Abstract
A prospective analysis of a retrospective data of patients with cervix carcinoma treated by minimal invasive surgery at high-volume gynecology oncology center analyzing that minimal access surgery is an acceptable treatment modality in cervix carcinoma. The study included 423 patients who underwent laparoscopic/robotic radical hysterectomy after pre-operative evaluation after taking their consent and obtaining ethical approval from the IRB. Post-operatively, patients were followed up at regular intervals for clinical examination and ultrasonography for a median range of 36 months. A PET scan was done only if there was any suspicious finding on clinical examination or ultrasonography. Patients with parametrial involvement, positive vaginal margins, and nodal involvement were treated with chemotherapy/radiotherapy. Four hundred twenty-three patients of cervix carcinoma were treated with minimal access surgery. Average duration of surgeries was 92 min. Median range of duration of post-operative follow-up was 36 months. None of the patients had positive resection margins indicating adequate parametrectomy with complete oncological clearance. On post-operative follow-up, only 2 patients had vaginal recurrence which is comparable to that observed in open surgery and no pelvic recurrence. With the understanding of the anatomical landmarks of the anterior parametrium and development of skills for adequate oncological clearance, minimal access surgery should be the preferred surgical modality in carcinoma of the cervix.
Keywords: Carcinoma cervix, Recurrence, Minimal access surgery, Parametrectomy, Oncological clearance, Pelvic recurrence
Introduction
Minimal access surgery was an accepted treatment modality in cervical cancer until the LACC trial in 2018. The LACC trial analyzed the incidence of recurrences in patients who were operated for cancer of the cervix comparing laparoscopic and open modalities of the surgery [1]. The results of LACC trial were a shock to the minimal access surgery community. Many of them questioned the trial, but since it was a multi-centric prospective trial, the results had to be accepted. We, in our modest way, have tried to analyze what would have been the reason for recurrence. After the publication of the trial, we retrospectively analyzed our data of radical hysterectomy.
In this study, we have described the anatomical landmarks of anterior parametrium. We feel that incomplete clearance of anterior parametrium may be the reason for pelvic recurrences following laparoscopy.
Materials and Methods
From 2014 to 2019, charts of more than 400 patients with cervical cancer stages IB1 and IB2, who underwent laparoscopic radical hysterectomy, were retrospectively analyzed after taking their consent and obtaining ethical approval from the IRB. These patients have been followed up at 6-monthly interval. The patients were evaluated for recurrence by clinical examination and ultrasonography. PET CT scan was performed only if there was any suspicious finding on clinical examination or ultrasonography.
All patients underwent laparoscopic radical hysterectomy/robotic radical hysterectomy with the technique which will be described in the technical part. Pre-operative investigations included biochemical tests, chest X-ray, and MRI of the pelvis. PET CT scan was done if MRI of the pelvis showed pelvic lymphadenopathy.
For FIGO 2018 stage IB1, type C1 radical hysterectomy (RH) was performed, which comprised of resection of the anterior parametrium up to 2 cm from vaginal wall. For carcinoma of the cervix FIGO 2018 stage IB2, type C2 radical hysterectomy (RH) was performed, resecting anterior parametrium up to 2 cm from vaginal wall. The only difference between types C1 and C2 radical hysterectomy was that C1 radical hysterectomy comprised of nerve preservation and less clearance of cardinal ligaments. The clearance of anterior parametrium was the same in C1 and C2 radical hysterectomy.
These patients were reviewed taking into consideration age, histopathological reports, requirement of adjuvant chemotherapy/radiotherapy, recurrence-free interval, and mortality.
In both C1 and C2 radical hysterectomy, the anterior and posterior parametrial clearance was the same (approximately 2.2–2.5 cm). The difference was that of nerve preservation in C1 radical hysterectomy which led to a lesser clearance of lateral parametrium as compared to C2.
Inclusion criteria are all patients with carcinoma cervix until FIGO 2018 stage IA1-IB2.
Technique
Patients underwent a standard mechanical bowel preparation and received peri-operative prophylactic antibiotics. Regional anesthesia, either spinal or epidural, was preferred in combination with general anesthesia.
