ABSTRACT
Introduction:
Perimenopause phase of a woman’s life is featured by decline in the ovarian activity, predisposing her to several health consequences. The signs and symptoms of thyroid disorders simulate those of menopausal features which may go unnoticed and can cause untoward complications in these women.
Aims and Objective:
The primary objective is to screen women of perimenopausal age for thyroid disorders. The secondary objective is to examine the variations in thyroid hormone levels in these women with advancing age.
Materials and Methods:
One hundred and forty-eight apparently healthy women between the age group of 46 and 55 years were study subjects. They were divided into, Group I which constituted women between 46 and 50 years and Group II consisted of women between 51 and 55 years. Thyroid profile comprising serum thyroid-stimulating hormone (TSH), serum total triiodothyronine (T3), and serum total thyroxine (T4) were estimated for all the women recruited in the study.
Results:
Subclinical hypothyroidism (SCH) and overt hypothyroidism (OH) were detected in 22 and 8 women who constituted 14.9% and 5.4%, respectively, of the total women populace. In Group I, it was noted that 17.1% and 1.8% of women were suffering from SCH and OH, respectively. In Group II, while 8.1% of the women had SCH, 16.2% of women had progressed to OH. TSH levels were significantly higher (P = 0.002) in women of Group II than in Group I, suggesting increase in TSH levels with advancing age.
Conclusion:
Screening of perimenopausal women for thyroid disorders will assure timely detection and proper management which will aid in reducing the morbidity and associated complications.
KEYWORDS: Estrogen, Hypothyroidism, Menopause, Thyroid-stimulating hormone
INTRODUCTION
A woman’s life encompasses five phases which are associated with considerable hormonal changes. These include infancy, puberty, reproductive age, climacteric period, and elderly years. Climacteric phase of a woman’s life is the period of 5 years preceding and following menopause.[1] The average age of menopause of an Indian woman is 46.6 years as per the latest data.[2] According to the recent data, women between the age group of 40 and 44 years constitute 6.1%, those between 45 and 49 years comprise 5.4%, and 4.3% of the women are between 50 and 54 years of the total population in India.[3] This suggests that currently, around 7 crore women in India are traversing the climacteric juncture. This stage is marked by decline in estrogen production by ovaries. Estrogen plays a major role in the normal functioning of cardiovascular, vasomotor, genitourinary, and skeletal systems.[4] As the estrogen secretion starts to dwindle, the normal functioning of the above-mentioned systems starts to give away and symptoms such as hot flashes, night sweats, dyspareunia, and muscle flaccidity ensues. Features of hypoestrogenemia also include osteoporosis,[5] mental disturbances such as anxiety, depression,[6] and hypercholesterolemia.[7]
Thyroid hormones play a vital role in regulating female reproductive system by modulating the metabolism and development of ovaries, uterus, and placental tissue.[8] There is mutual dependence of the thyroid gland and the gonadal axis throughout the reproductive life of a woman. Thyroid dysfunction can therefore lead to menstrual irregularities and infertility in women. Studies reveal that women are more prone to thyroid abnormalities than men and its prevalence increases with age.[9]
The signs and symptoms of thyroid disorders simulate those of perimenopause and menopausal features. The Stages of Reproductive Aging Workshop +10 staging system divides the female reproductive cycle into three stages based on the menstrual cycle: reproductive, menopause transition, and postmenopause. In the reproductive phase, the menstrual cycle is regular. The second stage is the menopause transition. During the early phase of this stage, the menstrual cycle becomes irregular, such that the length of time between menstruations varies by 7 or more days each cycle.[10] Very similar kind of menstrual disturbance is observed in patients with hypothyroidism. As women enter postmenopause phase, the menstrual cessation occurs with severe vasomotor symptoms. Hyperthyroidism disease characteristics such as excessive sweating, insomnia, and anxiety can be mistaken for those due to menopause.[11] Therefore, when a woman in this transitional phase of life is inflicted with thyroid disorder, there is maximum possibility of it being either dismissed or neglected as climacteric norm.
The aim of the current study is to screen women of perimenopause age for thyroid dysfunction. The secondary objective is to examine the variations in thyroid hormones in these women with advancing age.
