Abstract
There is near consensus that prophylactic lateral neck dissection has no role in the management of differentiated thyroid cancer, but the extent of lateral neck dissection in differentiated thyroid cancer remains controversial, especially whether level V should be addressed or not. There is lot of heterogeneity in reporting of the management of level V in papillary thyroid cancer. We at our Institute address the lateral neck positive papillary thyroid cancer with selective neck dissection involving levels II–IV, performing extended level IV dissection with inclusion of the triangular area delineated by the sternocleidomastoid muscle, the clavicle, and the perpendicular line drawn to the clavicle from the point where the horizontal line at the level of cricoid cuts the posterior border of sternocleidomastoid muscle. Retrospective analysis of the departmental data set related to thyroidectomy with lateral neck dissection from 2013 to mid-2019 for papillary thyroid cancer, was carried out. Patients with recurrent papillary thyroid cancer were excluded as were patients with involvement of level V. Data related to the demography of patients, histological diagnosis, and postoperative complications were compiled and summarized. Note was made of the incidence of ipsilateral neck recurrence and the neck level involved with recurrence noted. Data was analyzed for fifty-two patients of non-recurrent papillary thyroid cancer who had undergone total thyroidectomy and lateral neck dissection involving levels II–IV, with extended dissection at level IV. It should be noted that none of the patients had clinical involvement of level V. Only two patients had lateral neck recurrence, both the recurrences were in level III, one on the ipsilateral side and the other on the contralateral side. Recurrence in the central compartment was noted in two patients, with one of these patients also having ipsilateral level III recurrence. One of the patients had distal metastasis to the lungs. Transient paresis of the unilateral vocal cords was noted in seven patients which got resolved within 2 months in all of them. Transient hypocalcemia was noted in four patients. Although our series has a small sample size with limited follow-up, it is one of the few studies in which prophylactic level V dissection has been studied in a homogenous study population of non-recurrent papillary thyroid cancer. Our study has shown that prophylactic dissection of level V may have a limited role, but further large multi-institutional studies need to be carried out to come up with a definite answer.
Keywords: Prophylactic lateral neck dissection, Thyroid cancer, Limited prophylactic clearance
Introduction
There is near consensus that prophylactic lateral neck dissection has no role in the management of differentiated thyroid cancer (DTC), but the extent of therapeutic lateral neck dissection in differentiated thyroid cancer remains controversial. The main controversy pertaining to therapeutic neck dissection in DTC is the management of levels IIb and V. There is lot of heterogeneity in published literature regarding the management of level V in papillary thyroid cancer (PTC). Published articles detailing the management of level V in PTC are not clear whether level V in the published series was addressed prophylactically as part of therapeutic neck dissection or level V was involved in the first place. There is also variation in the extent to which level V needs to be removed, i.e., whether only sublevel Va or Vb or both sublevels need to be removed [1]. Moreover, level V dissection adds morbidity to the procedure, and various studies have documented increased shoulder morbidity after clearance of the posterior triangle of the neck [2].
We at our Institute address the node-positive PTC (without clinically involved level V nodes) with selective neck dissection involving levels II–IV, performing extended level IV dissection. The extended level IV dissection besides removing level IV involves removal of additional lymphatic tissue delineated by a triangular area lateral to level IV. We perform the neck dissection utilizing the lower neck crease and do not extend our incision into the level V area. Once the flaps are raised and level IV is being cleared, a triangular area of level V soft tissue gets delineated lateral to level IV due to the oblique course of the sternocleidomastoid muscle from the mastoid to clavicle, accommodating for a considerable area of level V. We believe that in the absence of any watershed boundary between levels IV and Vb, incorporating this sizable chunk of lymphatic tissue lateral to level IV constitutes an optimal addition to classic clearance of levels II to IV in PTC without the need for formal level Vb clearance, thus sparing the patient of shoulder morbidity due to CN XI dissection. We here in present our data with regard to ipsilateral neck recurrence in node-positive PTC using this approach.
