Abstract
Background
One‐third of people with gastrointestinal disorders, including functional dyspepsia, use some form of complementary and alternative medicine, including herbal medicines.
Objectives
The primary objective is to assess the effects of non‐Chinese herbal medicines for the treatment of people with functional dyspepsia.
Search methods
We searched the following electronic databases on 22 December 2022: Cochrane Central Register of Controlled Trials, MEDLINE, Embase, Allied and Complementary Medicine Database, Latin American and Caribbean Health Sciences Literature, among other sources, without placing language restrictions.
Selection criteria
We included RCTs comparing non‐Chinese herbal medicines versus placebo or other treatments in people with functional dyspepsia.
Data collection and analysis
Two review authors independently screened references, extracted data and assessed the risk of bias from trial reports. We used a random‐effects model to calculate risk ratios (RRs) and mean differences (MDs). We created effect direction plots when meta‐analysis was not possible, following the reporting guideline for Synthesis without Meta‐analysis (SWiM). We used GRADE to assess the certainty of the evidence (CoE) for all outcomes.
Main results
We included 41 trials with 4477 participants that assessed 27 herbal medicines. This review evaluated global symptoms of functional dyspepsia, adverse events and quality of life; however, some studies did not report these outcomes.
STW5 (Iberogast) may moderately improve global symptoms of dyspepsia compared with placebo at 28 to 56 days; however, the evidence is very uncertain (MD ‐2.64, 95% CI ‐4.39 to ‐0.90; I2 = 87%; 5 studies, 814 participants; very low CoE). STW5 may also increase the improvement rate compared to placebo at four to eight weeks' follow‐up (RR 1.55, 95% CI 0.98 to 2.47; 2 studies, 324 participants; low CoE). There was little to no difference in adverse events for STW5 compared to placebo (RR 0.92, 95% CI 0.52 to 1.64; I2 = 0%; 4 studies, 786 participants; low CoE). STW5 may cause little to no difference in quality of life compared to placebo (no numerical data available, low CoE).
Peppermint and caraway oil probably result in a large improvement in global symptoms of dyspepsia compared to placebo at four weeks (SMD ‐0.87, 95% CI ‐1.15 to ‐0.58; I2 = 0%; 2 studies, 210 participants; moderate CoE) and increase the improvement rate of global symptoms of dyspepsia (RR 1.53, 95% CI 1.30 to 1.81; I2 = 0%; 3 studies, 305 participants; moderate CoE). There may be little to no difference in the rate of adverse events between this intervention and placebo (RR 1.56, 95% CI 0.69 to 3.53; I2 = 47%; 3 studies, 305 participants; low CoE). The intervention probably improves the quality of life (measured on the Nepean Dyspepsia Index) (MD ‐131.40, 95% CI ‐193.76 to ‐69.04; 1 study, 99 participants; moderate CoE).
Curcuma longa probably results in a moderate improvement global symptoms of dyspepsia compared to placebo at four weeks (MD ‐3.33, 95% CI ‐5.84 to ‐0.81; I2 = 50%; 2 studies, 110 participants; moderate CoE) and may increase the improvement rate (RR 1.50, 95% CI 1.06 to 2.11; 1 study, 76 participants; low CoE). There is probably little to no difference in the rate of adverse events between this intervention and placebo (RR 1.26, 95% CI 0.51 to 3.08; 1 study, 89 participants; moderate CoE). The intervention probably improves the quality of life, measured on the EQ‐5D (MD 0.05, 95% CI 0.01 to 0.09; 1 study, 89 participants; moderate CoE).
We found evidence that the following herbal medicines may improve symptoms of dyspepsia compared to placebo: Lafonesia pacari (RR 1.52, 95% CI 1.08 to 2.14; 1 study, 97 participants; moderate CoE), Nigella sativa (SMD ‐1.59, 95% CI ‐2.13 to ‐1.05; 1 study, 70 participants; high CoE), artichoke (SMD ‐0.34, 95% CI ‐0.59 to ‐0.09; 1 study, 244 participants; low CoE), Boensenbergia rotunda (SMD ‐2.22, 95% CI ‐2.62 to ‐1.83; 1 study, 160 participants; low CoE), Pistacia lenticus (SMD ‐0.33, 95% CI ‐0.66 to ‐0.01; 1 study, 148 participants; low CoE), Enteroplant (SMD ‐1.09, 95% CI ‐1.40 to ‐0.77; 1 study, 198 participants; low CoE), Ferula asafoetida (SMD ‐1.51, 95% CI ‐2.20 to ‐0.83; 1 study, 43 participants; low CoE), ginger and artichoke (RR 1.64, 95% CI 1.27 to 2.13; 1 study, 126 participants; low CoE), Glycyrrhiza glaba (SMD ‐1.86, 95% CI ‐2.54 to ‐1.19; 1 study, 50 participants; moderate CoE), OLNP‐06 (RR 3.80, 95% CI 1.70 to 8.51; 1 study, 48 participants; low CoE), red pepper (SMD ‐1.07, 95% CI ‐1.89 to ‐0.26; 1 study, 27 participants; low CoE), Cuadrania tricuspidata (SMD ‐1.19, 95% CI ‐1.66 to ‐0.72; 1 study, 83 participants; low CoE), jollab (SMD ‐1.22, 95% CI ‐1.59 to ‐0.85; 1 study, 133 participants; low CoE), Pimpinella anisum (SMD ‐2.30, 95% CI ‐2.79 to ‐1.80; 1 study, 107 participants; low CoE). The following may provide little to no difference compared to placebo: Mentha pulegium (SMD ‐0.38, 95% CI ‐0.78 to 0.02; 1 study, 100 participants; moderate CoE) and cinnamon oil (SMD 0.38, 95% CI ‐0.17 to 0.94; 1 study, 51 participants; low CoE); moreover, Mentha longifolia may increase dyspeptic symptoms (SMD 0.46, 95% CI 0.04 to 0.88; 1 study, 88 participants; low CoE).
Almost all the studies reported little to no difference in the rate of adverse events compared to placebo except for red pepper, which may result in a higher risk of adverse events compared to placebo (RR 4.31, 95% CI 1.56 to 11.89; 1 study, 27 participants; low CoE). With respect to the quality of life, most studies did not report this outcome.
When compared to other interventions, essential oils may improve global symptoms of dyspepsia compared to omeprazole. Peppermint oil/caraway oil, STW5, Nigella sativa and Curcuma longa may provide little to no benefit compared to other treatments.
Authors' conclusions
Based on moderate to very low‐certainty evidence, we identified some herbal medicines that may be effective in improving symptoms of dyspepsia. Moreover, these interventions may not be associated with important adverse events. More high‐quality trials are needed on herbal medicines, especially including participants with common gastrointestinal comorbidities.
Keywords: Humans, Complementary Therapies, Dyspepsia, Dyspepsia/drug therapy, Plant Extracts, Quality of Life
Plain language summary
What are the effects of non‐Chinese herbal medicines for people with functional dyspepsia?
Key results
We identified multiple herbal medicines that were effective in improving symptoms and well‐being in people with functional dyspepsia. Also, they may not be associated with important unwanted events compared to sham treatment. However, we found little evidence on the comparative effectiveness of herbal medicines and other treatments.
The effect of herbal medicines may need to be compared to common medical treatments for functional dyspepsia to assess their relative effectiveness. More high‐quality trials are needed for functional dyspepsia, especially with people with common gastrointestinal comorbidities.
Background
What is functional dyspepsia?
Functional dyspepsia is a frequent problem among adults. It is characterized by pain and discomfort in the stomach. However, unlike organic dyspepsia, these symptoms can not be blamed on ulcers or other lesions in the stomach or intestines.
How is functional dyspepsia treated?
The treatments for this include drug and non‐drug approaches, but it is not known how well they work. A variety of herbal products have been tested, to an extent, as possible treatments for this condition.
What did we want to find out?
In this review, we looked at all available studies on this subject to find out if any of these herbs can improve symptoms and well‐being, and if they are safe.
Study characteristics
What did we do?
We searched for studies investigating non‐Chinese herbal medicines compared with usual treatment or other treatments in people with functional dyspepsia. We compared and summarized their results about symptoms, well‐being, and unwanted effects, and rated our confidence in the evidence according to study methods and the numbers of people in the studies.
Summary of results
What did we find?
We found 41 studies of 4477 people with functional dyspepsia that assessed 27 herbal products. Most of them compared herbal products against placebo (dummy tablets), although some studies compared them against drugs like omeprazole, H pylori treatment, or other treatments. The duration of the studies varied from 15 days to 12 weeks. The studies were conducted in many countries around the world; 12 of them took place in Iran. The pharmaceutical industry provided funds for 14 studies, government institutions funded eight, a medical association funded one study and the rest did not state how they were funded.
Main results
STW5 (known commercially as Iberogast because one of the herbs it contains is Iberis amara L.) may reduce global symptoms of dyspepsia compared with placebo in one or two months. SWT5 may not be more effective than placebo in improving the well‐being, but only one small study measured this. In terms of safety, unwanted effects may be similar when compared to placebo.
Peppermint and caraway oil probably result in a moderate to a large reduction in global symptoms of dyspepsia and improved well‐being compared to a simulated treatment at one month. However, there may be little to no difference in the rate of unwanted effects between this intervention and the placebo.
Curcuma longa probably reduces global symptoms of dyspepsia and improves well‐being compared to placebo at four weeks. There is probably little to no difference in the rate of unwanted effects between this intervention and placebo.
We found evidence that the following herbal medicines may improve symptoms of dyspepsia compared to placebo: Lafonesia pacari, Nigella sativa, artichoke, Boensenbergia rotunda, Pistacia lenticus, Enteroplant, Ferula asafoetida, ginger and artichoke, Glycyrrhiza glabra, OLNP‐ 06, red pepper, Cuadrania tricuspidata, jollab, and Pimpinella anisum. Mentha pulegium and cinnamon oil may provide little to no difference compared to placebo; moreover, Mentha longifolia may increase dyspeptic symptoms. Almost all the studies reported little to no difference in the rate of unwanted effects compared to placebo, except for red pepper, which may result in a higher risk of unwanted effects compared to placebo. Most studies did not report on participants' well‐being.
When compared to other drugs, we only found that a combination of essential oils seems to provide superior relief of symptoms compared to omeprazole.
Certainty of the evidence
What are the limitations of the evidence?
We have little confidence in the evidence, as we found few trials for each herbal medicine, few participants for each comparison, and few head‐to‐head comparisons. In addition, most studies had limitations in their design. Besides, many studies did not clearly state how they diagnosed functional dyspepsia.
How up to date is this evidence?
The evidence is current to 22 December 2022.
Summary of findings
Summary of findings 1. STW5 (Iberogast) compared to placebo for functional dyspepsia.
| STW5 compared to placebo for functional dyspepsia | ||||||
| Patient or population: participants with functional dyspepsia Setting: outpatient clinics Intervention: STW5 (Iberogast) Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with STW5 | |||||
|
Global symptoms of dyspepsia Assessed with: GIS Range 0 to 40 Follow‐up: 28 to 56 days |
The mean global symptoms of dyspepsia (continuous) was 5 points. | MD 2.64 lower (4.39 lower to 0.90 lower) | ‐ | 814 (5 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b,c | Higher scores mean worse symptoms. |
|
Global symptoms of dyspepsia (responders) Assessed with: > 20% improvement GIS scores Follow‐up: 4 to 8 weeks |
Study population | RR 1.55 (0.98 to 2.47) |
324 (2 RCT) | ⊕⊕⊝⊝ LOWd,e | Higher number of responders indicates a beneficial effect. | |
| 418 per 1000 | 648 per 1000 (410 to 1000) | |||||
|
Adverse events Assessed clinically Follow‐up: 28 to 56 days |
Study population | RR 0.92 (0.52 to 1.64) | 786 (4 RCTs) | ⊕⊕⊝⊝ LOWb,e | ||
| 57 per 1000 | 53 per 1000 (30 to 93) | |||||
|
Quality of life Assessed with: NDI Follow‐up: 4 weeks |
Not available | ‐ | 52 (1 RCT) |
⊕⊕⊝⊝ LOWd,f | The study stated that "differences between treatment groups did not yield significance." | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; GIS: Gastrointestinal Symptom Score; NDI: Nepean Dyspepsia Index; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to inconsistency; high statistical heterogeneity (I2 = 88%). bDowngraded one level due to risk of bias; most studies were at an overall unclear risk of bias. cDowngraded one level due to imprecision; 95% CI includes benefit and little to no effect. dDowngraded one level due to risk of bias; the included studies were presented as an abstract so there is little to no information to adequately assess the risk of bias. eDowngraded one level due to imprecision; 95% CI includes substantial benefits and little to no effect. fDowngraded one level due to imprecision; the study was reported as an abstract with no statistical data to assess precision; however, the sample size was small.
Summary of findings 2. Peppermint/caraway oil compared to placebo for functional dyspepsia.
| Peppermint/caraway oil compared to placebo for functional dyspepsia | ||||||
| Patient or population: participants with functional dyspepsia Setting: outpatient clinics Intervention: peppermint/caraway oil Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with Peppermint/caraway oil | |||||
|
Global symptoms of dyspepsia Assessed with: SMD Follow‐up: 4 weeks |
The mean global symptoms of dyspepsia (continuous) was 2.96 points. | SMD 0.87 lower (1.15 lower to 0.58 lower) | ‐ | 210 (2 RCTs) | ⊕⊕⊕⊝ MODERATEa | Indicates a moderate to large benefit. |
|
Global symptoms of dyspepsia (responders) Assessed with: clinical improvement Follow‐up: 4 weeks |
Study population | RR 1.53 (1.30 to 1.81) | 305 (3 RCTs) | ⊕⊕⊕⊝ MODERATEa | Higher number of responders indicates a beneficial effect. | |
| 537 per 1000 | 821 per 1000 (698 to 972) | |||||
|
Adverse events Assessed clinically Follow‐up: 4 weeks |
Study population | RR 1.56 (0.69 to 3.53) | 305 (3 RCTs) | ⊕⊕⊝⊝ LOW a,b | ||
| 141 per 1000 | 220 per 1000 (97 to 498) | |||||
|
Quality of life Assessed with: NDI Follow‐up: 4 weeks |
The mean quality of life was 218.3 points. | MD 131.4 lower (193.76 lower to 69.04 lower) | ‐ | 99 (1 RCT) | ⊕⊕⊕⊝ MODERATEa | Lower scores indicate better quality of life. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; NDI: Nepean Dyspepsia Index; RR: risk ratio; SMD: standardized mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to risk of bias; most studies were at an overall unclear risk of bias. bDowngraded one level due to imprecision; 95% CI included substantial benefits and harms.
Summary of findings 3. Curcuma longa compared to placebo.
| Curcuma longa compared to placebo for functional dyspepsia | ||||||
| Patient or population: participants with functional dyspepsia Setting: outpatient clinics Intervention:Curcuma longa Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with Curcuma longa | |||||
|
Global symptoms of dyspepsia Assessed with: Severity of Dyspepsia Assessment Follow‐up: 4 weeks |
The mean decrease in global symptoms of dyspepsia (continuous) was 10.94 points. | MD 3.33 lower (5.84 lower to 0.81 lower) | ‐ | 110 (2 RCTs) | ⊕⊕⊕⊝ MODERATEa | Lower scores indicates fewer symptoms. |
|
Global symptoms of dyspepsia (responders) Assessed with: clinical improvement Follow‐up: 1 week |
Study population | RR 1.5 (1.06 to 2.11) | 76 (1 RCT) | ⊕⊕⊝⊝ LOW a,b | ||
| 526 per 1000 | 789 per 1000 (558 to 1000) | |||||
|
Adverse events Assessed clinically Follow‐up: 4 weeks |
Study population | RR 1.26 (0.51 to 3.08) |
89 (1 RCT) | ⊕⊕⊕⊝ MODERATEa | ||
| 200 per 1000 | 252 per 1000 (102 to 616) | |||||
|
Quality of life Assessed with: EuroQoL EQ‐5D (range 0 to 1) Follow‐up: 4 weeks |
The mean quality of life was 0.92 points. | MD 0.05 higher (0.01 higher to 0.09 higher) | ‐ | 89 (1 RCT) | ⊕⊕⊕⊝ MODERATEa | Higher scores indicate better quality of life. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; MD: mean difference; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level due to imprecision; 95% CI included substantial benefits and little or no benefit/harms. bDowngraded one level due to risk of bias; most studies were at an overall unclear risk of bias.
Summary of findings 4. Other herbal medicines compared to placebo.
| Herbal preparation | Study | n |
Global symptoms (continuous) |
Global symptoms (dichotomous) |
Adverse Events |
Quality of life |
| Studies at low risk of bias | ||||||
| Lafoensia pacari | Da Mota Menezes 2006 | 97 | NR | ▲ | ⯇⯈ | NR |
| Mentha pulegium | Khonche 2017 | 100 | ⯇⯈ | NR | ⯇⯈ | ▲ |
| Nigella sativa | Mohtashami 2015 | 70 | ▲ | ⯇⯈ | ⯇⯈ | NR |
| Alizadeh‐Naini 2020 | 51 | NR | NR | |||
| Studies at unclear risk of bias | ||||||
| Artichoke | Holtmann 2003 | 244 | ▲ | NR | ⯇⯈ | ▲ |
| Astaxanthin | Kupcinskas 2008 | 131 | NR | NR | ⯇⯈ | NR |
| Boesenbergia rotunda (fingerroot) | Chitapanarux 2020 | 160 | ▲ | NR | ▲ | NR |
| Pistacia lentiscus (Chios mastic gum/oil) | Dabos 2010 | 148 | ▲ | NR | ⯇⯈ | NR |
| Sattarzadeh 2021 | 63 | NR | ||||
| Enteroplant | Sun 2016 | 198 | ▲ | NR | ⯇⯈ | ⯇⯈ |
| Ferula asafoetida | Mala 2018 | 43 | ▲ | NR | ⯇⯈ | ▲ |
| Ginger (Zingiber officinalis) and artichoke (Cynara cardunculus) | Giacosa 2015 | 126 | NR | ▲ | ⯇⯈ | NR |
| Glycyrrhiza glabra (Gutcard) | Allan 2012 | 50 | ▲ | NR | ⯇⯈ | ▲ |
| Mentha longifolia | Babaeian 2017 | 88 | ▼ | NR | ⯇⯈ | NR |
| OLNP‐06 | Panda 2020 | 48 | NR | ▲ | ⯇⯈ | NR |
| Pistacia atlantica | Eftekharafzali 2018 | 119 | NR | NR | ⯇⯈ | NR |
| Red pepper | Bortolotti 2002 | 27 | ▲ | NR | ▼ | NR |
| Studies at high risk of bias | ||||||
| Apium graveolens and Trachyspermum copticom | Azimi 2017 | 92 | NR | NR | ⯇⯈ | ▲ |
| Cinnamon oil | Zobeiri 2021 | 51 | ⯇⯈ | NR | ⯇⯈ | NR |
| Cuadrania tricuspidata | Shin 2021 | 83 | ▲ | NR | ⯇⯈ | ▲ |
| Jollab | Pasalar 2015 | 133 | ▲ | NR | ⯇⯈ | NR |
| Pimpinella anisum | Ghoshegir 2015 | 107 | ▲ | NR | ⯇⯈ | NR |
NR: not reported; Upward arrow ▲ = positive health impact, downward arrow ▼ = negative health impact, sideways arrow ⯇⯈ = no change.
Summary of findings 5. Herbal medicines compared to other treatments.
| Herbal preparation | Comparison | Study | n | Global symptoms(continous) |
Global symptoms (dichotomous) |
Adverse Events |
Quality of life |
| Studies at low risk of bias | |||||||
| Curcuma longa | Omeprazole | Yongwatana 2022 | 88 | ⯇⯈ | NR | ⯇⯈ | ⯇⯈ |
| Puttapitakpong 2016 | 22 | ⯇⯈ | NR | NR | |||
| Studies at unclear risk of bias | |||||||
| Curcuma longa | Flatulence | Thamlikitkul 1989 | 68 | NR | ⯇⯈ | NR | NR |
| Peppermint oil/caraway oil | Cisapride | Madisch 1999 | 118 | ⯇⯈ | NR | ⯇⯈ | NR |
| STW5 (Iberogast) | Cisapride | Rosch 2002 | 137 | ⯇⯈ | NR | ⯇⯈ | NR |
| STW5 (Iberogast) | Proton pump inhibitor | Holtmann 2013 | 57 | NR | ⯇⯈ | NR | NR |
| Trachyspermum ammi L., Anethum graveolens L., and Zataria multiflora Boiss herbal oils vs omeprazole | Omeprazole | Bordbar 2020 | 57 | ▲ | NR | ⯇⯈ | ▲ |
| Studies at a high risk of bias | |||||||
| Apium graveolens and Trachyspermum copticom | Omeprazole | Azimi 2017 | 100 | NR | NR | ⯇⯈ | ⯇⯈ |
| Nigella sativa at different doses: 1, 2 and 3 g | Clarithromycin, amoxicillin, and omeprazole | Salem 2010 | 88 | NR | ⯇⯈ | ⯇⯈ | NR |
| Pudin hara pearls | Pudin hara liquid | Sastry 2016 | 79 | ⯇⯈ | NR | ⯇⯈ | NR |
NR: not reported; Upward arrow ▲ = positive health impact, downward arrow ▼ = negative health impact, sideways arrow ⯇⯈ = no change.
Background
Description of the condition
The term 'dyspepsia' is commonly used to refer to epigastric abdominal pain. The definition of functional dyspepsia (FD), also called non‐ulcerous dyspepsia (Talley 2015), has undergone major changes since the initial working party definition in 1988 to the consecutive Rome I to IV diagnostic criteria (see Appendix 1 for a detailed description of the first three Rome criteria) (Pinto 2017; Stanghellini 2016). Rome IV criteria for FD include one or more of the following cardinal dyspepsia symptoms: bothersome postprandial fullness, early satiation, epigastric pain and burning that are unexplained after a routine clinical evaluation and with no evidence of structural disease detectable by diagnostic images, including the use of upper endoscopy (Stanghellini 2016). The criteria must be fulfilled for the last three months with symptom onset at least six months before diagnosis (Brun 2010). In order to optimize diagnostic and therapeutic approaches, Rome IV criteria divided FD into two groups, namely postprandial distress syndrome and epigastric pain syndrome, under the supposition of a differential and complex pathophysiology (Carbone 2017; Stanghellini 2016). Even considering that these categories frequently overlap, the classification would be useful in determining the initial treatment (Stanghellini 2014).
Epidemiological studies report a worldwide prevalence of FD ranging from 8% to 30% (Mahadeva 2006). The reported prevalence of dyspepsia varies considerably in different populations due to different interpretations and expressions of symptoms, diagnostic criteria adopted by environmental factors, and local prevalence of underlying organic diseases, such as peptic ulcer and gastric cancer (Aziz 2018; Mahadeva 2006; Stanghellini 2016).
Functional dyspepsia constitutes a highly prevalent condition, with direct and indirect significant economic costs (Talley 2017). Functional dyspepsia‐associated emotional distress, abdominal discomfort when ingesting food and drink, and even impaired vitality can reduce the quality of life of those with the condition (Brun 2010; Montoro 2004). Functional dyspepsia overlaps with other common gastrointestinal disorders: one‐third of people with FD also suffer from irritable bowel syndrome (Ford 2010), and more than one‐third experience gastroesophageal reflux (Choung 2012)
The current treatment of FD comprises both non‐pharmacological and pharmacological approaches. Non‐pharmacological treatment is based on changes in portion size and fat content of meals. Additionally, it is recommended that the consumption of coffee, alcohol, cigarettes and non‐steroidal anti‐inflammatory drugs (NSAIDs) be avoided, although the scientific evidence supporting this recommendation is scarce (Lacy 2012).
Pharmacological therapy for FD includes the following.
Acid suppression therapy with proton pump inhibitors (PPIs) or H2 receptor antagonists (H2RAs). While PPIs are considered first‐line therapy for FD, the majority of patients will not show an adequate response with this approach, even with high drug dosages (Moayyedi 2004). A recent systematic review demonstrated that PPIs are well‐tolerated and effective drugs for FD compared with placebo and slightly more effective than H2RAs and prokinetics (Pinto 2017). However, this evidence is controversial since other, more heterogeneous, meta‐analysis data show that H2 blockade might be more efficacious than PPIs (Talley 2017).
Prokinetic agents. Different meta‐analyses have shown that prokinetic therapy is superior to placebo overall. Nonetheless, these results are mainly driven by cisapride, which was withdrawn from the US market due to an increased risk of adverse cardiac events, including sudden death due to a prolonged QT interval (Brun 2010; Talley 2015). Itopride has shown improvements in symptom control, such as postprandial fullness and early satiety, with a low rate of adverse events; a meta‐analysis of nine trials supported its therapeutic use (Huang 2012). Similarly, domperidone versus placebo showed a beneficial effect on the global rate of dyspeptic symptoms (Brun 2010; Pittayanon 2018); however, evidence for its efficacy is scarce, and it may prolong the QT interval (Talley 2017). In contrast, a meta‐analysis of mosapride showed that it was not superior to placebo for improvement of symptoms (Bang 2015).
Tricyclic antidepressants and antipsychotics have shown to be superior to placebo overall (Ford 2020).
Mucosal‐protecting agents and antispasmodics. Trimebutine maleate, bismuth, and sucralfate have shown inconsistent results in the treatment of FD (Brun 2010; Talley 2015)
Other pharmacological agents, such as buspirone and sumatriptan, are sometimes used as second‐line therapies (Stanghellini 2016). These have a modest effect in terms of eradication of symptoms (Brun 2010; Talley 2015). Montelukast, a leukotriene receptor antagonist, and eosinophil stabilizer were shown to be superior to placebo in a randomized controlled trial in a paediatric FD population (Talley 2017).
Other interventions that have been evaluated for this condition include acupuncture (Lan 2014), which was found to be ineffective, and eradication of Helicobacter pylori infection (Moayyedi 2006), which had a small effect on the reduction of symptoms.
Description of the intervention
Over 30% of the Western population with gastrointestinal disorders use some form of complementary and alternative medicine (CAM) to treat their symptoms (Langmead 2001; Tillisch 2006). Within the field of CAM, herbal medicine is becoming increasingly popular, in particular for treating benign, chronic conditions that might be self‐managed, such as FD. A product is considered to be a herbal medicine when it contains active ingredients obtained only from plants, or parts of plants, in a crude or processed state (Langmead 2001; Thompson 2002). Such products are available in a variety of pharmaceutical preparations (i.e. powders, teas, tablets, capsules, suppositories, extracts, lotions, and fresh or dried plants) (NIH 2016). A non‐comprehensive list of herbal products used for dyspepsia is shown in Table 6. Explanations for their frequent use are related to their availability and common assumptions regarding their safety due to their 'natural' origin, in comparison to conventional medicine. Furthermore, they can be obtained without any medical prescription (i.e. rather than what can be a several‐month wait for a physician appointment to receive prescription medicine, herbal medicines are readily available in most supermarkets or shops in many countries) (Krueger 2004). Also, herbal therapy may be considered comparatively inexpensive in comparison with traditional pharmacological therapies.
1. Herbal medicinal products for treatment of dyspepsia.
| Common name (species) |
| Angelica (Angelica archangelica) |
| Anise (Pimpinella anisum) |
| Artichoke (Cynara scolymus) |
| Bitter orange peel (Citrus aurantium) |
| Blessed thistle (Cnicus benedictus) |
| Bogbean (Menyanthes trifoliate) |
| Boldo (Peumus boldus) |
| Caraway (Carum carvi) |
| Cardamom (Elettaria cardamomum) |
| Centuary (Centaurium minu) |
| Chicory (Cichorium intybus) |
| Cinchona (Cinchona pubescens) |
| Cinnamon (Cinnamomum verum) |
| Cloves (Syzygium aromaticum) |
| Coriander (Coriandrm sativum) |
| Dandelion (Taraxacum officinale) |
| Devil's claw (Harpagophytum procumbens) |
| Dill (Anethum graveolens) |
| Elecampane (Inula helenium) |
| Fenugreek (Trigonella foenum‐graecum) |
| Galangal (Alpinia officinarium) |
| Gentian (Gentiana lutea) |
| Ginger (Zingiber officinale) |
| Horsetail (Equisetum arvense) |
| Haronga (Harungona madagascariensis) |
| Horehound (Marrubium vulgare) |
| Juniper (Juniper communis) |
| Lemon balm (Melissa officinalis) |
| Meadowsweet (Filipendula ulmaria) |
| Milk thistle (Silybum marianum) |
| Mistletoe (Viscum album) |
| Oregon grape (Mahonia aquifolium) |
| Peach (Prumus persica) |
| Peppermint (Mentha piperita) |
| Radish (Raphanus sativus) |
| Rosemary (Rosemarinus officinalis) |
| Sage (Salvia officinalis) |
| Sandy everlasting (Helichrysum arenarium) |
| St John's wort (Hypericum perforatum) |
| Star anise (Ilisium verum) |
| Thyme (Thymus vulgaris) |
| Turmeric (Curcuma longa) |
| Wormwood (Artemisia absinthium) |
| Yarrow (Achillea millefolium) |
Table adapted from Thompson 2002.
Adverse effects can occur with the use of herbal products due to direct toxic effects from biologically active constituents, by contamination, and by interactions between herbal and traditional medications (Bent 2008). The majority of adverse events reported for herbal medicines are self limited and of minor importance, and include nausea, vomiting, and abdominal pain. However, serious adverse events have been reported, including acute and chronic hepatitis, fulminant hepatic failure, hepatic tumours, renal failure, and allergic reactions (Langmead 2001; Shaw 2012).
Herbal products are also used within the Traditional Chinese Medicine (TCM) approach. However, TCM uses a combination of formulations and complementary treatments that are not designed to treat the symptoms of a specific disease; instead, they are made specifically for the individual in accordance with the complex diagnostic and therapeutic principles of TCM described as "syndrome complex" (Teschke 2015). Chinese herbal medicine is widely used in Asian countries, both within TCM and separately as pharmaceutical products. Since there is a Cochrane group currently devoted to the study of Chinese herbal medicines in FD, we will exclusively analyze herbal medicine not considered in a TCM approach.
How the intervention might work
In vitro studies have suggested that the components of a variety of plants could have antibacterial, antioxidant, anticytokine, smooth muscle relaxation and antispasmodic effects, among others. However, the extrapolation of these findings from in vitro studies to humans is not entirely clear (Langmead 2001).
Herbal medications may also have psychological effects. People who use CAM therapies often report that they are helped to gain a feeling of control over their disease and treatment, perhaps thereby reducing their emotional distress and discomfort. A placebo effect may also contribute to the effectiveness of CAM therapies (Shaw 2012).
Approximately 4000 million people use herbal medicine as their primary source of health care (Ekor 2014). This is particularly important in low‐ to middle‐income countries since herbal medicine is a source of over‐the‐counter, inexpensive, and self‐managed medicines used for everyday ailments (Ekor 2014). This poses challenges when evaluating their effectiveness when compared with other biomedical products that usually require several stages of testing before commercialization, among other issues (Tilburt 2008).
Why it is important to do this review
Functional dyspepsia accounts for a significant number of primary care consultations and hospital referrals (Hungin 2009). At present, there are some reviews on this subject (Bent 2008, Langmead 2001; Melzer 2004; Thompson 2002); however, their methodological quality is low, and they do not incorporate GRADE for the assessment of the body of evidence.
Additionally, some clinical trials have been published on the subject (Meier 2013; Park 2010; Shim 2015), and a high‐quality systematic review evaluating the efficacy and safety of herbal medicines for the treatment of FD is vital to provide reliable data to inform decision‐making by patients, physicians, and CAM providers.
This protocol was designed in accordance with a series of Cochrane Review protocols related to this topic, in particular, the protocol for the Cochrane Review 'Proton pump inhibitors for functional dyspepsia' (Pinto 2017). We asked the study authors for their authorization when using similar criteria across the protocol.
Objectives
The primary objective is to assess the effects of non‐Chinese herbal medicines for the treatment of people with functional dyspepsia.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (parallel assignment, cluster‐randomized, and cross‐over). We included the first phase of cross‐over randomized controlled trials, since there may be a substantial risk of carry‐over effect. We included studies reported as full text, those published as abstract only, and unpublished data. We did not place any restrictions on our search based on the language of publication.
Types of participants
We included studies involving people suffering from FD according to the Rome I, II, III, or IV criteria (see Appendix 1), of both sexes, and aged 18 years old and older. We included studies with participants fulfilling said criteria even if there was no explicit reference to Rome criteria. In addition, we included studies involving people with FD and comorbidities such as irritable bowel syndrome and gastroesophageal reflux disease. If a study included populations with different conditions, we only considered people with FD if outcome data were disaggregated for this condition.
Types of interventions
We included studies assessing the effects of any form of herbal medicine, including oral preparations, decoctions, injections, powders, teas, tablets, capsules, suppositories, extracts, lotions, and fresh or dried plants.
We did not include studies addressing the effects of herbal medicines in the context of TCM and its variations (Kampo, Traditional Korean Medicine).
We included the following comparisons.
Herbal medicines versus placebo or usual care
Herbal medicines as a single agent or combined with other agents versus other agents: acid suppression agents (PPIs, H2RAs) or prokinetics
Types of outcome measures
We did not use the measurement of the outcomes listed in this section as eligibility criteria.
We have selected patient‐reported outcomes focusing on the impact of dyspepsia on symptoms, quality of life, and adverse events (Chassany 2012), employing the same approach as other Cochrane Reviews on the topic (Pinto 2017; Pittayanon 2018). We presented these outcomes in the summary of findings tables (see Data synthesis).
We planned to group the outcome measurements into three categories; short‐term (up to six months), medium‐term (between six and 12 months), and long‐term follow‐up (one year or more). Where outcomes were reported at multiple time points, we chose the latest available measurement for each category.
Primary outcomes
Global symptoms of dyspepsia, measured by a validated score or scale, such as the gastrointestinal symptom score (GIS), the severity of dyspepsia assessment scale (SODA), the dyspepsia symptom severity index (DSSI), or other validated instruments. This outcome could be measured both as a continuous outcome and the number of individuals with improved symptoms scores.
Adverse events: number of participants with at least one adverse event.
Secondary outcomes
Quality of life, measured by validated scales such as the Nepean Dyspepsia Index and the Glasgow Dyspepsia Severity Score (GDSS), 36‐Item Short‐Form Health Survey (SF‐36), EuroQol‐5D (EQ‐5D) questionnaire, or other validated scales.
Search methods for identification of studies
Electronic searches
We conducted a comprehensive literature search to identify all published and unpublished randomized controlled trials, as described in the Cochrane Handbook of Systematic Reviews of Interventions Chapter 4 (Lefebvre 2021). We did not impose any language, publication year, or publication status restrictions. We translated non‐English language papers and fully assessed them for potential inclusion in the review.
We searched the following electronic databases to identify potential studies on 22 December 2022:
Cochrane Central Register of Controlled Trials (CENTRAL) (via Ovid Evidence‐Based Medicine Reviews Database (EBMR)) (from inception to Issue 11, 2022; Appendix 2);
MEDLINE (via Ovid) (1946 to 22 December 2022) (Appendix 3);
Embase (via Ovid) (1974 to 22 December 2022) (Appendix 4);
AMED (Allied and Complementary Medicine Database) (via Ovid) (from 1985 to 22 December 2022; Appendix 5);
LILACS (Latin American and Caribbean Health Science Information database) (via BIREME) (from inception to 22 December 2022; Appendix 6)
We also searched the following clinical trial registers from inception to 22 December 2022:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov);
Current Controlled Trials meta Register of Controlled Trials (mRCT) (www.isrctn.com);
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (www.who.int/trialsearch).
Searching other resources
We attempted to identify other potentially eligible trials by checking the reference lists of retrieved trials, review articles, and meta‐analyses for additional references. We contacted authors of identified trials and experts in the field to identify any relevant ongoing or unpublished studies. We searched for errata or retractions from eligible trials on www.ncbi.nlm.nih.gov/pubmed.
We searched the following sources of grey literature:
Health Management Information Consortium (HMIC) database (www.ovid.com/site/catalog/DataBase/99.jsp);
National Technical Information Service (NTIS) database (dblease.ntis.gov/);
OpenGrey (www.opengrey.eu).
Data collection and analysis
Selection of studies
Two review authors (CP or MA) independently screened the titles and abstracts of all retrieved records for potential eligibility. After retrieval of full‐text study reports or publications of potentially relevant studies, two review authors (CP or MA) independently assessed the full texts and classified them as included studies, excluded studies, studies awaiting classification, or ongoing studies in accordance with the criteria for each provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022). Any disagreements were resolved through discussion or by consultation with a third review author (JVAF). We included studies irrespective of whether outcomes data were reported in a 'usable' way. We documented reasons for the exclusion of ineligible studies that may have reasonably been expected to have been included in the review in a 'Characteristics of excluded studies' table. We collated multiple reports of the same study so that each study, rather than each report, is the unit of interest in the review. We documented the selection process in sufficient detail to complete a PRISMA flow chart (Page 2021).
Data extraction and management
Two review authors (CV and GB) independently extracted the study characteristics from the included studies using a standard data collection form that was previously tested on at least one eligible study. Any disagreements were resolved through discussion or by consultation with a third review author (JVAF).
We collected characteristics of the included studies in sufficient detail to populate a ‘Characteristics of included studies’ table, such as the following.
Study design
Number of study centres and location
Study setting
Date of study
Participant eligibility criteria
Number of participants by trial and by study arm
Withdrawals
Participant demographic details at baseline, such as age, gender, ethnicity, and severity of the condition
Details about experimental intervention and comparison, such as herbal medicinal product name, characteristics of the herbal product, dosage regimen and quantitative description, and route of administration
Details about co‐interventions
Details about the primary and secondary outcomes assessed: definition, method and timing of outcome measurement, and relevant subgroups
Sources of study funding
Conflicts of interest reported by trial authors
Two review authors (GB and CV) independently extracted outcome data from the included studies. In the 'Characteristics of included studies' table, we noted if outcome data were reported in an unusable way. Any disagreements were resolved by consensus or by involving a third review author (JVAF). One review author (GB or CV) copied the data from the data collection form into the Review Manager software (RevMan Web 2021). Two authors (JVAF and MA or CP) double‐checked that the data were entered correctly by comparing the study reports with the presentation of the data in the systematic review.
We extracted the most detailed numerical data that might facilitate similar analyses of included studies. For dichotomous outcomes, we collected the number of events and totals to populate a 2 x 2 table, or effect estimates (e.g. odds ratios, risk ratios) with corresponding variance measures if more detailed data were not available. We collected means and standard deviations for continuous outcomes or the data needed to calculate this information if they were not available.
We attempted to contact study authors if any relevant information was missing at the end of the data extraction process, including information needed to assess the risk of bias.
Assessment of risk of bias in included studies
Two review authors (GB or CV) independently assessed the risk of bias for each study using the Cochrane risk of bias assessment tool RoB 1 (Higgins 2011). Any disagreements were resolved by consensus or by consultation with a third review author (JVAF).
We assessed the following domains.
Sequence generation (selection bias)
Allocation concealment (selection bias)
Blinding of participants and personnel (performance bias)
Blinding of outcome assessment (detection bias)
Incomplete outcome data (attrition bias)
Selective outcome reporting (reporting bias)
Other sources of bias
We judged each potential source of bias as 'high,' 'low,' or 'unclear' as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For each study, we presented a risk of bias table with the support for our judgment for each risk of bias domain. We noted in the risk of bias table if the information used to judge the risk of bias was provided by correspondence with study authors or was unpublished data. We considered blinding of participants and outcome assessors for all outcomes similarly since they were all patient‐reported outcomes. We considered a study to have a low risk of bias if all domains were assessed as at low risk of bias; high risk of bias if at least one domain was assessed as at high risk of bias; or unclear risk of bias if at least one domain was assessed as unclear risk without any domain at high risk of bias.
We summarized the risk of bias judgements across different studies for each of the domains listed. We presented a risk of bias summary figure to illustrate these findings.
Assessment of bias in conducting the systematic review
We conducted the review according to the published protocol and reported any deviations from it in the Differences between protocol and review section of the review.
Measures of treatment effect
For meta‐analysis of continuous outcome data, we presented results as mean differences (MD) with their associated 95% confidence intervals (CI) when the eligible trials used the same instrument to measure a given construct. We prioritized postintervention over change from baseline measurements as defined in Section 6.5.1 of the Handbook (Higgins 2022). If studies used different scales to measure the same outcome, we presented the results as standardized mean differences (SMDs) with 95% CI. We interpreted the SMD using guidance from the Handbook, with a threshold of 0.2 for a small effect, 0.5 for a moderate effect and 0.8 for a large effect (Schünemann 2021). We displayed these results in the summary of findings tables as mean differences for those comparisons with meta‐analysis. For Synthesis Without Meta‐Analysis (SWiM), we used SMDs to better estimate effect size across interventions. We also extracted the number of participants with improved symptoms as a dichotomous outcome. We presented results as risk ratios (RR) with their associated 95% CI for dichotomous outcome data.
Unit of analysis issues
The unit of analysis was the individual participant.
Where a single trial reported multiple trial arms, we included only the relevant arms. If two comparisons (e.g. drug A versus placebo and drug B versus placebo) had been entered into the same meta‐analysis, we would have halved the control group to avoid double‐counting.
We would have attempted to re‐analyse cluster‐RCTs that had not appropriately adjusted for the potential clustering of participants within clusters in their analyses. The variance of intervention effects would have been inflated by a design effect. Calculation of a design effect involves the estimation of an intracluster correlation coefficient (ICC), as specified in Chapter 23 of the Handbook (Higgins 2022).
Dealing with missing data
We attempted to contact primary study authors or sponsors to request missing numerical outcome data or any other relevant information for assessing the risk of bias. We included intention‐to‐treat analyses whenever possible; otherwise, we included available‐case analyses.
If we suspected that missing dichotomous outcome data were not missing at random, we performed sensitivity analyses by imputing outcomes to recreate the most extreme possible data sets, one reflecting the best‐case scenario for the experimental treatment and the other the worst‐case scenario, as described in Higgins 2008.
Assessment of heterogeneity
We assessed the presence of clinical heterogeneity across studies by examining the characteristics of the study population, interventions, comparisons, and outcome measurements from the extracted data (see Data extraction and management).
We identified inconsistency across studies through visual inspection of the forest plots to assess the amount of overlap of CIs, and used the I2 statistic to measure heterogeneity among the trials in each analysis (Higgins 2003). We interpreted the I2 statistic as follows:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: represents considerable heterogeneity.
If we identified substantial heterogeneity, we explored it by prespecified subgroup analysis and sensitivity analyses.
Assessment of reporting biases
We attempted to obtain study protocols to assess the presence of selective outcome reporting.
If we had been able to pool at least 10 trials for the same outcome, we would have used funnel plots to investigate small‐study effects. As asymmetry in funnel plots may have several explanations besides publication bias, we would have interpreted the results carefully.
Data synthesis
We undertook meta‐analysis only if we considered that the participants, interventions, comparisons, and outcome assessments were similar enough to ensure that an answer would be clinically meaningful. Otherwise, we presented a qualitative synthesis (see below) to describe the results across the included studies.
In the event that a quantitative synthesis was plausible due to clinical homogeneity, we performed statistical analyses according to guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022). We pooled data using a random‐effects model.
We categorized global symptoms of dyspepsia as overall symptom improvement. Since we sourced the data from the responder analysis of each individual study, we annotated the threshold or criteria for responders in each analysis as this was highly variable (e.g. improvement of 10%, 25%, or 50% in symptoms score, or categories 'markedly improved' or 'mildly improved'). We calculated the relative risk reduction (RR) and 95% CIs. For dichotomous outcomes, we used the Mantel‐Haenszel method.
We recorded the global symptom score at pre‐ and post‐treatment as well as the mean and standard deviation of change scores from baseline in each group if this information was available. We would have calculated the mean and standard deviation of change scores from baseline if only pre‐ and post‐treatment scores were reported, using the methods proposed in Section 6.5.1 of the Cochrane Handbook (Higgins 2022). For studies that did not report change scores from baseline or for scores that were not calculable, we used the final values, as the difference in mean final values is, on average, the same as the difference in mean change scores in randomised controlled trials (Higgins 2022). We calculated the MD and 95% CIs as the summary statistic for symptom scores for studies that used the same scales. We calculated the SMD and 95% CIs between two groups if different scales were used in the primary studies. However, we did not combine the final value and change scores as SMD and have reported them separately. For continuous outcomes, we used the inverse variance method. We used Review Manager Web software to perform analyses (RevMan Web 2021).
When meta‐analysis was not possible, or only a single trial was available for each comparison, we created narrative statements describing the effect estimates and their interpretation (Schünemann 2021). We created effect‐direction plots summarising the effect of each intervention for each outcome and the risk of bias assessments (Boon 2021; Thomson 2013). We chose SMD for continuous outcomes for qualitative comparability of effect sizes. We followed the reporting guidance for Synthesis Without Meta‐analysis (SWiM) (McKenzie 2021).
Subgroup analysis and investigation of heterogeneity
We had planned to carry out the following subgroup analyses.
Treatment duration (less than four weeks versus greater than four weeks)
Type of herbal preparation (oil extract, infusion, capsules, etc.)
Positive H pylori status defined by biopsy, culture, or another testing versus H pylori‐negative status
The presence of gastrointestinal comorbidities: irritable bowel syndrome, gastroesophageal reflux disease, or both.
We planned to assess the following outcomes in subgroup analysis.
Global symptoms of dyspepsia
Adverse events
We planned to use the formal statistical test employing the I2 statistic to test for subgroup interactions.
Sensitivity analysis
We performed sensitivity analysis defined a priori to assess the robustness of our conclusions. This involved the following.
Risk of bias: excluding studies at high risk of bias.
Case‐mix: excluding studies with > 20% of comorbidity with irritable bowel syndrome or gastroesophageal reflux disease, or both.
For dichotomous outcomes when missing data were not assumed to be missing at random (see Dealing with missing data).
Reaching conclusions
We based our conclusions only on findings from the meta‐analysis or Synthesis Without Meta‐analysis of the included studies for this review. We avoided making recommendations for practice, and our implications for research give the reader a clear sense of where the focus of any future research in the area should be and the remaining uncertainties.
Summary of findings and assessment of the certainty of the evidence
Considering the multiple interventions and comparisons and with the editorial feedback of the Cochrane Gut Review Group, we created summary of findings tables for comparisons that included a meta‐analysis of two or more trials, including the following outcomes.
Global symptoms of dyspepsia: symptom score (short‐term follow‐up)
Global symptoms of dyspepsia: number of participants with improved symptoms (short‐term follow‐up)
Adverse events (long‐term follow‐up)
Quality of life (short‐term follow‐up)
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of a body of evidence related to the studies that contributed data to the meta‐analyses for the prespecified outcomes. We used the methods and recommendations described in Chapter 14 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022), employing GRADEpro GDT software (GRADEpro GDT 2020). We justified all decisions to up‐ or downgrade the quality of studies using footnotes and made comments to aid the reader's understanding of the review where necessary. We created additional tables to summarise the evidence from individual trials following the guidance for Synthesis Without Meta‐analysis (SWiM) by creating effect direction plots summarising the effect of each intervention for each outcome and the risk of bias assessments (Boon 2021; Thomson 2013).
Results
Description of studies
See the details of the included studies in the Characteristics of included studies.
Results of the search
After deduplication, we retrieved and reviewed 4150 citations based on title/abstract for eligibility: 816 from MEDLINE, 2224 from Embase, 907 from the Cochrane Library, 37 from LILACS and 166 from AMED. Then we excluded 4020 citations after the screening of title/abstract eligibility; thus, we assessed 130 studies further in full text, of which 41 studies met the inclusion criteria. See Figure 1 for the PRISMA flow diagram.
1.
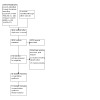
Flow chart of study selection
Included studies
We included 41 studies (52 reports) with 4477 participants.
Study design and setting
All studies were parallel‐group randomized controlled studies. The median sample size was 103. All studies were in an outpatient setting; however, participants remained in observation during the first dose in some studies.
Country of origin
Twelve of 41 studies were from Iran (Alizadeh‐Naini 2020; Azimi 2017; Babaeian 2017; Bordbar 2020; Eftekharafzali 2018; Ghoshegir 2015; Khonche 2017; Mohtashami 2015; Pasalar 2015; Rafieian‐Kopaei 2005; Sattarzadeh 2021; Zobeiri 2021); 10 were from Germany (Braden 2009; Holtmann 2003; Madisch 1999; Madisch 2001a; Madisch 2004; May 2000; Rich 2017; Rosch 2002; Vinson 2020; Von Arnim 2007); four from India (Allan 2012; Mala 2018; Panda 2020Sastry 2016); two from Italy (Bortolotti 2002; Giacosa 2015); three from Thailand (Chitapanarux 2020; Thamlikitkul 1989; Yongwatana 2022); one from Brazil (Da Mota Menezes 2006); one from China (Sun 2016); one from Greece (Dabos 2010); one from Lithuania (Kupcinskas 2008); one from Saudi Arabia (Salem 2010); one from Taiwan (Hu 2011); one from the USA (Chey 2019); one from Australia (Holtmann 2013); and one from Korea (Shin 2021). It is not clear where the final study was conducted (Puttapitakpong 2016).
Participants
We included participants with functional dyspepsia. However, 17 studies reported using Rome III criteria (Alizadeh‐Naini 2020; Allan 2012; Azimi 2017; Babaeian 2017; Bordbar 2020; Chey 2019; Eftekharafzali 2018; Ghoshegir 2015; Holtmann 2013; Hu 2011; Khonche 2017; Mala 2018; Mohtashami 2015; Panda 2020; Pasalar 2015; Rich 2017; Sun 2016), four studies used Rome IV (Chitapanarux 2020; Sattarzadeh 2021; Shin 2021; Yongwatana 2022), and 20 studies did not adequately report the type of functional dyspepsia (Bortolotti 2002; Braden 2009; Dabos 2010; Da Mota Menezes 2006; Giacosa 2015; Holtmann 2003; Kupcinskas 2008; Madisch 1999; Madisch 2001a; Madisch 2004; May 2000; Puttapitakpong 2016; Rafieian‐Kopaei 2005; Rosch 2002; Salem 2010; Sastry 2016; Thamlikitkul 1989; Vinson 2020; Von Arnim 2007; Zobeiri 2021). Most studies listed functional gastrointestinal comorbidities as exclusion criteria: irritable bowel disorder (Azimi 2017; Madisch 2001a; Pasalar 2015; Rafieian‐Kopaei 2005; Von Arnim 2007), gastroesophageal reflux (Bortolotti 2002; Braden 2009; Da Mota Menezes 2006; Eftekharafzali 2018; Hu 2011; Kupcinskas 2008; Mala 2018; May 2000; Mohtashami 2015), or both (Allan 2012; Babaeian 2017; Bordbar 2020; Ghoshegir 2015; Giacosa 2015; Holtmann 2003; Khonche 2017; Madisch 2004; Panda 2020; Rich 2017; Rosch 2002; Sattarzadeh 2021; Zobeiri 2021). The remaining 14 studies did not specify the inclusion/exclusion of these comorbidities.
Interventions
The studies included the following interventions.
Apium graveolens and Trachyspermum copticom (Azimi 2017)
Artichoke (Holtmann 2003)
Astaxanthin (Kupcinskas 2008)
Boesenbergia rotunda (Chitapanarux 2020)
Cinnamon oil (Zobeiri 2021)
Curcuma longa (Puttapitakpong 2016; Thamlikitkul 1989; Yongwatana 2022)
Cuadrania tricuspidata (Shin 2021)
Ferula asafoetida (Mala 2018)
Ginger (Hu 2011)
Ginger and Artichoke (Giacosa 2015)
Glycyrrhiza glabra (GutGard) (Allan 2012)
Jollab (Pasalar 2015)
Lafoensia pacari (Da Mota Menezes 2006)
Mentha longifolia (Babaeian 2017)
Mentha pulegium (Khonche 2017)
Nigella sativa (Alizadeh‐Naini 2020; Mohtashami 2015; Salem 2010)
Ocimum basilicum (Rafieian‐Kopaei 2005)
OLNP‐06 (Panda 2020)
Peppermint oil and caraway oil (Chey 2019 (COLM preparation); Madisch 1999; May 2000; Rich 2017)
Peppermint oil, caraway oil and camellia oil (Enteroplant) (Sun 2016)
Pimpinella anisum (Ghoshegir 2015)
Pistacia atlantica (Eftekharafzali 2018)
Pistacia lentiscus (Chios mastic gum/oil) (Dabos 2010; Sattarzadeh 2021)
Pudin hara (Sastry 2016)
Red pepper (Bortolotti 2002)
Iberogast [STW5/STW5s/ STW5 ll] (Braden 2009; Holtmann 2013; Madisch 2001a; Madisch 2004; Rosch 2002; Vinson 2020; Von Arnim 2007)
Trachyspermum ammi L. , Anethum graveolens L. and Zataria multiflora Boiss (Bordbar 2020)
Comparisons
Twenty‐nine studies compared the following herbal preparations with placebo.
Artichoke (Holtmann 2003)
Boesenbergia rotunda (Chitapanarux 2020)
Cinnamon oil (Zobeiri 2021)
Cuadrania tricuspidata (Shin 2021)
Ferula asafoetida (Mala 2018)
Ginger (Hu 2011)
Ginger and Artichoke (Giacosa 2015)
Glycyrrhiza glabra (GutGard) (Allan 2012)
Jollab (Pasalar 2015)
Lafoensia pacari (Da Mota Menezes 2006)
Mentha longifolia (Babaeian 2017)
Mentha pulegium (Khonche 2017)
Nigella sativa (Alizadeh‐Naini 2020; Mohtashami 2015)
Ocimum basilicum (Rafieian‐Kopaei 2005)
OLNP‐06 (Panda 2020)
Peppermint oil and caraway oil (Chey 2019 (COLM preparation); May 2000; Rich 2017)
Pimpinella anisum (Ghoshegir 2015)
Pistacia atlantica (Eftekharafzali 2018)
Pistacia lentiscus (Chios mastic gum/oil) (Dabos 2010; Sattarzadeh 2021)
Red pepper (Bortolotti 2002)
Iberogast [STW5/STW5s/ STW5 ll] (Braden 2009; Madisch 2001a; Madisch 2004; Vinson 2020; Von Arnim 2007)
The remaining twelve studies compared herbal preparations with other herbal products, the same herbal products with different dosing or other drugs, although some of them also included a placebo arm.
From studies of two arms, one compared Trachyspermum Ammi L., Anethum graveolens L., and Zataria multiflora Boiss and omeprazole (Bordbar 2020); one compared two different preparations of pudin hara (Sastry 2016), and one compared peppermint oil and caraway oil and cisapride (Madisch 1999).
From studies of three arms, three compared Curcuma longa with placebo and omeprazole (Puttapitakpong 2016; Yongwatana 2022) or flatulence (Thamlikitkul 1989); one compared STW5, STW5II, and cisapride (Rosch 2002); one compared Apium graveolens and Trachyspermum copticom, omeprazole and placebo (Azimi 2017); one compared two different doses of Enteroplant and placebo (Sun 2016) and one compared two different doses of Astaxanthin and placebo (Kupcinskas 2008).
One study of four arms compared three different doses of Nigella sativa and triple therapy (clarithromycin, amoxicillin, and omeprazole) (Salem 2010).
One study (Holtmann 2013) compared STW5 versus placebo and omeprazole.
Outcomes
The majority of studies reported the global symptoms of dyspepsia in a continuous or dichotomous fashion, except for (Alizadeh‐Naini 2020; Eftekharafzali 2018; Hu 2011; Kupcinskas 2008; Rafieian‐Kopaei 2005; Sattarzadeh 2021), which reported individual symptoms. In one study, exact results were impossible to extract as they were only expressed in a bar graph (Azimi 2017). Four studies did not measure adverse events (Madisch 2001a; Puttapitakpong 2016; Rafieian‐Kopaei 2005; Yongwatana 2022). Finally, 15 studies reported measurements of quality of life (Alizadeh‐Naini 2020; Allan 2012; Azimi 2017; Babaeian 2017; Bordbar 2020; Ghoshegir 2015; Holtmann 2003; Holtmann 2013; Khonche 2017; Kupcinskas 2008; Mala 2018; Mohtashami 2015; Pasalar 2015; Sun 2016; Yongwatana 2022).
The instruments used for the measurement of globals symptoms of dyspepsia were: the gastrointestinal symptom score (GIS) (Braden 2009; Holtmann 2013; Madisch 2001a; Madisch 2004; Rosch 2002; Shin 2021; Vinson 2020; Von Arnim 2007; Zobeiri 2021), Hong Kong dyspepsia index (HKDI) (Dabos 2010; Khonche 2017; Mohtashami 2015), gastrointestinal symptom rating scale (GSRS)(Bordbar 2020; Mala 2018; Shin 2021), short‐forms of Leeds dyspepsia questionnaire (Chitapanarux 2020; Pasalar 2015; Salem 2010), clinical global impression score (CGI) (Chey 2019; May 2000), global assessment of dyspepsia symptoms (Sun 2016; Thamlikitkul 1989), overall treatment efficacy scale (OTE) (Da Mota Menezes 2006; Panda 2020), functional dyspepsia severity scale (Babaeian 2017; Ghoshegir 2015), the severity of dyspepsia assessment (SODA) (Puttapitakpong 2016; Yongwatana 2022), and in some cases, a Likert, numbered or visual aspect scale was utilized (Alizadeh‐Naini 2020; Allan 2012; Azimi 2017; Bortolotti 2002; Eftekharafzali 2018; Giacosa 2015; Holtmann 2003; Hu 2011; Kupcinskas 2008; Madisch 1999; Rafieian‐Kopaei 2005).
To measure and report quality of life, the studies used two main scales: either the short‐form health survey 36 (SF‐36) (Alizadeh‐Naini 2020; Babaeian 2017; Bordbar 2020; Ghoshegir 2015; Khonche 2017; Kupcinskas 2008; Mohtashami 2015; Pasalar 2015; Sun 2016) or the Nepean dyspepsia index (NDI) (Allan 2012; Azimi 2017; Holtmann 2003; Holtmann 2013; Mala 2018; Rich 2017; Shin 2021). One study used the EuroQoL EQ‐5D questionnaire (Yongwatana 2022).
Most studies reported the incidence of adverse events, but the level of detail was variable. Six studies did not report this outcome (Holtmann 2013; Hu 2011; Puttapitakpong 2016; Rafieian‐Kopaei 2005; Von Arnim 2007; Yongwatana 2022).
Funding
Eight studies were funded by governmental institutions (Alizadeh‐Naini 2020; Bordbar 2020; Chitapanarux 2020; Kupcinskas 2008; Mohtashami 2015; Pasalar 2015; Rafieian‐Kopaei 2005; Thamlikitkul 1989); 14 studies were funded by the pharmaceutical industry (Chey 2019; Holtmann 2003; Khonche 2017; Madisch 1999; Madisch 2001a; Madisch 2004; Mala 2018; May 2000; Panda 2020; Rich 2017; Rosch 2002; Sastry 2016; Shin 2021; Von Arnim 2007), and one study was funded by a medical association (Yongwatana 2022). The rest of the studies did not specify their sources of funding.
Excluded studies
We excluded 53 studies for the following reasons.
21 studies with ineligible population: (ACTRN12619001236189; Asif 2015; Barnick 1990; CTRI/2022/03/041419; Dimitrov 1983; Dos 2010; Eady 2019; Hajiaghamohammadi 2016; IRCT20110310006026N9; IRCT20170317033107N3; IRCT20200128046288N3; Ivashkin 2022; Labenz 2023; ; Lee 2020; Lopresti 2018; Marakis 2002; Muss 2013; NCT04593836; Nili‐Ahmadabadi 2017; Shim 2019; Xiao 2013).
11 studies with ineligible study design: (Asha 2017; Aydin 1997; Bommer 2013; Di 2007; Fuhrer 2011; Hashem‐Dabaghian 2016; Kammerer 2001; Kelber 2017; Meier 2005; Metugriachuk 2008; Pasalar 2015a).
21 studies with an ineligible intervention: (Arai 2011; Arai 2012; Bekar 2011; Choi 2011; Choi 2020; Du 2014; Gao 2007; Gasbarrini 2010; Gong 2019; Guo 2011; Guo 2014; IRCT2017022332738N1; KCT0003761 2019; KCT0004085 2019; KCT0005265 2020; Lacy 2022; Kim 2010; Mihai 2019; Shim 2015; Shim 2019; Wang 2017).
For more details, see Characteristics of excluded studies.
Studies awaiting classification
We were unable to retrieve 13 full‐text articles (Borgia 1981; Borgia 1985; Chawla 1982; Ernst 2002; Fani 2007; Fintelmann 1996; Fintelmann 1999; Freise 1999; Madisch 2000; Madisch 2001b; May 1996; Rosch 2001; Roth 1996). When possible, we contacted the authors requesting further information, but received no response. We also identified eight studies with insufficient information to assess their eligibility (CTRI/2018/02/012101 2018; IRCT20130211012438N27; IRCT20200128046291N1; ISRCTN31202330; Ivashkin 2020 (abstract); KCT0005020; NCT04742985; TCTR20180530003). For more details, see Characteristics of studies awaiting classification.
Ongoing studies
We identified 15 studies that are currently recruiting people with functional dyspepsia.
One study for the comparison of anise, fennel, Trachyspermum and caraway versus placebo (IRCT20220304054179N1)
One study for the comparison of ginger extract versus placebo (CTRI/2020/04/024448).
One study for the comparison of Pistacia lentiscus versus sesame (IRCT20090527001957N8).
One study for the comparison of Apium graveolense beans plus Trachyspermum copticum beans versus domperidone (IRCT20150927024228N2).
One study for the comparison of Ajwain fruit plus Zataria multiflora and dill oil versus clarithromycin plus amoxiciline and omeprazole (IRCT20160721029026N4).
One study for the comparison of cinnamon oil versus sesame oil (IRCT20170802035460N2).
One study for the comparison of cumin powder plus coriander seed (IRCT20190304042911N1).
One study for the comparison of Govarcin versus metoclopramide (IRCT20190806044456N1).
One study for the comparison of a compound honey syrup versus placebo (IRCT20200303046677N6).
One study for sumac extract capsule versus placebo or omeprazole (IRCT20200424047192N1).
One study for the comparison of Gingest versus placebo (NCT03548363).
Two studies for the comparison of the extract of Dolichos lablab Linne versus placebo (KCT0005229; NCT04482478).
One study for the comparison of Iberogast and Iberogast‐N versus placebo (NCT04656730).
One study for the comparison of Maytenus ilicifolia at two different doses (RBR‐10yqwrk6).
For more details, see Characteristics of ongoing studies.
Risk of bias in included studies
We provide a summary of risk of bias assessments of the included studies, including support for our judgements, in Figure 2.
2.

