Abstract
Objective
To determine the proportions of patients who receive care from family physicians, specialists, and nurse practitioners for the management of common chronic medical conditions.
Design
Population-based retrospective cohort study.
Setting
Province of Alberta.
Participants
Adults aged 19 years or older who were registered for provincial health services and each had 2 or more interactions with the same provider between January 1, 2013, and December 31, 2017, for any of 7 specified chronic medical conditions: hypertension, diabetes, chronic obstructive pulmonary disease (COPD), asthma, heart failure, ischemic heart disease, and chronic kidney disease.
Main outcome measures
Numbers of patients being managed for these conditions and which provider types were involved in their care.
Results
Albertans receiving care for the chronic medical conditions being studied (n=970,783) had a mean (SD) age of 56.8 (16.3) years and 49.1% were female. Family physicians were the sole providers of care for 85.7% of patients with a diagnosis of hypertension, 70.9% with diabetes, 59.8% with COPD, and 65.5% with asthma. Specialists were sole providers of care for 49.1% of patients with ischemic heart disease, 42.2% with chronic kidney disease, and 35.6% with heart failure. Nurse practitioners were involved in the care of less than 1% of patients with these conditions.
Conclusion
Family physicians were involved in the care of most patients with any of 7 chronic medical conditions included in this study and were the sole providers of care for the majority of patients with hypertension, diabetes, COPD, and asthma. Guideline working group representation and the setting of clinical trials should reflect this reality.
Résumé
Objectif
Déterminer les proportions de patients dont les soins sont prodigués par des médecins de famille, des spécialistes et des infirmières praticiennes pour des problèmes de santé chroniques courants.
Type d’étude
Une étude rétrospective de cohortes dans la population.
Contexte
La province de l’Alberta.
Participants
Les adultes de 19 ans ou plus qui étaient inscrits auprès des services de santé provinciaux et qui avaient individuellement eu 2 interactions ou plus avec le même praticien entre le 1er janvier 2013 et le 31 décembre 2017 pour l’un ou l’autre de 7 problèmes de santé chroniques en particulier : hypertension, diabète, maladie pulmonaire obstructive chronique (MPOC), asthme, insuffisance cardiaque, cardiopathie ischémique et néphropathie chronique.
Principaux paramètres à l’étude
Le nombre de patients pris en charge pour ces problèmes et le type de praticiens impliqués dans leurs soins.
Résultats
Les Albertains qui ont reçu des soins pour les problèmes de santé chroniques à l’étude (n=970 783) avaient un âge moyen (ET) de 56,8 (16,3) ans et 49,1 % étaient des femmes. Leur médecin de famille était le seul prestataire de soins de 85,7 % des patients ayant reçu un diagnostic d’hypertension, de 70,9 % de ceux atteints de diabète, de 59,8 % ayant une MPOC et de 65,5 % de ceux souffrant d’asthme. Un spécialiste était le seul prestataire de soins de 49,1 % des patients atteints de cardiopathie ischémique, de 42,2 % de ceux ayant une néphropathie chronique et de 35,6 % de ceux ayant une insuffisance cardiaque. Les infirmières praticiennes étaient impliquées dans les soins de moins de 1 % des patients souffrant de ces problèmes.
Conclusion
Les médecins de famille étaient impliqués dans les soins de la plupart des patients souffrant de l’un ou l’autre des 7 problèmes de santé chroniques inclus dans cette étude et étaient les seuls prestataires de soins pour la majorité des patients atteints d’hypertension, de diabète, de MPOC et d’asthme. La représentation dans les groupes de travail sur les lignes directrices et le milieu des essais cliniques devraient refléter cette réalité.
