ABSTRACT
Ectopic adrenal tissue is an uncommon entity in females. It is usually seen in male children, and the commonly involved sites are the kidney, retroperitoneum, spermatic cord, and paratesticular region. The ectopic adrenal gland in adults has been described in few studies only. Ectopic adrenal tissue was diagnosed as an incidental finding in histopathological examination of serous cystadenoma of the ovary. A 44-year-old female presented with a complaint of vague abdominal discomfort for the past few months. Ultrasound was suggestive of a left ovarian complex cystic lesion. The histopathological examination revealed serous cystadenoma with ectopic adrenal cell rest. Here, we present this case as it is a rare finding incidentally detected in a patient being operated on for a different pathology.
KEYWORDS: Adrenal cell rest, adrenal remnants, ovary, serous cystadenoma
INTRODUCTION
Ectopic adrenal tissue in females has been reported in few studies and is usually identified as an incidental histopathological finding. Morgagni first described the presence of adrenal remnants away from the normal site in the 18th century.[1] Rare sites for ectopic adrenal remnants include liver, pancreas, colon, celiac plexus, placenta, and ovary.[2] The broad ligament may also be the site of predilection in females.[3] Although rare, these remnants may develop into functional adenomas at ectopic sites.[4]
CASE REPORT
A 44-year-old female presented with a complaint of vague abdominal discomfort for the past few months. The contrast-enhanced computed tomography (CECT) of the abdomen revealed a left ovarian complex cystic lesion measuring 7 cm × 6.8 cm. The mass showed an enhancing nodular irregular wall and enhancing irregular septations with a calcific eccentric mural nodule seen posteromedially. The CECT was suggestive of serous cystadenoma of the borderline serous tumor. The serum tumor markers alpha-fetoprotein and CA-125 were within normal limits. The patient subsequently underwent hysterectomy with bilateral salpingo-oophorectomy. Gross examination of the left adnexa showed a multiloculated cystic mass measuring 8 cm × 5 cm × 4 cm with an attached fallopian tube measuring 11 cm in length [Figure 1]. The external aspect was smooth with an intact capsule. On cut opening, thin straw-colored serous fluid came out. A small, calcified nodule measuring 0.5 cm × 0.5 cm was identified. The rest of the hysterectomy specimen with right-sided adnexa was grossly unremarkable. Microscopic examination of the left adnexa showed features of serous cystadenoma with the presence of adrenal cortical cell rests [Figure 2]. There was no evidence of atypia or malignancy. The ectopic adrenal cortical tissue was immunoreactive to inhibin and melan-A [Figure 3].
Figure 1.

Oval-to-round, cystic neoplasm with the smooth glistening surface
Figure 2.
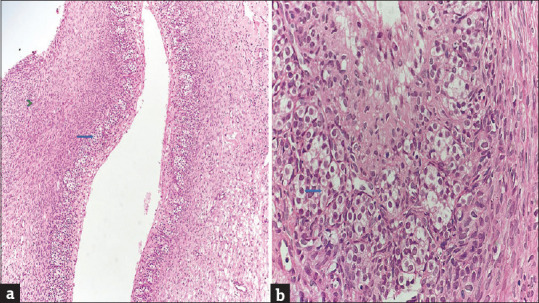
(a and b) Nest of ectopic adrenal cortical rest (blue arrow) along with normal ovarian parenchyma (green arrowhead) (H and E × 10, ×40)
Figure 3.