For uterine manipulation, “The uterine hitch technique” [2] was done (Figs. 1, 2, and 3). Laparoscopic radical hysterectomy was performed following the steps described in the Pune technique [3, 4].
Fig. 1.
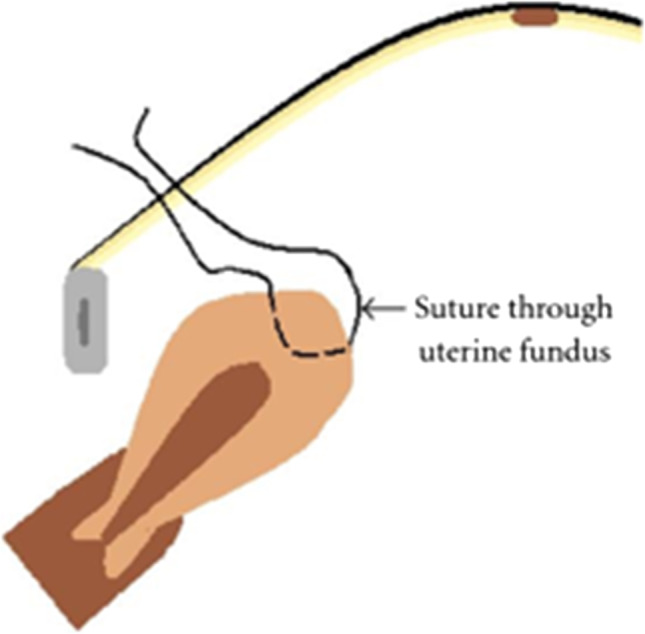
The uterine hitch technique
Fig. 2.

The uterine hitch technique
Fig. 3.
The uterine hitch technique
The posterior parametrial clearance was at least 2 cm from the lateral vaginal wall while the anterior parametrium was also taken at least 2 cm caudally from the vaginal wall.
A colpotomy was performed only after applying stapler (Figs. 4 and 5) or taking purse string sutures (Fig. 6) to prevent spillage of tumor. The average anterior and posterior parametrial clearance was the same in types C1 and C2 radical hysterectomy with an average of 2.2–2.5 cm. The lateral parametrial clearance was less than 1 cm in C1 radical hysterectomy due to nerve preservation as compared to type C2 radical hysterectomy.
Fig. 4.
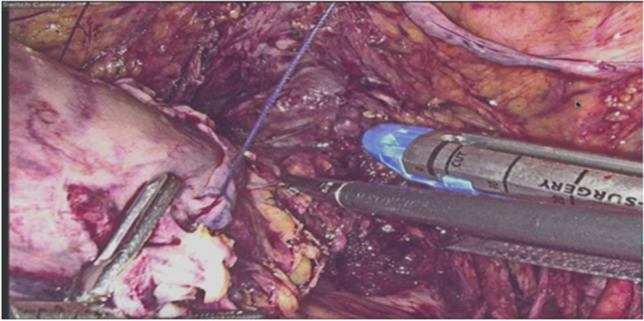
Colpotomy by stapler
Fig. 5.
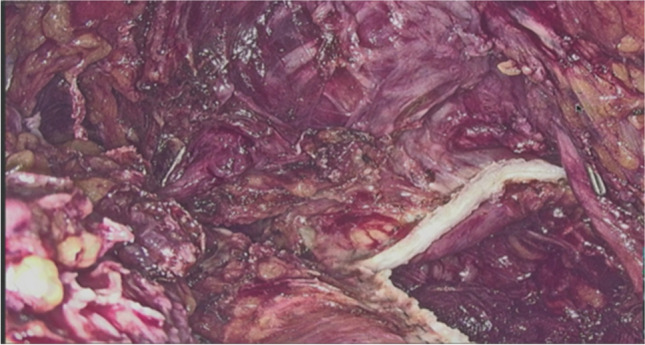
Sutured edges post stapler application
Fig. 6.