MATERIALS AND METHODS
This is a cross-sectional study, which was undertaken in the Clinical Biochemistry Laboratory of Rajarajeswari Medical College Hospital, Bengaluru. The institutional ethics committee approval was taken before the commencement of this research project. The study involved screening women between the age group of 46 and 55 years for thyroid disorders. Women, in this age group, who would visit either the gynecology or general medicine outpatient department for regular health checkup, were directed to the clinical biochemistry laboratory. Here, a detailed history about their medical and surgical illness was elicited. All those women with comorbidities, those on medication, pregnant women, and women already diagnosed with thyroid disorder were excluded from the study. The rest of the women who volunteered and gave written consent to be a part of the study were recruited. This study which spanned for 8 months included 148 women. A fasting venous blood sample was obtained from all the participants of the study and samples were analyzed for serum thyroid-stimulating hormone (TSH), serum total triiodothyronine (T3), and serum total thyroxine (T4). The estimation was done on Maglumi-1000 chemiluminescence-based immunoassay analyzer. The age-specific reference ranges for the thyroid parameters incorporated in the study are as follows:
Serum TSH: 0.3–5.1 mIU/L
Serum total triiodothyronine (T3): 69–215 ng/dl
Serum total thyroxine (T4): 5.2–12.7 μg/dl.
The thyroid disorders were diagnosed based following biochemical cutoff values:
The woman in the study was diagnosed as case of:
Subclinical hypothyroidism (SCH) when her TSH was >5.1 mIU/L and T3 and T4 were normal[12]
Overt hypothyroidism (OH) when TSH was >5.1 mIU/L and T3 and T4 were below the normal reference ranges[13]
Subclinical hyperthyroidism was defined as TSH was <0.3 mIU/L and T3 and T4 were normal and
OH when TSH was <0.1 mIU/L and T3 and T4 were above the normal reference ranges.
The study population of 148 women were segregated into two groups. Group I consisted of women between 46 and 50 years, whereas Group II included women between 51 and 55 years.
Statistical analysis
The results of the thyroid profile analysis of 148 women in the study were compiled and analyzed. The values were expressed as mean and standard deviation (SD). A comparison of the parameters between the two groups in the study was made using Student’s t-test. All statistical analysis was done at 5% level of significance.
RESULTS
Figure 1 depicts the division of the study population into two groups based on their age.
Figure 1.
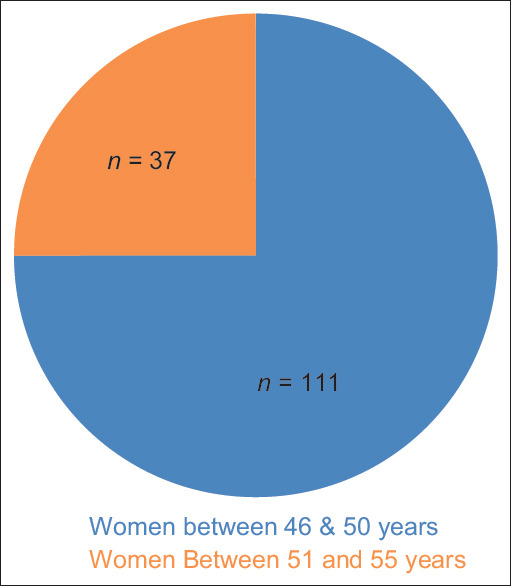
Distribution of study subjects based on age range
The age-specific reference range established for the local population for the three thyroid analytes was applied in the current research. The reference ranges along with the mean and SD of T3 and T4 and TSH for the entire study population, is enumerated in Table 1.
Table 1.
Reference ranges and descriptive statistics of biochemical parameters for the whole group (n=148)
| Parameter | Reference range | Mean±SD |
|---|---|---|
| T3 (ng/dL) | 69-215 | 145.16±33.88 |
| T4 (mg/dL) | 5.2-12.7 | 9.86±1.81 |
| Serum TSH (mIU/L) | 0.3-5.1 | 3.35±3.73 |
T3: Serum total triiodothyronine, T4: Serum total thyroxine, TSH: Thyroid-stimulating hormone, SD: Standard deviation
DISCUSSION
In the current study, we have noticed the Mean ± SD for all the three thyroid parameters are within the normal reference range for the whole group, as shown in Table 1. Further, we noticed SCH in 22 and OH in 8 women who constituted 14.9% and 5.4%, respectively, of the total women populace as depicted in Figure 2. Similar findings were reported by Panda et al. in their study.[14] In Group I, when thyroid dysfunction analysis was done, it was noted that 17.1%, and 1.8% of women were suffering from SCH and OH, respectively. This is in accordance with the findings of study by Goyal et al.[15] While progressing further to analyze the scenario among women in Group II, a change was observed. Here, while 8.1% of the women fit into SCH state of the thyroid gland and 16.2% were women had progressed to OH. These details are graphically represented in Figure 3. When the Mean ± SD of thyroid hormones were compared between the two groups, the TSH levels were significantly higher (P = 0.002) in women of Group II, i.e. in those women between 51 and 55 years. We noticed a significant increase in TSH levels with advancing age. There was no significant difference in T3 and T4 levels. Table 2 is compilation of these observations. The same outcome was noted by Kolanu et al. who had conducted a research akin to the present study.[16] Overall, the screening of women for thyroid disorders in the present study has brought to light the existence of hypothyroidism (SCH and OH) in around 19% (Group I) to 24% (Group II) in the described population. The percentage of women diagnosed with thyroid dysfunction in the 148 women of our study is 20.3%, which is quiet alarming. Incidentally, not a single case of hyperthyroidism was reported among the women of the study.
