Abstract
The sulcus deepening trochleoplasty procedure has been described for the management of patellofemoral instability in patients with severe trochlear dysplasia. Here, we describe the updated Lyon sulcus deepening trochleoplasty technique.
This technique with a stepwise approach allows one to prepare the trochlea, remove the subchondral bone, osteotomize the articular surface, and fix the facets with 3 anchors while minimizing the risk of complications.
Technique Video
This video shows a sulcus deepening trochleoplasty performed on a patient with objective patellar instability and trochlear dysplasia type D. The patient, under sedation and regional anesthesia, is positioned in a supine position with the knee flexed and 2 supports, one lateral and one distal. A 10-midline skin incision is performed. The transquadricipital tendon approach is preferred. The supratrochlear synovial membrane is performed. The native groove, the medial and lateral facets, and the new planned groove lines are marked. After measuring the prominence, a strip cortex is removed around the femorotrochlear osteochondral junction. Multiple convergent tunnels through the trochlear undersurface cancellous bone are performed and the bone bridges between the tunnels are removed. The cartilage marked lines are incised with a surgical blade No. 23 and then osteotomized. The facets are rotated slightly to increase the sulcus angle. Fixation of the facets is performed with 3 BioComposite Labral SwiveLock anchors. Gaps between the facets are fulfilled with bone and the supratrochlear synovium is closed.
Trochlear dysplasia has been shown to be the first risk factor for patella–femoral instability.1,2 This condition is characterized by a modified trochlear shape and an increased overhang of the groove relative to the anterior femoral cortex in high grade trochlear dysplasia. The trochleoplasty is a surgical correction of the trochlear groove shape with the aim of preventing recurrent patellar dislocations.
Three surgical techniques have been proposed to correct an abnormally shaped trochlea: the lateral wedge augmentation trochleoplasty (LWAT), the recession trochleoplasty (RT), and the deepening trochleoplasty (DT). The original techniques have undergone many modifications since their first descriptions. Unlike the LWAT and RT, which modify, respectively, the shape or the prominence, the aim of DT is to alter both features.
The LWAT was developed by Albee in 1915.3 This technique, performed with a lateral opening-wedge osteotomy and bone grafting, has been gradually replaced. The main concern with this procedure is the greater joint reaction force, due to the elevated lateral facet, with an increased risk of pain and secondary osteoarthritis.4
The RT, described initially by Goutallier et al.5 and later modified by Beaufils et al.,6 reduces the prominence without changing the groove’s shape and without any realignment.
The DT was first proposed by Bilton Pollard in 1890.7 It was then described by Masse et al. in 1978,8 who proposed to remove the subchondral bone and impact the trochlear cartilage with a punch.
The original technique was subsequently modified and standardized by Dejour in 1987, leading to 2 different procedures: the Lyon sulcus deepening trochleoplasty (or thick-flap procedure) and the “Bereiter” deepening trochleoplasty (or thin-flap procedure). The principal difference between the 2 lies in the preservation of cartilage.
In 1990, Dejour et al.9 proposed to add an osteotomy of both femoral condyles to create a V-shaped trochlear groove. This procedure was slightly changed by the senior author in 2010,10 with the addition of the groove lateralization for a “proximal realignment.”
Alternatively, in 1994, after visiting Dejour, Bereiter and Gautier11 developed a U-shaped DT technique. This technique has some technical adaptations to facilitate the procedure and doesn’t need trochlear osteotomies to be performed. A burr is used to remove part of the subchondral bone, modifying the shape of the bony sulcus. The osteochondral flap is then depressed and fixed to the new bony sulcus with VICRYL tape. In 2010, Blønd and Schöttle12 described how to perform this technique arthroscopically.
Since then, numerous deepening trochleoplasty techniques have been described, mixing or slightly modifying one of the two.13, 14, 15, 16 DT, whatever the technique used, finds its rational in modifying both the prominence and the shape of the trochlea. The technique we describe has been developed through the work of Pollard, Masse, Dejour, and the senior author (D.H.D.).
Here, we describe the most updated Lyon sulcus deepening trochleoplasty, with tips and tricks and modification to the original technique.
