Abstract
Introduction
The development and spread of innovation are known challenges in health care. The US Veterans Health Administration (VHA) created a “Shark Tank”-style competition directed at frontline employees. In this annual, systemwide competition, employees submit innovations to the competition, and winning innovations receive support for implementation in other facilities.
Method
A multiple case study design was used to understand facility engagement in the competition, and the relationship between engagement and organizational conditions. The authors created a typology to describe the relationship between facility engagement in the competition and organizational conditions for innovation.
Results
Overall, there was high participation in the VHA’s competition across all 130 facilities. The authors identified 7 mutually exclusive types of facility engagement.
Discussion
As expected, facilities with the most established conditions for innovation were the most engaged in the competition. Additionally, other facilities had various ways to be involved. Consequently, there may be benefit to the VHA tailoring how they work with facilities, based on organizational conditions. Larger facilities with ongoing research and more resources may be more suited to develop innovations, whereas smaller facilities could benefit from a focus on adoption.
Conclusion
These insights are valuable to the VHA and can be used by other health care systems to tailor innovation programs and allocate resources based on diverse needs across a vast health care system.
Keywords: diffusion of innovation, organizational innovation, health care system
Introduction
The development and spread of innovation is a known challenge in health care.1,2 Innovation includes the development, adoption, and spread of new ideas and services to improve health care delivery.1 Stymied innovation can have negative effects on health care cost,3 employee job satisfaction,4 and care quality.1,2,5,6 Improved innovation can have broad direct impacts on the quadruple aim: enhancing patient experience, improving population health, reducing costs, and improving staff experiences.7,8 Barriers to innovation include limited resources, insufficient leadership involvement or support,6 and limited knowledge and training.9 Strategies, such as employee empowerment, have been shown to decrease perceived barriers to innovation.10
To overcome barriers to innovation, the US Department of Veterans Affairs (VA) created the Diffusion of Excellence (DoE) Initiative. In 2015, the DoE started a national “Shark Tank”-style competition to encourage frontline Veterans Health Administration (VHA) employee engagement in innovation.11–13 In this annual, systemwide competition, frontline staff are invited to submit innovations to the competition that have previously been implemented in 1 or more VHA facilities.12 DoE practices include innovations supported by evidence from research studies and administrative or clinical experience and strive to address patient, employee, and/or facility needs. Applications go through several rounds of expert review, and a select few are chosen to be presented to facility directors who act as “Sharks.”13 Sharks bid on innovations they want to implement at their facilities and winning innovations receive “Promising Practice” designation along with support from the bidding facility (eg, money, staffing) and the DoE to spread their innovations.12–14 Promising Practices from the VHA’s competition have been successfully implemented with positive effects on the quadruple aim in enhancing patient experience,12,15 improving population health through telemonitoring,16 reducing costs for caregivers,17 and improving staff satisfaction.12 For example, a patient-centered direct scheduling system decreased wait times and improved patient and clinician satisfaction.12 These types of innovations rely on ground-up change and solutions; thus, it is essential to ensure widespread employee engagement in the competition. Further information on the competition and the DoE can be found in other publications.11–14,18,19
The VHA is not the only health care system to use innovation contests to engage frontline employees,20,21 but few others are broadly focused, national, systemwide efforts. The VHA is the largest integrated health care system in the United States, with 170 VA medical centers nationally.22 Consequently, it is a challenge to engage the diverse range of facilities in national program efforts like this one. Previous research has shown that organizational conditions are key to organizational innovation.23 Organizational conditions that predict an organization’s ability to produce, adopt, and spread innovation include facility size, resources, and knowledge utilization and networks.23 Use of experts has also been identified as a key factor in organizational innovation.24 In this case, as part of the broader VHA Innovation Ecosystem, facilities can apply to be a part of the Innovators Network (iNET) to receive support, such as an innovation specialist, as well as skills and development training in innovation for facility staff.25
The DoE has a history of working with embedded VHA researchers as a means of continuously learning and improving the program.25 Previous evaluations of the DoE have shown success in implementation and sustainment of Promising Practices13,14 and positive experiences from participants at the frontline staff and facility director levels.18 Given the size and complexity of the VHA health care system, it is important to understand variation in engagement across facilities to best position the VHA’s competition for ongoing success. This paper presents the results of a program evaluation, conducted in partnership with the DoE, with the goal of understanding 1) variation in engagement in the competition across VHA facilities and 2) organizational conditions for innovation that may explain that variation.
