Abstract
Hip abductor deficiency resulting from gluteus medius and minimus pathology is increasingly recognized as a generator of lateral-sided hip pain. In the setting of a failed gluteus medius repair or in patients with irreparable tears, transfer of the anterior portion of the gluteus maximus muscle can be performed to treat gluteal abductor deficiency. The classic description of the gluteus maximus transfer technique relies solely on bone tunnel fixation. This article describes a reproducible technique that incorporates the addition of a distal row to the tendon transfer, which may improve fixation by both compressing the tendon transfer to the greater trochanter and providing improved biomechanical strength to the transfer.
Technique Video
Gluteus maximus transfer for hip abductor deficiency. A surgical incision is placed over the femoral shaft and extended proximally and posteriorly toward the posterior superior iliac spine. Electrocautery is used to dissect down to the iliotibial tract. A Cobb elevator is used to lift the subcutaneous adipose tissue and identify the underlying fascial layer. Once developed, the iliotibial tract is split in the midline of the greater trochanter to establish the anterior edge. Next, the posterior aspect of the flap is planned using electrocautery to preliminarily identify the posterior edge of the gluteus maximus flap. A nonabsorbable braided suture is used to place a Krackow stitch in the distal portion of the flap. Scar tissue or prior suture must be removed to expose the greater trochanter, and a high-speed burr is used to decorticate the greater trochanter and create a bleeding footprint. A 2.6-mm drill is used to create 3 anterior and 3 posterior bone tunnels in the greater trochanter, and FiberWire sutures are placed through the muscle flap on the anterior and posterior edges and shuttled through the bone tunnels. A double-row repair is used, and 1 limb from each FiberWire suture is passed through a suture anchor. The holes for each anchor are drilled and then tapped distal to the vastus ridge.
Gluteus medius and minimus pathology is increasingly recognized as a source of lateral-sided hip pain. Operative intervention, through either open or arthroscopic approaches, with tendon repair has been shown to improve functional outcomes and decrease pain in most patients.1 However, the literature regarding failure rates and retears is inconsistent, with studies reporting failure rates between 5% and 35%.2 In the setting of a failed repair or in patients with irreparable tears, transfer of the anterior portion of the gluteus maximus can be performed to resolve lateral-sided hip pain and improve gait abnormalities related to abductor deficiency.3
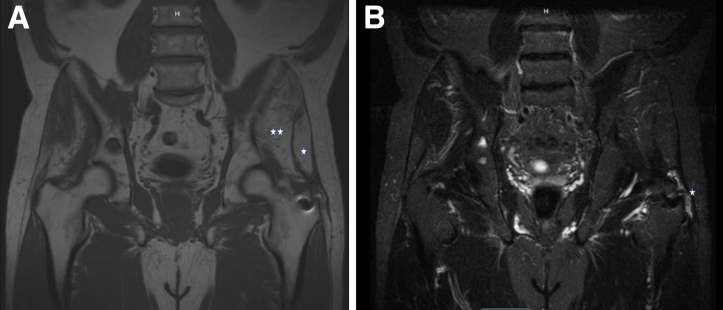
Prior to transfer, the clinician should examine gait patterns for evidence of gluteal deficiency (i.e., Trendelenburg gait) and assess for gluteus maximus function by asking the patient to extend the hip while prone on the examination table. Magnetic resonance imaging should be obtained to assess the integrity of the gluteal muscles—or of prior repair—and to assess for fatty muscle infiltration (Fig 1). At our institution, assessment of the gluteus maximus with electromyographic studies is required to confirm adequate function of the muscle, particularly to test for the integrity of the inferior gluteal nerve or concurrent spine pathology affecting gluteal function (L5-S2 nerve roots) (Table 1).
Fig 1.
(A) T1-weighted magnetic resonance image of pelvis in coronal plane showing fatty atrophy to left-sided gluteus medius (1 star) and minimus (2 stars) muscle. (B) T2-weighted image in coronal plane showing fluid (star) adjacent to rerupture of prior left-sided gluteal tendon repair.
Table 1.