Figure 2.
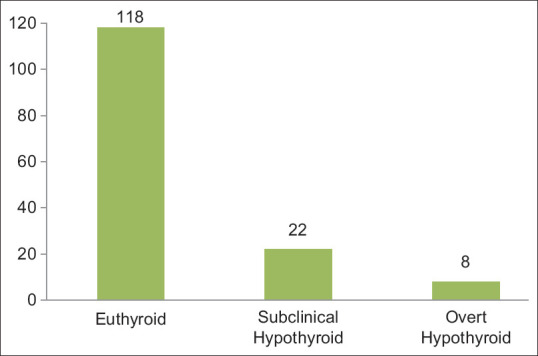
Number-wise distribution of women with normal and abnormal thyroid status in the entire study group (n = 148)
Figure 3.
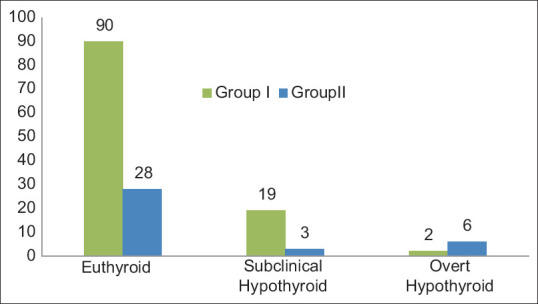
Number-wise distribution of women with normal and abnormal thyroid status in Group I and Group II
Table 2.
Comparison of biochemical parameters between two groups of the study
| Parameter | Mean±SD | P | |
|---|---|---|---|
|
| |||
| Group I (women between 46 and 50 years) (n=111) | Group II (women between 51 and 55 years) (n=37) | ||
| T3 (ng/dL) | 145.38±35.25 | 144.49±29.8 | 0.89 |
| T4 (μg/dL) | 9.83±1.89 | 9.94±1.59 | 0.84 |
| Serum TSH (mIU/L) | 2.80±2.78 | 4.98±5.44 | 0.002 |
T3: Serum total triiodothyronine, T4: Serum total thyroxine, TSH: Thyroid-stimulating hormone, SD: Standard deviation
Thyroid hormones regulate the female reproductive organ functions by increasing sex hormone-binding globulins thus causing low clearance of estrogen from circulation.[17] Estrogen secreted by ovaries, on the other hand, increases the concentration of thyroid-binding globulins by the liver thereby being indirectly responsible for reduced clearance of thyroid hormones.[18] The thyroid hormones and estrogen act synergistically to maintain the hormone milieu in woman during the reproductive age. However, ambiguity lies whether thyroid dysfunction is a cause or an effect of menopause transition. The similarity and overlap of symptoms in these two conditions make it clinically difficult to diagnose thyroid disorders in this age group. Postmenopausal women are at increased risk of both osteoporosis and cardiovascular disease, and untreated thyroid disease may exacerbate these risks. Thyroid screening involves estimating a serum TSH alone which is simple and cost-effective. Routine thyroid screening in elderly women has been recommended worldwide by various clinical and laboratory associations.[14] Recently, The Indian Menopause Society has come up with clinical guidelines and recommendations on menopause where in a routine screening of menopausal women for thyroid disorders by estimating serum TSH has been proposed.[19] This is welcome step which addresses this serious issue.
CONCLUSION
The climacteric stage of life is challenging both physically and psychologically for a woman. A holistic approach acknowledging the necessity for medical as well as psychiatric management involving doctors, family members, and the society is required. The screening of women in this age group for thyroid disorders is definitely a positive step in this direction. It will assure timely detection and proper management which will aid in reducing the morbidity and complications associated with thyroid diseases.