Methods
Study design
A multiple case study design was used to understand VHA facility competition engagement, as well as the relationship between engagement and organizational conditions. Case studies in health services research can be used to provide “in-depth, multi-faceted explorations of complex issues in their real-life setting.”26 Each VHA facility was considered a case. There is often debate over how to count VHA facilities; for the purposes of this study, 130 umbrella facilities (VA medical centers) were used, which may include several other hospitals and smaller outpatient clinics. This evaluation has been designated and approved as non-research quality improvement.
Data collection
The authors first compiled a database of the competition engagement status and organizational conditions for innovation of the 130 facilities. Data on engagement was gathered from the clinical operations partner (the DoE) and their contractor and included applications and competition data (winners, sharks, and bids). Facility data (including main VA medical centers and smaller satellite clinics) span 7 competitions (2016–2021). Each facility may include multiple hospitals and satellite clinics; for this study, data from individual clinics was collapsed under the 130 larger facilities. Measures of a facility’s engagement status included whether they were a Promising Practice winner, the number of applications submitted to the competition, and the number of bids placed by facility leadership.
Data on a facility’s organizational conditions for innovation were included using VHA administrative data. Three measures of organizational conditions were used: 1) facility complexity level, 2) presence of a research center, and 3) membership in iNET (ie, the presence of an innovation specialist). Complexity level is an administrative designation containing 5 levels of complexity—3 high complexity ratings, 1 medium complexity rating, and 1 low complexity rating—based on patient risk level and volume, teaching/research presence, and clinical units and services offered. High-complexity facilities have higher patient volume and risk and offer more complex services.22,27 As in previous research,28 the complexity designations were condensed into 2 levels: high complexity (including the 3 highest levels of complexity) and low complexity (including the medium and low levels). Presence of a research center was defined as having 1 or more of the following types of VHA research programs or centers on-site at the facility: Cooperative Studies Program; Geriatric Research Education and Clinical Center; Health Services Research & Development Center of Innovation; Mental Illness Research, Education and Clinical Center (headquarters facility); Quality Enhancement Research Initiative program and/or partnered evaluation; or Rehabilitation Research & Development Center.
Data analysis
First, to assess facility engagement in the competition, the authors conducted descriptive analyses on measures of engagement. Second, to explore variation in engagement and organizational conditions for innovation across facilities, the authors used Kluge’s29 typology methodology, including the following steps: 1) develop type dimensions using a qualitative iterative process, 2) group similar cases along dimensions, 3) analyze meaningful relationships to create types, and 4) characterize those types. The matrix was organized based on 2 major dimensions: engagement and organizational conditions. Initial attributes of the engagement domain included the following: winning Promising Practice (yes or no), number of applications (low or high), and bidding on Promising Practices (yes or no). Number of applications was categorized into low (below average) and high (above average). The organizational conditions domain was based on previous literature regarding organizational conditions impacting innovation and included facility size and resources, knowledge utilization and networks,23 and the use of experts.24 Facility size and resources was measured through facility complexity; knowledge utilization and networks, through the presence of research centers; and the use of experts, through the presence of an innovation specialist (iNET membership). Thus, the organizational conditions domain included the following attributes: facility complexity (high or low/medium), research facility (yes or no), and iNET facility (yes or no). The authors refined the final levels of each dimension through group consensus and grouped cases into the matrix along those dimensions (eg, by removing matrix cells with no cases or condensing cells). Finally, the authors developed an overarching typology to classify cases into groups based on how they were engaging in competition activities and their organizational conditions. The final levels for each dimension are described in this paper.
Dimension 1: Levels of Engagement
The engagement dimension is based on the 3 criteria discussed above (winning Promising Practice [yes or no], number of applications [low or high], and bidding on Promising Practices [yes or no]) and included the following levels: little to no participation, only applications, mostly bidding, bidding and applications, and Promising Practice winners (see Table 1).