Advantages and Disadvantages of Open Double-Row Gluteus Maximus Tendon Transfer
| Advantages | Disadvantages |
|---|---|
| The technique uses a flexible approach that typically allows incorporation of prior arthroscopic portals or open approaches. | A large surgical incision is required, with the risk of perioperative hematoma or wound complications. |
| The technique typically provides excellent pain relief in the setting of prior failed repair or long-standing gluteal tendon tears. | Available data indicate inconsistent resolution of Trendelenburg gate. |
| The double-row construct provides excellent compression across the transfer footprint. | Maximal clinical improvement is not achieved for 6 mo to 1 yr. |
| Using bone tunnels in the greater trochanter for the proximal row reduces surgical costs without significantly prolonging surgical time or technical difficulty. | The patient is required to wear an abduction brace for 8 wk postoperatively. |
| Open exposure of the gluteus maximus allows for precise tensioning and division of the muscle transfer. | |
| Lateral positioning and surgical setup are similar to total hip arthroplasty and thus familiar to most orthopaedic surgical teams. |
Initially described by Whiteside4 in 2012, transfer of the gluteus maximus has been shown to significantly improve patient outcomes in the short term in a case series. However, this “classic” description relies solely on bone tunnel fixation (Table 2). The addition of a distal row to the tendon transfer, as described in this article, may improve on prior techniques by both compressing the tendon transfer to the greater trochanter and providing improved biomechanical strength to the transfer.
Table 2.
Surgical Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Electromyographic evaluation must be obtained prior to the procedure to exclude spinal or peripheral nerve pathology that may affect gluteal muscle function. | Failure to appreciate muscle atrophy related to spine or peripheral nerve pathology may result in transferring weak or nonviable gluteal maximus muscle. |
| Perioperative administration of tranexamic acid reduces intraoperative blood loss and risk of postoperative hematoma. | An attempt to perform transfer through minimally invasive approaches makes flap division and tensioning inconsistent and technically challenging. |
| Packing a laparotomy sponge posterior to the greater trochanter during exposure protects the sciatic nerve and safely divides adhesions from areas of chronic inflammation or prior surgical exposure. | Failure to protect the sciatic nerve during Charnley retractor placement or bone tunnel drilling may result in neurapraxia or direct injury to the nerve. |
| Splitting the proximal vastus lateralis allows appropriate placement of the distal row and provides a cuff of tissue for repair over the distal aspect of the tendon transfer. | Failure to abduct the leg on a Mayo stand during graft tensioning may result in inadvertent laxity of the muscle transfer. |
| The addition of the distal row likely allows excellent compression across the footprint and improves repair strength. | No biomechanical or outcome data on this specific mechanism of repair are available yet. |
Surgical Technique
Surgical Setup
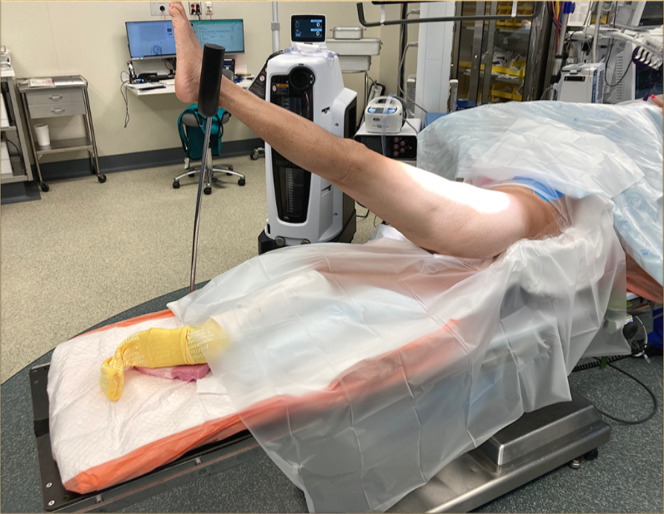
The patient is positioned lateral on a peg board, with care taken to pad both the positioning pegs and the down leg (Fig 2). Care must be taken to preserve a wide surgical field and maintain access to the top of the iliac crest because the surgical procedure requires adequate visualization of the proximal extent of the gluteus maximus origin. A sterile stockinet is placed over the distal portion of the surgical extremity, and iodine-impregnated surgical drapes (Ioband; 3M, Maplewood, MN) are circumferentially applied. A sterile Mayo stand with a pillow is also made available to assist with leg abduction during the surgical procedure.