Surgical Technique (With Video Illustration)
Indication for Surgery
The sulcus deepening trochleoplasty is indicated in patients with recurrent patellar dislocation, an abnormal patellar tracking, and high-grade trochlear dysplasia, classified as types B or D according to Dejour et al.17 with a trochlear prominence greater than 5 mm.18
Step 1: Position and Examination Under Anesthesia
Sedation and regional anesthesia are required to perform this procedure. The patient is positioned supine on the operating table (Fig 1, Table 1 and Video 1). Two supports, lateral and distal, are used to keep the knee in flexion. A high thigh tourniquet is placed to aid in visualization during surgery. Preprocedural prepping and draping is carried out through the entire lower extremity. Before the incision to be done, the medial tilt test and true patellar glide are assessed.
Fig 1.
Patient position (right side). The patient is placed in a supine position on the operating table. Two supports, lateral and distal, are used to keep the knee in flexion. A high thigh tourniquet is placed to optimize the knee exposure during surgery. The knee is positioned at 90° of flexion.
Table 1.
Step-by-Step Details of the Technique
| Step 1. Position and examination under anesthesia |
|
| Step 2. Surgical approach |
|
| Step 3. Trochlear preparation |
|
| Step 4. Prominence removal |
|
| Step 5. Trochlear undersurface preparation |
|
| Step 6. Trochlear surface osteotomies |
|
| Step 7. Fixation |
|
| Step 8. Closure |
|
Step 2: Surgical Approach
The knee is positioned at 90° of flexion. Starting from 5 cm proximal to the upper patellar pole, a longitudinal 10 cm midline skin incision is performed (Fig 2). A transquadricipital tendon approach with medial parapatellar arthrotomy is performed, removing the periosteum from the medial middle third of the anterior surface of the patella, to prepare it for subsequent medial patellofemoral ligament (MPFL) reconstruction, which is carried out systematically.
Fig 2.
The skin incision (right side). Starting from 5 cm proximal to the upper patellar pole, a longitudinal 10-cm midline skin incision is performed.
This approach is therefore preferred, simplifying distal femoral exposure and MPFL reconstruction. No patellar eversion is needed to assess the articular cartilage surface of both the patella and trochlea.
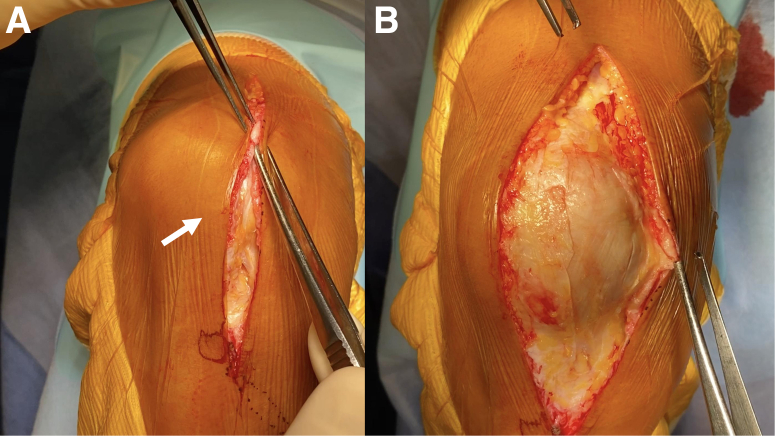
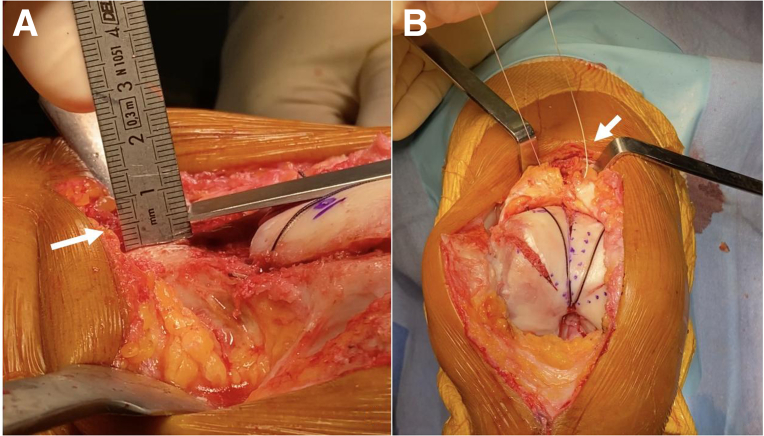
The supratrochlear synovial membrane is incised both longitudinally and along the proximal bone–cartilage transition of the distal femur (Fig 3). A periosteal elevator is then used to reflect it from the anterior femoral cortex. The anterior surface of the distal femur is used as a landmark to determine the amount of bone to be removed, making the new groove flush with it. The trochlear dysplasia is then assessed, measuring the supratrochlear spur and often evaluating an hypoplastic medial facet.
