Abstract
Calcaneal fracture is one of the most common foot and ankle fractures, but the best treatment of this fracture is still under debate. No matter the treatment strategy of this intra-articular calcaneal fracture, early and late complications frequently occur. In order to treat these complications, combination of various ostectomy, osteotomy, and arthrodesis techniques have been proposed to re-establish the calcaneal height, restore the talocalcaneal relationship, and create a stable, plantigrade foot. In contrast to this approach of addressing all the deformities, another feasible approach is concentrating on those aspects that are the most clinically pressing.10, 11, 12, 13, 14, 15 Different arthroscopic and endoscopic approaches focused on the patient’s symptoms and not the correction of the talocalcaneal relationship or restoration of the height or length of the calcaneus have been proposed to deal with late complications of calcaneal fractures. The purpose of this technical note is to describe the details of endoscopic screw removal, debridement of the peroneal tendons, and subtalar joint and lateral calcaneal ostectomy for management of chronic heel pain after calcaneal fracture. It has the advantage of dealing with various sources of lateral heel pain after calcaneal fracture, including the subtalar joint, peroneal tendons, lateral calcaneal cortical bulge and screws.
Technique Video
Endoscopic screw removal, debridement of the peroneal tendons and subtalar joint, and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The back-out screws are removed with the corresponding screw driver. The peroneal tendons are examined, and synovectomy and debridement of the torn tendons are performed with an arthroscopic shaver. The fibrous tissue of the posterior subtalar joint and sinus tarsi is debrided, and the fibrotic soft tissue envelop is stripped from the lateral calcaneal wall in order to expose the bony prominence. The bony prominence is then resected with an arthroscopic acromionizer.
Introduction
Calcaneal fracture is one of the most common foot and ankle fractures, and 75% of them are intra-articular.1,2 Although it is a common fracture, the best treatment of this fracture is still under debate.1, 2, 3, 4 If surgical treatment is considered, the surgeons should aim at anatomic restoration of the calcaneus architecture (height, width, and axis) and to restore the congruency of the subtalar and calcaneocuboid joint surfaces.3,5 Screw fixation compared to plating may be more difficult to restore the calcaneal width.6
However, many patients may experience poor outcomes, despite achieving apparent anatomic reduction. Adjunct arthroscopy to identify missed concomitant injuries and subtle articular malreduction has been proposed as a vehicle to enhance functional results for these patients.7 Moreover, minimally invasive approaches tend to preserve blood supplies and, thus, may lead to faster healing times and less chance of wound complications compared to traditional extensile approaches.2,4,7,8
No matter the treatment strategy of this intra-articular calcaneal fracture, early and late complications frequently occur and include wound complications and soft tissue necrosis, neurovascular injuries, malunion, nonunion, subtalar arthritis, calcaneofibular impingement and subsequent peroneal tendinitis, tibiotalar impingement due to dorsiflexion of the talus resulting in anterior ankle pain, flattening of the medial longitudinal arch, loss of hindfoot height or excessive varus or valgus, shortening and weakness of the gastrocnemius-soleus complex, sural neuritis, and leg length discrepancy.1,2,9, 10, 11, 12, 13, 14, 15
In order to treat these complications, a combination of various ostectomy, osteotomy, and arthrodesis techniques have been proposed to reestablish the calcaneal height, restore the talocalcaneal relationship, and create a stable, plantigrade foot.9 In contrast to this approach of addressing all the deformities, another feasible approach is concentrating on those aspects that are the most clinically pressing.10, 11, 12, 13, 14, 15 Different arthroscopic and endoscopic approaches focused on the patient’s symptoms and not the correction of the talocalcaneal relationship or restoration of the height or length of the calcaneus have been proposed to deal with late complications of calcaneal fractures.10, 11, 12, 13, 14, 15
The purpose of this technical note is to describe the technical details of endoscopic screw removal, debridement of the peroneal tendons and subtalar joint and lateral calcaneal ostectomy for management of chronic lateral heel pain after calcaneal fracture. It is indicated for lateral heel pain due to calcaneofibular impingement and peroneal tendon impingement by screws after open reduction and internal fixation of calcaneal fracture. It is contraindicated if the lateral heel pain is a result of severe subtalar osteoarthritis, sural neuritis, and impingement by plate; symptoms related to hindfoot malalignment or calcaneal shortening; and anterior ankle impingement related to severe collapse of posterior calcaneal facet and dorsiflexion of talus (Table 1).
