture loop through the thread inserted previously between anterolateral portal and femoral tunnel. Patient is positioned supine, while the left knee is being operated on.
Subsequently, the looped thread passed between anterolateral portal and femoral tunnel is retrieved through the femoral tunnel exit on the medial side of the thigh, passing suture loop through femoral tunnel (Fig 9). The next step is passing the graft. Another Hi-Fi Tape (Conmed, Largo, FL) is passed around the tibial end of the graft (Fig 10). The Hi-Fi Tape is then tied to suture loop, on the femoral end and passed through both femoral and tibial tunnels, by retrieving suture loop through tibial tunnel (Fig 11A). Under arthroscopic visualization, by pulling the Hi-Fi Tape on the tibial side, the autograft is introduced into the femoral tunnel and then into the tibial tunnel (Fig 11B). Hi-Fi Tape is then knotted on the Suture Disc sealing the exit of the tibial tunnel. Proper graft tension is achieved using Tensioner (B. Braun Melsungen AG, Melsungen, Germany) (Fig 12, Video 1). After the procedure, the wounds are closed in a layered fashion and sealed with sterile dressing. On postoperative radiographs, suture discs on femoral and tibial tunnel exits can be visible (Video 1).
Fig 9.
The looped thread that is passed between the anterolateral portal and femoral tunnel is retrieved through the femoral tunnel exit on the medial side of the thigh, passing the suture loop through the femoral tunnel. Patient is positioned supine, while the left knee is being operated on.
Fig 10.
Another Hi-Fi Tape is passed around the tibial end of the graft. STG, semitendinosus and gracilis autograft.
Fig 11.
(A) The Hi-Fi Tape is tied to the suture loop on the femoral end and passed through both femoral and tibial tunnels, by retrieving suture loop through the tibial tunnel. Patient is positioned supine, while the left knee is being operated on. STG, semitendinosus and gracilis autograft. (B) Under arthroscopic control, by pulling the Hi-Fi Tape on the tibial side, the autograft is introduced into the femoral tunnel and then into the tibial tunnel. Patient is positioned supine, while the left knee is being operated on. STG, semitendinosus and gracilis autograft.
Fig 12.
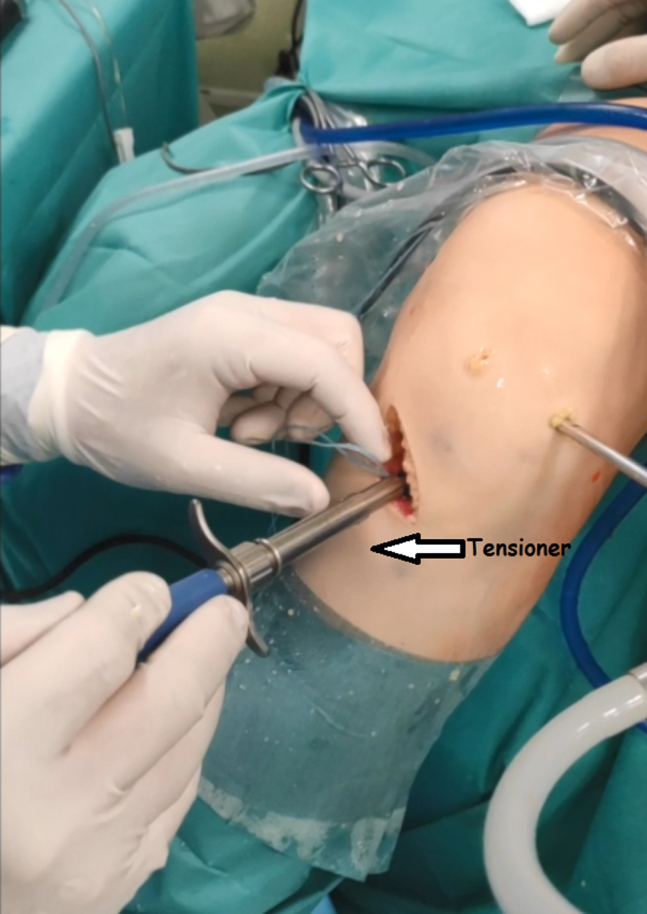
Hi-Fi Tape is knotted on the suture disc sealing the exit of the tibial tunnel. Proper graft tension is achieved using Tensioner. Patient is positioned supine, while the left knee is being operated on.
