Abstract
To audit the use of breast conservation surgery for breast cancer treatment in a tertiary care centre over a 7-year period, and also to chart the clinical, demographic and pathological characteristics of breast cancer patients treated in the setting of a referral centre in a middle income (MDI) group country. A retrospective analysis of the case records of all patients of invasive breast cancer treated at our institute between January 2014 and December 2020 was done after obtaining approval from the Institute Ethics Committee (IEC). The number of patients seen, age, parity, menopausal status, family history of cancer, laterality, site of tumour in the breast, the symptomatology, clinical stage and presence or absence of metastases was the clinical parameters examined. The pathological stage and grade of the tumour, receptor status, treatment offered according to stage and the patterns of failure with respect to the surgery performed were recorded. Statistical analysis was a direct head to head comparison of the percentage proportions of the different variables. A total of 685 patients of breast cancer were treated between January 2014 and December 2020. A total of 53% of the cohort was more than 45 years old and 56.7% were post menopausal. A total of 58.8% of the patients presented with a cancer in the left breast and in the upper outer quadrant. Nearly 41% of the tumours were more than 4 cm in size. The most common receptor profile in our patient population was ER positive, PR positive and HER 2 negative. A total of 27.7% of the patients were offered neo-adjuvant chemotherapy and 63.06% underwent upfront surgery. A total of 19.7% of all surgeries performed (overall) were breast conservation surgeries (BCS). The use of BCS showed an increasing trend over the 7 years studied rising from 16.79 to 25% (annually). The local failure rate for BCS was 11.8% but the incidence of distant metastases was not significantly different compared to the patients who underwent a mastectomy. Breast conservation is safe and feasible in a referral setting even in a middle income nation with multi-disciplinary treatment planning and needs to be adopted widely to preserve the body image and self esteem of patients with breast cancer.
Keywords: Breast conservation surgery, Audit, Trends, Multi-disciplinary management
Introduction
Over the past decade, breast cancer has overtaken cancer of the uterine cervix to emerge as the leading cause of cancer related morbidity among women in India. The number of new cases of breast cancer detected in India in 2020 was 178,361, which constituted 26.1% of all cancers in women, and about 11.6% of cancers in both sexes combined [1]. Along with this increasing number, there has been a changing demographic observed, with more cases being diagnosed in the less than 45-year age group. The availability of chemotherapy and radiation therapy along with the increasing number of younger patients should ideally have resulted in an exponential increase in the use of breast conservation surgery (BCS) in India.
However, the breast conservation rate in most centres in India has not gone beyond 30–35% (especially in the public sector) [2]. The reasons for this range from delayed presentation, lack of awareness about BCS, surgical hesitancy and patient preferences. Ours is a tertiary care referral centre located in a state in Southern India, with a literacy rate of 66% and a well-developed health care delivery system. With this in mind, we analysed the data of the patients of breast cancer treated in our institute and sought to establish the trends in the adoption of breast conservation surgery over the period of study.
Materials and Methods
A retrospective analysis of the case records of all patients of breast cancer, who received treatment at our Institute from January 2014 to December 2020, was undertaken. Treatment decisions were finalised after discussion in a multi-disciplinary tumour board. The AJCC (7th and then 8th) manual was followed with respect to the staging of the breast cancer. Clinical evaluation was followed by staging investigations (chest radiograph, ultra sonogram of the abdomen and pelvis, liver function tests) for early breast cancers (EBC) and a positron-emission computed tomography scan (PET-CT) for locally advanced breast cancers (LABC). All patients underwent a bilateral mammogram with ultra sonogram of the axilla, if it was clinically node-negative. A core needle biopsy was the investigation of choice to establish tissue diagnosis, as also to assess the hormone — receptor and HER 2 neu status of the tumour.
