Abstract
Background
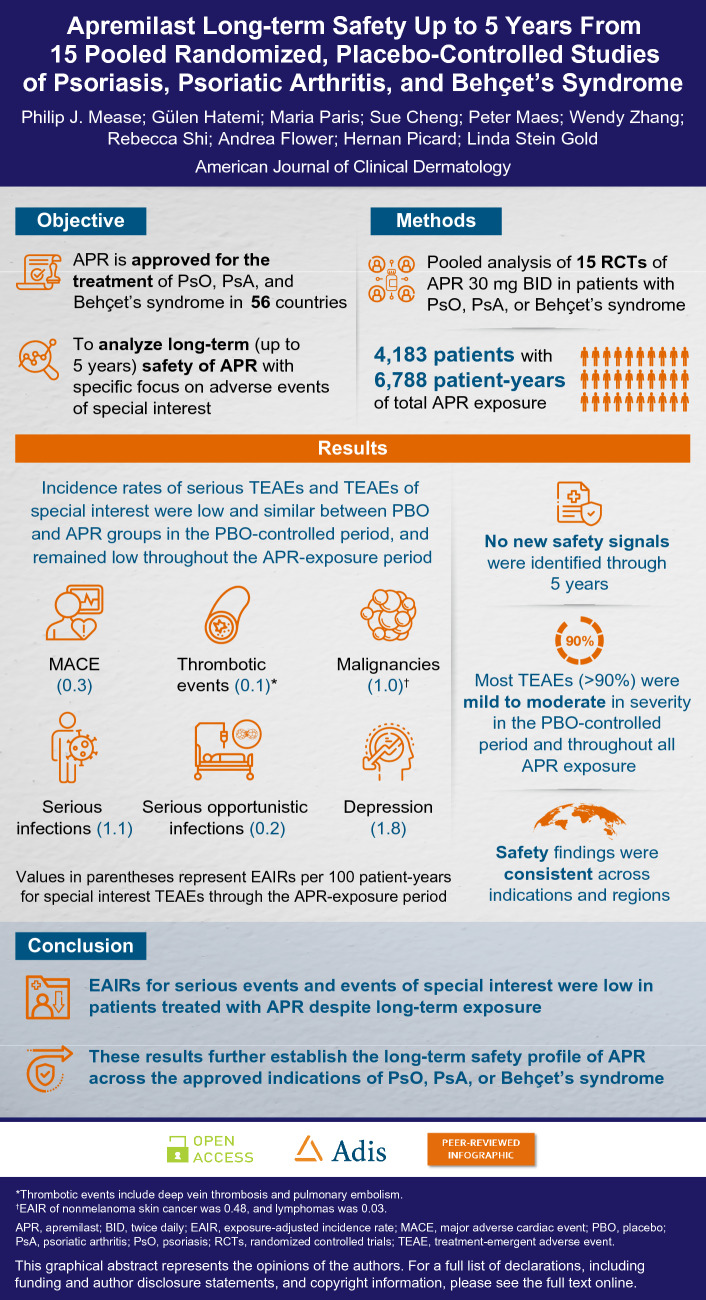
Since US FDA approval in 2014, apremilast has consistently demonstrated a favorable benefit–risk profile in 706,585 patients (557,379 patient-years of exposure) worldwide across approved indications of plaque psoriasis, psoriatic arthritis, and Behçet’s syndrome; however, long-term exposure across these indications has not been reported.
Objective
The aim of this study was to conduct a pooled analysis of apremilast data from 15 clinical studies with open-label extension phases, focusing on long-term safety.
Methods
We analyzed longer-term safety and tolerability of apremilast 30 mg twice daily across three indications for up to 5 years, focusing on adverse events of special interest, including thrombotic events, malignancies, major adverse cardiac events (MACE), serious infections, and depression. Data were pooled across 15 randomized, placebo-controlled studies and divided into placebo-controlled or all-apremilast-exposure groups. Treatment-emergent adverse events (TEAEs) were assessed.
Results
Overall, 4183 patients were exposed to apremilast (6788 patient-years). Most TEAEs were mild to moderate in the placebo-controlled period (96.6%) and throughout all apremilast exposure (91.6%). TEAE rates of special interest were similar between treatment groups in the placebo-controlled period and remained low throughout all apremilast exposure. Exposure-adjusted incidence rates per 100 patient-years during all apremilast exposure were MACE, 0.30; thrombotic events, 0.10; malignancies, 1.0; serious infections, 1.10; serious opportunistic infections, 0.21; and depression, 1.78. Safety findings were consistent across indications and regions. No new safety signals were identified.
Conclusions
The incidence of serious TEAEs and TEAEs of special interest was low despite long-term exposure, further establishing apremilast as a safe oral option for long-term use across indications with a favorable benefit–risk profile.
Clinical Trial Registration
NCT00773734, NCT01194219, NCT01232283, NCT01690299, NCT01988103, NCT02425826, NCT03123471, NCT03721172, NCT01172938, NCT01212757, NCT01212770, NCT01307423, NCT01925768, NCT00866359, NCT02307513.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s40257-023-00783-7.
Key Points
| Apremilast has demonstrated a favorable benefit–risk profile in 706,585 unique patients (557,379 patient-years) worldwide. |
| This analysis further demonstrates that apremilast is a safe, oral treatment option for long-term use up to 5 years in patients with psoriasis, psoriatic arthritis, or Behçet’s syndrome. |
Introduction
Apremilast is an oral phosphodiesterase 4 inhibitor that regulates pro-inflammatory and anti-inflammatory mediators [1, 2]. As such, it is differentiated from some biologics and the Janus kinase (JAK) inhibitor class of oral treatments, which have been associated with increased risk of serious cardiovascular events, cancer, venous thromboembolism, and death [3]. Since apremilast received initial regulatory approval in 2014, it is now approved in 56 countries, including the United States, Japan, and the European Union. As of 20 March 2022, 706,585 adults (557,379 patient-years) worldwide have received apremilast for the treatment of moderate-to-severe (approved for mild severity in certain countries) plaque psoriasis, who are candidates for phototherapy or systemic therapy, have active psoriatic arthritis [1, 4, 5], or have oral ulcers associated with Behçet’s syndrome [1, 4]. Apremilast 30 mg twice daily has an established safety and tolerability profile based on randomized, placebo-controlled trials across multiple indications, but long-term exposure across indications has not been reported [6–16].
Psoriasis, psoriatic arthritis, and Behçet’s syndrome are chronic inflammatory conditions requiring long-term treatment [17, 18]. Understanding the long-term effects of apremilast treatment in these populations can help physicians assess the risks and benefits of treatments and inform treatment decisions in clinical practice. Moreover, there is increasing interest in the potential relationship between therapies for psoriatic disease and specific safety events such as major adverse cardiovascular events (MACE), malignancies, thrombotic events, and serious opportunistic infections.