Materials and Methods
Retrospective analysis of the departmental data set related to thyroidectomy with lateral neck dissection from 2013 to mid-2019 for differentiated thyroid cancer, was carried out in our Institute, which is a tertiary care cancer hospital. We have a prospectively maintained database for all operated patients, and retrospective analysis of this database was carried out after obtaining permission from the institute’s ethics committee. Patients with, non-papillary thyroid cancer, aggressive PTC variants, recurrent papillary thyroid cancer, and patients having undergone less than level II to IV neck dissection, were excluded as were patients with clinically involved level V lymph nodes. Thus, patients with non-recurrent PTC with involvement of lateral neck nodes except level V constituted the study sample. Data related to demography of patients, histological analysis, and postoperative complications were compiled and summarized. All the patients with thyroid cancer in our department are subject to neck ultrasonography (USG) prior to surgery to delineate the levels of neck nodes involved clinically. The ultrasonographic features of neck nodes predictive of malignancy which are looked for during sonography include microcalcifications (sensitivity 5–69%, specificity 93–100%), cystic nature (sensitivity 10–34%, specificity 91–100%), peripheral vascularity (sensitivity 40–86%, specificity 57–93%), hyperechogenicity (sensitivity 30–87%, specificity 43–95%), and round shape (sensitivity 37%, specificity 70%) [3]. In case of equivocal USG findings, USG-guided fine-needle aspiration cytology was carried out. In light of sensitivity and specificity limitations, six out of 52 patients who underwent neck dissection were reported in our series as node negative on final histopathology. These six patients were excluded in neck recurrence and survival analysis. All the patients received 100 mCi of adjuvant radioactive iodine as per departmental nuclear medicine protocol. The patients were followed for a median period of 36 months. Note was made of the incidence of ipsilateral neck recurrence as well as the pattern of neck recurrence.
Operative Technique
All the study patients underwent total thyroidectomy, with central neck dissection and selective neck dissection of levels II–IV, with extended dissection at level IV. Our technique of thyroidectomy has been previously published [4]. The dissection at level IV besides removing level IV involved removal of additional lymphatic tissue delineated by a triangular area formed medially by the posterior border of the sternocleidomastoid muscle, inferiorly by the clavicle, and laterally by a perpendicular line drawn to the clavicle from the point where the horizontal line at the level of the cricoid cuts the posterior border of the sternocleidomastoid muscle (Fig. 1).
Fig. 1.
Triangular demarcated area showing the anatomic boundaries of level IV extension
Statistical Analysis
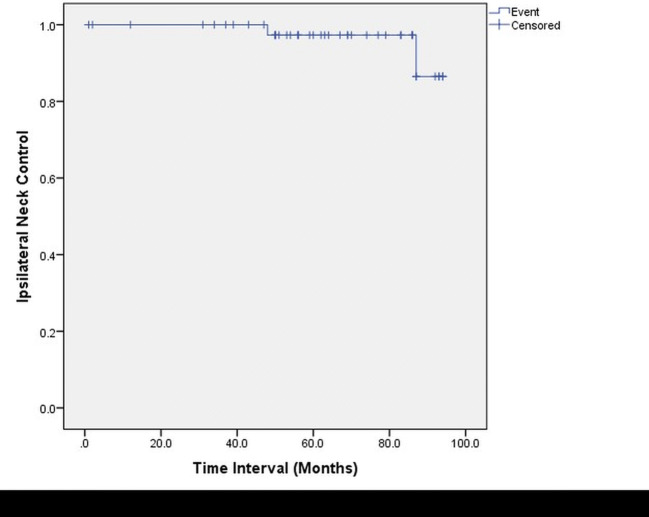
The relations among various variables were summarized in 2 × 2 tables. The categorical data were analyzed by the 2-tailed Fisher exact test, followed by multivariate analysis. A P value less than .05 was considered statistically significant. Kaplan-Meier estimates were performed for the ipsilateral regional control rate. These calculations were performed using SPSS 16.0 (SPSS, Inc., Chicago, IL).
Results
Data was analyzed for fifty-two patients of non-recurrent papillary thyroid cancer who had undergone total thyroidectomy and lateral neck dissection involving levels II–IV, with extended dissection at level IV. Demographic and clinico-pathological variables of operated cases are shown in Table 1. It should be noted that none of the patients had clinical involvement of level V. T1/T2 lesions constituted the majority of thyroid tumors in our series. Six patients who had histologically negative lateral neck were excluded from further analysis. Total of 49 neck dissections were performed in the remaining 46 patients, three neck dissections were performed bilaterally. None of the cases had level V (extended level IV) positive nodes on final histopathology. Levels II, III, and IV were involved combinedly in 31% of necks (Table 2). Levels II, III, and IV were involved in 33, 32, and 29 out of total of 49 neck dissections, respectively. Majority of patients (25 out of 46 necks dissections) had lymph node ratio, i.e., ratio of positive nodes to total nodes harvested, of < 1:4 and only three necks had lymph nodes greater than 3 cm. Only two patients had lateral neck recurrence, both had recurrence in level III, one on the ipsilateral side and the other on the contralateral side. Both the patients had recurrence after 1 year of their initial surgery. Recurrence in the central compartment was noted in two patients, with one of these patients also having ipsilateral level III recurrence. None of the demographic and histopathological variables had statistically significant association with ipsilateral neck recurrence (Table 3). Figure 2 shows Kaplan-Meier curve for ipsilateral neck control. One of the patients had distal metastasis to the lungs. Surgical complications of operated patients are shown in Table 4. Transient paresis of unilateral vocal cords was noted in six patients which got resolved within 2 months in all of them. Transient hypocalcemia was noted in four patients.