Table 1:
Levels of engagement dimension
| Levels of engagement | Promising Practice winner | Bids by facility leadership | Applications |
|---|---|---|---|
| Little or no participation | No | No | Low (below average) |
| Only applications | No | No | High (above average) |
| Mostly bidding | No | Yes | Low (below average) |
| Applications and bidding | No | Yes | High (above average) |
| Promising Practice winner | Yes | — | — |
Dimension 2: Levels of Organizational Conditions for Innovation
The organizational conditions dimension is based on the 3 criteria discussed in Dimension 1 (facility complexity [high or low/medium], research facility [yes or no], and iNET facility [yes or no]), and included the following levels: less established conditions for innovation, somewhat established conditions for innovation, moderately established conditions for innovation, and most established conditions for innovation (see Table 2).
Table 2:
Levels of organizational conditions for innovation dimension
| Levels of organizational conditions | Facility complexity | Research or iNET presence |
|---|---|---|
| Less established | Not/below high (low/medium/none) | Neither/none |
| Somewhat established | Not/below high (low/medium/none) | One or both |
| Moderately established | High | None or one |
| Most established | High | Both |
As a final step in the analytic process, the different types were given descriptive names. The names were designed to invoke an image that would resonate with the operational partner, the DoE. The authors strove for alliteration and consulted a thesaurus when needed.
Results
Facility engagement in the competition
There were 2342 total submissions of innovations (applications for Promising Practices) to the competition from 2016 to 2021. Of 130 VHA facilities, 129 submitted at least 1 innovation to the competition. Each facility submitted an average of 18 applications overall, ranging from none to 88. Forty-two facilities had a winning Promising Practice. The number of Promising Practices per facility ranged from 1 to 6, with 22 (52%) of 42 facilities having more than 1 winning Promising Practice. Promising Practice winning facilities also varied in how many applications they submitted, ranging from 3 to 88 total applications. Eighty-one facilities participated in bidding on innovative practices, with an average of 3.4 bids per facility, ranging from 1 to 34 total bids.
Variation in engagement and organizational conditions for innovation across facilities
Typology
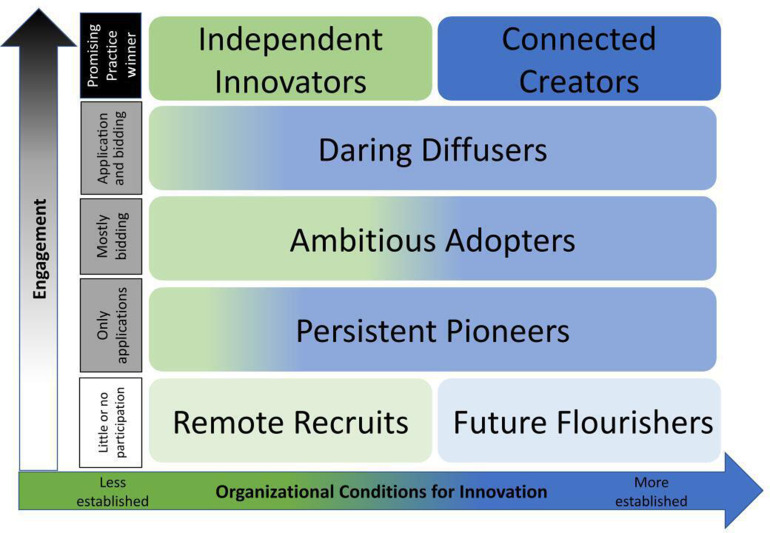
Based on the facility engagement by organizational conditions matrix, the authors identified 7 mutually exclusive types of facilities: Independent Innovators, Connected Creators, Daring Diffusers, Ambitious Adopters, Persistent Pioneers, Remote Recruits, and Future Flourishers. These typology titles were designed to be helpful for the operational partner, the DoE. The typology titles resonated with the DoE and demonstrated the potential of each type. Each type is shown within the facility engagement and organizational conditions figure (see Figure 1) and matrix (see Table 3). The types are described in detail in this paper.
Figure 1:
Facility engagement and organizational conditions matrix.
