Abstract
Background
Both men and women can have a wide range of physical, emotional, and sexual issues as a result of diabetes. One of them is sexual dysfunction, which has an effect on marital relationships as well as the effectiveness of therapy and can develop into a serious social and psychological condition. As a result, the purpose of this study was to identify the global prevalence of sexual dysfunction among diabetic patients.
Methods
Science Direct, Scopus, Google Scholar, and PubMed were all searched for information. Data were extracted using Microsoft Excel (v. 14), STATA statistical software, and STATA. Publication bias was investigated by a forest plot, rank test, and Egger's regression test. To detect heterogeneity, I2 was calculated and an overall estimated analysis was performed. Subgroup analysis was done by study region and sample size. The pooled odds ratio was also computed.
Results
The study was able to include 15 of the 654 publications that were evaluated since they met the criteria. 67,040 people participated in the survey in all. The pooled global prevalence of sexual dysfunction among diabetic patients was 61.4% (95% CI: 51.80, 70.99), I2 = 71.6%. The frequency of sexual dysfunction was highest in the European region (66.05%). For males, the prevalence of sexual dysfunction was 65.91%, while for females, it was 58.81%. Patients with type 2 diabetes mellitus were more likely (71.03%) to experience sexual dysfunction.
Conclusion
Finally, sexual dysfunction was fairly common all across the world. There were variations in the prevalence of sexual dysfunction depending on the sex, type of diabetes, and location of the study participant. Our findings imply that screening and appropriate treatment are required for diabetes persons exhibiting sexual dysfunction.
Keywords: Sexual dysfunction, Diabetic mellitus, Systematic review, And meta-analysis
1. Introduction
Diabetes mellitus, which is characterized by improper glucose metabolism and a deficiency of fat and protein, are all signs of the medical disorder. It is one of the most widespread and severe chronic diseases in the world, affecting about 2–5% of persons in industrialized countries [1]. By 2025, diabetes is expected to affect 380 million people, up from the current 246 million cases reported globally. Additionally, by 2025, diabetes prevalence will increase most rapidly in underdeveloped countries [2]. The International Federation of Diabetes reports that 5 million people between the ages of 20 and 79 have diabetes [3].
Sexual dysfunction is prevalent among people with diabetes [4]. According to studies, men with diabetes develop sexual dysfunction more frequently and earlier than men without diabetes [[4], [5], [6]]. It results in reduced levels of marital satisfaction, emotional stress, less communication, and challenges with problem-solving, and eventually, it may lead to divorce [7,8].
The term “sexual dysfunction” (SD) refers to a multi-factorial, heterogeneous group of illnesses that might present in various ways, but are primarily recognized by clinically significant impairments in a person's capacity to engage in or enjoy sexual activity [[9], [10], [11]]. Patients of both sexes are vulnerable to disorders [12]. Sexual dysfunction is more directly correlated with men's physical health, including illnesses associated with age and chronic disease [[13], [14], [15]] Arousal disorders, such as erectile dysfunction (ED), and orgasm disorders, such as premature, retrograde ejaculation and anorgasmia, are included in the sexual response cycle, which is used to describe the difficulties experienced by males [16,17]. Patients with chronic diseases are more prone to experience sexual dysfunction brought on by physiological disruption, drug side effects, emotional disturbance, or a combination of these factors [18].
Numerous factors, including psychogenic, hemodynamic, neurogenic, hormonal, and smooth muscle atrophy within the corpus cavernous bodies, contribute to sexual dysfunction associated with diabetes [19]. Studies in general show that women with diabetes have greater rates of sexual dysfunction than their counterparts, and diabetes-related comorbidities may make these patients' sexual dysfunction problems worse [8]. The most prevalent sexual problems in females with diabetes include lubrication, orgasmic disorder, sexual desire, sexual satisfaction, and orgasmic disorder [20,21]. The Intrusions vagina, labium minora, and clitoris are the most seriously damaged genital regions in diabetic women, indicating that the somatic sensory system may be affected by diabetes. Drugs can increase clitoral blood flow, even though sexual problems do not always manifest as expected [22,23].
Additionally, patients with this long-lasting illness may experience severe ocular, renal, and neuropathic repercussions such as blindness, renal failure, cardiovascular disease, amputation, and paralysis [[24], [25], [26]]. Such chronic and incapacitating illnesses have a major impact on the patient's capacity and day-to-day activities, which in turn affects their quality of life [27] No matter the variety of sexual desires that serve as the basis for important behaviors and promote sexual health, the WHO defines sexual health as a physical, emotional, psychological, and social well-being in terms of sexual desire, not just the absence of disease, dysfunction, or disability [28]. A set of diseases known as sexual dysfunction includes abnormalities in women's orgasm, arousal, pain, and unexplained sexual problems [29].
On the one hand, diabetic patients' sexual health has frequently been overlooked as a component of care, likely because many people still consider it taboo and don't discuss it [30]. Although several primary studies looked at sexual dysfunction in diabetic patients, there are no statistics at the global level. The objective of this study was to assess the overall global prevalence of sexual dysfunction in people with diabetes. The study's findings will enable clinicians and other interested parties to close any operational plan gaps and provide them with the crucial knowledge they need to manage and treat sexually dysfunctional individuals.
2. Methods
2.1. Reporting
Based on a single measurement result (sexual dysfunction), data analysis was done. The findings are displayed using tables, text, and a forest plot. This systematic review and meta-analysis study was carried out to determine the global prevalence of sexual dysfunction using the standard Meta-analysis Of Observational Studies in Epidemiology (MOOSE) method [31]. (Supplementary file1).
2.2. Search strategy
We thought about employing modified PICO questions, in which the “PEO” (Population, Exposure, and Outcome) style was used for the explicit presentation of our review question and the explicit clarification of the inclusion and exclusion criteria. These searches were built using the Boolean operators “OR” and “AND” and the following keywords and phrases and/or Medical Subject Headings (MeSH).
PECO guide.
2.3. Population
All males and females of diabetes mellitus patients with sexual dysfunction.
2.4. Exposure
All sexual dysfunction persons with diabetic mellitus.
2.5. Comparison
Normal sexual functioning persons without any diabetes mellitus.
3. Outcome
Sexual dysfunction.
Intending to find as many pertinent primary studies as possible, we created the following review question using the aforementioned modified PICO format:
Review question: “What is the prevalence of sexual dysfunction among diabetes mellitus patients around the globe?"