All patients of early breast cancer (cT1, T2 N0) who were receptor positive (ER + ve, PR + ve,) were offered breast conservation surgery upfront. A second category of patients with tumours classified as operable large breast cancers (OLBC) (cT3N0) was also offered surgery upfront. Patients with locally advanced breast cancers (LABC) were offered neo-adjuvant chemotherapy. Metastatic breast cancers (MBC) were given chemotherapy or hormone therapy and underwent surgery only if palliation was required.
The demographic characters of the patients were collected, along with the clinical data. Age, laterality of the tumour, symptomatology, the presence or absence of axillary nodes and whether any excision was done prior to presentation were some of the clinical parameters looked at. The stage distribution of the tumours, receptor status and HER 2 positivity and response to neo adjuvant chemotherapy was the pathological parameters collected. The treatment variables such as the type of surgery performed and whether it was upfront or post neo-adjuvant chemotherapy or as a palliative measure were also determined. The use of breast conservation surgery (BCS) over time was also charted.
Results
A total of 685 patients of breast cancer who came to our Institute for treatment were analysed. Eighty seven (12.7%) were detected to have metastatic breast cancer (MBC) at presentation and were referred for palliative chemotherapy. A total of 53% of this patient cohort were more than 45 years of age, with a median age of 44. The youngest patient was 23 years old and the eldest was 92 years old. Most patients were post menopausal and multiparous and only about 23.5% were nulliparous. A total of 58.8% of the tumours were located in the left breast, and almost 93% were located in the upper outer quadrant. The most common presenting complaint was the presence of a palpable lump, which was the main symptom in 605 patients (88.3%). The most common pathological stage of the tumours in our patient cohort was pT3N0 (40.7%), with early breast cancers (EBC) pT1, T2 N0 forming about 26.2% of the patient population (n = 180). Locally advanced breast cancers (LABC) constituted 20.2% of the cohort (n = 139) (Table 1).
Table 1.
Clinical and demographic characteristics of the patient cohort (N = 685)
| Parameter | Number | Percentage |
|---|---|---|
| Age | ||
| < 45 years | 324 | 47.6% |
| > 45 years | 361 | 52.7% |
| Laterality | ||
| Right | 282 | 41.1% |
| Left | 403 | 58.8% |
| Presenting symptoms | ||
| Palpable lump | 605 | 88.3% |
| Nipple discharge | 250 | 36.4% |
| Axillary swelling | 128 | 18.6% |
| Menopausal status | ||
| Premenopausal | 296 | 43.3% |
| Postmenopausal | 389 | 56.7% |
| Tumour stage | ||
| EBC | 180 | 26.2% |
| OLBC | 279 | 40.7% |
| LABC | 139 | 20.2% |
| MBC | 87 | 12.7% |
| Type of surgery | ||
| BCS | 135 | 19.7% |
| MRM | 463 | 67.5% |
| Palliative mastectomy | 16 | 2.3% |
Based on the pre operative biopsy the common receptor profile was ER, PR positive and HER 2 negative, which was observed in 57.08% of the patients (n = 391), followed by the triple negative sub type (n = 144; 21.02%).
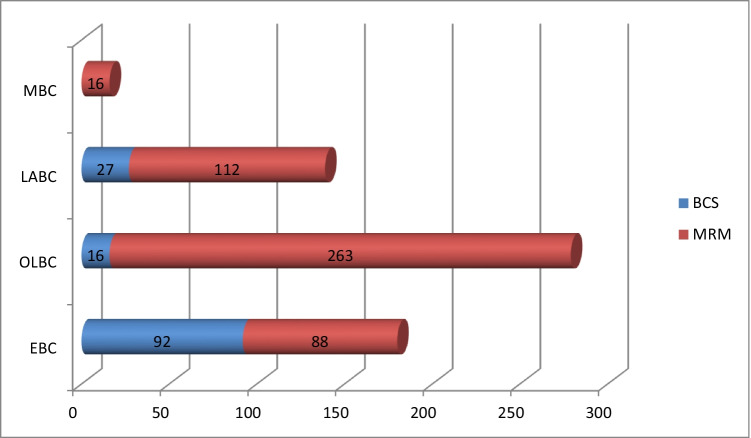
The rate of acceptance of BCS in the early breast cancer subset was only about 51.1% (92 out of 180). Most patients of OLBC underwent a modified radical mastectomy upfront (263 out of 279–94.2%), with only about 5.8% undergoing BCS. On the other hand, 19.4% of LABC patients were able to undergo BCS, possibly because of downstaging by neo-adjuvant chemotherapy. Sixteen patients (18.3%) who presented with metastatic breast cancer needed a palliative total mastectomy either during their chemotherapy or after completion (Table 2, Fig. 1).
