Abstract
Background
Prior to mid-2021, Australia’s approach to COVID-19 was to eliminate community transmission. However, between August-November 2021, the state of Victoria, Australia, experienced an outbreak of the Delta variant that continued to grow despite extensive lockdowns and public health measures in place. While these public health restrictions were ultimately unable to stop community transmission, they likely had a major impact reducing transmission and adverse health outcomes relative to voluntary risk-mitigation only (e.g., in response to rising cases and deaths, some people may avoid crowded settings, hospitality, retail, social occasions, or indoor settings). This study aims to estimate the impact of the August-November 2021 enforced public health restrictions in Victoria, compared to voluntary risk-mitigation only.
Methods
An agent-based model was calibrated to Victorian epidemiological, health and behavioural data from 1 August to 30 November 2021, as well as policies that were implemented over that period. Two counter-factual scenarios were run for the same period with (a) no restrictions in place; or (b) voluntary risk-mitigation only, based on behaviour measured over the December-January Omicron BA.1 epidemic wave when restrictions were not in place.
Results
Over August-November 2021, the baseline model scenario resulted in 97,000 (91,000−102,000) diagnoses, 9100 (8500−9700) hospital admissions, and 480 (430−530) deaths. Without any restrictions in place, there were 3,228,000 (3,200,000−3,253,000) diagnoses, 375,100 (370,200−380,900) hospital admissions, and 16,700 (16,000−17,500) deaths. With voluntary risk-mitigation equal to those observed during the Omicron BA.1 epidemic wave, there were 1,507,000 (1,469,000−1,549,000) diagnoses, 130,300 (124,500−136,000) hospital admissions, and 5500 (5000−6100) deaths.
Conclusion
Public health restrictions implemented in Victoria over August-November 2021 are likely to have averted more than 120,000 hospitalizations and 5000 deaths relative to voluntary risk-mitigation only. During a COVID-19 epidemic wave voluntary behaviour change can reduce transmission substantially, but not to the same extent as enforced restrictions.
Keywords: COVID-19, Modelling, Infectious diseases, Pandemic response, Retrospective, Analysis
1. Introduction
In 2020 and much of 2021, Australia pursued an “aggressive suppression” strategy for COVID-19, through border controls, isolation, quarantine, and extensive contact tracing together with other public health and social measures (i.e., “lockdowns” or other behavioural restrictions) to control outbreaks. Over this period the strategies implemented were largely successful in controlling outbreaks and bringing case numbers to zero. However, from early August 2021 the Australian state of Victoria experienced an outbreak of the Delta variant of COVID-19 which continued to grow despite extensive public health measures, including lockdowns. On August 5th 2021, Victoria reached 80 active COVID-19 cases in the community and extensive restrictive measures were enforced (Department of Health and Human Services, 2021). Under the restrictions, Victorians were only authorised to leave their homes for five reasons: essential shopping, exercise, care or caregiving, authorised work or education which could not be done from home, or vaccination. On these occasions people were required to wear masks. In parallel, vaccine availability and uptake increased; as of August 5th approximately 43 % of Victorians over 16 years of age had received their first dose of a vaccine and 21 % their second, with coverage being constrained largely by a limited supply. As vaccine doses became increasingly available the population coverage quickly increased, and by October 31st coverage had reached 96 % for first doses and 83 % for second doses.
Once it became clear that the enforced restrictions were not going to be able to prevent community transmission of the Delta variant, a policy shift was made. Under this paradigm restrictions were maintained with the aim of slowing and controlling the spread, rather than returning to zero cases. But the supply constraints on vaccines meant that restrictions would be required until sufficient vaccination coverage was achieved such that removing them would not overload the health system. The Victorian government developed a “roadmap” of restriction eases which would be triggered at predefined vaccine coverage thresholds, an adaptation of a similar strategy implemented during a lockdown in 2020, in which eases were triggered at set dates and case thresholds (Premier of Victoria, 2021, Coronavirus (COVID-19) Victoria, 2020). Despite the public health and social measures (PHSM) being ultimately unable to stop community transmission, it is likely that their implementation (and the conservative way they were relaxed) had a significant impact on the trajectory of the outbreak and therefore on the magnitude of the mortality due to COVID-19 observed over August-November 2021.
