Abstract
The uses of cervical mucus and basal body temperature as indicators of return to fertility postpartum have resulted in high unintended pregnancy rates. In 2013, a study found that when women used urine hormone signs in a postpartum/breastfeeding protocol this resulted in fewer pregnancies. To improve the original protocol's effectiveness, three revisions were made: (1) women were to increase the number of days tested with the Clearblue Fertility Monitor, (2) an optional second luteinizing hormone test could be done in the evening, and (3) instructions were given to manage the beginning of the fertile window for the first six cycles postpartum. The purpose of this study was to determine the correct and typical use effectiveness rates to avoid pregnancy in women who used a revised postpartum/breastfeeding protocol. A cohort review of an established data set from 207 postpartum breastfeeding women who used the protocol to avoid pregnancy was completed using Kaplan-Meier survival analysis. Total pregnancy rates that included correct and incorrect use pregnancies were eighteen per one hundred women over twelve cycles of use. For the pregnancies that met a priori criteria, the correct use pregnancy rates were two per one hundred over twelve months and twelve cycles of use and typical use rates were four per one hundred women at twelve cycles of use. The protocol had fewer unplanned pregnancies than the original, however, the cost of the method increased.
Keywords: breastfeeding, effectiveness, natural family planning (NFP), postpartum
Women value Natural Family Planning (NFP) as a safe and healthy method of spacing their children (Severy and Robinson 2004, 130–131). Variability in the first few menstrual cycles postpartum and inaccurate traditional biomarkers of fertility (e.g., mucus and temperature) have resulted in higher unintended pregnancy rates during the first three postpartum breastfeeding cycles, Institute for Natural Family Planning; (Bouchard et al. 2018, 407–408; Brown 2011, 7–8; Hatherley 1985, 332; Kennedy et al. 1995, 111). Typically, traditional NFP methods where women observe and record cervical mucus and basal body temperature (BBT) are between 68 percent and 84 percent effective in preventing pregnancy postpartum (Brown, Harrisson, and Smith 1985, 10; Hatherley 1985, 321–324; Howard and Stanford 1999, 395–396, 399; Klaus et al. 1979, R621). The high pregnancy rates (e.g., for cervical mucus and BBT methods of NFP) in postpartum breastfeeding women over the last fifty years are thought to be related to the dissociation found between traditional biomarkers of fertility and urine hormone biomarkers (Bouchard et al., 2018, 407–408; Kennedy et al. 1995, 111–112). This is because cervical mucus changes and shifts in BBT are not easily discernible during lactation amenorrhea (i.e., identified in this study as cycle zero) and the first few cycles postpartum. The use of these biological signs of fertility also requires a rigorous daily routine which can be difficult for women with a new baby (Barron and Fehring 2005, 294–295; Hatherley 1985, 321–322, Kennedy et al. 1995, 111–112). Therefore, since traditional NFP methods have high pregnancy rates and can be difficult for a busy postpartum mother to adhere to, more objective, effective, and efficient user-friendly methods of NFP are needed.
An objective postpartum breastfeeding NFP protocol that had women test their first-morning urine using the Clearblue Fertility Monitor (CBFM) has helped to reduce unintended pregnancies during the breastfeeding transition (Bouchard, Fehring, and Schneider 2013, 36). The protocol integrated the CBFM, a handheld device used to test for two pre-ovulatory hormones, estrone-3-glucuronide (E3G) and luteinizing hormone (LH). Comparison studies to identify LH where women tested urine hormones with the CBFM, had serum levels drawn, and transvaginal ultrasound found ovulation occurred within three days of when the CBFM identified LH surge (Behre et al. 2000, 2480; Johnson et al. 2015, 1100–1106, Roos et al. 2015, 7). The CBFM was integrated into an NFP postpartum/breastfeeding protocol, and the protocol was made available to women and couples in a secure, easy-to-use online fertility charting system. The effectiveness of the protocol has been reported to be 92 percent and 98 percent for avoiding an unintended pregnancy (Bouchard, Fehring, and Schneider 2013, 40; Fehring, Schneider, and Bouchard 2017, e133; Mu, Fehring, and Bouchard 2020, 5).