International web databases (Pub Med, Science Direct, Scopus, EMBASE, and Google Scholar) were used to search for articles on the prevalence of sexual dysfunction in the world. The following search terms and keywords were used: “Prevalence”, “Sexually Dysfunction”, “Sexual Behavior”, “Sexual Orientation”, “Sexual Disorder”, “diabetes mellitus”, “Blood glucose”, “Hyperglycemia”, “Type1 diabetes mellitus”, “Type2 diabetes mellitus”, “Non-insulin dependent” and “Insulin-dependent”. The search terms were combined as well as utilized separately using Boolean operators like “OR” and “AND”. February 1 to March 10 of 2023 served as the search window.
3.1. Study outcome
Sexual dysfunction: It was measured by using 14 items of change in the sexual functioning questionnaire (CSFQ) with a total score of 70 and a cutoff point of 47 [32].
Sexual dissatisfaction: it is considered to be sexually dissatisfied when the score is less than 5 from CSFQ item 14 [32].
Sexual desire disorder: It was categorized as sexual desire disorder when the Score is less than 20 from the sum of CSFQ-14 [32].
Arousal dysfunction: It was classified under arousal disorder when a score is less than 14 from the sum of CSFQ-14- (items 7 through 9) [32].
Orgasm disorder: It was Explained by a score less than 14 from the sum of CSFQ-14- (items-11 through 13) [32].
3.2. Inclusion and exclusion criteria
This meta-analysis only included studies that were conducted worldwide between 2008 and 2022, published in English, and had full texts that could be searched. There were also reports on studies that contained information on the frequency of sexual dysfunction. We email the associated author at least twice for articles for which full texts are not readily available. This systematic review and meta-analysis excluded qualitative studies, research from redundant sources, and articles without the full text. This systematic review and meta-analysis did not include any qualitative studies, research from duplicate sources, or articles lacking the entire text. Using the COCOPOP (Condition, Context, and Population) paradigm, the study's included articles' eligibility was assessed. The study population (POP) consisted of individuals with sexual dysfunction, with the frequency of such disorders acting as the condition (CO) and studies conducted around the world serving as the context (CO).
3.3. Quality assessment
Two authors (NAG and KDT) evaluated the quality of the research independently using a standardized quality rating checklist created by the Joanna Briggs Institute (JBI) [33]. The conflict that emerged during the quality assessment was settled through a conversation guided by the third author (GAA). There are boxes marked yes, no, uncertain, and not relevant for eight parameters on the critical analysis checklist. The following questions are included in the criteria: (1). Where was it explicitly specified what was required to be included in the sample? (2). Did you provide a detailed description of the study participants and, consequently, the surroundings? (3). The exposure measurement's findings: were they reliable and valid? (4) Was the main goal and acceptable standards met by the event? (5) Have you discovered any confounding factors? (6). Was anything said about confounding factor measures? (7). Was it possible to measure the results effectively and precisely? (8). Was the statistical evaluation accurate? Studies that received 50% or more on the quality evaluation parameters were considered to be low risk (Supplementary file 2).
3.4. Risk of bias assessment
Two authors (NAG and GAA) independently assessed the risk of bias in the included studies using the Hoy et al. [34] established bias assessment method, which consists of 10 items that evaluate four bias domains as well as internal and external validity. A debate facilitated by the third author (KDT) was used to settle any disputes that arose during the risk of bias assessment. Finally, a resolution and agreement to the dispute were reached. The first four questions (items 1–4) evaluate the presence of external validity, non-response bias, and selection bias. Measurement bias, analysis-related bias, and internal validity are all evaluated in the final six questions (items 5–10). If studies responded “yes” to eight or more of the ten questions, they were classified as having a “low risk of bias”. Studies were categorized as “high risk” if they received “yes” responses to five or fewer of the ten questions, while studies labeled as “moderate risk” received “yes” responses to six to seven of the ten questions (Supplementary file 3).
3.5. Data extraction
For data extraction and analysis, STATA 14 software and a Microsoft Excel spreadsheet dated 2016 were utilized, respectively. Two authors (NAG and KDT) separately extracted each relevant piece of information using a standardized Joanna Briggs Institute data extraction procedure. The third author (GAA) organized a conversation to settle the dispute that arose during the data extraction. We retrieved the first author's name, the year of publication, the study region, the study setting, the study design, the sample size, the prevalence of sexual dysfunction, the type of diabetes mellitus, the sex of the study participants, and the standard deviation for each paper.
3.6. Data analysis
The data were extracted from all relevant findings in a Microsoft Excel spreadsheet and then imported into STATA software version 14 for analysis. A meta-analysis was performed to generate a pooled prevalence using a weighted inverse variance random-effects model. Using a forest plot to visually assess the presence of heterogeneity, the pooled prevalence of sexual dysfunction was analyzed and estimated. Based on the study's continent, design, type of diabetes, and participant sex, subgroup analyses were conducted. Sensitivity analysis was utilized to assess the effect of a single study on the overall prevalence estimate from the meta-analysis. The funnel plot and Begg and Egger's regression tests were used to thoroughly investigate any potential publication bias. To test for heterogeneity, quantify the degree of total/residual heterogeneity, and assess variability brought on by heterogeneity, Cochran's Q X2 test and I2 statistics were used, respectively [35].To investigate the impact of sample size and publication year differences on between-study heterogeneity, a Univariate meta-regression analysis was utilized [36].
4. Results
4.1. Search results and study characteristics
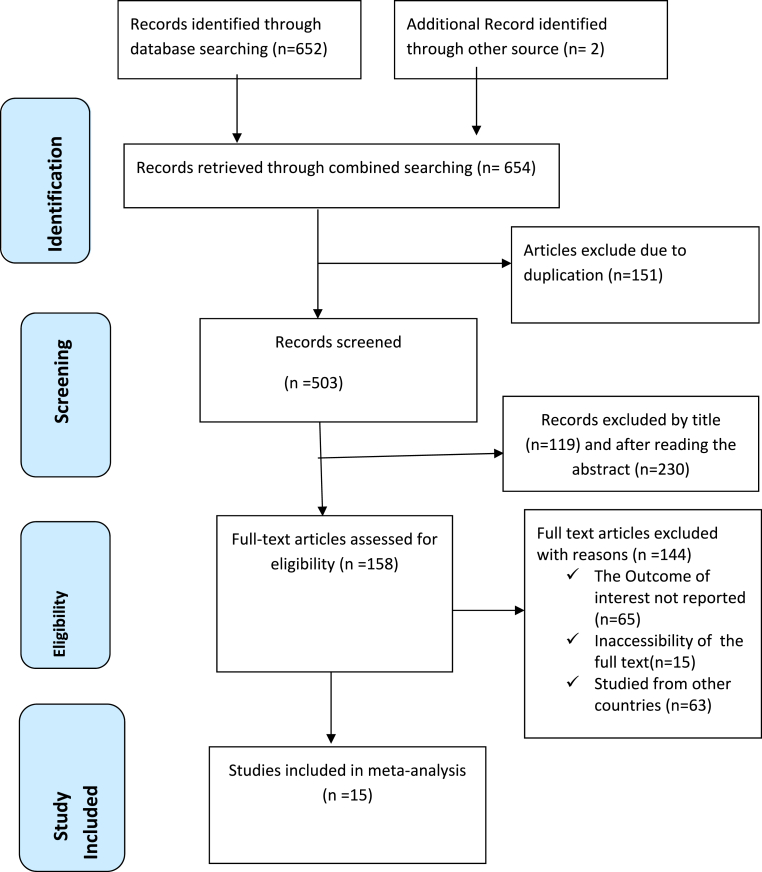
A total of 654 articles were obtained from several international web databases, including Google Scholar, PubMed, Scopus, EMBASE, and Science Direct. After excluding redundant studies, 503 studies remained, which were chosen for full title and abstract screening. The remaining 158 studies were assessed for full-text articles after 339 researchers had their titles and abstracts removed. After the full text was reviewed 143 items were deleted for further reasons. This systematic review and meta-analysis study included 15 publications [[37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51]] with 3724 study participants as part of its inclusion criteria (Fig. 1).