Fig 2.
Patient positioning prior to left-sided gluteus maximus transfer. The patient is positioned lateral on a peg board, with care taken to pad both the positioning pegs and the down leg.
A surgical timeout is performed prior to incision, with discussion of mean arterial pressure goals, administration of preoperative antibiotics, and administration of tranexamic acid (TXA). Given the large body of literature available on the safety and benefit of TXA administration, most patients at our institution receive 1 gram of TXA at incision and an additional gram at the initiation of surgical closure.
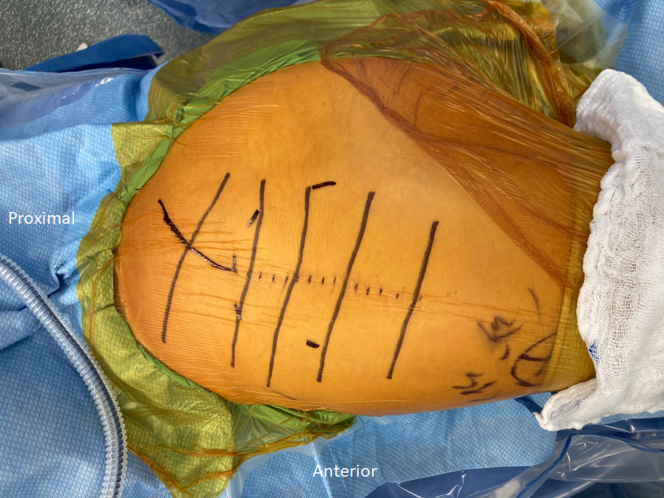
Surgical Exposure
The surgical incision is ideally placed over the center of the femoral shaft, with the proximal extent curving posteriorly toward the posterior superior iliac spine, beginning at the greater trochanter (Video 1). However, the surgeon should alter the incision to include prior surgical exposures (Fig 3). Most commonly, this will include a posterolateral incision from prior total hip arthroplasty. The surgical incision is carried sharply to the iliotibial (IT) tract, with care taken to achieve hemostasis and reduce the risk of postoperative hematoma. A Cobb elevator is used to bluntly identify the plane between the subcutaneous adipose tissue and the underlying fascial layer. The plane is developed from the level of the iliac crest to the distal IT tract (distal to the vastus ridge). This plane should be developed in its entirety prior to violation of the IT tract because the plane is both easier to develop prior to removing tension off the IT tract and essential to define prior to irreversibly determining the proximal extent of the gluteal flap.
Fig 3.
Patient positioning after preparation and draping of left hip. The dotted incision represents the patient’s prior surgical scar, and the line represents the proximal portion of the incision angles toward the posterior superior iliac spine.