To measure the impact of these restrictions on health outcomes, a counter-factual scenario must be designed that reflects a theoretical situation where they were not imposed. This counter-factual scenario is difficult to specify, since without enforcement of strict PHSM some degree of voluntary risk-mitigation would likely have occurred anyway. For example, during the Omicron BA.1 variant outbreak which began in Victoria in late December 2021, the most significant measure reintroduced by the Victorian government was indoor mask mandates, however the observed decrease in population-level mobility was proportional to that seen during previous lockdowns, despite not being enforced (Byrne, 2022). The term coined in reference to this behaviour was a “Shadow Lockdown”. Google mobility data for Victoria indicates that public transit movement was down by approximately 60 %; workplace, retail, recreation, and public park movement decreased by 20–40 %; and residential movement increased by 10–20 % over the January-February 2022 period (Google, 2022). Additionally, a behavioural survey (Optimise) taken at the time found that more than 50 % of participants “mostly” or “always” behaved in ways which reduced their risk of exposure, such as avoiding public transport, crowded locations, and social gatherings (Hellard et al., 2022).
The aim of this study was to estimate the COVID-19 infections, hospitalizations and deaths prevented by the enforced public health restrictions over August-November 2021 in Victoria, compared to voluntary risk-mitigation only (the Shadow Lockdown), or if there were no restrictions or risk-averse behaviours undertaken at all.
2. Methods
We used an established agent-based microsimulation model, Covasim, developed by the Institute for Disease Modelling (USA) and collaborators including the Burnet Institute, to model epidemics in Victoria (Kerr et al., 2021). The model is open source and available online (Covasim model GitHub repository). The model and its calibration to the Victorian Delta epidemic wave in 2021 is described in detail elsewhere (Scott et al., 2020), with additional details in the Supplementary materials. As a summary, agents in the model are assigned an age (which affects contact networks and infection outcomes) and are added to contact networks for key settings of transmission such as households, schools, and workplaces, as well as broader community settings like restaurants, pubs, places of worship, community sport, and small social gatherings. Additionally, agents receive vaccines with characteristics matching the Pfizer and AstraZeneca vaccines which were available in Australia at the time, with age-specific allocations and dose scheduling matched to data from the Australian Immunisation Registry (Abeysuriya et al., 2020). Additional details are available in (Scott et al., 2020, Abeysuriya et al., 2020, Abeysuriya et al., 2021, GOV.UK, 2022), and in the Supplementary materials.
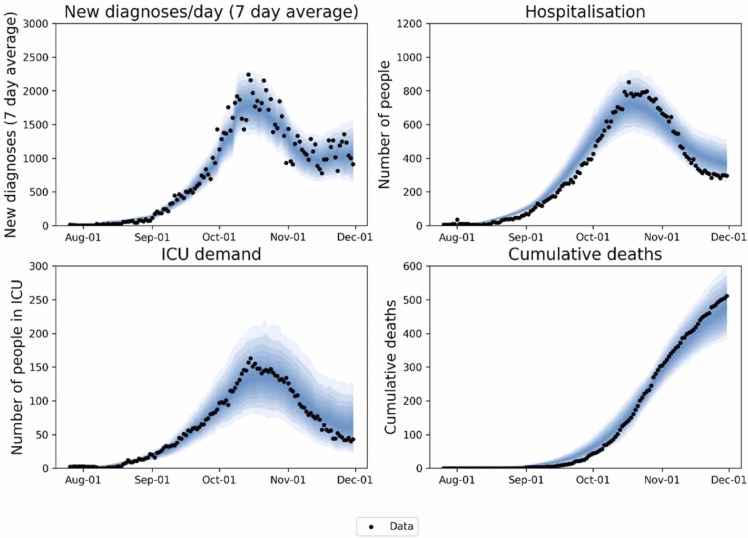
Three scenarios were considered in the analysis. First, a baseline scenario (i.e., “Mandatory PHSM”), which was calibrated to the empirical observed epidemic trajectory ( Fig. 1). This baseline scenario was then compared to two counter-factual scenarios, with (a) no enforced restrictions and no voluntary risk-mitigation (i.e., “No behaviour change”); or (b) no enforced restrictions but voluntary risk-mitigation (i.e., “Voluntary behaviour change”). A comparison of restriction levels and timings can be found in Table 1.