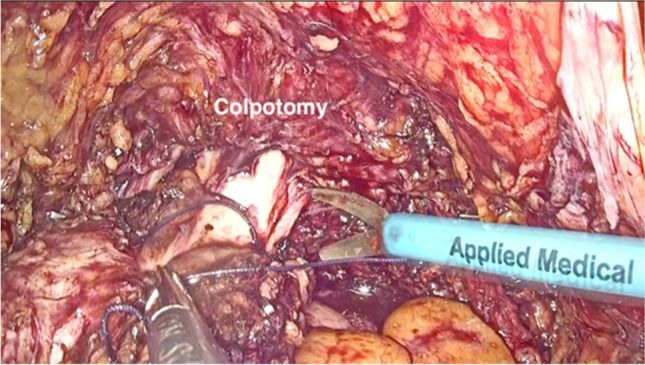
Colpotomy completed without tumor spillage
Description of the Parametrium
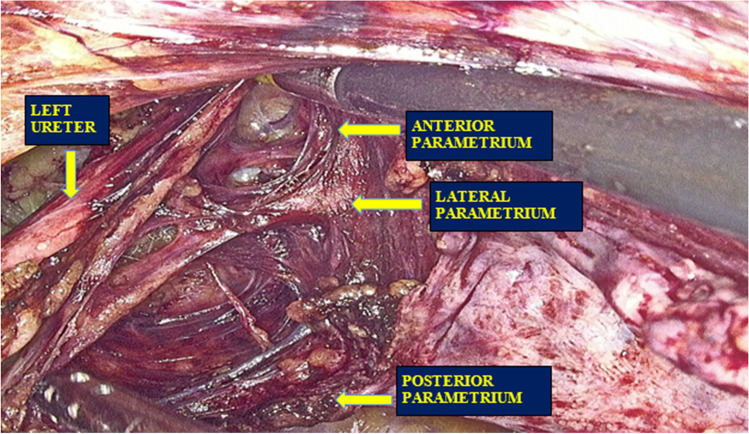
Laparoscopic radical hysterectomy (LRH) was performed by the Pune technique as described above. The process of exposing anterior parametrium and the importance of clamping it laterally are described now. The cervix is surrounded by three parametria (Fig. 7).
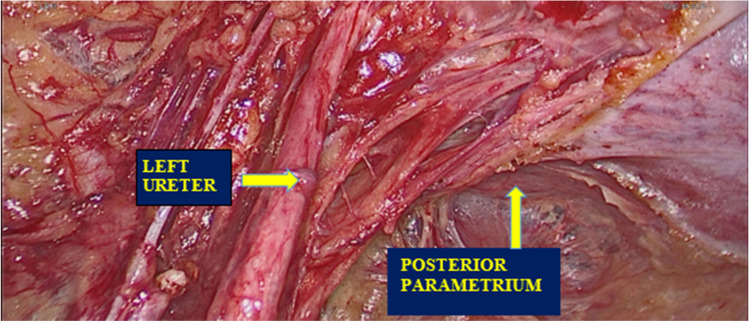
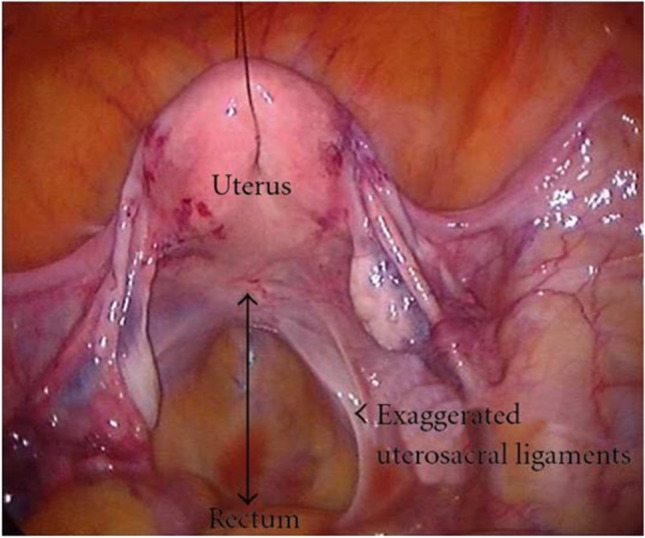
The posterior parametrium (Fig. 8)
Fig. 7.