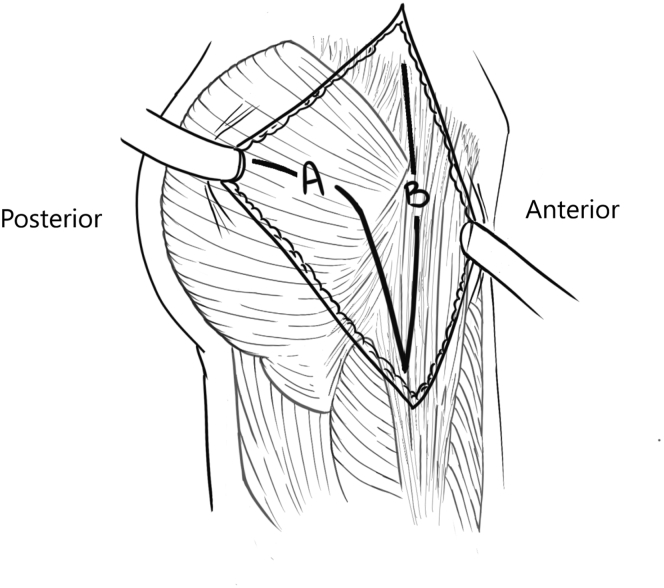
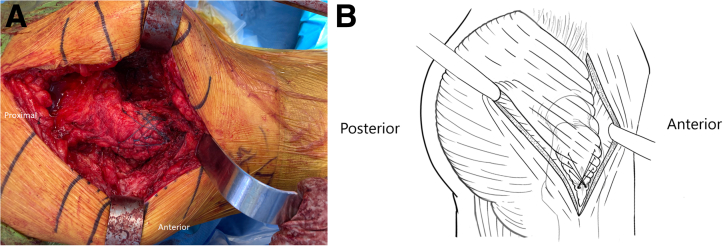
Creation of Gluteal Flap
Once the subcutaneous plane has been fully developed, the IT tract is split in the midline of the greater trochanter, thereby establishing the anterior edge of the gluteal flap (Fig 4). In cases of prior open gluteal repair or total hip arthroplasty, a pre-existing defect in the IT tract may be exploited to prevent an intrasubstance defect in the flap. Then, a laparotomy sponge is packed under the IT band, posterior and anterior to the greater trochanter, to re-create the deep gluteal space, which is often affected by adhesions from chronic bursal inflammation and prior surgical procedures. Moreover, blunt dissection of the adhesions with re-creation of the deep gluteal space also safely protects the sciatic nerve by placing it deeper in the surgical wound. At this juncture, a significant defect in the gluteal tendon insertion site (i.e., “bald trochanter”) and significant fatty atrophy of the gluteus medius muscle can be appreciated.
Fig 4.
Planning of gluteal flap in right hip. Line A indicates the posterior edge of the gluteal flap, and line B indicates the anterior edge of the gluteal flap. Illustration by Laura Baratta and Mandy Chan in association with InPrint at Washington University in St Louis.
Next, the posterior aspect of the flap is planned using electrocautery to preliminarily identify the posterior edge of the gluteus maximus flap. Although electrocautery should be used to create a full-thickness flap of the IT band at the distal extent of the flap, more proximally only the fascia should be divided such that the muscle belly can be bluntly divided in line with the gluteus maximus fibers. Care should be taken to protect the terminal branches of the superior gluteal artery to preserve blood supply to the gluteal flap and prevent unforeseen bleeding in the wound. After division of the anterior gluteal flap, a nonabsorbable braded suture (Ethibond; Johnson & Johnson, New Brunswick, NJ) is used to place a Krackow stitch in the distal portion of the flap to improve the ability to place tension on the flap and allow for supplemental fixation of the flap to the greater trochanter. Finally, adhesions are released from the superficial and deep aspects of the flap to allow for adequate mobilization and future tensioning of the muscle transfer.