Fig. 1.
Model baseline scenario, i.e., “Mandatory PHSM”. Outputs from model simulations which match the observed data over the calibration period. The model was calibrated against diagnoses, hospitalisations, ICU demand, and deaths over the Aug-Nov 2021 period.
Table 1.
Timelines of modelled restrictions. “Mandatory PHSM”, “No behaviour change” and “Voluntary behaviour change” run until November 30 2021 for the primary analysis. “Delta resurgence” runs until March 31 2022, and “Voluntary behaviour change” is rerun for the extended duration for comparison. Policy impacts detailed in Table S 3 in the Supplementary materials.
 |
1Work from home. 2Limit of one person per 4 square metres of venue space.
The extent of voluntary risk-mitigation was estimated based on behaviour measured over the December-January Omicron BA.1 epidemic wave, when no significant public health restrictions were in place in Victoria. The impacts of these behaviours on transmission within the model were estimated by calibrating the model to fit the case, hospitalisation, and mortality data over this period, while broadly aligning with the observed reductions in mobility, and risk-avoidant behaviours noted in Google mobility reports and the Optimise study (Google, 2022, Hellard et al., 2022). The resulting model inputs for this scenario are that transmission probability for agents in the model in their social and community networks such as pubs, bars, public transport, and social gatherings is reduced by approximately 30–70 % (varying by network). Model scenarios were run over August-November 2021 inclusive.
It is possible that enforced PHSM could be considered to simply delay an epidemic wave until restrictions are lifted, rather than to avert negative outcomes completely. In Victoria it is not possible to know whether a resurgence in Delta variant cases would have occurred after PHSM were lifted, because the Omicron BA.1 variant began to circulate and became dominant in late 2021. However, it is possible to model an additional counter-factual scenario (“Delta resurgence”) that considers the time after PHSM are lifted, but without the Omicron BA.1 variant. This provides a method to assess the potential for a Delta variant epidemic resurgence, and to estimate whether the infections and deaths averted by the lockdown would have occurred anyway once restrictions were lifted. In the “Delta resurgence” scenario, restrictions were equivalent to the “Mandatory PHSM” scenario, until they were eased to the level of the “Voluntary behaviour change” scenario from December 1st 2021 (see Table 1), and the model run was extended until the end of March 2022, but without the Omicron BA.1 variant.
3. Results
Over August-November 2021, the “Mandatory PHSM” model scenario resulted in 96,935 (91,426−102,467) diagnoses, 9105 (8483−9742) hospital admissions, and 478 (433−526) deaths (Fig. 1 and Table 2).
Table 2.
Cumulative outcomes over Aug-Nov 2021. Cumulative infection, diagnosis, hospital admission, ICU admission and mortality outcomes for the “Mandatory PHSM” scenario, “Voluntary behaviour change” counter-factual, and “No behaviour change” counter-factual.