Fig. 1.
PRISMA flow chart displays the article selection process for the global prevalence of sexual dysfunction among diabetes patients.
Eleven of the included studies were cross-sectional, three were case-control studies, and the final study was a prospective cohort. The studies covered were all institutional-based research. Four studies were carried out in Iran [38,44,48,51], two in Italy [46,47], two in Nigeria [39,41], two in Ethiopia [37,42], and one in each of Turkey [40], Poland [43], Kenya [45], Ghana [49], America [50]. Sample sizes varied from 77 to 593. 32.3%–88% of people reported having a sexual dysfunction. Using the Joanna Briggs Institute (JBI) quality appraisal checklist, all studies were evaluated, and the results showed low risk (Table 1).
Table 1.
Characteristics of the included studies in the systematic review and meta-analysis for the global prevalence of sexual dysfunction among diabetic patients.
| Author/Year | Country | Setting | Design | Sample size | Prevalence | DM Type | Sex | Quality |
|---|---|---|---|---|---|---|---|---|
| Asefa et al., /2019 | Ethiopia | Institutional | Cross-sectional | 398 | 53.3% | Any DM | Both | Low-risk |
| Vafaeimanesh et al., /2014 | Iran | Institutional | Cross-sectional | 110 | 53.6% | Type2 | Female | Low-risk |
| Ogbera et al., /2009 | Nigeria | Institutional | Case-control | 94 | 88% | Type2 | Female | Low-risk |
| BC Unadike/2009 | Nigeria | Institutional | Cross-sectional | 225 | 58% | Any DM | Males | Low-risk |
| E.Tuncel/2016 | Turkish | Institutional | Cross-sectional | 93 | 55.9% | Type 2 | Female | Low-risk |
| Getie Mekonen et al. | Ethiopia | Institutional | Cross-sectional | 416 | 69.5% | Any DM | Male | Low-risk |
| Ewelina Bak et al., /2017 | Poland | Institutional | Case-control | 114 | 68% | Type 2 | Female | Low-risk |
| Forouzan Elyasi/2015 | Iran | Institutional | Cross-sectional | 150 | 78.7% | Type 2 | Female | Low-risk |
| Geoffrey M/2012 | Kenya | Institutional | Cross-sectional | 164 | 36.6% | Any DM | Female | Low-risk |
| Giuseppe Derosa/2023 | Italy | Institutional | Cross-sectional | 77 | 87% | Type 2 | Female | Low-risk |
| K Esposito/2010 | Italy | Institutional | Cross-sectional | 593 | 53.4% | Type 2 | Female | Low-risk |
| Ziaei-Rad et al., /2011 | Iran | Institutional | Case-control | 200 | 82.5% | Type 2 | Both | Low-risk |
| Owiredu et al., /2011 | Ghana | Institutional | Cross-sectional | 280 | 69.3% | Any DM | Males | Low-risk |
| Paul Enzlin/2009 | America | Institutional | Cohort | 424 | 35.4% | Type 1 | Female | Low-risk |
| Omidvar et al., /2013 | Iran | Institutional | Cross-sectional | 500 | 32.3% | Any DM | Female | Low-risk |
5. Meta-analysis
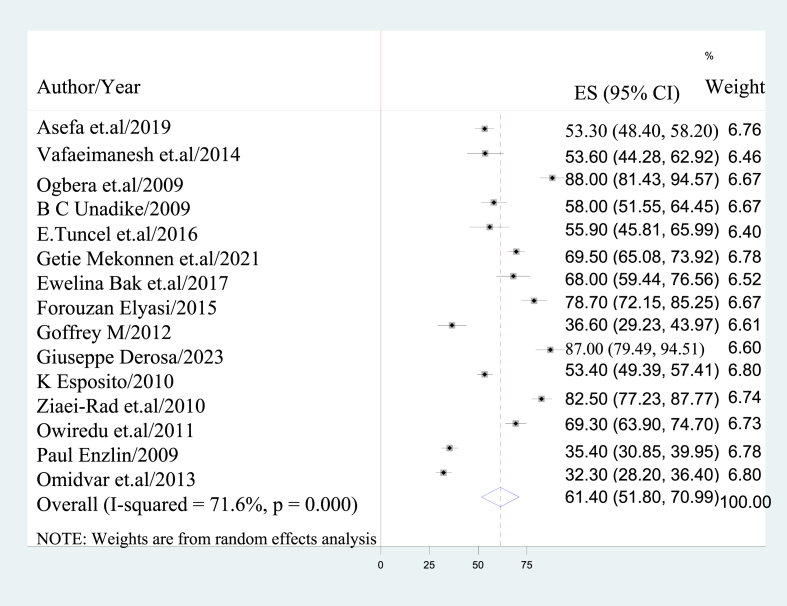
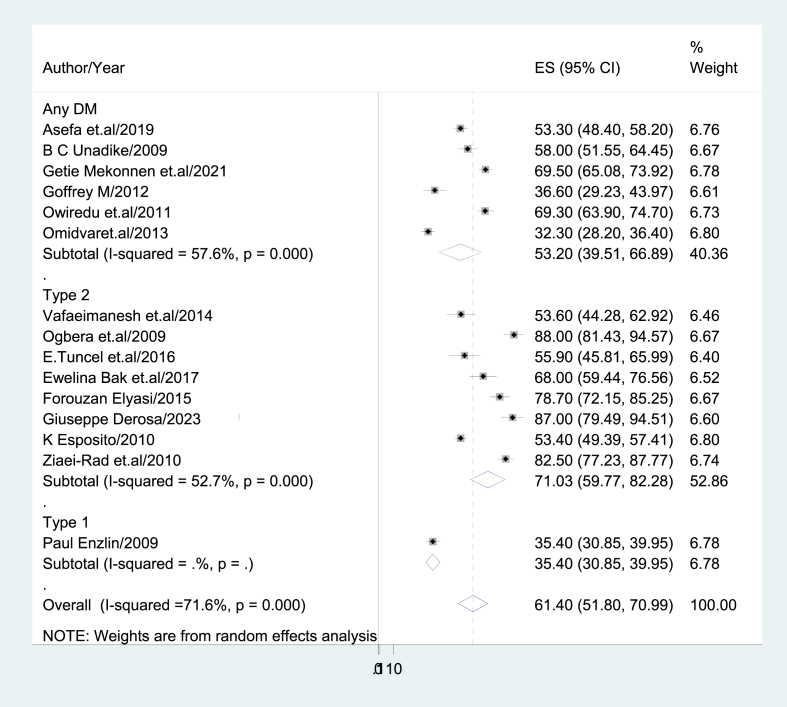
5.1. The global prevalence of sexual dysfunction
An overall estimate of sexual dysfunction among diabetic individuals was calculated using a random-effects model. Due to this, the prevalence of sexual dysfunction among diabetic patients was 61.4% globally (95% CI: 51.80, 70.99), I2 = 71.6% (Fig. 2). Sexual dysfunction in these individuals was seen in 75.3%, 59%, 54.6%, 58%, and 72.8% of them, respectively, in the domains of desire, arousal, orgasm, satisfaction, and erectile problems.