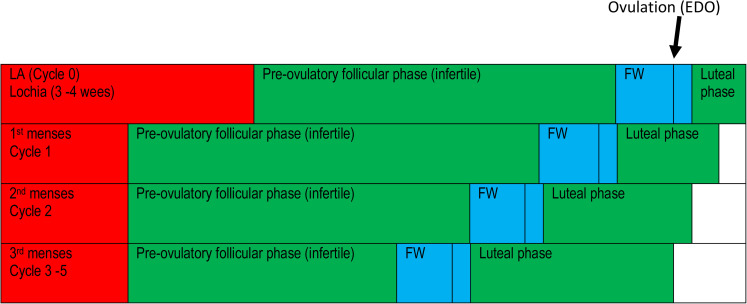
Revisions of the protocol published in 2013 (Bouchard, Fehring, and Schneider 2013, 36) were developed to improve effectiveness and ease of use. In the revised protocol, (1) women were instructed to test with the CBFM daily for ten days during cycle zero (i.e., lactation amenorrhea), (2) to start the fertile time in cycle one on day ten and then with each subsequent cycle shift the start of the fertile time earlier each cycle by one day (see Figure 1), and, (3) to add an optional LH urine test that could be done in the evening (Bouchard et al. 2018, 36). The purpose of this study was to determine the correct- and typical-use effectiveness pregnancy rates of the revised protocol at twelve months and twelve cycles of use (Bouchard, Fehring, and Schneider 2013, 36) (Figure 1).
Figure 1.
The fertile window (FW) shifts ahead a few days each cycle during the transition. The shifting of the FW shortens the pre-ovulatory fertile phase and lengthens the postovulatory luteal phase by a few days with each cycle. The FW itself remains the same length. For the MM protocol, the FW begins on day ten of the first cycle and is moved forward one day each cycle. That is in cycle two the FW begins on day nine, in cycle three the FW begins on day eight, in cycle four the FW begins on day seven and in cycle five the FW begins on day six.
Methods
This study was an analysis of archived data from fertility charts collected from a longitudinal prospective repeated measure cohort design of postpartum breastfeeding women who used the revised protocol to avoid pregnancy in the first six cycles postpartum. Demographic and chart data were from postpartum breastfeeding women who registered in an online NFP instruction program between July 1, 2015, and May 1, 2019, to learn the protocol. The objective of the study was to understand the correct-use and typical-use effectiveness of the protocol to avoid pregnancy in postpartum breastfeeding women.
Setting and Subjects
Subjects were women who registered as postpartum breastfeeding, between the ages of eighteen and forty-five years old. The setting was an online NFP education center. The center was managed by specially trained professional NFP nurses that provided online guidance to couples learning the revised protocol. Medical and ethical consultation was provided by a physician (Obstetrician–Gynecologist) and a medical bioethicist.
Data Collection and Variables
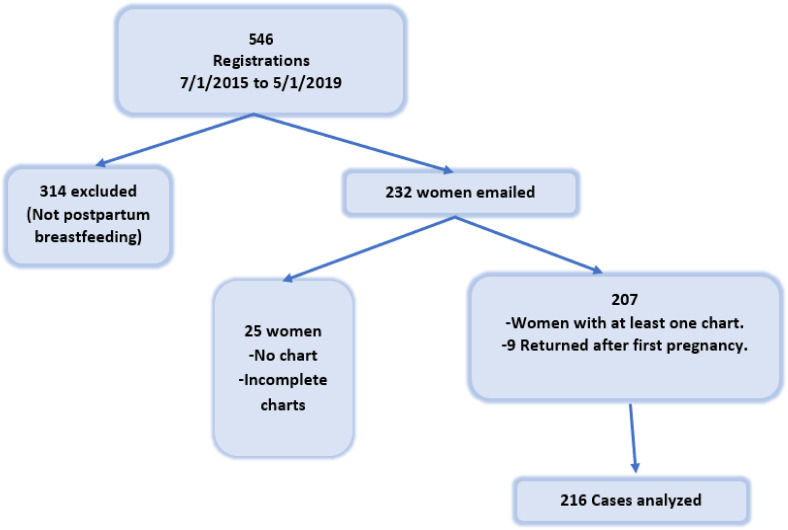
Data collection was completed in two phases (see Figure 2). In the first phase, data extraction was completed using minimum inclusion criteria. The inclusion criteria were women who (1) registered as either total or partial breastfeeding, (2) used the revised breastfeeding protocol, (3) and completed at least one cycle postpartum. Variables included the registrant's reproductive category, email and the number of cycles charted. Demographic information included the age of the woman, number of pregnancies, number of children, years married, religion, ethnicity, and education status.
Figure 2.
Inclusion collection flowchart.