| Scenario | Total infections Aug-Nov 2021 | Total diagnoses Aug-Nov 2021 | Total hospital admissions Aug-Nov 2021 | Total ICUaadmissions Aug-Nov 2021 | Total deaths Aug-Nov 2021 |
|---|---|---|---|---|---|
| Mandatory PHSM | 177,323 (168,170–187,899) | 96,935 (91,426–102,467) | 9105 (8483–9742) | 1581 (1446–1737) | 478 (433–526) |
| No behaviour change | 4,591,749 (4,564,532–4,618,075) | 3,227,677 (3,200,722–3,253,147) | 375,127 (370,188–380,875) | 62,245 (60,699–63,863) | 16,700 (15,972–17,497) |
| Voluntary behaviour change | 2,245,212 (2,187,945–2,311,337) | 1,507,505 (1,469,109–1,548,982) | 130,267 (124,487–136,032) | 19,553 (18,376–20,758) | 5507 (5018–6078) |
Intensive care unit
In the “No behaviour change” scenario, there were 3,227,677 (3,200,722−3,253,147) diagnoses, 375,127 (370,188−380,875) hospital admissions, and 16,700 (15,972−17,497) deaths. Comparing to the “Mandatory PHSM” results indicates that the enforced PHSM over the August-November period are estimated to have averted more than 96 % of the diagnoses and adverse outcomes.
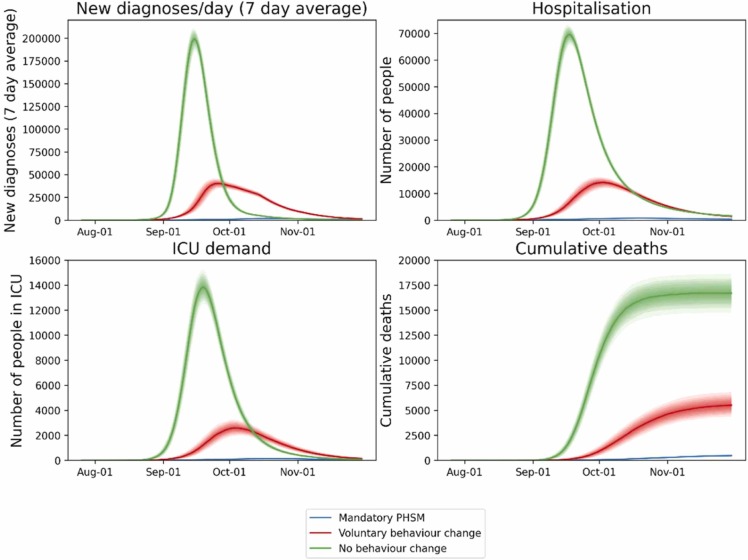
In the “Voluntary behaviour change” scenario, there were 1,507,505 (1,469,109−1,548,982) diagnoses, 130,267 (124,487−136,032) hospital admissions, and 5507 (5018−6078) deaths ( Fig. 2 and Table 2). So, we estimate that the enforced PHSM averted more than 91 % of the diagnoses and adverse outcomes observed in the “Voluntary behaviour change” scenario ( Fig. 3 and Table 3).
Fig. 2.
Model baseline and two counter-factual scenarios. Blue: the “Mandatory PHSM” scenario, in which PHSM were implemented and eased according to the Victorian government’s roadmap (i.e., Fig. 1). Red: a “Voluntary behaviour change” scenario with no enforced restrictions but voluntary risk-mitigation. Green: a “No behaviour change” scenario with no enforced restrictions or voluntary risk-mitigation.
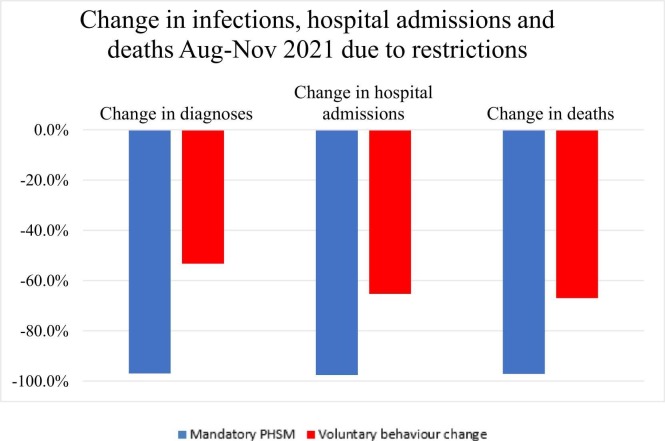
Fig. 3.