Table 1.
Indications and Contraindications of Endoscopic Screw Removal, Debridement of the Peroneal Tendons, and Subtalar Joint and Lateral Calcaneal Ostectomy for Management of Chronic Heel Pain After Calcaneal Fracture
| Indications | Contraindications |
|---|---|
|
|
Surgical Technique
Preoperative Planning and Patient Positioning
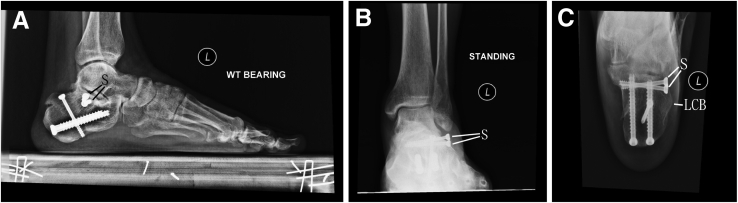
The anatomical site of pain should be determined clinically. Radiographs and computed tomogram are important to detect any screw back out, lateral cortical bulging of the calcaneus, and subtalar arthritis or hindfoot deformity (Fig 1).
Fig 1.
Endoscopic screw removal, debridement of the peroneal tendons, and subtalar joint and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. Radiographs of the illustrated foot showed the back out screws (S) and lateral calcaneal bony prominence (LCBP). There was no significant degeneration or intra-articular malunion of the posterior subtalar joint. A, lateral view; B, anteroposterior view; C, axial view.
The patient is in the lateral position. A thigh tourniquet is applied to provide a bloodless operative field. Fluid inflow is by gravity, and no arthro-pump is used. A 2.7-mm 30° arthroscope is used for this procedure.
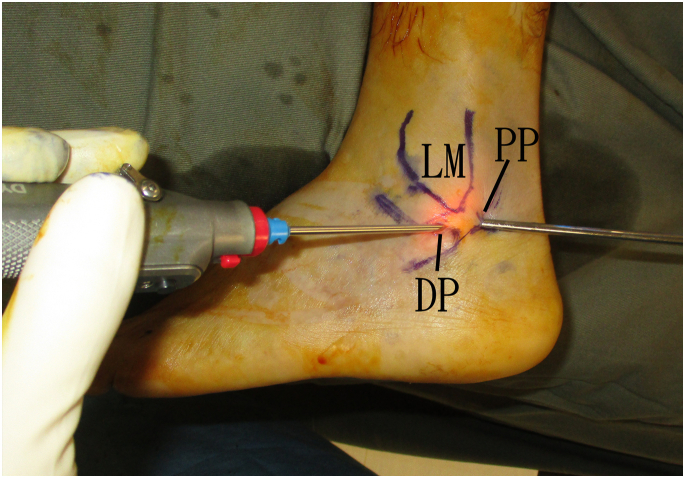
Portal Placement
This procedure is performed via the distal and proximal portals along the peroneal tendon sheath. The proximal portal is at the point where the peroneal tendons cross the posterior edge of the posterior subtalar joint. The distal portal is at the point closest to the posterior subtalar joint and the screw heads (Fig 2).
Fig 2.
Endoscopic screw removal, debridement of the peroneal tendons and subtalar joint and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. This procedure is performed via the distal and proximal portals along the peroneal tendon sheath. The proximal portal is at the point where the peroneal tendons cross the posterior edge of the posterior subtalar joint. The distal portal is at the point closest to the posterior subtalar joint and the screw heads. DP, distal portal; LM, lateral malleolus; PP, proximal portal.
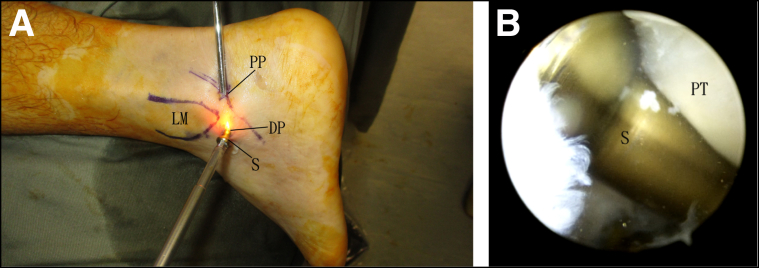
Endoscopic Removal of the Screws
The proximal portal is the viewing portal, and the distal portal is the working portal. The screw heads of the back-out screw can be easily identified after the peroneal tendons are retracted. The screws are removed via the distal portal by means of the corresponding screw driver (Fig 3).