Fig. 2.
Forest plot displaying the pooled global prevalence of sexual dysfunction among diabetic patients.
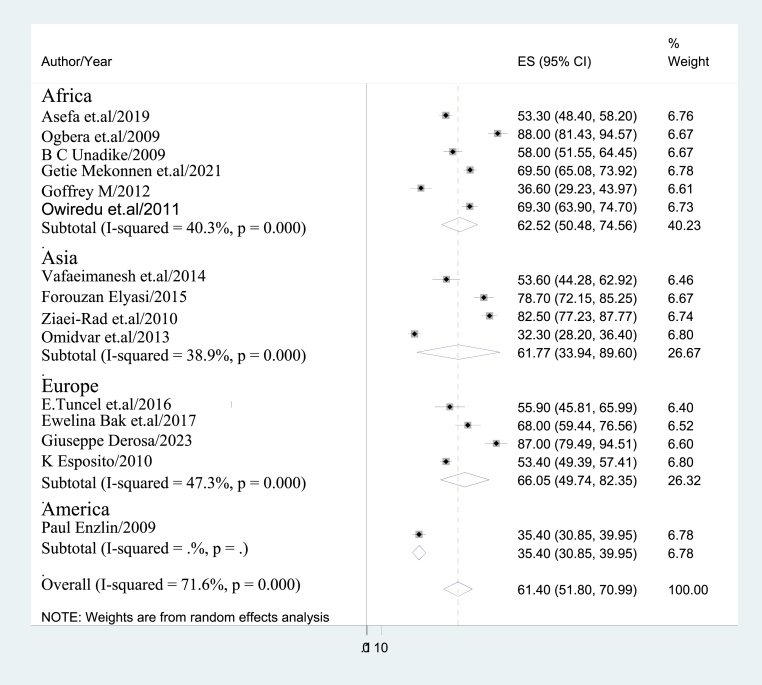
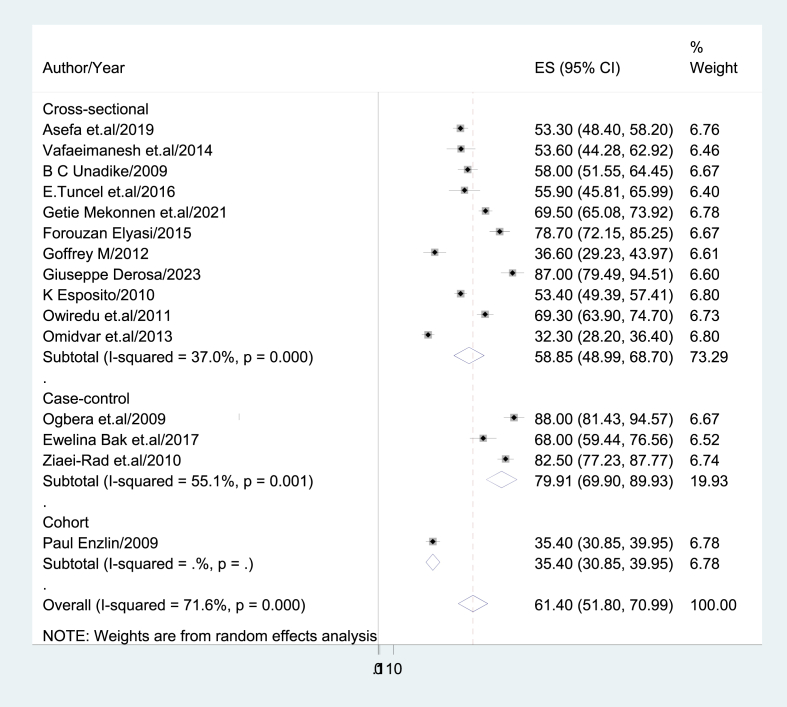
5.2. Subgroup analysis
Subgroup analyses were undertaken based on the continent, research design, type of diabetes mellitus, and sex of study participant due to the high heterogeneity that this meta-analysis revealed. Therefore, compared to America (35.40; 95% CI: 30.85, 39.95); I2 = 0%), the European region had a higher rate of sexual dysfunction (66.05%; 95% CI: 49.74, 82.35); I2 = 47.3% (Fig. 3). In terms of study design, case-control studies exhibited a greater prevalence of sexual dysfunction (79.91%; 95% CI: 69.90, 89.93); I2 = 55.1%; compared to cross-sectional studies (58.85%; 95% CI: 48.99, 68.70); I2 = 37%) (Fig. 4).
Fig. 3.
Sub-group analysis based region/continent where study done.
Fig. 4.
Sub-group analysis based study design.