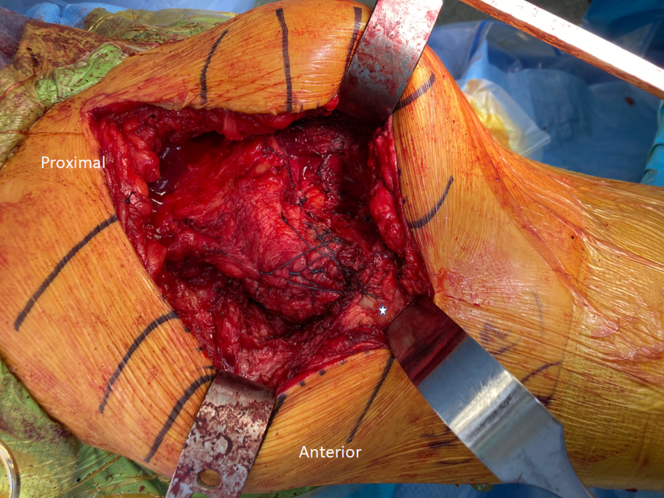
Preparation of Greater Trochanter and Securing of Gluteal Flap
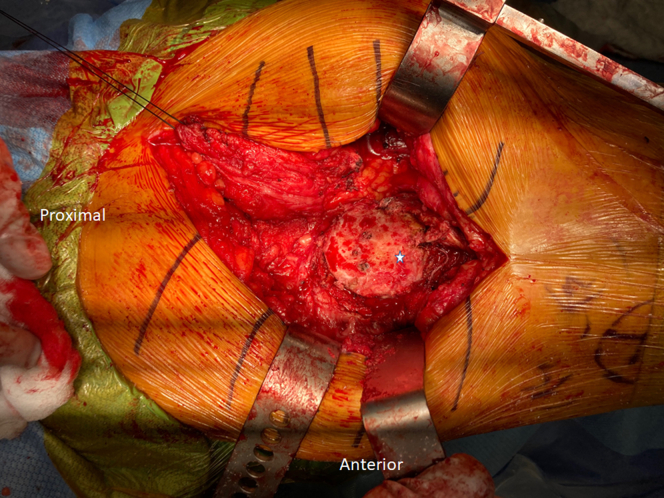
Typically, scar tissue or prior suture must be removed to expose the greater trochanter. Then, a Charnley curette is used to clear any residual scar tissue, and a high-speed burr is used to gently decorticate the greater trochanter and reveal a bed of clean, bleeding bone to serve as a footprint for the transfer (Fig 5).
Fig 5.
View of left-sided greater trochanter (star) after removal of all soft tissue and debris, prior to attachment of muscle transfer. This is performed to create an adequate footprint with bleeding bone to facilitate healing of the transferred flap.
After preparation of the trochanter, a 3.5-mm drill is used to create 3 anterior and 3 posterior bone tunnels in the greater trochanter. We recommend retraction on the deep aspect of the posterior greater trochanter to prevent possible injury to the sciatic nerve with an inadvertent pass of the drill.
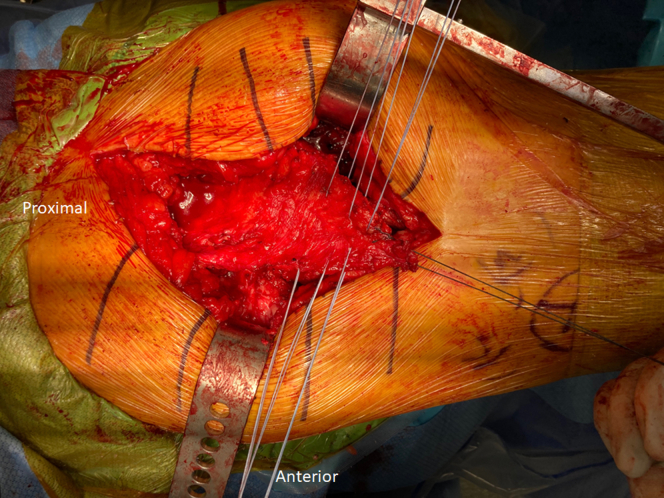
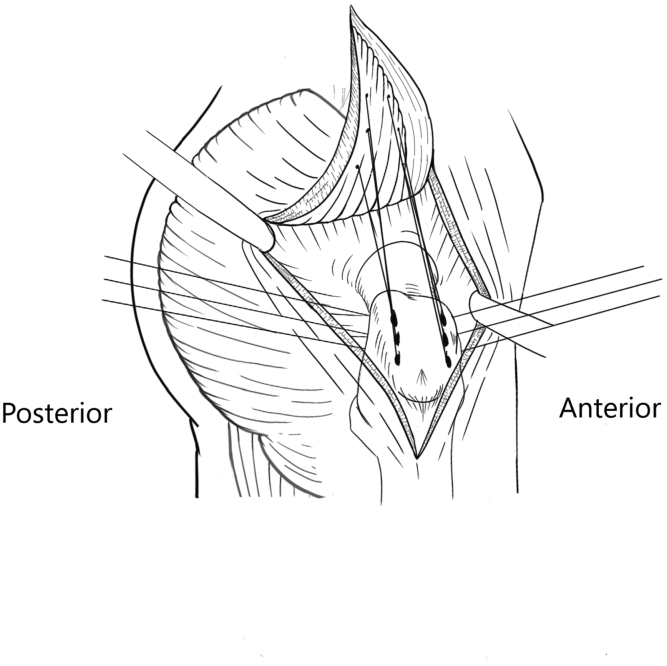
Three ultrahigh-molecular-weight polyethylene sutures (FiberWire; Arthrex, Naples, FL) should be placed through the muscle flap on the anterior and posterior edges (Fig 6). The location of these sutures is vital to ensure appropriate tension of the muscle transfer. By using the Ethibond traction suture to hold desired tension on the flap, each ultrahigh-molecular-weight polyethylene suture may be passed through the flap at the level of the anticipated bone tunnel (Fig 7). To ensure optimal tension, the leg should be maximally abducted on a sterile Mayo stand in neutral rotation. Failure to abduct the leg during this portion of the case may result in excessive laxity of the transfer and a residual Trendelenburg gait.