Postoperative Care and Rehabilitation
Two postoperative drainages are used, one in the joint and the second one in the graft harvesting and tibial tunnel site. In the early postoperative period, it is recommended to elevate the operated limb to reduce swelling. In the process of postoperative rehabilitation, the authors postulate partial load bearing of the operated limb for 4 weeks. Rehabilitation protocols should be tailored for the specific patient, taking into account any concomitant lesions.
Discussion
The presented surgical technique uses a specific way for graft passage, the reverse of the commonly used direction from tibia to femur. The sharp angle between created tunnels in PCL reconstruction, the so-called killer turn, has been troublesome for many surgeons, and a variety of solutions has been developed, like the rod and pulley technique or passing graft through the posteromedial or anteromedial, breaking graft passage into two stages.6,7,8 These techniques require additional maneuvering, whereas the presented technique is simple and easy to perform. Passing graft in the reverse direction, causes less stress on the killer turn. Moreover, the preserved PCL remnant acts like a cushion, facilitating graft passage. PCL remnant preservation also promotes graft healing and saves proprioceptors of the native ligament.7 Another advantage of this technique is using only 3 arthroscopic portals: anteromedial, anterolateral, and posteromedial, which are sufficient to provide good visualization during the reconstruction. The simplicity of this technique is beneficial in multiligamentous reconstructions, as it shortens the time of surgery and causes less stress on the patient. As in every surgical procedure, there are possible risks and disadvantages. Whereas autografts are beneficial for patients in terms of healing, there are risks of donor site morbidity. In case of multiligamentous reconstructions, the options of graft harvesting are limited, and the risk of tunnel convergence is increased. Moreover, there is a risk of neurovascular iatrogenic injury during creation of the tibial tunnel. Another disadvantage might be the fact, that the presented technique is a single-bundle reconstruction. Despite providing good stability, there is evidence that double-bundle reconstruction might be more beneficial for the patient (Table 1). Double-bundle reconstruction, however, can be difficult to achieve in multiligamentous injuries, where multiple tunnels have to be created.2 Despite good results of the procedure, further objective studies ought to be made, to assess long-term outcome of this technique. The procedure of arthroscopic remnant preserving PCL reconstruction with reverse passage of the graft is a valuable method of reconstruction, which can be used both in an isolated PCL tear or in multiligamentous injuries, reducing time and simplifying pitfalls that can be encountered in other described procedures.
Table 1.
Advantages and Disadvantages of the Technique
| Advantages | Disadvantages |
|---|---|
| Reverse passage of the graft creates less stress on the “killer turn” | Possible donor site morbidity |
| Only 3 portals are used in the procedure. Good visualization of PCL through the posteromedial portal | Possibility of compartment syndrome |
| Preserved PCL remnant acts like cushion while passing the graft | Possibility of iatrogenic neurovascular injury |
| Preserved PCL remnant promotes healing and saves native PCL proprioception | Single bundle reconstruction |
| Reduced the time of procedure |
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic remnant preserving PCL reconstruction with reverse passage of the graft. The left knee is being operated on. In the beginning, PCL injury is confirmed. Autograft is prepared from semitendinosus and gracilis tendon, which are quadrupled, and is strengthened using Hi-Fi Tape. Suture disc is implemented on the femoral end of the graft. With the knee in 90° flexion and visualization through anteromedial portal, the femoral PCL insertion point is dissected until the footprint is exposed. The guide pin introduced through anterolateral portal is drilled with a free-hand technique through the center of the footprint, and an incision is made above its exit point of the medial femoral condyle (MFC). The tunnel in medial femoral condyle is drilled using drill size matched to the obtained graft diameter. The posteromedial portal is created under visualization through the anterolateral portal. The arthroscopic cannula is used to facilitate tools maneuvering. The PCL tibial insertion site is located and dissected using a radiofrequency probe until the PCL