Table 2.
Treatment offered v/s stage of the disease
| Initial treatment offered | Early breast cancer (N = 180) | OLBC (N = 279) | LABC (N = 139) | Metastatic breast cancer (N = 87) |
|---|---|---|---|---|
| Surgery | 166 (92.2%) | 223 (79.9%) | 43 (30.9%) | 16@ (18.3%) |
| Neoadjuvant chemotherapy | 14 (7.7%) | 56 (20.1%) | 96 (69.0%) | 0 |
| Palliative chemotherapy | 0 | 0 | 0 | 87 (100%) |
@Palliative mastectomy during/after chemotherapy
Fig. 1.
BCS v/s mastectomy according to tumour stage
The highest rate of BCS was observed in tumours with the receptor subtype ER + ve, PR + ve and HER 2 negative, followed by receptor positive and HER 2-enriched tumours. Whether this has any clinical significance or is a function of the relative prevalence of the receptor phenotypes needs to be explored further (Table 3).
Table 3.
BCS v/s mastectomy with respect to receptor status
| Type of surgery | ER, PR + VE, HER 2 negative (N = 391) | ER, PR + VE, HER 2 enriched (N = 82) | ER − VE, PR − VE, HER 2 enriched (N = 68) | Triple negative (N = 144) |
|---|---|---|---|---|
| BCS (n = 135) | 78 | 22 | 16 | 19 |
| MRM (n = 479) | 296 | 58 | 32 | 93 |
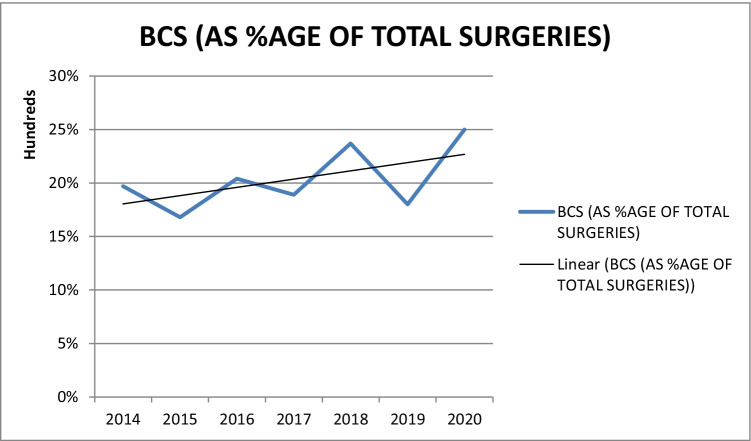
One of the main objectives of the study was to chart the use of BCS over time in our institute, and we found that over 7 years, the percentage of BCS done as a function of all breast cancer surgeries increased from 16.79 to 25% (2014 to 2020) (Fig. 2).
Fig. 2.
Trend of breast conservation surgery over time
On analysing the failure patterns in the patient population, we found that the BCS group had a 11.8% local recurrence rate; whereas in the MRM subset, this was 4.5%. Distant metastases were detected in 18.5% of patients who underwent MRM and 13.3% of patients in the BCS sub group (Table 4).
Table 4.
