Abstract
Objective:
Despite growing numbers of women Veterans, it is unclear whether the impact of common post-deployment mental health concerns on key aspects of family functioning varies by gender. We examined whether associations between PTSD, depression, and problematic alcohol use and intimate relationship quality and parenting self-efficacy differed among men and women in a large, gender-balanced sample of post-9/11 veterans.
Method:
Participants included 2,348 veterans (51.49% women) of the wars in Iraq and Afghanistan who were part of a larger study of gender differences in effects of wartime deployment. Veterans who were married or in a relationship (n = 1,536, 49.09% women) reported overall relationship quality. Veterans with children under age 18 (n = 1,049; 51.57% women) self-reported on their sense of efficacy as parents. All participants reported symptoms of PTSD, depression, and problematic alcohol use. We used a series of hierarchical linear regressions to test gender as a moderator of each post-deployment mental health concern and the family functioning constructs of interest.
Results:
Each post-deployment mental health concern was associated with reduced relationship quality and parenting self-efficacy, and these associations were largely consistent across gender. However, links between reduced parenting self-efficacy and increased PTSD and depressive symptoms were stronger in women compared to men.
Conclusions:
Post-deployment mental health concerns are associated with impairment in key family relationships for both men and women veterans. This impact may be particularly profound for parenting self-efficacy among women veterans, highlighting the potential importance of targeted interventions in this domain.
Keywords: Gender, veterans, PTSD, parenting, relationship quality
Post-Deployment Mental Health and Family Functioning in Men and Women Veterans
Mental health sequelae of military deployment can impact both an individual and their closest relationships, long after service members return home. Addressing the impact of post-deployment mental health concerns on both the individual who served and their family members is critical to enhancing veterans’ well-being and building resilience of the military family system overall (Committee on the Well-Being of Military Families et al., 2019; Vogt et al., 2019). As the number of women serving in the military has increased, so too has the number of women impacted by mental health concerns from a range of deployment-related experiences (Street et al., 2009). In light of these demographic changes, it is important to understand both similarities and differences in how men and women’s family relationships are impacted by post-deployment mental health concerns. The current manuscript addresses this question by examining associations of gender and post-deployment mental health concerns with two indicators of family functioning: romantic partnership quality and parenting self-efficacy.
Post-deployment mental health concerns have been linked to worsened quality of romantic relationships (Bakhurst et al., 2018; Creech et al., 2016; Monson et al., 2009; Smith et al., 2017; Vogt et al., 2017). The evidence is most robust for PTSD and depressive symptoms (Creech et al., 2019; Foran et al., 2013; Riviere et al., 2012; Smith et al., 2017; Vogt et al., 2017). In their reviews of the impact of PTSD on veterans’ families and marital relationships, Galovski & Lyons (2004) and Monson, Taft, and Fredman (2009) highlighted efforts dating back to the Vietnam War to understand drivers of marital distress among service members and veterans following deployment. A study of 2,101 Vietnam veterans identified an association of PTSD symptoms and marital distress that was mediated by the veterans’ engagement in “antisocial behaviors” (Gimbel & Booth, 1994). Later work with veterans of Operation Desert Storm showed that PTSD symptoms predicted worse family adjustment (which encompassed marital quality) after 1.5 to 2 years, although the effects were small (Taft et al., 2008). Research among the most recent cohort of service members and veterans (i.e., those deployed in support of the wars in Iraq and Afghanistan following 9/11/2001) largely echoes these findings. In one study of 194 service members, both PTSD and depressive symptoms showed small associations with marital distress; distress predicted intent to divorce at follow-up (Foran et al., 2013). More recent longitudinal analyses linked PTSD symptoms with subsequent relationship distress at follow-up periods of one year (Creech et al., 2019) and 3.5 years (Smith et al., 2017; Vogt et al., 2017). Related analyses demonstrated associations of depressive symptoms with subsequent relationship distress (Smith et al., 2017). One study among 1,143 National Guard members and partners identified associations of hazardous alcohol use and relationship distress, illustrating the importance of considering a range of post-deployment mental health concerns in addition to PTSD (Blow et al., 2013). Overall, the literature suggests that post-deployment mental health concerns, particularly PTSD and depressive symptoms, are linked with poor romantic relationship outcomes.
One major limitation of research on post-deployment mental health concerns and relationship quality to date is that much of this work has used samples comprised entirely or predominantly of men. There has been far less attention devoted to gender differences in associations of post-deployment mental health concerns and romantic relationship quality, although there are some exceptions. For example, Renshaw and colleagues evaluated the association of PTSD symptoms with relationship distress among 375 male Vietnam veterans and 90 female Vietnam veterans. PTSD symptoms were linked to distress for both men and women but the association was somewhat stronger for the women (Renshaw et al., 2014). In contrast, Creech and colleagues (2019) found cross-sectional support for an association between baseline PTSD symptoms and relationship distress among men but not women in a sample of post-9/11 veterans (70% male). They did not observe gender differences in the relation of PTSD symptoms and relationship distress over time (Creech et al., 2019). One of the few truly gender-balanced studies of post-deployment mental health concerns and relationship quality showed similar associations between PTSD and relationship at follow-up for men and women veterans (Smith et al., 2017; Vogt et al., 2017). Conversely, depressive symptoms were associated with relationship distress among women but not men in this sample (Smith et al., 2017). Taken together, these mixed findings and the relative dearth of studies with gender-balanced samples make it difficult to draw definitive conclusions about the role of gender in the association between post-deployment mental health concerns and romantic relationship quality.
Post-deployment mental health concerns have also been associated with negative parenting outcomes among veterans. As with studies of romantic partnership quality, much of this work has focused on PTSD specifically. Creech and Misca (2017) reviewed the literature on PTSD and parenting behavior and found support for an association of PTSD and self-reported deficits in parenting in multiple samples of male service members and veterans (evidence for a link with observed impairments in parenting behaviors was less clear). This association between PTSD and self-reported parenting deficits was also reported among post-9/11 veterans (Smith et al., 2017; Vogt et al., 2017). In contrast, a cross-sectional study among active-duty Navy fathers suggested that depressive symptoms but not PTSD symptoms mediated the association of exposure to warfare and parenting stress (Yablonsky et al., 2016). Less is known about parenting self-efficacy, a parent’s belief that they are capable and effective in the parenting role (Johnston & Mash, 1989). This construct is a component of reduced parenting self-competence, which has been linked to poor mental health outcomes in children (Zalta et al., 2018). Bui and colleagues (2017) found that greater parenting self-competence (which encompassed self-efficacy and satisfaction) was associated with improved family functioning in a predominantly male, post-9/11 veteran sample. Depressive symptoms showed a small association with reduced parenting self-competence (Bui et al., 2017). Subsequent work in this sample showed that reduced parenting sense of competence mediated the association of certain PTSD symptoms and overall family functioning (Laifer et al., 2017). The sample composition precluded gender comparisons. Overall, this literature indicates that various constructs of parenting, including self-competence, satisfaction, self-efficacy, and functioning, are negatively impacted by symptoms of depression and PTSD.