Laparoscopic view of all three parametria
Fig. 8.
Posterior parametrium
It is visualized once the rectovaginal space, para-rectal space, and para-vesical spaces are dissected. It consists of fibromuscular tissue comprising of uterosacral ligaments.
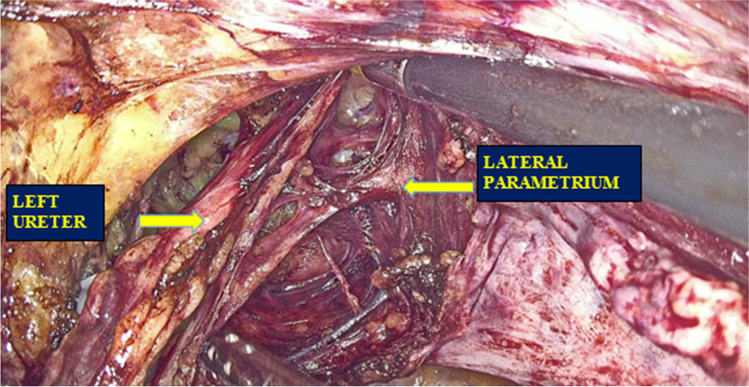
The lateral parametrium (Fig. 9)
Fig. 9.
Lateral parametrium
It consists of superficial and deep part made up of loose fibroareolar tissue. It is formed by the cardinal/Mackenrodt’s ligaments. The deep and superficial uterine veins travel through the Mackenrodt’s ligament.
The anterior parametrium (Fig. 10)
Fig. 10.
Anterior parametrium, lateral view
It comprises of fibroareolar tissue running parallel to the vagina. This fibroareolar tissue reaches caudally up to endopelvic fascia covering levator ani muscle.
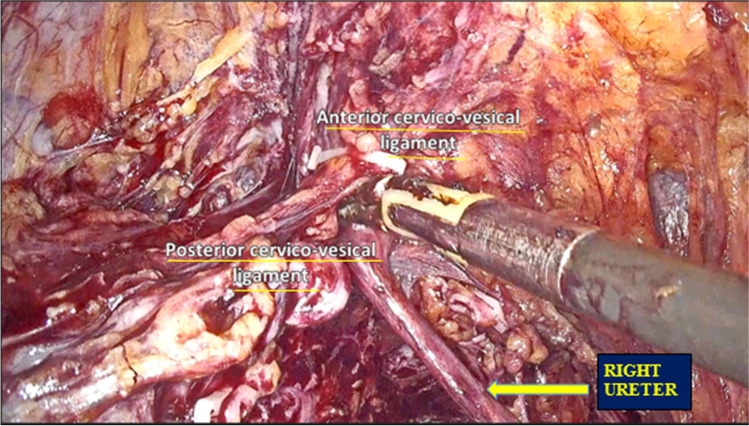
The anterior parametrium is exposed after incising the anterior cervicovesical ligament (Fig. 11). This exposes the ureter attached by the strands of fascia. These fascial strands have to be cut to lateralize the ureter. The posterior cervicovesical ligament is the beginning of anterior parametrium. It runs parallel to the cervix and the vagina and continues up to the endopelvic fascia covering the levator ani and the obturator internus muscles.
Fig. 11.