In phase two an email was sent to women who met the minimal inclusion criteria. The email included an introduction to the study and a link to an online Qualtrics survey. The Qualtrics survey opened with a statement about the study's purpose, why the participant received the invite, and a consent form approved by Marquette University IRB (HR 3666). Women could agree to participate by clicking “Yes” to proceed to the Qualtrics survey. In the survey, women were asked (1) their infant's date of birth, (2) their breastfeeding status, (3) their type of delivery and the health of their baby at birth, and, (4) if pregnancy occurred during the study period. If a pregnancy occurred, the women were directed to an evaluation form. A standardized pregnancy evaluation unique to users of the method was completed by women using either (1) the original website or, (2) the Qualtrics survey site. Both sites contained the same pregnancy evaluation. After phase two, the data was collected and deidentified (i.e., emails removed) for analysis.
Pregnancy Evaluation and Charting
All pregnancies required a pregnancy evaluation and the original fertility chart for review. Pregnancy evaluations completed by the user and reviewed by the authors came from either the user's membership portal on the original website or the Qualtrics questionnaire. Pregnancy classifications included intended, unintended, correct, and incorrect use of the protocol. A pregnancy evaluation tool adapted from a previous study (Fehring et al. 2013, 25–26) was used to evaluate each pregnancy. Pregnancies were considered incorrect-use when the intention recorded on the chart was “avoid,” and an act of intercourse was recorded during the fertile time, or when the fertile and infertile phases were not apparent on their chart or acts of intercourse were not recorded. Correct or perfect-use pregnancies were determined to be pregnancies that occurred when a couple became pregnant from an act of intercourse on a day that was identified as infertile by the method. A standardized menstrual cycle chart system (i.e., online fertility charts) was used by the women to record results from the CBFM. The CBFM screen showed either an “L, H or P” to indicate “Low,” “High,” or “Peak” fertility. The fertility chart system teaches women that when the CBFM shows “L” on the screen estrogen is low (fertility is low), when it shows “H” on the screen, the estrogen levels have increased (fertility is high), and when it shows “P” on the screen, the LH surge was detected and ovulation could occur within twenty-four and thirty six-hours (Swiss Precision Diagnostics GmbH 2015, 3). This recording system is used to identify the fertile and infertile days of the cycle and guide women using the postpartum breastfeeding protocol.
Data Analysis
A Kaplan-Meier survival analysis was completed using SPSS 27. The analysis included correct and incorrect use pregnancies at both twelve months and twelve cycles of use. Pregnancies that met a priori criteria included both correct- and incorrect-use cycles and correct-use pregnancies included only correct-use cycles.
Results
Data was collected from 207 women during 216 postpartum periods (nine women provided two separate postpartum periods for evaluation). Demographics presented in Table 1 show that most of the women (i.e., 86 percent) were Catholic, white non-Hispanic, and over half registered as total breastfeeding. These women provided 1660 months of use and 1256 cycles of use. The total months of correct use were 1,558, and the total cycles with correct use were 1,149 (n = 216). These cycles were used in the correct-use pregnancy calculations. The median number of correct months of use was 7.0 per woman with a mean of 7.21 (SD = 4.01, 95 percent CI [6.66, 7.76]), and the median number of correct cycles of use was 4.0 with a mean of 4.76 (SD = . 4.15, 95 percent CI [4.76, 5.88]). The median number of total cycles of use was 5.0 (per woman), with a mean of 5.81 (SD = 4.13, 95 percent CI [5.26, 6.37]) cycles of use. Total months of use and total cycles of use were used in the typical-use pregnancy calculations.
Table 1.
Demographics and Characteristics of the Breastfeeding Women.
| Variable | M | SD | |
|---|---|---|---|
| Age of the woman | 31 | (5.1) | |
| Years married | 5.1 | (4.6) | |
| Number of pregnancies | 3.1 | (2.5) | |
| Number of children | 3.0 | (2.6) | |
| Characteristics | (n) Percent of participants | ||
| Religion: | |||
| Catholic | (178) 86.0 | ||
| Protestant | (9) 4.3 | ||
| Other | (1) 0.5 | ||
| No response | (19) 9.2 | ||
| Ethnicity | |||
| Caucasian | (138) 66.7 | ||
| Hispanic | (13) 6.3 | ||
| Asian | (7) 3.4 | ||
| Other | (13) 6.3 | ||
| No response | (36) 17.4 | ||
| Education | |||
| 0–12 years | (15) 7.8 | ||
| 13–16 years | (62) 29.9 | ||
| 17 + years | (93) 44.9 | ||
| No response | (37) 17.9 | ||
| Breastfeeding status | |||
| Total breastfeeding | (113) 54.6 | ||
| Partial breastfeeding | (82) 39.5 | ||
| No response | (12) 5.8 | ||
| Baby's health at birth | |||
| Healthy | (62) 96.9 | ||
| Not healthy | (2) 3.1 | ||
| Country | |||
| USA | (136) 65.7 | ||
| Canada | (7) 3.4 | ||
| Other | (64) 30.9 | ||
Note: Baby's health at birth values came from the Qualtrics data set (N = 64).