Similar to the literature on post-deployment mental health concerns and romantic relationship quality, research on gender differences in post-deployment mental health and parenting has been limited by a low prevalence of participants identifying as women (Creech & Misca, 2017). In civilian samples, PTSD and depression have shown negative associations with parenting self-efficacy and satisfaction (Hershkowitz et al., 2017; Kohlhoff & Barnett, 2013), and this is true more often for mothers than for fathers (Reece & Harkless, 1998). Investigations of gender differences in related constructs (e.g., parenting satisfaction, functioning) in veterans have revealed somewhat mixed findings for their associations with post-deployment mental health concerns. For example, PTSD symptoms showed small associations with reduced parenting satisfaction in both an all-female (Berz et al., 2008) and all-male sample. (Samper et al., 2004). A gender-balanced study of post-9/11 veterans identified longitudinal associations of PTSD symptoms with impaired parenting functioning but not reduced satisfaction for both men and women (Smith et al., 2017). Depressive symptoms were linked to later reductions in parenting satisfaction for both men and women (Smith et al., 2017). However, probable PTSD diagnosis predicted reduced parenting satisfaction in men but not women in the same sample (Vogt et al., 2017). Our review did not identify evidence supporting gender differences in the association of problematic alcohol use and parenting. However, only one study examined a gender-balanced sample (Smith et al., 2017). This highlights the need for further research on alcohol misuse and other post-deployment mental health concerns, gender, and parenting.
The Current Study
Despite growing numbers of women in the military, there is limited research examining gender differences and similarities in how common post-deployment mental health concerns are related to important family functioning outcomes such as romantic relationship quality and parenting self-efficacy in post-9/11 veterans (Creech & Misca, 2017; Monson et al., 2009). Our goal in the present study was to examine whether associations of post-deployment mental health concerns with these outcomes differed in men versus women veterans using a large gender-balanced sample of veterans deployed in support of the wars in Iraq and Afghanistan after Sept. 11, 2001. We sought to build on a literature that has focused largely on PTSD by also examining the associations of depressive symptoms and problematic alcohol use with relationship quality and parenting self-efficacy. Regarding romantic relationship quality, we were unable to identify specific a priori hypotheses, given the inconsistent literature on gender differences in associations with mental health concerns. Regarding parenting self-efficacy, we hypothesized stronger associations between post-deployment mental health concerns and parenting self-efficacy for women relative to men based on existing literature in civilian samples for gender differences in parenting self-efficacy (Hershkowitz et al., 2017; Kohlhoff & Barnett, 2013; Reece & Harkless, 1998).
Method
Participants
Participants include 2,348 veterans, with women oversampled (51.49% women, 21.98% non-white, 10.52% Hispanic/Latino) who were deployed in support of the wars in Afghanistan and Iraq after Sept. 11, 2001. The veterans were part of a larger study on gender differences in deployment and post-deployment experiences and were randomly selected from a roster of service members who had since separated from active duty. The full participant inclusion criteria and recruitment details are described by Street, et al. (2013).
Veterans in the full sample ranged in age from 20 to 65 (M = 35.64, SD = 9.53). For the relationship analyses, we included only participants who reported that they were either married or in a romantic relationship (n = 1,536, Sample 1). Participants in Sample 1 ranged in age from 20 to 65. For the parenting analyses, we included only participants who had children under age 18 who were living at home at the time of the survey (n = 1,049, Sample 2). Participants in Sample 2 ranged in age from 22 to 63. See Table 1 for demographic characteristics by sample; there was some overlap of participants across samples.
Table 1.
Demographic Characteristics of Parenting, Relationship Satisfaction Subsamples
| Variable | Full Sample (n = 2,348) | Sample 1 (n = 1,536) | Sample 2 (n = 1,049) |
|---|---|---|---|
|
| |||
| Women (n, %) | 1,209 (51.49%) |
754 (49.09%) | 541 (51.57%) |
| Age (M, SD) | 35.64 (9.53) | 35.62 (9.25) | 35.25 (7.79) |
| Education (n, %) | |||
| High school graduate/GED | 244 (10.39%) | 152 (9.90%) | 110 (10.49%) |
| Vocational or technical training | 93 (3.96%) | 66 (4.30%) | 53 (5.05%) |
| Some college | 1,080 (46.0%) | 687 (44.73%) | 478 (45.57%) |
| Four-year college graduate | 437 (18.61%) | 305 (19.86%) | 203 (19.35%) |
| Some graduate or professional school | 185 (7.88%) | 124 (8.07%) | 80 (7.63%) |
| Graduate or professional degree | 296 (12.61%) | 199 (12.96%) | 123 (11.73%) |
| Race | |||
| Non-white | 516 (21.98%) | 285 (18.55%) | 252 (24.02%) |
| White | 1,743 (74.23%) |
1,203 (78.32%) |
761 (72.55%) |
| Ethnicity | |||
| Hispanic or Latino | 247 (10.52%) | 158 (10.29%) | 120 (11.44%) |
| Not Hispanic or Latino | 2,074 (88.33%) |
1,366 (88.93%) |
925 (88.18%) |
| Marital status | — | — | 876 (83.5%) |
| Number of children (M, SD) | 2.14 (1.19) | 1.52 (1.39) | 2.12 (1.22) |
| PTSD symptoms (M, SD) | 33.82 (18.11) | 32.54 (17.39) | 34.16 (18.37) |
| Depressive symptoms (M, SD) | 8.15 (6.88) | 7.30 (6.46) | 8.00 (6.84) |
| Problematic alcohol use (M, SD) | 0.67 (1.11) | 0.60 (1.06) | 0.59 (1.06) |
| Relationship quality (M, SD) | — | 30.82 (6.81) | — |
| Parenting self-efficacy (M, SD) | — | — | 31.36 (6.38) |
Note. Percent = Valid percent.
Measures
Demographics.
Participants were asked to self-report their gender (options included “male” or “female”), age, race, ethnicity, educational attainment, relationship status, and number of children. Table 1 summarizes demographic information and presents means and standard deviations for each study measure by sample.
PTSD Symptoms.