Fig 3.
The supratrochlear synovial membrane is incised both longitudinally and along the proximal bone-cartilage transition of the distal femur (A) (right side). The trochlear dysplasia is then assessed, measuring the supratrochlear spur (B).
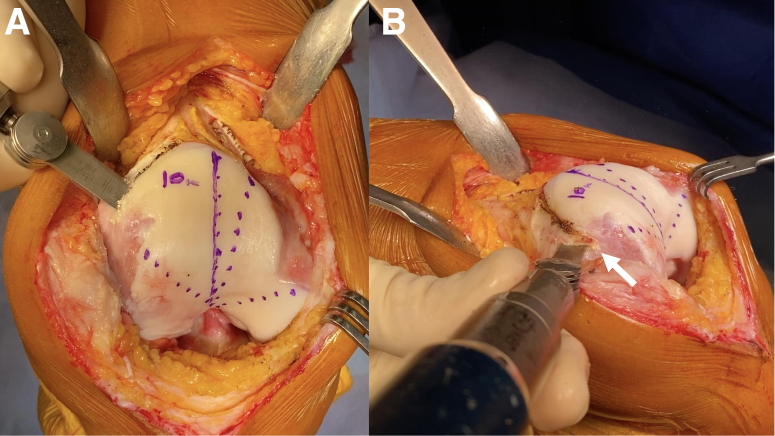
Step 3: Trochlear Preparation
A sterile marking pen is then used to draw 3 dashed lines from the top of the notch, representing the native groove and the lateral and medial facets limits (Fig 4). Frequently in those cases, the native groove goes medially with an abnormal direction. The medial and lateral dashed lines are drawn through the condylotrochlear grooves.
Fig 4.
A sterile marking pen is then used to draw 3 dashed lines (representing the native groove and the lateral and medial facets limits) and a continuous line (representing the new planned groove) (right side).
Then the new planned groove is marked with a continuous line in a more lateral position. The new sulcus should be aligned to the femoral anatomical axis and the resultant lateralized position might be adequate therefore to decrease a slightly elevated tibial tuberosity–trochlear groove distance without the need of addressing the tibial side. The distance between the native and new groove lives is then measured to assess the tibial tuberosity–trochlear groove modification.
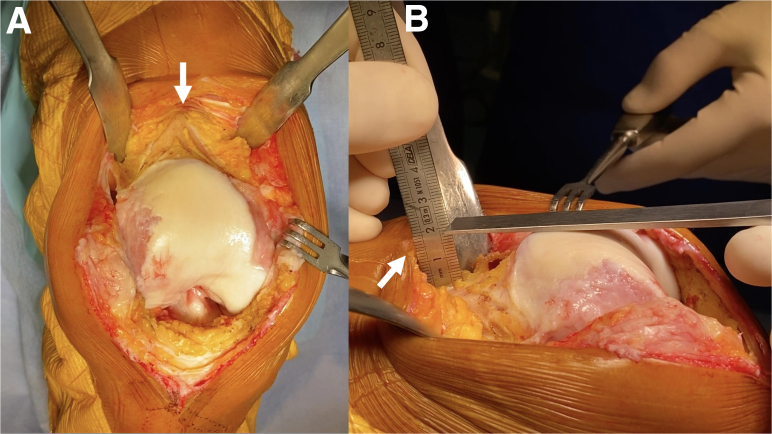
Step 4: Prominence Removal
A strip of cortex is removed around the femorotrochlear osteochondral junction, either with an oscillating saw or with an osteotome (Fig 5). This cortical wedge of bone thickness is equal to the prominence height, allowing the new groove to be flush with the anterior femoral cortex (Fig 6). The spur removal exposes the trochlear undersurface cancellous bone.
Fig 5.
A strip of cortex is removed around the femorotrochlear osteochondral junction with an oscillating saw (A-B) (right side).