Total Pregnancies
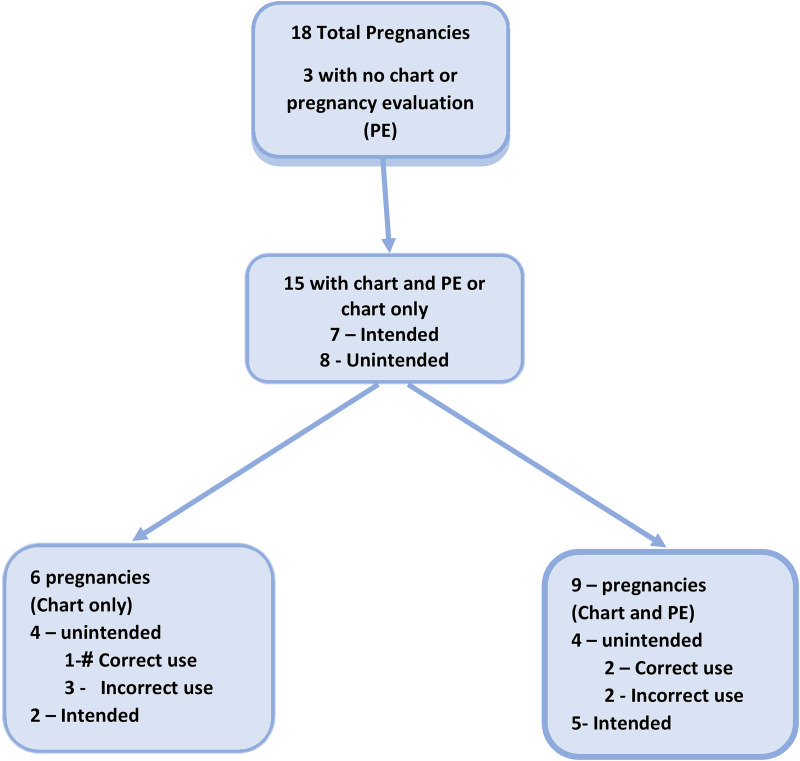
The total number of pregnancies was eighteen per 216 cases or sixteen women per one hundred at twelve months (SR = 0.859, SE = 0.032, n = 75, see Table 2) and twelve cycles (SR = 0.859, SE = 0.035, n = 40, see Table 3) of use. Three of the eighteen pregnancies did not have enough information to determine whether they were intended or unintended pregnancies (they identified a pregnancy that occurred but did not have any chart data nor provided a pregnancy evaluation). Among the other fifteen, there were seven intended pregnancies and eight unintended pregnancies. Only nine pregnancies of these fifteen pregnancies met the a priori inclusion criteria where both the pregnancy evaluation and a conception chart were available for analysis. Of the nine pregnancies five were intended and four were unintended. Among the six other pregnancies who had charts but no pregnancy evaluation, one was a correct-use unintended pregnancy, three were incorrect-use unintended pregnancy, and two were intended pregnancies (see Figure 3).
Table 2.
Total Pregnancy and Survival Rates per One Hundred Women Pregnant Within Twelve Months of Use (N = 216).
| Months | SR | SE | Preg. | N |
|---|---|---|---|---|
| 1 | .985 | .009 | 3 | 196 |
| 3 | .979 | .010 | 1 | 167 |
| 6 | .946 | .018 | 5 | 139 |
| 9 | .913 | .023 | 4 | 101 |
| 12 | .859 | .032 | 5 | 75 |
Note: Total pregnancy rates include all pregnancies outside of the inclusion criteria, SR = survival rate per one hundred women over twelve months of use, SE = standard error, Preg. = number of pregnancies per every three months of use, and N = number of women exposed.
Table 3.