Table 1.
Demographic and clinico-pathological variables of operated cases (total patients = 52)
| Variable | Number (%) |
|---|---|
| Age | |
| <55 years | 49 (~94%) |
| Sex | |
| Female | 33 (~64%) |
| Clinical T stage | |
| T1 | 30 (~58%) |
| T2 | 11 |
| T3 | 08 |
| T4 | 03 |
| Pathological T stage | |
| T1 | 32 (~62%) |
| T2 | 12 |
| T3 | 04 |
| T4 | 04 |
| Extrathyroidal extension | |
| Absent | 46 (~88.5%) |
| Present | 06 |
| Focality | |
| Unifocal | 42 (~81%) |
| Multifocal | 10 |
| Pathological lesion size | |
| <5 cm | 51 (~98%) |
| >5 cm | 01 |
| Capsular invasion | |
| Present | 36 (~69%) |
| Absent | 16 |
| Vascular invasion | |
| Present | 38 (~73%) |
| Absent | 14 |
| Extracapsular spread | |
| No | 47 (~90%) |
| Yes | 05 |
Table 2.
Pattern of lymph node involvement in patients with pathologically positive lateral nodes
| Variable | Number (total 49 neck dissections) |
|---|---|
| Lymph node levels involved | |
| II+III+IV | 15 (~31%) |
| II+III | 07 (~14%) |
| II+IV | 04 (~8%) |
| III+IV | 05 (~10%) |
| II | 07 (~14%) |
| III | 05 (~10%) |
| IV | 06 (~12%) |
| VI | 27 |
| Lymph node ratio | |
| <1:4 | 25 |
| 1:4 to 2:4 (1:2) | 19 |
| 2:4 to 3:4 | 05 |
| >3:4 | Nil |
| Any of the lymph nodes >3 cm | |
| Absent | 46 |
| Present | 03 |
Table 3.
Correlation of demographic and clinico-pathological variables of pathologically positive cases (number = 46), with ipsilateral neck recurrence
| Variable | Ipsilateral neck recurrence | Univariate analysis | Multivariate analysis |
|---|---|---|---|
| Age | 1.00 | 0.56 | |
| <55 years | 02 | ||
| >55 years | |||
| Sex | 1.00 | 0.61 | |
| Female | 01 | ||
| Male | 01 | ||
| Clinical T stage | 1.00 | 0.69 | |
| T1 | 02 | ||
| T2 | |||
| T3 | |||
| T4 | |||
| Pathological T stage | 1.00 | 0.63 | |
| T1 | 02 | ||
| T2 | |||
| T3 | |||
| T4 | |||
| Extrathyroidal extension | 1.00 | 0.97 | |
| Absent | 02 | ||
| Present | |||
| Focality | 0.39 | 0.50 | |
| Unifocal | 01 | ||
| Multifocal | 01 | ||
| Pathological lesion size | 1.00 | 0.97 | |
| <5 cm | 02 | ||
| >5 cm | |||
| Capsular invasion | 1.00 | 0.99 | |
| Present | |||
| Absent | 01 | ||
| Vascular invasion | 01 | 0.45 | 0.73 |
| Present | 01 | ||
| Absent | 01 | ||
| Extracapsular spread | 0.20 | 0.06 | |
| No | 01 | ||
| Yes | 01 | ||
| Central compartment involvement | |||
| Present | 02 | 1.00 | 0.97 |
| Absent | |||
Fig. 2.
Kaplan-Meier curve showing ipsilateral neck control
Table 4.
Various complications noted in operated patients
| Variable | Number |
|---|---|
| Recurrent laryngeal nerve palsy | |
| Transient | 06 |
| Permanenta | 01 |
| Hypocalcemia | |
| Transient | 04 |
| Permanent | Nil |
| Seroma/hematoma | 02 |
| Percutaneous fistula + tracheomalacia | 01 |
aRecurrent laryngeal nerve had to be sacrificed as it was involved by the tumor
Discussion
The final answer to level II–IV versus level II–V selective neck dissection in node-positive PTC patients is far from categorical, with pros and cons for both approaches. In our opinion, answer to such a question has to come from protocol-based studies, with homogenous study population answering the right question, i.e., recurrence in level V when not addressed prophylactically in a node-positive PTC. Our study, though having a comparatively small sample size, involved selective neck dissection of levels II–IV (extended IV), in PTC patients presenting with lateral neck node involvement upfront. In our study, no recurrent cases of PTC were included in the study sample. Thus, our study has a homogenous study population of newly diagnosed PTC patients with lateral neck node involvement excluding level V, in which selective neck dissection of levels II to IV was carried out, without addressing level V prophylactically. The primary end point of our study was to note ipsilateral neck recurrence in level V, not addressed prophylactically.