PTSD symptoms were assessed using the Posttraumatic Stress Disorder Checklist-Military (PCL-M), which measures the degree to which respondents were bothered by PTSD symptoms resulting from a stressful military experience (Weathers et al., 1991). The PCL-M is based on PTSD symptoms as defined in the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV). Participants reported their symptoms in the past month, using a response scale ranging from 1 (not at all) to 5 (extremely). Scores were summed to create a total score ranging from 17 – 85, with higher scores indicating greater distress due to PTSD symptoms. Internal consistency for the total score was excellent at 0.97 for both Samples 1 and 2.
Depressive Symptoms.
Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). The CES-D is a 10-item measure that assesses frequency of past-week symptoms of depression using a response scale ranging from 0 (none of the time or less than one day) to 3 (5–7 days). Responses for “I was happy” and “I enjoyed life” were reversed and scores were summed to create a total score ranging from 0 – 30. Higher scores reflected greater self-reported depressive symptoms. Internal consistency for the CES-D was excellent (Cronbach’s α = 0.90) in Sample 1 and good (Cronbach’s α = 0.89) in Sample 2.
Problematic Alcohol Use.
Problematic alcohol use was measured using the CAGE Questionnaire, a four-item measure that assesses self-reported signs of alcohol dependency (Mayfield et al., 1974). The measure abbreviation is derived from the four items: 1) Have you felt you ought to cut down on your drinking?; 2) have people annoyed you by criticizing your drinking?; 3) have you felt bad or guilty about your drinking?; 4) have you had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)? Respondents reply yes or no to these questions and a sum score is produced by totaling the number of yes responses. Internal consistency for the CAGE was acceptable in Sample 1 (Cronbach’s α = 0.74) and Sample 2 (Cronbach’s α = 0.73).
Relationship Quality.
Romantic relationship quality was measured in Sample 1 participants using the Dyadic Adjustment Scale-7 (DAS-7) (Hunsley et al., 2001). The original Dyadic Adjustment Scale is a 32-item measure that assesses multiple aspects of romantic relationship quality, including overall functioning, positive expression, and overall satisfaction (Spanier, 1976). We used the seven-item short form, which has shown strong convergent validity with the original measure. Participants reported the degree to which they agreed with their partner on key domains (e.g., philosophy of life) and engaged in certain activities together (e.g., collaborating on a project). Responses used a 1 to 6 Likert scale, with higher scores indicating greater agreement with the statement or more frequent engagement in the example activity. Participants also rated their overall happiness with the relationship on a 1 (extremely unhappy) to 7 (perfect) scale. Scores were summed to create a total score ranging from 7 – 43, with higher scores reflecting improved relationship quality. Internal consistency was good at 0.86 for Sample 1.
Parenting Self-Efficacy.
Parenting self-efficacy was measured among Sample 2 participants using the Parenting Sense of Competence (PSOC) self-efficacy subscale (Johnston & Mash, 1989). Parenting self-efficacy is linked to parenting satisfaction (one’s affective response to the role) but reflects the cognitive appraisals of one’s parenting capacity. Lower parenting self-efficacy is linked to worse family functioning and child mental health outcomes (Johnston & Mash, 1989; Laifer et al., 2019). The PSOC parenting self-efficacy subscale asks parents to report the degree to which they agreed with seven statements about their parenting competence, capability, and problem-solving skills (e.g., “I met my own personal expectations for expertise in caring for my child”), using a response scale ranging from 1 (strongly disagree) to 6 (strongly agree). Scores were summed to create a total score ranging from 7 – 42; lower scores reflected reduced parenting self-efficacy. This scale has been validated in a post-9/11 veteran sample (Bui et al., 2017; N = 178, 92.7% male). Internal consistency for the scale in Sample 2 was excellent (Cronbach’s α = 0.90).
Procedure
Potential participants were identified from the VA’s Environmental Epidemiology Operation Enduring Freedom/Operation Iraqi Freedom Registry; women were oversampled. Recruitment followed a multistage mailing process (Dillman, 2007; Street et al., 2013). An introductory letter describing the study was sent to potential participants, followed by an informed consent fact sheet, the survey, stamped return envelope, and a $5 incentive. Subsequent mailing stages included a thank-you/reminder note and additional copies of the survey for non-responders. Data collection took place between fall 2009 and summer 2010. The survey response rate was 48.6%. Study approval was obtained from the Institutional Review Board of VA Boston Healthcare System prior to initiating data collection.
Data Analytic Plan
We examined a series of hierarchical linear regression models using Sample 1 to test whether the associations of relationship quality with post-deployment mental health concerns varied by gender. Due to the high correlation of PTSD and depressive symptoms (rs = .76 in Samples 1 and 2), we elected to examine each post-deployment mental health concern via separate models. In each model, we entered relationship quality as the dependent variable and gender and mental health concern as main effects in Step 1, then examined mental health concern, gender, and a Gender × Mental health concern interaction term in Step 2. We centered all mental health symptoms to create their respective interaction terms. Finally, we adjusted for education level, age, and number of children, given known associations of these constructs with either mental health concerns or relationship quality (Sorokowski et al., 2017).
We followed a similar approach in Sample 2 to test whether associations of parenting self-efficacy with PTSD symptoms, depressive symptoms, or problematic alcohol use varied by gender. In these analyses we additionally adjusted for participants’ marital status. Missing data were addressed using listwise deletion for all analyses. In light of the increased focus on limitations of p-values as a heuristic guiding data interpretations particularly in large samples (Wasserstein & Lazar, 2016), we chose to base our analyses and conclusions on effect sizes. However, we present p-values in our tables to provide further context for our findings and interpretations. All data preparation and analyses were conducted using SPSS Statistical Software Version 26.
Results
Consistent with results from the parent study (Street et al. 2013), PTSD symptoms were comparable for men and women. Women reported higher depressive symptoms and parenting self-efficacy, and men reported higher problematic alcohol use. All observed differences were small (|d| ≤ 0.26, see Table 2).
Table 2.