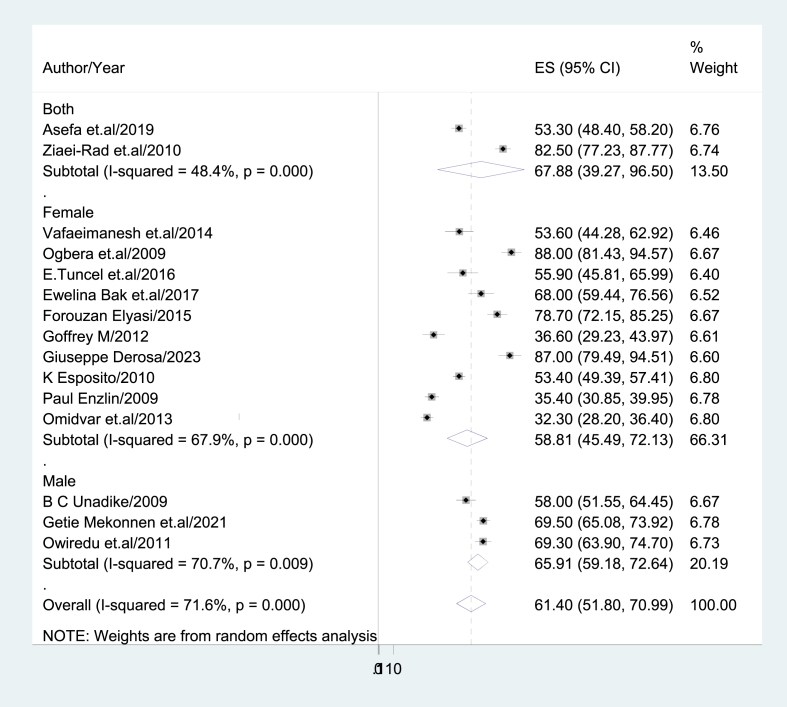
Males had a higher prevalence of sexual dysfunction than females (65.91%; 95% CI: 59.18, 72.64; I2 = 70.7% vs. 58.81%; 95% CI: 45.49, 72.134; I2 = 76.9%) (Fig. 5). The highest prevalence of sexual dysfunction, however, was found in people with type 2 diabetes mellitus (71.03%; 95% CI: 59.77, 82.28) (Fig. 6).
Fig. 5.
Sub-group analysis based gender.
Fig. 6.
Sub-group analysis based diabetic patients.
5.3. Heterogeneity and publication bias
We came up with a sub-group analysis based on region/continent, participant sex, type of diabetes, and study design to account for the study's reported heterogeneity (I2 = 78.3%). A univariate meta-regression using the sample size and year as covariates were also carried out to pinpoint the main causes of heterogeneity. It revealed that sample size affected the variation between studies (P = 0.021) (Table 2).
Table 2.
Meta-regression analysis of factors affecting between-study heterogeneity.
| Heterogeneity source | Coefficient's | Standard error | p-value |
|---|---|---|---|
| Sample size | 4.389242 | 1.669559 | 0.021 |
| Year | −34.55457 | 330.5618 | 0.918 |
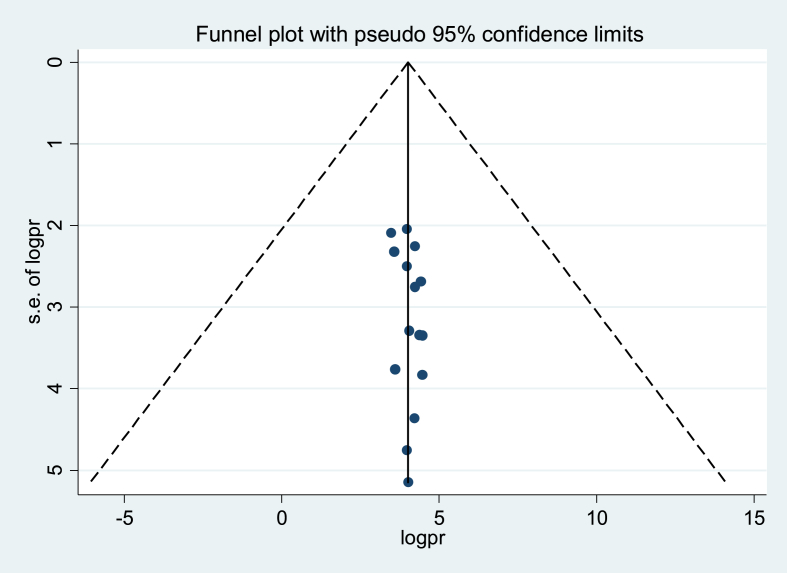
A funnel plot was used for the visual study of publication bias, and Egger's test and Begg's test were used for the statistical analysis. The funnel plot (Fig. 7) demonstrates a consistent distribution of research based on visual observation. The results of the Egger test (p = 0.20) and the Begg test (p = 0.373) did not reveal any proof of publication bias.
Fig. 7.
Forest plot symmetry displaying the absence of publication bias.
5.4. Leave –one-out-sensitivity analysis
The prevalence of sexual dysfunction among diabetic patients was examined using a leave-one-out sensitivity analysis, which tracked the effects of each study by removing one at a time. No evidence of a significant change in the general worldwide prevalence of sexual dysfunction among diabetic patients was found, according to the findings of the sensitivity analysis (Table 3).
Table 3.
The pooled prevalence of sexual dysfunction around the globe when one study omitted from the analysis a step at a time.
| Study omitted | Estimate | 95%Confidence interval |
|---|---|---|
| Asefa et al., /2019 | 61.99 | 51.58–72.39 |
| Vafaeimanesh et al., /2014 | 61.94 | 51.88–71.99 |
| Ogbera et al., /2009 | 59.49 | 50.01–68.98 |
| B C Unadike/2009 | 61.64 | 51.41–71.87 |
| E.Tuncel et al., /2016 | 61.77 | 51.73–71.82 |
| Getie Mekonnen et al., /2021 | 60.81 | 50.51–71.11 |
| Ewelina Bak et al., /2017 | 60.94 | 50.88–70.99 |
| Forouzan Elyasi/2015 | 60.16 | 50.28–70.04 |
| Geoffrey M/2012 | 63.15 | 53.29–73.02 |
| Giuseppe Derosa/2023 | 59.59 | 49.94–69.23 |
| K Esposito/2010 | 61.98 | 51.37–72.60 |
| Ziaei-Rad et.a/2010 | 59.87 | 50.29–69.45 |
| Owiredu et al., /2011 | 60.83 | 50.63–71.03 |
| Omidvar et al., /2013 | 63.52 | 54.58–72.46 |
| Paul Enzlin/2009 | 63.29 | 53.76–72.81 |
| Combined | 61.40 | 51.80–70.99 |
6. Discussion
Sexual dysfunction refers to the inability of a person to engage in the desired sexual interaction. Sexual function can be adversely affected by stress of any kind, emotional disorders, and a lack of knowledge about physiology and sexual function [52]. This disorder could be a sign of problems that have biological, intra-psychological, interpersonal, or a combination of these roots. 40 percent of couples endure sexual disorders or are at least somewhat unhappy with these irregularities, according to research findings [53]. One of the most ignored issues and a risk factor for many mental and physical diseases in diabetic patients is sexual dysfunction [50]. This study, which involved a systematic review and meta-analysis, looked at the global estimate of sexual dysfunction among diabetic individuals. The prevalence of sexual dysfunction among diabetic patients worldwide was therefore 61.4% (95% CI: 51.80–70.99), which is comparable to the findings of the Rahmanian et al. meta-analysis study (68.6%) [54].