Total Pregnancy and Survival Rates per One Hundred Women Pregnant Within Twelve Cycles of Use (N = 216 Cases and 1256 Cycles).
| Cycles | SR | SE | Preg. | N |
|---|---|---|---|---|
| 0 | .981 | .009 | 4 | 212 |
| 3 | .951 | .016 | 5 | 141 |
| 6 | .890 | .027 | 7 | 100 |
| 9 | .880 | .028 | 1 | 89 |
| 12 | .859 | .035 | 1 | 40 |
Note: Total pregnancy rate includes all pregnancies outside of the inclusion criteria, SR = survival rate per one hundred women over twelve cycles of use, SE = standard error, Preg. = number of pregnancies per every three cycles of use and N = number of women exposed.
Figure 3.
Breakdown of total pregnancies with and without a pregnancy evaluation (PE).
Correct-Use Unintended Pregnancy Rate
Of the four unintended pregnancies, two were correct-use. Table 4 shows the correct-use unintended pregnancies per one hundred women at one, three, six, nine, and twelve months of use. The two correct-use unintended pregnancies occurred at six and nine months of use. The survival rate for correct-use pregnancies per one hundred women at twelve months of use was 98 percent (SE = 0.011, n = 76). Survival rates were based on cycles of use, the two pregnancies occurred at one and three cycles of use, and the correct-use survival pregnancy rate was 98.7 percent or two pregnancies per one hundred users over twelve cycles of use (SR = 0.987, SE = 0.009, n = 36, see Table 5). If we include the additional six pregnancies with a chart but without a pregnancy evaluation, there was one other correct-use unintended pregnancy which would give a pregnancy rate of 95.6 percent (SE = .018, n = 82) for months of use and 95.5 percent (SE = .019, n = 99) for cycles of use.
Table 4.
Survival Rates per One Hundred Women Pregnant by Typical and Correct Months of Use (N = 216).
| Months | Typical | Correct | ||||||
|---|---|---|---|---|---|---|---|---|
| (1,660 months of use) | (1,558 months of use) | |||||||
| SR | SE | Preg. | N | SR | SE | Preg. | n | |
| 1 | 1.00 | .000 | 0 | 216 | 1.00 | .000 | 0 | 215 |
| 3 | 1.00 | .000 | 0 | 169 | 1.00 | .000 | 0 | 168 |
| 6 | .993 | .007 | 1 | 152 | .993 | .007 | 1 | 152 |
| 9 | .975 | .014 | 2 | 101 | .985 | .011 | 1 | 115 |
| 12 | .965 | .018 | 1 | 77 | .985 | .011 | 0 | 76 |
Note: SR = survival rate per one hundred women per twelve months of use, SE = standard error, Preg. = number of pregnancies per three cycles of use, and N = total number of women exposed.
Table 5.
Survival Rates per One Hundred Pregnant Women by Typical and Correct Cycles of Use.
| Cycle | Typical | Correct | ||||||
|---|---|---|---|---|---|---|---|---|
| (1,256 cycles of use) | (1,149 cycles of use) | |||||||
| SR | SE | Preg. | N | SR | SE | Preg. | n | |
| 0 | .995 | .005 | 1 | 215 | .995 | .005 | 1 | 209 |
| 3 | .982 | .011 | 2 | 128 | .987 | .009 | 1 | 120 |
| 6 | .973 | .014 | 1 | 105 | .987 | .009 | 0 | 79 |
| 9 | .973 | .014 | 0 | 58 | .987 | .009 | 0 | 50 |
| 12 | .973 | .014 | 0 | 40 | .987 | .009 | 0 | 36 |
Note: SR = survival rate per one hundred women per twelve cycles of use, SE = standard error, Preg. = number of pregnancies per three cycles of use, and N = total number of women exposed.
Typical Use Unintended Pregnancy Rate
A total of four typical use unintended pregnancies occurred at twelve months and twelve cycles of use. The first pregnancy occurred at six months, within cycle zero. Two pregnancies occurred at nine months during cycle one and the last pregnancy occurred at twelve months in cycle four. The survival rate at twelve months and cycles of use was around 97 percent or three pregnancies per one hundred women at twelve months and twelve cycles of use. If we include the additional six pregnancies with a chart but without a pregnancy evaluation, there were three other typical-use pregnancies which would give a pregnancy rate of 95.3 percent (SE = .020, n = 93) for months of use and 95.2 percent (SE = .020, n = 102) for cycles of use.
A summary of the four unintended pregnancies (see Table 6) shows details about where the acts of intercourse resulting in conception were recorded on the charts and the table identifies other factors important for understanding each of the pregnancies. These factors included (1) the date of the infant's birth and if this was not available when the woman started charting, (2) how these acts related to the estimated day of ovulation, and, (3) a description of the menses before the conception cycle.