Table 3:
Descriptions of facility types
| Description | Remote Recruits | Future Flourishers | Persistent Pioneers | Ambitious Adopters | Daring Diffusers | Independent Innovators | Connected Creators |
|---|---|---|---|---|---|---|---|
| Facilities (n) | 16 | 15 | 8 | 35 | 14 | 6 | 36 |
| Conditions for innovation | Less established | Moderately established | Moderately established | Less or moderately established | Moderately established | Less established | Most established |
| Level of engagement in competition | Little or no engagement in competition | Little engagement in competition | High engagement in applying to competition | High engagement in bidding in competition | High engagement in applying to and bidding in competition | Promising Practice Winner | Promising Practice Winner |
Facilities With Little or No Engagement in the Competition
Two types of facilities were less engaged in the competition: the Remote Recruits and the Future Flourishers. The Remote Recruits were 16 facilities with low engagement in the competition and less established conditions for innovation. Only 1 facility had a research center and was part of iNET, the rest had neither. All except 1 facility submitted some applications, ranging from 1 to 18, with 18 being the average number of applications. On the other hand, the Future Flourishers (15 facilities), were also less engaged but were facilities with more established conditions for innovation. Though these were high-complexity facilities, only 1 facility had both a research center and was part of iNET; most of these facilities (66.7%, n = 10) had neither a research center nor were part of iNET. All of these facilities submitted some applications, ranging from 4 to 18.
Facilities With High Engagement in the Competition
The next 3 types of facilities were highly engaged in the competition in different ways. First, the Persistent Pioneers (8 facilities) were highly involved in submitting above-average numbers of applications, but not in bidding. Most Persistent Pioneers had moderately established conditions for innovation (62.5%, n = 5). Their total number of applications ranged from 19 to 33. The Ambitious Adopters made up one of the largest groups (35 facilities), and they were most engaged in the competition with bidding. Some Ambitious Adopter facilities may have submitted applications but at a below-average rate. Nineteen of 35 facilities (54%) had less established conditions for innovation; only 1 facility had a research center. Finally, 14 facilities were Daring Diffusers, engaged in both applying to and bidding in the Shark Tank. Most of these facilities had moderately established conditions for innovation, but half (n = 7) had neither a research center nor were part of iNET. Their total number of applications ranged from 19 to 48.
Facilities With the Highest Engagement in the Competition
There were 2 types of facilities with the highest level of engagement, represented by a winning Promising Practice. The Independent Innovators were a small group of 6 facilities that had at least 1 Promising Practice, but they also had the least established conditions for innovation. These were low-to-medium complexity facilities, all without research centers. Only 2 of these facilities were part of iNET. The Independent Innovators had lower numbers of Promising Practices, with the most per facility as 2 Promising Practices. Total applications were generally below average, ranging from 3 to 34. Half of the Independent Innovators participated in bidding and half did not. Next, the Connected Creators were the most engaged facilities, with the most established conditions for innovation. This was the largest group, with 36 facilities. All facilities were high in complexity and almost all (83%, n = 30) had a research center, were part of iNET, or both. Many Connected Creators were prolific, winning multiple Promising Practices, ranging from 1 to 6. The total number of submitted applications for this group ranged from 8 to 88. Twenty-nine (80%) facilities were also involved in bidding.
Discussion
Overall, there was very high engagement in the competition across the VHA. In the data, almost every VHA facility was engaged in the competition; however, the level and type of engagement varied. The authors categorized VHA facilities into 7 different types of engagement with the competition. As expected, facilities with the most established conditions for innovation were highly engaged in innovation, for example, the Connected Creators. However, not all facilities with these conditions were engaged and there were a small group of facilities, the Independent Innovators, with the least established conditions, that were also involved in the competition. Other organizational conditions, not measured in this study, may help to explain the success of the Independent Innovators and may include leadership support, organizational structure (ie, centralization and power differential), external environment factors, and organization culture and climate.23 Additionally, facilities with less-established conditions for innovation were more likely to be involved with bidding on innovations in the competition to adopt them at their facility.