footprint is being exposed. With an eyelet pin, the looped surgical thread is passed between anterolateral portal and the exit point of the medial femoral condyle tunnel. The tibial tunnel drill-guide is inserted through anteromedial portal and passed between the thread inserted previously through the femoral tunnel. The arthroscope is switched to the posteromedial portal and the tibial tunnel drill-guide is placed on the center of the natural tibial PCL footprint. The tibial tunnel is drilled with a drill matched to the graft size. The next step is passing the suture loop through tibial and femoral tunnels. To facilitate suture passing, the metal wire with the suture loop attached to it is inserted through created tibial tunnel and hooked onto the drill guide. The drill guide is withdrawn, passing the suture loop through the thread inserted previously between anterolateral portal and femoral tunnel. Subsequently, the looped thread passed between anterolateral portal and femoral tunnel is retrieved through femoral tunnel exit on the medial side of the thigh, passing the suture loop through the femoral tunnel. The next step is passing the graft. Another Hi-Fi Tape is passed around the tibial end of the graft. The Hi-Fi Tape is then tied to suture loop, on the femoral end and passed through both femoral and tibial tunnels, by retrieving suture loop through tibial tunnel. Under arthroscopic visualization, the autograft is introduced into the femoral tunnel and then into the tibial tunnel. Hi-Fi Tape is then knotted on the Suture Disc, sealing the exit of the tibial tunnel. Proper graft tension is achieved using the Tensioner. Here, you can see a postoperative radiograph, with visible suture discs on the tibial and femoral side.
References
- 1.Kennedy N.I., Wijdicks C.A., Goldsmith M.T., et al. Kinematic analysis of the posterior cruciate ligament, part 1: The individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41:2828–2838. doi: 10.1177/0363546513504287. [DOI] [PubMed] [Google Scholar]
- 2.Kumar A., Sinha S., Arora R., Gaba S., Khan R., Kumar M. The 50 top-cited articles on the posterior cruciate ligament: A bibliometric analysis and review. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211057851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Floyd E.R., Falaas K.L., et al. The posterior cruciate ligament: Anatomy, biomechanics, and double-bundle reconstruction. J Arthrosc Surg Sports Med. 2021;2:94–107. [Google Scholar]
- 4.Hassebrock J.D., Gulbrandsen M.T., Asprey W.L., Makovicka J.L., Chhabra A. Knee ligament anatomy and biomechanics. Sports Med Arthrosc Rev. 2020;28:80–86. doi: 10.1097/JSA.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 5.Ahn J.H., Chung Y.S., Oh I. Arthroscopic posterior cruciate ligament reconstruction using the posterior trans-septal portal. Arthroscopy. 2003;19:101–107. doi: 10.1053/jars.2003.50017. [DOI] [PubMed] [Google Scholar]
- 6.Vasdev A., Rajgopal A., Gupta H., Dahiya V., Tyagi V.C. Arthroscopic all-inside posterior cruciate ligament reconstruction: Overcoming the "killer turn". Arthrosc Tech. 2016;5:e501–e506. doi: 10.1016/j.eats.2016.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chernchujit B., Samart S., Nakorn P.N. Remnant-preserving posterior cruciate ligament reconstruction: Arthroscopic transseptal, rod and pulley technique. Arthroscopy Tech. 2017;6:e15–e20. doi: 10.1016/j.eats.2016.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen T., Liu S., Chen J. All-anterior approach for arthroscopic posterior cruciate ligament reconstruction with remnant preservation. Arthrosc Tech. 2016;5:e1203–e1207. doi: 10.1016/j.eats.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic remnant preserving PCL reconstruction with reverse passage of the graft. The left knee is being operated on. In the beginning, PCL injury is confirmed. Autograft is prepared from semitendinosus and gracilis tendon, which are quadrupled, and is strengthened using Hi-Fi Tape. Suture disc is implemented on the femoral end of the graft. With the knee in 90° flexion and visualization through anteromedial portal, the femoral PCL insertion point is dissected until the footprint is exposed. The guide pin introduced through anterolateral portal is drilled with a free-hand technique through the center of the footprint, and an incision is made above its exit point of the medial femoral condyle (MFC). The tunnel in medial femoral condyle is drilled using drill size matched to the obtained graft diameter. The posteromedial portal is created under visualization through the anterolateral portal. The arthroscopic cannula is used to facilitate tools maneuvering. The