Fig 6.
The cortical wedge of bone is removed (A) and its height is equal to prominence, cortex (B) (right side).
Step 5: Trochlear Undersurface Preparation
A special drill guide with a 5-mm off-set marking hook (Arthrex, Naples, FL) is used to drill multiple convergent tunnels through the trochlear undersurface cancellous bone (Fig 7). The hook is placed at the top of the notch and the tunnels are drilled from proximal to distal. The offset guide enables to create an osteochondral flap of 5 mm, limiting the risk of cartilage damage and allowing for adequate healing. It is fundamental not to go beyond the medial and lateral marked line.
Fig 7.
A special drill guide with a 5 mm off-set marking hook (A-B) and a 4-mm egg-shaped high-speed burr (C) are used to prepare the trochlear undersurface (right side). The guide is used to drill multiple convergent tunnels through the trochlear undersurface cancellous bone. The hook is placed at the top of the notch and the tunnels are drilled from proximal to distal. Then, the burr is used to remove the cancellous bone bridges between the tunnels in a proximal-to-distal fashion.
Then, the cancellous bone bridges between the tunnels are removed in a proximal-to-distal fashion with a 4-mm egg-shaped high-speed burr on a Total Performance System (Stryker, Kalamazoo, MI), while irrigating it with physiological saline. The undersurface bone removal is adapted to the shape and the amount of deepness needed. A greater amount of bone is removed in the center midline below the planned sulcus. This would make the new groove flush with the anterior femoral cortex. The cancellous bone is removed from the metaphyseal part of the femur to preserve the trochlear thickness.
Step 6: Trochlear Surface Osteotomies
At this point, the whole trochlea might be mobilized by a pusher depression. It is not flexible enough to be shaped completely without the risk of fracture. A surgical scalpel blade No. 23 is then used for cartilage incision and positioned on the marked new groove and lateral and medial margins (Fig 8). A bone tamp and mallet are used along with the scalpel to perform the incision.
Fig 8.
A surgical scalpel blade No. 23 is used for cartilage incision (A) (right side). Three osteochondral cuts along the marked lines are completed with a 45° oriented osteotome (B). With surgical forceps, the facets are pushed to check the trochlea to be flush with the anterior femoral cortex (C).
Then, with a very thin osteotome oriented at 45° to trochlea, the 3 osteochondral cuts along the marked lines are completed from proximal to distal to allow greater molding. It is mandatory not to join the osteochondral cuts distally to keep a distal hinge.
With surgical forceps, the facets are pushed to check the trochlea to be flush with the anterior femoral cortex. Both facets might be rotated slightly to increase the sulcus angle.
Light pressure might be applied with a 145° polyethylene pusher to shape the 2 flaps (Fig 9). Part of the bone removed at the beginning of the procedure might be inserted peripherally under the facets aiding the flaps elevated position. Once the grove is satisfactory and perfectly flush, the fixation might be performed.
Fig 9.
The 145° polyethylene pusher. Light pressure might be applied with a 145° polyethylene pusher to shape the 2 flaps (right side).
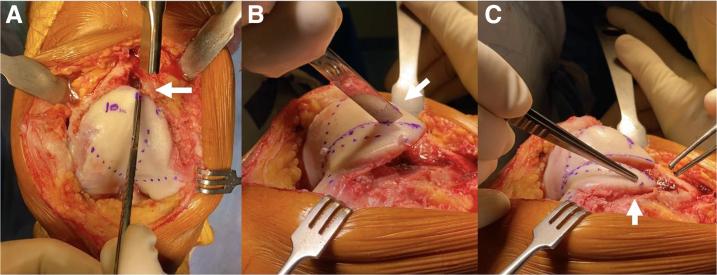
Step 7: Fixation
The fixation is performed with 3 BioComposite Labral SwiveLock Anchors, 3.5 mm (Arthrex) (Fig 10). The first anchor, loaded with 2 No. 2 VICRYL sutures (Ethicon, Cornelia, GA) is placed at the top of the notch. Each facet is compressed by a single pair of sutures, which are then tensioned and fixed with another BioComposite Labral SwiveLock Anchor, 3.5 mm at the proximal femorotrochlear margin. The sutures should be placed without the risk of sliding into the midline osteotomy. The sutures should not be overtensioned as this would increase the risk of anchor pull-out. While placing the anchor, it might be helpful to achieve the right compression, to push the facet with a surgical forceps.