To analyze the long-term safety and tolerability of apremilast 30 mg twice daily across indications, 15 randomized, placebo-controlled studies were pooled and analyzed, including more than 4000 patients who were treated with apremilast 30 mg twice daily and assessed for up to 5 years. This analysis focused on the most frequently observed adverse events (AEs), as well as AEs of special interest, including MACE, malignancies, serious infections, serious opportunistic infections, thrombotic events, and depression.
Methods
Study Designs and Patients
All studies included in this pooled analysis were conducted in accordance with the general ethical principles outlined in the Declaration of Helsinki and principles of Good Clinical Practice per the International Council for Harmonisation Guidelines and local regulations.
Data were pooled across 15 randomized, double-blind, placebo-controlled studies of apremilast for the treatment of adults with mild-to-moderate or moderate-to-severe plaque psoriasis (eight studies), psoriatic arthritis meeting the Classification Criteria for Psoriatic Arthritis (CASPAR; five studies), and Behçet’s syndrome meeting the International Study Group (ISG) criteria (two studies) [Online Resource 1]. Patients received oral apremilast 30 mg twice daily or placebo during the short-term placebo-controlled periods (12-, 16-, or 24-week duration), followed by long-term extension periods up to Week 260 during which all patients received apremilast 30 mg twice daily (Online Resource 1). Patients were dose-titrated over the first week of treatment. Relevant eligibility criteria are presented in Online Resource 1. The main exclusion criteria included having clinically significant cardiac, pulmonary, neurologic, psychiatric, hepatic, renal, hematologic, or immunologic disease, other major uncontrolled disease, or any condition that may confound the ability to interpret data or place the patient at unacceptable risk.
Pooled Safety Analyses
Across studies, data were pooled for randomized patients who received one or more doses of apremilast for the placebo-controlled phase. Apremilast-exposure analysis included all patients who were randomized at baseline, switched from placebo at early escape, or switched at the end of the placebo-controlled phase to apremilast 30 mg twice daily and received one or more doses of apremilast.
Safety assessments included treatment-emergent AEs (TEAEs), defined as AEs with a start date on or after the date of the first dose of study drug and no later than 28 days after the last dose of study drug. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA) version 23.1. TEAEs of special interest included thrombotic events (deep vein thrombosis, pulmonary embolism), malignancies, MACE (based on a prespecified preferred term search from the AE database, defined as myocardial infarction, acute myocardial infarction, cerebrovascular accident, cerebral infarction, brain stem stroke, hemorrhagic stroke, or ischemic stroke), serious infections (based on System Organ Class Infections and Infestations from the AE database), suicidal ideation/behavior, and depression. Each patient was counted once for each event. Safety data were summarized using descriptive statistics and exposure-adjusted incidence rate (EAIR) per 100 patient-years (100 times the number of patients reporting the event divided by patient-years within the phase, up to the first event start date for patients reporting the event). A subgroup analysis was conducted of TEAEs stratified by regions of the world. Statistical summaries were produced using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
The pooled analysis included 4763 patients, including 2676 patients initially randomized to apremilast 30 mg twice daily and 2087 initially randomized to placebo.
This population includes patients from studies of plaque psoriasis (n = 2881), psoriatic arthritis (n = 1564), and Behçet’s syndrome (n = 318). Primary reasons for discontinuation in the placebo-controlled period included AEs (n = 200 [4.2%]), withdrawal by the patient (n = 179 [3.8%]), lost to follow-up (n = 97 [2.0%]), and lack of efficacy (n = 82 [1.7%]) [Online Resource 2].
During the placebo-controlled periods, 2673 patients were exposed to apremilast and 2084 patients were exposed to placebo. Total exposure was 848.8 patient-years for apremilast 30 mg twice daily and 622.2 patient-years for placebo. The mean duration of total exposure to treatments during the placebo-controlled periods was 16.1 weeks (apremilast: 16.6; placebo: 15.6). Overall, 4183 patients were exposed to apremilast. Overall exposure was 6788.0 patient-years, and mean treatment duration was 84.7 weeks (Table 1). Primary reasons for discontinuation during apremilast exposure (Week 0 to Week 260) were lack of efficacy (n = 678 [16.2%]; 10.0/100 patient-years), withdrawal by the patient (n = 603 [14.4%]; 8.9/100 patient-years), AE (n = 387 [9.3%]; 5.7/100 patient-years), and lost to follow-up (n = 231 [5.5%]; 3.4/100 patient-years).
Table 1.
Treatment duration
| Placebo-controlled period | Placebo [n = 2087] |
Apremilast 30 mg bid [n = 2676] |
|---|---|---|
| Treatment duration, weeks [mean (SD)] | 15.6 (4.9) | 16.6 (5.7) |
| Exposure category [n (%)] | ||
| ≥ 1 day | 2086 (100.0) | 2672 (99.9) |
| ≥ 4 weeks | 2004 (96.0) | 2551 (95.3) |
| ≥ 8 weeks | 1908 (91.4) | 2458 (91.9) |
| ≥ 12 weeks | 1818 (87.1) | 2356 (88.0) |
| ≥ 16 weeks | 1314 (63.0) | 1772 (66.2) |
| ≥ 20 weeks | 275 (13.2) | 677 (25.3) |
| ≥ 24 weeks | 197 (9.4) | 459 (17.2) |
| Apremilast-exposure period | Apremilast 30 mg bid [n = 4183] |
|---|---|
| Treatment duration, weeks [mean (SD)] | 84.7 (85.3) |
| Exposure category [n (%)] | |
| ≥ 1 day | 4183 (100.0) |
| ≥ 4 weeks | 4027 (96.3) |
| ≥ 8 weeks | 3890 (93.0) |
| ≥ 12 weeks | 3782 (90.4) |
| ≥ 16 weeks | 3577 (85.5) |
| ≥ 24 weeks | 3159 (75.5) |
| ≥ 32 weeks | 2797 (66.9) |
| ≥ 52 weeks | 2020 (48.3) |
| ≥ 104 weeks | 1110 (26.5) |
| ≥ 156 weeks | 848 (20.3) |
| ≥ 208 weeks | 719 (17.2) |
| Up to 260 weeks | 252 (6.0) |
Treatment duration is the time interval between the date of the first dose of apremilast 30 mg bid and the date of the last dose of apremilast 30 mg bid, inclusive. For patients re-randomized to placebo at Week 32, the duration was the sum of the treatment duration up to Week 32 inclusive plus the duration after patients switched from placebo to apremilast 30 mg bid
bid twice daily, SD standard deviation
Baseline demographics and clinical characteristics were generally comparable in the pooled apremilast and placebo groups (Table 2). Mean age was 47.4 years, 44.2% of patients were women, 86.5% were White, and more than half (59.2%) were in North America (Table 2). Patients’ medical histories subdivided by psoriasis, psoriatic arthritis, and Behçet’s syndrome indications are shown in Online Resource 3; among the most common historical diagnoses were hypertension, gastroesophageal reflux disease, hypercholesterolemia, hyperlipidemia, and depression.