Means and Standard Deviations of Key Constructs By Sample and Gender
| Total Sample | Sample 1 | Sample 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Variable | Women M (SD) |
Men M (SD) |
d | p | Women M (SD) |
Men M (SD) |
d | p | Women M (SD) |
Men M (SD) |
d | p |
| PTSD symptoms |
33.39 (18.26) |
34.28 (17.93) |
0.05 | .937 | 31.88 (17.43) |
33.18 (17.35) |
0.08 | .143 | 34.11 (18.68) |
34.12 (18.06) |
<.001 | .993 |
| Depressive symptoms |
8.69 (7.14) |
7.57 (6.55) |
−0.16 | <.001 | 7.78 (6.73) |
6.84 (6.16) |
−0.15 | .004 | 8.65 (7.13) |
7.32 (6.44) |
−0.23 | .002 |
| Problematic alcohol use | 0.56 (1.03) |
0.78 (1.18) |
0.20 | <.001 | 0.51 (0.98) |
0.70 (1.13) |
0.18 | .001 | 0.46 (0.92) |
0.72 (1.17) |
0.26 | <.001 |
| Relationship quality |
— | — | — | — | 30.86 (7.00) |
30.77 (6.63) |
−0.01 | .797 | — | — | — | — |
| Parenting self-efficacy | — | — | — | — | — | — | — | — | 31.87 (6.67) |
30.81 (6.01) |
−0.17 | .008 |
Note. PCL-M = PTSD Symptom Checklist, Military Version; PSOC = Parenting Sense of Competence, Self-Efficacy Scale; DAS = Dyadic Adjustment Scale-Short Form; CES-D = Center for Epidemiological Studies Depression; CAGE = Problematic Alcohol Use (Cut down, Annoyed, Guilty, Eye-Opener). Sample 1 was used for relationship quality analyses; Sample 2 was used for analyses of parenting self-efficacy.
Post-Deployment Mental Health Concerns, Gender, and Relationship Quality
Table 3 shows results of analyses examining the associations of post-deployment mental health concerns, gender, and relationship quality, controlling for education, age, and number of children. We found a small association of PTSD symptoms (b = −0.08, SE = .01, 95%CI [−0.10, −0.06], β = −.19) with reduced relationship quality. The association between gender and relationship quality was negligible (b = −0.37, SE = 0.37, 95%CI [−1.08, 0.35], β = −.03). Other post-deployment mental health concerns showed small associations with reduced relationship quality (depressive symptoms: b = −0.32, SE = 0.03, 95%CI [−0.38, −0.27], β = −.31; Alcohol use: b = −0.64, SE = 0.17, 95%CI [−0.97, −0.31], β = −.10). The main effects of gender on relationship quality were similarly trivial in these models (see Table 3).
Table 3.
Main Effects and Moderation of the Relation Between Gender, Post-Deployment Mental Health Concerns, and Relationship Quality
| Predictor | b (SE) | β | p | 95% CL [LL, UL] | Adjusted R-square |
|---|---|---|---|---|---|
|
| |||||
| Main Effects Analyses | |||||
|
| |||||
| Model 1: PTSD | |||||
| Gender | −0.37 (0.37) | −0.03 | .315 | [−1.08, 0.35] | 0.04 |
| PTSD Total | −0.08 (0.01) | −0.19 | < .001 | [−0.10, −0.06] | |
| Model 2: Depressive Symptoms | |||||
| Gender | 0.09 (0.36) | 0.01 | .810 | [−0.61, 0.78] | 0.10 |
| Depressive sx | −0.33 (0.03) | −0.31 | < .001 | [−0.38, −0.28] | |
| Model 3: Problematic Alcohol Use | |||||
| Gender | −0.42 (0.37) | −0.03 | .262 | [−1.15, 0.31] | 0.01 |
| Alcohol | −0.64 (0.17) | −0.10 | < .001 | [−0.97, −0.31] | |
|
| |||||
| Moderation Analyses | |||||
|
| |||||
| Model 1: PTSD Total (n = 1,480) | |||||
| Gender | −0.35 (0.37) | −0.03 | .334 | [−1.07, 0.36] | |
| PTSD Total | −0.09 (0.01) | −0.23 | <.001 | [−0.12, −0.06] | |
| Gender x PTSD | 0.03 (0.02) | 0.06 | .106 | [−0.01, 0.07] | 0.04 |
| Model 2: Depressive Symptoms (n = 1,477) | |||||
| Gender | 0.09 (0.36) | 0.01 | 0.807 | [−0.61, 0.78] | |
| Depressive sx | −0.36 (.04) | −0.35 | <.001 | [−0.44, −0.29] | |
| Gender x Dep | 0.07 (0.05) | 0.05 | .205 | [−0.04, 0.17] | 0.10 |
| Model 3: Problematic Alcohol Use (n = 1,473) | |||||
| Gender | −0.42 (0.37) | −0.03 | .255 | [−1.15, 0.31] | |
| Alcohol | −0.87 (0.22) | −0.14 | <.001 | [−1.30, −0.43] | |
| Gender x Alcohol | 0.52 (0.34) | .05 | .124 | [−0.14, 1.17] | 0.01 |
Note. All models controlled for age, education, and number of children. Dep = depressive, PTSD = posttraumatic stress disorder, sx = symptoms
Table 3 also shows the results of analyses examining gender as a moderator of the associations of relationship quality with PTSD symptoms, depressive symptoms, and problematic alcohol use. In each model, the interaction terms were small, and all confidence intervals included 0, indicating that gender does not moderate associations between post-deployment mental health and relationship quality.
Post-Deployment Mental Health Concerns, Gender, and Parenting Self-Efficacy
We found a small association between PTSD symptoms and parenting self-efficacy (b = −0.07, SE = .01, 95%CI [−0.09, −0.05], β = −.21) and a negligible association between gender and parenting self-efficacy (b = 0.39, SE = 0.43, 95%CI [−0.45, 1.23], β = .03), after controlling for age, education, number of children, and marital status. See Table 4. Depressive symptoms and problematic alcohol use similarly showed small associations with reduced parenting self-efficacy in their respective models (depressive symptoms: b = −0.29, SE = .03, 95%CI [−0.35, −0.23], β = −.31; alcohol use: b = −0.62, SE = .20, 95%CI [−1.001, −0.23], β = −.10). There was little support for an association of parenting self-efficacy with gender in these models.
Table 4.