Sivanandan et al. [5] evaluated the pattern of lymph node metastases in 70 PTC patients who underwent 80 neck dissections. Comprehensive neck dissection involving dissection of levels I–V was carried out. Level V was positive in 23 out of 80 neck dissection specimens; however, level V nodes were not segregated into sublevels Va and Vb. Moreover, authors did not comment on percentage of level V positive nodes in clinically negative level V necks. Level V was not involved in isolation, although 14 (18%) specimens had single-level disease.
Pingpank et al. [6] evaluated 44 patients of PTC who underwent 51 comprehensive neck dissections involving levels I through V. Level V was positive for metastases in 14 out of 50 specimens. Lateral neck control was achieved in 35 (80%) out of 44 necks. Like a previous study of Sivanandan et al., the study sample was a mixed bag of new and previously treated cases.
Kupferman et al. [7] studied 39 patients of PTC, in whom 44 neck dissections involving dissection of levels II through V were carried out. Study involved evaluation of both new and recurrent cases. Out of 44 neck dissection specimens, 4 were negative for malignancy. Level V was involved in 9/44 (20%) neck dissection specimens Three patients each had disease at level III, IV, or V. Since level V was not dissected as sublevels, no distinction could be made as to how many had involvement of level Va, Vb, or both.
Lee et al. [8], evaluated 46 newly diagnosed cases of PTC, with clinical disease documented by ultrasonography, computed tomography (CT), and fine-needle aspiration cytology (FNAC). Fifty-five neck dissections involving levels II through V were performed. Although level V was involved in 11 (20%) specimens, it was not involved alone in any specimen. Once again, this study failed to make any distinction between various sublevels of level V and it showed high-level IIb involvement.
Ahn et al. [9], in their report of 37 patients undergoing total thyroidectomy and lateral (n = 28) or central (n = 9) neck dissection, noted that level V was positive in only 4 out of 26 (15%) neck specimens. For level V, positive predictive values for both USG and CT were 100%. One wonders that with such a high diagnostic accuracy, why is it not possible to dissect levels with not so high percentage involvement like IIb and V, only if they are highly suspicious on imaging studies.
Khafif et al. [10] studied 37 PTC patients, of which 11 were previously operated for thyroid without addressing the neck. Levels II–IV were dissected in 31 patients and II–V in 6 patients. Level V was dissected only when it was involved or retro-jugular nodes were involved; level V was involved only in five patients.
Kupferman et al. [11] evaluated predictors of level V metastasis in 70 patients of differentiated thyroid carcinoma who underwent 75 neck dissections ranging from radical to selective neck dissections. Both previously treated as well as new cases were included, 33% had prior neck dissection whereas 31% had prior neck biopsy. There were six cases of follicular carcinoma. Fifty-three percent (53%) of ipsilateral neck specimens had positive level V and 57% of contralateral neck specimens had disease. The presence of ipsilateral level V metastases was significantly associated with multifocal disease (P < .05) and ipsilateral level II (P < .05), III (P < .05), or IV (P < .01) metastases; also, ipsilateral involvement of level V was associated with contralateral lymph node metastases (P < .05). Isolated Level V positivity was seen in only 5% of specimens. One of the biggest drawbacks of this study viz-a-viz pattern of nodal metastasis in PTC is that it included patients with operated necks, besides having six follicular thyroid carcinoma patients.
Lee et al. [12] analyzed 167 patients of PTC who underwent 191 modified radical neck dissections (MRND). Modified radical neck dissections addressed levels II through V, being carried out upfront in 73% of necks whereas remaining 23% necks were recurrent necks. Level V nodes were involved in 16.8% of neck dissection specimens. No isolated level V metastasis was documented. This study did not detail the handling of level V nodes and sublevels of level V were not commented upon.
Roh et al. [13] evaluated fifty-two patients of PTC who underwent 57 modified radical neck dissections—Ib–V. All the patients were new cases and were evaluated with USG and FNAC before surgery. Level Va was divided into sublevels Vas (superior to spinal accessary nerve) and Vai (between the spinal accessary nerve and transverse line drawn at the level of cricoid). Out of 54 ipsilateral necks, seven necks were positive for Vai (13%). Levels V and IIb were not involved in isolation and were always associated with disease at other levels. Vai and Vb were positive for metastasis in 7 (13.0%) and 2 (3.7%) specimens; however, both the Vb-positive cases had negative Vai nodes. This study is one of the few studies which has mentioned in detail various sublevels of level V and has shown that level V is not so commonly involved.