Fig 3.
Endoscopic screw removal, debridement of the peroneal tendons and subtalar joint and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. The proximal portal is the viewing portal and the distal portal is the working portal. The screw heads of the back out screw can be easily identified after the peroneal tendons are retracted. The screws are removed via the distal portal by mean of the corresponding screw driver. (A) Clinical photo. (B) Arthroscopic photo. DP, distal portal; LM, lateral malleolus; PT, peroneal tendons; PP, proximal portal; S; screw.
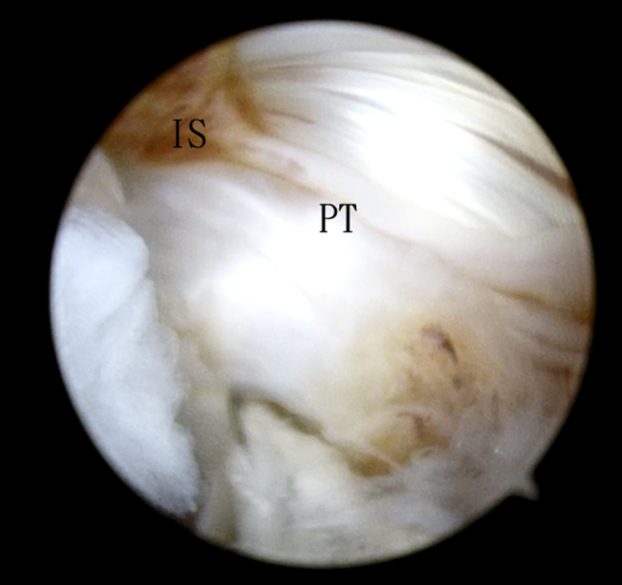
Debridement of the Peroneal Tendons
The proximal portal is the viewing portal and the distal portal is the working portal. The peroneal tendons are examined for any tenosynovitis or tears. Synovectomy is performed, and the torn tendons are debrided with an arthroscopic shaver (Dyonics, Smith and Nephew, Andover, MA) (Fig 4).
Fig 4.
Endoscopic screw removal, debridement of the peroneal tendons, and subtalar joint and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in the lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The peroneal tendons are examined for any tenosynovitis or tears. Synovectomy is performed and the torn tendons are debrided with an arthroscopic shaver. IS, inflamed synovium; PT, peroneal tendons.
Debridement of the Subtalar Joint
The proximal portal is the viewing portal, and the distal portal is the working portal. The fibrous tissue and inflamed synovium of the sinus tarsi and lateral capsule of the posterior subtalar joint is debrided with the shaver (Fig 5). The fibrotic soft tissue envelope is stripped from the lateral calcaneal wall by means of the shaver. The stripping is extended anteriorly to expose all the bony prominence of the lateral calcaneal wall.
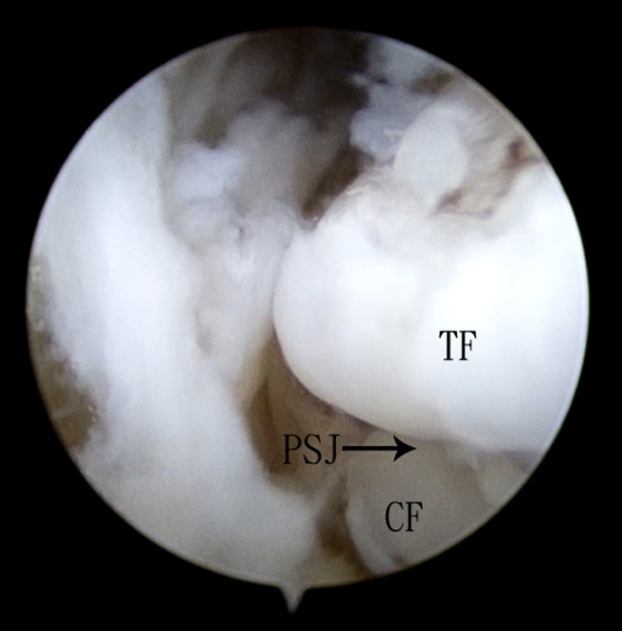
Fig 5.