PHSM and behavioural change impacts. Percentage reductions achieved in the “Mandatory PHSM” and “Voluntary behaviour change” scenarios, relative to “No behaviour change” scenario.
Table 3.
PHSM and behavioural change impacts. Percentage reductions achieved in the “Mandatory PHSM” and “Voluntary behaviour change” scenarios, relative to “No behaviour change” scenario.
| Relative impacts of scenarios | % infections averted Aug-Nov 2021 | % diagnoses averted Aug-Nov 2021 | % hospital admissions averted Aug-Nov 2021 | % ICUaadmissions averted Aug-Nov 2021 | % deaths averted Aug-Nov 2021 |
|---|---|---|---|---|---|
| Mandatory PHSM relative to No behaviour change | 96.1 % (4,414,426) | 97.0 % (3,130,542) | 97.6 % (366,022) | 97.5 % (60,664) | 97.1 % (16,222) |
| Voluntary behaviour change relative to No behaviour change | 51.1 % (2,346,537) | 53.3 % (1,719,972) | 65.3 % (244,860) | 68.6 % (42,692) | 67.0 % (11,193) |
| Mandatory PHSM relative to Voluntary behaviour change | 92.1 % (2,067,889) | 93.6 % (1,410,570) | 93.0 % (121,162) | 91.9 % (17,972) | 91.3 % (5029) |
Intensive care unit
It is worth noting that the risk-mitigation behaviours modelled in the “Voluntary behaviour change” had a significant impact themselves, averting 53 % of diagnoses and more than 65 % of severe outcomes relative to the “No behaviour change” scenario (Table 3). Both counter-factual scenarios have significantly higher and earlier peaks than occurred (and therefore to what the “Mandatory PHSM” scenario was calibrated). The lack of policy restrictions allows for a higher rate of transmission within the model and thus faster and more aggressive growth (Fig. 2). The “Voluntary behaviour change” scenario also led to a more elongated epidemic wave, with a greater proportion of infections occurring when vaccine coverage was higher, and hence a slightly lower case fatality rate (0.36 % versus 0.52 % in the “No behaviour change” scenario).
The “Delta resurgence” counter-factual scenario indicated that a second Delta variant wave could have occurred over December 2021-March 2022, had the Omicron BA.1 variant not taken over (see Figure S 1 and Figure S 2 in the Supplementary materials). However, the estimated number of infections was only 16 % of those observed in the August-November wave in the “Voluntary behaviour change” scenario, despite having equivalent behaviours and restrictions. Overall, we found that even if we include infections, hospitalizations, and deaths occurring from this hypothetical resurgence, the implemented restrictions still averted 77 % of infections and 83 % of deaths relative to the “Voluntary behaviour change” scenario by postponing the outbreak until high levels of vaccination could be achieved (Table S 1 in the Supplementary materials).
4. Discussion
This study estimated the impact of voluntary risk-mitigation, and enforced PHSM, on COVID-19 related outcomes in Victoria over the August-November 2021 Delta variant outbreak. While the enforced PHSM in Victoria over this period were unable to prevent the Delta variant COVID-19 outbreak, our results indicate that they were nonetheless effective mechanisms for “flattening the curve” and preventing significant morbidity and mortality (Abeysuriya et al., 2021). Without any restrictions or voluntary risk-mitigation, we estimated there could have been 16,700 deaths over this period. The “No behaviour change” scenario is clearly an implausible counter-factual, as it is difficult to imagine that an unvaccinated population facing a significant outbreak of COVID-19 would continue to behave “as usual”. As such, the “Voluntary behaviour change” counter-factual provides a more realistic estimate of population level behaviours, and suggests that had the government not enforced any PHSM then voluntary risk-mitigation would likely have had a substantial impact, reducing this from 16,700 to 5507 deaths. However, the enforcement of PHSM likely played a significant role, further reducing this to 478 deaths in the “Mandatory PHSM” scenario, which includes the full impact of the PHSM and observed behaviours.