Although past research has shown organizational conditions, including high facility complexity, the presence of research centers, and use of experts increase facility engagement in innovation,23,24 the results show potential for a deeper understanding of facility engagement. There were more facilities with high complexity engaged in innovation than low complexity facilities; however, this was not a straightforward relationship, as not all high complexity facilities were engaged in innovation. For example, of the 2high-complexity facilities types, the Future Flourishers (less engagement) and the Connected Creators (more engagement), the Connected Creators were more likely to be supported by a research center and/or part of iNET. This finding suggests that research centers and expert innovation support may be more determining factors to facility engagement than organizational complexity. Additionally, facilities with less-established conditions were more likely to be involved in bidding in the competition, which can be seen in the distinction between the Persistent Pioneers, Ambitious Adopters, and Daring Diffusers.
Previous research on organizational conditions and innovation often combines involvement in development, adoption, and spread of innovation,23,30 but the findings showing different types of engagement in innovation suggest that there may be benefit to separating these relationships and potentially tailoring roles within innovation based on organizational conditions. Larger facilities with ongoing research and more resources may be better suited to develop innovations, while smaller facilities could benefit from a focus on uptake and adoption. Differentiating roles would allow the VHA (and other health care systems) to focus on connecting these types of facilities and helping each advance toward increasing levels of innovation. For example, the DoE may allocate more resources and support to facilities with less organizational conditions for innovation. Additionally, these results can be used to work with facility leadership to better understand their facility’s engagement in the competition. In particular, the Future Flourishers (with moderately established conditions for innovation and little engagement in these types of competitions) may be motivated to increase their engagement by the knowledge that their peers are more engaged.
Knowledge of variation in engagement across facilities is essential to guide future work to engage frontline staff in innovation across the VA health care system. Based on earlier evaluations, these types of competitions (2016–2018) have resulted in 47 Promising Practices that were implemented 412 times across VA facilities.13 Approximately three-quarters of facilities implementing Promising Practices maintained the innovation 1.5 years later.18 Direct impacts on health care from these Promising Practices include (but are not limited to) $22.6 million in cost avoidance overall,13 decreased pneumonia cases from an oral care innovation,12,13 multiple interventions improving access to care for patients in rural areas,12 and improved patient and staff satisfaction.12 Competition innovations from frontline staff have made improvements in health care cost, quality, and access. This work provides valuable insight into the organizational conditions impacting engagement in the competition and varying engagement across VA facilities, which is essential to continuing to engage staff in organization-wide innovation and change.
Limitations
This study was limited by its observational design; therefore, causal inferences cannot be drawn between organizational conditions and engagement in the Shark Tank competition. Additionally, the classification of VHA facilities was dependent on self-identification, and satellite clinic data was collapsed into the larger medical center. This approach was necessary for managing the large data set, but it may obscure finer, detailed data on variations at the clinic level. Also, there are many organizational conditions that have been shown to impact innovation that could have influenced the findings. Future work should include facility visits and additional qualitative methods to further explore other organizational factors.
Despite these limitations, this study adds to the understanding of variation in facility engagement in innovation across a large integrated health care system. This study was part of a partnered evaluation with the VHA’s DoE. The results of this work will be used to help the DoE tailor how they work with distinct types of VHA facilities, which will aid in the most efficient allocation of resources, including, for example, focusing resources and support for facilities with fewer organizational conditions for innovation. Additionally, focused efforts can attract facilities with less engagement in the competition, that is, those which may have unique needs based on their organizational conditions. Future work may explore what helped the small group of positive deviant facilities, the Independent Innovators, win Promising Practices with less established conditions for innovation. It is likely that other factors may contribute that were not measured here, such as leadership support and organizational culture.23 Finally, to capture a fuller picture of engagement in innovation, future work may expand the criteria for facilities’ engagement in innovation beyond the competition to other innovation activities, including other DoE programs13,18,31 and the Lean Enterprise Transformation program.24
Conclusion
Engaging a large national health care system in the development and spread of innovation is essential for working to meet the quadruple aim (enhancing patient experience, improving population health, reducing costs, and improving staff satisfaction), but this can be a daunting undertaking. This study found high systemwide engagement in the VHA’s Shark Tank-style competition, suggesting substantial support from the DoE. However, there was variation in the level and type of engagement (development, adoption, or spread) based on organizational conditions, including complexity, research presence, and participation in an innovation expert support network. These insights shed light on the relationships between organizational conditions and facility engagement in innovation and can be used to inform resource allocation in the VHA and, potentially, in other health care systems. This study found that the VHA’s competition promoted innovation across a variety of medical centers, including those that may not otherwise have the resources to spread their innovations.