Table 6.
Characteristics of Unintended Pregnancies Included in Survival Analysis.
| User | Infant DOB or chart start date | Month of preg. when chart started or DOB | Cycle of preg. when chart started or if DOB provided | Act/s of I (related to the EDO or second peak day, e.g., P+/−) | Comments |
|---|---|---|---|---|---|
| 1 | May-2015 (inf. DOB) | 15 | 5 | P −4 or P + 3 | I's on CD 8, 9, and 10; FW started CD 7; Pregnancy occurred 15 months pp |
| 2 | Feb-2016 | 4 | 4 | P + 5 | FW started CD 7, I's on CD 21 |
| 3 | Nov-2015 | 15 | 3 | P + 3 | No menses were recorded |
| 4 | Jul-2016 | 2 | 1 | P + 6 | Mense score 10 over 5 days in pregnancy chart. FW CD6 – CD24. No I's during FW |
Note: Detailed description for each pregnancy and reason for classification. Abbreviations = Intercourse (I), fertile window (FW), estimated day of ovulation (EDO), cycle day (CD), and the peak day of fertility based on the last day of peak (P), date of birth (DOB).
Questions on the pregnancy evaluation included the couple's pregnancy intention. Responses included (1) the couple decided to conceive, (2) one person in the couple decided to conceive, (3) the couple took a chance, and (4) the couple did not think they were fertile. Of the four couples who indicated pregnancy was unintended, two couples recorded they took a chance, and two recorded they did not think they were fertile.
Discussion
This retrospective analysis of prospectively collected data from fertility charts recorded by postpartum breastfeeding women who used a revised protocol that integrated a urine hormone monitor demonstrated a correct-use pregnancy rate of two women per one hundred (i.e., 1,149 cycles), and typical-use pregnancy rate of four women per one hundred (i.e., 1,256 cycles). Results demonstrated a decrease in the number of pregnancies for women who used the revised protocol for the first six menstrual cycles compared to previously published studies (Fehring, Schneider, and Bouchard 2017, e133).
Results from past studies reported correct use pregnancy rates from women who used the original postpartum/breastfeeding protocol to be two and three per one hundred women over twelve months and twelve cycles of use (Bouchard, Fehring, and Schneider 2013, 40; Fehring, Schneider, and Bouchard 2017, e133 ; Mu, Fehring, and Bouchard 2020, 5). Typical use pregnancies in previous studies were eight pregnancies per one hundred women over twelve months of use (Mu, Fehring, and Bouchard 2020, 4–6) and 16 per one hundred women over twelve cycles of use (Fehring, Schneider, and Bouchard 2017, e132–e133). One study calculated the first six and twelve cycles of the postpartum/breastfeeding menstrual cycle transition, but it was unclear which protocol was being used (Fehring, Schneider, and Bouchard 2017, e132–e133) and the two other studies calculated pregnancy rates at twelve months of use (Bouchard, Fehring, and Schneider 2013, 36; Mu, Bouchard, and Fehring 2020, 4–6). The intent of this study was to focus on data from women who used the revised (i.e., current) protocol during the first six cycles postpartum.
A strength of this study is pregnancy rates have been reported both by months and by cycles of use. By counting cycle zero (i.e., lactation amenorrhea) as one cycle of use and calculating the pregnancy rate by menstrual cycles of use, this controls for ovulation occurring once in each cycle (i.e., even though cycle zero spans several months, there is usually only one chance of ovulation and conception). Calculating pregnancy rates as cycles and not months of use reduces the chance that pregnancy effectiveness rates are artificially deflated by the long duration of cycle zero. Also, by reporting results in both months and cycles of use these results can be used to compare with other studies, of which most pregnancy rates are reported as twelve months of use. A limitation of this study is that without both the conception cycle chart and the pregnancy evaluation there was no way to validate the pregnancy intention or if the couple was using the protocol, thus eliminating about half of the pregnancies for evaluation. Other threats to validity were the lack of a control group, multiple steps necessary for the data collection process, no randomization of subjects, and the use of retrospective data. (Feher Waltz, Strickland, and Lenz 2010).
Although this study showed women who used the revised protocol did experience fewer pregnancies the cost of the CBFM and online charting may have affected consistent use and contributed to large amounts of missing data. For women who begin testing at the recommended time of eight weeks postpartum the cost can be around US$600 for one year, however, if the protocol is started around five to six months the cost is around US$350–US$450 for the first year postpartum. The results of this study are important since over 61 percent of women learning this NFP method are postpartum and breastfeeding (Mu, Fehring, and Bouchard 2020. 4–6).