Patterns of failure (BCS v/s MRM)*@
| Surgery | No disease at last follow-up | Local recurrence | Distant metastases |
|---|---|---|---|
| BCS (n = 135) | 81 (60%) | 16 (11.8%) | 18 (13.3%) |
| MRM (n = 479) | 346 (72.2%) | 22 (4.5%) | 89 (18.5%) |
*@Last follow-up as of December 2020
Discussion
On the basis of evidence from numerous randomised trials, breast conservation surgery (BCS) has been accepted as the standard of care in early breast cancer (EBC) [3]. Selected cases of OLBC and LABC can also be offered BCS, without detrimental effect on the local recurrence rates or survival [4]. The utilisation of BCS varies widely between countries (67 to 85% in the Western hemisphere versus 11 to 23% in the Indian subcontinent), and also within the Indian sub-continent [2]. The socio-economic status of the population catered to, adequate surgical training, awareness of the patients, and availability of neo-adjuvant and adjuvant therapy are all parameters which determine whether an individual is offered BCS or mastectomy. A very important factor in this decision is the patient’s preference for a particular type of surgery, which usually tends towards mastectomy in India, irrespective of the stage of the disease.
The median age of our patients was 44 years, which is in accord with most studies from the Indian subcontinent. This is about a decade younger than what is reported from the West and is more likely due to the population demographic of our country, with a greater proportion of younger people, rather than indicating a difference in the biological behaviour of the tumour [5].
A total of 41% of our patients presented with tumours which were clinically T3N0, reflective of late presentation to the hospital, possibly due to the lack of public awareness and the absence of population-based screening programmes. This also indicates a clear divide between the patient cohort treated in a tertiary care referral centre in the public sector, as compared to some papers reporting a greater proportion of early breast cancers [6, 7].
The use of neo-adjuvant chemotherapy to downstage and downsize tumours to enable BCS has been well-described and now, universally accepted [8]. A total of 19.4% of LABC patients in our study underwent BCS after demonstrating an excellent response to neo-adjuvant chemotherapy. However, an overwhelming number of OLBC patients (94.6%) underwent mastectomy. Even in patients who presented with early breast cancer, only about 51.1% were willing to undergo BCS.
The impact of receptor status on the type of surgery is not very well studied. Tumours which overexpress HER 2 may have multi-centric disease, extensive lymph node involvement and positive cavity margins — and these patients are more likely to be offered a mastectomy by the treating surgeon [9, 10]. About 57.5% of the patients in our study had tumours which were ER and PR positive and HER 2 negative, but even in this subset, 75.7% of patients opted for mastectomy.
An increasing trend of the use of BCS over time has been reported by many papers from the Indian subcontinent [11]. The same was noted in our study, though this increase (from 16.7% in 2014 to 25% in 2020) has not been as rapid as the other reports [12]. We attribute this relatively lower rate and gradual rise to a greater proportion of OLBCs in our cohort and also to the preference of 49% of the patients with EBC for mastectomy. A lack of awareness about the biological behaviour of the tumour and a preference for mastectomy in patients are also contributory factors for the low rates of BCS in our study.
The local recurrence rate of 11.8% for the patients who underwent breast conservation did not affect their survival, and all of them were salvaged with a mastectomy or re-excision. This data correlates well with the report from India by Dinshaw et al. [13].
Age of the patient did not play a significant role in their decision to undergo mastectomy, in our patient cohort. A deep rooted belief that extirpation of the entire organ would lead to a longer life span was what prompted most of them to ask for a mastectomy.
Breast conservation surgery is a resource intense procedure which needs close cooperation between the surgeon, pathologist, radiologist, medical oncologist and radiation oncologist to deliver optimum results but is oncologically safe and feasible even in middle income nations like India [14, 15].
Conclusion
Breast conservation surgery is crucial in preserving the body image and self-esteem of patients with breast cancer. The increase in breast conservation surgeries in our unit can be attributed to improvement in patient counselling, better surgical training and the increased use of preoperative systemic therapy. Increasing the awareness about the disease in the lay public, multi-disciplinary treatment planning and adequate surgical training will help us to preserve the breast in a greater number of women, and this should be the goal to strive for.