Although the aim of this analysis is to estimate the impact of the PHSM on infections, hospitalisations, and deaths, it is also clear that voluntary risk-mitigation and behaviour changes can have a significant impact on population level outcomes during an outbreak. Taking personal responsibility for their own safety, and the safety of others, and interacting with fewer individuals across a range of settings, could help a population prevent more than 50 % of cases and severe outcomes compared to a scenario with no such changes. However, while these impacts are significant, they come with the caveat that not every member of a community can reasonably or safely stop going to work, or visiting vulnerable family and friends. As such, an overreliance on “personal responsibility” can place an undue burden of both disease and stigma on the members of the community who are less able to mitigate exposure and transmission risk, particularly those with structural and social disadvantage. This suggests there remains a clear role for government, as they can introduce measures to reduce risk for those who are unable to engage in voluntary risk-reduction, for example through work from home orders, indoor mask use and isolation of cases. They can also provide support that enables people to follow such measures such as payment to people with casualised work that enable them to stay at home when infected with COVID-19.
We also considered whether the implementation of restrictions only postpones the epidemic wave, rather than truly averting infections and deaths. Even after the restrictions were eased in Victoria in late October and early November, daily diagnoses remained relatively stable until the emergence of the Omicron BA.1 variant in December. The introduction of a new variant occurred so soon after the restrictions were eased that it is difficult to know if a resurgence of the Delta variant would have occurred over the summer. The results of our final counter-factual scenario indicates that another outbreak could have occurred in the absence of the Omicron BA.1 variant, but that by virtue of delaying the outbreak until high levels of vaccination could be achieved the outcomes were improved. Vaccination provides significant protection against both transmission and severe disease outcomes, and remains one of the most effective and least socially restrictive PHSM available to policy makers (GOV.UK, 2022). However, protection from vaccination can wane over time, and as observed over 2022 new variants can appear with immune evasive characteristics that reduce the individual and population-level impact of vaccines. Therefore, additional long-term measures and behaviour changes which can further reduce the transmission potential of the virus (such as improved air quality or targeted mask wearing) should continue to be considered by policy makers and individuals alike.
Several other modelling studies in other contexts have estimated the impacts of NPIs and vaccination on outbreaks of COVID-19 (Bisanzio et al., 2022, Vilches et al., 2022, Fair et al., 2022), however it is not feasible to compare findings across these studies as a form of validation as there are significant differences in modelling approaches, demographics, disease contexts, and scenarios compared. For example, in this study, the ratio of cumulative modelled diagnoses and deaths between the three scenarios was approximately 1:13:35 (“Mandatory PHSM”: “Voluntary behaviour change”: “No behaviour change”). Other studies have reported ratios of 1:9 for cumulative cases and deaths (“Mask 80 % | Distancing 70 %”: “No NPIs” in the Kingdom of Saudi Arabia in mid-late 2020 (Bisanzio et al., 2022)), 1:5 for peak daily cases and 1:14 for cumulative cases (“Observed data”: “No NPIs” in two different outbreaks in Nunavut, Canada in late 2020 and early 2021 (Vilches et al., 2022)), and 1:105 for peak daily cases and 1:64 for cumulative deaths (“Reported data”: “No NPIs” in Ontario, Canada in early-mid 2020 (Fair et al., 2022)). There is a significant range in the estimated impacts of NPIs across these studies, and while our reported ratios fall within this range, the differences in population sizes and disease contexts across the studies mean that we cannot know how well our estimated NPI impacts align with those found by other analyses.