Gender as a Moderator of the Relation Between Post-Deployment Mental Health Concerns and Parenting Self-Efficacy
| Predictor | b (SE) | β | p | 95% CL [LL, UL] | Adjusted R-square |
|---|---|---|---|---|---|
|
| |||||
| Main Effects Analyses | |||||
|
| |||||
| Model 1: PTSD Total | |||||
| Gender | 0.39 (0.43) | .03 | .360 | [−0.45, 1.23] | |
| PTSD Total | −0.07 (0.01) | −.21 | < .001 | [−0.09, −0.05) | .08 |
| Model 2: Depressive Symptoms | |||||
| Gender | 0.74 (0.42) | .06 | .075 | [−0.08, 1.56] | |
| Dep | −0.29 (0.03) | −.31 | < .001 | [−0.35, −0.23] | .13 |
| Model 3: Problematic Alcohol Use | |||||
| Gender | 0.19 (0.44) | .02 | .664 | [−0.68, 1.06] | .06 |
| Alcohol | −0.62 (0.20) | −.10 | .002 | [−1.00, −0.23] | |
|
| |||||
| Moderation Analyses | |||||
|
| |||||
| Model 1: PTSD Total (n = 948) | |||||
| Gender | 0.36 (0.43) | .03 | .399 | [−0.48, 1.20] | |
| PSTD Total | −0.04 (0.02) | −.11 | .020 | [−0.07, −0.01] | |
| Gender x PTSD | −0.07 (0.02) | −.13 | .003 | [−0.11, −0.02] | .09 |
| Model 2: Depressive Symptoms (n = 945) | |||||
| Gender | 0.71 (0.42) | .06 | .090 | [−0.11, 1.53] | |
| Dep | −.22 (0.04) | −.24 | <.001 | [−0.31, −0.14] | |
| Gender x Dep | −0.12 (0.06) | −.10 | .039 | [−0.23, −0.01] | .13 |
| Model 3: Problematic Alcohol Use (n = 939) | |||||
| Gender | .19 (0.44) | .02 | .675 | [−0.68,1.05] | |
| Alcohol | −.38 (0.25) | −.06 | .133 | [−0.88, .12] | |
| Gender x Alcohol | −0.58 (0.39) | −.06 | .145 | [−1.35, 0.20] | .06 |
Note. All models controlled for age, education, number of children, and marital status.
Table 4 also shows the results for models examining the interactions of gender with total PTSD symptoms, depressive symptoms, and problematic alcohol use. The associations of PTSD and depressive symptoms with reduced parenting efficacy were stronger for women as compared to men, although the observed effects were small (PTSD symptoms: b = −0.07, SE = 0.02, 95%CI [−0.11, −0.02], β = −.13; Depressive symptoms: b = −0.12, SE = 0.06, 95%CI [−0.23, −0.01], β = −.10). Figure 1 depicts the simple slopes for the interactions of gender with PTSD (Figure 1a) and depressive symptoms (Figure 1b). The confidence interval for the interaction term with problematic alcohol use included 0, indicating no effect (simple slopes not shown).
Figure 1a. Association of PTSD symptoms and parenting self-efficacy by gender.
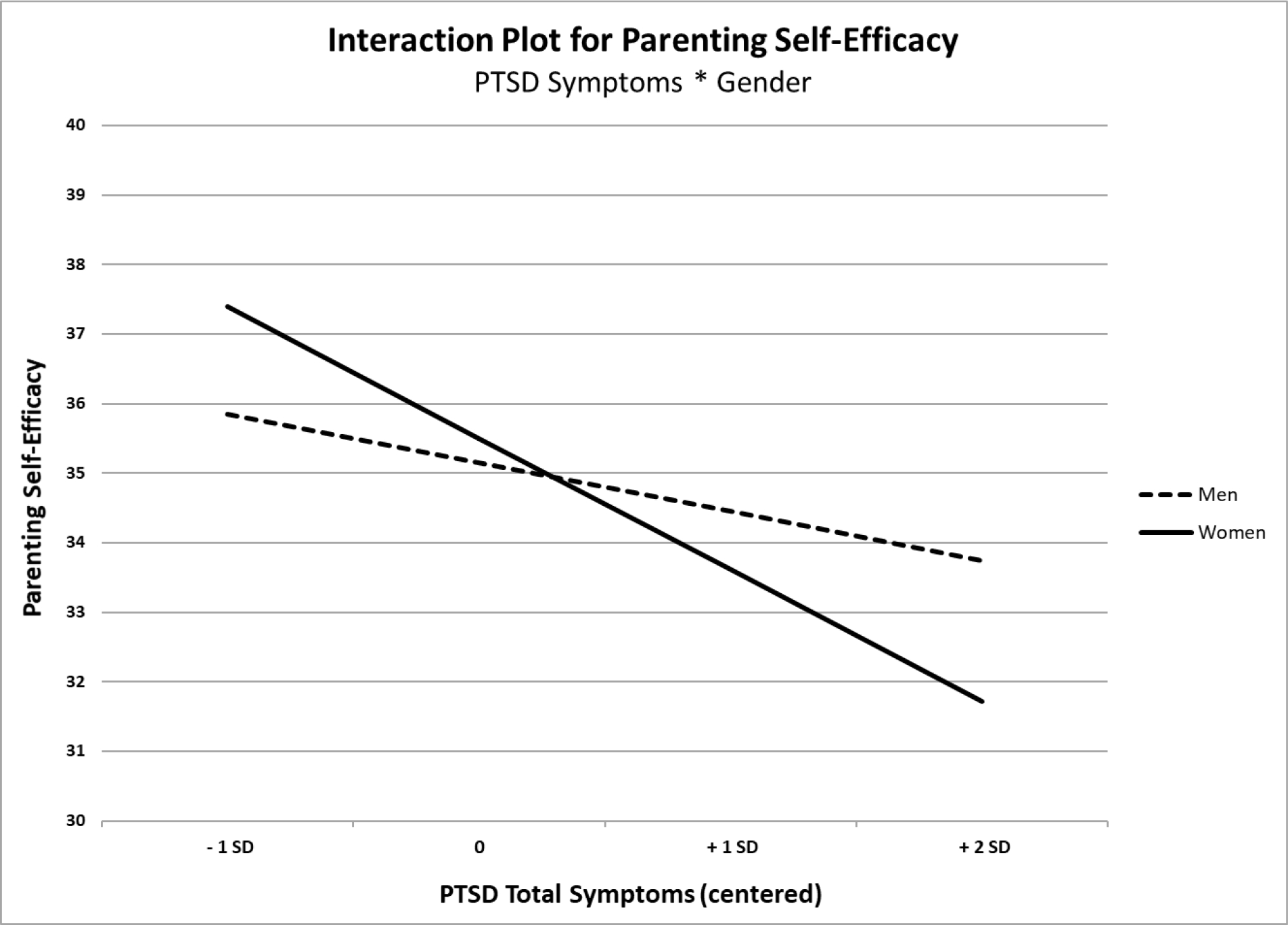
Note. Increased PTSD symptoms showed a stronger link to reduced parenting self-efficacy in women (solid line) than men (dashed line) in this sample.
Figure 1b. Association of depressive symptoms and parenting self-efficacy by gender.