Summary of the risk of bias assessment of the included studies.
Allocation
Random sequence generation
We rated 27 studies as having a low risk of bias (Alizadeh‐Naini 2020; Allan 2012; Babaeian 2017; Bordbar 2020; Chitapanarux 2020; Dabos 2010; Da Mota Menezes 2006; Eftekharafzali 2018; Giacosa 2015; Holtmann 2003; Khonche 2017; Kupcinskas 2008; Madisch 1999; Madisch 2001a; Madisch 2004; Mala 2018; May 2000; Mohtashami 2015; Pasalar 2015; Rich 2017; Rosch 2002; Sastry 2016; Sattarzadeh 2021; Shin 2021; Sun 2016; Von Arnim 2007; Yongwatana 2022). The rest of the studies did not adequately describe the random sequence generation.
Allocation concealment
We rated 25 studies as having a low risk of bias (Alizadeh‐Naini 2020; Allan 2012; Azimi 2017; Babaeian 2017; Bordbar 2020; Chitapanarux 2020; Dabos 2010; Da Mota Menezes 2006; Giacosa 2015; Holtmann 2003; Khonche 2017; Kupcinskas 2008; Madisch 1999; Madisch 2004; Mala 2018; May 2000; Mohtashami 2015; Pasalar 2015; Rich 2017; Rosch 2002; Sattarzadeh 2021; Shin 2021; Von Arnim 2007; Yongwatana 2022; Zobeiri 2021). One study had a high risk of bias because the participants who did not continue in follow‐up were replaced by new participants without being randomized (Rafieian‐Kopaei 2005). The rest of the studies did not adequately describe allocation concealment.
Blinding
Performance bias
We rated 25 studies as having a low risk of performance bias (Alizadeh‐Naini 2020; Allan 2012; Azimi 2017; Babaeian 2017; Bordbar 2020; Dabos 2010; Da Mota Menezes 2006; Ghoshegir 2015; Giacosa 2015; Holtmann 2003; Khonche 2017; Madisch 1999; Madisch 2004; Mala 2018; May 2000; Mohtashami 2015; Pasalar 2015; Rafieian‐Kopaei 2005; Rich 2017; Rosch 2002; Sattarzadeh 2021; Shin 2021; Von Arnim 2007; Yongwatana 2022; Zobeiri 2021). Two studies were open‐label, so we rated them as having a high risk of bias (Salem 2010; Sastry 2016). The rest of the studies did not adequately describe the blinding of participants and personnel.
Detection bias
We rated 34 studies as having a low risk of detection bias, mostly by the use of placebo to blind participants (patient‐reported outcomes) (Alizadeh‐Naini 2020; Allan 2012; Azimi 2017; Babaeian 2017; Bordbar 2020; Braden 2009; Chitapanarux 2020; Dabos 2010; Da Mota Menezes 2006; Eftekharafzali 2018; Ghoshegir 2015; Giacosa 2015; Holtmann 2003; Hu 2011; Khonche 2017; Kupcinskas 2008; Madisch 1999; Madisch 2001a; Madisch 2004; Mala 2018; May 2000; Mohtashami 2015; Panda 2020; Pasalar 2015; Rafieian‐Kopaei 2005; Rich 2017; Rosch 2002; Sattarzadeh 2021; Shin 2021; Sun 2016; Thamlikitkul 1989; Von Arnim 2007; Yongwatana 2022; Zobeiri 2021). We rated the two open‐label studies as having a high risk of bias (Salem 2010; Sastry 2016). The rest of the studies did not adequately describe the blinding of outcome assessment.
Incomplete outcome data
We rated 28 studies as having a low risk of attrition bias (Alizadeh‐Naini 2020; Allan 2012; Babaeian 2017; Bordbar 2020; Bortolotti 2002; Braden 2009; Chey 2019; Dabos 2010; Da Mota Menezes 2006; Eftekharafzali 2018; Ghoshegir 2015; Giacosa 2015; Holtmann 2003; Hu 2011; Khonche 2017; Kupcinskas 2008; Madisch 1999; Madisch 2001a; Madisch 2004; Mala 2018; May 2000; Mohtashami 2015; Panda 2020; Rosch 2002; Sattarzadeh 2021; Sun 2016; Thamlikitkul 1989; Yongwatana 2022). We rated three studies as having a high risk of bias due to substantial attrition (Azimi 2017; Shin 2021; Zobeiri 2021). The rest of the studies did not adequately describe the incomplete outcome data.
Selective reporting
We rated 10 studies as having a low risk of bias due to selective reporting as their results matched the study protocol or registry (Alizadeh‐Naini 2020; Chitapanarux 2020; Da Mota Menezes 2006; Khonche 2017; Mala 2018; Mohtashami 2015; Panda 2020; Shin 2021; Yongwatana 2022; Zobeiri 2021). Two studies (Ghoshegir 2015; Pasalar 2015) were rated as having a high risk of bias due to the lack of reporting of outcomes that were indicated in the study protocol. The rest of the studies provided insufficient data for judgement.
Other potential sources of bias
We rated five studies as having an unclear risk of bias: three were reported only as abstracts (Holtmann 2013; Puttapitakpong 2016; Vinson 2020), and two did not adequately baseline characteristics or how outcomes were measured (Mala 2018; Thamlikitkul 1989). The rest of the studies had a low risk of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
STW5 (Iberogast) versus placebo
Six studies with 970 participants were included in this comparison (Braden 2009; Holtmann 2013; Madisch 2001a; Madisch 2004; Vinson 2020; Von Arnim 2007). The duration of the trials varied from 4 to 12 weeks. Two studies were published only as conference abstracts (Holtmann 2013; Vinson 2020). One study used STW5 ll as the sole intervention (Madisch 2004), and another study utilized STW5s besides regular STW5 (Madisch 2001a). See Table 1.
Global symptoms of dyspepsia
Five studies with 814 participants presented the GIS score for this outcome (range 0 to 40; higher scores indicate worse symptoms) (Braden 2009; Madisch 2001a; Madisch 2004; Vinson 2020; Von Arnim 2007). STW5 may moderately improve global symptoms of dyspepsia compared with placebo at 28 to 56 days' follow‐up, but the evidence is very uncertain (MD ‐2.64, 95% CI ‐4.39 to ‐0.90; I² = 87%; Analysis 1.1). The certainty of the evidence is very low due to the risk of bias, inconsistency, and imprecision. We were unable to explore this inconsistency due to the characteristics of the studies (see Differences between protocol and review).
1.1. Analysis.

