Abstract
Background
Chronic venous insufficiency (CVI) is a condition related to chronic venous disease that may progress to venous leg ulceration and impair quality of life of those affected. Treatments such as physical exercise may be useful to reduce CVI symptoms. This is an update of an earlier Cochrane Review.
Objectives
To evaluate the benefits and harms of physical exercise programmes for the treatment of individuals with non‐ulcerated CVI.
Search methods
The Cochrane Vascular Information Specialist searched the Cochrane Vascular Specialised Register, CENTRAL, MEDLINE, Embase, and CINAHL databases and World Health Organization International Clinical Trials Registry Platform and ClinicalTrials.gov trials registers to 28 March 2022.
Selection criteria
We included randomised controlled trials (RCTs) comparing exercise programmes with no exercise in people with non‐ulcerated CVI.
Data collection and analysis
We used standard Cochrane methods. Our primary outcomes were intensity of disease signs and symptoms, ejection fraction, venous refilling time, and incidence of venous leg ulcer. Our secondary outcomes were quality of life, exercise capacity, muscle strength, incidence of surgical intervention, and ankle joint mobility. We used GRADE to assess the certainty of the evidence for each outcome.
Main results
We included five RCTs involving 146 participants. The studies compared a physical exercise group with a control group that did not perform a structured exercise programme. The exercise protocols differed between studies. We assessed three studies to be at an overall unclear risk of bias, one study at overall high risk of bias, and one study at overall low risk of bias. We were not able to combine data in meta‐analysis as studies did not report all outcomes, and different methods were used to measure and report outcomes.
Two studies reported intensity of CVI disease signs and symptoms using a validated scale. There was no clear difference in signs and symptoms between groups in baseline to six months after treatment (Venous Clinical Severity Score mean difference (MD) −0.38, 95% confidence interval (CI) −3.02 to 2.26; 28 participants, 1 study; very low‐certainty evidence), and we are uncertain if exercise alters the intensity of signs and symptoms eight weeks after treatment (MD −4.07, 95% CI −6.53 to −1.61; 21 participants, 1 study; very low‐certainty evidence).
There was no clear difference in ejection fraction between groups from baseline to six months follow‐up (MD 4.88, 95% CI −1.82 to 11.58; 28 participants, 1 study; very low‐certainty evidence).
Three studies reported on venous refilling time. We are uncertain if there is an improvement in venous refilling time between groups for baseline to six‐month changes (MD 10.70 seconds, 95% CI 8.86 to 12.54; 23 participants, 1 study; very low‐certainty evidence) or baseline to eight‐week change (MD 9.15 seconds, 95% CI 5.53 to 12.77 for right side; MD 7.25 seconds, 95% CI 5.23 to 9.27 for left side; 21 participants, 1 study; very low‐certainty evidence). There was no clear difference in venous refilling index for baseline to six‐month changes (MD 0.57 mL/min, 95% CI −0.96 to 2.10; 28 participants, 1 study; very low‐certainty evidence).
No included studies reported the incidence of venous leg ulcers.
One study reported health‐related quality of life using validated instruments (Venous Insufficiency Epidemiological and Economic Study (VEINES) and 36‐item Short Form Health Survey (SF‐36), physical component score (PCS) and mental component score (MCS)). We are uncertain if exercise alters baseline to six‐month changes in health‐related quality of life between groups (VEINES‐QOL: MD 4.60, 95% CI 0.78 to 8.42; SF‐36 PCS: MD 5.40, 95% CI 0.63 to 10.17; SF‐36 MCS: MD 0.40, 95% CI −3.85 to 4.65; 40 participants, 1 study; all very low‐certainty evidence). Another study used the Chronic Venous Disease Quality of Life Questionnaire (CIVIQ‐20), and we are uncertain if exercise alters baseline to eight‐week changes in health‐related quality of life between groups (MD 39.36, 95% CI 30.18 to 48.54; 21 participants, 1 study; very low‐certainty evidence). One study reported no differences between groups without presenting data.
There was no clear difference between groups in exercise capacity measured as time on treadmill (baseline to six‐month changes) (MD −0.53 minutes, 95% CI −5.25 to 4.19; 35 participants, 1 study; very low‐certainty evidence). We are uncertain if exercise improves exercise capacity as assessed by the 6‐minute walking test (MD 77.74 metres, 95% CI 58.93 to 96.55; 21 participants, 1 study; very low‐certainty evidence).
Muscle strength was measured using dynamometry or using heel lifts counts. We are uncertain if exercise increases peak torque/body weight (120 revolutions per minute) (changes from baseline to six months MD 3.10 ft‐lb, 95% CI 0.98 to 5.22; 29 participants, 1 study; very low‐certainty evidence). There was no clear difference between groups in baseline to eight‐week change in strength measured by a hand dynamometer (MD 12.24 lb, 95% CI −7.61 to 32.09 for the right side; MD 11.25, 95% CI −14.10 to 36.60 for the left side; 21 participants, 1 study; very low‐certainty evidence). We are uncertain if there is an increase in heel lifts (n) (baseline to six‐month changes) between groups (MD 7.70, 95% CI 0.94 to 14.46; 39 participants, 1 study; very low‐certainty evidence).
There was no clear difference between groups in ankle mobility measured during dynamometry (baseline to six‐month change MD −1.40 degrees, 95% CI −4.77 to 1.97; 29 participants, 1 study; very low‐certainty evidence). We are uncertain if exercise increases plantar flexion measured by a goniometer (baseline to eight‐week change MD 12.13 degrees, 95% CI 8.28 to 15.98 for right leg; MD 10.95 degrees, 95% CI 7.93 to 13.97 for left leg; 21 participants, 1 study; very low‐certainty evidence). In all cases, we downgraded the certainty of evidence due to risk of bias and imprecision.
Authors' conclusions
There is currently insufficient evidence to assess the benefits and harms of physical exercise in people with chronic venous disease. Future research into the effect of physical exercise should consider types of exercise protocols (intensity, frequency, and time), sample size, blinding, and homogeneity according to the severity of disease.
Keywords: Humans, Body Weight, Evidence Gaps, Exercise, Veins, Venous Insufficiency, Venous Insufficiency/therapy
Plain language summary
Can physical exercise improve blood flow in people with chronic venous insufficiency?
Key message
There is not enough evidence available to help us decide if physical exercise benefits people with chronic venous disease.
Why is this question important?
Veins are a type of blood vessel that carry blood from the body back to the heart ('venous blood return'). The process is aided by contractions of a series of muscle pumps within the legs. Problems with the veins or muscle pumps in the legs in some people can impair this process, resulting in a condition known as chronic venous insufficiency (CVI). CVI may cause pain, oedema (swelling due to fluid retention), and leg ulcers, and can impact a person's quality of life. It is thought that treatments such as physical exercise that increase the movement of the ankle joint and strengthen the muscle pump in the calf of the leg may help prevent the disease from getting worse.
What did we do?
We searched for randomised controlled trials that compared the effects of following exercise programmes with no exercise in people with CVI. In randomised controlled trials, the treatments people receive are decided at random, and these give the most reliable evidence about treatment effects.
What did we find?
We found five studies involving a total of 146 people with CVI that directly compared the effects of physical exercise with controls that did not include a structured physical exercise programme. The studies looked at possible changes in signs and symptoms of CVI; blood flow (measured by ejection fraction (the amount of blood the heart pumps each time it beats) and venous refilling index); quality of life; exercise capacity; muscle strength; and ankle joint mobility. Not all the studies reported on all of these outcomes, and the outcomes were measured in different ways. Most results came from small, single studies. None of the studies reported on new cases of venous leg ulcers or if surgical treatment was needed to relieve symptoms.
How certain are we about the evidence?
Although some studies reported improvements in some outcomes after an eight‐week period and a six‐month period in the exercise group compared to the control group, we are uncertain if these equal real differences due to concerns about how the studies were designed and because the results were from small, single studies.
How up‐to‐date is the evidence?
The evidence is current to 28 March 2022.
Summary of findings
Summary of findings 1. Physical exercise compared with no treatment for non‐ulcerated chronic venous insufficiency.
| Physical exercise compared with no treatment for non‐ulcerated chronic venous insufficiency | ||||||
| Population: people with non‐ulcerated chronic venous insufficiency Setting: hospitals, outpatient clinics, and home‐based (Europe, Asia, and North America) Intervention: physical exercise Comparison: no exercise | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no exercise | Risk with physical exercise | |||||
|
Intensity of disease signs and symptoms: VCSS Scale: 0 to 30 (lower is better) Follow‐up: baseline to 8‐week and 6‐month change |
We were not able to pool data as studies reported using different follow‐up periods. 1 study reported no clear difference in VCSS between the exercise and no exercise groups by 6 months (MD −0.38, 95% CI −3.02 to 2.26). 1 study reported lower VCSS in the exercise group at 8 weeks (MD −4.07, 95% CI −6.53 to −1.61). |
49 (2 RCTs) | ⊕⊝⊝⊝ Very low1, 2 | We are uncertain whether physical exercise alters the intensity of disease sign and symptoms in non‐ulcerated CVI. | ||
|
Ejection fraction assessed with plethysmography Scale: 0% to 100% (higher is better) Follow‐up: baseline to 6‐month change |
The MD in ejection fraction without physical exercise was −1.4%. |
The MD in ejection fraction with physical exercise was 3.48%. | MD 4.88% higher (1.82 lower to 11.58 higher) | 28 (1 RCT) | ⊕⊝⊝⊝ Very low1, 2 | There is no clear effect of physical exercise on ejection fraction in non‐ulcerated CVI. |
|
Venous refilling time assessed with plethysmography (higher is better) Follow‐up: baseline to 8‐week or 6‐month change |
We were not able to pool data as studies reported using very different time points, and in 1 study the MD was estimated using mean and SD reported at baseline and at follow‐up. 1 study reported higher venous filling time (baseline to 6‐month changes) in the exercise group (MD 10.70 seconds, 95% CI 8.86 to 12.54). 1 study reported an increase in venous refilling time (baseline to 8‐week changes) between the exercise and no exercise groups (MD 9.15 seconds, 95% CI 5.53 to 12.77 for the right side; MD 7.25 seconds, 95% CI 5.23 to 9.27 for the left side). 1 study reported no clear difference in venous refilling index (baseline to 6‐month changes) between the exercise and no exercise groups (MD 0.57 mL/min, 95% CI −0.96 to 2.10). |
72 (3 RCTs) | ⊕⊝⊝⊝ Very low1, 3 | We are uncertain whether physical exercise alters venous refilling time or index in non‐ulcerated CVI. | ||
| Incidence of venous leg ulcer | ‐ | ‐ | ‐ | No studies reported this outcome. | ||
|
Quality of life VEINES‐QOL/SF‐36/CIVIQ‐20 (lower is better) Follow‐up: baseline to 8‐week and 6‐month change |
We were not able to pool data as studies reported using different measurements and different follow‐up periods. 1 study reported no differences between groups without presenting data. 1 study reported QoL using 2 tools and reported better scores assessed by VEINES‐QOL (MD 4.60, 95% CI 0.78 to 8.42) and SF‐36 PCS (MD 5.40, 95% CI 0.63 to 10.17), but no clear difference using SF‐36 MCS (MD 0.40, 95% CI −3.85 to 4.65). 1 study reported better scores in the exercise group using CIVIQ‐20 (MD 39.36, 95% CI 30.18 to 48.54). |
61 (2 RCTs) | ⊕⊝⊝⊝ Very low1, 3 | We are uncertain whether exercise alters health‐related QoL in non‐ulcerated CVI. | ||
|
Exercise capacity assessed by: time on treadmill (higher is better) Follow‐up: baseline to 6‐month change 6‐minute walk test (higher is better) Follow‐up: baseline to 8‐week change |
We were not able to pool data as studies reported using different measurements and follow‐up periods. 1 study reported no clear difference in exercise capacity (time on treadmill) between the exercise and no exercise groups (MD −0.53 minutes, 95% CI −5.25 to 4.19). 1 study reported higher exercise capacity (6‐minute walk test) in the exercise group (MD 77.74 metres, 95% CI 58.93 to 96.55). |
56 (2 RCTs) | ⊕⊝⊝⊝ Very low1, 2 | We are uncertain whether physical exercise alters exercise capacity in non‐ulcerated CVI. | ||
|
Muscle strength assessed by: heel lifts (higher is better) Follow‐up: baseline to 6‐month change) dynamometry (higher is better) Follow‐up: baseline to 8‐week or 6‐month change |
We were not able to pool data as studies reported using different measurements. 1 study reported a difference between groups after exercise using dynamometry (MD 3.10 ft‐lb, 95% CI 0.98 to 5.22). 1 study reported higher number of heel lift repetitions in exercise group (MD 7.70, 95% CI 0.94 to 14.46). 1 study reported no clear difference between groups using dynamometry (MD 12.24 lb, 95% CI −7.61 to 32.09 for the right side; MD 11.25, 95% CI −14.10 to 36.60 for left side). |
89 (3 RCTs) | ⊕⊝⊝⊝ Very low1, 3 | We are uncertain whether exercise improves muscle strength in non‐ulcerated CVI. | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CIVIQ‐20: Chronic Venous Disease Quality of Life Questionnaire; CVI: chronic venous insufficiency; ft‐lb: foot‐pounds; MD: mean difference; QoL: quality of life; RCT: randomised controlled trial; SD: standard deviation; SF‐36 MCS: 36‐item Short Form Health Survey mental component score; SF‐36 PCS: 36‐item Short Form Health Survey physical component score; VCSS: Venous Clinical Severity Score; VEINES‐QOL: Venous Insufficiency Epidemiological and Economic Study Quality of Life Questionnaire | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Downgraded two levels for risk of bias concerns. 2Downgraded two levels for imprecision due to small numbers of participants and resulting wide CI. 3Downgraded one level for imprecision due to small numbers of participants.
Background
Description of the condition
Chronic venous disease is defined as long‐standing morphological and functional venous abnormalities that may or may not be symptomatic. This condition can be present in a less‐severe manifestation such as telangiectasia (small dilated blood vessels) or may progress to varicose veins and even skin ulceration (Beebe‐Dimmer 2005; Staffa 2002). Chronic venous insufficiency (CVI) is often clinically defined as chronic venous disease resulting in changes in skin and subcutaneous tissue (Eklof 2004; Evans 1999), and it may be a condition following deep vein thrombosis, also known as post‐thrombotic syndrome (PTS) (Busuttil 2016). CVI is more common in the elderly than in younger individuals (De Araujo 2003; Wipke‐Tevis 2000), and is the main cause of venous ulceration (De Araujo 2003). The age‐adjusted prevalence of CVI is estimated to be around 9% in men and 7% in women (Evans 1999), and it constitutes an economic burden to public health, especially when venous ulceration is present (De Araujo 2003; Wipke‐Tevis 2000). In the Edinburgh cohort study, the overall incidence of varicose veins after a 13‐year follow‐up was 18.2%, with similar age‐adjusted incidence in men (15.2%) and women (17.4%) (Robertson 2013). Risk factors associated with CVI include family history, female gender, number of pregnancies, old age, lifestyle and occupational activities. Its development is thought to be related to sustaining an erect posture (Beebe‐Dimmer 2005; Staffa 2002).
Physical alterations related to CVI, such as oedema, hyperpigmentation, eczema, and lipodermatosclerosis, occur mainly in the lower limbs. These alterations are the consequence of valvular insufficiency or venous obstruction, resulting in long‐term venous hypertension due to venous stasis in the lower limbs and generating a pressure‐driven inflammatory status (Pocock 2014). Foot, calf, and thigh muscle pump function may be impaired in people with CVI (Meissner 2005). Because these muscles cause displacement of venous blood in vertical directions towards the heart and are therefore are the strongest power source for venous return in the lower limbs, their dysfunction is involved in the progression of the disease (Goldman 1989; Recek 2013).
The diagnosis of CVI is primarily based on clinical examination and history. The CEAP (Clinical, Etiology, Anatomy, Pathophysiology) classification is a widely accepted international classification that was developed in 1994 to assist with the reporting and diagnosing of chronic venous disease, and updated in 2020 (Table 2) (Lurie 2020). Additional specific tests, such as venous duplex imaging, plethysmography, phlebography, and the ankle‐brachial index (ABI) test, can be used to make differential diagnoses (Collins 2010; Eberhardt 2014). Common symptoms are pain, ache, heaviness and discomfort in the lower limbs, which have a marked impact on quality of life (QoL) of those affected, alongside other symptoms such as throbbing, tightness, fatigue, swelling, cramps, itching, restless legs, and tingling sensation (Perrin 2016).
1. CEAP classification of chronic venous disease .
| The CEAP (Clinical‐Etiology‐Anatomy‐Pathophysiology) classification (Lurie 2020) | |
| Classification | Description/definition |
| Clinical | |
| 0 | No visible or palpable signs of venous disease |
| 1 | Telangiectases or reticular veins |
| 2 | Varicose veins |
| 2r | Recurrent varicose veins |
| 3 | Oedema |
| 4 | Changes in skin and subcutaneous tissue secondary to chronic venous disease |
| 4a | Pigmentation or eczema |
| 4b | Lipodermatosclerosis or atrophie blanche |
| 4c | Corona phlebectatica |
| 5 | Healed venous ulcer |
| 6 | Active venous ulcer |
| 6r | Recurrent active venous ulcer |
| S | Symptomatic, including ache, pain, tightness, skin irritation, heaviness, muscle cramp, and other complaints attributable to venous dysfunction |
| A | Asymptomatic |
| Etiology | |
| Ec | Congenital (present since birth) |
| Ep | Primary |
| Es | Secondary (post‐thrombotic, traumatic) |
| Es | Secondary (intravenous) |
| Ese | Secondary (extravenous) |
| En | No cause identified. |
| Anatomy distribution | |
| As | Superficial (great and short saphenous veins) |
| Ap | Perforator (thigh and calf perforating veins) |
| Ad | Deep (cava, iliac, pelvic, femoral, popliteal, peroneal, tibial, muscular, gastrocnemius and soleal veins) |
| An | No venous location identified. |
| Pathophysiology | |
| Pr | Reflux (axial and perforating veins) |
| Po | Obstruction (acute and chronic) |
| Pr,o | Combination of both reflux and obstruction (valvular dysfunction and thrombus) |
| Pn | No venous pathophysiology identified. |
Description of the intervention
Exercise modalities have been prescribed for the treatment of individuals with peripheral vascular disease (PVD) of different aetiologies. Data also support the use of exercise for the treatment of individuals with peripheral arterial disease (PAD) (Rooke 2011). However, the prescription of exercise for people with CVI is not well established (Davies 2008). Overall, physical activity has been associated with a marked decrease in cardiovascular mortality and all‐cause mortality (Nocon 2008). Prescribed exercise has been recommended for the primary prevention of cardiovascular disease, and its effects include, but are not limited to, glycaemic control; an increase in high‐density lipoprotein (HDL) cholesterol; a reduction in blood pressure; weight loss; a reduction in depression, anxiety, and psychological stress; and increases in cardiorespiratory fitness and muscle strength (Metkus 2010). In the clinical setting, exercises to increase ankle joint mobility or the flexibility and strength of the calf muscles have been recommended in individuals with CVI, with the aim of improving muscle pump function and, therefore, haemodynamics (Kan 2001; Yang 1999).
How the intervention might work
Studies have shown that the application of a physical exercise programme may have a number of benefits, including: reducing oedema of the lower limbs; improving the haemodynamic performance of the calf muscle through the strengthening of these muscles; improving ankle range of motion; and improving cardiorespiratory fitness, which in turn improves functional capacity and QoL (Orr 2017; Padberg 2004; Quilici 2009). Exercise programmes usually consist of the stretching and strengthening of lower limb muscles together with aerobic exercises that aim to improve venous return, such as walking. Even very small movements of the lower limbs may promote the important pumping action of the venous blood (Bergan 2006). Researchers suggest that treatments which aim to increase the movement of the ankle joint, with consequent strengthening of the calf muscle pump, improve the calf muscle pump function through an increase in the ejection fraction and a decrease in the residual fraction in the early stages of CVI; this may be useful in the prevention of disease progression and its consequences (Yang 1999).
Why it is important to do this review
CVI is a highly prevalent PVD. The disease can cause several symptoms (Perrin 2016), and may progress to a phase where subcutaneous alterations become evident and develop into a venous leg ulcer, which is a chronic hard‐to‐heal wound. Interventions that can improve the disease or reduce its progress are desirable. Therapeutic exercise, especially when prescribed in association with therapeutic compression, is usually indicated for individuals with CVI. There are studies investigating the effects of exercise on individuals with venous leg ulcers (Jull 2018; Orr 2017; Smith 2018); however, the outcomes are generally only ulcer‐related, such as wound area, recurrence, and time to heal. No available up‐to‐date systematic review has assessed the effects of exercise related to the outcomes of non‐ulcerated CVI. Furthermore, although CVI is highly prevalent in the elderly, the effects and safety of exercise prescription on CVI have not been systematically reviewed in this population (Brand 1988; Heit 2001; Robertson 2013). If effective, physical exercise may be considered a low‐cost treatment regimen that can be adopted by healthcare providers for the treatment of people with CVI and the prevention of disease progression. We have not assessed the effects of exercise on chronic venous leg ulcer healing in this review. This update will help to determine the safety and effectiveness of exercise in the treatment of individuals with non‐ulcerated CVI.
Objectives
To evaluate the benefits and harms of physical exercise programmes for the treatment of individuals with non‐ulcerated CVI.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) in which an exercise programme was used as the main or adjunctive treatment in individuals with non‐ulcerated chronic venous insufficiency (CVI).
Types of participants
We included RCTs involving individuals with non‐ulcerated CVI regardless of sex and ethnicity.
We used the CVI diagnosis as given by trial authors because the classification of CVI could differ between studies; some may have included individuals with a CEAP C score of 3 to 5, and others may have included individuals with less severe clinical manifestation, as designated by a CEAP C score of 2, and defined them as having CVI.
We included studies conducted in both non‐ulcerated and ulcerated CVI participants provided the outcomes for these two groups were reported separately. This is because the major outcomes for individuals with leg ulcers (e.g. percentage reduction in ulcer area or percentage of fully healed ulcers) differ from those in people with non‐ulcerated CVI, and it would be difficult to assess them within the same review. However, if data for the two groups were not analysed and presented separately, and the exercise treatment was carried out in some individuals with CVI and leg ulcers, we included the study if these participants constituted less than 25% of the total number of study participants.
We did not assess the effects of exercise on venous leg ulcer healing in this review.
We excluded studies in which the exercise treatment was investigated in individuals with PAD, unless the results were reported separately for the CVI subgroup.
Types of interventions
We compared supervised or unsupervised prescribed exercise programmes as the main or adjunctive treatment in individuals with non‐ulcerated CVI with either the same protocol without exercise or without treatment. We considered for inclusion studies using compression stockings in the exercise or control group. We excluded studies involving balneotherapy, as it would be difficult to determine if effects were due to the water pressure or to the exercise undertaken as part of this therapy. The effects of balneotherapy are investigated in another Cochrane Review (de Moraes Silva 2019).
Types of outcome measures
Primary outcomes
Intensity of disease signs and symptoms, measured using a validated instrument such as the Venous Clinical Severity Score (see Table 3) (Rutherford 2000; Vasquez 2010)
Ejection fraction, measured using air plethysmography or duplex ultrasonography
Venous refilling time, measured using plethysmography
Incidence of venous leg ulcer
2. Venous Clinical Severity Score.
| Clinical descriptor | Absent (0) | Mild (1) | Moderate (2) | Severe (3) |
| Pain | None | Occasional | Daily not limiting | Daily limiting |
| Varicose veins | None | Few | Calf or thigh | Calf and thigh |
| Venous oedema | None | Foot and ankle | Below knee | Knee and above |
| Skin pigmentation | None | Limited perimalleolar | Diffuse lower 1/3 calf | Wider above lower 1/3 calf |
| Inflammation | None | Limited perimalleolar | Diffuse lower 1/3 calf | Wider above lower 1/3 calf |
| Induration | None | Limited perimalleolar | Diffuse lower 1/3 calf | Wider above lower 1/3 calf |
| Number of active ulcers | None | 1 | 2 | 3 or more |
| Ulcer duration | None | < 3 months | 3 to 12 months | > 1 year |
| Active ulcer size | None | < 2 cm | 2 to 6 cm | > 6 cm |
| Compression therapy | None | Intermittent | Most days | Fully comply |
Secondary outcomes
QoL, measured using validated instruments (such as the Venous Insufficiency Epidemiological and Economic Study QoL and Symptoms (VEINES‐QOL/Sym) or the 36‐item Short Form Health Survey (SF‐36) questionnaires)
Exercise capacity, measured using an objective test, such as the 6‐minute walk test or the maximum distance walked on a treadmill
Muscle strength, measured using dynamometry
Incidence of the use of surgical intervention to treat symptoms related to CVI
Ankle joint mobility
Search methods for identification of studies
Electronic searches
The Cochrane Vascular Information Specialist conducted systematic searches of the following databases for RCTs and controlled clinical trials without language, publication year, or publication status restrictions:
Cochrane Vascular Specialised Register via the Cochrane Register of Studies (CRS‐Web) (most recent search 28 March 2022);
Cochrane Central Register of Controlled Trials (CENTRAL; Issue 2, 2022) via the Cochrane Register of Studies Online (CRSO) (most recent search 28 March 2022);
MEDLINE (Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE) (1946 to 28 March 2022);
Embase Ovid (1974 to 28 March 2022);
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature) (most recent search 28 March 2022);
AMED (Allied and Complementary Medicine Database) (1985 to 28 March 2022).