Endoscopic screw removal, debridement of the peroneal tendons, and subtalar joint and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in the lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The fibrous tissue and inflamed synovium of the sinus tarsi and lateral capsule of the posterior subtalar joint is debrided with an arthroscopic shaver. CF, calcaneal facet; PSJ, posterior subtalar joint; TF, talar facet.
Lateral Calcaneal Ostectomy
The proximal portal is the viewing portal, and the distal portal is the working portal. The bony prominence of lateral calcaneal wall is removed by means of an arthroscopic acromionizer (Dyonics, Smith and Nephew, Andover, MA) (Fig 6, Video 1, Table 2). Postoperatively, the patient is allowed free mobilization and weight bearing walking as pain tolerated.
Fig 6.
Endoscopic screw removal, debridement of the peroneal tendons, and subtalar joint and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in the lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The bony prominence of lateral calcaneal wall is removed by means of an arthroscopic acromionizer. AA, arthroscopic acromionizer; LCW, lateral calcaneal wall.
Table 2.
Pearls and Pitfalls of Endoscopic Screw Removal, Debridement of the Peroneal Tendons, and Subtalar Joint and Lateral Calcaneal Ostectomy for Management of Chronic Heel Pain After Calcaneal Fracture
| Pearls | Pitfalls |
|---|---|
|
|
Discussion
The reported minimal invasive technique has the advantage of dealing with various sources of lateral heel pain after calcaneal fracture, including the subtalar joint, peroneal tendons, lateral calcaneal cortical bulge, and screws. One of the keys of success is accurate localization of the proximal portal, which is at the junction of posterior edge of the posterior subtalar joint and the peroneal tendons. This allows visualization of all the operative sites, including peroneal tendons, subtalar joint, and the lateral calcaneal wall. In case of calcaneal malunion, the anatomy is distorted, and intraoperative fluoroscopy may be needed to locate the proximal portal. The placement of distal portal plantar and distal to the proximal portal makes less crowding of instruments, especially during debridement of the anterolateral calcaneal wall.
It should be noted that the operation may need to be converted to open surgery if there is extensive complex tear of the peroneal tendons requiring open repair.
The advantages of this minimally invasive approach include better cosmesis, less soft tissue dissection, less postoperative pain, allowing access to the various sources of lateral heel pain after calcaneal fracture. The potential risk of this procedure includes sural nerve injury, peroneal tendons injury, and persistent pain (Table 3). This technique is not technically difficult and can be attempted by averaged foot and ankle arthroscopists.
Table 3.
Advantages and Risks of Endoscopic Screw Removal, Debridement of the Peroneal Tendons and Subtalar Joint, and Lateral Calcaneal Ostectomy for Management of Chronic Heel Pain After Calcaneal Fracture
| Advantages | Risks |
|---|---|
|
|
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Endoscopic screw removal, debridement of the peroneal tendons and subtalar joint, and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The back-out screws are removed with the corresponding screw driver. The peroneal tendons are examined, and synovectomy and debridement of the torn tendons are performed with an arthroscopic shaver. The fibrous tissue of the posterior subtalar joint and sinus tarsi is debrided, and the fibrotic soft tissue envelop is stripped from the lateral calcaneal wall in order to expose the bony prominence. The bony prominence is then resected with an arthroscopic acromionizer.