Fig 6.
View of left-sided gluteus muscle flap with 3 FiberWire sutures passed anteriorly and posteriorly. The location of these sutures is vital to ensure appropriate tension of the muscle transfer. Each suture should be passed through the flap at the level of the anticipated bone tunnel with the leg in abduction to prevent excessive laxity of the flap.
Fig 7.
Illustration of each ultrahigh-molecular-weight polyethylene suture passed through flap at level of anticipated bone tunnel in right hip. Illustration by Laura Baratta and Mandy Chan in association with InPrint at Washington University in St Louis.
Once passed, the FiberWire suture is shuttled through the bone tunnel from superficial to deep. Given the angle required to pass a Hewson suture passer from deep to superficial through the bone, we prefer to pass the Hewson device from superficial to deep and to use a shuttle stitch to pass the FiberWire suture through the greater trochanter in the appropriate direction. Once all 6 sutures have been passed, 5 alternating half-hitches are placed to secure the flap to the trochanter.
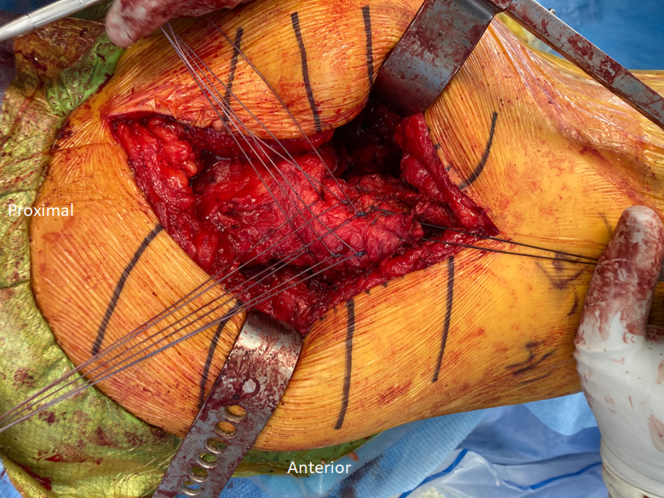
To provide compression across the footprint of the greater trochanter and increase biomechanical strength of the construct, a double-row repair is used (Figs 8 and 9). One limb from each FiberWire suture is passed through a suture anchor (Omega; Stryker, Kalamazoo, MI). The holes for each anchor are drilled and then tapped distal to the vastus ridge, under the sleeve of the vastus lateralis insertion previously created. The anchors are then placed, and each suture limb is independently tensioned to provide maximal compression across the muscle transfer.
Fig 8.
View of left-sided gluteus muscle flap after tying of proximal row of sutures (i.e., suture passing through bone tunnels) but prior to placement of distal-row anchors.
Fig 9.
(A) View of left-sided gluteus muscle transfer after placement of distal-row anchors. A double row is used to provide compression across the footprint of the greater trochanter and increase biomechanical strength of the construct. (B) Illustration of gluteus muscle transfer after placement of distal-row anchors in right hip. Illustration by Laura Baratta and Mandy Chan in association with InPrint at Washington University in St Louis.