We developed search strategies for other databases from the search strategy designed for MEDLINE. Where appropriate, search strategies were combined with adaptations of the Highly Sensitive Search Strategy designed by Cochrane for identifying RCTs and controlled clinical trials, as described in Chapter 4 of the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2022). Search strategies for major databases are provided in Appendix 1.
We searched the following trials registries:
World Health Organization International Clinical Trials Registry Platform (trialsearch.who.int/);
ClinicalTrials.gov (clinicaltrials.gov).
The most recent searches were carried out on 28 March 2022.
Searching other resources
We searched the bibliographies of relevant publications identified through the above searches for further studies. We attempted to contact trial authors to obtain unpublished data and information as required. We imposed no restrictions on language or publication status for studies eligible for inclusion in the review.
Data collection and analysis
Selection of studies
Two review authors (DA and FD) independently screened the titles and abstracts of the studies identified by the search strategy against the inclusion criteria. We obtained the full texts of articles that appeared to fulfil the inclusion criteria for further assessment. We intended to resolve any discrepancies by discussion with a third review author (GF), but this was not necessary. We recorded all reasons for study exclusion. We have presented our study selection process as a PRISMA flow diagram (see Results of the search) (Liberati 2009).
Data extraction and management
Two review authors (DA and FD), working independently, extracted data and summarised details of the eligible studies using Covidence (Covidence), and entered data into Review Manager Web (RevMan Web 2022). The two review authors then compared the data extractions and agreed on a final version after discussion. We intended to resolve any discrepancies by consulting a third review author (GF), but this was not necessary. If data were missing from reports, we attempted to contact the trial authors to obtain the missing information. According to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2022), we extracted the following information, where reported:
country of origin;
study authors and year of publication;
publication type;
study design;
care setting;
type of participants;
method of recruitment of participants;
types of outcome measures;
unit of investigation (per participant, cluster);
number of participants randomised to each trial;
eligibility criteria and key baseline participant data (gender, age, ethnicity, disease duration, prevalence of comorbidities such as diabetes and PAD);
details of the treatment regimen received by each group;
type of exercise;
details of any co‐interventions;
primary and secondary outcome(s) with definitions;
outcome data for primary and secondary outcomes (by group);
overall sample size and methods used to estimate statistical power (relates to the target number of participants to be recruited, the clinical difference to be detected, and the ability of the trial to detect this difference);
duration of treatment period;
duration of follow‐up;
number of withdrawals (by group with reasons);
statistical methods used for data analysis;
risk of bias criteria (sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting);
adverse events;
source of funding.
Assessment of risk of bias in included studies
Two review authors (DA and FD) independently assessed each included study using Cochrane's risk of bias tool (RoB 1). This tool addresses seven specific domains, namely random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and other sources of bias (see Appendix 2 for details of the criteria on which we based our judgements). We assessed blinding and completeness of outcome data for each outcome separately. We intended to search the protocols of all included RCTs in order to assess selective outcome reporting. When no protocol was identified, we made a judgement based on the congruence of information in the methods and results sections of the reports of RCTs. We completed a risk of bias table for each eligible study and classified each study as being at low, high, or unclear risk of bias, according to the methods described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We presented our assessment using a risk of bias summary figure, which shows all of our judgements in a cross‐tabulation of study by entry. This display of internal validity indicates the weight the reader may give the results of each study.
We judged trials to have an overall high risk of bias if they were rated as high for any one of three key criteria (randomisation sequence, allocation concealment, and blinded outcome assessment). We classified RCTs as having an overall unclear risk of bias if any one of the three key domains was rated as unclear. We judged RCTs to be at an overall low risk of bias if all three key domains were rated as low risk.
Measures of treatment effect
We performed data analysis according to Cochrane guidelines. Two review authors (DA and FD) selected studies, extracted data, and assessed risk of bias of the included studies using Covidence (Covidence). We then analysed data using Review Manager Web (RevMan Web 2022). We presented a narrative overview of all included RCTs, with results grouped according to the comparator intervention. We presented the outcome results for each trial with 95% confidence intervals (CIs). We reported estimates for continuous outcomes (such as ejection fraction and venous refilling time) as mean differences (MDs) and overall effect size (with 95% CIs). We planned to report dichotomous outcomes (such as ulcer incidence) as risk ratios (RRs) with associated 95% CIs.
Unit of analysis issues
We treated the individual participants as the unit of analysis in this review. When data were reported using the number of limbs instead of individual participants, we attempted to carry out the appropriate adjustments for data analysis. We planned to include cluster‐randomised trials in the analysis. Had we identified any cluster‐randomised trials, we would have adjusted the results when the unit of analysis in the trial was presented as the total number of individual participants instead of the number of clusters. We intended to adjust the results using the mean cluster size and intracluster correlation coefficient (Deeks 2022); however, we included no cluster‐randomised trials in the review. For meta‐analysis, we planned to pool data from individually randomised trials using the generic inverse‐variance method, as described in Chapter 10 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2022). We were not able to undertake meta‐analysis for any outcome.
Dealing with missing data
Where possible, we contacted the original investigators to request any missing data. No additional data were provided by study authors. If a trial did not specify participant group numbers prior to dropout, we presented only complete‐case analyses for primary and secondary outcomes.
Assessment of heterogeneity
If in future updates we are able to include a sufficient number of studies, we will pool data for meta‐analysis using Review Manager Web (RevMan Web 2022). We will consider clinical heterogeneity (that is the degree to which trials appear similar in terms of type of participants, type and duration of intervention, and type of outcome) and statistical heterogeneity. We will supplement this assessment of clinical and methodological heterogeneity with information regarding statistical heterogeneity, which we will evaluate using the Chi² test (considering a significance level of P < 0.10 to indicate significant heterogeneity) in conjunction with the I² statistic (Higgins 2003). The I² statistic examines the percentage of total variation across trials due to heterogeneity rather than variation due to chance (Higgins 2003). We will categorise heterogeneity as follows: I² ≤ 40% will indicate a low level of heterogeneity, and I² ≥ 75% will represent considerable heterogeneity (Deeks 2022).
Assessment of reporting biases
If in future updates we are able to include a sufficient number of studies (10 RCTs or more), we will attempt to assess publication bias using funnel plots as described in the Cochrane Handbook for Systematic Reviews of Interventions (Page 2022). If asymmetry is present, we will explore possible causes, including publication bias, poor methodological quality, and true heterogeneity.
Data synthesis
We included insufficient studies to pool data for meta‐analysis, and therefore have presented a narrative overview of the included RCTs. For future updates, we plan to present a narrative overview of the combined studies with a meta‐analysis of outcome data using Review Manager Web where appropriate (RevMan Web 2022). Our decision to include studies in a meta‐analysis will depend on the availability of treatment effect data and an assessment of heterogeneity. For comparisons where there is no apparent clinical heterogeneity and the I² value is ≤ 40%, we will apply a fixed‐effect model. Where there is no apparent clinical heterogeneity and the I² value is > 40%, we will apply a random‐effects model. However, we will not pool data where heterogeneity is considerable (I² ≥ 75%).
Subgroup analysis and investigation of heterogeneity
If in future updates we are able to include sufficient data (10 RCTs or more) and we identify substantial heterogeneity (i.e. I² > 50%), we will conduct subgroup analyses. We plan to carry out subgroup analyses according to differences in the following variables: studies that report the treatment in the presence or absence of compression therapy independent of type (elastic or non‐elastic) or level (moderate or high pressure) of compression.
Sensitivity analysis
We assessed three studies as at overall unclear risk of bias (Aydin 2022; Klonizakis 2009; Padberg 2004); one study as at overall high risk of bias (Hartmann 1997); and one study as at overall low risk of bias (Kahn 2011), therefore sensitivity analysis was not possible. However, if in future updates we are able to include a sufficient number of studies, we will undertake sensitivity analyses on studies with low overall risk of bias.
Summary of findings and assessment of the certainty of the evidence
We presented the main results of the review in a summary of findings table (Table 1). We presented our findings for the following outcomes: intensity of disease signs and symptoms, ejection fraction, venous filling time, incidence of leg ulcer, quality of life, exercise capacity, and muscle strength (see Types of outcome measures). Three review authors (DA, FD, CR) graded the certainty of the evidence for each outcome as one of four levels: high, moderate, low, or very low (Schünemann 2022a). The summary of findings table includes the overall grading of the evidence related to each of the main outcomes using the GRADE approach as described in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2022b), and employing GRADEpro GDT software (GRADEpro GDT). We based our judgements on the following factors:
limitations in the design and implementation of available studies suggesting a high likelihood of bias;
indirectness of evidence (indirect population, intervention, control, outcomes);
unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
imprecision of results (wide CIs and small total numbers of events and/or participants);
high probability of publication bias.
Results
Description of studies
Results of the search
For this update, our database searches identified a total of 1084 records. We identified seven additional reports by checking the reference lists of included trials. We assessed 28 records for eligibility by full text. We included three new studies (Aydin 2022; Kahn 2011; Klonizakis 2009), and excluded 14 new studies, with the reasons for exclusion provided (Carpentier 2009; CTRI/2018/10/015895; Hasan 2020; Kesterton 2019; Mancini 2003; Mutlak 2019; NCT02689557; NCT03562546; NCT04148950; O'Brien 2018; Ravikumar 2017; RBR‐9bhbrp; Sharifi 2020; Tew 2015). We assessed one registered clinical trial as an ongoing study since no publications were found (NCT02148029). We assessed three new studies as awaiting classification (Dogru‐Huzmeli 2020; Karakelle 2021; Volpe 2020). See Figure 1.
1.
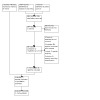
Study flow diagram.
Included studies
For further details, see Characteristics of included studies.
We included five studies with a total of 146 participants (Aydin 2022; Hartmann 1997; Kahn 2011; Klonizakis 2009; Padberg 2004), of which two were included in the first version of the review (Hartmann 1997; Padberg 2004), and three were newly included in the current update (Aydin 2022; Kahn 2011; Klonizakis 2009). Klonizakis 2009 was previously excluded because the study outcomes did not match the ones specified in our protocol. For this update, we reassessed this study as eligible for inclusion in the review as recommended by Cochrane methodology (Lefebvre 2022).
Study design and settings
All studies used a parallel‐group design; four were single‐centre RCTs (Aydin 2022; Hartmann 1997; Klonizakis 2009; Padberg 2004), and one was a multicentre RCT (Kahn 2011). Care settings were hospitals, Aydin 2022; Kahn 2011; Klonizakis 2009, or outpatient clinics and home (Hartmann 1997; Padberg 2004). The studies were conducted in Canada (Kahn 2011), Germany (Hartmann 1997), the UK (Klonizakis 2009), Turkey (Aydin 2022), and the USA (Padberg 2004).
All studies described randomisation at the participant level. In Hartmann 1997, the unit of analysis was the extremities (legs). There was no accounting for non‐independence of data in the analysis, resulting in a unit of analysis issue.
Participants
A total of 146 participants were randomised, from sample sizes ranging from 16 to 43, and 145 participants were allocated into groups. Of the 115 participants from RCTs that reported sex, 33 participants were male (28.7%). The mean age (years) ranged from 47, Kahn 2011, to 70, Padberg 2004.
Padberg 2004 allocated 31 participants with CEAP 4 to 6, six of them (20%) with CEAP classification C6. Hartmann 1997 included 24 participants with manifest varicose veins in both lower extremities. Kahn 2011 included 39 participants with unilateral post‐thrombotic syndrome (PTS), without leg ulcer. Severity classification was 51.2% mild, 37.2% moderate, and 11.6% severe. Klonizakis 2009 randomised 16 participants who had recently (within 4 to 5 weeks) had venous surgery (unilateral saphenofemoral ligation and partial stripping). Aydin 2022 allocated 32 participants with non‐ulcerated CVI, from CEAP 2 (8 participants), CEAP 3 (15 participants), CEAP 4 (5 participants), and CEAP 5 (4 participants).
Interventions
The intervention protocol in Hartmann 1997 was 60 minutes of exercise twice a week compared to no exercise, for 24 weeks. First, participants completed 20 minutes in an exercise bath, then the legs were doused with cold water for 30 seconds, then 25 minutes of floor exercises. In addition, participants performed unsupervised exercises for 15 minutes once a day. The authors reported the participants wore stockings during exercise. The control group did not perform exercise, but it is unclear whether they used compression stockings.
In Padberg 2004, participants performed 12 weeks of supervised therapy followed by 12 weeks of unsupervised therapy, versus a control group that received no exercise. The exercise programme consisted of 1 hour of individualised therapy focusing on leg strengthening (calf musculature) with progressed repetitions, sets, and weights throughout the first 12 weeks, with uphill treadmill walking to further strengthen the calf. In addition, participants were taught the principles of exercise progression and were asked to continue the progression during 12 weeks of unsupervised exercise. Participants were also encouraged to walk uphill while maintaining their exercise programme during the unsupervised component of the intervention. Participants in the control group were monitored monthly to confirm the use of compression stockings, and were evaluated at baseline and again after six months. All participants received class II (30 to 40 mmHg), below‐the‐knee compression hosiery.
In Klonizakis 2009, the intervention group performed treadmill walking exercise twice a week for eight weeks, versus a control group that did not perform the exercise protocol.
Kahn 2011 allocated participants to an intervention group that performed an exercise programme that lasted 6 months and included 15 one‐on‐one sessions with an exercise trainer. Participants were provided with an individualised exercise programme that consisted of strengthening, stretching, and aerobic components. Participants were instructed to do the strengthening programme three to four times per week, the stretching programme seven times per week, and the aerobics programme for 60 to 120 minutes per week. The control group received a one‐hour educational slide presentation and were asked not to alter their usual level of physical activity. Compression stocking use was not required for the participants, but its use was monitored.
Aydin 2022 allocated 32 participants into three groups. The intervention lasted eight weeks. All groups were assigned to compression therapy. Group 1 received compression plus inspiratory muscle training; group 2 received compression associated with calf muscle training; and group 3 received compression therapy alone. We extracted and compared data from groups 2 and 3 only. The pressure of compression therapy ranged from 18 to 32 mmHg, applied by compression stockings. The inspiratory muscle training was carried out by a threshold inspiratory resistive loading training protocol for 15 minutes twice a day. The calf muscle exercise training consisted of a static stretching exercise for the dorsiflexors and plantar flexors, an isotonic resistance exercise with elastic resistance bands, heel and toe raising on both feet, ankle pumping in a sitting position, and an isotonic exercise for knee flexion. The load, sets, and repetitions increased throughout the eight weeks of training.
Outcomes
The outcomes reported in the studies were as follows.
Intensity of signs and symptoms (Aydin 2022; Padberg 2004)
Ejection fraction (Padberg 2004)
Venous refilling time or venous filling index (Aydin 2022; Hartmann 1997; Padberg 2004)
Quality of life (Aydin 2022; Kahn 2011)
Exercise capacity (Aydin 2022; Kahn 2011)
Muscle strength (Aydin 2022; Kahn 2011; Padberg 2004)
Ankle joint mobility (Aydin 2022; Padberg 2004).
Klonizakis 2009 did not report any of the outcomes of interest for this review (they reported peak cutaneous flux responses to acetylcholine and sodium nitroprusside). We attempted to contact the study authors for information on the outcomes of interest; however, no information was obtained during the review process.
Excluded studies
See Characteristics of excluded studies.
We excluded a total of 18 studies (Carpentier 2009; Carpentier 2014; CTRI/2018/10/015895; Forestier 2014; Hartmann 1991; Hasan 2020; Kesterton 2019; Klyscz 1998; Mancini 2003; Mutlak 2019; NCT02689557; NCT03562546; NCT04148950; O'Brien 2018; Ravikumar 2017; RBR‐9bhbrp; Sharifi 2020; Tew 2015).
Three studies were not RCTs (Hartmann 1991; Klyscz 1998; NCT03562546). Eight studies investigated a CVI population but with the wrong intervention (Carpentier 2009; Carpentier 2014; CTRI/2018/10/015895; Forestier 2014; Mancini 2003; NCT02689557; Ravikumar 2017; Sharifi 2020). We excluded studies investigating balneotherapy (Carpentier 2009; Carpentier 2014; Forestier 2014; Mancini 2003; Sharifi 2020). Balneotherapy is generally comprised of water massage cycles in the whirlpool, bath with massaging jets, alternating warm and cold showers on the legs, leg or ankle massage or mobilisation or walking and swimming in the pool. We considered that any effects of the intervention could have been due to the other included steps and not just to the exercise component. Five studies investigated the wrong patient populations (Hasan 2020; Kesterton 2019; Mutlak 2019; O'Brien 2018; Tew 2015). Two studies used exercise in both control and intervention groups (NCT04148950; RBR‐9bhbrp).
Ongoing studies
We assessed one study as ongoing (NCT02148029). See Characteristics of ongoing studies.
Studies awaiting classification
See Characteristics of studies awaiting classification.
We assessed three new studies as awaiting classification (Dogru‐Huzmeli 2020; Karakelle 2021; Volpe 2020). Two of these studies are ongoing; however, one study does not specify the CEAP classification for inclusion (Dogru‐Huzmeli 2020), and the other study includes CEAP 6 participants (Volpe 2020), therefore we decided to categorise these studies as awaiting classification. We will consider these studies for inclusion if we are able to obtain data from non‐ulcerated and ulcerated participants reported separately. We will also consider Karakelle 2021 for inclusion if we are able to obtain data from non‐ulcerated and ulcerated participants separately. We assessed NCT00013273 as awaiting classification in the previous version of the review. This is registered as complete, but there is no publication history.
Risk of bias in included studies
Risk of bias is summarised in Figure 2 and Figure 3 and in the Characteristics of included studies section. We based the overall risk of bias on judgements of three key criteria (randomisation sequence, allocation concealment, and blinded outcome assessment). We assessed one included study as at overall high risk of bias because randomisation sequence and allocation concealment were at high risk of bias (Hartmann 1997). We judged three studies as at unclear risk of bias because at least one key criterion was at unclear risk of bias (Aydin 2022; Klonizakis 2009; Padberg 2004). We assessed Kahn 2011 as at overall low risk of bias because all key criteria were at low risk of bias.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Generation of the randomisation sequence
All studies were described as randomised, and four reported the method used to generate the randomisation sequence, therefore we judged these studies as being at low risk of bias (Aydin 2022; Kahn 2011; Klonizakis 2009; Padberg 2004). For generation of the randomisation sequence, Padberg 2004 used a previously prepared confidential list; Kahn 2011 used a web‐based program; Aydin 2022 used a website; and Klonizakis 2009 used a computer program. As Hartmann 1997 did not provide details on how matched pairs were generated, we assessed it as being at high risk of bias.
Concealment of the allocation process
In Padberg 2004, group assignment was revealed by the statistician only after the initial evaluation and consent, and so was judged as at low risk of bias. Kahn 2011 described the use of a web‐based program that ensured concealment of treatment allocation and was judged as at low risk of bias. Aydin 2022 described the use of envelopes for allocation concealment; however, no further details were provided regarding, for example, if envelopes were unsealed or translucent and how the content was revealed. Klonizakis 2009 did not describe the allocation concealment method. We assessed both studies as at unclear risk of bias. Hartmann 1997 formed two groups with matched pairs, but did not mention the methodology used for matching, and was therefore judged to be at high risk of allocation concealment bias.
Blinding
Kahn 2011 reported blinding of the outcome assessor, but not of personnel or groups, and was therefore judged to be at low risk of detection bias and high risk of performance bias. Aydin 2022 reported blinding of the outcome assessors, but not of personnel, and was therefore also judged to be at low risk of detection bias and high risk of performance bias. Padberg 2004 stated that all groups were unblinded, but it is unclear whether outcome assessment was blinded, therefore we rated the study as at high risk of performance bias and unclear risk of detection bias. In Hartmann 1997 and Klonizakis 2009, it is was unclear whether the groups or outcome assessment was blinded, therefore we judged both studies to be at unclear risk of bias.
Incomplete outcome data
Klonizakis 2009 reported that compliance with exercise was 100% and there were no dropouts, therefore we rated this study as at low risk of attrition bias. Aydin 2022 and Padberg 2004 properly described all dropouts and exclusion and were rated as at low risk of bias. Kahn 2011 reported attrition and exclusions; however, there was an imbalance between groups that could potentially impact the results, and a non‐accounted for difference in the number of participants provided in the CONSORT diagram and reported for two outcomes (PTS severity and QoL). For this reason we assessed Kahn 2011 as at high risk of attrition bias. We judged Hartmann 1997 to be at high risk of attrition bias because how outcomes were measured, as well as statistical variance, were not described or presented properly.
Selective reporting
We only judged Kahn 2011 to be at low risk for the domain because all outcomes presented were previously described in trial registries and were properly analysed. We judged the other four studies to be at high risk of selective reporting. Hartmann 1997 presented no results for maximum venous outflow (despite this being mentioned as having been measured). Padberg 2004 did not report data for ulcer healing and QoL, although it was stated there was no difference between groups for the latter. Klonizakis 2009 did not provide numerical data, therefore further analyses and extraction were not possible; additionally, the authors proposed to calculate the effect sizes (Cohen's d), but these data were not published. Aydin 2022 did not provide data on the control group for the outcomes "intensity of signs and symptoms" and "ankle joint mobility".
Other potential sources of bias
We judged Aydin 2022, Kahn 2011, and Klonizakis 2009 to be at low risk of bias of other potential bias. We assessed Hartmann 1997 and Padberg 2004 as at high risk of other bias. In Hartmann 1997, there was a unit of analysis issue: randomisation was performed at the participant level, and the unit of analysis was extremities (leg) and not the participant. Padberg 2004 presented no separate description of the results in participants with ulcerated CVI and non‐ulcerated CVI. The average data included 20% of ulcerated CVI. Additionally, there was an imbalance regarding physical performance during isokinetic exercise at baseline, with lower peak torque and total work in the treatment group.
Effects of interventions
See: Table 1
See Table 1 and Appendix 3.
It was not possible to undertake meta‐analysis because of clinical heterogeneity and differences in how the studies measured and reported outcomes. Not all outcomes were reported by all studies.
Primary outcomes
Intensity of disease signs and symptoms
Hartmann 1997 reported an improvement in symptoms in the exercise group compared with the control group. Change in percentage of participants reporting each symptom between baseline and week 24 (exercise versus control group) was: pain: −17% versus 56%, swelling: −9% versus 64%, restlessness: −16% versus 62%, cramps: −19% versus 67%, itching: −11% versus 52%, stasis oedema: −23% versus 59%. However, these data were obtained using a non‐validated tool, and standard deviations (SD) were not reported. The tool was a standardised questionnaire created by the authors of the study that generates a score for each symptom. This tool was neither published nor validated, therefore we did not consider it to be a reliable outcome measure.
Padberg 2004 used three tools to assess the intensity of signs and symptoms (Venous Clinical Severity Score (VCSS), Clinical Score, and Disability Score) at baseline. Only VCSS scores were compared before and after the intervention (six months follow‐up). There was no clear difference in signs and symptoms between the exercise and control groups when considering baseline to six‐month changes (mean difference (MD) −0.38, 95% confidence interval (CI) −3.02 to 2.26; 28 participants, 1 study; very low‐certainty evidence). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample size and CIs that may include both benefit and harm (Analysis 1.1).
1.1. Analysis.