PCL tibial insertion site is located and dissected using a radiofrequency probe until the PCL footprint is being exposed. With an eyelet pin, the looped surgical thread is passed between anterolateral portal and the exit point of the medial femoral condyle tunnel. The tibial tunnel drill-guide is inserted through anteromedial portal and passed between the thread inserted previously through the femoral tunnel. The arthroscope is switched to the posteromedial portal and the tibial tunnel drill-guide is placed on the center of the natural tibial PCL footprint. The tibial tunnel is drilled with a drill matched to the graft size. The next step is passing the suture loop through tibial and femoral tunnels. To facilitate suture passing, the metal wire with the suture loop attached to it is inserted through created tibial tunnel and hooked onto the drill guide. The drill guide is withdrawn, passing the suture loop through the thread inserted previously between anterolateral portal and femoral tunnel. Subsequently, the looped thread passed between anterolateral portal and femoral tunnel is retrieved through femoral tunnel exit on the medial side of the thigh, passing the suture loop through the femoral tunnel. The next step is passing the graft. Another Hi-Fi Tape is passed around the tibial end of the graft. The Hi-Fi Tape is then tied to suture loop, on the femoral end and passed through both femoral and tibial tunnels, by retrieving suture loop through tibial tunnel. Under arthroscopic visualization, the autograft is introduced into the femoral tunnel and then into the tibial tunnel. Hi-Fi Tape is then knotted on the Suture Disc, sealing the exit of the tibial tunnel. Proper graft tension is achieved using the Tensioner. Here, you can see a postoperative radiograph, with visible suture discs on the tibial and femoral side.
Arthroscopic remnant preserving PCL reconstruction with reverse passage of the graft. The left knee is being operated on. In the beginning, PCL injury is confirmed. Autograft is prepared from semitendinosus and gracilis tendon, which are quadrupled, and is strengthened using Hi-Fi Tape. Suture disc is implemented on the femoral end of the graft. With the knee in 90° flexion and visualization through anteromedial portal, the femoral PCL insertion point is dissected until the footprint is exposed. The guide pin introduced through anterolateral portal is drilled with a free-hand technique through the center of the footprint, and an incision is made above its exit point of the medial femoral condyle (MFC). The tunnel in medial femoral condyle is drilled using drill size matched to the obtained graft diameter. The posteromedial portal is created under visualization through the anterolateral portal. The arthroscopic cannula is used to facilitate tools maneuvering. The PCL tibial insertion site is located and dissected using a radiofrequency probe until the PCL footprint is being exposed. With an eyelet pin, the looped surgical thread is passed between anterolateral portal and the exit point of the medial femoral condyle tunnel. The tibial tunnel drill-guide is inserted through anteromedial portal and passed between the thread inserted previously through the femoral tunnel. The arthroscope is switched to the posteromedial portal and the tibial tunnel drill-guide is placed on the center of the natural tibial PCL footprint. The tibial tunnel is drilled with a drill matched to the graft size. The next step is passing the suture loop through tibial and femoral tunnels. To facilitate suture passing, the metal wire with the suture loop attached to it is inserted through created tibial tunnel and hooked onto the drill guide. The drill guide is withdrawn, passing the suture loop through the thread inserted previously between anterolateral portal and femoral tunnel. Subsequently, the looped thread passed between anterolateral portal and femoral tunnel is retrieved through femoral tunnel exit on the medial side of the thigh, passing the suture loop through the femoral tunnel. The next step is passing the graft. Another Hi-Fi Tape is passed around the tibial end of the graft. The Hi-Fi Tape is then tied to suture loop, on the femoral end and passed through both femoral and tibial tunnels, by retrieving suture loop through tibial tunnel. Under arthroscopic visualization, the autograft is introduced into the femoral tunnel and then into the tibial tunnel. Hi-Fi Tape is then knotted on the Suture Disc, sealing the exit of the tibial tunnel. Proper graft tension is achieved using the Tensioner. Here, you can see a postoperative radiograph, with visible suture discs on the tibial and femoral side.