Table 2.
Baseline patient demographics and clinical characteristics
| Placebo [n = 2087] | Apremilast 30 mg bid [n = 2676] |
|
|---|---|---|
| Age, years [mean (SD)] | 47.5 (13.4) | 47.3 (13.5) |
| Male [n (%)] | 1154 (55.3) | 1506 (56.3) |
| Race [n (%)] | ||
| American Indian or Alaska native | 10 (0.5) | 14 (0.5) |
| Asian | 198 (9.5) | 220 (8.2) |
| Black or African American | 44 (2.1) | 77 (2.9) |
| Native Hawaiian or other Pacific Islander | 7 (0.3) | 11 (0.4) |
| White | 1801 (86.3) | 2318 (86.6) |
| Other | 18 (0.9) | 27 (1.0) |
| Not collected or unknown | 7 (0.3) | 9 (0.3) |
| Missing | 2 (<0.1) | 0 (0) |
| Region [n (%)] | ||
| North America | 1163 (55.7) | 1659 (62.0) |
| Europe | 496 (23.8) | 571 (21.3) |
| Rest of the world | 428 (20.5) | 446 (16.7) |
| Weight, kg [mean (SD)] | 86.8 (22.0) | 85.1 (22.2) |
| BMI, kg/m2 [mean (SD)] | 30.0 (6.9) | 30.1 (6.8) |
| Psoriasis clinical featuresa | Placebo [n = 1147] |
Apremilast 30 mg bid [n = 1734] |
|---|---|---|
| Duration of plaque psoriasis, years [mean (SD)] | 17.4 (12.0) | 18.3 (12.4) |
| sPGA category [n (%)] | ||
| 0 (clear) | 0 (0) | 0 (0) |
| 1 (almost clear) | 1 (< 0.1) | 0 (0) |
| 2 (mild) | 108 (9.4) | 111 (6.4) |
| 3 (moderate) | 803 (70.0) | 1253 (72.3) |
| ≥ 4 (severe) | 235 (20.5) | 369 (21.3) |
| Missing | 0 (0) | 1 (< 0.1) |
| Psoriasis-involved BSA, % [mean (SD)] | 19.1 (15.2) | 19.9 (14.9) |
| PASI [mean (SD)] | 15.2 (8.6) | 15.8 (8.1) |
| DLQI [mean (SD)] | 10.6 (6.4) | 11.0 (6.5) |
| PsA clinical featuresb | Placebo [n = 781] |
Apremilast 30 mg bid [n = 783] |
|---|---|---|
| Duration of PsA, years [mean (SD)] | 5.9 (6.9) | 6.1 (7.1) |
| TJC (0–78) [mean (SD)] | 19.6 (14.4) | 20.7 (14.8) |
| SJC (0–76) [mean (SD)] | 11.0 (7.6) | 11.1 (8.0) |
| Patient Global Assessment of Disease Activity (0–100 mm VAS) [mean (SD)] | 49.0 (26.3) | 48.6 (26.6) |
| Physician Global Assessment of Disease Activity (0–100 mm VAS) [mean (SD)] | 47.4 (24.2) | 48.0 (24.3) |
| HAQ-DI score (0–3) [mean (SD)] | 1.1 (0.6) | 1.2 (0.6) |
| C-reactive protein, mg/dL [mean (SD)] | 1.1 (1.8) | 1.0 (1.4) |
| SF-36v2 Physical Functioning scale score (norm-based) [mean (SD)] | 34.6 (10.5) | 34.0 (10.6) |
| Disease Activity Score (DAS28) [mean (SD)] | 4.7 (1.0) | 4.7 (1.0) |
| Behçet’s Syndrome Clinical Featuresc | Placebo [n = 159] |
Apremilast 30 mg bid [n = 159] |
|---|---|---|
| Duration of Behçet’s syndrome, years [mean (SD)] | 6.6 (7.3) | 6.1 (6.5) |
| History of genital ulcers [n (%)] | 139 (87.4) | 146 (91.8) |
| History of skin lesions [n (%)] | 155 (97.5) | 155 (97.5) |
| History of arthralgia [n (%)] | 109 (68.6) | 99 (62.3) |
| History of arthritis [n (%)] | 44 (27.7) | 38 (23.9) |
bid twice daily, BMI body mass index, BSA body surface area, DLQI Dermatology Life Quality Index, FAS full analysis set, HAQ-DI Health Assessment Questionnaire-Disability Index, ITT intent to treat, PASI Psoriasis Area and Severity Index, PsA psoriatic arthritis, SF-36v2 36-Item Short Form Survey version 2, SJC swollen joint count, sPGA static Physician Global Assessment, SD standard deviation, TJC tender joint count, VAS visual analog scale
a Includes PSOR-005, ESTEEM 1, ESTEEM 2, LIBERATE, PSOR-011, UNVEIL, ADVANCE, and STYLE
bIncludes PALACE 1, PALACE 2, PALACE 3, PALACE 4, and ACTIVE. For PsA studies, the FAS population is selected, which is consistent with the definition of ITT for psoriasis studies
cIncludes BCT-001 and RELIEF. Behçet’s syndrome manifestations collected at the screening and randomization visits are summarized in this table.
A total of 4183 patients were exposed to apremilast 30 mg bid for up to 260 weeks
Common Treatment-Emergent Adverse Events
During the placebo-controlled period, 1780/2673 patients (66.6%) in the apremilast group and 1113/2084 (53.4%) in the placebo group reported one or more TEAEs (Table 3). The most common TEAEs (in ≥ 5% of patients in either group) during the placebo-controlled period were diarrhea, nausea, upper respiratory tract infection, nasopharyngitis, and headache (Table 3). Gastrointestinal TEAEs (including diarrhea or nausea) began mostly within the first 1–2 weeks of apremilast treatment and usually resolved within 30 days. Most TEAEs of diarrhea, nausea, and vomiting were mild or moderate; ≤ 0.3% of patients who reported these gastrointestinal events experienced severe events. Rates of TEAEs, including the most common TEAEs, during the apremilast-exposure period are presented in Table 3, and by year during the apremilast-exposure period in Online Resource 4. Most TEAEs were mild to moderate in both the placebo-controlled (96.6%) and apremilast-exposure (91.6%) periods.