Comparison 1: Intensity of signs and symptoms, Outcome 1: Venous Clinical Severity Score ‐ baseline to 6‐month changes
Aydin 2022 also used VCSS to assess symptoms before and after physical exercise for calf muscles. The study did not present within‐group score changes for the control groups, only for exercise; however, we were able to estimate the changes from baseline to eight weeks based on means and SD given at baseline and after the treatment period for the control group. We are uncertain if exercise alters the intensity of signs and symptoms when considering baseline to eight‐week changes between the exercise and control group (MD −4.07, 95% CI −6.53 to −1.61; 21 participants, 1 study; very low‐certainty evidence). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample size (Analysis 1.2). We did not combine data because we had to estimate data for the Aydin 2022 study, and due to clinical heterogeneity (different follow‐up periods).
1.2. Analysis.

Comparison 1: Intensity of signs and symptoms, Outcome 2: Venous Clinical Severity Score ‐ baseline to 8 weeks change
Kahn 2011 and Klonizakis 2009 did not investigate this outcome.
Ejection fraction
Padberg 2004 reported the mean change in ejection fraction from baseline to six‐month follow‐up. There was no clear difference in ejection fraction between the exercise and control groups (MD 4.88, 95% CI −1.82 to 11.58; 28 participants, 1 study; very low‐certainty evidence). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample size and CIs that may include both benefit and harm (see Analysis 2.1). The remaining four included studies did not investigate this outcome (Aydin 2022; Hartmann 1997; Kahn 2011; Klonizakis 2009).
2.1. Analysis.