Yanir et al. [14] evaluated 27 patients of well-differentiated thyroid carcinoma who underwent 28 selective neck dissections. Patients were evaluated with physical examination and CT, and 16 patients had upfront neck dissections while 11 had neck dissection after primary thyroid surgery. Three patients had follicular carcinoma. All the patients received radioactive iodine; hence, interval neck dissection patients (operated for neck pathology after a varying time interval after primary thyroidectomy) had received it prior to neck dissection. Twenty-four patients (25 necks) underwent selective neck dissection (SND) including levels II through VI, whereas three patients had SND including levels II–IV and VI. Level V was involved in 20% of neck dissections, and four out of six necks positive for level V metastasis had also level IV metastasis while two patients were positive at level V without level IV involvement. The study has heterogeneous patient population with a limited patient number.
Farrag et al. [15] analyzed 53 PTC patients who underwent therapeutic lateral neck dissection that included levels II (a & b) and/or level V (a & b). Only 10 of these patients were new cases, all others were either recurrent cases or cases with residual disease. Level V was excised 40 times and was positive in 16 specimens (16/40 = 40%). Level Va was not positive even in a single specimen. This study does not mention the basis on deciding whether or not to treat level V in these patients.
Koo et al. [16] evaluated 76 PTC patients with USG/CT and FNAC. There were 57 new patients and 19 recurrent patients, who underwent therapeutic lateral neck dissection of levels II through V. Level V metastasis was present in 12 out of 76 (15.8%) neck dissection specimens. This study, like many previous studies, addressed both new and recurrent cases and did not have a high percentage of level V involvement; moreover, level V was not reported in terms of sublevel involvement.
Lim et al. [17] evaluated 70 patients of PTC for occult disease at level V. Fifty-six patients underwent primary thyroidectomy and level II–V neck dissection, while 14 patients had salvage neck dissection for recurrence. All the patients had no suspicious nodes detected on USG at level V. Occult metastases at level V were observed in 11 (16%) patients. According to the subgroups of level V, eight patients had occult lymph node metastases at level Va, four patients had occult metastases at level Vb, and one patient had positive lymph nodes at both levels Va and Vb. No positive level V lymph nodes were found in 19 patients without suspicious metastatic lymph nodes at level IV. All the 11 patients confirmed as having a metastatic level V lymph node histopathologically were among the 51 patients, who had suspicious level IV lymph node metastasis on preoperative USG. This study probably hints at doing a more dedicated USG of the neck particularly levels IV and V, to further modify the levels to be included in the neck dissection.
Vayisoglu et al. [18] performed 47 neck dissections on 33 consecutive PTC patients. Neck dissection of levels II to V was carried out. Out of 33 patients, three patients were recurrent. Only 22 (46.8%) out of 47 neck dissections were positive for metastases and 18% of level V dissections were positive for metastases in node-positive necks. On considering all neck dissections, level V nodes were positive in only 8.5% of specimens. The study has an unusually low histological positive yield for necks operated upon with therapeutic purpose and has shown very low level V involvement.
Yuce et al. [19] studied the regional metastatic pattern in 48 PTC patients who underwent 61 neck dissections (levels II–VI). Seven patients had subtotal thyroidectomy performed previously, who underwent completion thyroidectomy and neck dissection. Level V was positive in 21/61 (34%) neck specimens. The study does not comment upon various level V sublevels, although it has shown high percentage involvement of level V.
King et al. [20] studied the management of lateral cervical metastases in 32 PTC patients who underwent 39 level II to VI neck dissections, in which 14 patients were operated for recurrent neck pathology. Level Va was involved in 8% (3/39) and level Vb in 31% (12/39) of neck specimens. This study like majority of previous studies detailed above, has shown a low level Va involvement.
Merdad et al. [21] have published the largest series on the pattern of neck nodes in PTC. They evaluated 185 patients with FNAC-confirmed lateral neck node involvement who underwent 248 neck dissections. Forty-four percent of patients had selective neck dissection of levels II through Vb for recurrent disease in the lateral neck and 56% had neck dissection at the time of their total thyroidectomy. Level Vb was found to harbor metastasis in 72 (29%) of patients. The authors while describing their approach to neck have detailed that they approach the posterior triangle of the neck at the level of spinal accessary nerve and dissect caudally. As per American Head and Neck Society consensus statement on the classification and terminology of neck dissection [22], the area between spinal accessory nerve and transverse line drawn at the level of cricoid is part of level Va; hence, we feel probably authors have included a much larger field of dissection at level Vb and have included a part of sublevel Va. This study also fails to mention about number of patients who had undergone radioactive iodine ablation prior to developing secondary disease in the neck.
Park et al. [23] found level V involvement in only one out of 32 neck dissections in patients with skip lymph node metastases.
Keum et al. [24] found occult metastases at level V in 23.6% of cases; it is of note that authors dissected whole level V although preponderance of literature suggests dissection of level Vb only.
Shim et al. [25] assessed factors predicting level V metastasis in PTC and found macroscopic extranodal extension as a predictive factor for level V metastasis; although eight regional recurrences were observed, none involved level V.