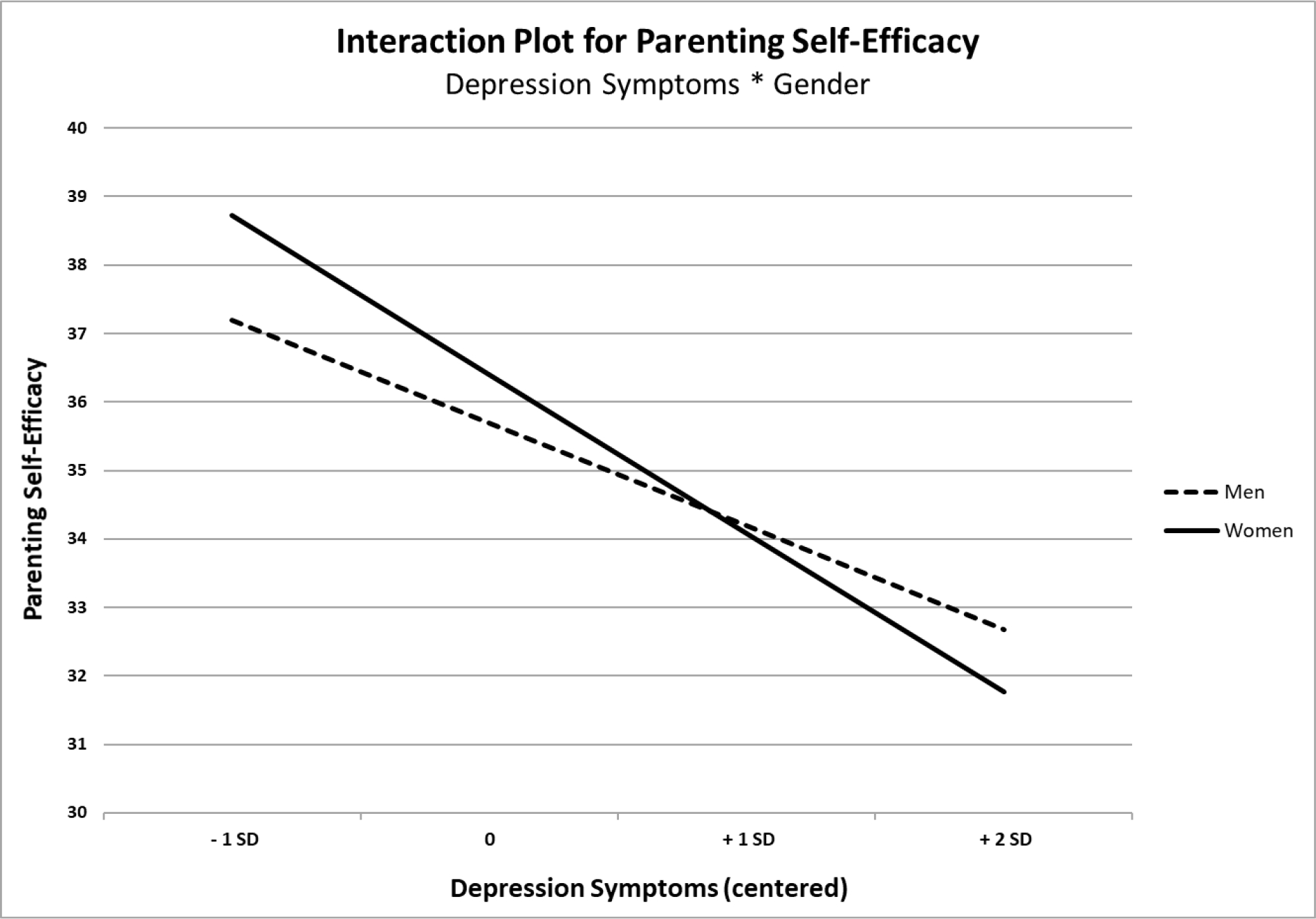
Note. Increased depressive symptoms showed a stronger link to reduced parenting self-efficacy in women (solid line) than men (dashed line) in this sample.
Discussion
The wars in Iraq and Afghanistan have formally drawn to a close, but the work to address the wounds of war among those who served and their families is ongoing. In an important shift from previous eras, women make up an increasing proportion of the veteran population (Committee on the Well-Being of Military Families et al., 2019). Adequately addressing the needs of this changing veteran population requires that we understand what role, if any, gender plays in the link between common post-deployment mental health concerns and impairment in family relationships. We evaluated the association of PTSD symptoms, depressive symptoms, and problematic alcohol use with romantic relationship quality and parenting self-efficacy in a large, gender-balanced sample of men and women veterans of the wars in Iraq and Afghanistan following Sept. 11, 2001. We found support for a deleterious impact of post-deployment mental health concerns on relationship quality, regardless of gender. Post-deployment mental health concerns also showed negative associations with one’s self-efficacy as a parent, and this association was stronger for women veterans struggling with PTSD or depressive symptoms.
Our results concerning romantic relationship quality are consistent with previous literature demonstrating the negative impact of combat-related PTSD symptoms on functioning in romantic relationships (Creech et al., 2019; Smith et al., 2017). We extended this work by using a large, gender-balanced sample and examining other important post-deployment mental health concerns. The current findings support the value of assessing and addressing relationship quality in both men and women veterans affected by PTSD symptoms, depressive symptoms, or problematic alcohol use. Unlike Smith and colleagues (2017), we did not find support for a gender difference in the association between depressive symptoms and relationship impairment. This may be due, in part, to differences in measurement of these constructs in our study versus work by Smith and colleagues (2017). Detailed assessment of functioning, behavior, and attitudes about romantic relationships will be necessary to fully understand the association of post-deployment mental health concerns, and particularly depressive symptoms, with this important domain for veterans.
Our second finding adds to the growing literature on post-deployment mental health symptoms and parenting-related constructs, offering some of the first evidence for gender differences in the association of such mental health concerns and parenting self-efficacy specifically among veterans. Our results were generally consistent with findings from the civilian literature in that the associations of parenting self-efficacy with post-deployment mental health concerns, particularly PTSD and depressive symptoms, were stronger for women (Hershkowitz et al., 2017; Kohlhoff & Barnett, 2013; Reece & Harkless, 1998). Previous research has explored the salience of parental identity on psychological distress in men and women (Simon, 1992). It is possible that women veterans in the current study more strongly identified with the parental role, and thus were more vulnerable to reduced parenting self-efficacy when managing mental health symptoms. An alternate hypothesis is that variable patterns of exposure to specific trauma types, with sexual trauma more common among women and combat trauma more prevalent among men (Street et al., 2013), may account for the pattern of gender differences we observed. Additional research is required to explore these potential mechanisms.