Comparison 2: Ejection fraction, Outcome 1: Baseline to 6‐month changes
Venous refilling time
Hartmann 1997 reported an increase in half and total venous refilling time in participants in the exercise group versus the control group after six months. The study authors did not report percentage change from baseline, but we were able to calculate based on means and SD given at baseline and after six months follow‐up. It should be noted that this is the best estimate we could reach using the data provided by the authors; however, it was calculated considering that the baseline data and the six months data were independent samples. We are uncertain whether there is an improvement in venous total refilling time between exercise and control groups (baseline to six‐month changes MD 10.70 seconds, 95% CI 8.86 to 12.54; 23 participants, 1 study; very low‐certainty evidence) (Analysis 3.1). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size. Aydin 2022 reported changes from baseline to eight weeks in venous refilling time. We are uncertain whether there is an improvement in venous total refilling time between exercise and control groups (MD 9.15 seconds, 95% CI 5.53 to 12.77 for the right side; MD 7.25 seconds, 95% CI 5.23 to 9.27 for the left side; 21 participants, 1 study; very low‐certainty evidence) (Analysis 3.2). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
3.1. Analysis.

Comparison 3: Venous refilling time, Outcome 1: Total refilling time(s) ‐ baseline to 6‐month changes
3.2. Analysis.

Comparison 3: Venous refilling time, Outcome 2: Venous refilling time baseline to 8 weeks
Padberg 2004 reported venous refilling index as changes from baseline to six months follow‐up. There was no clear difference in venous refilling index between exercise and control groups (MD 0.57 mL/min, 95% CI −0.96 to 2.10; 28 participants, 1 study; very low‐certainty evidence) (Analysis 3.3). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample sizes and CIs that may include both benefit and harm.
3.3. Analysis.

Comparison 3: Venous refilling time, Outcome 3: Venous filling index ‐ baseline to 6‐month changes
Kahn 2011 and Klonizakis 2009 did not investigate this outcome.
Incidence of venous leg ulcer
No studies reported the incidence of venous leg ulcers.
Secondary outcomes
Quality of life
Padberg 2004 stated that they observed no differences between groups with regard to QoL. However, the data were not presented.
Kahn 2011 investigated health‐related QoL using the VEINES‐QOL and SF‐36 (physical component score (PCS) and mental component score (MCS)) instruments. We are uncertain whether exercise alters baseline to six‐month changes in health‐related QoL between exercise and control groups (VEINES‐QOL: MD 4.60, 95% CI 0.78 to 8.42; SF‐36 PCS: MD 5.40, 95% CI 0.63 to 10.17; SF‐36 MCS: MD 0.40, 95% CI −3.85 to 4.65; 40 participants, 1 study; very low‐certainty evidence) (Analysis 4.1; Analysis 4.2; Analysis 4.3). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
4.1. Analysis.

Comparison 4: Quality of life, Outcome 1: QoL: VEINES score ‐ baseline to 6‐month changes
4.2. Analysis.

Comparison 4: Quality of life, Outcome 2: QoL: SF‐36 PCS score ‐ baseline to 6‐month changes
4.3. Analysis.

Comparison 4: Quality of life, Outcome 3: QoL: SF‐36 MCS score ‐ baseline to 6‐month changes
Aydin 2022 assessed health‐related quality of life using the Chronic Venous Disease Quality of Life Questionnaire (CIVIQ‐20). We are uncertain whether exercise alters baseline to eight‐week changes in health‐related QoL between exercise and control groups (MD 39.36, 95% CI 30.18 to 48.54; 21 participants, 1 study; very low‐certainty evidence) (Analysis 4.4). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
4.4. Analysis.

Comparison 4: Quality of life, Outcome 4: QoL: CIVIQ‐20, Global Index Score ‐ baseline to 8‐week change
Hartmann 1997 and Klonizakis 2009 did not investigate this outcome.
Exercise capacity
Kahn 2011 reported exercise capacity represented by time on treadmill in minutes. There was no clear difference in time on treadmill (baseline to six‐month changes) between exercise and control groups (MD −0.53, 95% CI −5.25 to 4.19; 35 participants, 1 study; very low‐certainty evidence) (Analysis 5.1). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample size and CIs that may include both benefit and harm.
5.1. Analysis.

Comparison 5: Exercise capacity, Outcome 1: Time on treadmill ‐ baseline to 6‐month changes
Aydin 2022 assessed exercise capacity using the 6‐minute walk test. We are uncertain whether exercise improves exercise capacity as measured using the 6‐minute walk test (baseline to eight‐week changes) (MD 77.74 metres, 95% CI 58.93 to 96.55; 21 participants, 1 study; very low‐certainty evidence) (Analysis 5.2). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
5.2. Analysis.

Comparison 5: Exercise capacity, Outcome 2: 6‐minute walk test ‐ baseline to 8‐week change
Muscle strength
Padberg 2004 assessed muscle strength using dynamometry at two different speeds: fast (120 revolutions per minute (rpm)) and slow (60 rpm), reporting a difference between groups only in variable peak torque/body weight at fast speed. We are uncertain whether exercise increases peak torque/body weight (changes from baseline to six months, ft‐lb, 120 rpm) compared to control (MD 3.10, 95% CI 0.98 to 5.22; 29 participants, 1 study; very low‐certainty evidence) (Analysis 6.1). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
6.1. Analysis.

Comparison 6: Muscle strength, Outcome 1: Ankle dynamometry ‐ baseline to 6‐month changes
Kahn 2011 used the heel rise test (heel lifts) to investigate the strength and endurance of the triceps surae. We are uncertain whether there is an increase in heel lifts (n) between exercise and control groups for changes from baseline to six months (MD 7.70, 95% CI 0.94 to 14.46; 39 participants, 1 study; very low‐certainty evidence) (Analysis 6.2). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
6.2. Analysis.

Comparison 6: Muscle strength, Outcome 2: Heel lifts ‐ baseline to 6‐month changes
Aydin 2022 used a hand dynamometer to investigate the strength of plantar flexor muscles. The study did not present within‐group score changes for the control groups, only for exercise; however, we were able to estimate the changes from baseline to eight weeks based on means and SD given at baseline and after the treatment period for the control group. There was no clear difference in strength between exercise and control groups for changes from baseline to eight weeks (MD 12.24 lb, 95% CI −7.61 to 32.09 for the right side; MD 11.25 lb, 95% CI −14.10 to 36.60 for the left side; 21 participants, 1 study; very low‐certainty evidence) (Analysis 6.3). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample size and CIs that may include both benefit and harm.
6.3. Analysis.

Comparison 6: Muscle strength, Outcome 3: Plantar flexion dynamometry ‐ baseline to 8‐week changes
Hartmann 1997 and Klonizakis 2009 did not investigate this outcome.
Incidence of surgical intervention to treat symptoms related to CVI
No included study reported the incidence of surgical intervention.
Ankle joint mobility
Ankle joint mobility, measured using dynamometry, was assessed in one study that measured changes from baseline to six‐month follow‐up (Padberg 2004). There was no clear difference in ankle mobility (degrees) between exercise and control groups (MD −1.40, 95% CI −4.77 to 1.97; 29 participants, 1 study; very low‐certainty evidence) (Analysis 7.1). We downgraded the certainty of evidence twice due to risk of bias and twice for imprecision due to small sample size and CIs that may include both benefit and harm.
7.1. Analysis.

Comparison 7: Ankle joint mobility, Outcome 1: Maximum range of motion in dynamometry ‐ baseline to 6‐month changes
Aydin 2022 measured ankle range of motion before and after the intervention using a digital goniometer. We are uncertain whether exercise increases ankle plantar flexion (degrees) (right leg: MD 12.13, 95% CI 8.28 to 15.98; left leg: MD 10.95, 95% CI 7.93 to 13.97; 21 participants, 1 study; very low‐certainty evidence) (Analysis 7.2). We downgraded the certainty of evidence twice due to risk of bias and once for imprecision due to small sample size.
7.2. Analysis.