Fig 10.
The fixation is performed with 3 BioComposite Labral SwiveLock Anchors, 3.5 mm (Arthrex) (A-C) (right side). The first anchor, loaded with 2 No. 2 VICRYL sutures (Ethicon, Cornelia, GA), is placed at the top of the notch. Each facet is compressed by a single pair of sutures, which are then tensioned and fixed with another BioComposite Labral SwiveLock Anchor, 3.5 mm at the proximal femorotrochlear margin.
Step 8: Closure
The strip of cortex harvested is then used to create anterior based wedge pieces of bone to fulfill longitudinally the 3 gaps between the facets (Fig 11). The height of the groove is then measured to evaluate the difference with the prominence assessed at the beginning of the procedure (Fig 12). The supratrochlear synovium is closed. The patellar tracking is then tested before the tibial tubercle osteotomy or MPFL to be performed. The MPFL is reconstructed systematically at the end of the procedure.
Fig 11.
The 3 gaps between are fulfilled with pieces of bone taken from the strip of cortex harvested (A-B) (right side).
Fig 12.
The height of the groove is then measured to evaluate the difference with the prominence assessed at the beginning of the procedure (A) (right side). The supratrochlear synovium is closed (B).
Discussion
The trochleoplasty has been shown to be effective in improving clinical outcomes in patients with objective patella instability associated with severe trochlear dysplasia.19 Furthermore, the redislocation rate is even lower when the procedure is carried out in combination with MPFL reconstruction.20,21
The most recent metanalysis by Leclerc et al.4 evaluated the clinical outcomes of 1,000 trochleoplasties, performed using different techniques. The rate of recurrent dislocation, instability without dislocation, patellofemoral (PF) osteoarthritis, stiffness, and need for subsequent surgery were respectively: 2.4%, 14%, 27%, 7%, and 17%.
The sulcus deepening trochleoplasty has several advantages compared with the other techniques. It has shown to be the most effective in reducing recurrence, with a rate of 0.28%.4,22 Leaving 5 mm of subchondral bone below the articular surface makes it a less-aggressive procedure relative to the cartilage layer. Performing 3 osteotomies enables a better reshaping of the trochlear groove. Pearls and pitfalls and advantages and disadvantages are, respectively, described in Table 2 and Table 3.
Table 2.
Pearls and Pitfalls
| Pearls |
|
| Pitfalls |
|
Table 3.
Advantages and Disadvantages of the Femoral Sulcus Deepening Trochleoplasty of Lyon
| Advantages |
|
| Disadvantages |
|
MPFL, medial patellofemoral ligament.
Davies et al.23 reviewed the outcomes of 702 patients undergoing specifically a sulcus-deepening trochleoplasty. The rate of dislocation and persistent apprehension test ranged, respectively, between 0% and 8% and 0% and 29%. Furthermore, up to 83% of patients were able to return to sport.
The results of deepening trochleoplasty might improve over time and beyond 1 year of follow-up. This would clarify the doubts of patients desiring to have a reliable prediction of the postoperative course.24
Controversial is whether this procedure also should be indicated for patients with severe trochlea dysplasia but no history of dislocations. Zimmermann et al.25 treated 15 patients with severe trochlear dysplasia and chronic PF pain with deepening trochleoplasty. The authors showed a reduced pain and improved clinical outcomes in this group of patients. The sulcus deepening trochleoplasty is a technically demanding procedure that has been feared and avoided for long time. The indications previously highlighted might change in the future, including also patients with severe trochlear dysplasia without any history of lateral patellar dislocation.
It reliably protects against recurrent patellar instability, leading to good postoperative clinical outcomes. However, it might not reduce the development of PF osteoarthritis and might lead to residual pain and range of motion limitation.