Table 3.
Overview of safety and commonly reported TEAEs
| Placebo-controlled period | All apremilast exposure | |||||
|---|---|---|---|---|---|---|
| Placebo [n = 2084] 622.2 patient-years | Apremilast 30 mg bid [n = 2673] 848.8 patient-years | Apremilast 30 mg bid [n = 4183] 6788.0 patient-years | ||||
| n (%) | EAIR/100 patient-years | n (%) | EAIR/100 patient-years | n (%) | EAIR/100 patient-years | |
| Any TEAE | 1113 (53.4) | 279.1 | 1780 (66.6) | 433.5 | 3265 (78.1) | 179.5 |
| Common TEAEs (≥5% of patients) | ||||||
| Diarrhea | 123 (5.9) | 20.6 | 481 (18.0) | 66.1 | 759 (18.1) | 13.1 |
| Nausea | 115 (5.5) | 19.1 | 432 (16.2) | 58.5 | 665 (15.9) | 11.3 |
| Headache | 121 (5.8) | 20.2 | 282 (10.5) | 36.0 | 470 (11.2) | 7.6 |
| URTI | 96 (4.6) | 15.8 | 178 (6.7) | 21.7 | 537 (12.8) | 9.0 |
| Nasopharyngitis | 93 (4.5) | 15.3 | 153 (5.7) | 18.6 | 491 (11.7) | 8.1 |
| Arthralgia | 39 (1.9) | 6.3 | 53 (2.0) | 6.3 | 227 (5.4) | 3.5 |
| Hypertension | 46 (2.2) | 7.5 | 50 (1.9) | 6.0 | 211 (5.0) | 3.3 |
A TEAE is an adverse event with a start date on or after the date of the first dose of apremilast 30 mg bid and no later than 28 days after the last dose of apremilast 30 mg bid. Each patient is counted once for each applicable category. Patient incidence is 100 times the number (n) of patients reporting the event divided by (m) the number of patients with treatment duration less than or equal to the lower bound of the exposure interval
bid twice daily, EAIR exposure-adjusted incidence rate, TEAEs treatment-emergent adverse events, URTI upper respiratory tract infection
Serious TEAEs
The incidence of serious TEAEs was low and similar in the apremilast and placebo groups during the placebo-controlled period (Table 4). Serious TEAEs (in two or more patients in the apremilast or placebo groups) during the placebo-controlled period were abdominal pain, acute pancreatitis, angina pectoris, atrial fibrillation, Behçet’s syndrome manifestations, congestive cardiac failure, cholelithiasis, hypertensive crisis, noncardiac chest pain, pneumonia, pregnancy, psoriatic arthropathy, and syncope (Table 4). Rates of serious TEAEs during the apremilast-exposure period are presented in Table 4, and by year during the apremilast-exposure period in Online Resource 5. Rates of serious TEAEs remained low across apremilast-exposure periods. Three deaths occurred during the placebo-controlled period (apremilast: n = 1; placebo: n = 2), and nine deaths occurred throughout all apremilast exposure, including the death during the placebo-controlled period. An additional death occurred 4 months after the last study dose and was not treatment-emergent. Descriptions of deaths that occurred during the study (e.g., indication, relatedness to study drug) are provided in Online Resource 6. One death that occurred was suspected by the investigator to be related to apremilast; a 30-year-old woman experienced lung congestion and bilateral edema consistent with cardiac failure on Day 111 of the placebo-controlled period after being treated with apremilast for 104 days.
Table 4.
Serious TEAEs
| Placebo-controlled period | All apremilast exposure | |||||
|---|---|---|---|---|---|---|
| Placebo [n = 2084] 622.2 patient-years | Apremilast 30 mg bid [n = 2673] 848.8 patient-years | Apremilast 30 mg bid [n = 4183] 6788.0 patient-years | ||||
| n (%) | EAIR/100 patient-years | n (%) | EAIR/100 patient-years | n (%) | EAIR/100 patient-years | |
| Any serious TEAE | 55 (2.6) | 8.9 | 58 (2.2) | 6.9 | 392 (9.4) | 6.20 |
| Serious TEAEs (≥ 2 patients) | ||||||
| Abdominal pain | 0 (0) | 0.0 | 2 (0.1) | 0.2 | 4 (0.1) | 0.06 |
| Acute pancreatitis | 2 (0.1) | 0.3 | 0 (0) | 0.0 | 4 (0.1) | 0.06 |
| Angina pectoris | 2 (0.1) | 0.3 | 1 (< 0.1) | 0.1 | 7 (0.2) | 0.10 |
| Atrial fibrillation | 0 (0) | 0.0 | 2 (0.1) | 0.2 | 7 (0.2) | 0.10 |
| Behçet’s syndrome manifestations | 2 (0.1) | 0.3 | 1 (< 0.1) | 0.1 | 5 (0.1) | 0.07 |
| Congestive cardiac failure | 2 (0.1) | 0.3 | 0 (0) | 0.0 | 1 (< 0.1) | 0.01 |
| Cholelithiasis | 1 (< 0.1) | 0.2 | 2 (0.1) | 0.2 | 8 (0.2) | 0.12 |
| Hypertensive crisis | 2 (0.1) | 0.3 | 0 (0) | 0.0 | 1 (< 0.1) | 0.01 |
| Noncardiac chest pain | 2 (0.1) | 0.3 | 0 (0) | 0.0 | 6 (0.1) | 0.09 |
| Pneumonia | 2 (0.1) | 0.3 | 4 (0.1) | 0.5 | 12 (0.3) | 0.18 |
| Pregnancy | 0 (0) | 0.0 | 2 (0.1) | 0.2 | 2 (< 0.1) | 0.03 |
| Psoriatic arthropathy | 3 (0.1) | 0.5 | 2 (0.1) | 0.2 | 14 (0.3) | 0.21 |
| Syncope | 2 (0.1) | 0.3 | 0 (0) | 0.0 | 2 (< 0.1) | 0.03 |
A TEAE is an adverse event with a start date on or after the date of the first dose of apremilast 30 mg bid and no later than 28 days after the last dose of apremilast 30 mg bid. Each patient is counted once for each applicable category. Patient incidence is 100 times the number (n) of patients reporting the event divided by (m) the number of patients with treatment duration less than or equal to the lower bound of the exposure interval.
bid twice daily, EAIR exposure-adjusted incidence rate, TEAEs treatment-emergent adverse events
TEAEs Leading to Study Discontinuation
Few TEAEs led to study discontinuation in the apremilast and placebo groups during the placebo-controlled period (Online Resource 7). The rates of TEAEs leading to discontinuation during the apremilast-exposure period are presented by year in Online Resource 7. TEAEs leading to discontinuation of five or more patients in the apremilast or placebo groups during the placebo-controlled period were nausea, diarrhea, vomiting, upper abdominal pain, fatigue, headache, dizziness, migraine, depression, psoriasis, and Behçet’s syndrome (Online Resource 7). Throughout all apremilast exposure, TEAEs leading to discontinuation in ≥30 patients were diarrhea, nausea, and headache.