The results of the current study were significantly greater compared to that of a meta-analysis study conducted by Y. Kouidrat et al. (52.5%) [55]. Variations in the socio-demographic characteristics of study participants, approaches taken to quantify study results, sample sizes, and times between studies could all be significant factors. Our study's participants were people in the general population, as opposed to Kouidrat et al.'s study, which included only male diabetic patients. Our study's results are therefore much lower than those of a study by Wondimenh Shibabaw Shiferaw et al. which found that erectile dysfunction was prevalent among male diabetic patients at a rate of 71.45% [56]. Variations in study intervals, sample sizes, and research participants as a whole could be to blame for this. Another explanation could be found in the study's contradictory findings. For instance, while the previous study revealed a prevalence of erectile dysfunction among diabetic males overall, our analysis showed a pooled incidence of sexual dysfunction among patients with any type of diabetes.
Subgroup analysis based on the continent, study design, participant sex, and type of diabetes mellitus was carried out. Because of this, the European region (66%) had more sexual dysfunction than the American region (35.4%). Males (65.9%) were more likely than females (58.8%) to experience sexual dysfunction. In our study, type 2 diabetes patients (71%) had a greater prevalence of sexual dysfunction than type 1 diabetic patients (35.4%).
A random-effects model was used in this investigation to address a sizable variance that existed in between-study heterogeneity. A leave-one-out sensitivity analysis revealed that no single study had a large effect on the prevalence of desire to use maternity waiting generally. Sub-group analysis was done based on region, sample size, and publication to find any heterogeneity. Variances in the sample populations, the nature of the paper, or variances in sociocultural, racial, and ethnic groupings may be the reason for the substantial heterogeneity. This study has some limitations. Initially, it is quite difficult to assess the findings of this study because there was no comparable prior research. Second, only articles written and published in English were permitted. Thirdly, the cross-sectional nature of each of the included studies suggests that additional confounding factors may affect the outcome variable. This research has some value as well. The first ones employed were compressive electronic web search engines. Second, we included the grey literature with the primary research in our review. Also noted was the incidence of sexual dysfunction in the region.
7. Conclusion
In conclusion, sexual dysfunction was very prevalent throughout the world. Based on the region, type of diabetes, study design, and sex of the study participants, the total prevalence of sexual dysfunction varied. As a result, individuals in the type 2 diabetes mellitus study who were male and from the European region had greater rates of sexual dysfunction. Sexual dysfunction should be identified and treated in diabetes follow-up clinics as part of routine medical care. Healthcare practitioners should be on the lookout for any indications of sexual dysfunction in patients who are dealing with a chronic illness, especially those with diabetes.
Ethics approval and consent to participants
Not applicable because no primary data were collected.
Consent for publication
Not applicable.
Availability of data and materials
All relevant data are within the Manuscript and its Supporting Information files.
Funding
The authors received no specific funding for this work.
Authors' contributions
NAG conceptualized the study: NAG, KDT, and GAA contributed during data extraction and analysis: YSK and GAK wrote the result interpretation: NAG, MAM, and KDT Prepared the first draft: ECA, MMG, and DTA contributed during the conceptualization and interpretation of results and substantial revision: NAG, WAB, AMD, TDA, NM, BB, SSF, YSK, GAK, MAM, MAZ, AMD, ECA, MMG, DTA, KDT and GAA. Revised and finalized the final draft manuscript. All the authors read and approved the final version of the manuscript.
Authors’ information
NAG: School of Midwifery, College of Medicine and Health Sciences, Wolaita Sodo University, Sodo, Ethiopia.
YSK: Department of Medical Laboratory Science, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia.
KDT: Department of Comprehensive Nursing, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia.
GAA: School of Public Health, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia.
GAK: Department of Epidemiology and Biostatistics, School of Public Health, Wolaita Sodo University, Wolaita Sodo, Ethiopia.
MAM: Department of Biochemistry, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia.
MAZ: Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
NA: Department of Pediatrics and Child Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
BB: Department of Comprehensive Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
SFF: Department of Public Health, College of Health Sciences, Woldia University, Woldia, Ethiopia.
TAD: Department of Biochemistry, College of Health Science, Gondar University, Gondar, Ethiopia.
ECA: Department of Comprehensive Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
MMG: Department of Comprehensive Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
DTA: Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
MAM: Department of Biochemistry, College of Health Science, Gondar University, Gondar, Ethiopia.
AMD: Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
WAB: Department of Maternal and Neonatal Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
Declaration of competing interest
The authors declared that they have no competing interests.
Acknowledgment
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.metop.2023.100247.
Supplementary material
-
1.
S1_File.Prisma checklist.
-
2.
S2_File. Methodological quality assessment of included studies using Joanna Brigg's Institute quality appraisal criteria scale (JBI). The eight-item questions assessing inclusion criteria, study setting and participant, exposure measurement, objectives, confounder, statically analysis, outcome measurement, and dealing confounder were used.
-
3.
S3_File. Risk of bias assessment for the included studies. The ten-item questions of which four items assess external and six items assess internal validity were used.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Zamanzadeh V., Zirak M., Hemmati Maslakpak M., Parizad N. Distance education and diabetes empowerment: a single-blind randomized control trial. Diabetes Metabol Syndr. 2017;11(Suppl 1):S247–S251. doi: 10.1016/j.dsx.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation (IDF). Diabetes facts and figures [http://www.idf.org/Facts_and_Figures].
- 3.International Diabetes Federation Middle EST and North Africa Iran vs world prevalence of diabetes. http://www.idf.org/membe ship/mena/Iran
- 4.Maiorino M.I., Bellastella G., Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes, Metab Syndrome Obes Targets Ther. 2014;7:95–105. doi: 10.2147/DMSO.S36455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute of Diabetes and Digestive and Kidney Diseases Sexual and urologic problems of diabetes. 2012. http://diabetes.niddk.nih.gov/dm/pubs/sup/ Available from.