A No. 1 Ethibond suture is used to repair the sleeve of the vastus lateralis overlying the muscle transfer (Fig 10). A No. 1 Stratafix PDS suture (Johnson & Johnson) is used to close the distal portion of the IT band, but re-approximation of the proximal extent is not possible given the defect resulting from the muscle transfer. A drain is used in selective cases but is not mandatory in cases of excellent hemostasis. The remainder of the Stratafix suture is used to close the deep subcutaneous fat in a layered fashion. Closure of this layer is essential to limit dead space and prevent postoperative hematoma formation, but care should be taken not to place excessive tension on the suture, which may cause fat necrosis. Finally, skin closure is performed with interrupted No. 2-0 Monocryl suture, running No. 3-0 Monocryl Stratafix suture, and the Dermabond PRINEO wound closure system (Johnson & Johnson) (Fig 11).
Fig 10.
View of left-sided closure of vastus lateralis (star) over gluteus muscle transfer. A No. 1 Stratafix PDS suture is used to close the distal portion of the iliotibial band, but re-approximation of the proximal extent is not possible given the defect resulting from the muscle transfer.
Fig 11.
View of left-sided final incision after closure with running Monocryl Stratafix suture. Closure of this layer is essential to limit dead space and prevent postoperative hematoma formation, but care should be taken not to place excessive tension on the suture, which may cause fat necrosis.
Postoperative Care
No adduction and no active abduction are allowed for the first 6 to 8 weeks, during which only flat-foot partial weight bearing (20 lb [9 kg]) is indicated with the assistance of a walker or crutches. The patient is directed to wear a low-profile abduction brace, with hip flexion limited to 90°, continuously except when bathing. Active hip abduction and internal rotation, as well as passive external rotation and adduction, are avoided for 6 weeks. At 8 weeks, physical therapy is initiated, and use of the abduction brace is discontinued. The patient is also weaned off using the crutches or walker and progresses to full weight bearing by 8 weeks as appropriate milestones for pain control, range of motion, and neuro-proprioception are met. Recovery should be expected with improved strength and activity tolerance over a 6- to 8-month period. The patient is instructed to take aspirin, 81 mg twice weekly for 4 weeks, to prevent blood clots unless there is a contraindication.
Discussion
Gluteus maximus transfer is indicated in the setting of symptomatic, failed abductor tendon repair or massive abductor tendon tears with severe fatty infiltration. The original description of this technique relies solely on bone tunnel fixation.3 Although further biomechanical studies are needed, in our experience a “double-row” construct is preferred to increase compression across the footprint of the muscle transfer and improve strength. Patients should be counseled that the available literature regarding gluteus maximus transfer3 indicates good pain relief in most patients but unreliable resolution of Trendelenburg gait. A significant postoperative rehabilitation course, including gait retraining, is required after the procedure. Moreover, significant additional research is required to understand the optimal indications, predictors of postoperative outcomes, and technical factors related to a successful outcome. Regardless, we believe this technique gives the surgeon the ability to provide direct compression across the muscle transfer and improve repair strength in the setting of gluteus maximus muscle transfer.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C.C. receives grants from Department of Defense–United States Army Medical Research Acquisition Activity (USAMRAA) (award No. W81XWH1920042) and Zimmer Biomet; is a consultant for Microport Orthopedics and Zimmer Biomet; receives publication royalties from Wolters Kluwer Health; and receives product royalties from Microport, outside the submitted work. C.P-G. receives grants from National Institutes of Health, Orthopaedic Research and Education Foundation, and Zimmer and is a consultant for Zed View Lexi 3D Developing Software, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Gluteus maximus transfer for hip abductor deficiency. A surgical incision is placed over the femoral shaft and extended proximally and posteriorly toward the posterior superior iliac spine. Electrocautery is used to dissect down to the iliotibial tract. A Cobb elevator is used to lift the subcutaneous adipose tissue and identify the underlying fascial layer. Once developed, the iliotibial tract is split in the midline of the greater trochanter to establish the anterior edge. Next, the posterior aspect of the flap is planned using electrocautery to preliminarily identify the posterior edge of the gluteus maximus flap. A nonabsorbable braided suture is used to place a Krackow stitch in the distal portion of the flap. Scar tissue or prior suture must be removed to expose the greater trochanter, and a high-speed burr is used to decorticate the greater trochanter and create a bleeding footprint. A 2.6-mm drill is used to create 3 anterior and 3 posterior bone tunnels in the greater trochanter, and FiberWire sutures are placed through the muscle flap on the anterior and posterior edges and shuttled through the bone tunnels. A double-row repair is used, and 1 limb from each FiberWire suture is passed through a suture anchor. The holes for each anchor are drilled and then tapped distal to the vastus ridge.