TEAEs of Special Interest
TEAEs of special interest during the placebo-controlled period and all apremilast exposure are shown in Table 5. Incidence of all events was low and similar between groups. In the placebo-controlled period, MACE occurred in 0.1% of patients in both the apremilast and placebo groups; similarly, serious opportunistic infections were reported in 0.1% of both apremilast and placebo patients (Table 5). Malignancies (apremilast: 0.3%; placebo: 0.4%), serious infections (apremilast: 0.3%; placebo: 0.4%), and thrombotic events (apremilast: < 0.1%; placebo: 0.0%) occurred at low rates during the placebo-controlled period. Rates remained low throughout all apremilast exposure (Table 5). Rates of depression were low, but slightly higher in apremilast patients (placebo-controlled period: [apremilast: 1.4%; placebo: 0.6%]; all apremilast exposure: 2.8%) (Table 5). The incidence of suicidal ideation/behavior was very low in both periods (placebo-controlled period: [apremilast: < 0.1%; placebo: 0.0%]; all apremilast exposure: 0.1%) (Table 5). EAIRs per 100 patient-years remained < 2 for every TEAE of special interest throughout exposure, except depression in the apremilast group during the placebo-controlled period (4.51), and were lower compared with placebo for malignancies (apremilast: 0.94; placebo: 1.45), serious infections (apremilast: 0.83; placebo: 1.45), and serious opportunistic infections (apremilast: 0.24; placebo: 0.48) (Table 5).
Table 5.
TEAEs of special interest per 100 patient-years in the placebo-controlled period and up to Week 260 in all apremilast-exposed patients
| TEAEs of special interest | Placebo-controlled period | All apremilast exposure | ||||
|---|---|---|---|---|---|---|
| Placebo [n = 2084] 622.2 patient-years | Apremilast 30 mg bid [n = 2673] 848.8 patient-years | Apremilast 30 mg bid [n = 4183] 6788.0 patient-years | ||||
| n (%) | EAIR/100 patient-years | n (%) | EAIR/100 patient-years | n (%) | EAIR/100 patient-years | |
| Depression | 12 (0.6) | 1.94 | 38 (1.4) | 4.51 | 118 (2.8) | 1.78 |
| Suicidal ideation/behavior | 0 (0) | 0.0 | 1 (< 0.1) | 0.12 | 3 (0.1) | 0.04 |
| MACEa | 2 (0.1) | 0.32 | 3 (0.1) | 0.35 | 20 (0.5) | 0.30 |
| Malignancies | 9 (0.4) | 1.45 | 8 (0.3) | 0.94 | 70 (1.7) | 1.0 |
| Nonmelanoma skin cancer | 7 (0.3) | 1.13 | 6 (0.2) | 0.71 | 32 (0.8) | 0.48 |
| Lymphomas | 0 (0) | 0.0 | 0 (0) | 0.0 | 2 (<0.1) | 0.03 |
| Serious infectionsb | 9 (0.4) | 1.45 | 7 (0.3) | 0.83 | 74 (1.8) | 1.10 |
| Serious opportunistic infections | 3 (0.1) | 0.48 | 2 (0.1) | 0.24 | 14 (0.3) | 0.21 |
| Thrombotic eventsc | 0 (0) | 0.0 | 1 (<0.1) | 0.12 | 7 (0.2) | 0.10 |
A TEAE is an adverse event with a start date on or after the date of the first dose of apremilast 30 mg bid and no later than 28 days after the last dose of apremilast 30 mg bid. Each patient is counted once for each applicable category. Patient incidence is 100 times the number (n) of patients reporting the event divided by N, the number of subjects exposed to apremilast 30 mg bid. Patients started treatment with apremilast at Week 0, Week 12, Week 16, or Week 24 depending on early escape and re-randomization in the respective studies
AE adverse event, bid twice daily, EAIR exposure-adjusted incidence rate, MACE major adverse cardiac event, TEAEs treatment-emergent adverse events
aIdentified through medical review based on prespecified preferred term search from the AE database and defined as myocardial infarction, acute myocardial infarction, cerebrovascular accident, cerebral infarction, brain stem stroke, hemorrhagic stroke, or ischemic stroke
bIdentified through medical review based on System Organ Class Infections and Infestations from the AE database
cDefined as deep vein thrombosis or pulmonary embolism
Subgroup Analysis
Rates of TEAEs during the placebo-controlled period were similar in Japan (apremilast: 55.8%; placebo: 48.1%) and the rest of the world (apremilast: 66.1%; placebo: 58.2%). During the apremilast-exposure period, overall rates of TEAEs were similar in North America (75.5%), Europe (82.4%), Japan (79.4%), and the rest of the world (82.4%).
Rates of TEAEs during apremilast exposure were similar between patients with psoriasis (74.6%), psoriatic arthritis (84.0%), or Behçet’s syndrome (86.8%). Patients with psoriatic arthritis had a slightly higher rate of serious TEAEs (16.5%) compared with patients with psoriasis (6.4%) or Behçet’s syndrome (8.0%).
Discussion
In this pooled, long-term analysis of 15 apremilast clinical trials including > 4000 patients with 6788 patient-years of apremilast exposure, apremilast 30 mg twice daily was well tolerated in patients with plaque psoriasis, psoriatic arthritis, or Behçet’s syndrome. The pooled analyses in the placebo-controlled and apremilast-exposure periods demonstrate that apremilast is well tolerated during short- and long-term exposure. Rates of serious TEAEs remained low throughout apremilast treatment. No new safety signals were identified. These long-term results contribute to the known safety profile of apremilast [6–16].