- 6.Várkonyi T., Kempler P. Sexual dysfunction in diabetes. Handb Clin Neurol. 2014;126:223–232. doi: 10.1016/B978-0-444-53480-4.00017-5. http://www.ncbi.nlm.nih.gov/pubmed/25410225%5Cnhttp://linkinghub.elsevier.com/retrieve/pii/B9780444534804000175 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 7.Manicardi V., Anguis M.F., Calabrese M., Ceriello A., Cristofaro M.R., Giorda C.B., Impronta M.R., Li Volsi P., Maffettone A., Mulas M.F., Napoli A., Nicolucci A., Rossi M.C., Russo G., Suraci C., Torlone E. Focus su: differenze di genere nel Diabete tipo 1. Associazione Medici Diabetologi (AMD); 2014. Le Monografie degli annali edizone. 2014. [Google Scholar]
- 8.Enzlin P., Mathieu C., Van Den Bruel A., Vanderschueren D., Demyttenaere K. Prevalence and predictors of sexual dysfunction in patients with type 1 diabetes. Diabetes Care. 2003;26:409–414. doi: 10.2337/diacare.26.2.409. [DOI] [PubMed] [Google Scholar]
- 9.McCabe M.P., Sharlip I.D., Lewis R., Atalla E., Balon R., Fisher A.D., et al. Risk factors for sexual dysfunction among women and men: a consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med. 2016;13(2):153–167. doi: 10.1016/j.jsxm.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Varga CAJAJoRH The forgotten fifty percent: a review of Sexual and reproductive health research and programs focused on Boys and young men in sub-Saharan Africa. Afr J Reprod Health. 2001;175–95 PMID: 12471940. [PubMed] [Google Scholar]
- 11.Adams M.J., Collins V.R., Dunne M.P., de Kretser D.M., Holden C.A. Male reproductive health disorders among Aboriginal and Torres Strait Islander men: a hidden problem? Med J Aust. 2013;198(1):33–38. doi: 10.5694/mja12.10490. [DOI] [PubMed] [Google Scholar]
- 12.Hidalgo-Tamola J., Chitaley K. Review type 2 diabetes mellitus and erectile dysfunction. J Sex Med. 2009;6:916–926. doi: 10.1111/j.1743-6109.2008.01116.x. [DOI] [PubMed] [Google Scholar]
- 13.Laumann E., Nicolosi A., Glasser D., et al. Sexual problems among women and men aged 40–80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot. 2005;17:39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- 14.Lewis R.W., Fugl-Meyer K.S., Corona G., Hayes R.D., Laumann E.O., Moreira E.D., Jr., et al. Definitions/epidemiology/risk factors for sexual dysfunction. J Sex Med. 2010;7(4pt2):1598–1607. doi: 10.1111/j.1743-6109.2010.01778.x. [DOI] [PubMed] [Google Scholar]
- 15.Colson M.-H. Sexual dysfunction and chronic illness. Part 1. Epidemiology, impact, and significance. Sexologies. March 2016;25(1):5–11. [Google Scholar]
- 16.Rösing D., Klebingat K.-J., Berberich H.J., Bosinski H.A., Loewit K., Beier K.M. Male sexual dysfunction: diagnosis and treatment from a sexological and interdisciplinary perspective. Dtsch Arztebl Int. 2009;106(50):821. doi: 10.3238/arztebl.2009.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lui P.S.C. Queensland University of Technology; 2016. Reproductive health problems faced by men in the Solomon Islands.https://eprints.qut.edu.au/101163 [Google Scholar]
- 18.Jackson G. Sexual dysfunction and diabetes. Int J Clin Pract. 2004;58(4):358–362. doi: 10.1111/j.1368-5031.2004.00180.x. [DOI] [PubMed] [Google Scholar]
- 19.Kolodny R.C., Kahn C.B., Goldstein H.H., Barnett D.M.J.D. vol. 23. 2000. pp. 306–309. (Sexual dysfunction in diabetic men). 4. [DOI] [PubMed] [Google Scholar]
- 20.Nowosielski K., Drosdzol A., Sipiński A., Kowalczyk R., Skrzypulec V. Diabetes mellitus and sexuality—Does it really matter? J Sex Med. 2010 Feb;7(2_Part_1):723–735. doi: 10.1111/j.1743-6109.2009.01561.x. [DOI] [PubMed] [Google Scholar]
- 21.Bultirini A., across E., Colpi E.M., Poccia G., Iannarelli R., Lembo D., Lenzi A., Jannini E.A. Possible correlation between type 1 diabetes mellitus and female sexual dysfunction: case report and literature review. J Sex Med. 2004;1:337–340. doi: 10.1111/j.1743-6109.04048.x. [DOI] [PubMed] [Google Scholar]
- 22.Erol B., Tefekli A., Sanli O., Ziylan O., Armagan A., Kendirci M., Eryasar D., Kadioglu A. Does sexual dysfunction correlate with deterioration of somatic sensory system in diabetic women? Int J Impot Res. 2003;15:198–202. doi: 10.1038/sj.ijir.3900998. [DOI] [PubMed] [Google Scholar]
- 23.Caruso S., Rugolo S., Mirabella D., Intelisano G., Di Mari L., Cianci A. Changes in clitoral blood flow in premenopausal women affected by type 1 diabetes after single 100-mg administration of sildenafil. Urology. 2006;68:161–165. doi: 10.1016/j.urology.2006.01.059. [DOI] [PubMed] [Google Scholar]
- 24.Psarou A., Cooper H., Wilding J.P.H. Patients' perspectives of oral and injectable type 2 diabetes medicines, their body weight and medicine-taking behavior in the UK: a systematic review and meta-ethnography. Diabetes Ther. 2018;9(5):1791–1810. doi: 10.1007/s13300-018-0490-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rieusset J. Role of endoplasmic reticulum-mitochondria communication in type 2 diabetes. Adv Exp Med Biol. 2017;997:171–186. doi: 10.1007/978-981-10-4567-7_13. [DOI] [PubMed] [Google Scholar]
- 26.Owiredu W.K., Amidu N., Alidu H., Sarpong C., Gyasi-Sarpong C.K. Determinants of sexual dysfunction among clinically diagnosed diabetic patients. Reprod Biol Endocrinol. 2011;9:70. doi: 10.1186/1477-7827-9-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vigersky R., Shrivastav M. Role of continuous glucose monitoring for type 2 in diabetes management and research. J Diabet Complicat. 2017;31(1):280–287. doi: 10.1016/j.jdiacomp.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization (WHO) Sexual and reproductive health. Defining sexual health 2006. .www.who.int/repro ducti vehea lth/topic s/sexua l_healt h/sh_defin ition s/en
- 29.American Psychiatric Association . fifth ed. American Psychiatric Association; Arlington: 2013. Diagnostic and statistical manual of mental health disorders. [Google Scholar]