More research is needed to learn ways to reduce the cost of the protocol and increase accessibility. Future studies should address ways to improve accessibility and ease of use. One way to do this is to have women use a mobile app platform with a chart where the protocol is integrated into the fertility algorithm.
Supplemental Material
Supplemental material, sj-docx-1-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-2-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-3-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-4-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-5-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Acknowledgments
Thank you to the postpartum breastfeeding couples who used Natural Family Planning and charted their biological signs of fertility during one of the most difficult times in a couple's reproductive life.
Biographical Notes
Mary Schneider, PhD, APRN, MSN, FNP-BC, MMCP, received her PhD from Marquette University and is the Director of the Marquette University Institute for Natural Family Planning at the College of Nursing. She is a provider and educator for the Marquette Method of NFP and an active member of the Marquette Method Professional Association (MMPA). Her doctoral work and area of interest are in menstrual cycle patterns during the transition to fertility in postpartum breastfeeding women.
Richard J. Fehring, PhD, RN, FAAN, is Professor Emeritus and Director of the Marquette University College of Nursing Institute for Natural Family Planning. He received his master's and doctorate in nursing from the Catholic University of America and baccalaureate degrees in biology and nursing from Marquette University. He has published numerous articles, and book chapters and co-edited three books on human fertility. He is a science consultant to the Department of NFP United States Conference of Catholic Bishops. His research interests include the effectiveness of fertility awareness methods of family planning, marital responses to family planning, and religious and spiritual influences on human sexuality.
Thomas Paul Bouchard, MD, completed his undergraduate at McGill University. He spent three years doing research on dementia in Parkinson's disease at the University of Alberta. He then completed medical school and residency at the University of Calgary. He now practices general family medicine and is the medical director at Fr. Lacombe and Providence Care Centres. He is a Clinical Lecturer at the University of Calgary and sits on the Perinatal Palliative Care Committee. He has published articles on a wide variety of issues from Natural Family Planning to Parkinson's disease.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Mary M. Schneider https://orcid.org/0000-0001-8090-4971
Richard J. Fehring https://orcid.org/0000-0001-9071-4813
Supplemental Material: Supplemental material for this article is available online.
References
- Barron Mary Lee, Fehring Richard. 2005. “Basal body temperature assessment: Is it useful to couples seeking pregnancy?” MCN The American Journal of Maternal/Child Nursing, 30(5): 290–298. 10.1097/00005721-200509000-00004 [DOI] [PubMed] [Google Scholar]
- Behre H. M., Kuhlage J., Gassner C., Sonntag B., Schem C., Schneider H. P., Nieschlag E.. 2000. “Prediction of Ovulation by Urinary Hormone Measurements With the Home Use ClearPlan Fertility Monitor: Comparison With Transvaginal Ultrasound Scans and Serum Hormone Measurements.” Human Reproduction (Oxford, England) 15 (12): 2478–82. 10.1093/humrep/15.12.2478. [DOI] [PubMed] [Google Scholar]
- Bouchard T., Blackwell L., Brown S., Fehring R., Parenteau-Carreau S.. 2018. “Dissociation between cervical mucus and urinary hormones during the postpartum return of fertility in breastfeeding women.” The Linacre Quarterly 85 (4): 399–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard T., Fehring R. J., Schneider M.. 2013. “Efficacy of a new postpartum transition protocol for avoiding pregnancy.” Journal of the American Board of Family Medicine 26 (1): 35–44. 10.3122/jabfm.2013.01.120126. [DOI] [PubMed] [Google Scholar]
- Brown James B.2011. “Types of Ovarian Activity in Women and Their Significance: The Continuum (a Reinterpretation of Early Findings).” Human Reproduction Update 17 (2): 141–58. 10.1093/humupd/dmq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J. B., Harrisson P., Smith M. A.. 1985. “A Study of Returning Fertility After Childbirth and During Lactation by Measurement of Urinary Oestrogen and Pregnanediol Excretion and Cervical Mucus Production.” Journal of Biosocial Science S9 (September): 5–23. 10.1017/S0021932000025098. [DOI] [PubMed] [Google Scholar]