Psoriasis, psoriatic arthritis, and Behçet’s syndrome are chronic systemic diseases associated with comorbidities and increased risk of cardiovascular and thrombotic events [19–22]. It is important to evaluate the long-term safety of systemic treatments in patients who are at risk for comorbid conditions. MACE incidence was low throughout treatment and was nearly identical between groups in the placebo-controlled period. This was consistent with the low rates of MACE observed in a French cohort study of patients with psoriatic arthritis treated with apremilast or a biologic disease-modifying rheumatic agent, as well as in the pooled analysis of the ESTEEM 1 and 2 trials in psoriasis patients [23, 24]. Similarly, our analysis was consistent with published findings that MACE risk in patients treated with apremilast was not significantly increased compared with patients newly treated with tumor necrosis factor (TNF) inhibitors [23]. Another cohort study found that patients with psoriatic arthritis who were treated with apremilast had lower rates of myocardial infarction and stroke versus those treated with TNF inhibitors or interleukin inhibitor biologics [25]. This pooled analysis demonstrated that rates of other TEAEs of special interest, including malignancies, serious infections, serious opportunistic infections, and thrombotic events, were low and similar between placebo and apremilast patients, demonstrating that apremilast exposure did not increase the risk of these events.
At screening, > 10% of patients with psoriasis or psoriatic arthritis reported a history of depression (Online Resource 3). During the placebo-controlled period, rates of depression were slightly higher in apremilast patients (4.51/100 patient-years) versus placebo patients (1.94/100 patient-years) but still low overall (1.78/100 patient-years all apremilast exposure). These findings are consistent with a study that concluded that rates of anxiety and depression were similar among patients treated with apremilast and those treated with other systemic psoriasis or psoriatic arthritis treatments [26].
Diarrhea and nausea were the most common TEAEs among patients treated with apremilast, occurred within the first 2 weeks of treatment, and resolved within 30 days. During the phase II Behçet’s syndrome study, a single reduction in apremilast dose was allowed to mitigate gastrointestinal adverse effects [15].
Pooled safety findings were consistent with prior studies of apremilast in patients with psoriasis, psoriatic arthritis, and Behçet’s syndrome, including the pivotal ESTEEM, PALACE, and RELIEF studies; common TEAEs were consistent with those previously reported and were mild-to-moderate in severity [6–16, 27–30].
Other treatments for plaque psoriasis, psoriatic arthritis, and Behçet’s syndrome may be associated with safety risks not observed with apremilast. For example, JAK inhibitors are systemic treatments that have been associated with liver abnormalities, which are not commonly reported with apremilast [31]. JAK inhibitors also pose a potential risk of thrombotic events, malignancies, and other serious cardiovascular events, whereas this analysis showed low incidence after apremilast exposure [3, 31]. Unlike apremilast, which had low rates of serious infections and serious opportunistic infections, some biologics may be associated with higher risk of infections with long-term use [32]. Similarly, the JAK inhibitors tofacitinib and upadacitinib, which are approved for psoriatic arthritis treatment, have a boxed warning for serious infections [33, 34]. Findings were consistent with an observational cohort study which found that apremilast had a significantly decreased risk of infection compared with both methotrexate and adalimumab [35]. Of note, in a retrospective cohort study, while patients with psoriasis were found to have 18% greater odds of incident coronavirus disease 2019 (COVID-19), apremilast use was associated with decreased odds (adjusted odds ratio: 0.70) of incident COVID-19 compared with patients receiving topical therapy only [36].
While methods, population, sample size, and study length vary and make direct comparisons difficult, rates of discontinuation due to AEs reported in clinical trials with tofacitinib, upadacitinib, secukinumab, ixekizumab, and guselkumab were generally comparable with rates observed in this pooled analysis with apremilast. In an analysis of tofacitinib in patients with psoriatic arthritis up to Month 36, 6.4% of patients had discontinued the trial due to AEs, for an incidence rate per 100 patient-years of 3.8 [37]. In an analysis of 907 patients with psoriatic arthritis treated with upadacitinib, the EAIR per 100 patient-years of AEs leading to discontinuation was 5.4 [38]. In the 5-year FUTURE 1 study of 587 patients with psoriatic arthritis treated with secukinumab, 8.3% had discontinued due to AEs [39]. Similarly, in the 5-year FUTURE 2 study of 299 patients treated with secukinumab, 8.4% discontinued treatment due to AEs [40]. In the UNCOVER-3 study of ixekizumab in 385 patients with psoriasis, the most common reason for discontinuation at Week 264 was AEs (10.1%) [41], while in the VOYAGE 1 and 2 studies of 1721 patients treated with guselkumab, 5.8% of patients had discontinued due to AEs by Week 252 (1.45/100 patient-years) [42].
Safety findings in the current pooled analysis remained consistent across indications, regions, and treatment duration. No differences in the pattern of safety were observed in the regional subgroup analysis.
Strengths of this pooled safety analysis include data from blinded, randomized, controlled short- to mid-term phases, a large sample size, and long-term data. Limitations include the inability to extrapolate placebo-controlled data to real-world settings, the observational design of extension phases, and the inability to control for confounders, such as the heterogeneity of patient cohorts.
Conclusion
This pooled analysis of 15 placebo-controlled clinical studies, including 4183 patients treated with apremilast 30 mg twice daily, confirms the safety of long-term apremilast use in patients with plaque psoriasis, active psoriatic arthritis, or oral ulcers associated with Behçet’s syndrome. EAIRs for serious events and events of special interest were low (< 1%) in patients treated with apremilast 30 mg twice daily despite significant exposure. Apremilast provides a therapeutic option with established long-term safety and a favorable benefit–risk profile for patients with psoriatic arthritis, psoriasis, or Behçet’s syndrome requiring chronic, systemic therapy.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
Writing support was funded by Amgen Inc. and provided by Christina Mulvihill, PharmD, of Peloton Advantage, LLC, an OPEN Health company, and Dawn Nicewarner, PhD, an employee of and stockholder in Amgen Inc.
Declarations
Funding
This study was sponsored by Amgen Inc.
Compliance with ethical standards
All studies included in this pooled analysis were conducted in accordance with the general ethical principles outlined in the Declaration of Helsinki and principles of Good Clinical Practice per the International Council for Harmonisation Guidelines and local regulations.
Conflicts of interest/competing interests
Philip J. Mease: AbbVie, Amgen Inc., Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, Sun, and UCB—grant/research support and consultant; Boehringer Ingelheim, GlaxoSmithKline—consultant; AbbVie, Amgen Inc., Eli Lilly, Janssen, Novartis, Pfizer, and UCB—speakers bureau. Gülen Hatemi: AbbVie, Amgen Inc., and Celgene Corporation—grant/research support; AbbVie, Boehringer Ingelheim, Novartis, and UCB Pharma—speaker. Maria Paris, Sue Cheng, Peter Maes, Wendy Zhang, Rebecca Shi, Andrea Flower, Hernan Picard: Amgen Inc.—employees and stockholders. Linda Stein Gold: AbbVie, Amgen, Arcutis, Celgene Corporation, Dermira, Dermavant, Eli Lilly, Galderma, LEO Pharma, Novartis, Pfizer, Regeneron, Sanofi Genzyme, UCB, and Valeant—honoraria, grants, and/or research funding as a speaker, investigator, and/or advisory board member.