Zhang et al. [26] observed location (whole thyroid), gross extrathyroidal extension, and simultaneous multilevel involvement (level II, III, and IV), as predictive factors for level V metastases.
Kang et al. [27] noted on multivariate analysis that tumor multifocality, image-based independent lateral level IV involvement, and macroscopic extranodal extension were independently associated with level II or V metastasis.
A meta-analysis was carried out by Eskander et al. [28], which detailed the pattern of lateral lymph node involvement in node-positive necks of PTC patients. Before we comment on this meta-analysis, it is worthwhile to know about I2 statistic, which was a static quantity described by Higgins et al. [29], ranging from 0 to 100%, that measures the degree of inconsistency across studies in a meta-analysis. The I2 statistic describes the percentage of variation across studies that is due to heterogeneity rather than chance. In Eskander et al.’ meta-analysis, the degree of heterogeneity between various studies is high and for level V, I2 measures 75.97. Even though authors carried out random model meta-regression analysis of various factors and observed that none of these factors explained or decreased the observed heterogeneity estimates leading to insignificant clinical implications, to us, the degree of heterogeneity is too high and has to be considered as one of the limitations of the study.
Javid et al. [30], in their analysis of PTC patients with lateral neck disease, noted that level V was involved in 12.8% of reoperations done for persistent or recurrent lateral neck disease. It is of note that all these patients had undergone MRND previously, and none of the patients with neck dissection of levels II to IV had level V persistence or recurrence.
Kim et al. [31] analyzed PTC patients with lateral neck node metastases and found level V involved in only 13.8% of 327 patients.
McNamara et al. [32] noted no difference in overall lateral neck recurrence-free status between comprehensive lymph node dissection (CLND) 94.4% and SND 89.4%, P = .15, but in the dissected neck, the ipsilateral lateral neck recurrence-free status was superior in the CLND patients (97.7% vs 89.4%, P < .001). None of the 120 patients who had undergone level II–IV neck dissection had isolated ipsilateral level V recurrence; only two patients had both in and out field ipsilateral neck recurrence, and outfield level of recurrence was not specified.
Kim et al. [33] analyzed 646 PTC patients who had undergone MRND and noticed overall and occult level V metastases in 13.9% and 8.6% of cases. It is of note that there were only two patients with level V recurrence out of 26 patients who recurred; moreover, it is not specified whether these two patients had clinically positive level V on initial imaging.
As can be gleaned from above, the studies quoted have a heterogenous study population, extent of the neck dissection carried out has varied across and within studies, whether level V was removed prophylactically or therapeutically is not clear, and moreover, the bigger question of recurrence at level V when not suspected to be involved preoperatively and subsequently not addressed has not been documented in any of the well-conducted studies. When such a thing is not well documented, quality of life issues has a bigger role to play. Cappiello et al. [2] evaluated shoulder disability after different selective neck dissections (levels II–IV versus levels II–V) and concluded that clearance of the posterior triangle of the neck increases shoulder morbidity.
Our philosophy of addressing clinically node-positive PTC with extended level IV approach limits the functional morbidity without any oncologic compromise. Our study sample, though comparatively small, is homogenous, and we have addressed the node-positive PTC in a protocol-based fashion, involving dissection of levels II–IV (extended level IV). Our study has tried to answer the question of level V recurrence, if not addressed prophylactically in a node-positive PTC. In our series, there was no out-of-field recurrence in level V, and only two recurrences were noted, both the recurrences were in level III, one on the ipsilateral side and the other on the contralateral side.
Conclusions
Although our series has small sample size with limited follow-up, it is one of the few studies in which prophylactic level V dissection has been studied in a homogenous study population of non-recurrent papillary thyroid cancer. Our study has shown that limited prophylactic dissection of level V may be an option to complete removal of level V which has attendant morbidities, but further large multi-institutional studies need to be carried out to come up with a definitive answer.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
No identifying information about participants is available in the article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Azhar Jan Battoo, Email: azatmsy@gmail.com.
Zahoor Ahmad Sheikh, Email: drskzahoor@rediffmail.com.
Jasif Nisar, Email: jasifnisar34@gmail.com.
Krishnakumar Thankappan, Email: drkrishnakumart@gmail.com.
Moni Abraham Kuriakose, Email: makuriakose@gmail.com.
Altaf Gowhar Haji, Email: oncosurgeon69@yahoo.com.