Author Contributions
Jenesse Kaitz, PhD, Kathryn DeLaughter, MA,Christine Deeney, and Gemmae M Fix, PhD,participated in the study design, acquisition,analysis of the data, and drafting of the finalmanuscript. Sarah L Cutrona, MD, MHP, Timothy P Hogan, PhD, Allen L Gifford, MD, GeorgeL Jackson, PhD, MHA, Brandolyn White, MPH,Heather King, PhD, Caitlin Reardon, MPH,Andrea Nevedal, PhD, and Blake Hendersonparticipated in the critical review and draftingof the final manuscript. All authors have givenfinal approval of the manuscript.
Footnotes
Funding: This material is based upon work supported by the Department of Veterans Affairs Quality Enhancement Research Initiative, PEC-17-002.
Conflicts of Interest: Dr Kaitz was supported by the US Department of Veterans Affairs, Office of Academic Affiliations, Advanced Fellowship Program in Health Services Research, Center for Healthcare Organization and Implementation Research, Veterans Affairs Bedford Healthcare System.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
References
- 1.Kelly CJ, Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017;4(2):121–125. 10.7861/futurehosp.4-2-121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herzlinger RE. Why innovation in health care is so hard. Harv Bus Rev. 2006;84(5):58–66. [PubMed] [Google Scholar]
- 3.Cutler DM. Where are the health care entrepreneurs? The failure of organizational innovation in health care. Innov Policy Econ. 2011;11(1):1–28. 10.1086/655816 [DOI] [Google Scholar]
- 4.Laker C, Callard F, Flach C, Williams P, Sayer J, Wykes T. The challenge of change in acute mental health services: Measuring staff perceptions of barriers to change and their relationship to job status and satisfaction using a new measure (VOCALISE). Implement Sci. 2014;9(1):23. 10.1186/1748-5908-9-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fascia M, Brodie J. Structural barriers to implementing open innovation in healthcare. Br J Health Care Manag. 2017;23(7):338–343. 10.12968/bjhc.2017.23.7.338 [DOI] [Google Scholar]
- 6.Berwick DM. Disseminating innovations in health care. JAMA. 2003;289(15):1969–1975. 10.1001/jama.289.15.1969 [DOI] [PubMed] [Google Scholar]
- 7.Damschroder LJ, Reardon CM, Opra Widerquist MA, Lowery J. Conceptualizing outcomes for use with the consolidated framework for implementation research (CFIR): The CFIR Outcomes Addendum. Implement Sci. 2022;17(1):7. 10.1186/s13012-021-01181-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parmar J, Sacrey LA, Anderson S, et al. Facilitators, barriers and considerations for the implementation of healthcare innovation: A qualitative rapid systematic review. Health Soc Care Community. 2022;30(3):856–868. 10.1111/hsc.13578 [DOI] [PubMed] [Google Scholar]
- 10.Demircioglu MA. The effects of empowerment practices on perceived barriers to innovation: Evidence from public organizations. Int J Public Adm. 2018;41(15):1302–1313. 10.1080/01900692.2017.1387143 [DOI] [Google Scholar]
- 11.Reardon C, Nevedal A, Widerquist MAO, et al. Sustainment of Diverse Evidence-Based Practices Disseminated in the Veterans Health Administration (VHA): Development and Administration of a Pragmatic Instrument; 2021. 10.21203/rs.3.rs-951440/v2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clancy C. Creating world-class care and service for our nation’s finest: How Veterans Health Administration Diffusion of Excellence Initiative is innovating and transforming Veterans Affairs health care. Perm J. 2019;23:23. 10.7812/TPP/18.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vega R, Jackson GL, Henderson B, et al. Diffusion of excellence: Accelerating the spread of clinical innovation and best practices across the nation’s largest health system. Perm J. 2019;23(18):309. 10.7812/TPP/18.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nevedal AL, Reardon CM, Jackson GL, et al. Implementation and sustainment of diverse practices in a large integrated health system: A mixed methods study. Implement Sci Commun. 2020;1(1):61. 