Anterior and posterior cervicovesical ligament
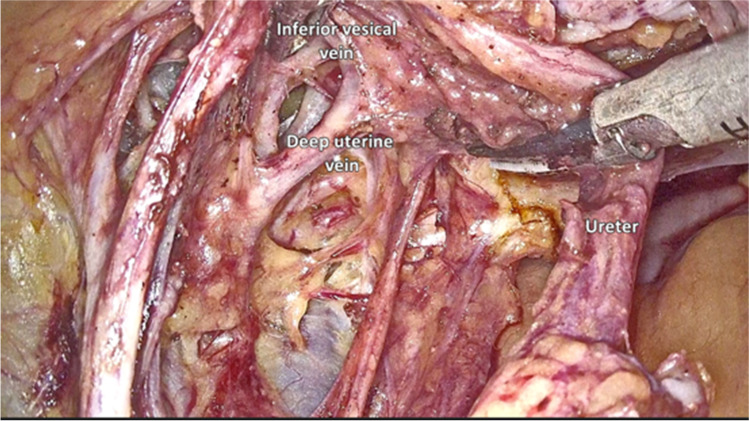
The anatomical landmark of the anterior parametrium is the inferior vesical vein (Fig. 12). This vein runs parallel to the vagina as it ascends from below upwards. It drains the urinary bladder and then joins the deep uterine vein (Fig. 12). The length of resection of the veins corresponds to the length of parametrial resection. Thus, the veins along with the fibroareolar tissue should be resected at least 2 cm lateral to the vault.
Fig. 12.
Inferior vesical vein and deep uterine vein
It is mandatory to trace the ureter up to the ureterovesical junction to get a complete vision of the anterior parametrium.
Criteria for Post-surgery CT/RT
The patients were followed every month for a period of 1 year. The follow-up included clinical examination and ultrasonography. The Sedli’s criteria was considered for post-surgery chemotherapy/radiotherapy.
Results
The patient and tumor characteristics are described in Table 1 with the median age of patients in the study being 61 years and average tumor size of about 33 mm. The mean parametrial involvement observed was 3–3.5 cm laterally, 2.5–3 cm posteriorly, and 2 cm anteriorly.
Table 1.
Patients and tumor characteristics
| Mean age (median and range) | 61 years (35–82) |
| Tumor size (median and range) | 33 mm (1–38) |
| Average length of parametrium | |
| Lateral | 3–3.5 cm |
| Posterior | 2.5–3 cm |
| Anterior | 2 cm |
The operative time was found to be around 65 to 120 min with a mean blood loss of 165 ml. The patients who underwent laparoscopic/radical hysterectomy had a mean hospital stay of 3–6 days.
The surgical findings regarding the average length of parametrium resected and the number of lymph nodes dissected are mentioned in Table 2.
Table 2.
Surgical observations
| Median range of | ||
|---|---|---|
| Average length of parametrium resected | C1 RH | C2 RH |
| Lateral | 2 cm | 3–3.5 cm |
| Posterior | 2.5–3 cm | 3 cm |
| Anterior | 2 cm | 2 cm |
| No. of lymph nodes removed | 18 (14–30) | |
| Duration of operation (in min) | 92 (65–120) | |
| Blood loss (in ml) | 165 (150–500) | |
| Length of hospital stay (in days) | 3 (3–6) | |
The specimen retrieved in the surgery was examined for various parameters as mentioned in Table 3. The histologic type found in the majority of the specimen was squamous carcinoma. Of the 423 patients analyzed, 174 had parametrial involvement on histological examination and the disease had spread to involve lymph nodes in 173 patients. The resection margins of all specimen were negative indicating complete oncological clearance.
Table 3.
Tumor parameters
| Parametrial involvement | |
| Yes | 174 |
| No | 249 |
| Lymph node metastasis | |
| Yes | 173 |
| No | 250 |
| Resection margins | |
| Positive | nil |
| Negative | 423 (100%) |
| Adjuvant treatment | |
| Yes | 174 |
| No | 249 |
| Vaginal involvement | 2 |
| Histologic type (n = 423) | |
| Squamous | 200 |
| Adenosquamous | 88 |
| Adenocarcinoma | 135 |
| Grade 1 | 245 |
| Grade 2 | 123 |
| Grade 3 | 55 |
| Stage Ia2 | 124 |
| Stage Ib1 | 208 |
| Stage Ib2 | 91 |
Except for one patient, all other patients with parametrial involvement had pathological nodal involvement. They were treated with chemotherapy and radiotherapy. On follow-up, none of the patients had pelvic recurrence as shown in Table 4.