References
- 1.Battoo AJ, Sheikh ZA, Thankappan K, Mir AW, Haji AG. Level V clearance in neck dissection for papillary thyroid carcinoma: a need for homogeneous studies. Int Arch Otorhinolaryngol. 2018;22:449–454. doi: 10.1055/s-0037-1608909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cappiello J, Piazza C, Giudice M, De Maria G, Nicolai P. Shoulder disability after different selective neck dissections (levels II-IV versus levels II-V): a comparative study. Laryngoscope. 2005;115:259–263. doi: 10.1097/01.mlg.0000154729.31281.da. [DOI] [PubMed] [Google Scholar]
- 3.Leenhardt L, Erdogan MF, Hegedus L, Mandel SJ, Paschke R, Rago T, Russ G. European Thyroid Association guidelines for cervical ultrasound scan and ultrasound-guided techniques in the postoperative management of patients with thyroid cancer. Eur Thyroid J. 2013;2:147–159. doi: 10.1159/000354537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Battoo AJ, Haji AG, Sheikh ZA, Thankappan K, Mir WA. Efficacy of drainless total thyroidectomy in intrathyroidal lesions of thyroid. Int Arch Otorhinolaryngol. 2018;22(3):256–259. doi: 10.1055/s-0037-1606183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sivanandan R, Soo KC. Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg. 2001;88:1241–1244. doi: 10.1046/j.0007-1323.2001.01843.x. [DOI] [PubMed] [Google Scholar]
- 6.Pingpank JF, Jr, Sasson AR, Hanlon AL, Friedman CD, Ridge JA. Tumor above the spinal accessory nerve in papillary thyroid cancer that involves lateral neck nodes: a common occurrence. Arch Otolaryngol Head Neck Surg. 2002;128:1275–1278. doi: 10.1001/archotol.128.11.1275. [DOI] [PubMed] [Google Scholar]
- 7.Kupferman ME, Patterson M, Mandel SJ, LiVolsi V, Weber RS. Patterns of lateral neck metastasis in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 2004;130:857–860. doi: 10.1001/archotol.130.7.857. [DOI] [PubMed] [Google Scholar]
- 8.Lee BJ, Wang SG, Lee JC, Son SM, Kim IJ, Kim YK. Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 2007;133:1028–1030. doi: 10.1001/archotol.133.10.1028. [DOI] [PubMed] [Google Scholar]
- 9.Ahn JE, Lee JH, Yi JS, Shong YK, Hong SJ, Lee DH, Choi CG, Kim SJ. Diagnostic accuracy of CT and ultrasonography for evaluating metastatic cervical lymph nodes in patients with thyroid cancer. World J Surg. 2008;32:1552–1558. doi: 10.1007/s00268-008-9588-7. [DOI] [PubMed] [Google Scholar]
- 10.Khafif A, Ben-Yosef R, Abergel A, Kesler A, Landsberg R, Fliss DM. Elective paratracheal neck dissection for lateral metastases from papillary carcinoma of the thyroid: is it indicated? Head Neck. 2008;30:306–310. doi: 10.1002/hed.20696. [DOI] [PubMed] [Google Scholar]
- 11.Kupferman ME, Weinstock YE, Santillan AA, Mishra A, Roberts D, Clayman GL, Weber RS. Predictors of level V metastasis in well-differentiated thyroid cancer. Head Neck. 2008;30:1469–1474. doi: 10.1002/hed.20904. [DOI] [PubMed] [Google Scholar]
- 12.Lee J, Sung TY, Nam KH, Chung WY, Soh EY, Park CS. Is level IIb lymph node dissection always necessary in N1b papillary thyroid carcinoma patients? World J Surg. 2008;32:716–721. doi: 10.1007/s00268-007-9381-z. [DOI] [PubMed] [Google Scholar]
- 13.Roh JL, Kim JM, Park CI. Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Ann Surg Oncol. 2008;15:1177–1182. doi: 10.1245/s10434-008-9813-5. [DOI] [PubMed] [Google Scholar]
- 14.Yanir Y, Doweck I. Regional metastases in well differentiated thyroid carcinoma: pattern of spread. Laryngoscope. 2008;118:433–436. doi: 10.1097/MLG.0b013e31815ae3e4. [DOI] [PubMed] [Google Scholar]
- 15.Farrag T, Lin F, Brownlee N, Kim M, Sheth S, Tufano RP. Is routine dissection of level II-B and V-A necessary inpatients with papillary thyroid cancer undergoing lateral neck dissection for FNA-confirmed metastases in other levels. World J Surg. 2009;33:1680–1683. doi: 10.1007/s00268-009-0071-x. [DOI] [PubMed] [Google Scholar]
- 16.Koo BS, Yoon YH, Kim JM, Choi EC, Lim YC. Predictive factors of level IIb lymph node metastasis in patients with papillary thyroid carcinoma. Ann Surg Oncol. 2009;16:1344–1347. doi: 10.1245/s10434-009-0367-y. [DOI] [PubMed] [Google Scholar]