In contrast to our findings for PTSD and depressive symptoms, we did not see support for gender moderation of the association between problematic alcohol use and parenting self-efficacy. These results echo findings by Smith and colleagues (2017), who did not identify evidence for gender differences in the association of alcohol misuse and parenting satisfaction or functioning. In both studies, the average score for alcohol misuse was below the clinical threshold for the respective measure used. It is possible then, that these findings reflected the relatively low severity of alcohol-related concerns in the samples. The CAGE screener used in the present study was developed to detect more severe hazardous alcohol use and has shown to be less sensitivity in samples of white women (Bradley et al., 1998; Dhalla & Kopec, 2007). It will thus be important to further explore the association of gender and parenting self-efficacy in clinical samples of individuals with alcohol use disorder and via more extensive clinical interviewing or self-report questionnaires.
We note several important limitations to this work. First, we relied on cross-sectional self-report data of the constructs of interest in this paper. The use of self-report data is consistent with the larger literature on relationship and parenting satisfaction, however, adding observational assessments of family and relationship functioning in future studies would allow us to examine the interplay of the associations of self-perceptions and actual behavior in these roles. Although we conceptualized post-deployment mental health concerns as impacting romantic relationship quality and parenting, our use of cross-sectional data means we cannot discern direction of effects or causality. Second, we assessed PTSD symptoms based on DSM-IV. The conceptualization of PTSD was expanded in DSM-5 to include a symptom cluster reflecting negative alterations in mood and cognitions. This new symptom cluster may be highly relevant to constructs such as parenting self-efficacy or relationship functioning and satisfaction. Finally, we relied on a binary conception of gender identity. Examining these constructs in non-binary veterans will be an important area of future research.
Despite these limitations, the current study represents an important contribution to the literature by examining the role of gender in associations of PTSD symptoms and family functioning outcomes in the largest gender-balanced sample to date of veterans deployed in support of the wars in Iraq and Afghanistan. It also has important clinical and policy implications. The Veterans Health Administration recently adopted a policy encouraging mental health providers to include family members when caring for veterans (Veterans Health Administration, 2019). The policy generally focused on spouses and caregivers, however, our findings illustrate the importance of potentially targeting parenting self-efficacy for veterans struggling with post-deployment mental health concerns who also have children. Interventions that incorporate both the veteran and their partner [e.g., cognitive-behavioral conjoint therapy for PTSD (CBCT for PTSD), Structured Approach Therapy) or children (e.g., After Deployment, Adaptive Parenting Tools; ADAPT program, Families Overcoming Under Stress; FOCUS] into treatment are an area of active research (Brown-Bowers et al., 2012; Sautter et al. 2014, Gewirtz et al., 2016, Lester et al., 2011). Our results support the importance of these efforts for men and women veterans and suggest gender-specific assessments and intervention for parenting concerns may be of particular value.
Clinical Impact Statement:
The impacts of post-deployment mental health concerns on relationship quality are generally similar among men and women veterans. Associations of post-deployment mental health concerns with parenting may be more problematic for women veterans vs. men, suggesting a potential need for gender-based assessment and intervention for these concerns.
Acknowledgments:
The views expressed in this paper are those of the authors and do not necessarily reflect those of the Veterans Health Administration or the United States government.
This research was supported by the National Center for PTSD, Office of Mental Health Services, Department of Veterans Affairs.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
CRediT:
RLZ: Conceptualization, methodology, supervision, writing (original draft, reviewing/editing)
EAA: Conceptualization, methodology, writing (original draft, reviewing/editing)
JLG: Conceptualization, methodology, funding acquisition, investigation, supervision, project administration, writing (review & editing)
AES: Conceptualization, methodology, funding acquisition, investigation, project administration, supervision, writing (review & editing)
References
- Bakhurst M, McGuire A, & Halford WK (2018). Trauma Symptoms, Communication, and Relationship Satisfaction in Military Couples. Family Process, 57(1), 241–252. 10.1111/famp.12285 [DOI] [PubMed] [Google Scholar]
- Berz JB, Taft CT, Watkins LE, & Monson CM (2008). Associations Between PTSD Symptoms and Parenting Satisfaction in a Female Veteran Sample. Journal of Psychological Trauma, 7(1), 37–45. 10.1080/19322880802125969 [DOI] [Google Scholar]
- Blow AJ, Gorman L, Ganoczy D, Kees M, Kashy DA, Valenstein M, Marcus SM, Fitzgerald HE, & Chermack S (2013). Hazardous drinking and family functioning in National Guard veterans and spouses postdeployment. Journal of Family Psychology, 27(2), 303–313. 10.1037/a0031881 [DOI] [PubMed] [Google Scholar]
- Bradley KA, Boyd-Wickizer J, Powell SH, & Burman ML (1998). Alcohol screening questionnaires in women: A critical review. JAMA, 280(2), 166–171. 10.1001/jama.280.2.166 [DOI] [PubMed] [Google Scholar]
- Bui E, Zakarian RJ, Laifer LM, Sager JC, Chen Y, Cohen S, Simon NM, & Ohye B (2017). Psychometric Properties of the Parenting Sense of Competence Scale in Treatment-Seeking Post-9/11 Veterans. Journal of Child and Family Studies, 26(2), 464–470. 10.1007/s10826-016-0580-9 [DOI] [Google Scholar]
- Committee on the Well-Being of Military Families, Board on Children, Youth, and Families, Division of Behavioral and Social Sciences and Education, & National Academies of Sciences, Engineering, and Medicine. (2019). Strengthening the Military Family Readiness System for a Changing American Society (Kizer KW & Menestrel SL, Eds.; p. 25380). National Academies Press. 10.17226/25380 [DOI] [PubMed] [Google Scholar]