Ethics approval
Studies received approval from an Institutional Review Board or Ethics Committee prior to commencement.
Consent to participate
Patients provided informed consent prior to study entry.
Consent for publication
Not applicable.
Availability of data and material
Qualified researchers may request data from Amgen clinical studies. Complete details are available at http://www.amgen.com/datasharing.
Code availability
Not applicable.
Authors' contributions
WZ, PM, and SC contributed to the study conception and design. Patient data collection was performed by PJM, LSG, and GH. Data analysis and interpretation were performed by HP, RS, AF, MP, and MC. All authors commented on previous versions of the manuscript, and all authors read and approved the final version of the manuscript.
Contributor Information
Philip J. Mease, Email: pmease@philipmease.com
Andrea Flower, Email: aflower@amgen.com.
References
- 1.Otezla [package insert]. Thousand Oaks, CA: Amgen, Inc.; 2021. https://www.pi.amgen.com/-/media/Project/Amgen/Repository/pi-amgen-com/Otezla/otezla_pi_english.pdf.
- 2.Schafer P. Apremilast mechanism of action and application to psoriasis and psoriatic arthritis. Biochem Pharmacol. 2012;83(12):1583–1590. doi: 10.1016/j.bcp.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 3.US FDA. FDA requires warnings about increased risk of serious heart-related events, cancer, blood clots, and death for JAK inhibitors that treat certain chronic inflammatory conditions. 2021. https://www.fda.gov/drugs/drug-safety-and-availability/fda-requires-warnings-about-increased-risk-serious-heart-related-events-cancer-blood-clots-and-death. Accessed 10 Dec 2021.
- 4.European Medicines Agency. Otezla Summary of Opinion (post authorisation). 2020. https://www.ema.europa.eu/en/documents/smop/chmp-post-authorisation-summary-positive-opinion-otezla-ii-29_en.pdf. Accessed 20 April 2020.
- 5.European Medicines Agency. Otezla EPAR summary for the public. 2015. https://www.ema.europa.eu/en/documents/overview/otezla-epar-summary-public_en.pdf. Accessed 10 Dec 2021.
- 6.Papp K, Cather JC, Rosoph L, et al. Efficacy of apremilast in the treatment of moderate to severe psoriasis: a randomised controlled trial. Lancet. 2012;380:738–746. doi: 10.1016/S0140-6736(12)60642-4. [DOI] [PubMed] [Google Scholar]
- 7.Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM 1]) J Am Acad Dermatol. 2015;73(1):37–49. doi: 10.1016/j.2015.03.049. [DOI] [PubMed] [Google Scholar]
- 8.Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate to severe plaque psoriasis over 52 weeks: a phase III, randomized, controlled trial (ESTEEM 2) Br J Dermatol. 2015;173(6):1387–1399. doi: 10.1111/bjd.14164. [DOI] [PubMed] [Google Scholar]
- 9.Stein Gold L, Papp K, Leonardi C, et al. Efficacy and safety of apremilast in patients with mild to moderate plaque psoriasis: results of a phase 3, multicenter, randomized, double-blind, placebo-controlled trial. J Am Acad Dermatol. 2022;86(1):77–85. doi: 10.1016/j.jaad.2021.07.040. [DOI] [PubMed] [Google Scholar]
- 10.Van Voorhees AS, Gold LS, Lebwohl M, et al. Efficacy and safety of apremilast in patients with moderate to severe plaque psoriasis of the scalp: results of a phase 3b, multicenter, randomized, placebo-controlled, double-blind study. J Am Acad Dermatol. 2020;83(1):96–103. doi: 10.1016/j.jaad.2020.01.072. [DOI] [PubMed] [Google Scholar]
- 11.Kavanaugh A, Mease PJ, Gomez-Reino JJ, et al. Longterm (52-week) results of a phase III randomized, controlled trial of apremilast in patients with psoriatic arthritis. J Rheumatol. 2015;42(3):479–488. doi: 10.3899/jrheum.140647. [DOI] [PubMed] [Google Scholar]
- 12.Cutolo M, Myerson GE, Fleischmann R, et al. A phase III, randomized, controlled trial of apremilast in patients with psoriatic arthritis: results of the PALACE 2 trial. J Rheumatol. 2016;43(9):1724–1734. doi: 10.3899/jrheum.151376. [DOI] [PubMed] [Google Scholar]
- 13.Edwards CJ, Blanco FJ, Crowley J, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with psoriatic arthritis and current skin involvement: a phase III, randomised, controlled trial (PALACE 3) Ann Rheum Dis. 2016;75(6):1065–1073. doi: 10.1136/annrheumdis-2015-207963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells AF, Edwards CJ, Kivitz AJ, et al. Apremilast monotherapy in DMARD-naive psoriatic arthritis patients: results of the randomized, placebo-controlled PALACE 4 trial. Rheumatology (Oxford) 2018;57(7):1253–1263. doi: 10.1093/rheumatology/key032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatemi G, Melikoglu M, Tunc R, et al. Apremilast for Behçet’s syndrome: A phase 2, placebo-controlled study. N Engl J Med. 2015;372(16):1510–1518. doi: 10.1056/NEJMoa1408684. [DOI] [PubMed] [Google Scholar]
- 16.Hatemi G, Mahr A, Ishigatsubo Y, et al. Trial of apremilast for oral ulcers of Behçet’s syndrome. N Engl J Med. 2019;381(20):1918–1928. doi: 10.1056/NEJMoa1816594. [DOI] [PubMed] [Google Scholar]
- 17.Yazici H, Seyahi E, Hatemi G, Yazici Y. Behçet’s syndrome: a contemporary view. Nat Rev Rheumatol. 2018;14(2):119. doi: 10.1038/nrrheum.2018.3. [DOI] [PubMed] [Google Scholar]
- 18.Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376(10):957–970. doi: 10.1056/NEJMra1505557. [DOI] [PubMed] [Google Scholar]
- 19.Yamazaki F. Psoriasis: comorbidities. J Dermatol. 2021;48(6):732–740. doi: 10.1111/1346-8138.15840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahn H, Lee D, Lee SY, et al. Increased cardiovascular risk and all-cause death in patients with Behçet’s disease: a nationwide population-based dynamic cohort study. J Rheumatol. 2020;47(6):903–908. doi: 10.3899/jrheum.190408. [DOI] [PubMed] [Google Scholar]
- 21.Ogdie A, Schwartzman S, Husni ME. Recognizing and managing comorbidities in psoriatic arthritis. Curr Opin Rheumatol. 2015;27(2):118–126. doi: 10.1097/BOR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 22.Eder L, Wu Y, Chandran V, Cook R, Gladman DD. Incidence and predictors for cardiovascular events in patients with psoriatic arthritis. Ann Rheum Dis. 2016;75(9):1680–1686. doi: 10.1136/annrheumdis-2015-207980. [DOI] [PubMed] [Google Scholar]