The ecology of health care refers to where, and from whom, patients seek health care services. This has been studied both generally1,2 and in the Canadian context.3 In all such settings, the majority of care—approximately two-thirds—is delivered by family physicians.1-3 While the management of chronic conditions such as hypertension and diabetes is one of the most common reasons for patients to visit a primary care provider,4 other providers such as specialists and nurse practitioners (NPs) also manage these conditions. Although primary care providers may deliver most health care interactions, it is unclear what proportion of patients with chronic conditions they manage. Knowing where care is provided and where most care takes place would be useful when creating guidelines and recommendations, and research on interventions would be most informative if it were conducted in the settings where care is actually provided. In a 2015 analysis of 176 primary care–focused guidelines, family physicians represented only 17% of guideline contributors.5
In this study, to better understand how patients are managed across the health care system, we determined the profession of providers contributing to the care of patients with 7 common chronic conditions. We did so on a population level, using administrative claims data (provider billings) routinely collected by Alberta Health Services on the more than 4 million residents of Alberta.6 Specifically, we determined the proportions of patients with hypertension, diabetes, chronic obstructive pulmonary disease (COPD), asthma, heart failure (HF), ischemic heart disease, or chronic kidney disease (CKD) who were managed by family physicians, NPs, and specialists.
METHODS
Design and setting
The province of Alberta has a government-funded universal health care system. Free of direct cost to patients, this model funds services provided by family physicians, NPs, and specialists for acute care and management of chronic conditions. This model of health care is common across Canada. Our retrospective cohort study examined health care services provided across Alberta in the 5-year period from January 1, 2013, to December 31, 2017. Ethics approval was obtained through the Health Research Ethics Board at the University of Alberta in Edmonton (Pro00081431).
Data sources
This study linked administrative health databases tracking hospitalizations, emergency department visits, hospital outpatient visits, community-based medical services, vital statistics, and registration with the provincial health care plan. All patient-level data were accessed securely and analyzed solely by the Alberta Health Services Data Steward, with the study team having no direct access to patient-level data.
Family physicians, NPs, and specialists submit billings and diagnostic codes to the Alberta government for services rendered to patients in hospitals or in outpatient or community care settings. The provider type is noted with each diagnosis and can distinguish between family physicians (or general practitioners), physicians with other specialty training, and NPs. While general internists provide primary care services in some countries, such as the United States, this is not often the case in Canada. In this study we considered general internists as providing specialty services for patients with whom they interacted.
Diagnostic codes are captured regardless of how practitioners are remunerated (eg, fee for service or salary), since practitioners who are paid by salary and do not bill the government directly still typically submit shadow billings that use the same diagnostic codes to track their activity. Academic physicians and NPs are the most common shadow billers. For any given patient interaction more than 1 diagnosis may be provided, with up to 3 diagnoses being provided for community services (using International Classification of Diseases [ICD]-9 diagnostic codes7) and up to 10 diagnoses for hospital-based care (using ICD-10 codes8). These administrative claims diagnoses have been validated for the detection of corresponding chronic conditions in an Albertan9,10 and a Canadian11 context. The number of diagnoses submitted is not linked to provider remuneration, which could lead to under-reporting and underestimation of the breadth of conditions managed in a single visit. Shadow billers may also have less incentive to capture all patient interactions given that it does not affect their income (eg, they may neglect to submit billings for telephone calls with patients or with other allied health professionals).