There are many other limitations in the use of modelling to study COVID-19 outbreaks. Most significantly, models are simplifications of the real world and cannot capture the full range of human behaviour. For example, model outcomes are driven by the number of infections, but we can only ever calibrate the model to diagnosed cases and estimate what the case ascertainment rate is. In these results the case ascertainment rate for the calibrated “Mandatory PHSM” scenario was ∼55 % (∼68 % for the counter-factual scenarios), and unfortunately there is little data against which to validate this. This rate arises largely from the symptomatic testing probability parameter within the model, which controls the likelihood of symptomatic agents having a test on any given day. This was calibrated to a cumulative probability of ∼22 %–33 % over seven days of symptoms in September 2021, which is approximately in line with the September 2021 testing behaviour findings of a COVID-19 behavioural survey (Optimise) (Saich et al., 2021). As it is unknown what the actual case ascertainment rate was over this period it is unclear whether the modelled ascertainment rate makes these results optimistic or pessimistic compared to reality. A limitation specific to the counter-factual “Voluntary behaviour change” scenario is that the estimated behaviour changes relate to those observed during the Omicron BA.1 epidemic wave in Victoria from December 2021-January 2022. This is a context of higher vaccine coverage and a less severe variant in circulation than during the August-November 2021 Delta outbreak considered in this study. Therefore, if mandatory PHSM had not been in place, voluntary risk-mitigation during the August-November 2021 Delta outbreak may have been greater than we have estimated.
Furthermore, there are many things that are unknown about COVID-19 disease dynamics, and models must approximate these with the evolving results from clinical trials and observational studies. During the outbreak, the implementation of vaccination within the model assumed a linear increase in protection against COVID-19 after each dose, but did not account for the waning of immunity post-vaccination (or post-infection). The counter-factual scenarios may be underestimated because testing capacity was assumed to scale with the outbreak size, which would not have been possible had these scenarios occurred. Similarly, the health care system would have been overwhelmed at a fraction of the modelled numbers, and inadequate care provided, exacerbating outcomes. These factors likely make the outcomes of the scenarios optimistic, however this work also does not include booster vaccination doses, which began in early November 2021, and may make the results slightly pessimistic.
5. Conclusion
The enforced PHSM over the 2021 Delta variant outbreak in Victoria are estimated to have averted about 121,162 hospitalizations and 5029 deaths over August-November compared to a counter-factual of voluntary risk-mitigation only. During a COVID-19 epidemic wave voluntary behaviour change can reduce transmission substantially, but not to the same extent as enforced restrictions.
CRediT authorship contribution statement
Dominic Delport: Conceptualization, Methodology, Software, Formal analysis, Investigation, Writing – original draft, Writing – review and editing, Visualization. Rachel Sacks-Davis: Methodology, Software, Writing – review and editing. Romesh Abeysuriya: Methodology, Software, Writing – review and editing. Margaret Hellard: Writing – review and editing. Nick Scott: Conceptualization, Methodology, Software, Writing – review and editing, Supervision, Project administration.
Declaration of Competing Interest
DD, RSD, RGA MH, NS have received funding from the Department of Health, State Government of Victoria, Australia for COVID-19-related work. DD is the recipient of a PhD scholarship from the National Health and Medical Research Council, Australia.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.epidem.2023.100702.
Appendix A. Supplementary material
Supplementary material
.
Data availability
I have provided a link to the published code and result files for this analysis in the supplementary materials.
References
- Abeysuriya R., Delport D., Hellard M., Scott N. Estimating risks associated with early reopening in Victoria. Melbourne (AU): Burnet Institute; 2020 Sep 26. 12p. Available from: https://burnet.edu.au/system/asset/file/4241/Burnet_Institute_COVASIM_Resurgence_analysis_2020-09-26.pdf.
- Abeysuriya R., Delport D., Sacks-Davis R., Hellard M., Scott N. Modelling the Victorian roadmap 2021. Melbourne (AU): Burnet Institute; 2021 Sep 18. 23p. Available from: https://www.burnet.edu.au/system/asset/file/4942/Burnet_Institute_VIC_Roadmap_20210918_-FINAL.pdf.
- Bisanzio D., Reithinger R., Alqunaibet A., et al. Estimating the effect of non-pharmaceutical interventions to mitigate COVID-19 spread in Saudi Arabia. BMC Med. 2022;20(51) doi: 10.1186/s12916-022-02232-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne, R. mobility-aus [Internet]. [Place unknown]: Github, Inc. [updated 2022 Mar 29; cited 2022 Aug 21]. Available from: https://rsbyrne.github.io/mobility-aus.