- 17.Lim YC, Choi EC, Yoon YH, Koo BS. Occult lymph node metastases in neck level V in papillary thyroid carcinoma. Surgery. 2010;147:241–245. doi: 10.1016/j.surg.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 18.Vayisoglu Y, Ozcan C, Turkmenoglu O, Gorur K, Unal M, Dag A, Ocal K. Level IIb lymph node metastasis in thyroid papillary carcinoma. Eur Arch Otorhinolaryngol. 2010;267:1117–1121. doi: 10.1007/s00405-009-1185-3. [DOI] [PubMed] [Google Scholar]
- 19.Yuce I, Cagli S, Bayram A, Karasu F, Guney E. Regional metastatic pattern of papillary thyroid carcinoma. Eur Arch Otorhinolaryngol. 2010;267:437–441. doi: 10.1007/s00405-009-1032-6. [DOI] [PubMed] [Google Scholar]
- 20.King JM, Corbitt C, Miller FR. Management of lateral cervical metastases in papillary thyroid cancer: patterns of lymph node distribution. Ear Nose Throat J. 2011;90:386–389. doi: 10.1177/014556131109000814. [DOI] [PubMed] [Google Scholar]
- 21.Merdad M, Eskander A, Kroeker T, Freeman J. Metastatic papillary thyroid cancer with lateral neck disease: pattern of spread by level. Head Neck. 2013;35(10):1439–1442. doi: 10.1002/hed.23149. [DOI] [PubMed] [Google Scholar]
- 22.Robbins KT, Shaha AR, Medina JE, Califano JA, Wolf GT, Ferlito A, Som PM, Day TA. Committee for Neck Dissection Classification, American Head and Neck Society. Consensus statement on the classification and terminology of neck dissection. Arch Otolaryngol Head Neck Surg. 2008;134(5):536–538. doi: 10.1001/archotol.134.5.536. [DOI] [PubMed] [Google Scholar]
- 23.Park JH, Lee YS, Kim BW, Chang HS, Park CS. Skip lateral neck node metastases in papillary thyroid carcinoma. World J Surg. 2012;36:743–747. doi: 10.1007/s00268-012-1476-5. [DOI] [PubMed] [Google Scholar]
- 24.Keum HS, Ji YB, Kim JM, Jeong JH, Choi WH, Ahn YH, Tae K. Optimal surgical extent of lateral and central neck dissection for papillary thyroid carcinoma located in one lobe with clinical lateral lymph node metastasis. World J Surg Oncol. 2012;10:221–226. doi: 10.1186/1477-7819-10-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shim MJ, Roh JL, Gong G, Choi KJ, Lee JH, Cho SH, Nam SY, Kim SY. Preoperative detection and predictors of level V lymph node metastasis in patients with papillary thyroid carcinoma. Br J Surg. 2013;100:497–503. doi: 10.1002/bjs.9024. [DOI] [PubMed] [Google Scholar]
- 26.Zhang XJ, Liu D, Xu DB, Mu YQ, Chen WK. Should level V be included in lateral neck dissection in treating papillary thyroid carcinoma. World J Surg Oncol. 2013;11:304–307. doi: 10.1186/1477-7819-11-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kang BC, Roh JL, Lee JH, Cho KJ, Gong G, Choi SH, Nam SY, Kim SY. Candidates for limited lateral neck dissection among patients with metastatic papillary thyroid carcinoma. World J Surg. 2013;38:863–871. doi: 10.1007/s00268-013-2361-6. [DOI] [PubMed] [Google Scholar]
- 28.Eskander A, Merdad M, Freeman JL, Witterick IJ. Pattern of spread to the lateral neck in metastatic well-differentiated thyroid cancer: a systematic review and meta-analysis. Thyroid. 2013;23(5):583–592. doi: 10.1089/thy.2012.0493. [DOI] [PubMed] [Google Scholar]
- 29.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Javid M, Graham E, Malinowski J et al (2016) Dissection of levels II through V is required for optimal outcomes in patients with lateral neck lymph node metastasis from papillary thyroid carcinoma. J Am Coll Surg. 10.1016/j.jamcollsurg.2016.02.006 [DOI] [PubMed]
- 31.Kim SK, Park I, Hur N, Lee JH, Choe JH, Kim JH, Kim JS. Routine level 2b dissection may be recommended only in N1b papillary thyroid carcinoma with three- or four-level lateral lymph node metastasis. Ann Surg Oncol doi. 2016;23:694–700. doi: 10.1245/s10434-016-5521-8. [DOI] [PubMed] [Google Scholar]
- 32.McNamara WF, Wang LY, Palmer FL et al (2016) Pattern of neck recurrence after lateral neck dissection for cervical metastases in papillary thyroid cancer. J Surg. 10.1016/j.surg.2016.02.005 [DOI] [PMC free article] [PubMed]
- 33.Kim SK, Park I, Hur N, Lee JH, Choe JH, Kim JH, Kim JS. Should level V be routinely dissected in N1b papillary thyroid carcinoma. Thyroid. 2016;27:253–260. doi: 10.1089/thy.2016.0364. [DOI] [PubMed] [Google Scholar]