Comparison 7: Ankle joint mobility, Outcome 2: Maximum range of motion ‐ plantiflexion baseline to 8‐week change
Hartmann 1997, Kahn 2011, and Klonizakis 2009 did not investigate this outcome.
Discussion
Summary of main results
In this review we have reported evidence from five RCTs, involving a total of 146 participants, on the effects of physical exercise on non‐ulcerated CVI. Using GRADE, we assessed the certainty of the evidence as very low for all outcomes in all comparisons. The reasons for these judgements are outlined in Table 1. It was not possible to undertake meta‐analysis because of clinical heterogeneity and differences in how the studies measured and reported outcomes. Studies also used very different time points for follow‐up (from eight weeks up to six months).
Although individual studies reported that physical exercise may improve the intensity of signs and symptoms of CVI, increased venous refilling time, and ejection fraction compared with control groups, indicating an improvement in venous haemodynamics (Aydin 2022; Hartmann 1997; Padberg 2004), we are uncertain whether these differences represent significant findings for these outcomes as the evidence is of very low certainty. Any conclusions regarding these results should therefore be interpreted with caution given concerns related to high risk of bias and imprecision.
Results for health‐related QoL varied, with reports showing no improvements associated with physical exercise (Padberg 2004), or better scores compared with control groups; however, we are uncertain whether exercise alters health‐related QoL in non‐ulcerated CVI as the evidence is of very low certainty (Aydin 2022; Kahn 2011). Exercise capacity was measured by time on a treadmill (Kahn 2011), or using the 6‐minute walk test (Aydin 2022); however, we are uncertain whether there is a difference between groups because the certainty of evidence is very low. Reports on muscle strength showed an improvement in only one dynamometry variable in a single study (Padberg 2004), and increased heel lift repetitions in another study (Kahn 2011); however, the certainty of the evidence is very low in both cases due to risk of bias and imprecision.
Ankle joint mobility measured by dynamometer was unchanged between groups in one study (Padberg 2004), and increased in one study that assessed mobility using a digital goniometer (Aydin 2022); however, we are uncertain whether exercise increases ankle plantar flexion because of risk of bias and imprecision. None of the included studies reported on the incidence of venous leg ulcer or surgical intervention to treat symptoms related to CVI.
In summary, the evidence on the efficacy and safety of physical exercise programmes for the treatment of individuals with non‐ulcerated CVI is uncertain.
Overall completeness and applicability of evidence
As detailed in Search methods for identification of studies, we undertook a comprehensive set of literature searches to maximise the relevant studies included in this review. This review addressed the efficacy and safety of physical exercise in the treatment of individuals with non‐ulcerated CVI. Included studies compared exercise protocols to no exercise.
The included studies reported the following outcomes: intensity of signs and symptoms; ejection fraction; venous refilling time; health‐related QoL; exercise capacity; muscle strength; and ankle joint mobility. One study investigated exercise effects on cutaneous microvascular function after eight weeks of treadmill‐walking exercise twice a week (Klonizakis 2009), and reported differences in the exercise group compared to controls. However, this single study did not report any primary or secondary outcomes of interest for this review, therefore its data were not incorporated in the review. Two important outcomes (incidence of venous ulcers and incidence of surgical intervention to treat symptoms related to CVI) were not reported by any of the included studies. Another important outcome, ejection fraction, was reported by one study only. However, given the high risk of bias and imprecision in all outcomes investigated by the studies, we are not able to conclude that the available evidence supports physical exercise as an effective intervention for CVI.
All of the included studies were small, recruiting fewer than 100 participants, and the geographical scope was restricted to two countries in Europe (the UK and Germany), one in Asia (Turkey), and two in North America (the USA and Canada). Care settings were hospitals, Aydin 2022; Kahn 2011; Klonizakis 2009, or outpatient clinics and homes (Hartmann 1997; Padberg 2004). Even though the duration and intensity of the exercise protocol varied among studies, three studies presented a reasonable duration of follow‐up, corresponding to 24 weeks (Hartmann 1997; Kahn 2011; Padberg 2004).
Based on the available evidence, we are uncertain whether there is efficacy and safety of physical exercise programmes for the treatment of individuals with non‐ulcerated CVI. The results of this systematic review show a lack of RCTs of high methodological quality addressing the effectiveness of this intervention.
Quality of the evidence
We judged the overall certainty of evidence as very low according to the GRADE approach, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2022b). Using the GRADE approach, we found very low‐certainty of evidence for all outcomes. See Table 1. We downgraded the certainty of evidence due to high risk of bias and imprecision. Because of the small number of studies and small sample sizes, we were unable to verify GRADE indirectness and publication bias. We were not able to combine studies in a meta‐analysis and further explore possible unexplained heterogeneity, therefore we did not downgrade the certainty of the evidence for inconsistency.
Potential biases in the review process
We applied robust methods in the process of analysing the search, assessing risk of bias, collecting data, performing analyses, and assessing the certainty of evidence. Nevertheless, some points must be taken into consideration. In the case of Hartmann 1997, we estimated the baseline to six‐month changes in venous refilling time using data provided from baseline and six‐month follow‐up. We adopted the same procedure to estimate baseline to eight‐week changes in muscle strength and intensity of signs and symptoms for Aydin 2022. It is important to note that this is the best estimate we could reach using the data provided by the study authors; however, we recognise that these calculated data might be inaccurate.
Padberg 2004 investigated the intervention in participants with venous ulcers, but did not provide data separately for participants with non‐ulcerated CVI. We included this study because fewer than 25% of all participants had venous ulcers. In Hartmann 1997, the unit of analysis was extremities (legs) and not participants; hence, the study, which included 23 participants, accounted for 46 extremities, but we were unable to obtain raw data to calculate the appropriate adjustments.
Klonizakis 2009 did not investigate any of the outcomes of interest for this review, but was included as it met our inclusion criteria. We considered it relevant to discuss the authors' conclusions since they mention an outcome that none of the other included studies investigated.
We were unable to obtain any publications from one report that could have been considered for inclusion (NCT00013273), therefore we have assessed this study as awaiting classification until publications become available.
We were unable to obtain publications from three registered clinical trials (Karakelle 2021; NCT00013273; Volpe 2020). Two of these trials are still ongoing, and they will only be considered for inclusion if data from ulcerated and non‐ulcerated CVI are reported separately.
Agreements and disagreements with other studies or reviews
The first published version of this review included two studies (Hartmann 1997; Padberg 2004), and this update includes three additional studies (Aydin 2022; Kahn 2011; Klonizakis 2009). Despite the availability of more data, our conclusion remains as there is insufficient evidence available to assess the efficacy of physical exercise in people with non‐ulcerated CVI.
The review by de Moraes Silva 2019 assessed the effects of balneotherapy. The authors identified moderate‐ to low‐certainty evidence of this therapy for improvement in CVI patients when compared to no treatment. Balneotherapy consists of treatments that involve water, and may have some features related to physical exercises such as walking in the pool or gymnastics, but it is also influenced by water properties such as temperature, osmotic and hydrostatic pressure. Generally, physical exercise is not the major component part of balneotherapy treatment. In order to specifically address the effect of physical exercise, we did not include studies using balneotherapy.
There are reviews investigating the effects of exercise on individuals with CVI; however, they all include studies with ulcerated CVI, and the outcomes are generally only ulcer‐related, such as wound area, recurrence, and time to heal (Jull 2018; Orr 2017; Smith 2018). The scope of this review was to address the effects of physical exercise on non‐ulcerated CVI.
Authors' conclusions
Implications for practice.
There is currently insufficient evidence to assess the benefits and harms of physical exercise in people with chronic venous disease. Further research is required to help inform decision‐making by health professionals and people with chronic venous insufficiency (CVI).
Implications for research.
Future research into the effect of physical exercise on individuals with CVI should consider types of exercise protocols (intensity, frequency, and time), sample size, blinding, and homogeneity according to the severity of disease. Trials should also utilise standardised outcome measures, such as ejection fraction, venous refilling time, the incidence of venous ulcers, and the intensity of signs and symptoms using validated tools. Studies should consider using all the steps from the CONSORT document to improve the reporting of findings (Schulz 2010). Further multicentre studies on the epidemiology and aetiology of CVI are also needed to improve the understanding of this disease and its treatment in different countries.
What's new
| Date | Event | Description |
|---|---|---|
| 14 June 2023 | New citation required but conclusions have not changed | Search updated. Three new studies included, 14 new studies excluded, one new ongoing study identified, and three new studies assessed as awaiting classification. Text updated to reflect current Cochrane standards. No change to conclusions. |
| 14 June 2023 | New search has been performed | Search updated. Three new studies included, 14 new studies excluded, one new ongoing study identified, and three new studies assessed as awaiting classification. |
History
Protocol first published: Issue 7, 2013 Review first published: Issue 12, 2016
Acknowledgements
The review authors would like to thank Dr Marlene Stewart (Managing Editor) and Dr Cathryn Broderick (Assistant Managing Editor) for their assistance in the development of this review update. The review authors and the editorial base wish to thank the following reviewers for their comments: Ralph G DePalma, MD, Department of Veterans Affairs, Office of Research and Development, Washington, DC, USA; Mr Brian Duncan, USA; Dr Muataz Kashbour, Diagnostic Radiology Department, National Cancer Institute, Misrata, Libya.
Appendices
Appendix 1. Sources searched and search strategies
| Source | Search strategy | Hits retrieved |
| 1. VASCULAR REGISTER IN CRSW (Date of most recent search: 28 March 2022) |
#1 Venous Insufficiency AND INREGISTER #2 Varicose Veins AND INREGISTER #3 CVI AND INREGISTER #4 #1 OR #2 OR #3 #5 Exercise AND INREGISTER #6 Sport* AND INREGISTER #7 Physical Therapy Modalities AND INREGISTER #8 Physical activit* AND INREGISTER #9 Physical therap* AND INREGISTER #10 Physical fitness AND INREGISTER |
March 2020: 39 March 2022: 5 |
| 2. CENTRAL via CRSO (Date of most recent search: 28 March 2022) |
#1 MESH DESCRIPTOR Venous Insufficiency EXPLODE ALL TREES 563 #2 MESH DESCRIPTOR Leg EXPLODE ALL TREES 2852 #3 MESH DESCRIPTOR Varicose Veins EXPLODE ALL TREES 1123 #4 CVI:TI,AB,KY 234 #5 (((varicos* or tortu*) adj3 (vein* or veno*))):TI,AB,KY 1280 #6 ((incomp* adj3 (vein* or veno* or saphenous or valv*))):TI,AB,KY 162 #7 (((insuffic* or reflux) adj3 (vein* or veno* or saphenous))):TI,AB,KY 311 #8 ("chronic venous disease*"):TI,AB,KY 145 #9 ("Chronic venous insufficiency"):TI,AB,KY 491 #10 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 5421 #11 MESH DESCRIPTOR Exercise EXPLODE ALL TREES 22946 #12 MESH DESCRIPTOR Exercise Therapy EXPLODE ALL TREES 12594 #13 MESH DESCRIPTOR Sports EXPLODE ALL TREES 14951 #14 MESH DESCRIPTOR Physical Therapy Modalities EXPLODE ALL TREES 23575 #15 (Physical activit*):TI,AB,KY 27036 #16 (Physical therap*):TI,AB,KY 8911 #17 (Physical conditioning):TI,AB,KY 621 #18 (Physical fitness):TI,AB,KY 4357 #19 (Physical therap*):TI,AB,KY 8911 #20 Exercis*:TI,AB,KY 91831 #21 sport*:TI,AB,KY 8034 #22 train*:TI,AB,KY 93128 #23 fitness:TI,AB,KY 9576 #24 walk*:TI,AB,KY 26518 #25 run*:TI,AB,KY 18833 #26 treadmill*:TI,AB,KY 7537 #27 swim*:TI,AB,KY 1149 #28 aerobic*:TI,AB,KY 13422 #29 #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 204031 #30 #10 AND #29 1458 |
March 2020: 301 March 2022: 101 |
| 3. Clinicaltrials.gov (Date of most recent search: 28 March 2022) |
Venous Insufficiency OR Varicose Veins OR CVI | Exercise OR Sport OR Physical Therapy OR Physical activity OR Physical fitness | March 2020: 18 March 2022: 6 |
| 4. ICTRP Search Portal (Date of most recent search: 28 March 2022) |
Venous Insufficiency OR Varicose Veins OR CVI AND Exercise OR Sport OR Physical Therapy OR Physical activity OR Physical fitness | March 2020: 13 March 2022: 2 |
| 5. MEDLINE (Ovid MEDLINE® Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE®) 1946 to present (Date of most recent search: 28 March 2022) |
1 exp Venous Insufficiency/ 2 exp Leg/bs [Blood Supply] 3 exp Varicose Veins/ 4 CVI.ti,ab. 5 ((varicos* or tortu*) adj3 (vein* or veno*)).ti,ab. 6 (incomp* adj3 (vein* or veno* or saphenous or valv*)).ti,ab. 7 ((insuffic* or reflux) adj3 (vein* or veno* or saphenous)).ti,ab. 8 "chronic venous disease*".ti,ab. 9 "Chronic venous insufficiency".ti,ab. 10 or/1‐9 11 exp Exercise/ 12 exp Exercise Therapy/ 13 exp Sports/ 14 exp Physical Therapy Modalities/ 15 "Physical activit*".ti,ab. 16 "Physical therap*".ti,ab. 17 "Physical conditioning".ti,ab. 18 "Physical fitness".ti,ab. 19 "Physical therap*".ti,ab. 20 Exercis*.ti,ab. 21 sport*.ti,ab. 22 train*.ti,ab. 23 fitness.ti,ab. 24 walk*.ti,ab. 25 run*.ti,ab. 26 treadmill*.ti,ab. 27 swim*.ti,ab. 28 aerobic*.ti,ab. 29 or/11‐28 30 10 and 29 31 randomized controlled trial.pt. 32 controlled clinical trial.pt. 33 randomized.ab. 34 placebo.ab. 35 drug therapy.fs. 36 randomly.ab. 37 trial.ab. 38 groups.ab. 39 or/31‐38 40 exp animals/ not humans.sh. 41 39 not 40 42 30 and 41 |
March 2020: 133 March 2022: 78 |
| 6. Embase via OVID 1974 to present (Date of most recent search: 28 March 2022) |
1 exp vein insufficiency/ 2 exp varicosis/ 3 CVI.ti,ab. 4 ((varicos* or tortu*) adj3 (vein* or veno*)).ti,ab. 5 (incomp* adj3 (vein* or veno* or saphenous or valv*)).ti,ab. 6 ((insuffic* or reflux) adj3 (vein* or veno* or saphenous)).ti,ab. 7 "chronic venous disease*".ti,ab. 8 "Chronic venous insufficiency".ti,ab. 9 or/1‐8 10 exp exercise/ 11 exp kinesiotherapy/ 12 exp sport/ 13 exp physiotherapy/ 14 "Physical activit*".ti,ab. 15 "Physical therap*".ti,ab. 16 "Physical conditioning".ti,ab. 17 "Physical fitness".ti,ab. 18 "Physical therap*".ti,ab. 19 Exercis*.ti,ab. 20 sport*.ti,ab. 21 train*.ti,ab. 22 fitness.ti,ab. 23 walk*.ti,ab. 24 run*.ti,ab. 25 treadmill*.ti,ab. 26 swim*.ti,ab. 27 aerobic*.ti,ab. 28 or/10‐27 29 9 and 28 30 randomized controlled trial/ 31 controlled clinical trial/ 32 random$.ti,ab. 33 randomization/ 34 intermethod comparison/ 35 placebo.ti,ab. 36 (compare or compared or comparison).ti. 37 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 38 (open adj label).ti,ab. 39 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 40 double blind procedure/ 41 parallel group$1.ti,ab. 42 (crossover or cross over).ti,ab. 43 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 44 (assigned or allocated).ti,ab. 45 (controlled adj7 (study or design or trial)).ti,ab. 46 (volunteer or volunteers).ti,ab. 47 trial.ti. 48 or/30‐47 49 29 and 48 |
March 2020: 170 March 2022: 120 |
| 7. CINAHL via EBSCO (Date of most recent search: 28 March 2022) |
S46 S30 AND S45 S45 S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 S44 MH "Random Assignment" S43 MH "Triple‐Blind Studies" S42 MH "Double‐Blind Studies" S41 MH "Single‐Blind Studies" S40 MH "Crossover Design" S39 MH "Factorial Design" S38 MH "Placebos" S37 MH "Clinical Trials" S36 TX "multi‐centre study" OR "multi‐center study" OR "multicentre study" OR "multicenter study" OR "multi‐site study" S35 TX crossover OR "cross‐over" S34 AB placebo* S33 TX random* S32 TX trial* S31 TX "latin square" S30 S10 AND S29 S29 S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 S28 TX aerobic* S27 TX swim* S26 TX treadmill* S25 TX run* S24 TX walk* S23 TX fitness S22 TX train* S21 TX sport* S20 TX Exercis* S19 TX "Physical therap*" S18 TX "Physical fitness" S17 TX "Physical conditioning" S16 TX "Physical therap*" S15 TX "Physical activit*" S14 (MH "Physical Therapy+") S13 (MH "Sports+") S12 (MH "Therapeutic Exercise+") S11 (MH "Exercise+") S10 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 S9 TX "Chronic venous insufficiency" S8 TX "chronic venous disease*" S7 TX (insuffic* or reflux) N3 (vein* or veno* or saphenous)) S6 TX incomp* N3 (vein* or veno* or saphenous or valv*) S5 TX (varicos* or tortu*) N3 (vein* or veno*) S4 TX CVI S3 (MH "Varicose Veins+") S2 (MH "Leg/BS") S1 (MH "Venous Insufficiency+") |
March 2020: 54 March 2022: 43 |