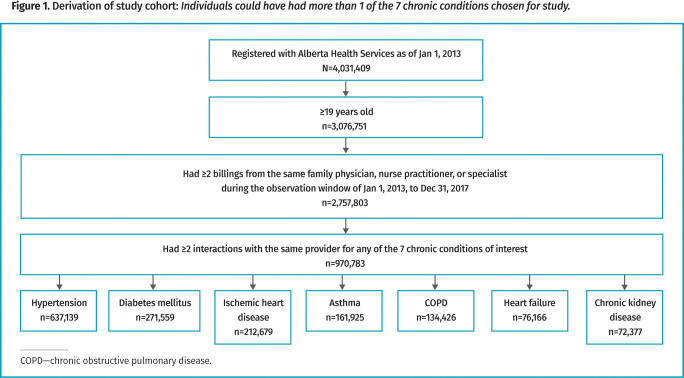
Study cohort
We examined administrative claims for all Albertans registered for provincial health services as of January 1, 2013, and identified 2,757,803 patients who were 19 years of age or older and had each had 2 or more billings with the same family physician, NP, or specialist during the 5-year study period (Figure 1). From there we identified those with 2 or more interactions with the same provider for any of the 7 specified common chronic medical conditions, which included hypertension (ICD-9 codes 401-405, 997.91; ICD-10 codes I10 to I13, I15), diabetes mellitus (ICD-9 codes 249, 250; ICD-10 codes E10 to E14), COPD (ICD-9 codes 490 to 492, 496; ICD-10 codes I278, I279, J684, J701, J703, J40 to J47, J60 to J67), asthma (ICD-9 code 493; ICD-10 code J45), HF (ICD-9 codes 428, 425; ICD-10 code I50), ischemic heart disease (ICD-9 codes 410 to 414; ICD-10 codes I20 to I25), and CKD (ICD-9 codes 403 to 404, 582, 583, 585, 586 to 589, 285.21, 753, 249.4, 250.4, V45.1, V56; ICD-10 codes Z490 to Z492, N032 to N037, N052 to N057, I120, I131, Z940, Z992, N250, N18, N19), thereby composing our study cohort (n=970,783). These chronic conditions were deemed important and commonly encountered based on consensus of the authors, all of whom participate in chronic disease management. It is estimated that 22.6% of Canadians have hypertension,12 5.0% have heart disease, and 1.0% have HF.13 Asthma, diabetes mellitus, and COPD affect 8.1%, 6.9%, and 3.1% of Canadians, respectively,14 and 12.5% of Canadians have been diagnosed with CKD.15
Figure 1.
Derivation of study cohort: Individuals could have had more than 1 of the 7 chronic conditions chosen for study.
Main measures and patient characteristics
We determined how many patients were being managed for each chronic medical condition and recorded which provider types were involved in their care. We also collected basic demographic characteristics for the patient population (eg, age, sex, and presence of complex comorbidity). We defined complex comorbidity as the presence of 3 or more of the studied chronic conditions, recognizing that this would not detect comorbidity in individuals with other chronic physical and mental health conditions that were not examined in this study.
Statistical analysis
For each studied chronic condition, we allocated patients to the following mutually exclusive categories: management exclusively by a family physician; management exclusively by a specialist; co-management by a family physician and a specialist; and any involvement of an NP, regardless of which other providers (family physician or specialist) might be involved. We aggregated patients with NP involvement into a single category as we expected the number of patients with NP involvement to be small relative to those seen by other provider types, given the much lower number of practising NPs in the province compared with both physician types. Our results are presented as the total number and percentage of patients for each provider category.
RESULTS
The 970,783 unique patients included in our analysis had a mean (SD) age of 56.8 (16.3) years and 49.1% were female. Moreover, 15% were 75 years of age or older and 10.8% had 3 or more of the 7 chronic medical conditions studied. Demographic characteristic details according to provider relationship are provided in Table 1. Of the 7 highlighted chronic conditions, hypertension was by far the most commonly treated condition, followed by diabetes mellitus and ischemic heart disease (Table 2).
Table 1.
Characteristics of study cohort by provider type
| CHARACTERISTIC | OVERALL COHORT n=970,783 |
MANAGED BY FAMILY PHYSICIAN ONLY n=580,230 (59.8%) |
MANAGED BY SPECIALIST ONLY n=100,665 (10.4%) |
MANAGED BY FAMILY PHYSICIAN AND SPECIALIST n=288,764 (29.7%) |
ANY NP INVOLVEMENT n=1124 (0.1%) |
|---|---|---|---|---|---|
| Mean (SD) age, y | 56.8 (16.3) | 56.1 (16.0) | 49.2 (16.8) | 60.9 (15.4) | 54 (13.6) |
| Female, n (%)* | 476,206 (49.1) | 291,936 (50.3) | 52,024 (51.7) | 131,733 (45.6) | 513 (45.6) |
| Age ≥75 y, n (%)* | 145,620 (15.0) | 78,431 (13.5) | 8077 (8.0) | 59,029 (20.4) | 83 (7.4) |
| ≥3 studied chronic conditions, n (%)* | 104,483 (10.8) | 72,998 (12.6) | 15,834 (15.7) | 15,640 (5.4) | 11 (1.0) |
NP—nurse practitioner.
Percentages calculated from column total.
Table 2.