Table 4.
Recurrences
| Total | 27 |
| Vaginal recurrence | 2 |
| Pelvic recurrence | 0 |
| Para-aortic recurrence | 10 |
| Distant metastasis | 15 |
Discussion
In cervical cancer, the presence of cervicovesical fascia anteriorly and Denonvilliers fascia posteriorly restricts the spread to the bladder or rectum until late stages of the tumor.
The cervicovesical fascia splits into anterior cervicovesical ligament and posterior cervicovesical ligament. The ureter passes between these two ligaments to reach the bladder. This causes a potential deficient part through which the cancer cells can spread into the anterior parametrium.
Cervical cancer surgery is about the resection of anterior, lateral, and posterior parametria. Recurrence after cervix carcinoma surgery is inversely proportional to the parametrial clearance.
Thus, the main focus of the surgery in cervical cancer involves the removal of parametria. The cardinal rule of the body is that the lymphatics follow the veins. In cervical cancer of squamous origin, the spread of the tumor is via the lymphatic permeation.
The optimal removal of parametria is of paramount importance to prevent pelvic recurrence. This goal can be achieved if one understands the anterior parametrium. Total parametrectomy involves complete removal of posterior, lateral, and anterior parametria.
In our patients, the only difference between C1 and C2 radical hysterectomy was the length of lateral parametrial clearance. The posterior and anterior parametrial clearance was the same. Irrespective of types C1 or C2 radical hysterectomy, we did not have pelvic recurrence. The only difference was the length of lateral parametrial clearance in types C1 and C2. Thus, the patients in whom type C1 radical hysterectomy was done would be expected to have high incidence of pelvic recurrence. Thus, we feel that the key to avoid pelvic recurrence is adequate anterior parametrial clearance. A complete anterior parametrectomy is mandatory due to its close proximity to the tumor. We had no patients with positive anterior parametrial margins, indicating complete clearance. Therefore, it is not about lateral or posterior parametrial clearance but about anterior parametrial clearance.
The larger question is how is it that in open radical hysterectomy the anterior parametrial clearance is adequate leading to decreased incidence of pelvic recurrence. The probable explanation is that during open surgery, the ureter is pushed bluntly with the thumb to achieve lateralization. A clamp is then applied as laterally as possible by palpation. Thus, complete anterior parametrial clearance is achieved inadvertently. During laparoscopic surgery, anterior parametrial clearance requires technical expertise and understanding. The anterior cervicovesical ligament has to be resected. This process can be bloody as there are two veins draining from the bladder. Secondly, the lateralization of the ureter with subsequent lateral clamping of the anterior parametrium can be compromised. This invariably leads to less lateralization of the ureter and therefore less anterior parametrial clearance.
The posterior and lateral parametria being easily visualized can be excised as laterally as possible without much effort. The anatomical understanding of the anterior parametrium is most critical when treating cervix carcinoma.
The nomenclature is paracolpos, paravaginal tissue, and cervicovaginal tissue. This is also called as the infra-ureteral parametrium [5]. The exposure of anterior parametrium involves the cutting of the anterior cervicovesical ligament and pushing the ureter laterally. This has two veins, draining into the deep uterine vein, which have to be clipped. This process can be bloody if anatomy is not understood. The ureter can be pushed laterally only when the fibers which attach the ureter to the parametrium are cut. The ureter must be traced up to the ureterovesical junction. The anatomical landmarks are not well described leading to confusion. The anatomical landmarks are Yabuki’s space, which is medial to the ureter and is characterized by the presence of terminal fibers of hypogastric nerve on its way to the urinary bladder. The exposure of the inferior vesical vein is of paramount importance to view the anterior parametrium.
The technical inability and absence of understanding the anatomical landmarks of the anterior parametrium can lead to inadequate clearance in laparoscopy.
So, our hypothesis is that failure to identify the inferior vesicle vein and clamping it at least 2 cm laterally probably leads to spillage of the cancer cells in the pelvis. This may increase the chances of pelvic recurrences. Larger the lesion, more are the chances of spillage of cancer cells. So, for a tumor which is more than 2 cm, adequate parametrectomy is of utmost importance.