This article describes a stepwise approach to prepare the trochlea, remove the subchondral bone, osteotomize the articular surface, and fix the facets with 3 anchors while minimizing the risk of complications.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.H.D. reports royalties from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows a sulcus deepening trochleoplasty performed on a patient with objective patellar instability and trochlear dysplasia type D. The patient, under sedation and regional anesthesia, is positioned in a supine position with the knee flexed and 2 supports, one lateral and one distal. A 10-midline skin incision is performed. The transquadricipital tendon approach is preferred. The supratrochlear synovial membrane is performed. The native groove, the medial and lateral facets, and the new planned groove lines are marked. After measuring the prominence, a strip cortex is removed around the femorotrochlear osteochondral junction. Multiple convergent tunnels through the trochlear undersurface cancellous bone are performed and the bone bridges between the tunnels are removed. The cartilage marked lines are incised with a surgical blade No. 23 and then osteotomized. The facets are rotated slightly to increase the sulcus angle. Fixation of the facets is performed with 3 BioComposite Labral SwiveLock anchors. Gaps between the facets are fulfilled with bone and the supratrochlear synovium is closed.
References
- 1.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 2.Dejour D.H., Mesnard G., Giovannetti de Sanctis E. Updated treatment guidelines for patellar instability: "Un menu a la carte". J Exp Orthop. 2021;8:109. doi: 10.1186/s40634-021-00430-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albee F. Bone graft wedge in the treatment of habitual dislocation of the patella. Med Rec. 1915;88:257–259. [Google Scholar]
- 4.Leclerc J.T., Dartus J., Labreuche J., et al. Complications and outcomes of trochleoplasty for patellofemoral instability: A systematic review and meta-analysis of 1000 trochleoplasties. Orthop Traumatol Surg Res. 2021;107 doi: 10.1016/j.otsr.2021.103035. [DOI] [PubMed] [Google Scholar]
- 5.Goutallier D., Raou D., Van Driessche S. Retro-trochlear wedge reduction trochleoplasty for the treatment of painful patella syndrome with protruding trochleae. Technical note and early results. Rev Chir Orthop Reparatrice Appar Mot. 2002;88:678–685. [in French] [PubMed] [Google Scholar]
- 6.Beaufils P., Thaunat M., Pujol N., Scheffler S., Rossi R., Carmont M. Trochleoplasty in major trochlear dysplasia: Current concepts. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:7. doi: 10.1186/1758-2555-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pollard B. Old dislocation of patella reduced by intra articular operation. Lancet. 1891;1:988. [Google Scholar]
- 8.Masse Y. Trochleoplasty. Restoration of the intercondylar groove in subluxations and dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot. 1978;64:3–17. [in French] [PubMed] [Google Scholar]
- 9.Dejour H., Walch G., Neyret P., Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:45–54. [in French] [PubMed] [Google Scholar]
- 10.Dejour D., Saggin P. The sulcus deepening trochleoplasty—the Lyon's procedure. Int Orthop. 2010;34:311–316. doi: 10.1007/s00264-009-0933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bereiter H., Gautier E. Trochleoplasty as surgical approach for the treatment of recurrent patella instability in patients with trochlear dysplasia of the femur. Arthroskopie. 1994;7:281–286. [in German] [Google Scholar]
- 12.Blønd L., Schöttle P.B. The arthroscopic deepening trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:480–485. doi: 10.1007/s00167-009-0935-5. [DOI] [PubMed] [Google Scholar]
- 13.Camathias C., Speth B.M., Rutz E., et al. Solitary trochleoplasty for treatment of recurrent patellar dislocation. JBJS Essent Surg Tech. 2018;8:e11. doi: 10.2106/JBJS.ST.17.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dean C.S., Chahla J., Serra Cruz R., Cram T.R., LaPrade R.F. Patellofemoral joint reconstruction for patellar instability: Medial patellofemoral ligament reconstruction, trochleoplasty, and tibial tubercle osteotomy. Arthrosc Tech. 2016;5:e169–e175. doi: 10.1016/j.eats.2015.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vogel L.A., Pace J.L. Trochleoplasty, medial patellofemoral ligament reconstruction, and open lateral lengthening for patellar instability in the setting of high-grade trochlear dysplasia. Arthrosc Tech. 2019;8:e961–e967. doi: 10.1016/j.eats.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laidlaw M.S., Feeley S.M., Ruland J.R., Diduch D.R. Sulcus-deepening trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar instability. Arthrosc Tech. 2018;7:e113–e123. doi: 10.1016/j.eats.2017.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dejour D., Renaud P., Lecoultre B. Douleur et instabilité rotulienne: Essai de classification. Médecine et Hygiène. 1998;56:1466–1470. [Google Scholar]