No. of Albertans with chronic conditions of interest managed by family physicians, specialists, or NPs
| CHRONIC CONDITION | TOTAL PATIENTS, n |
PATIENTS BY PROVIDER TYPE, n (%)* | |||
|---|---|---|---|---|---|
| MANAGED BY FAMILY PHYSICIAN ONLY |
MANAGED BY SPECIALIST ONLY |
MANAGED BY FAMILY PHYSICIAN AND SPECIALIST |
ANY NP INVOLVEMENT† |
||
| Hypertension | 637,139 | 546,132 (85.7) | 22,951 (3.6) | 67,678 (10.6) | 378 (0.06) |
| Diabetes mellitus | 271,559 | 192,469 (70.9) | 13,674 (5.0) | 64,816 (23.9) | 600 (0.22) |
| COPD | 134,426 | 80,423 (59.8) | 24,437 (18.2) | 29,406 (21.9) | 160 (0.12) |
| Asthma | 161,925 | 106,141 (65.5) | 33,352 (20.6) | 22,362 (13.8) | 70 (0.04) |
| Heart failure | 76,166 | 26,486 (34.8) | 27,148 (35.6) | 22,514 (29.6) | 18 (0.02) |
| Chronic kidney disease | 72,377 | 26,170 (36.2) | 30,510 (42.2) | 15,677 (21.7) | 20 (0.03) |
| Ischemic heart disease | 212,679 | 48,683 (22.9) | 104,436 (49.1) | 59,539 (28.0) | 21 (0.01) |
COPD—chronic obstructive pulmonary disease, NP—nurse practitioner.
All provider categories are mutually exclusive.
Whenever an NP billed for a service 2 or more times, that patient was assigned to this category regardless of involvement by any other provider type.
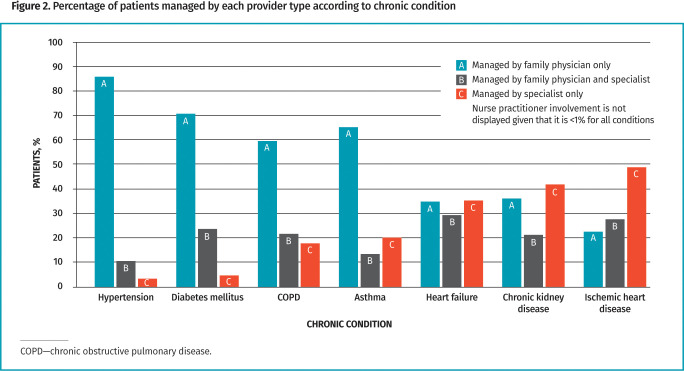
Family physicians provide a large proportion of chronic disease management in Alberta, with or without specialist involvement. Family physicians were the sole health care providers for most patients with hypertension (85.7%), diabetes (70.9%), asthma (65.5%), and COPD (59.8%); very few patients with hypertension (3.6%) or diabetes (5.0%) were managed solely by specialists. Although family physicians were still involved in the management of most patients, specialists were more likely to be the sole managers of patients with ischemic heart disease (49.1%), CKD (42.2%), and HF (35.6%). Regardless of condition, NPs were involved in the care of less than 1% of patients. Details are provided in Table 2 and in Figure 2.
Figure 2.
Percentage of patients managed by each provider type according to chronic condition
DISCUSSION
The ecology of health care concept shows the majority of medical care is provided by family physicians.1,3,16 While this framework does not speak to the complexity of patients’ conditions, our findings demonstrate that family physicians play a role in managing most patients with chronic conditions, often as the sole manager of that condition. In seeming contradiction to this, Tonelli et al have suggested that patients attached to family physicians are the least complex of those seen by all medical specialists17; however, their finding is hardly surprising. In a health care system where many patients have a family physician, the complexity of a primary care patient panel cannot help but approach the population average. Whether family physicians are spending more of their time with their more complex patients, which is likely, is not captured by such an analysis.