Comparison 1: STW5 versus placebo, Outcome 1: Global symptoms of dyspepsia (continuous)
Two studies with 324 participants presented a responder analysis (> 20% to 50% improvement in GIS scores) (Holtmann 2013; Vinson 2020). STW5 may increase the responder rate compared to placebo at four to eight weeks' follow‐up (RR 1.55, 95% CI 0.98 to 2.47; Analysis 1.2). The certainty of the evidence is low due to the risk of bias and imprecision.
1.2. Analysis.

Comparison 1: STW5 versus placebo, Outcome 2: Global symptoms of dyspepsia (responders)
Adverse events
Four studies with 786 participants reported this outcome (Braden 2009; Madisch 2004; Vinson 2020; Von Arnim 2007). SWT5 may result in little to no differences in adverse events compared to placebo (RR 0.92, 95% CI 0.52 to 1.54; I2 = 0%; Analysis 1.3). Another study reported that there was one case of a mild adverse event possibly attributable to the intervention (Madisch 2001a). The certainty of the evidence is low due to the risk of bias and imprecision.
1.3. Analysis.

Comparison 1: STW5 versus placebo, Outcome 3: Adverse events
Quality of life
One study with 52 participants reported this outcome (Holtmann 2013). It stated, "differences between treatment groups did not yield significance." The certainty of the evidence is low due to the risk of bias and imprecision.
Peppermint and caraway oil versus placebo
Three studies with 305 participants were included in this comparison (Chey 2019; May 2000; Rich 2017). See Table 2. Chey 2019 categorised patients into 'no improvement', 'much improvement' or 'very much improvement' on a scale (0, 1 or 2 points respectively).
Global symptoms of dyspepsia
Two studies with 210 participants presented continuous outcome data (CGI scores in May 2000; NDI pain and discomfort subscale in Rich 2017). Peppermint and caraway oil probably result in a large improvement in global symptoms of dyspepsia compared to placebo at four weeks (SMD ‐0.87, 95% CI ‐1.15 to ‐0.58; I2 = 0%; Analysis 2.1). The certainty of the evidence is moderate due to the risk of bias.
2.1. Analysis.

Comparison 2: Peppermint and caraway oil versus placebo, Outcome 1: Global symptoms of dyspepsia (continuous)
All studies presented a responder analysis (minimal, much, or very much clinical improvement) (Chey 2019; May 2000; Rich 2017). Peppermint and caraway oil probably increase the improvement rate of global symptoms of dyspepsia compared to placebo at four‐week follow‐up (RR 1.53, 95% CI 1.30 to 1.81; I2 = 0%; Analysis 2.2). The certainty of the evidence was moderate due to the risk of bias.
2.2. Analysis.

Comparison 2: Peppermint and caraway oil versus placebo, Outcome 2: Global symptoms of dyspepsia (responders)
Adverse events
Three studies with 305 participants reported this outcome (Chey 2019; May 2000; Rich 2017). Peppermint and caraway oil may result in little to no difference in adverse events compared to placebo at four‐week follow‐up (RR 1.56, 95% CI 0.69 to 3.53; I2 = 47%; Analysis 2.3). The certainty of the evidence is low due to the risk of bias and imprecision.
2.3. Analysis.

Comparison 2: Peppermint and caraway oil versus placebo, Outcome 3: Adverse events
Quality of life
One study with 99 participants reported this outcome on the NDI scale (Rich 2017). Peppermint oil and caraway oil probably improve quality of life compared to placebo at four‐week follow‐up (MD ‐131.40, 95% CI ‐193.76 to ‐69.04; Analysis 2.4). The certainty of the evidence was moderate due to the risk of bias.
2.4. Analysis.

Comparison 2: Peppermint and caraway oil versus placebo, Outcome 4: Quality of life
Curcuma longa versus placebo
Three studies with 190 participants assessed the effect of this herbal medicine (Puttapitakpong 2016; Thamlikitkul 1989; Yongwatana 2022). See Table 3.
Global symptoms of dyspepsia
Two studies with 110 participants assessed the effect of Curcuma longa using the GIS score for this outcome (range 0 to 40; higher scores indicate worse symptoms) (Puttapitakpong 2016; Yongwatana 2022). Curcuma longa probably results in a moderate improvement of global symptoms of dyspepsia compared to placebo at four‐week follow‐up (MD ‐3.33, 95% CI ‐5.84 to ‐0.81; I2 = 47%; Analysis 3.1). The certainty of the evidence is moderate due to imprecision.
3.1. Analysis.

Comparison 3: Curcuma longa versus placebo, Outcome 1: Global symptoms of dyspepsia (continuous)
An additional study with 76 participants also indicates that Curcuma longa may increase the improvement rate of global symptoms of dyspepsia compared to placebo (RR 1.5, 95% CI, 1.06 to 2.11; Analysis 3.2). The certainty of the evidence is low due to the risk of bias and imprecision.
3.2. Analysis.

Comparison 3: Curcuma longa versus placebo, Outcome 2: Global symptoms of dyspepsia (responders)
Adverse events
One study with 89 participants reported this outcome (Yongwatana 2022). Curcuma longa probably results in little to no difference in adverse events compared to placebo at four‐week follow‐up (RR 1.26, 95% CI 0.51 to 3.08; Analysis 3.3). The certainty of the evidence is moderate due to imprecision.
3.3. Analysis.

Comparison 3: Curcuma longa versus placebo, Outcome 3: Adverse events
Another study stated that the "frequency of the side effects was the same" (Thamlikitkul 1989).
Quality of life
One study with 89 participants reported this outcome (Yongwatana 2022). Curcuma longa may result in a small improvement in quality of life compared to placebo at four‐week follow‐up (MD 0.05, 95% CI 0.01 to 0.09; Analysis 3.4). The certainty of the evidence is moderate due to imprecision.
3.4. Analysis.

Comparison 3: Curcuma longa versus placebo, Outcome 4: Quality of life
Other herbal medicines versus placebo
See the Table 4 for the effect direction plot and the analyses for the forest plots for each trial (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.4).
4.1. Analysis.

Comparison 4: Herbal medicines versus placebo, Outcome 1: Global symptoms of dyspepsia (continuous)
4.2. Analysis.

Comparison 4: Herbal medicines versus placebo, Outcome 2: Global symptoms of dyspepsia (responders)
4.3. Analysis.

Comparison 4: Herbal medicines versus placebo, Outcome 3: Quality of life
4.4. Analysis.

Comparison 4: Herbal medicines versus placebo, Outcome 4: Adverse events
Studies at low risk of bias
Lafoensia pacari
Based on one study with 97 participants (Da Mota Menezes 2006), this herbal medicine may improve global symptoms of dyspepsia (RR 1.52, 95% CI 1.08 to 2.14). In terms of adverse events, there was little to no difference compared to placebo (RR 1.52, 95% CI 0.66 to 3.49). There was no information on the quality of life. The overall certainty of the evidence for these results is moderate due to imprecision.
Mentha pulegium
Based on one study with 100 participants (Khonche 2017), this herbal medicine might result in little to no difference in global symptoms of dyspepsia (SMD ‐0.38, 95% CI ‐0.78 to 0.02). There were no adverse events reported in control or intervention groups. The intervention may have a moderate effect on the improvement of quality of life (SMD ‐0.61, 95% CI ‐1.01 to ‐0.21). The overall certainty of the evidence for these results is moderate due to imprecision.
Nigella sativa
Two studies assessed the effect of Nigella sativa on FD. The first study included 70 participants and found that this herbal medicine may have a large effect on the improvement of global symptoms of FD (SMD ‐1.59, 95% CI ‐2.13 to ‐1.05) (Mohtashami 2015). There was no information on the quality of life. The overall certainty of the evidence for these results is high. The second study included 51 participants (Alizadeh‐Naini 2020), but it did not report the effect of the intervention on global symptoms and quality of life as a global score. There may be little to no difference in adverse events (RR 1.0, 95% CI 0.53 to 1.88, I² = 0%, 2 studies, 121 participants). The overall certainty of the evidence for these results is moderate due to imprecision.
Studies at unclear risk of bias
Artichoke
Based on one study with 244 participants, this intervention may have a low effect on the improvement of global symptoms of dyspepsia (SMD ‐0.34, 95% CI ‐0.59 to ‐0.09) (Holtmann 2003). It might result in little to no difference in adverse events (RR 1.44, 95% CI 0.84 to 2.44). The intervention may have a small effect on the improvement of quality of life (SMD ‐0.38, 95% CI ‐0.64 to ‐0.13). The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Astaxanthin
One study with 131 participants did not report its effects on global symptoms of dyspepsia (Kupcinskas 2008). In terms of adverse events, there was little to no difference compared to placebo (RR 1.23, C 0.55 to 2.74). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Boesenbergia rotunda (fingerroot)
Based on one study with 160 participants (Chitapanarux 2020), this herbal medicine may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐2.22, 95% CI ‐2.62 to ‐1.83). In terms of adverse events, there was little to no difference compared to placebo (RR 0.75, 95% CI 0.17 to 3.24). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Pistacia lentiscus (Chios mastic gum/oil)
Based on one study with 148 participants (Dabos 2010), this intervention may have a low effect on the improvement of global symptoms of dyspepsia (SMD ‐0.33, 95% CI ‐0.66 to ‐0.01). There were no differences in adverse events compared to placebo (RR 5.00, 95% CI 0.24 to 102.40). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision. One study with 63 participants compared Pistacia lentiscus (topic mastic oil) with placebo (Sattarzadeh 2021). The study reported that there were no adverse events in both arms, but no other outcomes of interest of this review.
Enteroplant
Based on one study with 198 participants (Sun 2016), this intervention may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐1.09, 95% CI ‐1.40 to ‐0.77). There were no differences in adverse events compared to placebo (RR 0.98, 95% CI 0.09 to 10.58). Regarding the quality of life, there was little to no difference compared to placebo (SMD 0.22, 95% CI ‐0.07 to 0.52). The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Ferula asafoetida
Based on one study with 43 participants (Mala 2018), this herbal medicine may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐1.51, 95% CI ‐2.20 to ‐0.83). There were no adverse events reported in control or intervention groups. The intervention may have a large effect on the improvement of quality of life (SMD ‐2.56, 95% CI ‐3.38 to ‐1.74). The certainty of the evidence for improving global symptoms of dyspepsia is low due to the unclear risk of bias and imprecision but moderate for improving quality of life due to the unclear risk of bias.
Ginger (Zingiber officinalis) and artichoke thistle (Cynara cardunculus)
Based on one study with 126 participants (Giacosa 2015), this intervention may improve global symptoms of dyspepsia (RR 1.64, 95% CI 1.27 to 2.13). There were no adverse events reported in control or intervention groups. There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Glycyrrhiza glabra (Gutcard)
Based on one study with 50 participants (Allan 2012), this herbal medicine may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐1.86, 95% CI ‐2.54 to ‐1.19). There were no adverse events reported in control or intervention groups. The intervention may have a large effect on the improvement of quality of life (SMD ‐3.01, 95% CI ‐3.84 to ‐2.18). The overall certainty of the evidence for these results is moderate due to the unclear risk of bias.
Mentha longifolia
Based on one study with 88 participants (Babaeian 2017), this herbal medicine may have a moderate effect on the worsening of global symptoms of dyspepsia (SMD 0.46, 95% CI 0.04 to 0.88). However, it might result in little to no difference in adverse events (RR 1.00, 95% CI 0.06 to 15.49). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
OLNP‐06
Based on one study with 48 participants (Panda 2020), this intervention may improve global symptoms of dyspepsia (RR 3.80, 95% CI 1.70 to 8.51). There were no differences in adverse events compared to placebo (RR 1.0, 95% CI 0.15 to 6.55). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Pistacia atlantica
One study with 119 participants assessed this herbal product but did not report its effects on global symptoms of dyspepsia (Eftekharafzali 2018). In terms of adverse events, there was little to no difference compared to placebo (RR 0.95, 95% CI 0.14 to 6.53). The effect on the quality of life was not assessed. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Red pepper
Based on one study with 27 participants (Bortolotti 2002), this intervention may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐1.07, 95% CI ‐1.89 to ‐0.26). However, the intervention group had a higher risk of adverse events (RR 4.31, 95% CI 1.56 to 11.89). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Studies at high risk of bias
Apium graveolens and Trachyspermum copticom
One study with 92 participants assessed this herbal product but did not report its effects on global symptoms of dyspepsia (Azimi 2017). There were no differences in adverse events compared to placebo (RR 0.18, 95% CI 0.01 to 3.57). The intervention may have a large effect on the improvement of quality of life (SMD ‐1.03, 95% CI ‐1.44 to ‐0.61). The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Cinnamon oil
Based on one study with 51 participants (Zobeiri 2021), this herbal medicine may produce little to no difference in global symptoms of dyspepsia (SMD 0.38, 95% CI ‐0.17 to 0.94). Regarding adverse effects, there was little to no difference compared to placebo (RR 0.75 95% CI 0.14 to 4.12). The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Cudrania tricuspidata
Based on one study with 83 participants (Shin 2021), this herbal medicine may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐1.19, 95% CI ‐1.66 to ‐0.72) and a moderate benefit in quality of life (SMD ‐0.89, 95% CI ‐1.35 to ‐0.44), with little to no difference in adverse events compared to placebo (RR 0.80, 95% CI 0.42 to 1.53). The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Jollab
Based on one study with 133 participants (Pasalar 2015), this intervention may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐1.22, 95% CI ‐1.59 to ‐0.85). There were no differences in adverse events compared to placebo (RR 2.39, 95% CI 0.48 to 11.89). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Pimpinella anisum
Based on one study with 107 participants (Ghoshegir 2015), this herbal medicine may have a large effect on the improvement of global symptoms of dyspepsia (SMD ‐2.30, 95% CI ‐2.79 to ‐1.80). In terms of adverse events, there was little to no difference compared to placebo (RR 0.25, 95% CI 0.01 to 5.17). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Other studies
Hu 2011 (ginger) and Rafieian‐Kopaei 2005 (Ocimum basilicum) assessed the effects of herbal products, but they did not report outcomes relevant to this review.
Herbal medicines compared to other treatments
See Table 5 for the effect direction plot and the analyses for the forest plots for each trial (Analysis 5.1; Analysis 5.2; Analysis 5.3; Analysis 5.4).
5.1. Analysis.

Comparison 5: Herbal medicine versus other agents, Outcome 1: Global symptoms of dyspepsia (continuous)
5.2. Analysis.

Comparison 5: Herbal medicine versus other agents, Outcome 2: Global symptoms of dyspepsia (responders)
5.3. Analysis.

Comparison 5: Herbal medicine versus other agents, Outcome 3: Quality of life
5.4. Analysis.