| 8. AMED (Allied and Complementary Medicine) 1985 to present (Date of most recent search: 28 March 2022) |
1 CVI.ti,ab. 2 ((varicos* or tortu*) adj3 (vein* or veno*)).ti,ab. 3 (incomp* adj3 (vein* or veno* or saphenous or valv*)).ti,ab. 4 ((insuffic* or reflux) adj3 (vein* or veno* or saphenous)).ti,ab. 5 "chronic venous disease*".ti,ab. 6 "Chronic venous insufficiency".ti,ab. 7 or/1‐6 8 "Physical activit*".ti,ab. 9 "Physical therap*".ti,ab. 10 "Physical conditioning".ti,ab. 11 "Physical fitness".ti,ab. 12 "Physical therap*".ti,ab. 13 Exercis*.ti,ab. 14 sport*.ti,ab. 15 train*.ti,ab. 16 fitness.ti,ab. 17 walk*.ti,ab. 18 run*.ti,ab. 19 treadmill*.ti,ab. 20 swim*.ti,ab. 21 aerobic*.ti,ab. 22 or/8‐21 23 7 and 22 24 exp CLINICAL TRIALS/ 25 RANDOM ALLOCATION/ 26 DOUBLE BLIND METHOD/ 27 Clinical trial.pt. 28 (clinic* adj trial*).tw. 29 ((singl* or doubl* or trebl* or tripl*) adj (blind* or mask*)).tw. 30 PLACEBOS/ 31 placebo*.tw. 32 random*.tw. 33 PROSPECTIVE STUDIES/ 34 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 35 23 and 34 |
March 2020: 0 March 2022: 1 |
| TOTAL before deduplication | March 2020: 728 March 2022: 356 |
|
| TOTAL after deduplication | March 2020: 603 March 2022: 288 |
|
| TOTAL after combining 2020 and 2022 | March 2022: 864 | |
Appendix 2. Cochrane's tool for assessing risk of bias
1. Was the allocation sequence randomly generated?
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table; using a computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots.
High risk of bias
The investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example: sequence generated by odd or even date of birth; sequence generated by some rule based on date (or day) of admission; sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process to permit a judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based, and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes.
High risk of bias
Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on: using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or nonopaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure.
Unclear
Insufficient information to permit a judgement of low or high risk of bias. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definitive judgement; for example, if the use of assignment envelopes is described, but it is unclear whether envelopes were sequentially numbered, opaque, and sealed.
3. Blinding ‐ was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias
Any one of the following.
No blinding, but the review authors judge that the outcome and the outcome measurement are not likely to be influenced by lack of blinding.
Blinding of participants and key study personnel ensured, and it is unlikely that the blinding could have been broken.
Either participants or some key study personnel were not blinded, but outcome assessment was blinded, and the non‐blinding of others is unlikely to introduce bias.
High risk of bias
Any one of the following.
No blinding or incomplete blinding, and the outcome or outcome measurement is likely to be influenced by lack of blinding.
Blinding of key study participants and personnel attempted, but it is likely that the blinding could have been broken.
Either participants or some key study personnel were not blinded, and the non‐blinding of others is likely to introduce bias.
Unclear
Any one of the following.
Insufficient information to permit a judgement of low or high risk of bias.
The study did not address this outcome.
4. Were incomplete outcome data adequately addressed?
Low risk of bias
Any one of the following.
No missing outcome data.
Reasons for missing outcome data are unlikely to be related to true outcome (for survival data, censoring is unlikely to be introducing bias).
Missing outcome data are balanced in numbers across intervention groups, with similar reasons for missing data across groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk is not enough to have a clinically relevant impact on the intervention effect estimate.
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes is not enough to have a clinically relevant impact on observed effect size.
Missing data have been imputed using appropriate methods.
High risk of bias
Any one of the following.
Reason for missing outcome data is likely to be related to true outcome, with either an imbalance in numbers or reasons for missing data across intervention groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk is enough to induce clinically relevant bias in the intervention effect estimate.
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes is enough to induce clinically relevant bias in observed effect size.
‘As‐treated’ analysis carried out with substantial departure of the intervention received from that assigned at randomisation.
Potentially inappropriate application of simple imputation.
Unclear
Any one of the following.
Insufficient reporting of attrition/exclusions to permit a judgement of low or high risk of bias (e.g. number randomised not stated, no reasons for missing data provided).
The study did not address this outcome.
5. Are reports of the study free of the suggestion of selective outcome reporting?
Low risk of bias
Any of the following.
The study protocol is available, and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way.
The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon).
High risk of bias
Any one of the following.
Not all of the study’s prespecified primary outcomes have been reported.
One or more primary outcomes are reported using measurements, analysis methods, or subsets of the data (e.g. subscales) that were not prespecified.
One or more of the reported primary outcomes were not prespecified (unless a clear justification for their reporting is provided, such as an unexpected adverse effect).
One or more of the outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis.
The study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Unclear
Insufficient information to permit a judgement of low or high risk of bias. It is likely that the majority of studies will fall into this category.
6. Other potential sources bias
Low risk of bias
The study appears to be free of other sources of bias.
High risk of bias
There is at least one important risk of bias. For example, the study:
had a potential source of bias related to the specific study design used;
had extreme baseline imbalance;
has been claimed to have been fraudulent; or
had some other problem.
Unclear
There may be a risk of bias, but there is either:
insufficient information to assess whether an important risk of bias exists; or
insufficient rationale or evidence that an identified problem will introduce bias.
Appendix 3. GRADE assessment of additional outcomes
No studies reported on the outcome of surgical interventions to treat symptoms related to chronic venous insufficiency.
Ankle joint mobility was assessed using dynamometry or digital goniometry. One study reported no changes in range of motion (baseline to 6‐months change MD: ‐1.4 degrees, 4.77 lower to 1.97 higher; 29 participants) and another study reported higher ankle plantar flexion (degrees) from baseline to 8‐weeks change (right leg: MD 12.13, 8.28 higher to 15.98 higher; left leg: MD 10.95, 7.93 higher to 13.97 higher; 21 participants, 1 study). Certainty of evidence is considered very low. We downgraded the certainty of evidence twice for risk of bias and twice for imprecision due to small number of participants and wide confidence interval.
Data and analyses
Comparison 1. Intensity of signs and symptoms.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Venous Clinical Severity Score ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2 Venous Clinical Severity Score ‐ baseline to 8 weeks change | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Comparison 2. Ejection fraction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 3. Venous refilling time.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Total refilling time(s) ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.2 Venous refilling time baseline to 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.2.1 Right side | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.2.2 Left side | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.3 Venous filling index ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 4. Quality of life.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 QoL: VEINES score ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.2 QoL: SF‐36 PCS score ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.3 QoL: SF‐36 MCS score ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.4 QoL: CIVIQ‐20, Global Index Score ‐ baseline to 8‐week change | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 5. Exercise capacity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Time on treadmill ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.2 6‐minute walk test ‐ baseline to 8‐week change | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6. Muscle strength.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Ankle dynamometry ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.2 Heel lifts ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.3 Plantar flexion dynamometry ‐ baseline to 8‐week changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.3.1 Right side | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.3.2 Left side | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 7. Ankle joint mobility.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Maximum range of motion in dynamometry ‐ baseline to 6‐month changes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2 Maximum range of motion ‐ plantiflexion baseline to 8‐week change | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.1 Right side | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.2 Left side | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aydin 2022.
| Study characteristics | ||
| Methods | Study design: randomised clinical trial Study grouping: parallel group Method of randomisation: website Exclusion postrandomisation: 4 exclusions ITT analysis: not applied | |
| Participants |
Country: Turkey
Setting: Department of Cardiovascular Surgery and Gerontology Research and Application Center, Medical Faculty of Cerrahpasa, Istanbul University‐Cerrahpasa, Istanbul
Number of participants: 32
Baseline characteristics: Exercise
Control
Overall
Inclusion criteria: age 18 to 75 years, diagnosis of CVI using duplex ultrasound, and CEAP classification of C2, C3, C4, or C5 Exclusion criteria: patients with acute DVT, active ulcers, previous vein ablations, and/or a psychiatric disorder requiring prescription medication were excluded. Patients with NYHA class III to IV heart and those receiving treatment for a neurologic, orthopaedic, or rheumatologic disease were also excluded. |
|
| Interventions |
Exercise
Control
|
|
| Outcomes |
Intensity of signs and symptoms (by VCSS, pain by VAS)
Venous refilling time (right and left limb)
Quality of life (by CIVIQ‐20 ‐ global index score)
Exercise capacity (6‐minute walk test)
Muscle strength (dynamometer, right and left limb, in plantar flexion and dorsiflexion)
Ankle joint mobility (digital goniometer, right and left limb, in plantar flexion and dorsiflexion)
|
|
| Funding | None received. | |
| Declarations of interest | None declared. | |
| Notes | Group 1 (n = 11) performed only respiratory exercises and compression therapy, therefore we did not include this group in our analysis. *Muscle strength unit of measurement is not stated in the study; however, their reference for the measurement uses pounds (lb), and that is the usual output given by the equipment used in the study, therefore we used pounds as the unit in our analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The Research Randomizer website was used to enter the number of participants and groups for randomization, and the resulting numbers were placed in envelopes. The groups were created using the numbers from the randomly drawn envelopes. Randomization was performed confidentially to ensure the blindness of the groups" |
| Allocation concealment (selection bias) | Unclear risk | The study mentions the use of envelopes for allocation concealment; however, no further details were provided regarding, for example, if envelopes were unsealed or translucent and how the content was revealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were blinded, but personnel were not. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Pre‐ and post‐treatment evaluations were performed by another physiotherapist and cardiovascular surgeon who did not know to which group the patients had been randomized" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All exclusions and attrition were stated. |
| Selective reporting (reporting bias) | High risk | Data from baseline to after treatment for the outcomes "intensity of signs and symptoms" and "ankle joint mobility" from the control group were not presented. |
| Other bias | Low risk | Baseline characteristics were properly described, and groups were reasonable balanced except by a higher proportion CEAP 4 to 5 in control group. |
Hartmann 1997.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial Study grouping: parallel group Method of randomisation: no description of the randomisation method provided Exclusions postrandomisation: 1 dropout from the control group who declined to submit to further control measurements ITT analysis: not applied | |
| Participants |
Country: Germany
Setting: Institute of Applied Physiology, Universitat Freidburg, Bad Krozingen
Number of participants: 24
Baseline characteristics: the authors state the groups were balanced: "For the purpose of the study these two groups formed matched pairs, corresponding to one another in all relevant measurement parameters." Exercise
Control
Overall
Inclusion criteria: patients suffering from manifest varicose veins in both lower extremities with increased venous capacity, as determined by SGP, and reduced venous filling time, as determined by PPG Exclusion criteria: concomitant heart or arterial disease, orthopaedic disorders of the lower extremities, or vasoactive medication |
|
| Interventions |
Exercise
Control
|
|
| Outcomes |
Pain
Swelling
Restlessness
Cramps
Itching
Stasis oedema
Half refilling time
Total refilling time
|
|
| Funding | Supported in part by grants from the Union of Balneotherapy and Climatotherapy and the Ministry of Commerce Baden‐Wurttemberg | |
| Declarations of interest | Not reported | |
| Notes | There are 2 publications in different journals that report exactly the same data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "After receiving detailed information about test procedures, they were randomized into two groups. For the purpose of the study these two groups formed matched pairs, corresponding to one another in all relevant measurement parameters" There is no mention of how the groups were matched. |
| Allocation concealment (selection bias) | High risk | "After receiving detailed information about test procedures, they were randomized into two groups. For the purpose of the study these two groups formed matched pairs, corresponding to one another in all relevant measurement parameters" There is no mention of a method for allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The authors do not mention blinding of participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The authors do not mention blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "During the study there was 1 dropout from the control group who declined to submit to further control measurements" Data were not presented properly; assessment of pain, swelling, restlessness, cramps, itching, and stasis oedema are presented in percentage change, without SE or SD, and the instrument ("standardized questionnaire") was improperly described. |
| Selective reporting (reporting bias) | High risk | In the measurement section of the study report, the authors say: "After a fifteen‐minute rest period, two measurements each of venous capacity and maximum venous outflow were made at intervals of five minutes by means of a strain‐gauge plethysmograph". However, there are no reports of maximum venous outflow. Additionally, venous capacity data is not fully presented in the results section (data were extracted from abstract). As noted above for attrition bias, data from several outcomes were not properly presented. |
| Other bias | High risk | The authors refer to "balanced groups at baseline"; however, data were not presented. There is a unit of analysis issue, as the unit of analysis is extremities (legs) and not participant. |
Kahn 2011.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial Study grouping: parallel group Method of randomisation: via a web‐based program (Dacima Software Inc) Exclusions postrandomisation: 11 participants withdrew or were lost to follow‐up ITT analysis: authors report using a modified ITT analysis that included all participants with data at baseline and 6 months | |
| Participants |
Country: Canada
Setting: General Hospital (based on indirect information provided in ethics approval)
Number of participants: 39
Baseline characteristics: Exercise
Control
Overall
Inclusion criteria: 18 to 75 years with unilateral, symptomatic DVT objectively diagnosed at least 6 months previously and current ipsilateral manifestations in the leg consistent with PTS. Those with a score of > 5 were classified as having PTS. Exclusion criteria: contraindications to exercise training (e.g. lower extremity arthritis, angina, severe obstructive lung disease), had a life expectancy less than 6 months, were pregnant or lactating, had an open venous leg ulcer, were not English‐ or French‐speaking, were geographically inaccessible for follow‐up visits, or were unwilling or unable to provide signed informed consent. Participants whose exercise test was stopped for reasons other than fatigue alone (e.g. severe dyspnoea, chest pain, electrocardiographic coronary ischaemia or arrhythmia) were excluded from the trial. |