Our finding that NPs are involved in the care of less than 1% of patients with these conditions is consistent with what is known about the deployment of NPs in Alberta. Although at the time of our analysis there were roughly 600 NPs practising in Alberta, only 50 worked in primary care settings.18 Most worked in hospitals, in acute care, and in specialty outpatient clinics as specialist extenders. This compares with 5652 family physicians and general practitioners operating in Alberta in 2018, according to Canadian Medical Association data.19
Limitations
Our findings are strengthened by the ability to examine an entire population, but they are limited by being specific to the Alberta health care system and by physician billing data not being intended for research purposes. In a fee-for-service environment where only one diagnosis is required for billing, providers have no incentive to record all diagnoses relevant to an encounter along with their billing. Family physicians, for instance, might be managing patients with HF or ischemic heart disease but recording only one aspect of risk management, such as care related to diabetes or hypertension, and not recording ischemic heart disease or HF as reasons for the consultation unless the patient is symptomatic. Academic physicians and NPs are typically also on salary and submit shadow billings, which means they have less personal incentive to capture all clinical activity. This might have reduced the apparent involvement of NPs. It should also be noted that this study did not look at non-billable health services, such as naturopathic or chiropractic care. Lastly, our study is limited by considering only 7 common chronic medical conditions. Mental health conditions such as depression, anxiety, and substance use disorders, for instance, are commonly encountered in primary care and were not included in this analysis.
Future research
An examination of the extent to which community family practices are sites of randomized trials would be beneficial in the creation of primary care guidelines, particularly those pertaining to hypertension and diabetes. Research is also needed to outline the footprint of NPs in Canada. Although it is often assumed NPs are augmenting primary care services, only a few of those in Alberta appear to be serving in that role. The geographic variability in terms of the nature and availability of primary care NP services—whether as solo providers or as part of a medical home20—needs clarification.
Conclusion
Family physicians are involved in managing the majority of patients with chronic conditions, and for conditions such as diabetes and hypertension they are the sole provider for most patients. Interventions for these conditions should be studied in primary care settings where possible, and consideration should be given to family physicians playing a larger role in clinical guideline development and screening recommendations.
Editor’s key points
▸ Family physicians provide a large proportion of chronic disease management in Alberta, either as the sole physician treating a patient or in collaboration with specialists. This population-based study found that the majority of patients with hypertension (85.7%), diabetes (70.9%), asthma (65.5%), and chronic obstructive pulmonary disease (59.8%) were managed by family physicians alone.
▸ Nurse practitioners were involved in the care of less than 1% of patients with the studied conditions, pointing to a need to better understand geographic variability in the roles they play in the health system.
▸ Clinical trials and guidelines for chronic conditions should take into account which practitioners are most involved in their management and the settings where patients with these conditions are most likely to be seen.
Points de repère du rédacteur
▸ Les médecins de famille s’acquittent d’une vaste proportion de la prise en charge des maladies chroniques en Alberta, que ce soit comme unique médecin traitant du patient ou en collaboration avec des spécialistes. Cette étude populationnelle a fait valoir que la majorité des patients souffrant d’hypertension (85,7 %), de diabète (70,9 %), d’asthme (65,5 %) et de maladie pulmonaire obstructive chronique (59,8 %) étaient pris en charge par un médecin de famille seulement.
▸ Les infirmières praticiennes étaient impliquées dans les soins de seulement 1 % des patients souffrant des problèmes à l’étude, ce qui souligne la nécessité de mieux comprendre la variabilité géographique dans les rôles qu’elles jouent dans le système de santé.
▸ Les essais cliniques et les lignes directrices sur les problèmes chroniques devraient tenir compte des praticiens qui sont les plus impliqués dans leur prise en charge et des milieux dans lesquels il est le plus probable que les patients souffrant de ces problèmes soient traités.