- Creech SK, Benzer JK, Meyer EC, DeBeer BB, Kimbrel NA, & Morissette SB (2019). Longitudinal associations in the direction and prediction of PTSD symptoms and romantic relationship impairment over one year in post 9/11 veterans: A comparison of theories and exploration of potential gender differences. Journal of Abnormal Psychology, 128(3), 245–255. 10.1037/abn0000420 [DOI] [PubMed] [Google Scholar]
- Creech SK, & Misca G (2017). Parenting with PTSD: A Review of Research on the Influence of PTSD on Parent-Child Functioning in Military and Veteran Families. Frontiers in Psychology, 8, 1101. 10.3389/fpsyg.2017.01101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creech SK, Swift R, Zlotnick C, Taft C, & Street AE (2016). Combat exposure, mental health, and relationship functioning among women veterans of the Afghanistan and Iraq wars. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 30(1), 43–51. 10.1037/fam0000145 [DOI] [PubMed] [Google Scholar]
- Dhalla S, & Kopec JA (2007). The CAGE questionnaire for alcohol misuse: A review of reliability and validity studies. Clinical and Investigative Medicine. Medecine Clinique Et Experimentale, 30(1), 33–41. 10.25011/cim.v30i1.447 [DOI] [PubMed] [Google Scholar]
- Dillman DA (2007). Mail and internet surveys: The tailored design method. Wiley. [Google Scholar]
- Foran HM, Wright KM, & Wood MD (2013). Do Combat Exposure and Post-Deployment Mental Health Influence Intent to Divorce? Journal of Social and Clinical Psychology, 32(9), 917–938. 10.1521/jscp.2013.32.9.917 [DOI] [Google Scholar]
- Gimbel C, & Booth A (1994). Why Does Military Combat Experience Adversely Affect Marital Relations? Journal of Marriage and the Family, 56(3), 691. 10.2307/352879 [DOI] [Google Scholar]
- Johnston C, & Mash EJ (1989). A Measure of Parenting Satisfaction and Efficacy. Journal of Clinical Child Psychology, 18(2), 167–175. 10.1207/s15374424jccp1802_8 [DOI] [Google Scholar]
- Laifer LM, Blackburn AM, Goetter EM, Ohye BY, Simon NM, & Bui E (2019). Potential Mediating Role of Parenting Competence in the Relationship Between Posttraumatic Stress Disorder and Family Functioning Post-9/11 Veteran Parents. Journal of Child and Family Studies, 28(7), 1843–1849. 10.1007/s10826-019-01405-9 [DOI] [Google Scholar]
- Monson CM, Taft CT, & Fredman SJ (2009). Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review, 29(8), 707–714. 10.1016/j.cpr.2009.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renshaw KD, Campbell SB, Meis L, & Erbes C (2014). Gender Differences in the Associations of PTSD Symptom Clusters With Relationship Distress in U.S. Vietnam Veterans and Their Partners: Gender Differences in PTSD and Distress. Journal of Traumatic Stress, 27(3), 283–290. 10.1002/jts.21916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riviere LA, Merrill JC, Thomas JL, Wilk JE, & Bliese PD (2012). 2003–2009 marital functioning trends among U.S. enlisted soldiers following combat deployments. Military Medicine, 177(10), 1169–1177. 10.7205/milmed-d-12-00164 [DOI] [PubMed] [Google Scholar]
- Samper RE, Taft CT, King DW, & King LA (2004). Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. Journal of Traumatic Stress, 17(4), 311–315. 10.1023/B:JOTS.0000038479.30903.ed [DOI] [PubMed] [Google Scholar]
- Simon RW (1992). Parental Role Strains, Salience of Parental Identity and Gender Differences in Psychological Distress. Journal of Health and Social Behavior, 33(1), 25. 10.2307/2136855 [DOI] [PubMed] [Google Scholar]
- Smith BN, Taverna EC, Fox AB, Schnurr PP, Matteo RA, & Vogt D (2017). The Role of PTSD, Depression, and Alcohol Misuse Symptom Severity in Linking Deployment Stressor Exposure and Post-Military Work and Family Outcomes in Male and Female Veterans. Clinical Psychological Science, 5(4), 664–682. 10.1177/2167702617705672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorokowski P, Randall AK, Groyecka A, Frackowiak T, Cantarero K, Hilpert P, Ahmadi K, Alghraibeh AM, Aryeetey R, Bertoni A, Bettache K, Błażejewska M, Bodenmann G, Bortolini TS, Bosc C, Butovskaya M, Castro FN, Cetinkaya H, Cunha D, … Sorokowska A (2017). Marital Satisfaction, Sex, Age, Marriage Duration, Religion, Number of Children, Economic Status, Education, and Collectivistic Values: Data from 33 Countries. Frontiers in Psychology, 8, 1199. 10.3389/fpsyg.2017.01199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB (1976). Measuring Dyadic Adjustment: New Scales for Assessing the Quality of Marriage and Similar Dyads. Journal of Marriage and the Family, 38(1), 15. 10.2307/350547 [DOI] [Google Scholar]
- Street AE, Gradus JL, Giasson HL, Vogt D, & Resick PA (2013). Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. Journal of General Internal Medicine, 28 Suppl 2, S556–562. 10.1007/s11606-013-2333-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street AE, Vogt D, & Dutra L (2009). A new generation of women veterans: Stressors faced by women deployed to Iraq and Afghanistan. Clinical Psychology Review, 29(8), 685–694. 10.1016/j.cpr.2009.08.007 [DOI] [PubMed] [Google Scholar]
- Taft CT, Schumm JA, Panuzio J, & Proctor SP (2008). An examination of family adjustment among Operation Desert Storm veterans. Journal of Consulting and Clinical Psychology, 76(4), 648–656. 10.1037/a0012576 [DOI] [PubMed] [Google Scholar]
- Vogt D, Smith BN, Fox AB, Amoroso T, Taverna E, & Schnurr PP (2017). Consequences of PTSD for the work and family quality of life of female and male U.S. Afghanistan and Iraq War veterans. Social Psychiatry and Psychiatric Epidemiology, 52(3), 341–352. 10.1007/s00127-016-1321-5 [DOI] [PubMed] [Google Scholar]
- Vogt D, Taverna EC, Nillni YI, Booth B, Perkins DF, Copeland LA, Finley EP, Tyrell FA, & Gilman CL (2019). Development and Validation of a Tool to Assess Military Veterans’ Status, Functioning, and Satisfaction with Key Aspects of their Lives. Applied Psychology: Health and Well-Being, 11(2), 328–349. 10.1111/aphw.12161 [DOI] [PubMed] [Google Scholar]
- Wasserstein RL, & Lazar NA (2016). The ASA Statement on p -Values: Context, Process, and Purpose. The American Statistician, 70(2), 129–133. 10.1080/00031305.2016.1154108 [DOI] [Google Scholar]
- Weathers FW, Huska JA, & Keane TM (1991). PCL·M for DSM·IV. Boston; National Center for PTSD - Behavioral Science Division, 1991. [Google Scholar]
- Yablonsky AM, Yan G, & Bullock L (2016). Parenting Stress After Deployment in Navy Active Duty Fathers. Military Medicine, 181(8), 854–862. 10.7205/MILMED-D-15-00302 [DOI] [PubMed] [Google Scholar]
- Zalta AK, Bui E, Karnik NS, Held P, Laifer LM, Sager JC, Zou D, Rauch PK, Simon NM, Pollack MH, & Ohye B (2018). Examining the Relationship Between Parent and Child Psychopathology in Treatment-Seeking Veterans. Child Psychiatry and Human Development, 49(2), 209–216. 10.1007/s10578-017-0743-y [DOI] [PMC free article] [PubMed] [Google Scholar]