References
- 1.Almeida J.F., Vale C., Gonzalez T., Gomes T.M., Oliva X.M. Osteosynthesis or primary arthrodesis for displaced intra-articular calcaneus fractures Sanders type IV: A Systematic Review. J Foot Ankle Surg. 2022;28:281–287. doi: 10.1016/j.fas.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Allegra P.R., Rivera S., Desai S.S., Aiyer A., Kaplan J., Gross C.E. Intra-articular calcaneus fractures: Current concepts review. Foot Ankle Orthop. 2020;5 doi: 10.1177/2473011420927334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schepers T. Fixation by open reduction and internal fixation or primary arthrodesis of calcaneus fractures. Foot Ankle Clin. 2020;25:683–695. doi: 10.1016/j.fcl.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Shi F., Wu S., Cai W., Zhao Y. Comparison of 5 treatment approaches for displaced intra-articular calcaneal fractures: A systematic review and Bayesian network meta-analysis. J Foot Ankle Surg. 2020;59:1254–1264. doi: 10.1053/j.jfas.2020.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Smitaman E.E., Davis M. Hindfoot fractures: Injury patterns and relevant imaging findings. Radiographics. 2022;42:661–682. doi: 10.1148/rg.210167. [DOI] [PubMed] [Google Scholar]
- 6.Khazen G., Rassi C.K. Sinus tarsi approach for calcaneal fractures: The new gold standard? Foot Ankle. Clin. 2020;25:667–681. doi: 10.1016/j.fcl.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Williams C.E., Joo P., Oh I., Miller C., Kwon J.Y. Arthroscopically assisted internal fixation of foot and ankle fractures: A systematic review. Foot Ankle Orthop. 2021;6 doi: 10.1177/2473011420950214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilkinson B.G., Marsh J.L. Minimally invasive treatment of displaced intra-articular calcaneal fractures. Orthop Clin North Am. 2020;51:325–338. doi: 10.1016/j.ocl.2020.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Guan X., Xiang D., Hu Y., Jiang G., Yu B., Wang B. Malunited calcaneal fracture: The role and technique of osteotomy-a systematic review. Int Orthop. 2021;45:2663–2678. doi: 10.1007/s00264-021-05130-1. [DOI] [PubMed] [Google Scholar]
- 10.Chu K.M., Lui T.H. Endoscopic lateral calcaneal ostectomy and peroneal tendon decompression with the patient in the prone position as management of subfibular impingement after calcaneal fracture. Arthrosc Tech. 2019;19:e1069–e1073. doi: 10.1016/j.eats.2019.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lui T.H. Endoscopic lateral calcaneal ostectomy for calcaneofibular impingement. Arch Orthop Trauma Surg. 2007;127:265–267. doi: 10.1007/s00402-006-0194-6. [DOI] [PubMed] [Google Scholar]
- 12.Bauer T., Deranlot J., Hardy Ph. Endoscopic treatment of calcaneo-fibular impingement. Knee Surg Sports Traumatol Arthrosc. 2011;19:131–136. doi: 10.1007/s00167-010-1149-6. [DOI] [PubMed] [Google Scholar]
- 13.Lui T.H., Chan K.B. Arthroscopic management of late complications of calcaneal fractures. Knee Surg Sports Traumatol Arthrosc. 2013;21:1293–1299. doi: 10.1007/s00167-012-2086-3. [DOI] [PubMed] [Google Scholar]
- 14.Lui T.H., Siu Y.C., Ngai W.K. Endoscopic management of calcaneofibular impingement and posterior ankle impingement syndrome secondary to malunion of joint depressed type calcaneal fracture. Arthrosc Tech. 2018;7:e71–e76. doi: 10.1016/j.eats.2017.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lui T.H., Pan X.H., Pan Y. Arthroscopic and endoscopic management of common complications after displaced intra-articular calcaneal fractures. Clin Podiatr Med Surg. 2019;36:279–293. doi: 10.1016/j.cpm.2018.10.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic screw removal, debridement of the peroneal tendons and subtalar joint, and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The back-out screws are removed with the corresponding screw driver. The peroneal tendons are examined, and synovectomy and debridement of the torn tendons are performed with an arthroscopic shaver. The fibrous tissue of the posterior subtalar joint and sinus tarsi is debrided, and the fibrotic soft tissue envelop is stripped from the lateral calcaneal wall in order to expose the bony prominence. The bony prominence is then resected with an arthroscopic acromionizer.
Endoscopic screw removal, debridement of the peroneal tendons and subtalar joint, and lateral calcaneal ostectomy of the left foot for management of chronic heel pain after calcaneal fracture. The patient is in lateral position. The proximal portal is the viewing portal, and the distal portal is the working portal. The back-out screws are removed with the corresponding screw driver. The peroneal tendons are examined, and synovectomy and debridement of the torn tendons are performed with an arthroscopic shaver. The fibrous tissue of the posterior subtalar joint and sinus tarsi is debrided, and the fibrotic soft tissue envelop is stripped from the lateral calcaneal wall in order to expose the bony prominence. The bony prominence is then resected with an arthroscopic acromionizer.