Authors’ contributions
Dr. S. M. R. Usha designed the study and wrote the protocol. Dr. C. M. Bindu was instrumental in collecting the samples and managed the analysis of the study. Dr. Chandrika N wrote the first draft of the study, performed the statistical analysis, managed the literature searches All authors read and approved the final manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Takeda Y. Understanding the life stages of women to enhance your practice. Japan Med Assoc J. 2010;53:273–8. [Google Scholar]
- 2.Prasad JB, Tyagi NK, Verma P. Age at menopause in India: A systematic review. Diabetes Metab Syndr. 2021;15:373–7. doi: 10.1016/j.dsx.2021.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Sample Registration Systems (Field work 2016). Office of the Registrar General &Census Commissioner, India. Ministry of Home affairs Government of India New Delhi Statistical report Detailed Tables. 2016 [Google Scholar]
- 4.Souza Guerra GE, Jr, Prates Caldeira A, Piana Santos Lima de Oliveira F, Santos Figueiredo Brito MF, de Oliveira Silva Gerra KD, Mendes D'Angelis CE, et al. Quality of life in climacteric women assisted by primary health care. PLoS One. 2019;14:e0211617. doi: 10.1371/journal.pone.0211617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crandall CJ, Tseng CH, Crawford SL, Thurston RC, Gold EB, Johnston JM, et al. Association of menopausal vasomotor symptoms with increased bone turnover during the menopausal transition. J Bone Miner Res. 2011;26:840–9. doi: 10.1002/jbmr.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maheshwari P, Agrawal P, Garg R, Upadhyay S. Understanding climacteric depression and depression in other phases of a women's life. J South Asian Fed Menopause Soc. 2015;3:20–3. [Google Scholar]
- 7.Thurston RC, Sutton-Tyrrell K, Everson-Rose SA, Hess R, Matthews KA. Hot flashes and subclinical cardiovascular disease: Findings from the Study of Women's Health Across the Nation Heart Study. Circulation. 2008;118:1234–40. doi: 10.1161/CIRCULATIONAHA.108.776823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silva JF, Ocarino NM, Serakides R. Thyroid hormones and female reproduction. Biol Reprod. 2018;99:907–21. doi: 10.1093/biolre/ioy115. [DOI] [PubMed] [Google Scholar]
- 9.Gesing A, Lewiński A, Karbownik-Lewińska M. The thyroid gland and the process of aging;what is new? Thyroid Res. 2012;5:16. doi: 10.1186/1756-6614-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peacock K, Ketvertis KM. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [Last updated on 2022 Feb 02]. Menopause. Available from:https://www.ncbi.nlm.nih.gov/books/NBK50782 . [Google Scholar]
- 11.Gietka-Czernel M. The thyroid gland in postmenopausal women: Physiology and diseases. Prz Menopauzalny. 2017;16:33–7. doi: 10.5114/pm.2017.68588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brenta G, Vaisman M, Sgarbi JA, Bergoglio LM, Andrada NC, Bravo PP, et al. Clinical practice guidelines for the management of hypothyroidism. Arq Bras Endocrinol Metabol. 2013;57:265–91. doi: 10.1590/s0004-27302013000400003. [DOI] [PubMed] [Google Scholar]
- 13.Patil N, Rehman A, Jialal I. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [Last updated on 2022 Jun 19]. Hypothyroidism. Available from:https://www.ncbi.nlm.nih.gov/books/NBK519536/ [Google Scholar]
- 14.Panda S, Das A. Analyzing thyroid dysfunction in the climacteric. J Midlife Health. 2018;9:113–6. doi: 10.4103/jmh.JMH_21_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goyal G, Goyal LD, Singla H, Sheenam, Arora K, Kaur H. Subclinical hypothyroidism and associated cardiovascular risk factor in perimenopausal females. J Midlife Health. 2020;11:6–11. doi: 10.4103/jmh.JMH_38_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kolanu BR, Vadakedath S, Boddula V, Kandi V. Evaluation of the activities of thyroid hormones among pre- and post-menopausal Euthyroid women: A cross-sectional Study from a tertiary care teaching hospital in India. Cureus. 2019;11:e4259. doi: 10.7759/cureus.4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Honour JW. Biochemistry of the menopause. Ann Clin Biochem. 2018;55:18–33. doi: 10.1177/0004563217739930. [DOI] [PubMed] [Google Scholar]
- 18.del Ghianda S, Tonacchera M, Vitti P. Thyroid and menopause. Climacteric. 2014;17:225–34. doi: 10.3109/13697137.2013.838554. [DOI] [PubMed] [Google Scholar]
- 19.Meeta M, Harinarayan CV, Marwah R, Sahay R, Kalra S, Babhulkar S. Clinical practice guidelines on postmenopausal osteoporosis: An executive summary and recommendations –Update 2019-2020. J Midlife Health. 2020;11:96–112. doi: 10.4103/jmh.JMH_143_20. [DOI] [PMC free article] [PubMed] [Google Scholar]