Comparison 5: Herbal medicine versus other agents, Outcome 4: Adverse events
Studies at low risk of bias
Curcuma longa vs omeprazole
Two studies assessed the effect of this herbal medicine versus omeprazole. The first study included 22 participants (Puttapitakpong 2016). There was little to no difference in global symptoms (SMD ‐0.44, 95% CI ‐1.29 to 0.41). There was no information on adverse events or quality of life. The certainty of the evidence for this result is low due to the unclear risk of bias and imprecision. The second study included 88 participants (Yongwatana 2022). There was little to no difference between the interventions in terms of global symptoms of dyspepsia (SMD ‐0.36, 95% CI ‐0.78 to 0.06), quality of life (SMD 2.26, 95% CI ‐0.16 to 0.68), or adverse events (RR 1.43, 95% CI 0.56 to 3.69). The certainty of the evidence for this result is moderate due to imprecision. We did not combine the studies as it is not clear if the former is a preliminary report of the latter.
Studies at unclear risk of bias
Curcuma longa vs flatulence
Based on one study with 68 participants with FD (Thamlikitkul 1989), there was little to no difference between the interventions in terms of global symptoms of dyspepsia (RR 0.95, 95% CI 0.75 to 1.19). There was no information about adverse events or quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Peppermint oil/caraway oil vs cisapride
Based on one study with 118 participants (Madisch 1999), there was little to no difference between the interventions in terms of global symptoms of dyspepsia (SMD 0.11, 95% CI ‐0.25 to 0.47) and adverse events (RR 0.83, 95% CI 0.42 to 1.64). There was no information on quality of life. The certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
STW5 I‐II vs cisapride
Based on one study with 137 participants (Rosch 2002), there was little to no difference between the interventions in terms of global symptoms of dyspepsia (SMD ‐0.29, 95% CI ‐0.65 to 0.07) and adverse events (RR 0.55, 95% CI 0.29 to 1.03). There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
STW5 vs proton pump inhibitor
One study reported this comparison, including 57 participants (Holtmann 2013). There was little to no difference in terms of global symptoms (RR 0.88, 95% CI 0.57 to 1.35). There was no information on adverse events or quality of life. The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Trachyspermum ammi L, Anethum graveolens L, and Zataria multiflora Boiss herbal oils vs omeprazole
Based on one study with 57 participants (Bordbar 2020), this intervention may have a moderate effect on the improvement of global symptoms of dyspepsia compared to omeprazole (SMD ‐0.66, 95% CI ‐1.19 to ‐0.12). There were no differences in adverse events (RR 5.33, 95% CI 0.27 to 106.61). The intervention may have a large effect on the improvement of quality of life (SMD 0.86, 95% CI 0.33 to 1.39). The overall certainty of the evidence for these results is low due to the unclear risk of bias and imprecision.
Studies at high risk of bias
Apium graveolens and Trachyspermum copticom vs omeprazole
Based on one study with 100 participants (Azimi 2017), the effects on global symptoms of dyspepsia were not reported. There was little to no difference between interventions in terms of adverse events (RR 0.31, 95% CI 0.01 to 7.34) and quality of life (SMD ‐0.24, 95% CI ‐0.64 to 0.15). The certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Nigella sativa and omeprazole vs triple therapy
Based on one study with 88 participants with FD and H pylori infection (Salem 2010), there was little to no difference between the interventions in terms of global symptoms of dyspepsia (RR 1.06, 95% CI 0.76 to 1.49). There were no adverse events reported in control or intervention groups. There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Pudin hara (pearls vs liquid)
Based on one study with 79 participants (Sastry 2016), there were no differences between the interventions in terms of global symptoms of dyspepsia (SMD ‐0.25, 95% CI ‐0.69 to 0.20). There were no adverse events reported in control or intervention groups. There was no information on the quality of life. The overall certainty of the evidence for these results is low due to the high risk of bias and imprecision.
Discussion
Summary of main results
We included 41 trials with 4477 participants that compared 27 herbal medicines to placebo or other treatments. Most of the trials evaluated a single substance, with the exception of some on dual combinations (e.g. peppermint and caraway oil) and polyherbal products (STW5). This review evaluated global symptoms of functional dyspepsia, quality of life, and adverse events; however, some studies did not report these outcomes. The evidence for most interventions is of low to very low certainty since for each comparison, there was usually one small trial with unclear risk of bias.
STW5 (commercially known as Iberogast because one of the included herbs is Iberis amara L.) may reduce the effect on global symptoms of dyspepsia compared with placebo in one or two months. Besides, SWT5 may not be more effective than placebo in improving the quality of life, but only one small study evaluated this outcome. In terms of safety, adverse events may be similar when compared to placebo.
Peppermint and caraway oil probably result in a moderate to a large reduction in global symptoms of dyspepsia and improved quality of life compared to a simulated treatment at one month, and there may be little to no difference in the rate of adverse events between this intervention and the placebo.
Curcuma longa probably reduces global symptoms of dyspepsia and improves the quality of life compared to placebo at four weeks. There is probably little to no difference in the rate of adverse events between this intervention and placebo.
We found evidence that the following herbal medicines may improve symptoms of dyspepsia compared to placebo: Lafonesia pacari, Nigella sativa, artichoke, Boensenbergia rotunda, Pistacia lenticus, Enteroplant, Ferula asafoetida, ginger and artichoke, Glycyrrhiza glabra, OLNP‐ 06, red pepper, Cuadrania tricuspidata, jollab, Pimpinella anisum. The following may provide little to no difference compared to placebo: Mentha pulegium and cinnamon oil; moreover, Mentha longifolia may increase dyspeptic symptoms. Almost all the studies reported little to no difference in the rate of adverse events compared to placebo, except for red pepper, which may result in a higher risk of adverse events compared to placebo. With respect to the quality of life, most studies did not report this outcome.
Essential oils may provide superior relief of symptoms compared to omeprazole. Peppermint and caraway oil, STW5, Nigella sativa and Curcuma longa may provide little to no benefit compared to other treatments.
Overall completeness and applicability of evidence
Management guidelines for FD recommend using proton pump inhibitors or eradication of H pylori as the first treatment for dyspeptic symptoms. Tricyclic antidepressants are considered over prokinetics as the second line of treatment in the main guidelines (ACG 2017; UEG 2021), while prokinetics are regarded as such in others (KSNM 2020). Psychotherapy, weight loss, and changes in diet habits might also be used as part of treatment in selected patients. There is a lack of consensus on the role of herbal medicines in the treatment of FD, as current guidelines agree that herbal products require further research before implementing them as a routine treatment. Yet, it is mentioned as another resource of complementary treatment of this condition. However, treatment algorithms do not include herbal products (ACG 2017; KSNM 2020; UEG 2021). Furthermore, some guidelines do not endorse the effectiveness of this kind of treatment due to the low quality of evidence (UEG 2021).
The physiopathology of FD is multifactorial and not completely elucidated. H pylori infection, psychological stress, visceral hypersensitivity, impaired gastric accommodation, duodenal mucosal barrier dysfunction and delayed gastric emptying are just some components of this disease (Tack 2004; Komori 2019; Vanheel 2017). Along with this, the direct relation of symptoms with diet components is still unclear (Pesce 2020). Many herbal products included in this review do not possess a clearly elucidated mechanism of action related to FD that would be common to all people with this condition. Therefore, choosing which type of herbal medicine to use might be challenging due to the expected variable response to treatment, as with other more traditional pharmacological treatments.
Most comparisons in the included trials of this review were against placebo. We found few trials comparing herbal medicines with common treatments for FD, and their comparative effectiveness remains unknown. Five studies compared their products against proton pump inhibitors (Azimi 2017; Bordbar 2020; Holtmann 2013; Puttapitakpong 2016; Yongwatana 2022), two of them used T copticum and A graveolence as interventions (Azimi 2017; Bordbar 2020), while another two used Curcuma longa (Puttapitakpong 2016; Yongwatana 2022), and the remaining one used STW‐5 (Holtmann 2013). One more study used eradication therapy for H pylori as a comparison (Salem 2010). Two studies used cisapride as a comparator (Madisch 1999; Rosch 2002), a drug no longer used to treat FD. Moreover, for more than 30 herbal products predefined as possible treatments in this review, there is a lack of information, with no eligible trials for most of them: Angelica (Angelica archangelica), Bitter orange peel (Citrus aurantium), Blessed thistle (Cnicus benedictus), Bogbean (Menyanthes trifoliate) Boldo (Peumus boldus), Cardamom (Elettaria cardamomum), Centuary (Centaurium minu), Chicory (Cichorium intybus), Cinchona (Cinchona pubescens), Cinnamon (Cinnamomum verum), Cloves (Syzygium aromaticum), Coriander (Coriandrm sativum), Dandelion (Taraxacum officinale), Devil's claw (Harpagophytum procumbens), Elecampane (Inula helenium), Fenugreek (Trigonella foenum‐graecum), Galangal (Alpinia officinarium), Gentian (Gentiana lutea), Horsetail (Equisetum arvense), Haronga (Harungona madagascariensis), Horehound (Marrubium vulgare), Juniper (Juniper communis), Lemon balm (Melissa Officinalis), Meadowsweet (Filipendula ulmaria), Milk thistle (Silybum marianum), Mistletoe (Viscum album), Oregon grape (Mahonia aquifolium), Peach (Prumus persica), Radish (Raphanus sativus), Rosemary (Rosemarinus Officinalis), Sage (Salvia officinalis), Sandy everlasting (Helichrysum arenarium), St John's wort (Hypericum perforatum), Thyme (Thymus vulgaris), Wormwood (Artemisia absinthium), Yarrow (Achillea millefolium).
Reporting deficiencies may limit the applicability of the findings of this review. Many studies did not define their population precisely with FD, and the use of Rome criteria was often missing (Bortolotti 2002; Da Mota Menezes 2006; Madisch 2001a; May 2000; Puttapitakpong 2016; Rafieian‐Kopaei 2005; Salem 2010; Sastry 2016; Thamlikitkul 1989). Moreover, these studies did not include people with comorbid functional disorders, including irritable bowel syndrome, common in people with FD. Seventeen studies did not assess the presence of H pylori, and the trials which included this information did not always report which method was used for the diagnosis (Babaeian 2017; Braden 2009; Da Mota Menezes 2006; Giacosa 2015; Khonche 2017; Rosch 2002; Von Arnim 2007). Finally, many studies failed to report key outcomes relevant to this review. Six studies did not report global symptoms of dyspepsia (Alizadeh‐Naini 2020; Azimi 2017; Eftekharafzali 2018; Hu 2011; Kupcinskas 2008; Rafieian‐Kopaei 2005). Quality of life was only measured in a useful way in 13 studies (Alizadeh‐Naini 2020; Allan 2012; Babaeian 2017; Ghoshegir 2015; Holtmann 2003; Holtmann 2013; Khonche 2017; Kupcinskas 2008; Mala 2018; Mohtashami 2015; Rich 2017; Sun 2016; Yongwatana 2022). Five studies did not assess adverse events (Holtmann 2013; Hu 2011; Puttapitakpong 2016; Rafieian‐Kopaei 2005; Yongwatana 2022).
Quality of the evidence
Limitations in study design and implementation
We found few randomized controlled trials for each comparison and few head‐to‐head comparisons. In addition, most studies had an unclear risk of bias due to inadequate reporting of their methods and analysis plan.
Indirectness of the evidence
Many studies did not specify Rome criteria for defining functional dyspepsia, and they were heterogeneous in the degree of investigation of the possible underlying causes of dyspepsia. Moreover, the presence of H pylori was not systematically assessed in many studies. We decided not to downgrade the certainty of the evidence since this does not imply that the underlying causes of dyspepsia were different across the included studies.
Inconsistency of the results
We found unexplained inconsistency in one of our meta‐analyses of STW5 (Iberogast), but in most cases, we only had one trial per comparison, and inconsistency could not be assessed.
Imprecision of the results
Many studies were underpowered to provide precise effect estimates of symptom scores due to a small sample size or high within‐study variance. Moreover, studies assessing the improvement of gastrointestinal symptoms as a dichotomous outcome sometimes also yielded wide confidence intervals. The reporting of adverse events was inconsistent across studies, and all studies were probably underpowered to detect and analyze adverse events.
Publication bias
We included mostly one study per comparison and few studies in meta‐analyses, which prevented us from assessing publication bias using funnel plots. In addition, we identified ongoing trials and trials with unknown status which could have been completed, contributing to publication bias.
Potential biases in the review process
Our search was designed to retrieve a broad spectrum of phytotherapeutic agents for dyspepsia and did not include specific names of herbal products (e.g. artichoke, ginger, peppermint oil) or variations on terms for dyspepsia (e.g. Abdominal Pain/, Heartburn/, upset stomach, stomach upset, abdominal discomfort, abdominal pain, stomach pain, stomach ache, stomachache). Incorporating such terms in future updates will increase the sensitivity of our search. Moreover, the truncation of some terms to retrieve the plural form (phytopharmaceutical/phytopharmaceuticals) may further improve the yield of our search. In addition, we could not retrieve several full‐text articles that might include eligible trials, and we listed them under Characteristics of studies awaiting classification. We also intended to perform quantitative synthesis for most comparisons; however, most of them only included one trial, so we modified our initial protocol and used newer methods, including effect direction plots to summarize the results. Finally, we could not perform subgroup and sensitivity analyses due to the few studies in each comparison. In future updates of this review, we expect to gather data from studies with a clearer definition of the inclusion criteria for functional dyspepsia to perform our sensitivity analyses.
Agreements and disagreements with other studies or reviews
A comprehensive review of alternative therapies included six trials that were also included in our review, with similar results in terms of improvements of symptoms with Curcuma longa, ginger, artichoke, Mentha piperita, caraway oil and STW5 (iberogast) (Chiarioni 2018). This review also included another pilot trial comparing dried banana powder in 46 people suffering from non‐ulcer dyspepsia, with positive results compared to placebo, and an additional trial of STW‐5, for which we could not retrieve the full text.
A systematic analysis of evidence evaluated different herbal preparation of iberogast (STW5, STW5 II, STW5 S, STW6) compared with cisapride and placebo in people with functional dyspepsia (Holtmann 2004). This analysis, led by one of the authors of the trials included in the present review, reached similar results in terms of the effectiveness of iberogast; however, it included observational studies and studies on participants with irritable bowel syndrome. These findings were similar to previous reviews (Saller 2002; Melzer J 2004).
A review of herbal medicinal products for non‐ulcer dyspepsia included several studies also present in our review, with similar results (Thompson 2002); however, this review also included a randomized clinical trial of caraway oil versus placebo in people with FD or irritable bowel syndrome, and another two controlled trials of a mix of fennel, caraway oil, and peppermint oil versus metoclopramide for functional upper abdominal disorders.
A review of potato‐derived products by Vlachojannis 2010 included two observational studies with promising results of raw potato juice on dyspeptic symptoms, although no diagnosis of functional dyspepsia was made. We could not include any of these studies in our review since they did not meet our criteria for study design. A review regarding the use of ginger in gastrointestinal disorders by Bodagh 2018 included the same studies that this review found, and reported similar results in improving symptoms.
Authors' conclusions
Implications for practice.
We identified multiple herbal medicines that may be effective in improving symptoms of dyspepsia compared to placebo. Some herbal products also indicated an improvement in quality of life, but this outcome was inconsistently reported. Moreover, these interventions may not be associated with important adverse events. However, the certainty of the evidence for most comparisons was low to very low. In addition, we found little evidence on the effectiveness and safety of these interventions compared to other treatments for functional dyspepsia, including proton pump inhibitors. Considering the lack of highly effective treatments for this condition and the evidence from this review, people with functional dyspepsia can discuss the role of herbal medicines with their healthcare provider through shared‐decision making.
Implications for research.
Future placebo‐controlled trials should adequately report their predefined protocols and statistical plans, and achieve a sample size that would provide a precise estimate of the effect of these interventions. More research is needed with a focus on participants fulfilling strict diagnostic criteria for functional dyspepsia and participants with common gastrointestinal comorbidities. Finally, the effect of herbal medicines may need to be compared to common medical treatments for functional dyspepsia to assess their relative effectiveness.
What's new
| Date | Event | Description |
|---|---|---|
| 19 July 2023 | Amended | Typo in Plain Language Summary corrected |
History
Protocol first published: Issue 4, 2019 Review first published: Issue 6, 2023
Acknowledgements
We acknowledge the help and support of the Cochrane Gut Review Group. The authors would also like to thank the following editors and peer referees who provided comments to improve the protocol: Sarah Rhodes (Editor), Claudio AR Gomes Junior, Marilyn Walsh, and Lisa Winer for copy‐editing the protocol. We also thank Kachonsak Yongwatana for the information provided on his trial.
The authors would like to thank the following editors and peer referees who provided feedback to improve the review: Paul Moayyedi (Sign‐off Editor, McMaster University), Anne‐Marie Stephani (Managing Editor, Cochrane Central Editorial Service), Lisa Wydrzynski (Editorial Assistant Cochrane Central Editorial Service), Robin Featherstone (Information Specialist, Cochrane Central Editorial Service), Andrew Bäck (Statistical Editor, Cochrane), and Andrea Takeda (Copy‐Editor, Cochrane Central Production Service).
The methods section of this review was based on a standard template used by the Cochrane Upper Gastrointestinal and Pancreatic Diseases Review Group and the methods used in two other reviews on the same topic (Pinto 2017; Pittayanon 2018).
The authors would like to thank Virginia Garrote for reviewing the search strategy for MEDLINE in the protocol stage and the authors of the protocol that were not involved in the review stage: Valeria Vietto, Iara Alonso, and Débora Szeinman. In addition, we would like to thank Camila Micaela Escobar Liquitay for designing and running the search in LILACS.
The search strategies were designed and run by Yuhong Yuan (Information Specialist at the Cochrane Gut Group).
Appendices
Appendix 1. Rome diagnostic criteria
| Functional dyspepsia |
Rome I (Talley 1991) |
Rome II (Talley 1999) |
Rome III (Tack 2006) |
Rome IV (Stanghellini 2016) |
| Main criteria | Pain or discomfort centered in the upper abdomen with no evidence of organic disease | Persistent or recurrent symptoms (pain or discomfort centered in the upper abdomen) AND No evidence that dyspepsia is exclusively relieved by defecation or associated with the onset of a change in stool frequency or stool form (exclude irritable bowel syndrome and exclude reflux) |
≥ 1 symptoms need to be present: • Bothersome postprandial fullness • Early satiation • Epigastric pain • Epigastric burning AND No evidence of structural disease, including the use of upper endoscopy, that is likely to explain the symptoms. Criteria should be fulfilled for at least 3 months with symptom onset at least 6 months previously. |
≥ 1 symptoms need to be present: • Bothersome postprandial fullness • Bothersome early satiation • Bothersome epigastric pain • Bothersome epigastric burning AND No evidence of structural disease, including the use of upper endoscopy, that is likely to explain the symptoms. Must fulfill criteria for a) postprandial distress syndrome or b) epigastric pain syndrome, or both. Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis. |
Appendix 2. CENTRAL search strategy
exp Dyspepsia/
(dyspep* or "NUD" or "FD").tw,kw.
(indigestion* or indigestive).tw,kw.
or/1‐3
exp plant preparations/
exp Plants, Medicinal/
exp phytotherapy/
exp Herbal Medicine/
exp Beverages/
(plant or plants or flower* or seeds or seed or tea or teas or tree or trees or phytotherap* or phyto‐therap* or beverage* or oil* or extract* or phytopharmaceutical or phyto‐pharmaceutical).tw,kw.
(herbal or herbals or herb or herbs).tw,kw.
or/5‐11
4 and 12
Appendix 3. MEDLINE search strategy
exp Dyspepsia/
(dyspep* or "NUD" or "FD").tw,kw.
(indigestion* or indigestive).tw,kw.
or/1‐3
exp plant preparations/
exp Plants, Medicinal/
exp phytotherapy/
exp Herbal Medicine/
exp Beverages/
(plant or plants or flower* or seeds or seed or tea or teas or tree or trees or phytotherap* or phyto‐therap* or beverage* or oil* or extract* or phytopharmaceutical or phyto‐pharmaceutical).tw,kw.
(herbal or herbals or herb or herbs).tw,kw.
or/5‐11
4 and 12
randomized controlled trial.pt.
controlled clinical trial.pt.
random*.ab.
placebo.ab.
drug therapy.fs.
trial.ab.
groups.ab.
or/14‐20
exp animals/ not humans.sh.
21 not 22
13 and 23
Note: Line 14‐23 RCT filter: “Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE: sensitivity‐maximizing version (2008 revision); Ovid format”. We made the following minor revision: we used “random*.ab.” instead of “randomized.ab” or “randomly.ab.” to capture word variations such as “randomised, randomization, random”.
Appendix 4. Embase search strategy
exp dyspepsia/
(dyspep* or "NUD" or "FD").tw,kw.
(indigestion* or indigestive).tw,kw.
or/1‐3
exp herbal medicine/
exp plant medicinal product/
exp phytotherapy/
exp beverage/
(plant or plants or flower* or seeds or seed or tea or teas or tree or trees or phytotherap* or phyto‐therap* or beverage* or oil* or extract* or phytopharmaceutical or phyto‐pharmaceutical).tw,kw.
(herbal or herbals or herb or herbs).tw,kw.
or/5‐10
4 and 11
random:.tw.
placebo:.mp.
double‐blind:.tw.
or/13‐15
exp animal/ not human/
16 not 17
12 and 18
Note: Lines #13‐16, Hedge Best balance of sensitivity and specificity filter for identifying"therapy studies" in Embase. hiru.mcmaster.ca/hiru/HIRU_Hedges_EMBASE_Strategies.aspx
Appendix 5. AMED search strategy
exp Dyspepsia/
(dyspep* or "NUD" or "FD").tw.
(indigestion* or indigestive).tw.
or/1‐3
exp Plants, Medicinal/
exp phytotherapy/
exp Beverages/
(plant or plants or flower* or seeds or seed or tea or teas or tree or trees or phytotherap* or phyto‐therap* or beverage* or oil* or extract* or phytopharmaceutical or phyto‐pharmaceutical).tw.
(herbal or herbals or herb or herbs).tw.
or/5‐9
4 and 10
Appendix 6. LILACS search strategy
(Dyspepsia OR dispepsia OR dyspep* OR dispep* OR "NUD" OR "FD" OR indigestion* OR indigestive) AND (plant preparation* OR “Preparaciones de Plantas” OR Preparações de Plantas OR Medicinal plant* OR Plantas Medicinales OR Plantas Medicinais OR Phytotherapy OR Fitoterapia OR Herbal Medicine OR Medicina de Hierbas OR Medicina Herbária OR Beverages OR plant* OR flor* OR seed* OR semilla* OR tea* OR te OR tree* OR oil* OR extract* OR phytopharmaceutical OR phyto‐pharmaceutical OR aceite* OR árbol OR óleo OR árvore OR chá)
Data and analyses
Comparison 1. STW5 versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Global symptoms of dyspepsia (continuous) | 5 | 814 | Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐4.39, ‐0.90] |
| 1.2 Global symptoms of dyspepsia (responders) | 2 | 324 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.98, 2.47] |
| 1.3 Adverse events | 4 | 786 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.52, 1.64] |
Comparison 2. Peppermint and caraway oil versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Global symptoms of dyspepsia (continuous) | 2 | 210 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.87 [‐1.15, ‐0.58] |
| 2.2 Global symptoms of dyspepsia (responders) | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [1.30, 1.81] |
| 2.3 Adverse events | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.69, 3.53] |
| 2.4 Quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. Curcuma longa versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Global symptoms of dyspepsia (continuous) | 2 | 110 | Mean Difference (IV, Random, 95% CI) | ‐3.33 [‐5.84, ‐0.81] |
| 3.2 Global symptoms of dyspepsia (responders) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.3 Adverse events | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.4 Quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 4. Herbal medicines versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Global symptoms of dyspepsia (continuous) | 14 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.1 Mentha longifolia | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.2 Chios mastic gum | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.3 Artichoke | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.4 Mentha pulegium | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.5 Red pepper | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.6 Enteroplant | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.7 Jollab | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.8 Ferula asafoetida | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.9 Nigella sativa | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.10 Glycyrrhiza glabra (Gutcard) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.11 Boesenbergia rotunda (fingerroot) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.12 Pimpinella anisum | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.13 Cinnamon oil | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.14 Cudrania tricuspidata | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.2 Global symptoms of dyspepsia (responders) | 3 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.2.1 Lafoensia pacari | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.2.2 Ginger (Zingiber officinalis) and Artichoke (Cynara cardunculus) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.2.3 OLNP‐06 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.3 Quality of life | 8 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.1 Enteroplant | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.2 Artichoke | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.3 Mentha pulegium | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.4 Ferula asafoetida | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.5 Glycyrrhiza glabra (Gutcard) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.6 Apium graveolens and Trachyspermum copticom | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.7 Curcuma longa | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3.8 Cudrania tricuspidata | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.4 Adverse events | 22 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.4.1 Mentha pulegium | 1 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 4.4.2 Mentha longifolia | 1 | 88 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 15.49] |
| 4.4.3 Pistacia lentiscus (Chios mastic gum) | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 5.00 [0.24, 102.40] |
| 4.4.4 Glycyrrhiza glabra | 1 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 4.4.5 Artichoke | 1 | 244 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.84, 2.44] |
| 4.4.6 Pistacia atlantica | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.14, 6.53] |
| 4.4.7 Ferula asafoetida | 1 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 4.4.8 Jollab | 1 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 2.39 [0.48, 11.89] |
| 4.4.9 Fingerroot | 1 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.17, 3.24] |
| 4.4.10 Ginger and artichoke | 1 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 4.4.11 OLNP‐06 | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.15, 6.55] |
| 4.4.12 Pimpinella Anisum | 1 | 107 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.01, 5.17] |
| 4.4.13 Nigella sativa | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.53, 1.88] |
| 4.4.14 Red pepper | 1 | 27 | Risk Ratio (M‐H, Random, 95% CI) | 4.31 [1.56, 11.89] |
| 4.4.15 Lafoensia pacari | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.66, 3.49] |
| 4.4.16 Enteroplant | 1 | 198 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.09, 10.58] |
| 4.4.17 Apium Graveolence and Trachyspermum Copticum | 1 | 92 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 3.57] |
| 4.4.18 Astaxanthin | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.55, 2.74] |
| 4.4.19 Cinnamon oil | 1 | 51 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.14, 4.12] |
| 4.4.20 Cudrania tricuspidata | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.42, 1.53] |
| 4.4.21 Curcuma longa | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.51, 3.08] |
Comparison 5. Herbal medicine versus other agents.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Global symptoms of dyspepsia (continuous) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.1 Trachyspermum ammi L., Anethum graveolens L., and Zataria multiflora Boiss herbal oils vs omeprazole | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.2 Pudin hara pearls vs pudin hara liquid | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.3 STW5 vs cisapride | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.4 Peppermint oil/caraway oil vs cisapride | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.5 Curcuma longa vs omeprazole | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.2 Global symptoms of dyspepsia (responders) | 3 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.2.1 Curcuma longa vs flatulence | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.2.2 STW5 vs proton pump inhibitor | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.2.3 Nigella sativa and Omeprazol vs Triple therapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.3 Quality of life | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3.1 The Trachyspermum ammi L. (TA), Anethum graveolens L. (AG), and Zataria multiflora Boiss (ZM) herbal oils vs Omeprazole | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3.2 Apium graveolens and Trachyspermum copticom vs omeprazole | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3.3 Curcuma longa vs omeprazole | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.4 Adverse events | 6 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.4.1 Pepermint/caraway oil vs cisapride | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.4.2 STW5 I‐II vs Cisapride | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.4.3 The Trachyspermum ammi L. (TA), Anethum graveolens L. (AG), and Zataria multiflora Boiss (ZM) herbal oils vs Omeprazole | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.4.4 Pudin hara | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.4.5 Apium Graveolence and Trachyspermum Copticum vs omeprazole | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.4.6 Curcuma longa vs omeprazole | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alizadeh‐Naini 2020.
| Study characteristics | ||
| Methods |
Study design: randomized, double‐blind, placebo‐controlled clinical trial Study dates: 2017 to 2018 Setting and number of centres: outpatient, national Country: Iran |
|
| Participants |
Inclusion criteria: patients diagnosed with ROME III and with H pylori infection. Exclusion criteria: patients who had a history of gastric cancer or gastric surgery, active gastrointestinal bleeding and Intense gastritis, inflammatory and chronic diseases such as kidney and liver diseases, inflammatory bowel disease, heart ischaemia, diabetes mellitus, lung disease, asthma, cancer, HIV infection, and systemic inflammation, patients who were pregnant or lactating, those having body mass index greater than 30 kg/m2, taking any antibiotics or bismuth 6 weeks before the study, getting any medication for H pylori eradication prior to the onset of the study, drinking alcohol or using narcotics Sample size: 51 randomized Withdrawals Group 1: 2 were excluded because of their intolerance to quadruple therapy. Group 2: 3 were excluded, one who did not adhere to the study protocol, one who got out of reach, and one who was not willing to continue the study. Age (mean ± SD years) Group 1 (40.61 ± 2.15); Group 2 (40.12 ± 2.15) Ethnicity by group: not stated. Sex (M/F) Group 1 (Study); 10 M/16 F Group 2 (Control) 6 M/19 F Symptom severity at baseline: not available. |
|
| Interventions |
Group 1 (n = 26):N sativa powder 2 grs. 2 capsules twice daily 30 min after the meal Group 2 (n = 25): coloured pharmaceutical starch 2 grs. 2 capsules twice daily 30 min after the meal Co‐interventions: 500 mg metronidazole twice daily, 1000 mg amoxicillin twice daily, 240 mg bismuth subcitrate twice daily, and 40 mg omeprazole twice daily for 2 weeks. |
|
| Outcomes |
Adverse events How measured: by phone call Time points measured: every 7 days Time points reported: end of study Subgroups: no Quality of life How measured: Short‐ form 36 (SF‐36) Time points measured: at the beginning and at the end of 8 weeks of intervention. Time points reported: end of weeks 1, 2, and cumulative incidence of the remaining 6 weeks Subgroups: none Other outcomes reported in the review Global symptoms of dyspepsia were not measured. The study reported each symptom separately (using ROME III). Hs‐CRP serum levels, serum level of malondialdehyde (MDA), IL‐8 (pg/ml). |
|
| Funding | Financially supported (grant no #95‐01‐84‐13771) by the Vice Chancellery of Research and Technology in Shiraz University of Medical Sciences, Shiraz, I.R. Iran. | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "block randomization using random allocation software". |
| Allocation concealment (selection bias) | Low risk | “N. sativa and placebo capsules were completely similar in color, size, and smell to blind the participants, gastroenterology clinic staff, and the researcher to group allocation”. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “N. sativa and placebo capsules were completely similar in color, size, and smell to blind the participants, gastroenterology clinic staff, and the researcher to group allocation”. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “N. sativa and placebo capsules were completely similar in color, size, and smell to blind the participants, gastroenterology clinic staff, and the researcher to group allocation”. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of five withdrawals) for all results. |
| Selective reporting (reporting bias) | Low risk | All outcomes in the protocol (en.irct.ir/trial/27133) are reported in the study. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Allan 2012.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: December 2009 to March 2010 Setting and number of centres: inpatients in two centres Country: India |
|
| Participants |
Sample size: 50 Inclusion criteria: Rome‐III criteria Exclusion criteria: Age less than 18 years or over 65 years, advanced chronic illness that would impair follow‐up or monitoring, pregnancy or breastfeeding, previous surgery for ulcers, people with a previous history of gastroesophageal reflux, people with concomitant symptoms of the irritable bowel syndrome, drug and alcohol abuse, mental illness or dementia Withdrawals: none Age (mean ± SD years) Group 1 (Study); mean age 38.12 ± 1.84 Group 2 (Control) mean age of 45.16 ± 2.06 Ethnicity by group: not stated Sex (M/F) Group 1 (Study); 15 M/10 F Group 2 (Control) 16 M/9 F Symptom severity at baseline: total symptoms scores of dyspepsia Group1 (Study) 29.96 ± 0.55 Group 2 (Control) 28.68 ± 0.62 |
|
| Interventions |
Group 1 (n = 25 ): Glycyrrhiza glabra (GutGard) (75 mg twice daily) for 30 days after meals (morning and night) with a glass of water. GutGard has following phytochemical specifications, namely, glabridin (≥ 3.5% w/w), glabrol (≥ 0.5% w/w), eicosanyl caffeate (≥ 0.1% w/w), docosyl caffeate (≥ 0.1% w/w), glycyrrhizin (≤ 0.5% w/w), and total flavonoids (≥ 10% w/w). Group 2 (n = 25): placebo twice a day for 30 days Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: list of 10 gastrointestinal symptoms (7‐point Likert scale) Time points measured: baseline, after 15 days and after a month. Time points reported: baseline, after 15 days and after a month Subgroups: none Adverse events How measured: reported by participants when they attended the centre. Time points measured: Day 15 and 30 Time points reported: cumulative incidence Subgroups: none Quality of life How measured: Nepean Dyspepsia Index (NDI) Time points measured: Days 0, 15 and 30 Time points reported: Days 0, 15 and 30 Subgroups: none Other outcomes reported in the review: laboratory investigations |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A list of unique integer random numbers considered as patient code (i.e., random allocation sequence) was generated using a computer‐aided programme” “randomization sequence was developed at Natural Remedies Pvt. Ltd., Bangalore, India, and forwarded to study centre. The entire process was performed in a confidential manner and all the concerned in study centre namely, investigators, patients, and other supportive staff were unaware of the random allocation sequence” |
| Allocation concealment (selection bias) | Low risk | “As per the random allocation sequence, the containers (either placebo or GutGard capsules) were labeled with unique random numbers.” ‐ central allocation (pharmacy) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “The investigators, patients, and pharmacist dispensing the interventions were all concealed to group assignment. The blinding process was maintained till all the data were compiled and verified for accuracy and then forwarded for statistical analysis” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The investigators, patients, and pharmacist dispensing the interventions were all concealed to group assignment. The blinding process was maintained till all the data were compiled and verified for accuracy and then forwarded for statistical analysis” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data for every outcome were reported. No participant was lost. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | We did not identify other sources of bias. |
Azimi 2017.
| Study characteristics | ||
| Methods |
Study design: 3 arms ‐ RCT Study dates: 2015 to 2016 Setting and number of centres: outpatient, national, single centre Country: Iran |
|
| Participants |
Inclusion criteria: aged 18 to 60 years old, diagnosed according to ROME III criteria. Exclusion criteria: pregnancy, breastfeeding, convulsion, active urinary tract infection, any severe side effects possibly relating to the drug, simultaneous use of other chemical or herbal drugs related to symptoms of FD, intake anticoagulants, digestive ulcers or reflux, Irritable Bowel Syndrome (IBS), serious diseases like diabetes and cardiovascular diseases, oesophagus and gastrointestinal surgery, severe mental retardation, drug abuse, patient’s unwillingness to continue the project, not filling out the consent form, and the emergence of warning symptoms including sudden severe weight loss, anaemia, blood in the stool, dysphagia. Sample size: 150 randomized Withdrawals: 13 (group 1: after 2 weeks because not regularly using (1); group 2: because not regularly used (2), drug intolerance (1) and using other drugs (2); group 3: not regularly using (2), drug intolerance (2), using other drugs (2) and wanted to be pregnant (1)) Age (years): ages are expressed in age subgroups for each group. Group 1 (Study): 18 to 30 (15), 31 to 45 (23), and 46 to 60 (11); Group 2 (Placebo): 18 to 30 (12), 31 to 45 (19), and 46 to 60 (11) Group 3 (Omeprazol): 18 to 30 (16), 31 to 45 (18), and 46 to 60 (11). Ethnicity by group: not stated. Sex (M/F) Group 1 (Study); 16 M/32 F Group 2 (Placebo) 17 M/28 F Group 3 (Omepraol) 16 M/27 F Symptom severity at baseline: Stangellini’s symptom severity and ROME III. The symptom severity questionnaire includes 8 items with the final score ranging between 8 and 32. The symptom frequency questionnaire is comprised of 8 items with the final score ranging between 8 and 48. |
|
| Interventions |
Group 1 (n = 50): capsule with Apium graveolence (herbarium number of KF1447) 250 mg and Trachyspermum copticum 250 mg (herbarium number of KF1138), twice daily (after breakfast and another one after dinner) Group 2 (n = 50): capsule of omeprazole 20 mg before breakfast daily Group 3 (n=50): placebo cornstarch, 500 mg, twice daily (after breakfast and another one after dinner) Co‐interventions: none |
|
| Outcomes |
Adverse events How measured: questionnaire at follow‐up Time points measured: at baseline, 4 and 8 weeks Time points reported: at baseline, 4 and 8 weeks Subgroups: none Quality of life How measured: Nepean Dyspepsia Index (NDI) short questionnaire Time points measured: at baseline, 4 and 8 weeks Time points reported: at baseline, 4 and 8 weeks Subgroups: none Other outcomes reported in the review: Global symptoms of dyspepsia were not measured. The study reported each symptom separately (using Stangellini’s symptom severity and ROME III) measured at the baseline, 2, 4 and 8 weeks. |
|
| Funding | Non‐reported | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was performed by minimisation, in which 15 patients were divided into three intervention groups by randomizing the numbers 1, 2, and 3, and their multiples, to the subjects. The patients were then intentionally placed into these groups based on potential confounders, namely age and sex, to match these three groups with respect to the factors mentioned." There is no explanation on how data were handled nor the use of software. |