Declarations
Ethics Approval
None (Approval obtained from Institute Ethics Committee).
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cancer fact sheet (2020) – India. Globocan 2020; IARC March 2021(1–2)
- 2.Raina V, Bhutani M, Bedi R, Sharma A, Deo SVS, Shukla NK, et al. Clinical features and prognostic factors of early breast cancer at a major centre in North India. Indian J Cancer. 2005;42:36–41. doi: 10.4103/0019-509X.15099. [DOI] [PubMed] [Google Scholar]
- 3.Fisher B, Redmond C, Poisson R, Margolese R, Wolmark N, Wickerham L, et al. Eight year results of a randomised clinical trial comparing total mastectomy and lumpectomy with or without irradiation in the treatment of breast cancer. NEJM. 1989;320:822–828. doi: 10.1056/NEJM198903303201302. [DOI] [PubMed] [Google Scholar]
- 4.Tewari M, Krishnamurthy A, Shukla HS. Breast conservation in locally advanced breast cancer in developing countries: wise or waste. Surg Oncol. 2009;18:3–13. doi: 10.1016/j.suronc.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Narendra H, Ray S. Breast conserving surgery for breast cancer: single institutional experience from Southern India. Indian J Cancer. 2011;48(4):415–422. doi: 10.4103/0019-509X.92260. [DOI] [PubMed] [Google Scholar]
- 6.Shaziya Hassan A, Somashekhar SP, Arun Kumar N. Rate of breast conserving surgery versus mastectomy in breast cancer; a tertiary care centre experience from South India. IJSO. 2019;10(1):72–76. doi: 10.1007/s13193-018-0818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma MM, Chauhan A. Oncoplastic breast surgery: initial experience in an oncology centre. Med J Armed Forces India. 2014;70:175–178. doi: 10.1016/j.mjafi.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tiezzi DG, Andrade JM, Marana HR. Breast conserving surgery after neoadjuvant therapy for large primary breast cancer. Eur J Surg Oncol. 2008;34:863–867. doi: 10.1016/j.ejso.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 9.Desai SB, Moonim MT, Gill AK, Poonia RS, Naresh KN, Chinoy RF. Hormone receptor status of breast cancer in India – a study of 798 tumors. Breast. 2000;9:267–270. doi: 10.1054/brst.2000.0134. [DOI] [PubMed] [Google Scholar]
- 10.Kumar N, Patni P, Agarwal A, Khan MA, Parashar N (2015) Prevalence of molecular subtypes of invasive breast cancer: a retrospective study. Med J Armed Forces India 71(3):254–8 [DOI] [PMC free article] [PubMed]
- 11.Bharath Rangarajan, Tanuja Shet, Tabassun Wadasadawala, Nita S Nair, R Madhu Sairam, Sachin S Hingmire et al (2016) Breast cancer: an overview of published Indian data. South Asian J Cancer 5(3) 86–92. [DOI] [PMC free article] [PubMed]
- 12.Morrow M, Jagsi R, Alderman AK. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA. 2009;302:1551–1556. doi: 10.1001/jama.2009.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ketayun A. Dinshaw, Rajiv Sarin, Ashwini N Budrukkar, Shyam Kishore Shrivastava, Deepak Dattatraya Deshpande et al (2006) Safety and feasibility of breast conserving therapy in Indian women: two decades of experience at Tata Memorial Hospital. JSO 94 105–113. [DOI] [PubMed]
- 14.Murugappan K, Apoorva Saboo Lu, Kuo OU. Paradigm shift in the local treatment of breast cancer: mastectomy to breast conservation surgery. Gland Surg. 2018;7(6):506–519. doi: 10.21037/gs.2018.09.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacobson JA, Danforth DN, Cowan KH. Ten year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med. 1995;332:907–911. doi: 10.1056/NEJM199504063321402. [DOI] [PubMed] [Google Scholar]