Footnotes
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.White KL, Williams TF, Greenburg BG.. The ecology of medical care. N Engl J Med 1961;265:885-92. [DOI] [PubMed] [Google Scholar]
- 2.Johansen ME, Kircher SM, Huerta TR.. Reexamining the ecology of medical care [letter]. N Engl J Med 2016;374(5):495-6. [DOI] [PubMed] [Google Scholar]
- 3.Stewart M, Ryan B.. Ecology of health care in Canada. Can Fam Physician 2015;61: 449-53 (Eng), e249-54 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 4.Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician 2018;64:832-40. [PMC free article] [PubMed] [Google Scholar]
- 5.Allan GM, Kraut R, Crawshay A, Korownyk C, Vandermeer B, Kolber MR.. Contributors to primary care guidelines. What are their professions and how many of them have conflicts of interest? Can Fam Physician 2015;61:52-8. [PMC free article] [PubMed] [Google Scholar]
- 6.Annual population report. Alberta 2020-21. Edmonton, AB: Alberta Treasury Board and Finance; 2021. Available from: https://open.alberta.ca/dataset/1050cf0a-8c1d-4875-9800-b7d2f3199e41/resource/608764dd-e247-4fc4-a99d-cbc59fc78a0c/download/2020-21-population-report.pdf. Accessed 2023 May 12. [Google Scholar]
- 7.International statistical classification of diseases and related health problems. 9th revision. Geneva, Switz: World Health Organization; 1978. [Google Scholar]
- 8.International statistical classification of diseases and related health problems. 10th revision. Geneva, Switz: World Health Organization; 1992. [Google Scholar]
- 9.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43(11):1130-9. [DOI] [PubMed] [Google Scholar]
- 10.Tonelli M, Wiebe N, Fortin M, Guthrie B, Hemmelgarn BR, James MT, et al. Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 2015;15:31. Erratum in: BMC Med Inform Decis Mak 2019;19(1):177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lix L, Yogendran M, Burchill C, Metge C, McKeen N, Moore D, et al. Defining and validating chronic diseases: an administrative data approach. Winnipeg, MB: Manitoba Centre for Health Policy; 2006. Available from: http://mchp-appserv.cpe.umanitoba.ca/reference/chronic.disease.pdf. Accessed 2023 May 15. [Google Scholar]
- 12.Padwal RS, Bienek A, McAlister FA, Campbell NRC; Outcomes Research Task Force of the Canadian Hypertension Education Program . Epidemiology of hypertension in Canada: an update. Can J Cardiol 2016;32(5):687-94. Epub 2015 Aug 15. [DOI] [PubMed] [Google Scholar]
- 13.Chow CM, Donovan L, Manuel D, Johansen H, Tu JV; Canadian Cardiovascular Outcomes Research Team . Regional variation in self-reported heart disease prevalence in Canada. Can J Cardiol 2005;21(14):1265-71. [PubMed] [Google Scholar]
- 14.Roberts KC, Rao DP, Bennett TL, Loukine L, Jayaraman GC.. Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Health Promot Chronic Dis Prev Can 2015;35(6):87-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arora P, Vasa P, Brenner D, Iglar K, McFarlane P, Morrison H, et al. Prevalence estimates of chronic kidney disease in Canada: results of a nationally representative survey. CMAJ 2013;185(9):E417-23. Epub 2013 May 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Green LA, Fryer GE Jr, Yawn BP, Lanier D, Dovey SM.. The ecology of medical care revisited. N Engl J Med 2001;344(26):2021-5. [DOI] [PubMed] [Google Scholar]
- 17.Tonelli M, Wiebe N, Manns BJ, Klarenbach SW, James MT, Ravani P, et al. Comparison of the complexity of patients seen by different medical subspecialists in a universal health care system. JAMA Netw Open 2018;1(7):e184852. Erratum in: JAMA Netw Open 2019;2(3):e190147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellefontaine M. Alberta will hire 30 new nurse practitioners to work in under-served areas of province. CBC News 2019. Sep 17. Available from: https://www.cbc.ca/news/canada/edmonton/alberta-30-new-nurse-practitioners-to-work-in-under-served-areas-of-alberta-1.5287500. Accessed 2023 May 15.
- 19.Number of physicians by province/territory and specialty, Canada, 2018. Ottawa, ON: Canadian Medical Association; 2018. Available from: https://www.cma.ca/sites/default/files/pdf/Physician%20Data/01-physicians-by-specialty-province-e.pdf. Accessed 2023 May 11. [Google Scholar]
- 20.Kidd Wagner K, Austin J, Toon L, Barber T, Green LA.. Differences in team mental models associated with medical home transformation success. Ann Fam Med 2019;17(Suppl 1):S50-6. [DOI] [PMC free article] [PubMed] [Google Scholar]