Though we have not done any comparative study, we had no pelvic recurrences in stage Ib2. There were only 2 vaginal recurrences.
Very few articles have described the correct anatomical landmarks to achieve complete clearance of anterior parametrium. Additional steps needed to explore the anterior parametrium in laparoscopic radical hysterectomy are not described in detail. The inferior vesical vein is of paramount importance. Clamping the vein 2 cm lateral to the vaginal wall would lead to adequate anterior parametrectomy.
The results of our study were compared with various other studies (Table 5). In a study conducted by Laterza et al., 150 patients were included, 82 submitted to LRH and 68 submitted to ARH. Sites of recurrence were also comparable between the 2 groups: 2/9 versus 2/13 local recurrence, 4/9 versus 8/13 pelvic recurrence, LRH and ARH groups, respectively [6].
Table 5.
Comparison of pelvic recurrence after LRH in cervix carcinoma in various studies
| Study | Total no. of LRH | Pelvic recurrence |
|---|---|---|
| Laterza et al | 82 | 4 |
| Toptas et al | 22 | 3 |
| Zhu et al | 30 | 5 |
| Yan et al | 148 | 21 |
| Kanno et al | 210 | 5 |
| Liang et al | 163 | 0 |
| Wang et al | 203 | 0 |
Toptas et al. conducted a study in which 22 out of a total of 68 patients underwent laparoscopic radical hysterectomy and recurrence was observed in 3 patients in a 3-year follow-up interval [7].
Another study conducted by Zhu et al. analyzed 30 patients out of a total of 112 who underwent LRH and observed recurrence in 5 patients [8].
Yan et al. observed 21 recurrences out of 148 patients who underwent LRH in a median follow-up period of 28 months [9].
In a study conducted by Kanno et al., with a median follow-up of 73 months (range, 30–146 months), five out of 210 patients developed recurrent disease with a median disease-free interval of 68 months (range, 11–146 months) [10].
In a study conducted by Liang et al., 163 consecutive patients with cervical cancer underwent laparoscopic radical hysterectomy (LRH) and pelvic lymphadenectomy, with no recurrence observed within 4 years of follow-up [11].
Wang et al. observed a 5-year recurrence-free survival (RFS) in their study that included analysis of 203 patients who underwent LRH [12].
Thus, we feel that cervical cancer surgery involves a thorough anatomical knowledge of anterior parametrium.
The optimal removal of parametrium is more of a technical issue and is directly proportional to the skill of the surgeon. Recurrences in pelvis are thus indirectly proportional to the skills of the surgeon.
We did not use uterine manipulators during radical hysterectomy. The vagina was closed with a stapler before colpotomy. This is the reason for just 2 vaginal recurrences.
A recent study conducted by Nica et al. concluded that the use of an intra-uterine manipulator in patients with early cervical cancer who underwent minimally invasive radical hysterectomy was not contributory to the rate of recurrence [13].
Conclusion
The accidental exposure of anterior parametrium during open surgery leads to less pelvic recurrence in open surgery. If adequate attention is given to exposure of anterior parametrium in laparoscopy, the pelvic recurrences may not occur. With this hypothesis, we conclude that adequate infra-ureteral or anterior parametrectomy is the key to prevent pelvic recurrences.