References
- 1.Nazal M.R., Abraham P.F., Conaway W.K., et al. Endoscopic repair of full-thickness gluteus medius and minimus tears—Prospective study with a minimum 2-year follow-up. Arthroscopy. 2020;36:2160–2169. doi: 10.1016/j.arthro.2020.04.025. [DOI] [PubMed] [Google Scholar]
- 2.Longstaffe R., Dickerson P., Thigpen C.A., et al. Both open and endoscopic gluteal tendon repairs lead to functional improvement with similar failure rates: A systematic review. J ISAKOS. 2021;6:28–34. doi: 10.1136/jisakos-2020-000474. [DOI] [PubMed] [Google Scholar]
- 3.Whiteside L.A. Surgical technique: Transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop Relat Res. 2012;470:503–510. doi: 10.1007/s11999-011-1975-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maldonado D.R., Annin S., Chen J.W., et al. Combined transfer of the gluteus maximus and tensor fasciae latae for irreparable gluteus medius tear using contemporary techniques: Short-term outcomes. JB JS Open Access. 2020;5 doi: 10.2106/JBJS.OA.20.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Gluteus maximus transfer for hip abductor deficiency. A surgical incision is placed over the femoral shaft and extended proximally and posteriorly toward the posterior superior iliac spine. Electrocautery is used to dissect down to the iliotibial tract. A Cobb elevator is used to lift the subcutaneous adipose tissue and identify the underlying fascial layer. Once developed, the iliotibial tract is split in the midline of the greater trochanter to establish the anterior edge. Next, the posterior aspect of the flap is planned using electrocautery to preliminarily identify the posterior edge of the gluteus maximus flap. A nonabsorbable braided suture is used to place a Krackow stitch in the distal portion of the flap. Scar tissue or prior suture must be removed to expose the greater trochanter, and a high-speed burr is used to decorticate the greater trochanter and create a bleeding footprint. A 2.6-mm drill is used to create 3 anterior and 3 posterior bone tunnels in the greater trochanter, and FiberWire sutures are placed through the muscle flap on the anterior and posterior edges and shuttled through the bone tunnels. A double-row repair is used, and 1 limb from each FiberWire suture is passed through a suture anchor. The holes for each anchor are drilled and then tapped distal to the vastus ridge.
Gluteus maximus transfer for hip abductor deficiency. A surgical incision is placed over the femoral shaft and extended proximally and posteriorly toward the posterior superior iliac spine. Electrocautery is used to dissect down to the iliotibial tract. A Cobb elevator is used to lift the subcutaneous adipose tissue and identify the underlying fascial layer. Once developed, the iliotibial tract is split in the midline of the greater trochanter to establish the anterior edge. Next, the posterior aspect of the flap is planned using electrocautery to preliminarily identify the posterior edge of the gluteus maximus flap. A nonabsorbable braided suture is used to place a Krackow stitch in the distal portion of the flap. Scar tissue or prior suture must be removed to expose the greater trochanter, and a high-speed burr is used to decorticate the greater trochanter and create a bleeding footprint. A 2.6-mm drill is used to create 3 anterior and 3 posterior bone tunnels in the greater trochanter, and FiberWire sutures are placed through the muscle flap on the anterior and posterior edges and shuttled through the bone tunnels. A double-row repair is used, and 1 limb from each FiberWire suture is passed through a suture anchor. The holes for each anchor are drilled and then tapped distal to the vastus ridge.