| Allocation concealment (selection bias) | Low risk | "Drugs were identically packaged and coded in the Pharmacognosy Department of Kerman University of Medical Sciences. The person who did the coding was not involved in the study." ‐ Central allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "This study was conducted in the double‐blinded" "The person who coded the drugs did not have any role until the end of the intervention. Without any knowledge of the study objectives, the second person divided the patients into the three groups purposefully based on each patient’s basic information" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The patient’s information was analyzed by a fourth person blind about grouping and drugs coding." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Unbalanced attrition: 7/50 in the placebo group, 1/50 in the herbal therapy group, 5/50 in the omeprazole group. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Babaeian 2017.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial. Study dates: not available. Setting and number of centres: single‐centre, outpatient. Country: Iran |
|
| Participants |
Inclusion criteria: age 18 to 65 years and a diagnosis of postprandial distress syndrome according to the ROME III criteria. Exclusion criteria: pregnancy, breastfeeding, peptic ulcer, gastroesophageal reflux disease, dysphagia, celiac sprue, gastrointestinal surgery, irritable bowel syndrome, abdominal pain, night diarrhoea, greasy or black stool, blood in stool, mental retardation, immune system disorders, severe recent weight loss, cancer, renal disorders, and the current need for or use of the following medications: antibiotics, proton pump inhibitors, H2 blockers, bismuth, metoclopramide, domperidone, lactulose, non‐steroidal anti‐inflammatory drugs, corticosteroids, and herbal medicines Sample size: 100 participants allocated equally to each group Withdrawals: 12 in total (4 because of the lack of regular use of the medication, this happened equally in both groups; 6 due to drug intolerance, 5 of them were in the intervention branch; and 2 due to adverse events, 1 in each branch; 1 participant of the placebo group was lost for other reasons). Age (mean ± SD years) Group 1 (43 ± 12.3); Group 2 (42.8 ± 14) Ethnicity by group: not stated Sex (M/F) Group 1 (Study); 10 M/40 F Group 2 (Control) 10 M/40 F Symptom severity at baseline: evaluated with the FD severity scale. All symptoms were distributed similarly between the two groups. Group 1: 13.9 ± 7.60 Group 2: 14.2 ± 7.23 No significant difference was seen in different symptoms of postprandial distress syndrome in the two groups (13.9 ± 7.60 vs. 14.2 ± 7.23, P = 0.84). |
|
| Interventions |
Group 1 (n = 50): 750 mg Mentha longifollia 3 times a day for 4 weeks (each pill contains 250 mg + 250 of cornstarch) Group 2 (n = 50): placebo 500 mg of cornstarch Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: validated scale using Likert rating (‐2 to +2). Range ‐32 to 32 (higher scores indicate fewer symptoms of discomfort/bloating/pain/fullness/burning, preprandial and postprandial nausea and epigastric pain, night epigastric pain, morning nausea, vomiting, retching, belching, loss of appetite, and early satiety were assessed) Time points measured: end of weeks 2, 4 and 12 Time points reported: end of weeks 2, 4 and 12 Subgroups: none Adverse events How measured: any side effects from their medications were recorded at each follow‐up. Time points measured: end of weeks 2, 4 and 12 Time points reported: cumulative incidence of events Subgroups: none Quality of life How measured: QOL was evaluated with Persian version of the Short Form‐36 (SF36) questionnaire (higher scores indicate better quality of life) Time points measured: baseline and end of week 12 Time points reported: baseline and end of week 12 Subgroups: none Other outcomes reported in the review: epigastric discomfort/bloating/pain/fullness/burning, preprandial and postprandial nausea and epigastric pain, night epigastric pain, morning nausea, vomiting, retching, belching, loss of appetite, and early satiety were assessed individually as well. |
|
| Funding | None | |
| Declaration of interest | The authors declare no conflicts of interest | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization and enrollment of the patients in the MLE and placebo groups were done by the gastroenterologist equally and alternatively using permuted random blocks with a block size of two” |
| Allocation concealment (selection bias) | Low risk | “The MLE and placebo were packaged and alphabetically labeled with the same appearance. An independent pharmacist set the codes on the drug or placebo packets using a confidential list that contained the secret codes and was kept in sealed, opaque envelopes until the end of the study and until they were needed.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “The current study was a double‐blind, randomized clinical trial study. The gastroenterologist, patients, and outcome assessor were not informed which participants had received the drug and which had been given the placebo” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The gastroenterologist, patients, and outcome assessor were not informed which participants had received the drug and which had been given the placebo.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data for every outcome were reported. 12/100 patients were excluded (six in each group, balanced attrition). |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No other sources of bias were identified. |
Bordbar 2020.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized controlled trial Study dates: 2017 to 2018 Setting and number of centres: outpatient, national Country: Iran |
|
| Participants |
Inclusion criteria: diagnosed with FD based on the ROME III criteria as the presence of postprandial distress syndrome (PDS) (including postprandial fullness or early satiation) and epigastric pain syndrome (EPS) (including epigastric pain, or epigastric burning), for 3 months in the past 6 months; and dyspepsia symptoms with scores of 6 or higher on the 11‐point Numerical Rating Scale (NRS) for more than 4 of the 14 days prior to registration. Exclusion criteria: lack of consent to continue the study; taking antibiotics or nonsteroid anti‐inflammatory drugs two weeks before the study; gastroesophageal reflux disease (heartburn, acid regurgitation); drug or alcohol abuse; the presence of gastroesophageal malignancy, chronic digestive diseases, and peptic ulcer disease based on history, physical examination, laboratory tests (e.g. white blood cell count, C reactive protein (CRP) or erythrocyte sedimentation rate (ESR)), and upper endoscopy; liver and kidney dysfunction based on laboratory tests; planned or current pregnancy; the history of a severe allergic reaction to medicinal plants; the history of upper gastrointestinal tract surgery; and serious illnesses like heart failure, diabetes and epilepsy, and previous or current significant psychiatric comorbidity. Sample size: 64 randomized participants Withdrawals Group 1: excluded study (n = 3): because of lack of co‐operation Group 2: excluded study (n = 1): because of lack of co‐operation Age (mean ± SD years): Group 1: (32.5 ± 10.2); Group 2: (34.5 ± 9.3) Ethnicity by group: not stated Sex (M/F) Group 1 (Study); 13 M/19 F Group 2 (Control) 12 M/20 F Symptom severity at baseline: Gastrointestinal Symptom Rating Scale (GSRS). The questions on this questionnaire are scored on a 7‐point Likert scale, ranging from “No discomfort at all” (0) to “Very severe discomfort”. Group 1: 44.5 ± 7.4 Group 2: 42.3 ± 7 |
|
| Interventions |
Group 1 (n = 32): 250 mg soft‐gel capsules containing pure essential oils of Zataria multiflora Boiss (28.8%), Anethum graveolens L. (21.6%), and Trachyspermum ammi (21.6%), and sunflower oil (28%) as an excipient twice a day for 2 weeks. Group 2 (n = 32): 20 mg omeprazole capsule once a day for 2 weeks Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: GSRS Time points measured: baseline, week 2 and 4 Time points reported: baseline, week 2 and 4 Subgroups: none Adverse events How measured: not mentioned Time points measured: end of study Time points reported: end of study Subgroups: none Quality of life How measured: 36‐ Item Short‐Form Health Survey (SF‐36). Time points measured: baseline, week 2 and 4 Time points reported: baseline, week 2 and 4 Subgroups: none Other outcomes reported in the review: laboratory tests (serum alanine aminotransferases and aspartate aminotransferases, alkaline phosphatase, total and direct bilirubin, random blood sugar, blood urea nitrogen, and creatinine) |
|
| Funding | This study was funded by the Hormozgan Province Science & Technology Park with grant number 93/3/1986. | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was done by using a random allocation software software‐generated list and in a 1:1 ratio" |
| Allocation concealment (selection bias) | Low risk | “the randomization and medicine administration was done by someone other than the investigators. The medicines were put in similar cans, and the code of the medicinal regimen was labeled on each can” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “The code of medicine given to each patient and their clinical symptoms was recorded on the treatment of the evaluator’s personal information form (a trained medical student). The investigators, patients, and treatment assessors were not aware of the medicine regimens type” “aromatized sunflower oil soft‐gel capsules twice a day and starch hard gel capsules once a day in the same shape, size, and color as placebo were given to control and intervention arms, respectively” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The code of medicine given to each patient and their clinical symptoms was recorded on the treatment of the evaluator’s personal information form (a trained medical student). The investigators, patients, and treatment assessors were not aware of the medicine regimens type” “aromatized sunflower oil soft‐gel capsules twice a day and starch hard gel capsules once a day in the same shape, size, and color as placebo were given to control and intervention arms, respectively” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of three withdrawals) for all results. Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Bortolotti 2002.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial. Study dates: Study dates not available Setting and number of centres: outpatient, single‐centre, national Country: Italy |
|
| Participants |
Inclusion criteria: Patients aged 18‐ 65 years were eligible. Presenting with persistent or recurrent pain or discomfort centred in the upper abdomen associated with food intake, which compelled the patients to require medical consultation. This included symptoms such as a feeling of post‐prandial epigastric fullness, upper abdominal bloating without visible distension, epigastric burning, burping–belching, early satiety, nausea or vomiting. The persistence of symptoms was for at least 3 months before the study and their occurrence at least three times a week. Absence of other functional gut disorders, such as gastro‐oesophageal reflux disease (excluded based on symptoms and, in some dubious cases, by 24‐h pH‐metry), irritable bowel syndrome (diagnosed based on Manning’s criteria) and biliary motility disorders (selected based on symptoms and ultrasonography). Exclusion criteria: (i) organic alterations of the gut, such as hiatal hernia, oesophagitis, duodenitis, ulcers, erosions, stenosis, neoplasms, gallstones, etc.; (ii) previous surgery of the digestive tract (excluding appendectomy); (iii) history of gastric or duodenal ulcer; (iv) hepatic, cardiac, renal, neurological and systemic diseases, in which involvement of the digestive tract was possible (diabetes, scleroderma, etc.); (v) pregnancy and lactation; (vi) alcohol intake > 20 g ⁄ day; (vii) coffee intake > 3 cups/day; (viii) smoking > 10 cigarettes/day; (ix) drug addiction; (x) chronic use of NSAIDs and other ulcerogenic drugs, as well as drugs which may interfere with gut motility. Sample size: 30 enrolled participants Withdrawals: 2 (of the appearance of severe epigastric pain or burning after the first administration of red pepper). Loss to follow‐up: 1 (patient in the placebo group did not complete the trial) Age (years ): Group 1 (40.2 range, 19–63); Group 2 (43.3 range, 21–58) Ethnicity by group: not stated. Sex (M/F): Group 1 (Study); 7 M/8 F Group 2 (Control) 8 M/7 F Symptom severity at baseline: Epigastric pain, epigastric fullness, epigastric burning, epigastric swelling, belching‐belching, early satiety, nausea and/or vomiting. Their intensity was scored based on the five‐point Likert scale (1, absent; 2, mild, can be ignored when not thinking about it; 3, moderate, cannot be ignored, but does not influence daily activities; 4, strong, influences concentration in daily activities; 5, unbearable, greatly influences in daily activities and/or requires rest). The higher the score, the greater the symptoms. This scale was validated for dyspeptic symptoms according to previous studies. Overall symptoms intensity: Group 1: 3.31 ± 0.64 Group 2: 3.44 ± 0.72 |
|
| Interventions |
Group 1 (n =14): Intervention. Red pepper capsule (administered in opaque gelatine capsules, each containing 500 mg, the content of pure capsaicin and hydrocapsaicin was 0.7 mg ⁄ g of red pepper powder. one capsule before breakfast (continental), two before lunch and two before dinner for 5 weeks (5 capsules by day). Group 2 (n = 13): Placebo. Administered in opaque gelatine capsules, each containing 500 mg of tomato powder. one capsule before breakfast (continental), two before lunch and two before dinner for 5 weeks (5 capsules by day). Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: List of symptoms (7) based on a 5‐point Likert scale. Time points measured: Daily. Time points reported: The averages of the scores were reported daily scores. Subgroups: none Adverse events How measured: based on spontaneous complaints reported in the diary or on the answer to specific questions at the final visit. Time points measured: at complete follow‐up. Time points reported: narratively. Subgroups: none. Other outcomes reported in the review: none. |
|
| Funding | Not available | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomization of the participants is not explicitly stated. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment is not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The study mentions that it is double‐blind and that "The study was carried out by an investigator who did not know the meaning of the variations in symptoms after the administration of capsaicin and placebo"; however, it is not specified if the study personnel was blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants were blinded (patient‐reported outcomes). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of three withdrawals) for all results. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | No other sources of bias were detected. |
Braden 2009.
| Study characteristics | ||
| Methods |
Study design: parallel‐group placebo‐controlled Study dates: not available Setting and number of centres: outpatient, multicentre, national Country: Germany |
|
| Participants |
Inclusion criteria: aged 18 to 85 years, diagnosed with FD according to the Rome II criteria, 3 or more items on a GIS Profile had to be judged at least moderate (grade 2), determination of the status of H pylori. Exclusion criteria: people with endoscopically proven oesophageal erosions, Barrett’s, oesophagus, gastroduodenal ulcers or erosions (have had to be ruled out by an abdominal ultrasound examination and an oesophagogastroduodenoscopy within the preceding 3 months), diabetes mellitus, a history of abdominal surgery (apart from appendectomy and cholecystectomy) or predominant gastro‐oesophageal reflux disease were not eligible for the study. Sample size: 103 participants enrolled: 93 randomized, 86 in results (7 participants unclear) Withdrawals: withdrawals of consent (n = 6) new intercurrent diseases (n = 2), a violation of in‐/exclusion criteria (n = 1) or for other reasons (n = 1) Age (mean ± SD years): Group 1 (45.9 ± 15.2); Group 2 (48.6 ± 17.3) Ethnicity by group: not available. Sex (M/F): Group 1 (Study); 10 M/16 F Group 2 (Control) 6 M/19 F Group 1 (14 (31.8%)); Group 2 (12 (28.6%)) Symptom severity at baseline: Gastrointestinal symptoms score (GIS). Each symptom was graded on a validated five‐point Likert scale, ranging from 0 (no problem) to 4 (very severe problem, markedly influencing daily activities or requiring rest). Max score: 40 points, minimum for inclusion greater than or equal to 6 points. Group 1: 11.6 ± 4.4 Group 2: 12.0 ± 4.7 |
|
| Interventions |
Group 1 (n = 44 ): Intervention. STW 5 tincture 20 drops 3 times a day for 28 days Group 2 (n = 42 ): Placebo. Liquid placebo 20 drops 3 times a day for 28 days. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Gastrointestinal symptoms score (GIS) Time points measured: Start of treatment (visit 2) and end of treatment (visit 3) Time points reported: Total score start of treatment (visit 2) and end of treatment (visit 3) Subgroups: none Adverse events How measured: Cumulative incidence Time points measured: At complete follow‐up Time points reported: Narratively Subgroups: none Other outcomes reported in the review: 13C octanoic acid breath test (13C‐OBT) for the assessment of gastric emptying, Infection with H. pylori, laboratory parameters and global assessment of efficacy. |
|
| Funding | Not available | |
| Declaration of interest | Dr Vinson is an employee of the Steigerwald Arzneimittelwerk GmbH, Darmstadt, Germany. The other authors (B.B., W.C., N.B., A.S.) do not have conflicts of interest to declare. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method used to generate the random sequence is not described |
| Allocation concealment (selection bias) | Unclear risk | The methods for allocation concealment are not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | It was only mentioned in the article that it was double blind. It is unclear whether personnel was blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded by the use of placebo (patient‐reported outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Seven participants were not included in the analysis (7/93) without explaining the reasons for withdrawal. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Chey 2019.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial. Study dates: not available. Setting and number of centres: outpatient, multicentric (7 sites). Country: USA |
|
| Participants |
Inclusion criteria: 18 to 65 years, diagnosed with Rome III and present at least moderate symptoms in the Global Overall Symptom (GOS) (at least 4 points in the epigastric pain syndrome (EPS) or postprandial distress syndrome (PDS) (postprandial fullness) question) in at least 4 days of the screening period (14 days). Exclusion criteria: evidence of structural disease that explains symptoms (as verified by a normal upper endoscopy performed within the past 36 months) test positive for H pylori by blood antibody test during the screening period or the previous 12 months. Sample size: 100 randomized; 95 finally randomized (in results) Withdrawals: 5 (intervention: 2; placebo: 3: causes are not explained) Age ((mean ± SD years) Group 1 (43.7± 11.33) Group 2 (43.1 ±12.90) Ethnicity by group (race): Asian (group 1 (3) group 2 (1)), Black or African‐American (group 1(11) group 2 (9)), White (group 1 (36) group 2 (35)). Sex (M/F): Group 1 (Study): 11M/39F; Group 2 (Control): 12M/33F Symptom severity at baseline: GOS Participants rate the overall severity of their symptoms from 1 (no problem) to 7 (a very serious problem that cannot be ignored and severely limits daily activities and often requires rest) on a Likert scale. PDS symptoms Group 1: 4.5 Group 2: 4.4 EPS symptoms Group 1: 4.4 Group 2: 4.4 |
|
| Interventions |
Group 1 (n = 52): intervention. Capsules containing 25 mg of caraway oil and 20.75 mg of L‐menthol (the key active ingredient and equivalent to 50 mg of peppermint oil) (COLM) using microsphere‐based Site‐Specific Targeting (SST) microsphere delivery system, with an average particle size of approximately 1 mm (Active microspheres in the COLM‐SST capsules contained 60% fibre). 2 capsules in the morning and 2 capsules at dinner time, 30 to 60 minutes before a meal for 4 weeks. Group 2 (n =48): placebo capsules contained microspheres of the same size (1.2 mm in diameter) and density. (The placebo microspheres in the capsules contained 100% fibre). 2 capsules in the morning and 2 capsules at dinner time, 30 to 60 minutes before a meal for 4 weeks. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: physician‐reported symptom improvement per clinical global impression (CGI) (item 2) at day 28. Time points measured: Day 28 Time points reported: Day 28 Subgroups: none Adverse events How measured: following of treatment Time points measured: 1, 3, 14, and 28 days. Time points reported: cumulative incidence. Subgroups: none Quality of life How measured: none Time points measured: none Time points reported: none Subgroups: none Other outcomes reported in the review: the study reported symptoms divided into 2 subgroups: postprandial distress syndrome (PDS) and epigastric pain syndrome (EPS) by Global Overall Symptom (GOS) measured 2,14 and 28 days. |
|
| Funding | Funded by IM Health Science, LLC | |
| Declaration of interest | The authors perform various services (consultant, Chief Medical Advisor, Director of Product Development and Technical Operations and Chief Innovation Officer) of the company that financed the RCT. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The article indicates that they were randomized; however, it is not indicated how this was carried out. |
| Allocation concealment (selection bias) | Unclear risk | "Subjects were randomized 1: 1 to either COLM‐SST or placebo using concealed allocation." It is not indicated how this was carried out. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "The microspheres of the active and matching placebo were encapsulated and blister packaged to prevent patients from distinguishing active therapy from placebo by detecting the odor of L‐menthol or caraway oil." It is unclear whether personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The blinding of the outcome assessment was not mentioned: "The investigators completed their own assessment of the subjects’ improvement." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of five withdrawals) for all results. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Chitapanarux 2020.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: August 2017 to July 2019. Setting and number of centres: 1 centre, outpatients, national Country: Thailand |
|
| Participants |
Inclusion criteria: Rome IV for FD Exclusion criteria: pregnancy, breastfeeding, a history of malignancy or gastrointestinal tract surgery, irritable bowel syndrome, severe medical conditions such as heart, kidney, liver diseases, poorly controlled diabetes, psychological disorders, and alcohol/substance abuse. Participants were not allowed to be treated with PPIs, H2‐receptor antagonists, antacids, prokinetics, antidepressant drugs, tranquillizers, anticholinergic agents, cholinergic agents, or nonsteroidal anti‐inflammatory drugs within one week. Upper endoscopic examination was performed within 7 days before starting the study. During endoscopy, biopsy specimens were obtained for a rapid urease test and histologic examination. Sample size: 160 Withdrawals: 22 Control group: 2 participants desire to withdraw, 5 discontinue study medication, 3 noncompliance Control group: 6 participants desire to withdraw, 4 discontinue study medication, 2 noncompliance Age (mean + SD years): Group 1 (Study group): 57.65 ± 13.69; Group 2 (Control group): 56.14 ± 15.91 Ethnicity by group: not reported Sex (M/F): Group 1 (Study group): 32M/48F; Group 2 (Control group): 30M/50F Symptom severity at baseline: Short‐Form Leeds Dyspepsia Questionnaire (SF‐LDQ) scores Group 1 (Study) Summed total score 16.05 ± 3.17 Summed frequency score 10.2 ± 2.11 Summed severity score 5.85 ± 1.61 Group 2 (Control) Summed total score 15.13 ± 2.87 Summed frequency score 10.18 ± 2.19 Summed severity score 4.95 ± 1.11 |
|
| Interventions |
Group 1 (n = 80): fingerroot extract powder. 350 mg of powder orally 3 times a day. Boesenbergia rotunda. The total flavonoid content (alpinetin, pinostrobin, 5,7‐dihydroxyflavone, and 5,7‐dimethoxyflavone) measured by the modified colourimetric method was 150 mg quercetin equivalent per gram of dry weight. Group 2 (n = 80): placebo 350 mg orally in powder 3 times a day. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: SF‐LDQ, an item‐based questionnaire that was developed to quantify symptom severity and frequency during or at the end of a trial. It contained 4 questions (indigestion, heartburn, regurgitation, and nausea) which had the greatest validity to diagnose dyspepsia. Categorized scores were calculated by rating the single most frequent or severe symptom from 0 points (not at all) to 4 points (once a day or more). Time points measured: baseline, day 14 and day 28 Time points reported: baseline, day 14 and day 28 Subgroups: none Adverse events How measured: inquired at each visit, with laboratories, and self‐reported by telephone Time points measured: day 0 to 28 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: secondary endpoints were the rate of complete relief (categorized scores of 1 for all dyspeptic symptoms), the rate of satisfactory relief (scores of > 2 for all symptoms) of symptoms, the reduction of blood inflammatory markers (procalcitonin, ESR, CRP, and WBC count) and the improvement of gastric histology assessed by the Updated Sydney System. The normal range of procalcitonin, ESR, and CRP were 0 to 0.5 ng/mL, 0 to 20.0 mm/h, and 0.0 to 3.0 mg/L, respectively. |
|
| Funding | The study was supported by the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand (Grant No. MED‐64/2559) on the Field for Knowledge Integration and Innovation by Ministry of Higher Education, Science, Research, and Innovation. | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Participants with FD who had severity score > 4 for at least 1 symptom of dyspepsia according to the SF‐LDQ were recruited and randomized to treatment period. The participants were allocated into 2 groups using consecutive and growing numbers of randomization, starting with number 1, according to a ratio of 1:1.” |
| Allocation concealment (selection bias) | Low risk | Central allocation: “The BR and placebo capsules were identical in all aspects. A sample of the BR and placebo capsules was prepared and kept by the Maharaj Nakorn Chiang Mai University Hospital Pharmacy” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | “This randomized, parallel‐group, double‐blind” ‐ it is unclear whether personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded by the use of placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Nearly complete data were available, 22 participants were lost to follow‐up (14%). "Missing values for all measured parameters were handled by using the last observed carried forward method." |
| Selective reporting (reporting bias) | Low risk | Every outcome is reported as planned in the registry (TCTR20170816002). |
| Other bias | Low risk | No other sources of bias were identified. |
Da Mota Menezes 2006.
| Study characteristics | ||
| Methods |
Study design: randomized double‐blind placebo‐controlled trial Study dates: 2004 Setting and number of centres: outpatient, national, single centre Country: Brazil |
|
| Participants |
Inclusion criteria: 18 years or older, dyspeptic complaints and positive for H pylori, detected by a rapid urease test. Exclusion criteria: patients who received any medication containing nonsteroidal anti‐inflammatory drugs, antibiotics, or gastric antisecretory agents in the last 3 weeks; gastrectomized and vagotomized patients, and individuals with a history of stenosis, perforation, or digestive haemorrhage in the last 2 months prior to inclusion in the study; patients with any malignancy; pregnant patients; patients who did not agree to sign the informed consent form. Sample size: 100 randomized Withdrawals: 3 (1 for allergic reaction and 2 for being prescribed an eradicating drug by the assistant physician) Loss to follow‐up: 4 (2 participants reported improvement of symptoms) Non‐adherent: 1 Age (years and SD): all participants 47 (15.6) Ethnicity by group: not stated Sex (M/F): all participants (36M/64F) Symptom severity at baseline: not available |
|
| Interventions |
Group 1 (n = 55): capsule with 500 mg powder of 20% methanolic extract of Lafoensia pacari, obtained after drying, orally, twice a day. Group 2 (n = 45): capsule with 500 mg of inert material (placebo), orally, twice a day. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: “Overall Treatment Evaluation” Time points measured: end of week 2. Time points reported: end of week 2. Subgroups: none Adverse events How measured: “Self‐Evaluation” card Time points measured: end of week 2. Time points reported: end week 2. Subgroups: none Other outcomes reported in the review: total blood count with platelet count, alkaline phosphatase, GOT, GPT, urea, creatinine, and total cholesterol. |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization. |
| Allocation concealment (selection bias) | Low risk | "130 identical cards were numbered, from 001 to 130, and each card was placed in one of the 130 identical brown envelopes which were sealed. After selecting the patients the attending physician took one of the sealed envelopes, opened it, and removed the card with a number corresponding to the bottle to be given to the patient” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Todos os participante‐médico assistente, endoscopista, farmacêutico, patologista, pacientes e pesquisado resestavam “cegos” durante todo o processo" (All the participant‐attending physicians, endoscopist, pharmacist, pathologist, patients and researchers "blind" during all process) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinding using placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of 8 withdrawals/100 participants) for all results. |
| Selective reporting (reporting bias) | Low risk | The outcomes match the protocol (available in the full thesis document). |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Dabos 2010.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: January 2006 to November 2008 Setting and number of centres: outpatients, various clinics, national Country: Greece |
|
| Participants |
Inclusion criteria: participants 18 to 75 years of age were eligible for the trial if they were found to satisfy Rome II criteria for functional dyspepsia. Symptoms had to be present for at least 12 weeks in the previous 9 months. Exclusion criteria: patients whose main (more than once a week) or the only complaint was gastroesophageal reflux; Helicobacer pylori infection; gastritis or duodenitis on endoscopy; participants using medication that could alter gastric function notably narcotics, tricyclic antidepressants and calcium channel blockers. Sample size: 148 participants randomized Withdrawals: 1 participant in the active treatment was lost to follow‐up. 4 participants (1 in the active treatment group and 3 in the placebo group) discontinued treatment because of a lack of efficacy Age (mean years): Group 1 (Study) 48.8; Group 2 (Control) 46.8 Ethnicity by group: not reported Sex (M/F): Group 1 (Study): 22M/52F; Group 2 (Control) 21M/53F Symptom severity at baseline: Mean and SD Hong Kong index of dyspepsia scores before treatment Group 1 23.68 ± 1.64; Group 2 23.27 ± 1.93 |
|
| Interventions |
Group 1 (n = 74 ): Chios mastic gum 350 mg 3 times daily for 3 weeks. (A resinous exudate which is derived from the stem of the bush Pistacia lentiscus var. chia) Group 2 (n = 74): placebo Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Hong Kong index of dyspepsia and participants’ own global assessment of efficacy Time points measured: baseline and after 3 weeks of treatment. Time points reported: baseline and after 3 weeks Subgroups: participants with oesophagal reflux symptoms. Adverse events How measured: an inquiry after the treatment completion. Time points measured: one‐month follow‐up. Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: each symptom improvement and participants’ own global assessment of efficacy. |
|
| Funding | This study used a grant from the Mastic Gum Producers Cooperative to KJ Dabos. The study was designed by the principal investigator and the design was approved by the sponsor. | |
| Declaration of interest | KJ Dabos received travel bursaries from the sponsor. E Sfika was an employee of the sponsor during the study period. LJV, DF, GIA, GG, have nothing to declare | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The randomization was generated using Proc random (SAS version 6.9). Patients were enrolled at the Dyspepsia clinic of the Gastroenterology Department” |
| Allocation concealment (selection bias) | Low risk | “Central pharmacy assigned participants to their groups. Patients received one capsule three times a day for 3 weeks. The study medication was packaged identically for the two study groups and was identifiable only by a randomization number.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “Participants, researchers that conducted the study and those who assessed the outcomes were blinded to group assignment.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “those who assessed the outcomes were blinded to group assignment.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data for every outcome were reported. 5 participants were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | Patients with only reflux symptoms were excluded. |
Eftekharafzali 2018.
| Study characteristics | ||
| Methods |
Study design: randomized double‐blind placebo‐controlled trial Study dates: 2016 Setting and number of centres: outpatient, national, single centre Country: Iran |
|
| Participants |
Inclusion criteria: based on Rome III criteria, the presence of early satiation, postprandial fullness, epigastric pain, or epigastric burning for the last 3 months with symptom onset at least 6 months prior to diagnosis. Exclusion criteria: organic or structural evidence (including upper endoscopy), history of peptic ulcer or reflux, underlying disease, including heart failure, renal failure, cirrhosis, diabetes, hypothyroidism, and history of abdominal surgeries after evaluation of a gastroenterologist, that participants using herbal, and chemical drugs, and those drinking alcohol, and abusing opiates, pregnant and lactating females. Sample size: 119 randomized participants Withdrawals: loss follow‐up: 18 Group 1: 8 (not regularly using the medication (n = 6) and adverse effects (n = 2)) Group 2: 10 (not regularly using the medication (n = 8) and adverse effects (n = 2)). Age (mean ± SD years): Group 1 (38.30 ± 12.57); Group 2 (44.85 ± 13.08) Ethnicity by group: not stated. Sex (M/F) Group 1 (Study) 19 M/34 F Group 2 (Control) 13 M/35 F Symptom severity at baseline: Rome III criteria (8 symptoms) with Likert scale, according to its severity as follows: absent = 0, mild = 1, moderate = 2 (diverting from but not urging modifications in daily activities), and severe = 3 (influencing daily activities markedly enough to urge modifications). There is a table showing the mean symptom score in Figure 1 of the manuscript, however, there are no baseline values. |
|
| Interventions |
Group 1 (n = 61): intervention. Capsules 500 mg (containing 350 mg Pistacia atlantica mutica resin plus 150 mg sugar), twice daily (1 after lunch, and 1 after dinner) for 4 weeks. Group 2 (n = 58): placebo. Capsules 500 mg (containing 350 mg starch powder plus 150 mg sugar), twice daily (1 after lunch, and 1 after dinner) for 4 weeks. Co‐interventions: none |
|
| Outcomes |
Adverse events How measured: as related to the intervention. Time points measured: at each visit (weeks 2, 4 and 8?) Time points reported: narratively Subgroups: none Other outcomes reported in the review Global symptoms of dyspepsia were not measured. The study reported each symptom separately (using ROME II using 3‐point Likert scale and the list of symptoms (8)) at baseline, weeks 2, 4 and 8. |
|
| Funding | Not available | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "simple randomization using random numbers (Random digit number)" |
| Allocation concealment (selection bias) | Unclear risk | Not described in the article |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Paper mentions that the study is double‐blind without giving more details about it. The placebo capsule was similar in appearance and taste to the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind study, participants were likely blinded (patient‐reported outcomes). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for almost all participants (there are 18 losses to follow‐up) for all outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Ghoshegir 2015.
| Study characteristics | ||
| Methods |
Study design: double‐blind randomized clinical trial Study dates: 2013 to 2014 Setting and number of centres: outpatient, national, single centre Country: Iran |
|
| Participants |
Inclusion criteria: participants aged 18 to 65 years and diagnosed with postprandial distress syndrome (PDS) according to Rome III criteria Exclusion criteria: pregnancy, breastfeeding, peptic ulcer, gastroesophageal reflux disease, dysphagia, coeliac, GI surgery, irritable bowel syndrome, abdominal pain, night diarrhoea, greasy or black stool, blood in stool, mental retardation, immune system disorders, major depression, bipolar disorder and psychosomatic disorders, severe recent weight loss, cancer, renal disorders, current use of antibiotics, proton pump inhibitors, H2 blockers, bismuth, metoclopramide, domperidone, lactulose, nonsteroid anti‐inflammatory drugs, corticosteroids, herbal medicines and drug abuse. Sample size: 180 enrolled; 107 randomized Withdrawals: 8 (intervention: 2 not regularly using the medication; 1 wanted to be pregnant; 1 drug intolerance; 1 medication administration/ placebo: 2 not regularly using the medication; 2 drug intolerance). Age (years): Group 1 (45.5 ±15.5); Group 2 (41 ±11.7) Ethnicity by group: not stated. Sex (M/F) Group 1 (Study) 26 M/21 F Group 2 (Control) 28 M/32 F Symptom severity at baseline: FD severity scale with 4‐item Likert scale was employed to answer the questions (16). Total score (good) 0 to 64 (bad); Each participant's total score was between 0 and 48. Group 1: 10.6 Group 2: 10.96 |
|
| Interventions |
Group 1 (n = 47): anise powder, 3 g after each meal (3 times/day) for 4 weeks (This plant specimen was kept in their herbarium with number 1697). Group 2 (n = 60): corn starch powder, 3 g after each meal (3 times/day) for 4 weeks. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: FD severity scale with 4‐item Likert scale was employed to answer the questions. Time points measured: at baseline and end of weeks 2, 4 and 12 Time points reported: none Subgroups: none Adverse events How measured: questionnaire Time points measured: possibly at complete follow‐up Time points reported: narratively. Subgroups: none Quality of life How measured: Persian version SF‐36 Time points measured: at baseline and at the end of week 12 Time points reported: at baseline and at the end of week 12 Subgroups: none Other outcomes reported in the review: none |
|
| Funding | Not available | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors do not explain how the randomization was performed ("They were randomized by simple randomization method into intervention and placebo groups"). |
| Allocation concealment (selection bias) | Unclear risk | Authors do not explain how the randomization was performed or the manner of concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Doctors and patients were blind to the assigned treatments". "The placebo were packed similar to anise powder in shape, color and size. Both powders were prepared in similar packages" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Doctors and participants were blind to the assigned treatments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of eight withdrawals from 107 randomized participants) for all results. |
| Selective reporting (reporting bias) | High risk | The study protocol points out the assessment of the severity of the disorder, quality of life (primary outcomes) and side effects (secondary outcome), but quality of life and side effects were not reported. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Giacosa 2015.
| Study characteristics | ||
| Methods |
Study design: parallel‐group: randomized trial Study dates: 2012 Setting and number of centres: outpatients, 2 centres Country: Italy |
|
| Participants |
Inclusion criteria: patients with functional dyspepsia According to Rome II criteria. Exclusion criteria: patients with relevant gastroesophageal reflux symptoms (retrosternal pain, burning, or regurgitation) as well as patients with clear evidence of irritable bowel syndrome, patients with a previous diagnosis of cancer or with previous surgery of the upper gastrointestinal tract or of the biliopancreatic system (except for cholecystectomy) and patients with active HP infection or with gastric or duodenal ulcer, as well as pregnant women, were excluded. Sample size: 126 Withdrawals: none Age (mean ± SD years): Group 1 (Study): 45.85 ± 16.61; Group 2 (Control) 48.05 ± 17.02 Ethnicity by group: not reported Sex (M/F): Group 1 (Study): 19 M/46 F; Group 2 (Control) 20 M/41 F Symptom severity at baseline: only homogenous allocation by dyspepsia typology is reported. Ulcer‐like FD Group 1: 5; Group 2: 6. Dysmotility‐like FD Group 1: 39; Group 2: 33. Unspecified FD Group 1: 21; Group 2:22 |
|
| Interventions |
Group 1 (n =65 ): 100 mg of artichoke and 20 mg of ginger extracts in hard gelatin capsules twice a day before starting lunch and dinner for 30 days. Group 2 (n = 61): placebo twice a day before starting lunch and dinner for 30 days. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: intensity of functional dyspepsia as defined by patient’s rating. Patient’s ratings were ascribed to 1 of 4 categories (0: not improved or worsened, 1: slightly improved, 2: markedly improved, and 3: completely improved). Time points measured: Day 0, after 2 and 4 weeks Time points reported: Day 0, after 2 and 4 weeks Subgroups: ulcer‐like FD, dysmotility‐like and unspecified FD Study (0 to 3 rating, 0 means without improvement, 3 completely improved) Adverse events How measured: unwanted adverse events, tolerability, vital signs, and clinically significant modifications in laboratory values were monitored in each visit. Time points measured: Day 0, after 2 and 4 weeks Time points reported: not reported. Subgroups: none Other outcomes reported in the review: intensity of 6 dyspeptic symptoms, epigastric fullness, bloating, early satiety, nausea, vomiting, and epigastric pain |
|
| Funding | Not available | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients who met the admission criteria and who signed the informed consent to the study have been assigned consecutive and growing numbers of randomization, starting with number 1, according to a 1: 1 ratio” |
| Allocation concealment (selection bias) | Low risk | Central allocation: “Identical and odorless capsules for each treatment group (intervention and placebo) were assigned according to a randomization code. Both products (active supplement and placebo) were provided free of charge by Indena (Milan) in packaging specifically designed for this study” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “Investigators were blinded to the randomization table.” “Identical and odorless capsules for each treatment group (intervention and placebo) were assigned according to a randomization code. Both products (active supplement and placebo) were provided free of charge by Indena (Milan) in packaging specifically designed for this study” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded with the use of placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data for every outcome were reported. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available. Adverse events were measured but not reported. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Holtmann 2003.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: not available Setting and number of centres: multicentre, outpatient, national Country: Germany |