|
| Interventions | The intervention was a 6‐month exercise training programme consisting of strengthening, stretching, and aerobic components designed to improve leg strength, leg flexibility, and overall cardiovascular fitness. Exercise
Control
Exercise training group had a higher proportion of men and higher levels of self‐reported habitual physical activity at baseline (shown in table of Appendix 1 in the original report). |
|
| Outcomes |
QoL (VEINES‐QOL)
Villalta score
Exercise capacity
QoL (SF‐36 physical component score)
QoL (SF‐36 mental component score)
Leg flexibility (quadriceps)
Leg flexibility (hamstring)
Leg flexibility (gastrocnemius)
Leg flexibility (soleus)
Muscle strength
|
|
| Funding | Canadian Institutes for Health Research (CIHR) | |
| Declarations of interest | Susan Kahn is a principal investigator of an ongoing trial funded by the Canadian Institutes for Health Research (CIHR) investigating active versus placebo compression stockings to prevent post‐thrombotic syndrome after deep vein thrombosis, for which Sigvaris Corp has provided active and placebo compression stockings. She is a co‐applicant and steering committee member on a trial funded by the US National Institutes of Health of pharmacomechanical catheter‐directed thrombolysis plus standard anticoagulation alone. She has received honoraria to speak on post‐thrombotic syndrome at various national and international academic conferences. Clive Kearon is principal investigator for a CIHR grant for the evaluation of a D ‐dimer‐based management strategy for selecting patients with unprovoked venous thromboembolism for indefinite anticoagulation. He is a steering committee member for 1 recently completed and 2 ongoing studies of venous thromboembolism treatment by Boehringer Ingelheim. Marc Rodger served on an advisory board for Boehringer Ingelheim, Sanofi‐Aventis, and bio‐Mérieux. He is appointed at the Ottawa Hospital Research Institute, which received compensation from Boehringer Ingelheim, Sanofi‐Aventis, bioMérieux, and LEO Pharma for this service No competing interests declared by other authors. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to exercise training or control via a web‐based program (Dacima Software Inc) that ensured concealment of treatment allocation. |
| Allocation concealment (selection bias) | Low risk | Used software for randomisation and to ensure concealment of treatment allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Outcome assessor was blinded to allocation; however, other personnel were not. Blinding of participants was not possible because control group did not perform exercise. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor was blinded to allocation: "The blinded assistant performed the baseline, three‐month and six‐month assessments of all participants, who were instructed not to reveal their allocated treatment." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition and exclusions were reported; however, there is an imbalance between control and intervention groups that could potentially impact the results. The number of participants in the CONSORT diagram is less than reported in 2 outcomes (PTS severity and QoL) in the results section, with no specific explanation provided. |
| Selective reporting (reporting bias) | Low risk | All outcomes presented were previously described in trial registries and were properly analysed. |
| Other bias | Low risk | Baseline characteristics were properly described, and groups were balanced except by a higher proportion of men and higher levels of self‐reported habitual physical activity at baseline in the intervention group. The severity of disease was similar between groups, and quantitative methods for muscle flexibility, strength, and exercise capacity (time on treadmill) were adopted which minimise the bias regarding reported physical activity. |
Klonizakis 2009.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial Study grouping: parallel group Method of randomisation: computer program (nQueryAdvisor 6.0, Statistical Solutions, Ireland) Exclusions postrandomisation: none ITT analysis: all randomised participants were included in the analysis | |
| Participants |
Country: UK
Setting: general hospital
Number of participants: 16
Baseline characteristics: Exercise
Control
Overall
Inclusion criteria: "Patients who had recently (within 4 – 5 weeks) had venous surgery (unilateral saphenofemoral ligation and partial stripping)" Exclusion criteria: "Patients with skin changes of the gaiter area, diabetes, cardiovascular disease, or those who were taking vasodilatory therapy were excluded from participation. Those who were nonambulatory or not able to meet the physical requirements of the study were also excluded." |
|
| Interventions |
Exercise
Control
|
|
| Outcomes |
Peak perfusion supine (ACh)
Peak perfusion standing (ACh)
Peak perfusion supine (SNP)
Peak perfusion standing (SNP)
|
|
| Funding | Not reported | |
| Declarations of interest | Not reported | |
| Notes | We were not able to obtain numerical data for data presented in graphs, thereby precluding further analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomised, using a computer programme (nQueryAdvisor 6.0, Statistical Solutions, Ireland), to either a treadmill walking exercise group or a non‐exercise control group" |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment method was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | There was no description of blinding of personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | There was no description of blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Compliance to the twice weekly exercise sessions was 100% and there were no drop‐outs or exercise‐related complications." |
| Selective reporting (reporting bias) | High risk | We did not find a clinical trial registration. Numerical data were not provided (only bar graphs), therefore further analyses and extraction were not possible. Effect sizes (Cohen's d) were described in the methods, but these data were not published. |
| Other bias | Low risk | Groups were balanced at baseline, including number of males and females in the sample. |
Padberg 2004.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial Study grouping: parallel group Method of randomisation: prepared confidential randomisation list Exclusions postrandomisation: 3 participants ITT analysis: no | |
| Participants |
Country: USA
Setting: outpatient clinic and home
Number of participants: 31 randomised
Baseline characteristics: groups were balanced at baseline regarding disease severity and comorbidities. There was an imbalance in physical performance during isokinetic exercise at baseline, with lower peak torque and total work in the treatment group; however, peak torque/body weight was similar. Exercise
Control
Overall
Inclusion criteria: patients with advanced CVI were recruited for this trial from an outpatient veterans clinic population. Inclusion criteria required the presence of skin changes or ulceration (CEAP clinical classes 4, 5, 6), as well as objective evidence of CVI as determined with duplex ultrasound scanning and APG. Exclusion criteria: ulceration > 4 cm in diameter, painful ulceration, active local infection, recognised non‐compliance, absence of objective evidence of a venous cause, uncompensated cardiorespiratory insufficiency, ABI < 0.7, and recent venous thrombosis. In general, limbs with active ulceration or infection were stabilised, with a decrease in ulcer diameter to < 2 cm and control of pain or local infection before screening; volunteers did not proceed to consideration for inclusion until they could wear the study stocking regularly (no alternative bandages were used once recruitment and testing had begun). |
|
| Interventions |
Exercise
Control
All participants received 2 pairs of class II (30 to 40 mmHg), below‐knee compression hosiery. |
|
| Outcomes |
Ejection fraction
Residual volume fraction
Venous filling index
Outflow volume
Venous volume
Ejected volume
Intensity of signs and symptoms
Ankle joint mobility
Calf muscle strength
Note: muscle strength here was measured by total work of calf movement evaluated by Biodex. |
|
| Funding | Funding was awarded through the Merit Review Board of the Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research and Development Service. | |
| Declarations of interest | None declared. | |
| Notes | Data for participants with ulcerated CVI and non‐ulcerated CVI were not presented separately; 6/30 (20%) participants had CEAP classification C6. The N on the control group is wrong in the study publication in the "baseline to 6‐month change", because it states 15 instead of 13. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was made by a previously prepared confidential randomisation list (topic "Randomization and statistics"). |
| Allocation concealment (selection bias) | Low risk | Only the statistician was aware of the allocation and responsible for group assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of outcome assessment is not described in the paper. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All dropouts and exclusions were properly described by the trialists. |
| Selective reporting (reporting bias) | High risk | No QoL data were reported, even though the outcome was described in the methods. |
| Other bias | High risk | There was no separate description of results in participants with ulcerated CVI and non‐ulcerated CVI, although the average data included 20% of ulcerated CVI. There was an imbalance regarding physical performance during isokinetic exercise at baseline, with lower peak torque and total work in the treatment group. |
ABI: ankle‐brachial index ACh: acetylcholine chloride APG: air plethysmography BMI: body mass index CEAP: Clinical, Etiology, Anatomic, Pathophysiology CVI: chronic venous insufficiency CIVIQ‐20: Chronic Venous Insufficiency Quality of Life Questionnaire DVT: deep vein thrombosis ITT: intention‐to‐treat NYHA: New York Heart Association PPG: photoplethysmography PTS: post‐thrombotic syndrome QoL: quality of life SD: standard deviation SE: standard error SEM: standard error of the mean SGP: strain‐gauge plethysmography SF‐36: 36‐item Short Form Health Survey SNP: sodium nitroprusside VAS: visual analogue scale VCSS: Venous Clinical Severity Score Veines‐QOL: Venous Insufficiency Epidemiological and Economic Study ‐ Quality of Life
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Carpentier 2009 | Wrong intervention. Participants underwent a spa treatment with balneotherapy sessions. |
| Carpentier 2014 | Wrong intervention. Participants underwent a spa treatment with balneotherapy sessions. |
| CTRI/2018/10/015895 | Wrong intervention. Participants underwent naturopathy. |
| Forestier 2014 | Wrong intervention. Participants underwent balneotherapy sessions. |
| Hartmann 1991 | Wrong study design. Not a randomised trial |
| Hasan 2020 | Wrong patient population. Participants were children with post‐thrombotic syndrome. |
| Kesterton 2019 | Wrong patient population. Participants had venous leg ulcers. |
| Klyscz 1998 | Wrong study design. Not a randomised trial |
| Mancini 2003 | Wrong intervention. Participants underwent balneotherapy sessions. |
| Mutlak 2019 | Wrong patient population. Participants had venous leg ulcers. |
| NCT02689557 | Wrong intervention. The investigated intervention was a single walking session to compare assessment methods. |
| NCT03562546 | Wrong study design. Cohort study |
| NCT04148950 | Wrong comparator. Both control and intervention groups underwent an exercise protocol, and the investigated intervention was Kinesio tape. |
| O'Brien 2018 | Wrong patient population. Participants had venous leg ulcers. |
| Ravikumar 2017 | Wrong intervention. The investigated intervention was neuromuscular electrical stimulation. |
| RBR‐9bhbrp | Wrong comparator. Both control and intervention groups underwent a exercise protocol, and the investigated intervention was Kinesio tape. |
| Sharifi 2020 | Wrong intervention. Participants underwent balneotherapy/aquatic therapy. |
| Tew 2015 | Wrong patient population. Participants had venous leg ulcers. |
Characteristics of studies awaiting classification [ordered by study ID]
Dogru‐Huzmeli 2020.
| Methods | RCT |
| Participants | Individuals with CVI, aged 16 to 60 years |
| Interventions | Dance therapy, consisting of a combination of PNF exercise patterns combined with dance movements, diaphragmatic breathing exercises, and breath retraining. Exercise patterns carried out to music. |
| Outcomes | Signs and symptoms (by VCSS), constipation complaint, assistive breath muscle activity, lower limb circumference, lower limb muscle strength, range of movement, and QoL (by SF‐36 Turkish version) |
| Notes | Authors do not state CEAP classification of included participants. We contacted the corresponding author, but have received no response. |
Karakelle 2021.
| Methods | RCT |
| Participants | Individuals with CVI CEAP 3 to 6 |
| Interventions | Compression therapy, exercise training |
| Outcomes | QoL, venous reflux, disease severity, pain, exercise capacity, muscle strength, calf girth |
| Notes | The study includes individuals with CVI C3 to 6. We contacted the authors to obtain data from non‐ulcerated participants separately for inclusion in the review, but they stated that these data would not be available for this purpose. |
NCT00013273.
| Methods | Randomised, open‐label, single‐group efficacy study |
| Participants | Individuals with severe form of CVI |
| Interventions | A 6‐month structured programme of physical therapy conducted 1 to 3 times per week |
| Outcomes | Lower limb muscle strength, mobility, and QoL |
| Notes | Unable to classify the study because there is no access to any publication |
Volpe 2020.
| Methods | RCT |
| Participants | Individuals aged 35 to 69 years, with CVI CEAP 2 to 6, ABI 0.9 to 1.3 |
| Interventions | Exercise |
| Outcomes | Functional mobility, sural triceps muscle resistance, ankle range of motion, QoL |
| Notes | We may be able to include this study if future CEAP 2 to 5 results are described separately from CEAP 6 results. |
ABI: ankle‐branchial index CEAP: Clinical, Etiology, Anatomic, Pathophysiology CVI: chronic venous insufficiency PNF: proprioceptive neuromuscular facilitation QoL: quality of life RCT: randomised clinical trial SF‐36: 36‐item Short Form Health Survey VCSS: Venous Clinical Severity Score
Characteristics of ongoing studies [ordered by study ID]
NCT02148029.
| Study name | Role of a novel exercise program to prevent post‐thrombotic syndrome (EFFORT2) |
| Methods | RCT |
| Participants | Adults with lower‐extremity DVT documented within 4 weeks of onset of symptoms |
| Interventions | Exercise, anticoagulation, compression, ad‐lib ambulation |
| Outcomes | Severity of DVT, QoL |
| Starting date | 1 July 2014 |
| Contact information | Brajesh K Lal, Baltimore VA Medical Center |
| Notes |
DVT: deep vein thrombosis QoL: quality of life RCT: randomised clinical trial
Differences between protocol and review
2022
We had previously excluded Klonizakis 2009 as it did not report the outcomes of interest for this review. For this update, we reassessed the study as included in keeping with Cochrane recommendations, where all studies meeting the inclusion criteria should be included regardless of whether the outcomes of interest to the review are reported or not.
2016
We considered venous refilling time to be a relevant variable and have added this as a primary outcome. We amended the review to allow for both ejection fraction and venous refilling time to be obtained using the same evaluation procedure (plethysmography). We considered including studies investigating individuals with chronic venous insufficiency and venous ulcers if data for the two ulcerated and non‐ulcerated groups were not analysed and presented separately provided participants with leg ulcers formed less than 25% of the total study population.
Contributions of authors
DA: reviewed the protocol, selected studies, extracted data, and assessed risk of bias; approved the final version prior to submission and made an intellectual contribution to this update.
CR: graded the certainty of evidence, approved the final version prior to submission, and made an intellectual contribution to this update.
AM: made an intellectual contribution to this update and approved the final version of the review prior to submission.
SB: made an intellectual contribution to this update and approved the final version of the review prior to submission.
FD: reviewed the protocol, selected studies, extracted data, and assessed risk of bias; advised, developed, and co‐ordinated this update; approved the final version of the review prior to submission and made an intellectual contribution to this update.
GF: made an intellectual contribution to this update and approved the final version of the review prior to submission.
Sources of support
Internal sources
-
No source of support, Other
Not applicable
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
Declarations of interest
DA: none known. CR: none known. AM: none known. SB: none known. FD: none known. GF: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Aydin 2022 {published data only}
- Aydin G, Yeldan I, Akgul A, Ipek G. Effects of inspiratory muscle training versus calf muscle training on quality of life, pain, venous function and activity in patients with chronic venous insufficiency. Journal of Vascular Surgery 2022;10(5):1137-46. [DOI: 10.1016/j.jvsv.2022.04.012] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT04215133. Inspiratory muscle training versus calf muscle on venous function. clinicaltrials.gov/ct2/show/NCT04215133 (first received 2 January 2020).
Hartmann 1997 {published data only}
- Hartmann B. Physical therapy improves venous haemodynamics in cases of primary varicosity: results of a controlled study. Journal of the Japanese Society of Balneology, Climatology and Physical Medicine 1995;58(3):198-204. [Google Scholar]