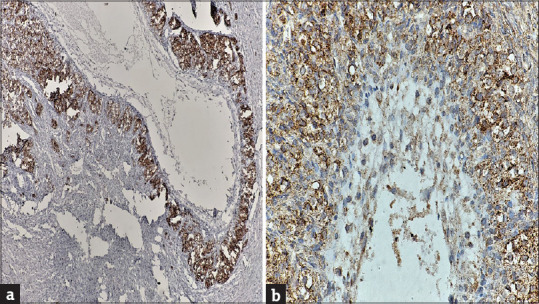
(a and b) Ectopic adrenal cortical rest showing cytoplasmic immunoreactivity to inhibin and melan-A (×40)
DISCUSSION
Although uncommon, ectopic adrenal cell rest can be found anywhere in the genitourinary tract. Most of the time, adrenal heterotopias are reported within the kidney, whereas it is also found at other sites such as retroperitoneum, male genital tract,[1] liver, pancreas, colon, celiac plexus, placenta, and ovary.[2] Ectopic adrenal rests are exceedingly rare in females, but if they occur, the broad ligament is the site of predilection.[3] Ectopic adrenal tissue is commonly detected in autopsies or as an incidental finding in patients with other pathologies, thus carrying a minimal clinical significance.[4] Most of the adrenal cortical rests are nonfunctional. However, functional adenomas can occur at the ectopic sites.[4] The serum cortisol, serum aldosterone, and serum estradiol levels may be raised in hyperplasia or adenoma. The ectopic adrenal gland is typically an incidental finding with unknown origin, but some studies believe in the role of pluripotent stem cells responsible for these heterotopias.[5] These ectopic adrenal cell rests are usually found in children, whose median age is 5.8 years. Heterotopic adrenal cell rests are five times more common in children than adults.[6] The adrenal remnants are usually composed entirely of cortical cells without any medullary cells of normal adrenal, as elucidated by the different embryological origin of the two components.[7,5] The adrenal cortex is derived from the mesoderm and medulla from chromaffin neuroectodermal cells of the neural crest.[1] These two components merge to form a single unit during embryonic development.[7] Over time, cortical fragments can get trapped in descending gonads, and these entrapped fragments may get engulfed by the developing organs.[5,8] With time, the adrenal remnants become atrophic and disappear because of reduced hormonal stimulation by the normal functioning adrenal gland.[7,8] These ectopic adrenal rests do not produce any clinical symptoms but may become symptomatic with a change in biological behavior. The ectopic tissue generally undergoes atrophy because of nonstimulation. However, they can show hyperplasia or neoplasia, and then, such transformation may cause considerable morbidity and mortality to patients.[4,9] Ectopic tissue can be misunderstood as metastatic tissue deposits; then, the patient might be overmanaged in such scenario. The patient can be followed up by magnetic resonance imaging/computed tomography and serum cortisol, aldosterone, and estradiol even if asymptomatic.
CONCLUSION
Ectopic adrenocortical rests constitute a rare entity and are uncommonly found in females. It carries a limited clinical significance because these are asymptomatic and were discovered incidentally during the histopathological examination. Although indolent in most cases, it can rarely show altered biological behavior encountered as hyperplasia or neoplasia, leading to potential complications. Hence, surgeons and pathologists should be aware of this uncommon entity. We reported this case as it is an uncommon finding and was incidentally detected in a patient operated on for a different pathology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Schechter DC. Aberrant adrenal tissue. Ann Surg. 1968;167:421–6. doi: 10.1097/00000658-196803000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khandakar B, Dey S, Ray PS, Sarkar R, Bhattacharyya P. Ectopic paratubal adrenal cell rest associated with mucinous cystadenoma of ovary. J Clin Diagn Res. 2015;9:ED13–4. doi: 10.7860/JCDR/2015/15411.6638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tingi E, Ogah J. Ectopic adrenal rest cells of the fallopian tube: A case report and review of the literature. J Obstet Gynaecol. 2018;38:578–9. doi: 10.1080/01443615.2017.1379063. [DOI] [PubMed] [Google Scholar]
- 4.Surrey LF, Thaker AA, Zhang PJ, Karakousis G, Feldman MD. Ectopic functioning adrenocortical oncocytic adenoma (oncocytoma) with myelolipoma causing virilization. Case Rep Pathol. 2012;2012:326418. doi: 10.1155/2012/326418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson JR, Ross AH. Ectopic adrenal tissue in adults. Postgrad Med J. 1980;56:806–8. doi: 10.1136/pgmj.56.661.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mendez R, Tellado MG, Somoza I, Liras J, Sanchez-Abuin A, Pais E, et al. Ectopic adrenal tissue in the spermatic cord in pediatric patients: Surgical implications. Int Braz J Urol. 2006;32:202–7. doi: 10.1590/s1677-55382006000200013. [DOI] [PubMed] [Google Scholar]
- 7.Alimoradi M, El-Helou E, Sabra H, Azaki R, Khairallah M, Matta N. Ectopic adrenal gland in an adult inguinal hernial sac: A case report. Int J Surg Case Rep. 2020;72:66–8. doi: 10.1016/j.ijscr.2020.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Şahin Ç, Taylan E, Akdemir A, Zekioglu O, Seyidova P, Ergenoglu AM. Ovarian serous cystadenoma with ectopic adrenal tissue in a 65-year-old patient: A case report. Int J Surg Case Rep. 2017;33:89–91. doi: 10.1016/j.ijscr.2017.02.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kasajima A, Nakamura Y, Adachi Y, Takahashi Y, Fujishima F, Chiba Y, et al. Oncocytic adrenocortical neoplasm arising from adrenal rest in the broad ligament of the uterus. Pathol Int. 2014;64:183–8. doi: 10.1111/pin.12154. [DOI] [PubMed] [Google Scholar]