|
| Participants |
Inclusion criteria: functional dyspepsia was diagnosed if the participants had upper abdominal pain or discomfort (an unpleasant sensation not reaching the level of pain characterized by one or more of the following symptoms: early satiety, postprandial fullness, bloating and nausea) for at least 2 months. Exclusion criteria: identifiable underlying structural or biochemical cause of these symptoms. Marked reflux symptoms (retrosternal pain, burning and regurgitation) were considered to be associated with gastro‐oesophageal reflux disease. People whose symptoms were predominantly those of irritable bowel syndrome were not eligible. Sample size: 246 participants Withdrawals: 13 participants were lost Group 1 (Study): 6 in total, 2 due to adverse effects, 3 because of participant's request and 1 for other reason. Group 2 (Control): 7 in total, 2 due to adverse events, 2 because of participant's request, 1 for other reason and 2 dropped out after screening. Age (mean ± SD years): Group 1 (Study): 48.5 ± 13.3; Group 2 (Control): 46.1 ± 13.3 Ethnicity by group: not available Sex (M/F): Group 1 (Study): 44 M/ 85 F; Group 2 (Control): 46 M/ 69 F Symptom severity at baseline: only the type of dyspepsia in each group was reported. Group 1 (Study): ulcer‐type: 18 (14 %); dysmotility‐type: 74 (57.4 %); unspecified 37 (28.7%) Group 2 (Control) ulcer‐type: 18 (15.7 %); dysmotility‐type: 66 (57.4 %); unspecified 37 31 (27 %) |
|
| Interventions |
Group 1 (n = 129): 320 mg artichoke leaf extract, 2 capsules, 3 times a day. A dry extract had a drug‐to‐extract ratio of 3.8–5.5: 1. The main substance classes are caffeoylquinic acids, flavonoids and sesquiterpene lactones (bitters). Group 2 (n = 115): placebo 2 capsules 3 times a day Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: sum score of the participant’s weekly rating of the overall change in dyspeptic symptoms (4‐point scale) (0 = not improved; 1 = slightly improved; 2 = markedly improved; 3 = completely improved) Time points measured: weeks 1, 2, 3, 4, 5 and 6 Time points reported: weeks 1, 2, 3, 4, 5 and 6 Subgroups: participants without additional irritable bowel symptoms (N = 159) gained much more benefit from artichoke leaf extract Adverse events How measured: inquired in each follow‐up Time points measured: weeks 1, 2, 3, 4, 5 and 6 Time points reported: cumulative incidence Subgroups: an accumulation of adverse events for a specific symptom or disease was not observed. Quality of life How measured: NDI Time points measured: baseline and weeks 2, 4 and 6 Time points reported: baseline and weeks 2, 4 and 6 Subgroups: none Other outcomes reported in the review: course of overall changes in individual dyspeptic symptoms during treatment, the sum score of the participant’s self‐rating of the intensity of each dyspeptic symptom, the sum score of differences to baseline |
|
| Funding | This study was sponsored by Lichtwer Pharma AG, Berlin, German | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization was done electronically with ‘Rancode’ (idv GmbH, Germany) assigning patient numbers to either ALE or placebo (1:1) in ascending order.” |
| Allocation concealment (selection bias) | Low risk | “Placebo capsules were identical in appearance, smell and taste to the test drug but without pharmacologically active ingredients. Neither the patient nor the physician were aware of the randomization as active or placebo.” ‐ Central allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “Neither the patient nor the physician were aware of the randomization as active or placebo.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Neither the patient nor the physician were aware of the randomization as active or placebo.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data were available (13/246 participants were lost to follow‐up). |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Other bias | Low risk | Not other sources of bias were identified. |
Holtmann 2013.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized controlled trial Study dates: unclear Setting and number of centres: not available Country: not available |
|
| Participants |
Inclusion criteria: not available Exclusion criteria: unclear Sample size: 124 recruited;110 randomized Withdrawals: not available Age (years): not available Ethnicity by group: not available Sex (M/F): not available Symptom severity at baseline: not available |
|
| Interventions |
Group 1 (n = 25): placebo Group 2 (n = 27): STW5 Group 3 (n=30): PPI Group 4 (n=28): STW5+PPI Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Gastrointestinal symptoms score (GIS) Time points measured: before and after 2 and 4 weeks of treatment Time points reported: unclear Subgroups: unclear Quality of life How measured: The Nepean Dyspepsia Index (NDI). Time points measured: before and after 2 and 4 weeks of treatment Time points reported: unclear (narrative statement) Subgroups: unclear |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | We found 4 abstracts for this study. The first 2, published in 2012 reported a smaller number of participants than those published in 2013. Considering that these were labelled as preliminary results, the study arms were identical and the author team was the same, we mapped them to the same study. We contacted study authors to verify this but we obtained no response (g.holtmann@uq.edu.au; nicholas.talley@newcastle.edu.au). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This domain cannot be answered because the full text article is not available. |
| Allocation concealment (selection bias) | Unclear risk | This domain cannot be answered because the full text article is not available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | This domain cannot be answered because the full text article is not available. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | This domain cannot be answered because the full text article is not available. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | This domain cannot be answered because the full text article is not available. |
| Selective reporting (reporting bias) | Unclear risk | This domain cannot be answered because the full text article is not available. |
| Other bias | Unclear risk | This domain cannot be answered because the full text article is not available. |
Hu 2011.
| Study characteristics | ||
| Methods |
Study design: parallel‐group: randomized trial Study dates: not available Setting and number of centres: outpatients, national, single centre Country: Taiwan |
|
| Participants |
Inclusion criteria: Rome lll criteria for functional dyspepsia Exclusion criteria: symptoms of retrosternal pain, burning, and regurgitation were considered features of gastroesophageal reflux disease, rather than of functional dyspepsia Sample size: 11 Withdrawals: none Age (years): not available Ethnicity by group: not available Sex (M/F): not available Symptom severity at baseline: not available |
|
| Interventions |
Group 1 (n =6 ): 3 capsules of 1.2 g ginger root powder Group 2 (n =5 ): 3 identical placebo capsules that contained starch, together with 50 mL water. Co‐interventions: 500 ml of low‐nutrient hot soup; chicken and corn. |
|
| Outcomes |
Global symptoms of dyspepsia How measured: VAS for symptoms of pain, nausea, abdominal discomfort, bloating and abdominal fullness, was administered at 10‐min intervals between t = ‐10 and 90 min. Grading was made on a 100‐mm unmarked line between “no symptoms” at one end and “excruciating symptoms” at the other. Time points measured: day 1 and day 7 Time points reported: day 1 and day 7 Subgroups: none Other outcomes reported in the review: the Antral area, fundus area and diameter, and the frequency of antral contractions were measured using ultrasound at frequent intervals, and the gastric half‐emptying time was calculated from the change in the antral area. blood was taken for measurement of plasma glucagon‐like peptide‐1 (GLP‐1), motilin and ghrelin concentrations. |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Eleven patients with functional dyspepsia were studied twice in a randomized double‐blind manner” |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | “Three capsules that contained a total of 1.2 g ginger root powder, or three identical placebo capsules that contained starch, together with 50 mL water.” ‐ it is unclear if personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Three capsules that contained a total of 1.2 g ginger root powder, or three identical placebo capsules that contained starch, together with 50 mL water.” ‐ participants (outcome assessors) were likely blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data were available for all participants. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Other bias | Low risk | No other sources of bias were detected. |
Khonche 2017.
| Study characteristics | ||
| Methods |
Study design: randomized placebo‐controlled clinical trial Study dates: December 2015 to March 2016 Setting and number of centres: outpatient, national, single centre Country: Iran |
|
| Participants |
Inclusion criteria: participants aged 20 to 80 fulfilling Rome III for functional dyspepsia. Exclusion criteria: patients with peptic ulcer disease, inflammatory bowel disease, irritable bowel syndrome, pure gastro‐oesophagal reflux disease, biliary motility disorder and any organic gastrointestinal disease; patients with a history of H pylori infection eradicating drugs use within the past 3 months; patients with a history of gastrointestinal system surgery; patients with background systemic diseases such as diabetes mellitus, heart failure, hepatic failure, renal failure, asthma, chronic obstructive pulmonary disease, neoplasms and severe psychiatric diseases; patients addicted to alcohol and opium; patients using cardiac, antihypertensive, antipsychotic, antianxiety, antibiotic and corticosteroid drugs and iron and calcium; patients with a history of discontinuing prescribed pharmacotherapy and incomplete treatment; pregnant women; women planning pregnancy; breast‐feeding women. Sample size: 103 participants randomized. Withdrawals: ‐ Loss to follow‐up: 3 (they did not come for a monthly visit due to personal reasons) Age (mean ± SD years): Group 1 (38.31 ± 12.57); Group 2 (42.87 ± 13.33) Ethnicity by group: not stated Sex (M/F): Group 1 (25/25); Group 2 (23/27) Symptom severity at baseline: the Hong Kong dyspepsia index Group 1: 27.79 ± 7.32; Group 2: 24.91 ± 6.10 |
|
| Interventions |
Group 1 (n = 52): intervention, Mentha pulegium capsule (drug extract ratio: 15.9:1, extraction solvent: 70% v/v aqueous ethanol). 330 mg (dosage regimen for the extract was empirically determined) 3 times daily taken for 8 weeks. Group 2 (n = 51): placebo, capsule (roasted powder) 3 times a day orally for 8 weeks. Co‐interventions: Famotidine 40 mg tablet per day for 8 weeks |
|
| Outcomes |
Global symptoms of dyspepsia How measured: The Hong Kong Dyspepsia Index Time points measured: before and after 2, 4 and 8 weeks of intervention Time points reported: before and after 2, 4 and 8 weeks of intervention (reported in table 2 and 3) Subgroups: none Adverse events How measured: as related to the intervention Time points measured: possibly at complete follow‐up Time points reported: narratively Subgroups: none Quality of life How measured: SF‐36 Health Survey scores Time points measured: before and after 2, 4 and 8 weeks of intervention Time points reported: before and after 2, 4 and 8 weeks of intervention (reported in table 4) Subgroups: none Other outcomes reported in the review: infection with H pylori, complete blood cell count and the blood levels of aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, blood urea nitrogen and creatinine |
|
| Funding | Possibly by the Institute of Medicinal Plants (Karaj, Iran) and Baqiyatallah University of Medical Sciences (Tehran, Iran) | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | Phenolics, flavonoids, quercetin, rosmarinic acid, chlorogenic acid and antioxidant activity were quantified in the M. pulegium extract. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Block randomization with computer generated random number table and sequentially numbered containers each representing a block consisting of two patients was used for the treatment allocation.” |
| Allocation concealment (selection bias) | Low risk | "Three different persons generated the random allocation sequence, enrolled the patients and assigned them to interventions. These persons, care‐providers and patients were blinded to interventions." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Care providers and patients were blinded to interventions.” "The M. pulegium and placebo capsules were identical in all respects (to make the placebo capsules smell like the M. pulegium, essential oil was put in the placebo capsules containers)." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Care providers and patients were blinded to interventions.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for nearly all participants (with the exception of 3 withdrawals from 103 randomized patients) for all results. |
| Selective reporting (reporting bias) | Low risk | The outcomes shown in the study protocol were reported in the article. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Kupcinskas 2008.
| Study characteristics | ||
| Methods |
Study design: RCT Study dates: not available Setting and number of centres: outpatient, national Country: Lithuania |
|
| Participants |
Inclusion criteria: non‐lactating and non‐pregnant, aged 18 to 70 years. Symptoms of functional dyspepsia were defined as per the Rome II. Exclusion criteria: patients with predominant reflux symptoms were considered to have non‐erosive gastroesophageal reflux disease (NERD), clinically relevant abnormalities in physical examination or laboratory screening tests with a history of peptic ulcer and/or reflux‐esophagitis at endoscopy or any evidence of significant hematological, hepatic, renal, cardiac, pulmonary, metabolic, and other structural diseases. Sample size: 132 randomized. Withdrawals: 16 (5 per each group prematurely withdrawn and 1 group 2 not treatment) Age (mean ± SD years): Group 1 (45.7 ± 11,9); Group 2 (42.9 ± 13); Group 3 (43.2 ± 14) Ethnicity by group: not stated. Sex (M/F) Group 1 (Control): 5 M/39 F Group 2 (Low dose): 4 M/39 F Group 3 (High dose): 9 M/35 F) Symptom severity at baseline: Gastrointestinal Symptom Rating Scale (GSRS) 15 questions using a scale from 1 (no discomfort at all) to 7 (very severe discomfort) Group 1: 2.61 ± 1.45 Group 2: 2.27 ± 1.09 Group 3: 2.66 ± 1.38 |
|
| Interventions |
Group 1 (n = 44): 40 mg astaxanthin: 5 capsules twice daily for 4 weeks Group 2 (n = 43): 16 mg astaxanthin: 5 capsules twice daily for 4 weeks Group 3 (n = 44): placebo. 5 capsules placebo twice daily for 4 weeks Co‐interventions: none |
|
| Outcomes |
Adverse events How measured: as related to the intervention Time points measured: at complete follow‐up Time points reported: at complete follow‐up Subgroups: none Quality of life How measured: SF‐36 Healthy Survey (by sub‐item) Time points measured: weeks 0, 4, and 8 Time points reported: weeks 0, 4, and 8 Subgroups: none Other outcomes reported in the review: urea breath test by H pylori Global symptoms of dyspepsia were not measured: The study reported each symptom separately (using GSRS score) at baseline, week 4 and week 8. Divided results in abdominal pain, indigestion syndrome, reflux syndrome. |
|
| Funding | AZT Grant from Lund University (Grant 16x‐04723) | |
| Declaration of interest | Dr. Ake Lignell was the representative of the sponsor, AstaReal AB. Other authors declare that the answer to the question on competing interest is No and therefore have nothing to declare. No dependence from funders to researchers occurred | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated random list with permuted blocks." |
| Allocation concealment (selection bias) | Low risk | "The patient number assigned corresponded to the treatment given and also appeared on the medication container and ran through numbers 001–132." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Intervention and placebo capsules were elaborated with identical characteristics. It is unclear if personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded with the use of placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data are available for almost all participants (with the exception of 16 withdrawals from 131 randomized patients) for all outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Madisch 1999.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: unknown Setting and number of centres: 25 centres, outpatients Country: Germany |
|
| Participants |
Inclusion criteria: participants aged 18 or older with functional dyspepsia defined as epigastric pain (intensity at least 4 cm on the visual analogue scale) at least one of the following dyspeptic symptoms in addition: a sensation of pressure, heaviness or fullness; early satiety; non‐acid eructation; food intolerance; nausea with symptoms present for at least 14 days. Participants had upper abdominal sonography, esophagogastroduodenoscopy (if indicated other endoscopic surveillance) finding with biopsy and H pylori urease rapid test not more than 6 weeks previously. Exclusion criteria: operations on the gastrointestinal tract (exception: appendectomy or cholecystectomy at least five years ago); confirmed organic cause of the acute or chronic dyspepsia symptoms or suspicion of an organic cause respectively; cisapride treatment during the past seven days; simultaneous or participation in further clinical trials within the past four weeks; pregnancy, lactation; dementia or severe intellectual impairment which make selfassessment impossible for the patient; chronic alcohol and medication abuse; hypersensitivity to one of the constituents of the test or reference preparation; concomitant diseases such as severe cardiovascular, liver, kidney or respiratory insufficiency; neoplasia, epilepsy; diseases of extrapyramidal motor system; febrile diseases; severe metabolic disorders or hormonal disorders which may cause abdominal symptoms; severe functional diseases apart from functional dyspepsia and irritable colon; severe diarrhea; known QT prolongation or patients with known risk factors for QT prolongation; intake of inadmissible concomitant medication: other peristaltic stimulants than cisapride; agonists and antagonists of gastrointestinal hormones; motilides; acid‐reducing medication; bismuth preparations; benzodiazepines or other sedative preparations, laxatives; opioids; all preparations with side effects on the gastrointestinal tract; other phytogastroenterological preparations; all preparations known to interact with cisapride Sample size: 120 Withdrawals: 6 and 3 in each group, respectively. 3 due to deterioration in symptoms with peppermint oil and caraway, one due to diarrhoea and two cases of deterioration of symptoms with cisapride. Age (mean ± SD years): Group 1 (study group): 47.6 ± 16.0; Group 2 (control group): 46.9 ± 14.4 Ethnicity by group: not stated Sex (M/F): Group 1 (study): F = 38 M = 22; Group 2 (control): F = 28 M = 30 Symptom severity at baseline Mean Dyspeptic Discomfort Score score and SD Group 1 (study): 36.7 ± 12.2 Group 2 (control): 35.8 ± 12.9 |
|
| Interventions |
Group 1 (n =62 ): enteric‐coated soft‐gelatin capsule of the test preparation (Enteroplant) contained 90 mg peppermint oil and 50 mg caraway oil. The daily dose was 2 × 1 capsule, corresponding to 180 mg peppermint oil and 100 mg caraway oil Group 2 (n = 58): cisapride was taken 3 times a day before meals (daily dose: 30 mg cisapride Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Dyspeptic Discomfort Score (DDS) ‐ Categorical Time points measured: baseline, day 15 and 29 Time points reported: baseline, day 15 and 29 Subgroups: none Adverse events How measured: clinical and laboratory assessments Time points measured: baseline, day 15 and 29 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: Clinical Global Impressions (CGI ) and the intensity of pain in the upper abdomen (VAS 0 to 10) |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Software was used to generate random numbers on the basis of which the patients were allocated to the treatment groups in balanced blocks of four patients. The study sites did not know the block size.” |
| Allocation concealment (selection bias) | Low risk | “In order to ensure the double‐blind character of the study, the capsules or tablets were inserted into hard‐gelatin capsules which were soluble in acid milieu of gastric juice. The test and reference preparation, as well as the placebo capsules, could therefore not be distinguished on the basis of their outward appearance.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “The randomization list was kept sealed and only opened after the conclusion of all data corrections and classification of the evaluation groups. Furthermore, decoding envelopes were prepared which enabled the randomization codes to be broken in individual cases when there were compelling reasons for this. However, these envelopes remained sealed at all times.'' |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The randomization list was kept sealed and only opened after conclusion of all data corrections and classification of the evaluation groups” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data were available (6 participants were lost). |
| Selective reporting (reporting bias) | Unclear risk | Every outcome is reported, but the study protocol/registry was unavailable. |
| Other bias | Low risk | None. |
Madisch 2001a.
| Study characteristics | ||
| Methods |
Study design: parallel‐group: randomized trial Study dates: not available Setting and number of centres: multicentre, outpatients Country: Germany |
|
| Participants |
Inclusion criteria: men and women aged 25 to 70 years; confirmed functional dyspepsia (normal findings esophagogastroduodenoscopy, abdominal ultrasound, basic laboratory); at the start of the study, florid dyspepsia symptoms lasting more than 4 weeks Exclusion criteria: known ulcer disease; malignancies of the entire gastrointestinal tract; inflammatory bowel disease; pancreatitis; cholecystitis, cholangitis; diverticulitis; food allergies; well‐known laxative abuse; additional medication that affects gastrointestinal function; psychiatric illnesses; allergies to verum substances; abdominal surgery excluding appendectomy (at least 6 months ago); known irritable bowel syndrome; participation in other studies; HIV positive status; known malabsorption, maldigestion; diseases of the genitourinary tract; heart disease; thyroid disease Sample size: 60 participants; no information regarding sample size estimation. Withdrawals: 1/20 lost to follow‐up in the placebo group. Age (mean years): Group 1 (STW‐5): 49.2; Group 2 (STW‐5 s): 47.2; Group 3 (Placebo): 44.2 Ethnicity by group: unknown Sex (M/F) Group 1 (STW‐5): 4 M/16 F Group 2 (STW‐5 s): 9 M/11 F Group 3 (Control): 9 M/11 F Symptom severity at baseline: strength of the complaints (number of participants in each group) Group 1 (STW‐5): easy 1; moderate 12; strong 6; very strong 1 Group 2 (STW‐5 s): easy 2; moderate 14; strong 4; very strong ‐ Group 3 (Placebo): easy 2; moderate 15; strong 2; very strong 1 |
|
| Interventions |
Group 1 and 2 (n = 40): STW‐5 or STW‐5: 3 pills a day for 4 weeks. (Dose unclear) Group 3 (n = 20): placebo 3 times a day Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: GIS Time points measured: Day 0, 14 and 28 Time points reported: Day 0, 14 and 28 Subgroups: none Adverse events How measured: by notification of all adverse events at each time of the examination and by global notification at the end of treatment, including the course of the visual parameters and routine laboratory Time points measured: alongside the study and on day 14 and 28 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: time of stable improvement |
|
| Funding | Company: Steigerwald Arzneimittel CmbH (Darmstadt) | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "All patients received enł according to the randomized allocation to the respective therapy groups (randomisation 1: 1: l) or 3 times daily." |
| Allocation concealment (selection bias) | Unclear risk | Not specified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | “A double‐blind, placebo‐controlled, randomized multicenter trial.” ‐ it is unclear whether personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded with placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data are available. |
| Selective reporting (reporting bias) | Unclear risk | Each outcome is reported but the registry or protocol is unavailable. |
| Other bias | Low risk | None noticed |
Madisch 2004.
| Study characteristics | ||
| Methods |
Study design: parallel group randomized trial Study dates: not available Setting and number of centres: multicentre, outpatients, national Country: Germany |
|
| Participants |
Inclusion criteria: participants aged 21 to 70 years; endoscopically confirmed functional dyspepsia with at least 6 months of persistent or recurrent symptoms (ulcer‐type and/or dysmotility‐type dyspepsia); no organic findings following upper GI endoscopy, abdominal sonography (both in preceding 6 weeks), and routine blood count and blood chemistry analysis; a baseline of at least 3 moderate to very severe dyspeptic symptoms Exclusion criteria: History of peptic ulcer disease and GERD; predominant symptoms of irritable bowel syndrome; predominant symptoms of GERD; any alarm symptoms (e.g. weight loss, black stool, dysphagia); cardiac, pulmonary, liver or kidney disease; surgical procedures in the gastrointestinal tract, excluding appendectomy, carried out more than 6 months previously; pregnancy or breastfeeding; current alcoholism or drug abuse; current intestinal or extraintestinal organic disease (e.g. cholangitis, pancreatitis, enteropathy, etc.); severe organic or psychiatric illness; allergies to one of the component substances in the trial medication (active medication); intake of any medication influencing the gastrointestinal tract; participation in another clinical trial less than 3 months previously; HIV positive status; malabsorption, maldigestion Sample size: 120 participants Withdrawals: 8 in total, Group 1 STW 5‐ll for 8 weeks = 0 Group 2 STW 5‐ll for 4 weeks followed by placebo = 4 in total, 2 due to no compliance, 1 because of a personal wish, 1 discontinued treatment due to insufficient efficacy. Group 3 4 weeks of placebo followed by STW 5‐ll = 3 in total, 1 due to adverse events, 1 discontinued treatment because of insufficient efficacy, and 1 because of complete relief of symptoms. Group 4 placebo for eight weeks = 1 in total discontinued treatment because of insufficient efficacy Age (mean ± SD years): Group 1 (STW 5‐ll): 44.1 ± 13.0; Group 2 (STW 5‐ll and placebo): 45.5 ± 13.2; Group 3 (placebo and STW 5‐ll): 43.8 ± 12.6; Group 4 (placebo): 45.2 ± 13.0 Ethnicity by group: not available Sex (M/F) Group 1 (STW 5‐ll): 21 F/9 M Group 2 (STW 5‐ll and placebo: 19 F/11 M Group 3 (placebo and STW 5‐ll): 24 F/6 M Group 4 (placebo): 21 F/9 M Symptom severity at baseline: GIS at baseline (mean ± SD): Group 1 (STW 5‐ll): 12.3 ± 4.7; Group 2 (STW 5‐ll and placebo): 12.1 ± 4.6; Group 3 (placebo and STW 5‐ll): 12.4 ± 3.8; Group 4 (placebo): 12.2 ± 3.9 |
|
| Interventions | Treatment during the final 4‐week period was based upon the investigators’ judgements of treatment efficacy during the second 4‐week period of randomized treatment. In patients with appropriate control of symptoms, treatment with the compound they had received during the preceding 4 weeks was continued Group 1 (n = 30 ): STW 5‐ll =15 ml of Iberis amara totalis (1:2, 50% v/v ethanol), 30 ml of matricaria flower (1:3, 30% v/v ethanol), Liquiritiae radix, 10 ml and Melissae folium 15 ml, peppermint leaves (Menthae piperitae folium, 10 ml), caraway (Carvi fructus, 20 ml), and lemon balm (Melissae folium, 15 ml) per 100 ml (3 x 20 drops daily prior to meal) for 8 weeks. Group 2 (n =30 ): STW 5‐ll for 4 weeks followed by placebo Group 3 (n =30 ): placebo for 4 weeks followed by STW 5‐ll Group 4 (n =30 ): placebo for 8 weeks Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: GIS and Likert scale of each symptom (absent, 0; mild, 1; moderate, 2; severe, 3; very severe, 4) Time points measured: baseline, 4, 8 and 12 weeks. Time points reported: baseline, 4, 8 and 12 weeks. Subgroups: none Adverse events How measured: reported in follow‐ups. Time points measured: baseline, 4, 8 and 12 weeks. Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: VAS used to determine the participant's global judgement of intensity of discomfort (ranging from 0 (no complaints) to 10 (most intense complaints) by diary cards. |
|
| Funding | Steigerwald Arzneimittelwerk GmbH, Darmstadt, Germany | |
| Declaration of interest | Not available | |
| Notes | This study had a component of cross‐over. For the purpose of this review we included the first part of the randomization. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A random code based on the method of permuted blocks, with a block size of four, was prepared in advance for each study center.” |
| Allocation concealment (selection bias) | Low risk | “Investigators had only numbered bottles and no allocation lists. Thus, patients, investigators and study centers maintained strict blinding.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “Investigators had only numbered bottles and no allocation lists. Thus, patients, investigators and study centres maintained strict blinding.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It is not clearly stated whether the clinicians who assessed the outcomes were blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data were available (8/120 patients were lost). |
| Selective reporting (reporting bias) | Unclear risk | Study protocol/registry unavailable. |
| Other bias | Low risk | No other sources of bias were identified. |
Mala 2018.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: 28 December 2015 to 10 February 2017 Setting and number of centres: outpatients, 1 centre Country: India |
|
| Participants |
Inclusion criteria: age 25 to 60 years (both inclusive); male and female participants; fulfilling Rome III Diagnostic Criteria for Functional Dyspepsia; must meet the criteria for 3 months and must begin experiencing symptoms for at least 6 months before diagnosis; willing to give written informed consent Exclusion criteria: history of Peptic ulcer, Gastro‐oesophageal Reflux Disease, Gastrointestinal surgery or any other clinically significant gastrointestinal disease; psychiatric illness; pregnant or lactating women; history of congestive heart failure or uncontrolled hypertension; abnormal haematological or biochemical parameters; taken antibiotics or any other drugs in last 2 weeks whose primary site of action is in the Gastrointestinal tract; any condition that in the opinion of the investigator, does not justify participation in the study. Sample size: 43; no information regarding the reason for the sample size. Withdrawals: 3 in group 1, 2 in group 2. Age (mean years): overall 29.46 ± 6.24 Ethnicity by group: not stated Sex (M/F): not stated Symptom severity at baseline (mean and SEM) Group 1 (study): Gastrointestinal symptom rating scale: 43.91 ± 0.76; Glasgow dyspepsia severity scale: 10.45 ± 0.21 Group 2 (control): Gastrointestinal symptom rating scale: 45.33 ± 0.77; Glasgow dyspepsia severity scale: 10.79 ± 0.20 |
|
| Interventions |
Group 1 (n = 24): Asafin (Ferula asafoetida) 1 capsule before breakfast and another 1 before dinner (250 mg × 2/day). Its relative composition of asafoetida gum, dietary fibre, volatile oil, and ferulic acid content was carefully measured. Asafin containing about 42% (w/w) asafoetida‐gum‐oleoresin formulated with debittered fenugreek powder rich in soluble dietary fibre, so that each 250 mg capsules of Asafn provided 90 ± 5 mg of asafoetida‐gum. Group 2 (n = 24): placebo 250 mg twice a day. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Gastrointestinal Symptom Rating Scale (GSRS) and Glasgow Dyspepsia Severity Score (GDSS). Both seem to be validated. GSRS consists of a 7‐point graded Likert‐type scale where 1 represents the absence of troublesome symptoms and 7 represents the most troublesome symptoms. This study used a modified version of GDSS where 0 was the minimum possible score and 20 was the maximum score, in the ascending order of discomfort. Time points measured: baseline and day 30 Time points reported: baseline and day 30 Subgroups: none Adverse events How measured: evaluated by specifically collecting the individual data regarding any adverse reactions, clinical changes, or discomforts. Haematological and biochemical parameters at the beginning and at the end of the study were also conducted as a measure of safety. Short phone calls were used Time points measured: weekly, 4 weeks Time points reported: cumulative incidence Subgroups: none Quality of life How measured: Nepean dyspepsia index NDI. The present study employed the short form (NDI‐SF) of NDI having 10 items, with a 5‐point Likert scale ranging from 0 (not at all or not applicable) to 4 (extremely applicable) Time points measured: day 0 and day 30 Time points reported: day 0 and day 30 Subgroups: none Other outcomes reported in the review: none |
|
| Funding | Akay Flavours and Aromatics Private Limited Malaidamthuruthu Ernakulam KERALA 683561 India | |
| Declaration of interest | Asafn is the registered trademark of M/s Akay Flavours & Aromatics Pvt. Ltd, India. Tree of the co‐authors were members of Akay Flavours & Aromatics Pvt. Ltd. And Dr. K. N. Mala, who conducted the present study, has no conficts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A total of 60 subjects (aged between 25 and 55 years) were enrolled and provided with a unique three‐digit randomization code." |
| Allocation concealment (selection bias) | Low risk | “Asafin has the characteristic smell of asafoetida oleo‐gum‐resin and the placebo was MCC. In order to have the asafoetida oleo‐gum‐resin like smell, MCC was plated with 0.01% of asafoetida oleo‐gum‐resin. Thus, each bottle (Asafn and placebo) of capsules was managed to have identical smell.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Randomized, double‐blinded, placebo‐controlled design." “Blinding efficacy was assessed by giving a chance to guess the group to which each subject was assigned to ensure the smell identification is possible or not.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Blinding efficacy was assessed by giving a chance to guess the group to which each subject was assigned to ensure the smell identification is possible or not.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Most of the data were available; 5/48 participants dropped out. |
| Selective reporting (reporting bias) | Low risk | The primary outcome and adverse events were reported as the registry (CTRI/2018/01/011149) although quality of life was not prespecified. |
| Other bias | Unclear risk | Baselines characteristics of each group were poorly described. |
May 2000.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: 1997 to 1998 Setting and number of centres: outpatient, single‐centre, national Country: Germany |
|
| Participants |
Inclusion criteria: at least 18 years of age, secured diagnosis of functional dyspepsia (diffuse, unspecific, variable, moderately intense epigastric pain with at least four points on the visual analogue scale, at least one additional dyspeptic key symptom, organ pathology excluded by in‐depth clinical examination sonography and esophagogastroduodenoscopy), with a current episode lasting for at least 14 days. Exclusion criteria: Severe organic disorders, disorders that could cause gastrointestinal symptoms, severe functional disorders other than dyspepsia, severe diarrhoea, inability to discontinue a concomitant medication that could be expected to interact with the assessment of the study's outcome variables (e.g. prokinetics, agonists and antagonists of gastric hormones, acid‐reducing drugs, bismuth preparations, sedatives, laxatives, non‐steroidal antiphlogistics), history of major gastrointestinal surgery, presence of gastrointestinal 'alarm symptoms' pointing to a malignant, ulcer, reflux oesophagitis, or reflux dyspepsia. Sample size: 96 randomized Withdrawals: 2 participants were withdrawn because of symptom aggravation. Loss to follow‐up: 19 (intervention 10; placebo 7 for protocol violations, the most frequent of which were the use of disallowed concomitant medication and failure to complete the study period as scheduled. Age (years): Group 1 (51); Group 2 (51.4) Ethnicity by group: not stated. Sex (M/F): Group 1 (16/32); Group 2 (16/32) Symptom severity at baseline Dysmotility‐type dyspepsia: Group 1 50.0%; Group 2 47.9% Ulcerous dyspepsia: Group 1 14.6%; Group 2 10.4% idiopathic/essential dyspepsia: Group 1 35.4%; Group 2 41.7% |
|
| Interventions |
Group 1 (n = 48): intervention: 90 mg peppermint oil and 50 mg caraway oil, 1 in the morning, 1 at lunchtime for 28 days. Group 2 (n = 48): placebo: capsules 1 in the morning, 1 at lunchtime for 28 days. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Clinical Global Impressions item 2 Time points measured: 15 and 29 days of treatment. Time points reported: 29 days of treatment. Subgroups: none Adverse events How measured: throughout the follow‐up using a questionnaire Time points measured: all through follow‐up Time points reported: narratively Subgroups: none Other outcomes reported in the review: standardized self‐rating questionnaire using continuous 10 cm VAS: 0 absent to 10 maximum intensity), Dyspeptic Discomfort Score (DSS) and CGI |
|
| Funding | This study was supported by Dr Willnar Schwabe Pharmaceuticals, Karlsruhe, and Spitzner Pharmaceuticals, Ettlingen, Germany. | |
| Declaration of interest | Non reported | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated randomization procedure in blocks of four was used." |
| Allocation concealment (selection bias) | Low risk | "The randomization schedule was known only to the sponsors packaging unit." "Treatment allocation was concealed from all investigators, but in case of an emergency the investigators had access to sealed envelopes containing the treatment code." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The study drugs were indentical in all aspects of their appearance." "Treatment allocation was concealed from all investigators, but in case of an emergency the investigators had access to sealed envelopes containing the treatment code.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded using placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were available for nearly all participants (with the exception of 19 (?) withdrawals) for all results. |
| Selective reporting (reporting bias) | Unclear risk | Dyspeptic Discomfort Score (DDS) values are not reported. No registry available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Mohtashami 2015.
| Study characteristics | ||
| Methods |
Study design: randomized placebo‐controlled clinical trial Study dates: 2014 Setting and number of centres: outpatient, single‐centre, national Country: Iran |
|
| Participants |
Inclusion criteria: diagnosis of functional dyspepsia by Rome III criteria and confirmed by upper gastrointestinal endoscopy. Exclusion criteria: organic causes of dyspepsia, peptic ulcer disease, inflammatory bowel disease or pure gastroesophageal reflux disease, history of taking H pylori eradicating medication in previous 3 months or any gastrointestinal surgery, clinical history of any underlying disease such coronary heart disease, diabetes mellitus, asthma, chronic obstructive pulmonary disease, cancer or taking any routine medication such as corticosteroids, iron or calcium supplements and antibiotics. Sample size: 70 randomized Withdrawals: 5 (intervention (2) and placebo (3): not fully adhering to the protocol, taking other medication) Age (mean, SD years): Group 1 (42.3 ± 13.85); Group 2 (36.31 ± 13.64) Ethnicity by group: not stated Sex (M/F): Group 1 (17 M/18F) Group 2 (18 M/17 F) Symptom severity at baseline: Hong Kong Index of Dyspepsia Severity Group 1: 28.08 ± 8.11; Group 2: 29.74 ± 8.05 |
|
| Interventions |
Group 1 (n = 35): intervention. Honey based formulation of N sativa, 5 ml orally daily (the formulation was made according to traditional product instructions through mixing the N sativa oil honey and water with 1:1:1 ratio). Group 2 (n = 35): placebo. 5 ml orally daily (formulation was made Mineral oil to honey and water 1:1:1 ratio + 0.1 ml of a mixture consisting of chlorophyll and red chilli pepper extract in equal proportions dissolved in oil was added to 100 ml of mineral oil) Co‐interventions: famotidine |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Hong Kong Index of Dyspepsia Severity Time points measured: 2nd, 4th and 8th weeks Time points reported: 2nd, 4th and 8th weeks Subgroups: H pylori eradication Adverse events How measured: as related to the intervention Time points measured: after 8 weeks Time points reported: after 8 weeks Subgroups: none Quality of life How measured: Short form (SF‐36) health survey (subdivided into items) Time points measured: before and after 8 weeks Time points reported: before and after 8 weeks Subgroups: none Other outcomes reported in the review: serum biochemistry profile including fasting blood sugar, lipid profile, liver and kidney function tests and complete blood count |
|
| Funding | Baqiyatallah University of Medical Sciences, Tehran, Iran (Grant number: 22‐340/s) | |
| Declaration of interest | Declared no conflict of interest | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized list using Microsoft Excel with a method of randomization in block, carried out by the secretary. |
| Allocation concealment (selection bias) | Low risk | "The physicians, reseachers, and statisticians were blind to the allocation of patients". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Based on the same shape and size of the drug and placebo packages and similarity in color and taste, patients were blind to drug allocation". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The physicians, reseachers, and statisticians were blind to the allocation of patients". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were available for nearly all participants (with the exception of five withdrawals from 70 randomized participants) for all results. |
| Selective reporting (reporting bias) | Low risk | The primary and secondary outcomes declared in the registry (IRCT201505031157N11) were reported in the article. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Panda 2020.
| Study characteristics | ||
| Methods |
Study design: parallel group randomized trial Study dates: August 2019 to October 2019 Setting and number of centres: outpatients, one centre, national Country: India |
|
| Participants |