- Hartmann BR, Drews B, Kayser T. Physical therapy improves venous hemodynamics in cases of primary varicosity: results of a controlled study. Angiology 1997;48(2):157-62. [DOI: 10.1177/000331979704800209] [DOI] [PubMed] [Google Scholar]
Kahn 2011 {published data only}
- Kahn SR, Shrier I, Shapiro S, Houweling AH, Hirsch AM, Reid RD, et al. Six-month exercise training program to treat post-thrombotic syndrome: a randomized controlled two-centre trial. Canadian Medical Association Journal 2011;183(1):37-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klonizakis 2009 {published data only}
- Klonizakis M, Tew G, Michaels J, Saxton J. Exercise training improves cutaneous microvascular endothelial function in post-surgical varicose vein patients. Microvascular Research 2009;78(1):67-70. [DOI] [PubMed] [Google Scholar]
Padberg 2004 {published data only}
- Padberg FT Jr, Johnston MV, Sisto SA. Structured exercise improves calf muscle pump function in chronic venous insufficiency: a randomized trial. Journal of Vascular Surgery 2004;39:79-87. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Carpentier 2009 {published data only}
- Carpentier PH, Satger B. Randomized trial of balneotherapy associated with patient education in patients with advanced chronic venous insufficiency. Journal of Vascular Surgery 2009;49(163):163-70. [DOI] [PubMed] [Google Scholar]
Carpentier 2014 {published data only}
- Carpentier P, Satger B. Thermes and veines: a multicenter randomized controlled trial evaluating balneotherapy in patients with advanced chronic venous insufficiency. Annals of Physical and Rehabilitation Medicine 2014;57(Suppl 1):e161. [DOI] [PubMed] [Google Scholar]
- Carpentier PH, Blaise S, Satger B, Genty C, Rolland C, Roques C, et al. A multicenter randomized controlled trial evaluation balneotherapy in patients with advanced chronic venous insufficiency. Journal of Vascular Surgery 2014;59(2):447-54. [DOI] [PubMed] [Google Scholar]
CTRI/2018/10/015895 {published data only}
- CTRI/2018/10/015895. Effect of yoga and naturopathy on abnormally dilated veins of legs. trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2018/10/015895 (first received 5 October 2018).
Forestier 2014 {published data only}
- Forestier JR, Briancon G, Francon A, Erol FB, Mollard JM. Balneohydrotherapy in the treatment of chronic venous insufficiency. VASA 2014;43(5):365-71. [DOI: 10.1024/0301-1526/a000374] [DOI] [PubMed] [Google Scholar]
Hartmann 1991 {published data only}
- Hartmann B, Kayser T, Drews B, Bassenge E. Effect of several weeks of functional venous training in venous insufficiency: results of a controlled study [Wirkungen eines mehrwöchigen funktionellen venentrainings bei venöser insuffizienz: Ergebnisse einer kontrollierten studie]. VASA 1991;33(Suplementum):225. [PubMed] [Google Scholar]
Hasan 2020 {published data only}
- Hasan R, Hanna M, Zhang S, Malone K, Tong E, Salas N, et al. Physical activity in children at risk of postthrombotic sequelae: a pilot randomized controlled trial. Blood Advances 2020;4(15):3767-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kesterton 2019 {published data only}
- Kesterton S, Crank HJ, Tew GA, Michaels J, Gumber A, McIntosh E, et al. Participant experiences in a feasibility trial of supervised exercise training in adults with venous leg ulcers: a qualitative study. International Wound Journal 2019;16(6):1559-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klyscz 1998 {published data only}
- Klyscz T, Horstmann T, Nicolaus M, Junger M. Clinical improvement in patients with chronic venous incompetence (CVI) by an intensified 6 weeks lasting physical exercise training. International Journal of Sports Medicine 1998;19:S8. [Google Scholar]
- Klyscz T, Horstmann T, Nikolaus M, Piening C, Dickhuth HH, Jünger M. Therapeutic benefits of a 6-week-long exercise program in patients with chronic venous incompetence [Klinische Verbesserungen bei Patienten mit chronischer Veneninsuffizienz (CVI) durch ein intensivierter 6-Wochen-Trainingsprogram]. Deutsche Zeitschrift für Sportmedizin 1998;49:37-41. [Google Scholar]
Mancini 2003 {published data only}
- Mancini S, Piccinetti A, Nappi G, Mancini S, Caniato A, Coccheri S. Clinical, functional and quality of life changes after balneokinesis with sulphurous water in patients with varicose veins. VASA 2003;32(1):26-30. [DOI] [PubMed] [Google Scholar]
Mutlak 2019 {published data only}
- Mutlak O, Aslam M, Standfield NJ. Chronic venous insufficiency: a new concept to understand pathophysiology at the microvascular level - a pilot study. Perfusion 2019;34(1):84-9. [DOI] [PubMed] [Google Scholar]
NCT02689557 {published data only}
- NCT02689557. VEINEX: Venous Investigations During Exercise. clinicaltrials.gov/ct2/show/NCT02689557 (first received 24 February 2016).
NCT03562546 {published data only}
- NCT03562546. The effect of structured exercise on chronic venous insufficiency. clinicaltrials.gov/ct2/show/NCT03562546 (first received 19 June 2018).
NCT04148950 {published data only}
- NCT04148950. Effects of kinesio taping method on functional capacity and quality of life in patients with chronic venous disease. clinicaltrials.gov/ct2/show/NCT04148950 (first received 4 November 2019).
O'Brien 2018 {published data only}
- O'Brien J, Finlayson K, Kerr G, Shortridge-Baggett L, Edwards H. Using a theoretical approach to identify factors influencing adherence to an exercise programme for adults with venous leg ulcers. Journal of Health Psychology 2018;23(5):691-700. [DOI] [PubMed] [Google Scholar]
Ravikumar 2017 {published data only}
- Ravikumar R, Williams KJ, Babber A, Lane TR, Moore HM, Davies AH. Randomised controlled trial: potential benefit of a footplate neuromuscular electrical stimulation device in patients with chronic venous disease. European Journal of Vascular and Endovascular Surgery 2017;53(1):114-21. [DOI] [PubMed] [Google Scholar]
RBR‐9bhbrp {published data only}
- RBR-9bhbrp. Changes in oxygenation of skin and muscles after the use of functional bandage in women with varicose veins [Uso de bandagem funcional no oxigênio da pele e músculos em mulheres com varizes]. ensaiosclinicos.gov.br/rg/RBR-9bhbrp (first received 26 June 2018).
Sharifi 2020 {published data only}
- Sharifi M, Bay RC, Karandish K, Emrani F, Snyder R, D'Silva S, et al. The randomized, controlled ATLANTIS trial of aquatic therapy for chronic venous insufficiency. Journal of Vascular Surgery: Venous and Lymphatic Disorders 2021;9(4):961-70. [DOI] [PubMed] [Google Scholar]
Tew 2015 {published data only}
- Tew GA, Michaels J, Crank H, Middleton G, Gumber A, Klonizakis M. Supervised exercise training as an adjunctive therapy for venous leg ulcers: study protocol for a randomised controlled trial. Trials 2015;16(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Dogru‐Huzmeli 2020 {published data only}
- Dogru-Huzmeli E, Fansa I, Cetisli-Korkmaz N, Oznur-Karabicak G, Lale C, Gokcek O, et al. Dancing: more than a therapy for patients with venous insufficiency. Vascular 2020;28(2):189-95. [DOI: 10.1177/1708538119893534] [PMID: ] [DOI] [PubMed] [Google Scholar]
Karakelle 2021 {published data only}
- Gürdal Karakelle S, Ipek Y, Tulin O, Alpagut IU. The efficiency of exercise training in patients with venous insufficiency: a double blinded, randomized controlled trial. Phlebology 2021;36(6):440-9. [DOI: 10.1177/0268355520985759] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT03755180. Exercise training in venous insufficiency. clinicaltrials.gov/ct2/show/NCT03755180 (first received 27 November 2018).
NCT00013273 {published data only}
- NCT00013273. Physical conditioning in management of chronic venous insufficiency. clinicaltrials.gov/ct2/show/NCT00013273 (first received 14 March 2001).
Volpe 2020 {published data only}
- RBR-57xtk7. Efficacy of a physical exercises protocol for legs in patients with venous chronic insufficiency [Eficácia de um protocolo de exercícios para pernas em pacientes com insuficiência venosa crônica]. ensaiosclinicos.gov.br/rg/RBR-57xtk7 (first received 19 September 2016).
- Volpe EFT, Resqueti VR, da Silva AAM, Gualdi LP, Fregonezi GAF. Supervised exercise protocol for lower limbs in subjects with chronic venous disease: an evaluator-blinded, randomized clinical trial. Trials 2020;21(1):414. [DOI: ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT02148029 {published data only}
- NCT02148029. Role of a novel exercise program to prevent post-thrombotic syndrome. clinicaltrials.gov/ct2/show/NCT02148029 (first received 28 May 2014).
Additional references
Beebe‐Dimmer 2005
- Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Annals of Epidemiology 2005;15(3):175-84. [DOI] [PubMed] [Google Scholar]
Bergan 2006
- Bergan JJ, Schmid-Schonbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Mechanisms of disease - chronic venous disease. New England Journal of Medicine 2006;355(5):488-98. [DOI] [PubMed] [Google Scholar]
Brand 1988
- Brand FN, Dannenberg AL, Abbot RD, Kannel WB. The epidemiology of varicose veins: the Framingham study. American Journal of Preventive Medicine 1988;4(2):96-101. [PubMed] [Google Scholar]
Busuttil 2016
- Busuttil A, Lim CS, Davies AH. Post thrombotic syndrome. In: Thrombosis and Embolism: from Research to Clinical Practice. Advances in Experimental Medicine and Biology. Vol. 906. Springer, Cham, September 2016. [DOI: ] [DOI] [PubMed] [Google Scholar]
Collins 2010
- Collins L, Seraj S. Diagnosis and treatment of venous ulcers. American Family Physician 2010;81(8):989-96. [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Version accessed 28 March 2022. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Davies 2008
- Davies J, Bull R, Farrelly I, Wakelin M. Improving the calf pump using home-based exercises for patients with chronic venous diseases. Wounds UK 2008;4(3):48-58. [Google Scholar]
De Araujo 2003
- De Araujo T, Valencia I, Federman DG, Kirsner RS. Managing the patient with venous ulcers. Annals Internal Medicine 2003;138(4):326-34. [DOI] [PubMed] [Google Scholar]
de Moraes Silva 2019
- Moraes Silva MA, Nakano LCU, Cisneros LL, Miranda F Jr. Balneotherapy for chronic venous insufficiency. Cochrane Database of Systematic Reviews 2019, Issue 8. Art. No: CD013085. [DOI: 10.1002/14651858.CD013085.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2022
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Eberhardt 2014
- Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation 2014;130:333-46. [DOI: 10.1161/CIRCULATIONAHA.113.006898] [DOI] [PubMed] [Google Scholar]
Eklof 2004
- Eklof B, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, Kistner RL, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. Journal of Vascular Surgery 2004;40(6):1248-52. [DOI] [PubMed] [Google Scholar]
Evans 1999
- Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. Journal of Epidemiology and Community Health 1999;53:149-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldman 1989
- Goldman MP, Fronek A. Anatomy and pathophysiology of varicose veins. Journal of Dermatologic Surgery Oncology 1989;15(2):138-45. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed March 2022. Hamilton (ON): McMaster University (developed by Evidence Prime). Available from gradepro.org.
Heit 2001
- Heit JA, Rooke TW, Silverstein MD, Mohr DN, Lohse CM, Petterson TM, et al. Trends in the incidence of venous stasis syndrome and venous ulcer: a 25-year population-based study. Journal of Vascular Surgery 2001;33(5):1022-7. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JAC. Chapter 8: assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Jull 2018
- Jull A, Slark J, Parsons J. Prescribed exercise with compression vs compression alone in treating patients with venous leg ulcers: a systematic review and meta-analysis. JAMA Dermatology 2018;154(11):1304-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kan 2001
- Kan YM, Delis KT. Hemodynamic effects of supervised calf muscle exercise in patients with venous leg ulceration. Archives of Surgery 2001;136(12):1364-9. [DOI: 10.1001/archsurg.136.12.1364] [DOI] [PubMed] [Google Scholar]
Lefebvre 2022
- Lefebvre C, Glanville J, Briscoe S, Featherstone R, Littlewood A, Marshall C, et al. Chapter 4: Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI: 10.1136/bmj.b2700] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lurie 2020
- Lurie F, Passman M, Meisner M, Dalsing M, Masuda E, Welch H, et al. The 2020 update of the CEAP classification system and reporting standards. Journal of Vascular Surgery: Venous and Lymphatic Disorders 2020;8(3):342-52. [DOI: 10.1016/j.jvsv.2019.12.075] [DOI] [PubMed] [Google Scholar]
Meissner 2005
- Meissner MH. Lower extremity venous anatomy. Seminars in Interventional Radiology 2005;22(3):147-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Metkus 2010
- Metkus TS Jr, Baughman KL, Thompson PD. Exercise prescription and primary prevention of cardiovascular disease. Circulation 2010;121(123):2601-4. [DOI] [PubMed] [Google Scholar]
Nocon 2008
- Nocon M, Hiemann T, Muller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. European Journal of Cardiovascular Prevention and Rehabilitation 2008;15(3):239-46. [DOI] [PubMed] [Google Scholar]
Orr 2017
- Orr L, Klement KA, McCrossin L, O'Sullivan-Drombolis D, Houghton PE, Spaulding S, et al. A systematic review and meta-analysis of exercise intervention for the treatment of calf muscle pump impairment in individuals with chronic venous insufficiency. Ostomy/Wound Management 2017;63(8):30-43. [DOI] [PubMed] [Google Scholar]
Page 2022
- Page MJ, Higgins JP, Sterne JAC. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Perrin 2016
- Perrin M, Eklöf B, Rij A, Labropoulos N, Vasquez M, Nicolaides A, et al. Venous symptoms: the SYM Vein Consensus statement developed under the auspices of the European Venous Forum. International Angiology 2016;35(4):374-98. [PubMed] [Google Scholar]
Pocock 2014
- Pocock ES, Alsaigh T, Mazor R, Schmid-Schönbein GW. Cellular and molecular basis of venous insufficiency. Vascular Cell 2014;6(24):1-8. [DOI: 10.1186/s13221-014-0024-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Quilici 2009
- Quilici BC, Gildo C Jr, De Godoy JM, Quilici BS, Augusto CR. Comparison of reduction of edema after rest and after muscle exercises in treatment of chronic venous insufficiency. International Archives of Medicine 2009;2(18):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Recek 2013
- Recek C. Calf pump activity influencing venous hemodynamics in the lower extremity. International Journal of Angiology 2013;22(1):23-30. [DOI: 10.1055/s-0033-1334092] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2022 [Computer program]
- Review Manager Web (RevMan Web). Version 4.12.0. The Cochrane Collaboration, 2022. Available at revman.cochrane.org.
Robertson 2013
- Robertson L, Lee AJ, Evans CJ, Boghossian S, Allan PL, Ruckley CV, et al. Incidence of chronic venous disease in the Edinburgh Vein Study. Journal of Vascular Surgery: Venous and Lymphatic Disorders 2013;1(1):59-67. [DOI: 10.1016/j.jvsv.2012.05.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rooke 2011
- Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, et al. 2011 ACCF/AHA focused update of the guideline for the management of patients with peripheral artery disease (updating the 2005 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2011;124(18):2020-45. [DOI] [PubMed] [Google Scholar]
Rutherford 2000
- Rutherford RB, Padberg FT, Comerota AJ, Kistner RL, Meissner MH, Moneta GL. Venous severity scoring: an adjunct to venous outcome assessment. Journal of Vascular Surgery 2000;31(6):1307-12. [DOI: 10.1067/mva.2000.107094] [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group 2010. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Annals of Internal Medicine 2010;152(11):1-8. [DOI] [PubMed] [Google Scholar]
Schünemann 2022a
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Schünemann 2022b
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3.0 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Smith 2018
- Smith D, Lane R, McGinnes R, O'Brien J, Johnston R, Bugeja L, et al. What is the effect of exercise on wound healing in patients with venous leg ulcers? A systematic review. International Wound Journal 2018;15(3):441-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Staffa 2002
- Staffa R. Chronic venous insufficiency – epidemiology. Bratislavske Lekarske Listy 2002;103(4-5):166-8. [PubMed] [Google Scholar]
Vasquez 2010
- Vasquez MA, Rabe E, McLafferty RB, Shortell CK, Marston WA, Gillespie D, et al. Revision of the venous clinical severity score: venous outcomes consensus statement. Special communication of the American Venous Forum Ad Hoc Outcomes Working Group. Journal of Vascular Surgery 2010;52:1387-96. [DOI: 10.1016/j.jvs.2010.06.161] [DOI] [PubMed] [Google Scholar]
Wipke‐Tevis 2000
- Wipke-Tevis DD, Rantz MJ, Mehr DR, Popejoy L, Petroski G, Madsen R, et al. Prevalence, incidence, management, and predictors of venous ulcers in the long-term-care population using the MDS. Advances in Skin and Wound Care 2000;13(5):218-24. [PubMed] [Google Scholar]
Yang 1999
- Yang D, Vandogen YK, Stacey MC. Effect of exercise on calf muscle pump function in patients with chronic venous disease. British Journal of Surgery 1999;86:338-41. [DOI: 10.1046/j.1365-2168.1999.00993.x] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Araujo 2013
- Araujo DN, Ribeiro CTD, Maciel ACC, Bruno SS, Fregonezi GAF, Dias FAL. Physical exercise for the treatment of non-ulcerated chronic venous insufficiency. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD010637. [DOI: 10.1002/14651858.CD010637] [DOI] [PMC free article] [PubMed] [Google Scholar]
Araujo 2016
- Araujo DN, Ribeiro CTD, Maciel ACC, Bruno SS, Fregonezi GAF, Dias FAL. Physical exercise for the treatment of non-ulcerated chronic venous insufficiency. Cochrane Database of Systematic Reviews 2016, Issue 12. Art. No: CD010637. [DOI: 10.1002/14651858.CD010637.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