10.1186/s43058-020-00053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lange TM, Hilgeman MM, Portz KJ, Intoccia VA, Cramer RJ. Pride in all who served: Development, feasibility, and initial efficacy of a health education group for LGBT veterans. J Trauma Dissociation. 2020;21(4):484–504. 10.1080/15299732.2020.1770147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crowley MJ, Tarkington PE, Bosworth HB, et al. Effect of a comprehensive telehealth intervention vs telemonitoring and care coordination in patients with persistently poor type 2 diabetes control: A randomized clinical trial. JAMA Intern Med. 2022;182(9):943–952. 10.1001/jamainternmed.2022.2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nichols LO, Chang C, Lummus A, et al. The cost-effectiveness of a behavior intervention with caregivers of patients with Alzheimer’s disease. J Am Geriatr Soc. 2008;56(3):413–420. 10.1111/j.1532-5415.2007.01569.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson GL, Cutrona SL, White BS, et al. Merging implementation practice and science to scale up promising practices: The Veterans Health Administration (VHA) Diffusion of Excellence (DoE) program. Jt Comm J Qual Patient Saf. 2021;47(4):217–227. 10.1016/j.jcjq.2020.11.014 [DOI] [PubMed] [Google Scholar]
- 19.Elnahal SM, Clancy CM, Shulkin DJ. A framework for disseminating clinical best practices in the VA health system. JAMA. 2017;317(3):255–256. 10.1001/jama.2016.18764 [DOI] [PubMed] [Google Scholar]
- 20.Terwiesch C, Mehta SJ, Volpp KG. Innovating in health delivery: The Penn Medicine innovation tournament. Healthc (Amst). 2013;1(1–2):37–41. 10.1016/j.hjdsi.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 21.Jung OS, Jackson J, Majmudar M, McCree P, Isselbacher EM. Engaging frontline employees using innovation contests: Lessons from Massachusetts General Hospital. Healthc (Amst). 2022;10(2):100615. 10.1016/j.hjdsi.2022.100615 [DOI] [PubMed] [Google Scholar]
- 22.National Academies of Sciences, Engineering, and Medicine . Facilities Staffing Requirements for the Veterans Health Administration—Resource Planning and Methodology for the Future; 2019. [PubMed] [Google Scholar]
- 23.Anderson N, Potočnik K, Zhou J. Innovation and creativity in organizations: A state-of-the-science review, prospective commentary, and guiding framework. J Manage. 2014;40(5):1297–1333. 10.1177/0149206314527128 [DOI] [Google Scholar]
- 24.Azevedo KJ, Gray CP, Gale RC, et al. Facilitators and barriers to the Lean Enterprise Transformation program at the Veterans Health Administration. Health Care Manage Rev. 2021;46(4):308–318. 10.1097/HMR.0000000000000270 [DOI] [PubMed] [Google Scholar]
- 25.Vashi AA, Orvek EA, Tuepker A, et al. The Veterans Health Administration (VHA) Innovators Network: Evaluation design, methods and lessons learned through an embedded research approach. Healthc (Amst). 2021;8(suppl 1):100477. 10.1016/j.hjdsi.2020.100477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med Res Methodol. 2011;11:100. 10.1186/1471-2288-11-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Veterans Health Administration, FY 2017 Facility Complexity Level Model. 2017.
- 28.Wong JK, Kim TE, Mudumbai SC, et al. Are case volume and facility complexity level associated with postoperative complications after hip fracture surgery in the Veterans Affairs healthcare system? Clin Orthop Relat Res. 2019;477(1):177–190. 10.1097/CORR.0000000000000460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kluge S. Empirically grounded construction of types and typologies in qualitative social research. Forum qualitative sozialforschung/Forum: Qualitative social research. 2000;1(1). 10.17169/fqs-1.1.1124 [DOI] [Google Scholar]
- 30.Crossan MM, Apaydin M. A multi-dimensional framework of organizational innovation: A systematic review of the literature. J Manage Stud. 2010;47(6):1154–1191. 10.1111/j.1467-6486.2009.00880.x [DOI] [Google Scholar]
- 31.Vega RJ, Kizer KW. VHA’s innovation ecosystem: Operationalizing innovation in health care. NEJM Catalyst. 2020;1(6). 10.1056/CAT.20.0263 [DOI] [Google Scholar]