- 18.Giovannetti de Sanctis E., Mesnard G., Dejour D.H. Trochlear dysplasia: When and how to correct. Clin Sports Med. 2022;41:77–88. doi: 10.1016/j.csm.2021.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Dejour D.H. Editorial Commentary: Trochlear dysplasia: Can we change its natural history or degenerative prognosis? Arthroscopy. 2020;36:3028–3030. doi: 10.1016/j.arthro.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Zaffagnini S., Previtali D., Tamborini S., Pagliazzi G., Filardo G., Candrian C. Recurrent patellar dislocations: Trochleoplasty improves the results of medial patellofemoral ligament surgery only in severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2019;27:3599–3613. doi: 10.1007/s00167-019-05469-4. [DOI] [PubMed] [Google Scholar]
- 21.Ren B., Zhang X., Zhang L., et al. Isolated trochleoplasty for recurrent patellar dislocation has lower outcome and higher residual instability compared with combined MPFL and trochleoplasty: A systematic review. Arch Orthop Trauma Surg. 2019;139:1617–1624. doi: 10.1007/s00402-019-03244-1. [DOI] [PubMed] [Google Scholar]
- 22.van Sambeeck JDP, van de Groes S.A.W., Verdonschot N., Hannink G. Trochleoplasty procedures show complication rates similar to other patellar-stabilizing procedures. Knee Surg Sports Traumatol Arthrosc. 2018;26:2841–2857. doi: 10.1007/s00167-017-4766-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies M.R., Allahabadi S., Diab T.E., et al. Sulcus-deepening trochleoplasty as an isolated or combined treatment strategy for patellar instability and trochlear dysplasia: A systematic review. Arthrosc Sports Med Rehabil. 2020;2:e661–e669. doi: 10.1016/j.asmr.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McNamara I., Bua N., Smith T.O., Ali K., Donell S.T. Deepening trochleoplasty with a thick osteochondral flap for patellar instability: Clinical and functional outcomes at a mean 6-year follow-up. Am J Sports Med. 2015;43:2706–2713. doi: 10.1177/0363546515597679. [DOI] [PubMed] [Google Scholar]
- 25.Zimmermann F., Milinkovic D.D., Balcarek P. Outcomes after deepening trochleoplasty and concomitant realignment in patients with severe trochlear dysplasia with chronic patellofemoral pain: Results at 2-year follow-up. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows a sulcus deepening trochleoplasty performed on a patient with objective patellar instability and trochlear dysplasia type D. The patient, under sedation and regional anesthesia, is positioned in a supine position with the knee flexed and 2 supports, one lateral and one distal. A 10-midline skin incision is performed. The transquadricipital tendon approach is preferred. The supratrochlear synovial membrane is performed. The native groove, the medial and lateral facets, and the new planned groove lines are marked. After measuring the prominence, a strip cortex is removed around the femorotrochlear osteochondral junction. Multiple convergent tunnels through the trochlear undersurface cancellous bone are performed and the bone bridges between the tunnels are removed. The cartilage marked lines are incised with a surgical blade No. 23 and then osteotomized. The facets are rotated slightly to increase the sulcus angle. Fixation of the facets is performed with 3 BioComposite Labral SwiveLock anchors. Gaps between the facets are fulfilled with bone and the supratrochlear synovium is closed.
This video shows a sulcus deepening trochleoplasty performed on a patient with objective patellar instability and trochlear dysplasia type D. The patient, under sedation and regional anesthesia, is positioned in a supine position with the knee flexed and 2 supports, one lateral and one distal. A 10-midline skin incision is performed. The transquadricipital tendon approach is preferred. The supratrochlear synovial membrane is performed. The native groove, the medial and lateral facets, and the new planned groove lines are marked. After measuring the prominence, a strip cortex is removed around the femorotrochlear osteochondral junction. Multiple convergent tunnels through the trochlear undersurface cancellous bone are performed and the bone bridges between the tunnels are removed. The cartilage marked lines are incised with a surgical blade No. 23 and then osteotomized. The facets are rotated slightly to increase the sulcus angle. Fixation of the facets is performed with 3 BioComposite Labral SwiveLock anchors. Gaps between the facets are fulfilled with bone and the supratrochlear synovium is closed.