- Feher Waltz Carolyn, Strickland Ora Lea, Lenz Elizabeth R.. 2010. “Introduction to Measurement.” In Measurement in Nursing and Health Research, 4th ed., 3–26. New York: Springer publishing company. [Google Scholar]
- Fehring R. J., Schneider M.. 2008. “Variability in the hormonally estimated fertile phase of the menstrual cycle.” Fertility and Sterility, 90 (4): 1232–1235. 10.1016/j.fertnstert.2007.10.050. [DOI] [PubMed] [Google Scholar]
- Fehring R. J., Schneider M., Bouchard T.. 2017. “Effectiveness of an online natural family planning program for breastfeeding women.” Journal of Obstetric ,Gynecologic & Neonatal Nursing 46 (June): 1–9. 10.1016/j.jogn.2017.03.010. [DOI] [PubMed] [Google Scholar]
- Fehring R. J., Schneider M., Raviele K., 2006. “Variability in the phases of the menstrual cycle.” JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35 (3): 376–384. https://doi.org/DOI:10.1111/j.1552-6909.2006.00051.x. [DOI] [PubMed] [Google Scholar]
- Fehring R. J., Schneider M., Raviele K., Rodriguez D., Pruszynski J.. 2013. “Randomized comparison of two Internet-supported fertility-awareness-based methods of family planning.” Contraception, 88 (1): 24–30. 10.1016/j.contraception.2012.10.010. [DOI] [PubMed] [Google Scholar]
- Hatherley L. I.1985. “Lactation and Postpartum Infertility: The Use-Effectiveness of Natural Family Planning (NFP) After Term Pregnancy.” Clinical Reproduction and Fertility 3 (4): 319–34. [PubMed] [Google Scholar]
- Howard M P, Stanford J B. 1999. “Pregnancy Probabilities During Use of the Creighton Model Fertility Care System.” Archives of Family Medicine 8 (5): 391–402. http://www.ncbi.nlm.nih.gov/pubmed/10500511. [DOI] [PubMed] [Google Scholar]
- Johnson S., Weddell S., Godbert S., Freundl G., Roos J., Gnoth C.. 2015. “Development of the First Urinary Reproductive Hormone Ranges Referenced to Independently Determined Ovulation Day.” Clinical Chemistry and … 53 (7): 1099–1108. 10.1515/cclm-2014-1087. [DOI] [PubMed] [Google Scholar]
- Kennedy Kathy I., Gross Barbara A., Parenteau-Carreau Suzanne, Flynn Anna M., Brown James B., Visness Cynthia M.. 1995. “Breastfeeding and the Symptothermal Method.” Studies in Family Planning 26 (2): 107–15. 10.2307/2137936. [DOI] [PubMed] [Google Scholar]
- Klaus H., Goebel J., Muraski B., Egizio M., Weitzel D., Taylor R., Fagan M., Ek K., Hobday K.. 1979. “Use Effectiveness and Client Satisfaction in Six Centers Teaching the Billings Ovulation Method.” Contraception 19 (6): 613–29. https://www.contraceptionjournal.org/article/0010-7824(79)90008-8/pdf. [DOI] [PubMed] [Google Scholar]
- Mu Q., Fehring R. J., Bouchard T.. 2020. “Multisite effectiveness study of the marquette method of natural family planning program.” The Linacre Quarterly, 002436392095751. 10.1177/0024363920957515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos Judith, Johnson Sarah, Weddell Sarah, Godehardt Erhard, Schiffner Julia, Freundl Günter, Gnoth Christian. 2015. “Monitoring the Menstrual Cycle: Comparison of Urinary and Serum Reproductive Hormones Referenced to True Ovulation.” The European Journal of Contraception & Reproductive Health Care : The Official Journal of the European Society of Contraception 20 (6): 438–50. 10.3109/13625187.2015.1048331. [DOI] [PubMed] [Google Scholar]
- Severy L., Robinson J.. 2004. “Psychological Aspects of Achieving and Avoiding Pregnancy.” In In Integrating Faith and Science Through Natural Family Planning, edited by Fehring R., Notare T., 111–33. Milwaukee: Marquette University Press. [Google Scholar]
- Swiss Precision Diagnostics GmbH. 2015. Clearblue Fertility Monitor Instruction Booklet . https://www.clearblue.com/sites/default/files/wysiwyg/fam_booklet_800834-14.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-2-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-3-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-4-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly
Supplemental material, sj-docx-5-lqr-10.1177_00243639231167235 for Effectiveness of a Postpartum Breastfeeding Protocol for Avoiding Pregnancy by Mary M. Schneider, Richard J. Fehring and Thomas Paul Bouchard in The Linacre Quarterly