Inclusion criteria: participants fulfilling Rome III criteria for functional dyspepsia aged 18 to 55. People with at least 1 of the following 2 symptoms for at least 6 months before the inclusion in this study: post‐prandial fullness, early satiety; or people with 2 or more of the following symptoms at a moderate or severe level within the previous 3 months (at least 1 symptom of postprandial fullness, upper abdominal bloating or early satiety should be included), upper abdominal pain, upper abdominal discomfort, postprandial fullness, upper abdominal bloating, early satiety, nausea, or vomiting. Female participants were included if willing to use effective contraception during the study and willing to undergo a pregnancy test. Exclusion criteria: pregnant and lactating women. People having heartburn as the most bothersome symptom or if they had moderate or severe heartburn during the baseline period. History of peptic ulcer or gastroesophageal reflux disease (GERD). Current prominent symptoms of irritable bowel syndrome. Subjects who have had a previous gastrointestinal surgery except for appendectomy and laparoscopic cholecystectomy. Use of aspirin or other non‐steroidal anti‐inflammatory drugs antibiotics, H2 receptor blockers, bismuth or proton pump inhibitors and prokinetics in the preceding two weeks. Participation in other clinical trials within the last 1 month. Evidence or history of clinically significant (in the judgment of the Investigator) hematological, renal, endocrine, pulmonary, gastrointestinal, cardiovascular, hepatic, neurologic diseases or malignancies. People with alcohol abuse (daily alcohol intake more than 40 g), drug dependence or neuropsychiatric disorders that are difficult to control, as well as others who are not appropriate to participate in a drug trial. Person with a known history of hypersensitivity to any ingredient of investigational product. Any medical condition deemed exclusionary by the Principal Investigator. People with a history of drug and/or alcohol abuse at the time of enrollment. Sample size: 50 Withdrawals: none Age (mean years): Group 1 (Study): 42.12 ± 9.23; Group 2 (Control) 43.16 ± 8.69 Ethnicity by group: not available Sex (M/F): the only information available is that both sexes were included. Symptom severity at baseline: overall treatment efficacy (OTE) score: "There were no significant differences in age, height, weight, body mass index (BMI) and in dyspeptic symptoms scores at baseline between the groups.” Exact numbers not stated. |
|
| Interventions |
Group 1 (n = 25): OLNP‐06, 200 mg twice daily before meals. Ginger (Zingiber officinale) extract standardized to have 26% of total gingerols. The total gingerols composed of 6‐gingerol, 8‐gingerol, 10‐gingerol, 6‐shogoal, 8‐shogoal and 10‐shogoal. Group 2 (n = 25): placebo 200 mg twice a day. Co‐interventions: none described. |
|
| Outcomes |
Global symptoms of dyspepsia How measured: overall treatment efficacy (OTE) score (% of improvement from baseline): 7‐point Likert scale. Participants were asked ‘How were your stomach symptoms during the last week in comparison to the baseline period?’ Participants scored as either extremely improved, improved, slightly improved, not changed, slightly aggravated, aggravated, and extremely aggravated. The improvement/responder rate was calculated by combining the percentage of participants who scored ‘extremely improved’ or ‘improved’. Time points measured: on day 1, day 14, and day 28 Time points reported: on day 1, day 14, and day 28 Subgroups: none Adverse events How measured: reporting of adverse events, clinical laboratory assessment, vital signs and physical examination. The entire population under treatment was included in the safety analysis. A complete medical history was taken during the screening period and updated throughout the study period at each visit. Time points measured: on day 1, day 14 and day 28. Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: elimination rate (score 0) for each individual symptom and for the 3 major symptoms. |
|
| Funding | The research was funded by Olene Life Sciences Private Limited, Chennai who manufactured OLNP‐06. Neither the funding agency nor any outside organization has participated in study design or have any competing of interest. Olene life Sciences had final approval of the manuscript. | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “After selection, the subjects were randomly distributed into two groups;” “The subjects were randomized into two different arms to receive either OLNP‐06 or placebo and were requested to visit the study site on day 1, day 14 and day 28.“ The sequence generation is unclear. |
| Allocation concealment (selection bias) | Unclear risk | The method for allocation concealment is not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | It is unclear if participants and/or personnel were blinded. The study only states: "This was a randomized, double‐blind, placebo controlled, parallel‐group, comparative study." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded with the use of placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data were available. There were 2 dropouts, 1 in each group. |
| Selective reporting (reporting bias) | Low risk | Primary and secondary outcomes in the study protocol were the same (CTRI/2019/09/021019). |
| Other bias | Low risk | No other sources of bias were detected. |
Pasalar 2015.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: November 2013 Setting and number of centres: outpatients Country: Iran |
|
| Participants |
Inclusion criteria: Rome lll criteria for functional dyspepsia Exclusion criteria: steatorrhoea; coeliac disease; night diarrhea; beginning of FD after the age of 40 years; cancer (any form); liver disease; pulmonary disease; auto‐immune disease; psychiatry disease; pregnanc; lactation; IBS; history of abdominal surgery; treatment with Lactolose or similar drugs; consumption of drugs contributed to FD simultaneously; consumption of analgesic or narcotic drugs Sample size: 160 randomized Withdrawals: treatment group lost 12 participants during follow‐up: adverse events (n = 5); participant wished to withdraw (n = 6); other (n = 1); control group lost to follow‐up (n = 15): adverse events (n = 2); participant wished to withdraw (n = 11); other (n = 2) Age (mean, SD years): Group 1 study (80): 36.51 ± 11.71; Group 2 (80): 39.33 ± 11.56 Ethnicity by group: absolute numbers and % Fars: Study group 60 (75.0); Control group 51 (63.8) Lors: Study group 11 (13.8); Control group 23 (28.8) Turk: Study group 9 (11.2); Control group 6 (7.4) Sex (M/F) Group 1 (Study): 22 M/58 F Group 2 (Control): 24 M/56 F Symptom severity at baseline: self‐reported stress and/or self‐reported food‐related dyspepsia symptoms were rated the most bothersome causes of FD symptoms in both groups. The rates did not differ between the two groups, mean score results are not available. |
|
| Interventions |
Group 1 (n = 80): 15 ml of jollab 3 times a day every day for 4 weeks, 45 ml in total. Jollab consists of a mixture of rose water, saffron, white rock candy, and water. Every 15 ml of jollab consisted of 10.5 ml rose water, 15 mg saffron, 9.25 g white rock candy, and 3.75 ml water. Group 2 (n = 80): placebo 15 ml 3 times a day every day for 4 weeks Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: relief in gastrointestinal symptoms in functional dyspepsia patients assessed by Leeds Questionaire Time points measured: baseline and day 7, 14, 21 and 28 Time points reported: baseline and day 7, 14, 21 and 28 Subgroups: none Adverse events How measured: printed diaries were given to the participants to record any side effects. They were also given the telephone number of the first author so that they could report side effects in emergency situations. All participants underwent a physical examination, and results of their clinical laboratory tests and electrocardiograms were evaluated both in the screening period (baseline visit) and at the end of the treatment (visit 3). Time points measured: Day 7, 14, 21 and 28 Time points reported: Day 7, 14, 21 and 28 Subgroups: none Quality of life How measured: protocol says quality of life assessed using SF‐36, but that is not reported in this paper Other outcomes reported in the review: none |
|
| Funding | Shahid Beheshti University of Medical Science | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization was performed using a computer‐generated program, and a random number was allocated to each patient by an independent clinical research coordinator.” |
| Allocation concealment (selection bias) | Low risk | "The patients were recorded on a list together with the random number allocated to each of them, and the list was concealed from the researchers" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “To ensure adequate blinding of all personnel and patients, these randomization codes were not examined until the end of the trial” “The patients were recorded on a list together with the random number allocated to each of them, and the list was concealed from the researchers.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “To ensure adequate blinding of all personnel and patients, these randomization codes were not examined until the end of the trial.” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 12/80 and 15/80 participants were lost during the follow‐up in the intervention and control group respectively. Missing data were handled using the last observed–carried forward method. |
| Selective reporting (reporting bias) | High risk | The study protocol states that depression and quality of life are secondary outcomes, but these variables were not reported in the article. |
| Other bias | Low risk | None noticed. |
Puttapitakpong 2016.
| Study characteristics | ||
| Methods |
Study design: parallel‐group single‐blind randomized trial Study dates: not available Setting and number of centres: not available Country: not available |
|
| Participants |
Inclusion criteria: symptom of dyspepsia and underwent esophagogastroduodenoscopy which revealed no ulcer or lesion explain the symptoms. Exclusion criteria: not available Sample size: 34 randomized Withdrawals: (number and reasons): not available Age (years): not available Ethnicity by group: not available Sex (M/F): not available Symptom severity at baseline: not available |
|
| Interventions |
Group 1 (n = 12):Curcuma longa Group 2 (n = 10): omeprazole Group 3 (n=9): placebo Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: severity of dyspepsia assessment Time points measured: at baseline, 2 weeks and 6 weeks Time points reported: at baseline, 2 weeks and 6 weeks Subgroups: unclear Adverse events How measured: not available Quality of life How measured: not measured Other outcomes reported in the review: satisfaction score and pain score. |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | Abstract only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not available ‐ abstract only |
| Allocation concealment (selection bias) | Unclear risk | Not available ‐ abstract only |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not available ‐ abstract only |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not available ‐ abstract only |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not available ‐ abstract only |
| Selective reporting (reporting bias) | Unclear risk | Not available ‐ abstract only |
| Other bias | Unclear risk | Not available ‐ abstract only |
Rafieian‐Kopaei 2005.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: unknown Setting and number of centres: single‐centre, outpatient, national Country: Iran |
|
| Participants |
Inclusion criteria: Rome III criteria for functional dsypepsia. Exclusion criteria: peptic ulcer disease, having symptoms related to irritable bowel syndrome, biliary disease, pregnancy, daily intake of non steroidal anti‐inflammatory drugs (NSAIDs), bismuth, and antibiotic, intake of H2‐blockers or proton pump inhibitors were excluded. Patients with organic causes of gastroparesis (e.g. diabetes mellitus) and other serious diseases (including drug dependencies, any bowel surgery or malignancy) and patients having mild dyspepsia were also excluded. Sample size: 200 randomized Withdrawals: unclear “five patients from placebo group and two patients from Shaspram treated group did not follow the four‐week study procedures and dropped out. These patients were substituted with new participants” Age (mean years): Group 1 42 ± 11; Group 2 39 ± 11 Ethnicity by group: not stated Sex (M/F) Group 1 (Study); 40 M/60 F Group 2 (Control) 30 M/70 F Symptom severity at baseline: number of participants Group 1: mild 0; moderate 52; severe 43; very severe 5 Group 2: mild 0; moderate 46; severe 48; very severe 6 |
|
| Interventions |
Group 1 (n = 100): 30 drops or 1.5 gr of Shaspram 30 minutes before lunch and dinner. (Ocimum Basilicum) Group 2 (n = 100): placebo, drops or dry extract, 30 minutes before dinner and lunch. 30 drops or 1.5 gr Co‐interventions: none |
|
| Outcomes |
Adverse events How measured: participants were visited by the gastroenterologist every 8 to 10 days for four weeks for a check‐up Time points measured: days 7, 14, 21 and 28 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: score divided by symptoms. Symptoms obtained from participants were designated as mild (1 to 13), moderate (14 to 26), severe (27 to 39), and very severe (39 to 52), based on the total dyspepsia score of 52.9. Results of Shaspram treated and placebo groups before and after treatment are compared using c 2 test. |
|
| Funding | Shahrekord University of Medical Sciences, for financial support of the study. | |
| Declaration of interest | Not available | |
| Notes | Only adverse events were usable. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation is not clearly stated. |
| Allocation concealment (selection bias) | High risk | “The gastroenterologist prescribed the drugs with codes of 1 or 2, without of being aware of the contents until the end of the study” ‐ "Only five patients from placebo group and two patients from Shaspram treated group did not follow the four‐week study procedures and dropped out. These patients were substituted with new participants." ‐ some of the allocation could have violated the random allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “The gastroenterologist prescribed the drugs with codes of 1 or 2, without being aware of the contents until the end of the study.” ‐ personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded using placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Nearly complete data were available; there were 7 dropouts, and they were replaced with more participants. |
| Selective reporting (reporting bias) | Unclear risk | Each outcome was reported, but the protocol/registry was not available. |
| Other bias | Low risk | No other sources of bias were identified. |
Rich 2017.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: February 1998 to December 1999 Setting and number of centres: outpatients, multicentre. Country: Germany |
|
| Participants |
Inclusion criteria: participants with functional dyspepsia persisting for at least 6 months and the current episode lasting for at least 1 week with symptom severity requiring treatment. The sum of intensity scores of Nepean Dyspepsia Index ≥ 8 points. Rome lll criteria for functional dyspepsia with no evidence for structural causes of symptoms based upon upper gastrointestinal endoscopy (including biopsy and Helicobacter pylori testing), abdominal sonography and blood tests. Exclusion criteria: gastro‐esophageal reflux disease (GERD) grade I to IV, functional dyspepsia from reflux type or predominantly symptoms of GERD (eg, heartburn, acid regurgitation) or irritable bowel syndrome. Sample size: 114 participants Withdrawals: 8: 5 participants in the active group (8.6%) and 3 participants in the placebo group (5.4%) discontinued treatment before the end of week 4. The most frequent reason was lack of efficacy (active 4, placebo 3). Age (mean ± SD years): Group 1 (Study): mean age 46.6 ± 14.3; Group 2 (Control) mean age 48.5 ± 14.3 Ethnicity by group: not reported Sex (M/F): Group 1 (Study): 24/34; Group 2 (Control): 27/39 Symptom severity at baseline: Nepean Dyspepsia Index (NDI) total score (mean ± SD) Group 1 (Study): 342.3 ± 172.8 (n = 46) Group 2 (Control): 395.4 ± 187.3 (n = 45) |
|
| Interventions |
Group 1 (n = 53): 90 mg peppermint oil (Mentha piperita L.; WS® 1340) and 50 mg caraway oil (Carum carvi; WS® 1520) per capsule. Once a day both together for 4 weeks Group 2 (n = 53): placebo once a day, 2 pills together for 4 weeks Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: 2 predefined summary scores were computed by adding up the intensity ratings of upper gastrointestinal symptoms assessed by the NDI as co‐primary outcome measures of treatment efficacy: (a) a pain intensity score summarizing the items “pain or ache in upper abdomen,” “discomfort in upper abdomen,” “cramps in upper abdomen,” and “bloating in upper abdomen,” and (b) a discomfort intensity score computed from the items “pressure in upper abdomen” and “fullness after eating or slow digestion.” and NDI symptom score. Time points measured: baseline, after weeks 2 and 4. Time points reported: baseline, after weeks 2 and 4. Subgroups: none Adverse events How measured: participants were questioned for adverse events in each visit. Time points measured: baseline, after weeks 2 and 4. Time points reported: cumulative incidence Subgroups: none Quality of life How measured: Nepean Dyspepsia Index (NDI) (by subitem) Time points measured: baseline, after weeks 2 and 4. Time points reported: baseline, after weeks 2 and 4. Subgroups: none Other outcomes reported in the review: NDI epigastric pain syndrome; NDI postprandial distress syndrome (PDS); frequency of pain (VAS); pressure/heaviness/ fullness; global improvement (CGI, item 2) ‐ “very much improved” |
|
| Funding | The reported study, as well as medical writing services for an initial draft manuscript, was funded by Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany | |
| Declaration of interest | GR, AS, and NK have nothing to declare; PF, BS, and SK are employees of Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany; GH has received honoraria and travel reimbursement from Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization was performed in permuted blocks with a ratio of 1:1 (stratified by center) by a biostatistician otherwise not involved in the trial, using validated random number generator software. Each patient was to receive the lowest yet unassigned number available at the center.” |
| Allocation concealment (selection bias) | Low risk | “Randomization was performed in permuted blocks with a ratio of 1:1 (stratified by center) by a biostatistician otherwise not involved in the trial, using validated random number generator software. Each patient was to receive the lowest yet unassigned number available at the center.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “Double‐blind, multicenter trial, 114 outpatients with chronic or recurrent FD were randomized.” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Medication or an identically appearing placebo.” Participants were blinded by the use of placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data are unavailable. |
| Selective reporting (reporting bias) | Unclear risk | Declared outomes have been reported, but the register is unavailable. |
| Other bias | Low risk | No other sources of bias were identified. |
Rosch 2002.
| Study characteristics | ||
| Methods |
Study design: factorial parallel‐group randomized trial Study dates: February 1997 to June 1999 Setting and number of centres: multicentre, national, outpatient Country: Germany |
|
| Participants |
Inclusion criteria: male or female outpatients, 21 to 70 years old; clinical diagnosis of functional dyspepsia of the dysmotility type, relapsing or with symptoms for over 6 months; 2 or more of the symptoms of the Gastrointestinal Symptom Score (GIS) had to be classified as moderate or more (exclusive the symptoms ‘acidic eructation/heartburn’ and ‘retrosternal pain’); echosonography of upper abdomen and endoscopy of the upper gastrointestinal tract did not show relevant disorders; written informed consent of the participant Exclusion criteria: known organic disease which could have explained the dyspeptic symptoms; reflux esophagitis, gastrointestinal tumours or findings suspicious of tumours, gastric or duodenal ulcer, acute erosive gastritis/duodenitis with more than 5 erosions; Whipple’s disease, diverticulitis, polyposis coli, ulcerative colitis, Crohn’s disease, diabetic or infectious enteropathy, food allergies, malabsorption, maldigestion; bulbus scars as signs of chronic ulcer; predominance of symptoms of an irritable bowel disease; relevant defecation frequency anomalies; mesenteric vascular disorders; cholecystitis, cholangitis; pancreas tumours, pancreatitis; thyroid disorders; relevant hepatic disea; diseases of the urogenital system; history of abdominal surgery (with exception of appendectomy, hysterectomy or cholecystectomy, when at least 6 months before study start, without complications and without connection to dyspeptic symptoms); history of gastrointestinal ulcers; abuse of laxatives, regular intake of NSAIDs; concomitant medication influencing the gastrointestinal tract Sample size: 186 Withdrawals: 10 STW‐5 group: adverse event (2) STW 5‐II group: participant's request (1); personal reasons (1) Cisapride group: participant's request (2); adverse event (3); lost to follow‐up (1) Age (mean, SD years) Group 1 (STW‐5): 44.2 ± 14.3; Group 2 (STW 5‐II): 42.9 ± 13.2; Group 3 (Cisapride): 47.9 ± 15.2 Ethnicity by group: not stated Sex (M/F): Group 1 (STW‐5): 29/32; Group 2 (STW 5‐II): 24/37; Group 3 (Cisapride): 24/37 Symptom severity at baseline: GIS sum score Group 1 (STW‐5): 14.3 ± 4.9; Group 2 (STW 5‐II): 13.9 ± 4.0; Group 3 (Cisapride): 14.0 ± 4.1 |
|
| Interventions |
Group 1 STW‐5 (n = 61): 20 drops of STW 5 plus cisapride‐placebo 3 times a day. STW‐5 composition: contains alcoholic extracts of Iberis amara, Angelicae radix, Cardui mariae fructus, Chelidonii herba, Liquiritiae radix, Matricariae flos, Melissae folium, Carvi fructus, and Menthae piperitae. Group 2 TW 5‐II (n = 61): 20 drops of STW 5‐ll plus cisapride‐ placebo 3 times a day. STW‐ll composition: Does not contain Angelicae radix, Cardui mariae fructus, and Chelidonii herba. Contains higher concentrations of the other plant extracts. Group 3 Cisapride (n = 61): tablet containing 10 mg cisapride plus 20 drops STW 5/5‐II‐placebo 3 times a day. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: GIS Time points measured: day –7, Day 0, Day 14 and Day 28 Time points reported: day –7, Day 0, Day 14 and Day 28 Subgroups: “STW 5 and STW 5‐II showed a trend towards a higher efficacy than cisapride in the patients with a family history of functional dyspepsia” Adverse events How measured: adverse effects were assessed in each of the first 4 visits. Time points measured: Day –7, Day 0, Day 14 and Day 28 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: global efficacy evaluations by investigator and participant. |
|
| Funding | Steigerwald Arzneimittelwerk GmbH, Darmstadt. | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A random code based on the method of permuted blocks with a block size of three was prepared in advance. This code allocated the patients randomly and symmetrically to the three treatment groups (STW 5, STW 5‐II, cisapride).” |
| Allocation concealment (selection bias) | Low risk | “Because STW 5 and STW 5‐II are liquid preparations and cisapride was only available as tablets, in this study a double‐dummy method was used. The placebos used were identical in appearance to the corresponding active medication and could not be distinguished from it.” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “Patients, investigators, and study centres maintained strict blinding throughout the study." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Patients, investigators, and study centres maintained strict blinding throughout the study. The random code was not known and could not be accessed by anyone involved in study performance, study management, or data analysis” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data for every outcome were reported; 10/186 participants were lost. |
| Selective reporting (reporting bias) | Unclear risk | Every outcome was reported. However, certain subgroup analyses were not reported. Registry was unavailable. |
| Other bias | Low risk | No other sources of bias were identified. |
Salem 2010.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: 2007 to 2008 Setting and number of centres: outpatient, single‐centrer, national. Country: Saudi Arabia |
|
| Participants |
Inclusion criteria: people with complaints of dyspeptic symptoms and positive results for H pylori infection by histopathology and rapid urease test Campylobacter‐Like Organism (CLO) test (2 positive results). Exclusion criteria: 1) the endoscopy showed peptic ulcer, gastric cancer or gastrointestinal bleeding; 2) they had taken proton‐pump inhibitors, bismuth or antibiotics in the last four weeks before endoscopy; 3) they were pregnant or lactating; 4) they were intolerant or allergic to therapeutic regimens, or 5) they failed to report for follow‐up. Sample size: 110 randomized; 88 complete the protocol Withdrawals: Group 1: 2 excluded; Group 2: 3 excluded; Group 3: 3 excluded; Group 4: 2 excluded (reason not given). Loss to follow‐up: Group 1: 2; Group 2: 6; Group 3: 2; Group 4: 2 Age (mean ± SD years): Group 1 (41.7 ± 14.7); Group 2 (43.5 ± 14.6); Group 3: (43.5 ± 9.9); Group 4: (40.8 ± 11.9) Ethnicity by group: not stated. Sex (M/F): Group 1 (8/15); Group 2 (8/13); Group 3 (5/16); Group 4: (11/12) Symptom severity at baseline: not available |
|
| Interventions |
Group 1 (n = 27): triple therapy comprising of clarithromycin (500 mg twice daily), amoxicillin (1 gr twice daily for 1 week) and the co‐intervention (omeprazole) Group 2 (n = 30): 1 g Nigella sativa seed (1 capsule twice daily after meals) for 4 weeks Group 3 (n = 26): 2 g Nigella sativa seed (2 capsules twice daily after meals) for 4 weeks Group 4: (n = 27): 3 g Nigella sativa seed (2 capsules thrice daily after meals) for 4 weeks Nigella sativa: obtained from BioExtract (Pvt.) Ltd., Sri Lanka, and each capsule contained 500 mg of ground N sativa L seeds. The doses of 1, 2 and 3 g/d were considered safe in light of the acute and chronic toxicity studies of N sativa fixed oil and of thymoquinone (the active ingredient in N sativa) in mice. Co‐interventions: omeprazole 40 mg daily for 4 weeks |
|
| Outcomes |
Global symptoms of dyspepsia How measured: simplified adaptation of Short‐form Leeds Dyspepsia Questionnaire Time points measured: weekly by phone for 4 weeks Time points reported: narratively Subgroups: none Adverse events How measured: follow‐up information regarding improvement of the dyspeptic symptoms, appearance of side effects and compliance of the participants was documented in the hospital file of each participant. Time points measured: end of weeks 1, 2, 3 and 4 Time points reported: cumulative incidence Subgroups: none Quality of life How measured: not measured Other outcomes reported in the review: Other outcomes reported in the review: eradication of H pylori (primary outcome). |
|
| Funding | Not reported | |
| Declaration of interest | Not reported | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not specified. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label study |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 88/110 randomized participants completed the study and were analyzed (per‐protocol analysis). |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
Sastry 2016.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: unknown Setting and number of centres: unicentre, outpatient Country: India |
|
| Participants |
Inclusion criteria: males and females between 12 and 60 years of age suffering from functional dyspepsia i.e. indigestion and its related signs and symptoms such as fullness, bloating, nausea, gassy discomfort loss of appetite, spasm and pain in the chest or abdomen for at least on 2 occasions in the preceding week and with normal hepatic and renal functions were included Exclusion criteria: People with persistent dyspepsia, vomiting, severe epigastric pain, unintentional weight loss, iron deficiency anaemia, gastrointestinal bleeding, dysphasia, odynophagia, previous gastric surgery, epigastric mass, suspicious barium meal, peptic ulcer and NSAID use. Organic deformity or malignancy of the gastrointestinal tract, significant systemic and psychological condition (s) which may hamper the study proceedings, conditions requiring immediate surgical intervention, known hypersensitivity to study product or its ingredients, concomitant medications known to adversely interact with study products or their ingredients, alcohol or drug abuse, pregnancy, lactation and females planning to conceive in near future were excluded Sample size: 90 Withdrawals: 11. None discontinued treatment because of adverse events Age (mean ± SD years): Group 1 (Pudin Hara Pearl) 32.97 ± 1.92; Group 2 (Pudin Hara Liquid) 34.31 ± 10.99 Ethnicity by group: not reported Sex (% female): Group 1 (Pudin Hara Pearl): 72.10%; Group 2 (Pudin Hara Liquid): 58.33% Symptom severity at baseline: Global Evaluation of Symptoms Therapeutic Response Group 1 (Pudin Hara Pearl): 11.41 ± 6.45; Group 2 (Pudin Hara Liquid): 11.50 ± 5.68 |
|
| Interventions |
Group 1 (n = 43): Pudin Hara Pearls 1 capsule orally three times a day after meals. Group 2 (n = 36): Pudin Hara Liquid 10 drops, orally three times a day after meals. Each 180 mg of Pudin Hara Pearls comprises of Mentha oil (Mentha piperata, Aerial part, Ol.) ‐ 0.174 ml and spearmint oil (Mentha spicata, Aerial part, Ol.) ‐ 0.034 ml along with excepients, preservatives and colors. Each 1 ml (20 drops approx) of Pudin Hara Liquid comprises Pudinah Satva (Mentha piperata, Aerial part, Ol. ) ‐ 0.0337 ml along with excepients, preservatives and colors Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Global Evaluation of Symptoms Therapeutic Response (Subjective Symptoms of Dyspepsia) Time points measured: baseline and days 1 to 5 Time points reported: baseline and days 1 to 5 Subgroups: none Adverse events How measured: reported each day Time points measured: days 1 to 5 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: individual symptoms of dyspepsia. |
|
| Funding | Dabur India Limited | |
| Declaration of interest | Authors JLN Sastry, Sasibhushan Vedula and Sunil Kumar are currently employed with Dabur India Limited which manufactures/ markets study products Pudin Hara Liquid and Pudin Hara Pearls | |
| Notes | Not blinded | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomization was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not specified. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Open‐label study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Most of the data were available; 11/90 participants were lost. |
| Selective reporting (reporting bias) | Unclear risk | The registry is poorly described: CTRI/2017/08/009227. |
| Other bias | Low risk | No other sources of bias were detected. |
Sattarzadeh 2021.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: unknown Setting and number of centres: unicentre, outpatient Country: Iran |
|
| Participants |
Inclusion criteria: age between 18 and 60 years old, both sexes, FD diagnosed based on the Rome IV Diagnostic Criteria, negative test result regarding H pylori status (confirmed by endoscopic examination), not taking chemical or herbal medications from two weeks before beginning the study, and informed consent signed. Exclusion criteria: diagnosed with dyspepsia along with dominant symptoms of heartburn; warning signs (including weight loss) hematemesis, pitch‐like stools or iron‐deficiency anaemia, dysphagia or odynophagia, frequent vomiting or return of the food, abdominal mass, lymphadenopathy or ascites, family history of gastric malignancies in the first‐degree relatives as well as IBD; gastritis; duodenitis; peptic ulcer; reflux (the most important complaint); taking nonsteroidal anti‐inflammatory drugs or corticosteroids for more than a month; taking other herbal and chemical medications for the treatment of dyspepsia; obstruction of the gastrointestinal tract in the endoscopy; the presence of malignant tumours in the gastrointestinal tract; history of gastric surgery; body mass index (BMI) above 30; pregnancy and lactation; smoking and consumption of alcohol and drugs; chronic heart, kidney, liver, and gallbladder diseases; diabetes; and other metabolic diseases causing the dyspepsia. Sample size: 63: 28 participants were considered for each group taking into account the alpha error of 0.05 and the study power of 80% to observe the effect size of 75% (for the four symptoms of dyspepsia). Withdrawals: 3 in total Grup 1: 1 due to difficulty in commuting Group 2: 2, 1 due to difficulty in commuting, another due to colon cancer diagnosis. Age (mean ± SD years) Group 1: 37.34 ± 2.43 Group2: 35.87 ± 3.20 Ethnicity by group Not stated Sex (M/F) Group 1: 5 M/27 F Group2: 23 M/ 8 F Symptom severity at baseline: (mean± SD) Only available divided in symptoms Group 1: postprandial fullness 7.37 ± 0.16; early satiation 7.71 ± 1.59; epigastric pain 6.64 ± 0.57; epigastric burning 6.33 ± 0.50 Group 2: postprandial fullness 7.47 ± 0.50; early satiation 6.44 ± 0.90; epigastric pain 6.60 ± 2.70; epigastric burning 6.35 ± 0.81 |
|
| Interventions |
Group 1: 134 g of mastic gum with 536 g of sesame oil for topical application as a massage Group 2: placebo (sesame oil) Co‐interventions: both branches received pantoprazole (40 mg daily). |
|
| Outcomes |
Adverse events How measured: reported at each follow‐up Time points measured: baseline, week 1, 2,3 and 4. Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: individual symptoms of dyspepsia including the severity of early satiation, postprandial fullness, epigastric pain, and epigastric burning; (all of them measured with visual analogue scale), patients’ satisfaction was measured with TSTMQ (treatment satisfaction with traditional medicines questionnaire) |
|
| Funding | Not available. | |
| Declaration of interest | The authors declare they do not have any conflict of interest. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Block randomization method was used to randomly assign the subjects into two groups. After selecting the four blocks randomly, random list was prepared by the statistical consultant and given to the executor" |
| Allocation concealment (selection bias) | Low risk | "Closed envelopes were used for allocation concealment, with the patient’s number written on the envelope and type of intervention in the envelope." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The treatments were presented as A and B with the same shape and appearance in order to blind the patients, executor, and analyst. Closed envelopes were used for allocation concealment, with the patient’s number written on the envelope and type of intervention in the envelope." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No other information stated beyond 'triple‐blind controlled trial'. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Nearly complete data were available. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | None other sources of bias were identified. |
Shin 2021.
| Study characteristics | ||
| Methods |
Study design: randomized double‐blind placebo‐controlled trial Study dates: unknown Setting and number of centres: unicentre, outpatient Country: Korea |
|
| Participants |
Inclusion criteria: adults aged between 20 and 70 years; 1 gastrointestinal symptom, such as bloated after meals, early satiety, epigastric area pain, burning in the upper abdomen, which started at least 6 months before the study and has been occurring for 3 months according to the Rome IV criteria; without evidence of structural lesions in the upper gastrointestinal system on endoscopy; at least 4 symptoms with moderate or severe intensity among 10 items of the gastrointestinal symptom scale (GIS) in the last 2 weeks; agreement to participate in the study and a signed written consent form. Exclusion criteria: malignancy, stroke, or cardiovascular disease that was being treated or not being controlled; Pregnant, lactating, history of ulcers in the last six months, gastrointestinal surgery, heavy drinkers (male 14 units and female 7 units), or taking an H2‐receptor inhibitor, corticosteroids, non‐steroidal anti‐inflammatory drug, or aspirin; Uncontrolled hypertension, uncontrolled diabetes mellitus (fasting glucose level ≥180 mg/dL), abnormal results, creatinine, GOT or GPT (≥ 3 times the standard upper limit), amylase or lipase (≥ 2 times the standard upper limit), TSH, or known hypersensitivity to experimental agents Sample size: 100 participants. Considering 1:1 allocation, a power of 80%, and a type 1 error rate (alpha) of 5%, at least 37 participants in the experimental group were calculated as the appropriate number of participants in the study. The total number of participants to establish an effect was estimated to be 100, considering a 25% dropout rate. Withdrawals: 17 in total Grup 1: 11 in total (2 withdrew their consent; 1 took a prohibited medication; 8 had less than 80% compliance) Group 2: 6 in total (3 took a prohibited medication; 3 had less than 80% compliance) Age (mean ± SD years) Group 1: 39.9 ± 12.7 Group 2: 38.0 ± 12.5 Ethnicity by group Not stated Sex (M/F): Group 1 (Study): 20 M/19 F Group 2 (Control): 15 M/29 F Symptom severity at baseline: GIS mean (SD) Group 1 (Study): 19.7 (7.4) Group 2 (Control): 19.3 (6.2) |
|
| Interventions |
Group 1: 50 mg of CTE (Cudrania tricuspidata extract) for 8 weeks. Group 2: placebo Co‐interventions Other components in both branches: microcrystalline cellulose 279 mg, calcium carboxymethyl cellulose 5.25 mg, magnesium stearate 7.0 mg, silicon dioxide 5.25 mg, hydroxypropyl methylcellulose 3.50 mg) |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Rating Scale (GSRS); GIS; Nepean Dyspepsia Index (NDI‐K); Time points measured: baseline, end of week 4, and end of week 8 Time points reported: baseline, end of week 4, and end of week 8 Subgroups: none Quality of life How measured: FD‐related quality of life (FD‐QoL) Time points measured: baseline, end of week 4, and end of week 8 Time points reported: baseline, end of week 4, and end of week 8 Subgroups: none Adverse events How measured: narratively Time points measured: baseline, end of week 4, and end of week 8 Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: Laboratory test as ESR and CPR |
|
| Funding | This research was funded by Hy Co., Ltd., Yongin, South Korea, and the APC was funded by Hy. Co., Ltd., Yongin, South Korea. | |
| Declaration of interest | JYK, JJS. and J‐LL are employees of Hy. Co., Ltd. and their roles of this study reflect as researchers and do not represent their position of current or past employers. JS and THO have no financial or non‐financial competing interests to declare. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Enrolled participants were assigned to either the CTE group or control group by block randomization using the SAS® system." |
| Allocation concealment (selection bias) | Low risk | "We kept the master randomization list with the details of allocation safely and confidentially with the sponsor." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Regarding the medication and placebo: "These were identical in appearance, shape, color, and packaging." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind study (see above) ‐ participant‐reported outcomes (participants were outcome assessors) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Unbalanced attrition: At 8 weeks 11 participants were lost to follow‐up in the intervention group (8 due to poor compliance), and 6 in the control group (3 due to poor compliance). |
| Selective reporting (reporting bias) | Low risk | Each outcome was reported as described in the trial registry (KCT0005020). However, the demographics of lost participants were not included. |
| Other bias | Low risk | None detected. |
Sun 2016.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: July 2011 to November 2013 Setting and number of centres: outpatients, multicentre Country: China |
|
| Participants |
Inclusion criteria: 18 to 65 years old, Rome III criteria, normal gastroscopy, and a symptom severity score greater than 2 points. Exclusion criteria: allergic to the components of the test drug and/or excipients; a history of organic diseases of the digestive tract, angle‐closure glaucoma, a history of abdominal surgery; diabetes and hyperlipidemia that require drug control; severe primary diseases such as heart, liver, kidney and other important organs and/or hematopoietic system; use of prokinetic agents together (such as constipation, gastroparesis) and people with dyspeptic symptoms caused by severe mental or psychological factors (such as depression, anxiety, hypochondriasis, and papillary disease); pregnancy, breastfeeding women and those who have recent birth plans. Sample size: 228 Withdrawals: none Age (years, mean, SD) Group 1 (Study high dose): 42.69 ± 11.95 Group 2 (Study low dose): 39.17 ± 12.83 Group 3 (Control): 38.28 ± 10.26 Ethnicity by group: not stated Sex (M/F): Group 1 (Study high dose): 23/44; Group 2 (Study low dose): 15/51; Group 3 (Control): 23/42 Symptom severity at baseline: global assessment of symptoms at baseline (mean ± SD) Group 1 (Study high dose): 23.49 ± 7.52 Group 2 (Study low dose): 25.35 ± 9.63 Group 3 (Control): 23.77 ± 8.17 |
|
| Interventions |
Group 1 (n = 67 ): Tibetan solution gelatin, 260 mg/capsule, containing peppermint oil (90 mg), sesame oil (50 mg), tea oil (120 mg) twice a day, after lunch and dinner, for 4 weeks. (High dose) Group 2 (n = 66): Tibetan solution gelatin, 260 mg/capsule, containing peppermint oil (90 mg), sesame oil (50 mg), tea oil (120 mg) once a day, after dinner for 4 weeks. (Low dose) Group 3 (n = 65): Placebo, 260 mg capsules, containing 230 mg of tea oil once a day, after dinner for 4 weeks. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: global assessment of symptoms Time points measured: baseline, weeks 2, 4 and 6 Time points reported: baseline, weeks 2, 4 and 6 Subgroups: none Adverse events How measured: self‐reported Inquiry electrocardiogram and lab tests Time points measured: weeks 2, 4 and 6 Time points reported: cumulative incidence Subgroups: none Quality of life How measured: SF‐36 Time points measured: baseline, weeks 2, 4 and 6 Time points reported: baseline, weeks 2, 4 and 6 Subgroups: none |
|
| Funding | Not available | |
| Declaration of interest | Not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “They were randomly divided into groups A, B, and C, with 76 cases in each group” |
| Allocation concealment (selection bias) | Unclear risk | No information available. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | “Double blinded trial” ‐ unclear whether personnel were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Two unblinding methods were used. At the end of the experiment, after verifying the information of each patient, the first exposure was carried out, and groups A, B, and C were determined according to random numbers. And carry out statistical analysis; the second unblinding to determine A, B, C components and 1J as high‐dose, low‐dose, placebo group” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data at follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Other bias | Low risk | The study appears to be unaffected by other sources of bias. |
Thamlikitkul 1989.
| Study characteristics | ||
| Methods |