- 23.Pina Vegas L, Le Corvoisier P, Penso L, Paul M, Sbidian E, Claudepierre P. Risk of major adverse cardiovascular events in patients initiating biologics/apremilast for psoriatic arthritis: a nationwide cohort study. Rheumatology (Oxford) 2022;61:1589–1599. doi: 10.1093/rheumatology/keab522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crowley J, Thaci D, Joly P, et al. Long-term safety and tolerability of apremilast in patients with psoriasis: pooled safety analysis for ≥156 weeks from 2 phase 3, randomized, controlled trials (ESTEEM 1 and 2) J Am Acad Dermatol. 2017;77(2):310–317. doi: 10.1016/j.jaad.2017.01.052. [DOI] [PubMed] [Google Scholar]
- 25.Persson R, Hagberg KW, Qian Y, Vasilakis-Scaramozza C, Jick S. The risk of myocardial infarction, stroke, and revascularization among patients with psoriasis treated with apremilast compared with biologics and disease-modifying antirheumatic drugs: a cohort study in the US MarketScan database. J Am Acad Dermatol. 2020;83(1):271–274. doi: 10.1016/j.jaad.2020.03.043. [DOI] [PubMed] [Google Scholar]
- 26.Vasilakis-Scaramozza C, Persson R, Hagberg KW, Jick S. The risk of treated anxiety and treated depression among patients with psoriasis and psoriatic arthritis treated with apremilast compared to biologics, DMARDs and corticosteroids: a cohort study in the United States MarketScan database. J Eur Acad Dermatol Venereol. 2020;34(8):1755–1763. doi: 10.1111/jdv.16231. [DOI] [PubMed] [Google Scholar]
- 27.Nash P, Ohson K, Walsh J, et al. Early and sustained efficacy with apremilast monotherapy in biological-naive patients with psoriatic arthritis: a phase IIIB, randomised controlled trial (ACTIVE) Ann Rheum Dis. 2018;77:690–698. doi: 10.1136/annrheumdis-2017-211568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strober B, Bagel J, Lebwohl M, et al. Efficacy and safety of apremilast in patients with moderate plaque psoriasis with lower BSA: week 16 results from the UNVEIL study. J Drugs Dermatol. 2017;16(8):801–808. [PubMed] [Google Scholar]
- 29.Ohtsuki M, Okubo Y, Komine M, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in the treatment of Japanese patients with moderate to severe plaque psoriasis: efficacy, safety and tolerability results from a phase 2b randomized controlled trial. J Dermatol. 2017;44(8):873–884. doi: 10.1111/1346-8138.13829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reich K, Gooderham M, Green L, et al. The efficacy and safety of apremilast, etanercept, and placebo, in patients with moderate to severe plaque psoriasis: 52-week results from a phase 3b, randomized, placebo-controlled trial (LIBERATE) J Eur Acad Dermatol Venereol. 2017;31(3):507–517. doi: 10.1111/jdv.14015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kerschbaumer A, Smolen JS, Nash P, et al. Points to consider for the treatment of immune-mediated inflammatory diseases with Janus kinase inhibitors: a systematic literature research. RMD Open. 2020;6(3):e001374. doi: 10.1136/rmdopen-2020-001374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Penso L, Dray-Spira R, Weill A, Pina Vegas L, Zureik M, Sbidian E. Association between biologics use and risk of serious infection in patients with psoriasis. JAMA Dermatol. 2021;157(9):1056–1065. doi: 10.1001/jamadermatol.2021.2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xeljanz [package insert]. New York, NY: Pfizer Labs; 2021. https://labeling.pfizer.com/ShowLabeling.aspx?id=959.
- 34.Rinvoq [package insert] North Chicago, IL: AbbVie Inc.; 2022. https://www.rxabbvie.com/pdf/rinvoq_pi.pdf.
- 35.Dommasch ED, Kim SC, Lee MP, Gagne JJ. Risk of serious infection in patients receiving systemic medications for the treatment of psoriasis. JAMA Dermatol. 2019;155(10):1142–1152. doi: 10.1001/jamadermatol.2019.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu JJ, Liu J, Thatiparthi A, Martin A, Egeberg A. The risk of COVID-19 in patients with psoriasis: a retrospective cohort study. J Am Acad Dermatol. 2022;87(6):1395–1398. doi: 10.1016/j.jaad.2022.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nash P, Coates LC, Kivitz AJ, et al. Safety and efficacy of tofacitinib in patients with active psoriatic arthritis: interim analysis of OPAL balance, an open-label, long-term extension study. Rheumatol Ther. 2020;7(3):553–580. doi: 10.1007/s40744-020-00209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burmester GR, Cohen SB, Winthrop KL, et al. Safety profile of upadacitinib over 15 000 patient-years across rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and atopic dermatitis. RMD Open. 2023;9(1):e002735. doi: 10.1136/rmdopen-2022-002735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mease PJ, Kavanaugh A, Reimold A, et al. Secukinumab provides sustained improvements in the signs and symptoms of psoriatic arthritis: final 5-year results from the phase 3 FUTURE 1 study. ACR Open Rheumatol. 2020;2(1):18–25. doi: 10.1002/acr2.11097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McInnes IB, Mease PJ, Kivitz AJ, et al. Long-term efficacy and safety of secukinumab in patients with psoriatic arthritis: 5-year (end-of-study) results from the phase 3 FUTURE 2 study. Lancet Rheumatol. 2020;2(4):e227–e235. doi: 10.1016/S2665-9913(20)30036-9. [DOI] [PubMed] [Google Scholar]
- 41.Blauvelt A, Lebwohl MG, Mabuchi T, et al. Long-term efficacy and safety of ixekizumab: a 5-year analysis of the UNCOVER-3 randomized controlled trial. J Am Acad Dermatol. 2021;85(2):360–368. doi: 10.1016/j.jaad.2020.11.022. [DOI] [PubMed] [Google Scholar]
- 42.Blauvelt A, Tsai TF, Langley RG, et al. Consistent safety profile with up to 5 years of continuous treatment with guselkumab: pooled analyses from the phase 3 VOYAGE 1 and VOYAGE 2 trials of patients with moderate-to-severe psoriasis. J Am Acad Dermatol. 2022;86(4):827–834. doi: 10.1016/j.jaad.2021.11.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.