Abbreviations
- ARH
Abdominal radical hysterectomy
- CT/RT
Chemotherapy/radiotherapy
- LRH
Laparoscopic radical hysterectomy
- RFS
Recurrence-free survival
- RH
Radical hysterectomy
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira MA, Ribeiro R. Phase III randomized trial of laparoscopic or robotic versus abdominal radical hysterectomy in patients with early-stage cervical cancer: LACC trial. Gynecol Oncol. 2018;1(149):245. doi: 10.1016/j.ygyno.2018.04.552. [DOI] [Google Scholar]
- 2.Puntambekar SP, Patil AM, Rayate NV, Puntambekar SS, Sathe RM, Kulkarni MA (2010) A novel technique of uterine manipulation in laparoscopic pelvic oncosurgical procedures: “The uterine hitch technique” [DOI] [PMC free article] [PubMed]
- 3.Puntambekar SP, Palep RJ, Puntambekar SS, Wagh GN, Patil AM, Rayate NV, Agarwal GA. Laparoscopic total radical hysterectomy by the Pune technique: our experience of 248 cases. J Minim Invasive Gynecol. 2007;14(6):682–689. doi: 10.1016/j.jmig.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Puntambekar SP, Agarwal GA, Joshi SN, Rayate NV, Puntambekar SS, Sathe RM. Robotic radical hysterectomy: applying principles of the laparoscopic Pune technique. J Robot Surg. 2010;4(4):259–264. doi: 10.1007/s11701-010-0224-9. [DOI] [PubMed] [Google Scholar]
- 5.Possover M (2021) The “modified Schauta-Stoeckel “procedure. J Minim Invasive Gynecol 28(3):391 [DOI] [PubMed]
- 6.Laterza RM, Uccella S, Casarin J, Morosi C, Serati M, Koelbl H, Ghezzi F. Recurrence of early stage cervical cancer after laparoscopic versus open radical surgery. Int J Gynecol Cancer. 2016;26(3):547–552. doi: 10.1097/IGC.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 7.Toptas T, Simsek T. Total laparoscopic versus open radical hysterectomy in stage IA2–IB1 cervical cancer: disease recurrence and survival comparison. J Laparoendosc Adv Surg Tech. 2014;24(6):373–378. doi: 10.1089/lap.2013.0514. [DOI] [PubMed] [Google Scholar]
- 8.Zhu T, Chen X, Zhu J, Chen Y, Yu A, Chen L, Shou H, Wu M, Zhang P (2017) Surgical and pathological outcomes of laparoscopic versus abdominal radical hysterectomy with pelvic lymphadenectomy and/or para-aortic lymph node sampling for bulky early-stage cervical cancer. Int J Gynecol Cancer 27(6) [DOI] [PubMed]
- 9.Yan X, Li G, Shang H, Lin F, Yang X, Zheng F (2012) Outcome and prognostic factors of laparoscopic radical hysterectomy and pelvic lymphadenectomy in 148 patients with stage IB1 cervical cancer. Int J Gynecol Cancer 22(2) [DOI] [PubMed]
- 10.Kanno K, Andou M, Yanai S, Toeda M, Nimura R, Ichikawa F, Teishikata Y, Shirane T, Sakate S, Kihira T, Hamasaki Y. Long-term oncological outcomes of minimally invasive radical hysterectomy for early-stage cervical cancer: A retrospective, single-institutional study in the wake of the LACC trial. J Obstet Gynaecol Res. 2019;45(12):2425–2434. doi: 10.1111/jog.14116. [DOI] [PubMed] [Google Scholar]
- 11.Liang Z, Chen Y, Xu H, Li Y, Wang D. Laparoscopic nerve-sparing radical hysterectomy with fascia space dissection technique for cervical cancer: description of technique and outcomes. Gynecol Oncol. 2010;119(2):202–207. doi: 10.1016/j.ygyno.2010.06.033. [DOI] [PubMed] [Google Scholar]
- 12.Wang W, Chu HJ, Shang CL, Gong X, Liu TY, Zhao YH, Huang JM, Yao SZ (2016) Long-term oncological outcomes after laparoscopic versus abdominal radical hysterectomy in stage IA2 to IIA2 cervical cancer: a matched cohort study. Int J Gynecol Cancer 26(7) [DOI] [PubMed]
- 13.Nica A, Kim SR, Gien LT, Covens A, Bernardini MQ, Bouchard-Fortier G, Kupets R, May T, Vicus D, Laframboise S, Hogen L (2020) Survival after minimally invasive surgery in early cervical cancer: is the intra-uterine manipulator to blame? Int J Gynecol Cancer 30(12) [DOI] [PubMed]