- 30.Ali R.M.A., Hajeri R.M.A., Khader Y.S., Shegem N.S., Ajlouni K.M. Sexual dysfunction in Jordanian diabetic women. Diabetes Care. 2008;31(8):1580–1581. doi: 10.2337/dc08-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 32.C A.H. Reliability and construct validity of the changes in sexual functioning questionnaire short-form (CSFQ-14) Sex Marital Ther. 2006;32:43–52. doi: 10.1080/00926230500232909. [DOI] [PubMed] [Google Scholar]
- 33.Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetcu R., et al. Joanna Briggs Institute Reviewer's Manual; 2017. Checklist for analytical cross-sectional studies. Available from: JBI critical appraisal checklist for analytical cross-sectional Studies 2017. [Google Scholar]
- 34.Hoy D., et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of inter-rater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 35.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 36.Viechtbauer W. Conducting meta-analyses in R with the metaphor package. J Stat Software. 2010;36 [Google Scholar]
- 37.Asefa Adane, Nigussie Tadesse, Henok Andualem, Mamo Yitagesu. Prevalence of sexual dysfunction and related factors among diabetes mellitus patients in Southwest Ethiopia. BMC Endocr Disord. 2019;19:141. doi: 10.1186/s12902-019-0473-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vafaeimanesh Jamshid, Raei Mehdi, Hosseinzadeh Fatemeh, Parham Mahmoud. Evaluation of sexual dysfunction in women with type 2 diabetes. Indian Journal of Endocrinology and Metabolism. 2014;18(2) doi: 10.4103/2230-8210.129107. Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Unadike B.C., Eregie A., Ohwovoriole A.E. Prevalence and types of sexual dysfunction among males with diabetes in Nigeria: 18 Mera. Diabetes Int. November 2008:18–20. [Google Scholar]
- 40.Tuncel Ercan, Durgun Onur, Peynirci Hande, Ersoy Canan. Sexual dysfunction in female patients with type 2 diabetes mellitus: a cross-sectional single-center study among Turkish patients. Hum Fertil. 2016 doi: 10.1080/14647273.2016.1266039. [DOI] [PubMed] [Google Scholar]
- 41.Ogbera, et al. Frequency and correlates of sexual dysfunction in women with diabetes mellitusjsm_. J Sex Med. 2009;6:3401–3406. doi: 10.1111/j.1743-6109.2009.01396.x1396.3401.3406. [DOI] [PubMed] [Google Scholar]
- 42.Getie Mekonnen E., Yeshita H.Y., Bishaw Geremew A. Sexual dysfunction among men with diabetes mellitus attending chronic out-patient department at the three hospitals of Northwest Amhara region, Ethiopia: prevalence and associated factors. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0256015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ewelina Ba˛k 1. Marcisz Czeslaw, Sylwia Krzemin´ ska. Dobrzyn-Matusiak Dorota, Foltyn Agnieszka, Drosdzol-Cop Agnieszka. Relationships of sexual dysfunction with depression and acceptance of illness in women and men with type 2 diabetes mellitus. Int J Environ Res Publ Health. 2017;14:1073. doi: 10.3390/ijerph14091073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elyasi Forouzan, Kashi Zahra, Tasfieh Bentolhoda, Bahar Adele, Khademloo Mohammad. Sexual dysfunction in women with type 2 diabetes mellitus. Int J Math Stat. May 2015;40(No 3) [PMC free article] [PubMed] [Google Scholar]
- 45.Ungaya Likata Geoffrey M., Kuria Mary W., Olando Yvonne, Owiti Fred R. Sexual dysfunction among patients with diabetes mellitus. Greener Journal of Medical Sciences. December 2012;2(6):138–145. ISSN: 2276-7797. [Google Scholar]
- 46.Derosa Giuseppe, Romano Davide, D'Angelo Angela, Maffioli Pamela. Female sexual dysfunction in subjects with type 2 diabetes mellitus. Sex Disabil. 2023 doi: 10.1007/s11195-023-09781-3. [DOI] [Google Scholar]
- 47.Esposito K., et al. Determinants of female sexual dysfunction in type 2 diabetes. Int J Impot Res. 2010;22:179–184. doi: 10.1038/ijir.2010.6. [DOI] [PubMed] [Google Scholar]
- 48.Ziaei-Rad Marzieh, Vahdaninia Mariam, Ali Montazeri. Sexual dysfunctions in patients with diabetes: a study from Iran. Reprod Biol Endocrinol. 2010;8:50. doi: 10.1186/1477-7827-8-50. http://www.rbej.com/content/8/1/50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Owiredu, et al. Determinants of sexual dysfunction among clinically diagnosed diabetic patients. Reprod Biol Endocrinol. 2011;9:70. doi: 10.1186/1477-7827-9-70. http://www.rbej.com/content/9/1/70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paul Enzlin, et al. vol. 32. MAY 2009. (Sexual dysfunction in women with type 1 diabetes: diabetes care). NUMBER 5. [Google Scholar]
- 51.Omidvar, et al. Sexual dysfunction among women with diabetes mellitus in a diabetic center in Amol. J Nat Sci Biol Med. July 2013;4(Issue 2) doi: 10.4103/0976-9668.116992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ponholzer A., Froehlich M., Racz U., Temml C., Madersbacher S. Female sexual dysfunction in a healthy Austrian cohort: prevalence and risk factors. Eur Urol. 2005;47(3):366–374. doi: 10.1016/j.eururo.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 53.Hartmann U., Philippsohn S., Heiser K., Ruffer-Hesse C. Low sexual desire in midlife and older women: personality factors, psychosocial development, present sexuality. Menopause. 2004;11(6 Pt 2):726–740. doi: 10.1097/01.gme.0000143705.42486.33. [DOI] [PubMed] [Google Scholar]
- 54.Rahmanian, et al. Evaluation of sexual dysfunction and female sexual dysfunction indicators in women with type 2 diabetes: a systematic review and meta-analysis. Diabetol Metab Syndrome. 2019;11:73. doi: 10.1186/s13098-019-0469-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kouidrat Y., et al. Systematic Review or Meta-analysis High prevalence of erectile dysfunction in diabetes: a systematic review and meta-analysis of 145 studies: diabet. Méd. 2017;34:1185–1192. doi: 10.1111/dme.13403. [DOI] [PubMed] [Google Scholar]
- 56.Shiferaw Wondimeneh Shibabaw, et al. Prevalence of erectile dysfunction in patients with diabetes mellitus and its association with body mass index and glycated hemoglobin in africa: a systematic review and meta-analysis. Int. J. Endocrinol. 2020:10. doi: 10.1155/2020/5148370. Article ID 5148370. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are within the Manuscript and its Supporting Information files.