- Coronavirus (COVID-19) Victoria[Internet]. Melbourne: State Government of Victoria (AU). Victoria’s roadmap for reopening – How we live in Victoria; 2020 Sep 5 [cited 2022 Aug 21]. Available from: https://www.coronavirus.vic.gov.au/sites/default/files/2020-11/Victoria%27s%20roadmap%20for%20reopening%20-%20How%20we%20live%20in%20Victoria.pdf.
- Covasim model GitHub repository. Available from: https://github.com/InstituteforDiseaseModeling/covasim.
- Department of Health and Human Services [Internet]. Melbourne: State Government of Victoria(AU). Coronavirus update for Victoria – 5 August 2021; 2021 Aug 5 [cited 2022Aug 21]. Available from: https://www.dhhs.vic.gov.au/coronavirus-update-victoria-5-august-2021.
- Fair K.R., Karatayev V.A., Anand M., Bauch C.T. Estimating COVID-19 cases and deaths prevented by non-pharmaceutical interventions, and the impact of individual actions: a retrospective model-based analysis. Epidemics. 2022:39. doi: 10.1016/j.epidem.2022.100557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Google L.L.C. [Internet]. [place unknown]: Google LLC. Google COVID-19 Community Mobility Reports. [updated 2022 Aug 21; cited 2022 Aug 21]. Available from: https://www.google.com/covid19/mobility.
- GOV.UK [Internet]. [Place unknown]: Government Digital Services (UK). [cited 2022 Aug 24]. SPI-M-O: Summary of further modelling of easing restrictions – Roadmap Step 4. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1075056/S1287_SPI-M-O_Summary_Roadmap_step_4.pdf.
- Hellard M., Gibney K., Stoové M., Young K., Altermatt A., Heath K., Thomas A., Nguyen T., Wilkinson A., Merner B., Hill S., Saich F., Jin D. The Optimise Study: Summer 2021–2022 Snapshot, Special report. Melbourne (AU): Burnet Institute; 2022 Apr. 20p. Available from: https://optimisecovid.com.au/wp-content/uploads/2022/04/Optimise_snapshot_summer_final-1.pdf.
- Kerr C.C., Stuart R.M., Mistry D., Abeysuriya R.G., Rosenfeld K., Hart G.R., et al. Covasim: An agent-based model of COVID-19 dynamics and interventions. PLOS Comp. Biol. 2021;17(7) doi: 10.1371/journal.pcbi.1009149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premier of Victoria[Internet]. Melbourne: State Government of Victoria (AU). Victoria’s Roadmap: Delivering the National Plan; 2021 Sep 19 [cited 2022 Aug 21]. Available from: https://www.premier.vic.gov.au/sites/default/files/2021-09/210919%20-%20Roadmap-Delivering%20the%20National%20Plan.pdf.
- Saich F., Heath K., Altermatt A., Munari S., Merner B., Hill S., Stoové M., Gibney K., Hellard M. The Optimise Study: COVID-19 testing and vaccination, Report 11. Melbourne (AU): Burnet Institute; 2021 Oct. 11p. Available from: https://optimisecovid.com.au/wp-content/uploads/2021/11/Optimise_REPORT11_final.pdf.
- Scott N., Palmer A., Delport D., Abeysuriya R., Stuart R., Kerr C.C., et al. Modelling the impact of relaxing COVID‐19 control measures during a period of low viral transmission. Med. J. Aust. 2020;214(2):79–83. doi: 10.5694/mja2.50845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilches T.N., Abdollahi E., Cipriano L.E., et al. Impact of non-pharmaceutical interventions and vaccination on COVID-19 outbreaks in Nunavut, Canada: a Canadian Immunization Research Network (CIRN) study. BMC Public Health. 2022;22(1042) doi: 10.1186/s12889-022-13432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
I have provided a link to the published code and result files for this analysis in the supplementary materials.