Study design: multicentre, randomized, double‐blind trial. Study dates: September 1987 to May 1988. Setting and number of centres: outpatient, multicentre (1 provincial hospital and 5 community hospitals in various parts of Thailand) Country: Thailand |
|
| Participants |
Inclusion criteria: 12 years old or older and inflicted with dyspepsia syndrome, acid dyspepsia, flatulent dyspepsia, or atonic dyspepsia Exclusion criteria: pregnant, had gut obstruction or severe abdominal pain, gastrointestinal infection, cholecystitis, hepatitis, pancreatitis, appendicitis, or peritonitis. Sample size: 116 included in the study. Loss to follow‐up: Group 1 3/39; Group 2/36 6; Group 3 1/41 Age (mean years): Group 1 (42); Group 2 (48); Group 3: (41) Ethnicity by group: not available Sex (M/F): Group 1 (18/21); Group 2 (19/17); Group 3: (22/19) Symptom severity at baseline: not available. |
|
| Interventions |
Group 1 (n = 39):Curcuma longa (Curcuma domestica val) (powder form of dried rhizome, 250 mg, containing 0.02 ml of volatile oil and 0.024 g of total curcuminoids per capsule) 2 capsules 4 times a day for 7 days. Group 2 (n = 36): flatulence (cascara dry extract 65 mg, nux vomica dry extract 16 mg, asofoetida tincture 0.325 mg, capsicum powder, 8 mg, ginger powder 48 mg and diastase 3 mg) for 7 days. Group 3: (n = 41): placebo (starch powder) 2 capsules 4 times a day for 7 days Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: not mentioned how global symptomatology was measured, even though the results are according to response (cured, improved, not improved, worse). Time points measured: daily by self‐report (postcard) for 7 days Time points reported: end of treatment (7 days) Subgroups: none Adverse events How measured: unclear Time points measured: daily by self‐report (postcard) for 7 days Time points reported: end of treatment Subgroups: none Other outcomes reported in the review: satisfaction and compliance of treatment |
|
| Funding | German agency for technical cooperation (GTZ) | |
| Declaration of interest | not available | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were assigned by simple randomization (no other details provided). |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment were mentioned in the article. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | It was only mentioned that all medications were in identical capsules. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded using placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study results of the 106 participants with complete follow‐up are shown (116 randomized). |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Other bias | Unclear risk | The article does not mention how the outcomes were measured. |
Vinson 2020.
| Study characteristics | ||
| Methods |
Study design: double‐blind, randomized, multicentre trial Study dates: unknown Setting and number of centres: multicentre, outpatient Country: Germany |
|
| Participants |
Inclusion criteria: FD according to ROME criteria Exclusion criteria: not available Sample size: 272, no information regarding sample size calculation is available Withdrawals: not available Age (mean ± SD years) Not available. Text only mentions that both groups are comparable. Ethnicity by group Not stated Sex (M/F) Not stated. Text only mentions that both groups are comparable. Symptom severity at baseline: GIS (mean ± SD) Group 1: (11.9 ± 3.66) Group 2: 12.1 ± 4.0 |
|
| Interventions | Group 1: 3 x 20 drops/day of STW 5‐II Group 2: same posology of placebo Co‐interventions: none |
|
| Outcomes |
Global symptoms of dypepsia How measured: Gastrointestinal Symptom Score (GIS) Time points measured: not available Time points reported: 8 weeks Adverse events How masured: narratively Time points measured: not available Time points reported: possibly at complete follow‐up |
|
| Funding | Unknown | |
| Declaration of interest | Unknown | |
| Notes | Only congress abstract is available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No informartion (only abstract available). |
| Allocation concealment (selection bias) | Unclear risk | No informartion (only abstract available). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Text only states that this is a double‐blinded study (only abstract available). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Text only states that this is a double‐blinded study (only abstract available). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only abstract is available; therefore, complete outcome data are not published. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available (only abstract available). |
| Other bias | Unclear risk | Only abstract available. |
Von Arnim 2007.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: not available Setting and number of centres: multicentre, outpatients, national Country: Germany |
|
| Participants |
Inclusion criteria: presence of “moderate” as the degree of severity for at least 3 Gastrointestinal Symptom (GIS) score, epigastric pain or discomfort was required to have persisted in a permanent or recurrent form for a minimum period of 12 wk before the initial examination. Exclusion criteria: esophagogastroduodenoscopy and other routine examinations which indicate any clinically relevant organic disease; the relief of dyspeptic symptoms exclusively through evacuation or in relation to change in stool frequency or form permitted as a clinical sign of irritable bowel syndrome. Sample size: 315 Withdrawals: 46; 15 due to adverse effects, 8 in the study group and 7 in the control group. 6 because of lack of compliance, 2 in the study group and 4 in the control group. 5 due to private reasons, 3 in the study group and 2 in the other. 12 for other reasons, 7 in the study branch and 5 in the control one. Another 8 participants were lost in the follow‐up of the last visit, 4 in each branch. Age (mean, SD, years): Group 1 (Study): 49.3 ± 15.2; Group 2 (Control): 48.9 ± 15.9 Ethnicity by group: not reported Sex (M/F): Group 1 (Study): 52/105; Group 2 (Control): 51/100 Symptom severity at baseline: GIS sum score Group 1 (Study): 11.6 ± 3.5; Group 2 (Control): 11.9 ± 4.3 |
|
| Interventions |
Group 1 (n = 158 ): 3 x 20 drops daily of STW5 for 8 weeks. Every 100 ml: alcoholic fresh plant extract (extraction agent 50% ethanol by volume) from Iberis amara totalis 1 : 2 15.0 mL alcoholic drug extracts (extraction agent 30% ethanol by volume) from Angelicae radix 1 : 3 10.0 mL Cardui mariae fructus 1 : 3 10.0 mL Carvi fructus 1 : 3 10.0 mL Chelidonii herba 1 : 3 10.0 mL Liquiritiae radix 1 : 3 10.0 mL Marticariae flos 1 : 3 20.0 mL Melissae folium 1 : 3 10.0 mL Menthae piperitae folium 1: 3 5.0 mL Group 2 (n = 157): Placebo, drops for 20 weeks. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: GIS Time points measured: baseline and after 14, 28, and 56 days. Also after 8 months. Time points reported: baseline and after 14, 28, and 56 days. Also after 8 months. Subgroups: none Quality of life Not measured Adverse events How measured: any side effects from their medications were recorded at each follow‐up. Time points measured: baseline and after 14, 28, and 56 days. Also after 8 months. Time points reported: cumulative incidence Subgroups: none Other outcomes reported in the review: secondary target variables comprised the overall efficacy and tolerability of the 8‐wk treatment with STW 5 or the placebo, assessed by investigator and participant using a 6‐point Likert scale ranging from very good (1) to very poor (6) |
|
| Funding | Steigerwald Arzneimittelwerke GmbH, Darmstadt, Germany. | |
| Declaration of interest | Dr Bettina Vinson is an employee of Steigerwald Arzneimittelwerke GmbH, Darmstadt, Germany | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Block randomization was performed over all centers without stratification. The randomization list for the study with a parallel‐group design with two independent treatment groups was elaborated using the randomization program IDVRANCODE 3.6. Block size was 4” |
| Allocation concealment (selection bias) | Low risk | “For blinding, an alcoholic tincture identical to the verum drug in organoleptic properties was manufactured. Organoleptic means that color, smell, taste, viscosity, and alcohol content are identical in the STW 5 preparation and placebo” |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “This is the largest double‐blind, randomized, placebo‐controlled multicenter study with STW 5 in F” “For blinding, an alcoholic tincture identical to the verum drug in organoleptic properties was manufactured” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The investigator’s allocation of study medication was blind, being supervised by Harrison Clinical Research GmbH, Munich.” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Most of the data for each outcome were reported. There were 46/315 dropouts |
| Selective reporting (reporting bias) | Unclear risk | Every outcome was reported that was declared in the method, but the protocol was unavailable. |
| Other bias | Low risk | No other sources of bias were detected. |
Yongwatana 2022.
| Study characteristics | ||
| Methods |
Study design: randomized, double‐blind, placebo‐controlled trial Study dates: 2017 to 2018 Setting and number of centres: national, outpatient Country: Thailand |
|
| Participants |
Inclusion criteria: 18 to 80 years diagnosed with FD according to ROME IV criteria. Organic causes were discarded by upper gastrointestinal endoscopy and Helicobacter pylori testing. Exclusion criteria: evidence of organic disease, for example, peptic ulcers; active Helicobacter pylori infection; serum total bilirubin > 2 mg/dL; anaemia (Hb < 10 g/dL); chronic kidney disease at least stage 4 (Glomerular Filtration Rate < 30 mL/min/1.73 m2); history of previous gastric surgery, gastric bypass surgery, or malignancy; history of nonsteroidal anti‐inflammatory drugs, aspirin, or other antiplatelet or anticoagulant use within four weeks before enrollment; pregnancy or lactation; and history of allergy to curcumin or omeprazole. Sample size: 132 randomized Withdrawals: none Age (years): Group 1 55.82 ± 14.62; Group 2 56.49 ± 14.44; Group 3 56.8 ± 13.1 Ethnicity by group: not available Sex (M/F): Group 1 13/32; Group 2 13/30; Group 3 13/31 Symptom severity at baseline: Severity of Dyspepsia Assessment score: Group 1 54.38 ± 8.31; Group 2 53.97 ± 8.12; Group 3 54.42 ± 6.92 |
|
| Interventions |
Group 1 (n = 45) curcumin: 1 capsule of curcumin (500 mg per capsule) 4 times daily after meals and bedtime and omeprazole placebo once daily. Group 2 (n = 43) omeprazole: 1 capsule of omeprazole once daily before breakfast and curcumin placebo 4 times daily after meals and bedtime. Group 3 (n = 44) placebo: omeprazole placebo and curcumin placebo in identical capsules. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: Severity of Dyspepsia Assessment total score Time points measured: 4 weeks Time points reported: 4 weeks Subgroups: not available Quality of life How measured: EuroQoL EQ‐5D questionnaire + EQ‐VAS (visual analogue scale). Time points measured: 4 weeks Time points reported: 4 weeks Subgroups: not available Adverse events How measured: narratively Time points measured: 4 weeks Time points reported: 4 weeks Subgroups: not available Other outcomes reported in the review: The study also reported the severity of pain and non‐pain symptoms separately (using the Severity of Dyspepsia Assessment (SODA) measured in the baseline, 2 and 4 weeks after the treatment. |
|
| Funding | Gastroenterological Association of Thailand. | |
| Declaration of interest | "The authors disclose no conflicts." | |
| Notes | It is not clear if it is a follow‐up study of Puttapitakpong 2016. We contacted Dr Kachonsak Yongwatana at: plancake86@hotmail.com. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Eligible patients were randomly assigned by a computer‐generated sequence into three groups: omeprazole group, curcumin group, or placebo group. A research assistant managed the randomization and treatment allocation of each patient. The principal investigator, laboratory staff, and patients were blinded to the allocation." |
| Allocation concealment (selection bias) | Low risk | "Eligible patients were randomly assigned by a computer‐generated sequence into three groups: omeprazole group, curcumin group, or placebo group. A research assistant managed the randomization and treatment allocation of each patient. The principal investigator, laboratory staff, and patients were blinded to the allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "In the omeprazole group, subjects received one capsule of omeprazole once daily before breakfast and curcumin placebo four times daily after meals and bedtime. In the curcumin group, subjects received one capsule of curcumin(500 mg per capsule) four times daily after meals and a bedtime and omeprazole placebo once daily. In the placebo group, subjects received omeprazole placebo and curcumin placebo in identical capsules. The study medication was given in a double‐blind fashion for 4 weeks." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "In the omeprazole group, subjects received one capsule of omeprazole once daily before breakfast and curcumin placebo four times daily after meals and bedtime. In the curcumin group, subjects received one capsule of curcumin(500 mg per capsule) four times daily after meals and a bedtime and omeprazole placebo once daily. In the placebo group, subjects received omeprazole placebo and curcumin placebo in identical capsules. The study medication was given in a double‐blind fashion for 4 weeks." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data at follow‐up. |
| Selective reporting (reporting bias) | Low risk | The outcomes match the trial registry (TCTR20171218001). |
| Other bias | Low risk | No other sources of bias were identified. |
Zobeiri 2021.
| Study characteristics | ||
| Methods |
Study design: parallel‐group randomized trial Study dates: April 2018 to May 2019 Setting and number of centres: outpatients ‐ 1 centre Country: Iran |
|
| Participants |
Sample size: 64 Inclusion criteria: Age between 18 years and 80 years, and their diseases are confirmed by complete medical evaluation, as well as people who sign the testimonials and co‐operate during the study and people who have not been treated with cinnamon oil soft capsule during the last month. Exclusion criteria: people with inflammatory bowel disease, pure gastroesophageal reflux, peptic ulcer disease, or irritable bowel syndrome; people with a history of gastrointestinal system surgery; and pregnant and breastfeeding women. Loss to follow‐up Group 1 (study): 5 participants Group 2 (control) : 8 participants Age (mean in years) Group 1 (study): 41.9 Group 2 (control): 37.63 Ethnicity by group: not stated Sex (M/F) Group 1 (study): 10 M/19 F Group 2 (control): 11 M/24 F Symptom severity at baseline: Gastrointestinal symptom score (GIS) Group 1 (study): 20.72 (mean) Group 2 (control: 21.94 (mean) |
|
| Interventions |
Group 1 (n = 29): Cinnamon oil capsule, 1 capsule 3 times a day for 6 weeks. Cinnamomum zeylanicum is a spice plant (native of Sri Lanka). 500 grams of plant’s bark coarse powder was soaked 40 days in 3.26 L sesame oil. A soft gelatin capsule was made using the rotary die process. The final capsule was standardized based on its cinnamaldehyde amount (55% to 75% of cinnamaldehyde as the significant pharmacological component of cinnamon essential oil) and analyzed by high‐performance liquid chromatography method. Group 2 (n = 35): placebo (sesame oil capsule), 1 capsule 3 times a day for 6 weeks. Obtained from Iranian white sesame seeds. Chemical composition analysis of this sesame oil showed that it contains 75 to 80% of liquid fatty acids (oleic and linoleic acids), 15% of solid fatty acids (palmitic, stearic, and arachidic acids), and 1% of lecithin. Co‐interventions: none |
|
| Outcomes |
Global symptoms of dyspepsia How measured: GIS Time points measured: baseline and after 6 weeks Time points reported: baseline and after 6 weeks Subgroups: none Adverse events How measured: throughout follow‐up Time points measured: at the complete follow‐up Time points reported: narratively Subgroups: none Other outcomes reported in the review: none |
|
| Funding | Not available | |
| Declaration of interest | The authors declare no conflicts of interest. | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the random sequence was generated and linked to the numbers assigned in each group "Odd number was allocated to an intervention group and even number was allocated to the placebo group". |
| Allocation concealment (selection bias) | Low risk | "The capsule box of both groups looked identical, so in addition to the physicians and researchers, the patients were also blinded to the drug allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The capsule box of both groups looked identical "the physicians and researchers, the patients were also blinded to the drug allocation" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The capsule box of both groups looked identical "the physicians and researchers, the patients were also blinded to the drug allocation" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition due to loss to follow‐up (5/29 and 8/35 in the active and control group, respectively). |
| Selective reporting (reporting bias) | Low risk | Data were available for all participants. |
| Other bias | Low risk | The study does not appear to be affected by other sources of bias. |
CGI: Clinical Global Impressions; CRP: C‐reactive protein; ESR: erythrocyte sedimentation rate; F: female; FD: functional dyspepsia; GERD: Gastroesophageal reflux disease; GIS: Gastrointestinal Symptom Score; GOT: glutamic oxaloacetic transaminase; GPT: glutamic pyruvic transaminase; IBD: Inflammatory bowel disease; M: male; NDI: Nepean dyspepsia index; PPI: proton pump inhibitor; RCT: randomized controlled trial; SD: standard deviation; TSH: Thyroid‐stimulating hormone; VAS: visual analogue scale; WBC: white‐blood count
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12619001236189 | Ineligible population: participants with gastrointestinal symptoms in general (not restricted to dyspepsia). |
| ACTRN12621000116820 | Ineligible study population: healthy volunteers |
| Arai 2011 | Ineligible intervention: Kampo herbal medicine |
| Arai 2012 | Ineligible intervention: Kampo herbal medicine |
| Asha 2017 | Ineligible study design: non‐randomised trial |
| Asif 2015 | Ineligible population: people with no functional dyspepsia |
| Aydin 1997 | Ineligible study design: non‐randomised trial |
| Barnick 1990 | Ineligible population: people with no functional dyspepsia |
| Bekar 2011 | Ineligible intervention: triple therapy for the erradication of Helicobacter pylori |
| Bommer 2013 | Ineligible study design: single‐arm trial of Boldocynara (a proprietary combination product consisting of artichoke leaves, milk thistle fruits, dandelion herb and root, and boldo leaves). |
| Choi 2011 | Ineligible intervention: Korean herbal medicine |
| Choi 2020 | Ineligible intervention: Chinese herbal medicine ("crude medicine for abdominal symptoms in East Asia since the Ming Dynasty of China") |
| CTRI/2022/03/041419 | Wrong patient population: diabetic gastroparesis. |
| Di 2007 | Ineligible study design: single‐arm study |
| Dimitrov 1983 | Ineligible population: people with no functional dyspepsia |
| Dos 2010 | Ineligible population: people with no functional dyspepsia |
| Du 2014 | Ineligible intervention: Chinese herbal medicine |
| Eady 2019 | Ineligible population: people with no functional dyspepsia |
| Fuhrer 2011 | Ineligible study design: this study tested capsaicin as a diagnostic test for people with dyspepsia. |
| Gao 2007 | Ineligible intervention: Chinese herbal medicine |
| Gasbarrini 2010 | Ineligible intervention: cold dessert |
| Gong 2019 | Ineligible intervention: teprenone (antiinflammatory drug) |
| Guo 2011 | Ineligible intervention: Chinese herbal medicine |
| Guo 2014 | Ineligible intervention: Chinese herbal medicine |
| Hajiaghamohammadi 2016 | Ineligible population: people with no functional dyspepsia |
| Hashem‐Dabaghian 2016 | Ineligible study design: non‐randomised trial |
| IRCT20110310006026N9 | Randomised clinical trial protocol with an ineligible population (people with Helicobater pylori but with no functional dyspepsia) |
| IRCT2017022332738N1 | Randomised clinical trial protocol with a Chinese herbal medicine |
| IRCT20170317033107N3 | Randomised clinical trial protocol which only includes people with migraine associated with functional dyspepsia |
| IRCT20200128046288N3 | Randomised clinical trial protocol which only assesses reflux related symptoms |
| Ivashkin 2022 | Ineligible patient population: case mix with IBS (no dissagregated data for functional dyspepsia). |
| Kammerer 2001 | Ineligible study design: narrative review |
| KCT0003761 2019 | Randomised clinical trial protocol which assesses a Chinese yam extract |
| KCT0004085 2019 | Randomised clinical trial protocol which assesses a Chinese herbal medicine |
| KCT0005265 2020 | Randomised clinical trial protocol which assesses a Chinese herbal medicine |
| Kelber 2017 | Ineligible study design: systematic review |
| Kim 2010 | Ineligible intervention: Chinese herbal medicine |
| Labenz 2023 | Ineligible patient population: only people with heartburn. |
| Lacy 2022 | Ineligible study design: observational study of caraway oil and L‐menthol. |
| Lee 2020 | Ineligible population: people with no functional dyspepsia |
| Lopresti 2018 | Ineligible population: participants with gastrointestinal complaints (not functional dyspepsia) |
| Marakis 2002 | Ineligible population: healthy people with dyspeptic complaints (not functional dyspepsia) |
| Meier 2005 | Ineligible study design: non‐randomised trial |
| Metugriachuk 2008 | Ineligible study design: the study refers to randomisation but there is no control group (they used a matched control group of healthy individuals) |
| Mihai 2019 | Ineligible intervention: probiotic |
| Muss 2013 | Ineligible population: participants had irritable bowel syndrome (not functional dyspepsia) |
| NCT04593836 | Randomised clinical trial protocol with an ineligible population |
| Nili‐Ahmadabadi 2017 | Ineligible population: people with no functional dyspepsia |
| Pasalar 2015a | Ineligible study design: the objective of the study was to assess the effect of the drug on depressive symptoms |
| Shim 2015 | Ineligible intervention: Korean herbal medicine |
| Shim 2019 | Ineligible population: people with no functional dyspepsia |
| Wang 2017 | Ineligible intervention: Chinese herbal medicine |
| Xiao 2013 | Ineligible population: children |
Characteristics of studies awaiting classification [ordered by study ID]
Borgia 1981.
| Methods |
Study design: parallel group randomized trial Study dates: unknown Setting and number of centres: outpatients, one centre Country: unknown |
| Participants |
Inclusion criteria: healthy people
Exclusion criteria: unknown Sample size: 24, there is no information regarding the reason for the sample size. Withdrawals: unknown Age (years): unknown Ethnicity by group: not stated Sex (M/F): unknown Symptom severity at baseline: only healthy people were studied |
| Interventions | Six groups: herbs extract, the composition is not available. Six different treatments administered according to a 6 x 6 Latin square. Test preparation versus two pairs of its components and versus placebo |
| Outcomes | Other outcomes: main outcome measured was salivary secretion, method unknown. |
| Notes | Full‐text not available. |
Borgia 1985.
| Methods | Parallel group randomized trial |
| Participants | Not available |
| Interventions | Not available |
| Outcomes | Not available |
| Notes | Neither the full text nor the abstract are available. |
Chawla 1982.
| Methods | Not available |
| Participants | Not available |
| Interventions | It is only stated that Emblica officinalis Linn was utilized as an ayurvedic drug. |
| Outcomes | Not available |
| Notes | Neither the full text nor the abstract are available. |
CTRI/2018/02/012101 2018.
| Methods | Randomized, paralle‐group, active‐controlled trial |
| Participants | People with functional dyspepsia and people with gastro‐esophageal reflux disease with esophagitis |
| Interventions | Pudin hara antacid suspension |
| Outcomes | Any improvement or relief from clinical symptoms related to acidity at the end of 2 weeks and 4 weeks or by the resolution of symptoms whichever stands early. 2 and 4 weeks. |
| Notes |
Ernst 2002.
| Methods | Not available. |
| Participants | Not avaialable. |
| Interventions | Red pepper, no details of the interventions or groups are available. |
| Outcomes | Not available. |
| Notes | Neither the full text nor the abstract are available. |
Fani 2007.
| Methods |
Study design: controlled clinical trial Study dates: not available Setting and number of centres: unknown Country: India |
| Participants | Not available. |
| Interventions |
Group 1 (study): garlic‐omeprazole combined therapy Group 2 (control): standard quadruple therapy Co‐interventions: omeprazole |
| Outcomes | Not available. |
| Notes | Neither the full text nor the abstract are available. The main outcome was most likely erradication of H pylori. |
Fintelmann 1996.
| Methods |
Study design: clinical study Study dates: not available. Setting and number of centres: not available Country: not available |
| Participants | Sample size: 553; there was no information available regarding the reason for the sample size. |
| Interventions | Group 1 (study): artichoke (Cynara scolymus) |
| Outcomes | Not available |
| Notes | Neither the full text nor the abstract are available. No information on what the comparison was, or if this was a one‐branch study. |
Fintelmann 1999.
| Methods |
Study design: clinical study Study dates: not available. Setting and number of centres: not available Country: not available |
| Participants | Not available |
| Interventions |
Group 1 (study): artichoke extract No information on what the comparison was, or if this was a one‐branch study. |
| Outcomes | Not available |
| Notes | Neither the full text nor the abstract are available. No information on what the comparison was, or if this was a one‐branch study. "Dyspeptic symptom complex" is the only clue regarding the participants. |
Freise 1999.
| Methods |
Study design: parallel‐group randomized trial Study dates: not available Setting and number of centres: outpatients, multicentre Country: not available |
| Participants |
Inclusion criteria: non‐ulcer dyspepsia (dysmotility type dyspepsia or essential/idiopathic dyspepsia, also in combination with irritable bowel syndrome). Sample size: 223 participants; there is no information available regarding this sample size. |
| Interventions |
Group 1 (study): enteric‐coated capsule containing 90 mg peppermint oil and 50 mg caraway oil. Group 2 (control): enteric soluble formulation containing 36 mg peppermint oil and 20 mg caraway oil. Co‐interventions: none |
| Outcomes |
Global symptoms of dyspepsia How measured: difference in pain intensity between the beginning and the end of therapy, measured by the participant on a visual analogue scale (0 = no pain, 10 = extremely strong pain). Time points measured: not available. Time points reported: not available. Subgroups: none Adverse events How measured: not available. Time points measured: not available. Time points reported: baseline and day 30 Subgroups: none |
| Notes | Only the abstract is available. |
IRCT20130211012438N27.
| Methods | Randomized, double‐blind, placebo‐controlled clinical trial |
| Participants | Helicobacter pylori as the cause of diseases classified elsewhere |
| Interventions | Intervention 1: Intervention group: routine treatment (Omeprazole 20 mg + Amoxicillin 1 g+ Clarithromycin 500 mg BID) + herbal soft capsule containing essential oil of Satureja hortensis BID for two weeks orally. Intervention 2: Control group: routine treatment (Omeprazole 20 mg + Amoxicillin 1 g + Clarithromycin 500 mg BID) + placebo soft capsule BID for two weeks orally. |
| Outcomes | Clinical signs. Timepoint: before the intervention, two weeks after the initial intervention. Method of measurement: questionnaire. The eradication rate of Helicobacter pylori. Timepoint: 1 month after the end of treatment. Method of measurement: stool antigen for Helicobacter pylori |
| Notes |
IRCT20200128046291N1.
| Methods | Randomized controlled trial |
| Participants |
Inclusion: People aged 18 to 60 years, with functional dyspepsia (based on ROME IV syndrome) Exclusion: history of a gastrointestinal ulcer or reflux disease with natural endoscopy without specific pathologic findings, underlying diseases including heart failure, hypertension, renal failure and uremic disease, cirrhosis; history of abdominal surgery; any malignancy or individuals NSAIDs are used, having a history of chemotherapy and radiotherapy or exposure to radiation. Use of any other herbal medicine; pregnancy and lactation; positive urea breath test for Helicobacter pylori infection |
| Interventions |
Intervention group: capsules containing Ghors‐Vard 3 times daily (after meals) for 1 month. Control group: placebo capsules 3 times daily (after meals) for 1 month. |
| Outcomes | Clinical symptoms of people with functional dyspepsia |
| Notes | The status of the trial and the components of the intervention (the polyherbal preparation) are unclear. |
ISRCTN31202330.
| Methods |
Study design: placebo‐controlled clinical trial Study dates: not available Setting and number of centres: outpatient Country: not available |
| Participants |
Inclusion criteria: aged >18 years, GI‐tract discomfort such as dyspepsia‐like and/or IBS‐like symptoms. Exclusion criteria: people receiving any other medication for the GI‐tract symptoms in the previous 2 weeks, pregnant women and people with history of cancer |
| Interventions |
Group 1: A mixture of Origanum vulgare subsp. Hirtum and/or Origanum onites, Salvia fruticosa and/or Salvia officinalis and Origanum dictamnus dissolved in olive oil droplets of 0.5 ml each, once a day. Group 2: olive oil droplets of 0.5 ml each once a day. Co‐interventions: none |
| Outcomes |
Global symptoms of dyspepsia How measured: Quality Of Life in Reflux and Dyspepsia (QOLRAD) questionnaire Time points measured: baseline and after a month. Time points reported: baseline and after a month. Subgroups: none Adverse events How measured: not available Time points measured: unknown Time points reported: unknown |
| Notes | Only abstract was available. |
Ivashkin 2020.
| Methods |
Study design: double‐blind, randomized placebo‐controlled trial Study dates: study dates not available Setting and number of centres: 1 centre Country: unknown |
| Participants |
Inclusion criteria: people with FD with irritable bowel disease Exclusion criteria: non‐functional causes for the symptoms were excluded by the evaluation of detailed medical history, physical examination, blood tests, stool analysis, and endoscopy with biopsies. Sample size: 56 participants randomized Withdrawals Age (mean in years): 31 to 33 years Ethnicity by group: not stated. Sex (M/F): 23/33 Symptom severity at baseline: average total “7x7” of questionnaire points was 13 for the intervention arm and 15,5 for the control |
| Interventions |
Group 1 (n = 26): 1 capsule of food supplement (peppermint oil (40% menthol, 1.5% limonene) 240 mg; ginger oil (14% gingerol) 50 mg; olive oil 440 mg) or placebo (olive oil 730 mg) once a day in addition to the standard treatment for 30 days Group 2 (n = 25): placebo Co‐interventions: unknown |
| Outcomes | Global symptoms: 7x7 symptom score |
| Notes | This is an abstract. It is not clear how functional dyspepsia was defined in IBS patients. Moreover,it is not clear if the main results relate to IBS, dyspepsia or both. |
KCT0005020.
| Methods | Multicentre, randomized, double‐blind, placebo‐controlled clinical trial |
| Participants | People with diseases of the digestive system |
| Interventions | Dietary Supplement: The control and the experimental group were randomized 1:1. The experimental drug contains 50 mg of CTE (350 mg), which is taken twice a day in the morning and evening, and is orally taken for a total of 8 weeks. The comparator is a placebo that does not contain extracts of the same nature and is taken in the same number of times and period |
| Outcomes | Primary outcome: epigastric area scales among the Gastrointestinal Symptom Rating Scale |
| Notes |
Madisch 2000.
| Methods | Not available |
| Participants | Not available |
| Interventions | Not available |
| Outcomes | Not available |
| Notes | Full text not available ‐ possibly a secondary report of Madisch 1999 |
Madisch 2001b.
| Methods | Not available |
| Participants | Not available |
| Interventions | Not available |
| Outcomes | Not available |
| Notes | Possibly a secondary reference of Madisch 2001a. However, the full text is not available. |
May 1996.
| Methods |
Study design: parallel‐group randomized trial Study dates: not available Setting and number of centres: not available Country: not available |
| Participants |
Sample size: 45 Withdrawals: 6 in total |
| Interventions |
Group 1 (n = 19): peppermint oil/caraway oil combination Group 2 (n = 20): placebo Co‐interventions: none |
| Outcomes |
Global symptoms of dyspepsia How measured: change in the intensity of pain and the global clinical impression (CGI) Time points measured: baseline, after a month Time points reported: baseline, after a month Subgroups: none |
| Notes | Only abstract is available |
NCT04742985.
| Methods | Randomized clinical trial |
| Participants | 24 adults with functional dyspepsia (Rome IV criteria). |
| Interventions | Green tea 320 mg/day for 8 weeks |
| Outcomes | Primary outcomes: Gastrointestinal Symptom Rating Scale Secondary outcomes: biomarkers. |
| Notes | Status: Completed (2 August 2021) ‐ no results available. |
Rosch 2001.
| Methods | Not available |
| Participants | Not available |
| Interventions | Not available |
| Outcomes | Not available |
| Notes | Only title available |
Roth 1996.
| Methods | Not available |
| Participants | Not available |
| Interventions | Not available |
| Outcomes | Not available |
| Notes | Only title available |
TCTR20180530003.
| Methods | Randomized study |
| Participants | Inclusion criteria: 1. Age 18 ‐ 70 years 2. Participants with acid reflux disease: Patients with a burning sensation or tightness in the chest or have food Stomach back up in the oesophagus or sour or bitter. These symptoms interfere with the quality of life. 2. Participants with functional dyspepsia ROME IV criteria with at least one of the following symptoms: bothersome postprandial fullness, early satiety, epigastric pain, and epigastric burning pain. Symptoms Continued for at least three months and started onset for at least six months. 3. Upper gastrointestinal endoscopy for six months prior to the study. |
| Interventions | Anti‐OxA(R) in 1 capsule contains curcumin extract equivalent to curcuminoid 250 mg as the main substance and other compounds, including colloidal silicon dioxide, a small amount of magnesium dioxide. |
| Outcomes | Response to curcuminoid after 4 weeks of intervention Relationship between treatment response and physiological changes of oesophagus and stomach at 4 weeks |
| Notes |
GI: gastrointestinal; NSAIDs: non‐steroidal anti‐inflammatory drugs
Characteristics of ongoing studies [ordered by study ID]
CTRI/2020/04/024448.
| Study name | A clinical study to check the efficacy and safety of investigational product in indigestion |
| Methods | Randomised controlled study |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | Intervention: GGE03 is a steamed ginger extract powder. Comparator: contains pharmacological inactive ingredients. Dose: 2 tablets per day orally, morning meal intake (1,600 mg/day, with GGE03 480 mg/day) |
| Outcomes | Primary outcome Clinically significant positive change from baseline to EOT (End of treatment) in the following efficacy parameters:
Secondary outcomes
|
| Starting date | 15 April 2020 |
| Contact information | Name Dr Santosh Saklecha Designation General Medicine Consultant Affiliation Santosh Hospital, India Phone 9845306703 Email ssaklecha@gmail.com |
| Notes | None |
IRCT20090527001957N8.
| Study name | Effect of Pistacia lentiscus in functional dyspepsia |
| Methods | Clinical trial with control group, with parallel groups, triple‐blind, randomized |
| Participants | Criteria for inclusion in the study.
Non‐inclusion criteria
|
| Interventions | 1: Mastic oil group, patients in this group consume Mastic oil. 2: lacebo group, patients in this group take placebo. |
| Outcomes | Description Severity of Dyspepsia symptoms Timepoint Before the intervention, the end of the first month Method of measurement One and two Dyspepsia questionnaire |
| Starting date | Expected recruitment start date 16 April 2019 |
| Contact information | Research Insstitute for Islamic and Complementary Medicine Fataneh Hashem Dabaghian Phone +98 21 3311 1619 Email fatanehdabaghian@yahoo.com |
| Notes | None |
IRCT20150927024228N2.
| Study name | Efficacy of Apium graveolense and Trachyspermum copticum versus Domperidone on clinical symptoms of patients with postprandial distress syndrome |
| Methods | Clinical trial with community‐based and control group, with parallel groups, double‐blind, randomized |
| Participants | Inclusion criteria: 18‐60 years old with postprandial distress syndrome based on Rome IV criteria Non‐entry criteria
|
| Interventions | Intervention group: traditional remedy of Trachyspermum copticum and Apium graveolence, 1 gr daily, for 4 weeks Control group 1: hydrialcoholic extraction of 1 gr Trachyspermum copticum and Apium graveolence, daily, for 4 weeks Control group 2: Domperidone tablet 10 mg, 30 mg daily, for 4 weeks |
| Outcomes | Symptom severity and quality of life |
| Starting date | Expected recruitment start date 20 February 2019 |
| Contact information | Kerman University of Medical Sciences Maryam Azimi Phone: +98 34 3211 0123 Email: Dr.azimm@gmail.com |
| Notes | None |
IRCT20160721029026N4.
| Study name | Efficacy of herbal drug that is composed of essential oil of Zataria Multiflora Boiss, Trachyspermum Ammi and Anethum Graveolens L, in treatment of Functional dyspepsia (FD) and eradication of Helicobacter pylori (H.pylori) infection. |
| Methods | Study population is people that are referred to gastroenterology clinic, and sample size for study is 60. Patients are divided into two control and intervention groups by simple randomization and using the Random Allocation software. |
| Participants | The inclusion criteria are written consent, complete knowledge about the study; being diagnosed with functional dyspepsia based on the ROME III criteria and presence of H pylori infection using Stool Ag test. The exclusion criteria are lack of consent to continue their participation, kidney or liver diseases, warning symptoms of gastric and oesophageal cancers, other chronic gastrointestinal diseases and peptic ulcer disease. |
| Interventions | Intervention group: 3 capsules daily containing the essential oil of the plant for 20 days, Control group: standard treatment regimen for 4 weeks |
| Outcomes | Two weeks after the end of treatment, participants in the two groups will be compared from the point of eradication of H pylori infection. Participant characteristics such as severity of disease symptoms, and quality of life will be entered into a form at the beginning, at the end, and two weeks after completion of treatment. The safety of the treatment regimen is assessed by laboratory tests and through recording adverse drug reactions. |
| Starting date | Expected recruitment start date 20 March 2017 |
| Contact information | Hormozgan University of Medical Sciences Majid Sarnay Zade Phone: +98 76 3333 7192 Email: research@hums.ac.ir |
| Notes | None |
IRCT20170802035460N2.
| Study name | Evaluation of the effectiveness of Cinnamon Oil Soft Capsule on Bloating in patients with Functional Dyspepsia |
| Methods | In this research, 68 participants will be treated randomly with either cinnamon oil soft capsule (intervention) or placebo (control) 3 times a day for 6 weeks. Each time, 1 capsule is used. |
| Participants | Inclusion criteria: aged between 18 and 80; people who sign the testimonials and co‐operate during the study and people who have not been treated with cinnamon oil soft capsule during the last month Exclusion criteria: people with peptic ulcer disease, inflammatory bowel disease, irritable bowel syndrome, pure gastro‐esophageal reflux disease; people with a history of gastrointestinal system surgery and pregnant and breast‐feeding women. |
| Interventions | Intervention: oral use of cinnamon oil soft capsule 3 times a day for 6 weeks. Control: oral use of sesame oil soft capsule 3 times a day for 6 weeks. |
| Outcomes | Bloating |
| Starting date | Expected recruitment start date 22 December 2017 |
| Contact information | Kermanshah University of Medical Sciences Fateme Parvizi Phone: +98 83 3429 9220 Email: fatemeparvizi4@gmail.com |
| Notes | None |
IRCT20190304042911N1.
| Study name | Evaluating Efficacy of traditional preparation containing Bunium persicum and Coriandrum sativum on clinical symptoms of patients with functional dyspepsia |
| Methods | A randomized, double‐blind, placebo‐controlled clinical trial as a pilot study with a sample size of 30 in each group |
| Participants | Patients 18 to 60 years old with functional dyspepsia Exclusion criteria: pregnant or breastfeeding; people with allergies to ginger and similar herbs; haemorrhagic diseases; history of gastrointestinal ulcer or reflux disease; IBS; history of surgery in the oesophagus, stomach and intestines |
| Interventions | Intervention group: 250 mg of cumin powder, 250 mg of coriander powder, twice daily for 4 weeks Control group: capsule containing 500 mg of starch powder, twice daily for 4 weeks |
| Outcomes | Description Indigestion severity score Time point 4 times: on arrival, 2, 4 and 8 weeks Method of measurement Gastrointestinal Symptom Rating Scale |
| Starting date | Expected recruitment start date: 6 April 2019 |
| Contact information | Kerman University of Medical Sciences Abbas Pardakhti Phone: +98 34 3231 5041 Email: Abpardakhty@kmu.ac.ir |
| Notes | None |
IRCT20190806044456N1.
| Study name | Comparison of the effects of herbal capsule SOE HAZEMEH (Govarcin) and Metoclopramide on the quality of life in patients with functional dyspepsia |
| Methods | A randomized, controlled, double‐blind clinical trial with 60 participants, Comparison of two types of drug |
| Participants | Inclusion criteria: aged 14 to 65 years with an abnormality of upper gastrointestinal endoscopic results; abdominal ultrasound; not taking anti‐depressant drugs; not allergic to metoclopramide; participation in the study Exclusion criteria: gastrointestinal ulcer or gastroesophageal reflux disease and Irritable Bowel Syndrome Gastrointestinal; narcotic use; Diabetics; Gastrointestinal cancers; Pregnant or; lactating women; use of non‐steroidal anti‐inflammatory drugs; Use of central nervous system weakening drugs; Patient non‐cooperation |
| Interventions | Intervention group: SOE HAZEMEH (Govarcin) herbal capsules containing Nigella sativa, Satureja hortensis,Thymus vulgaris, Trachyspermum copticum, Plantago major, Rosa damascena, Pistacia vera; Half an hour before each meal; oral use. Control group: metoclopramide 10 mg. Dosage: half an hour before each meal as a pill |
| Outcomes | Description: postprandial fullness Time point: before taking the drug and 4 weeks after starting medication Method of measurement ROM III questionnaire |
| Starting date | Expected recruitment start date 23 September 2019 |
| Contact information | Ghoum University of Medical Sciences Ahmad Hormati Phone: +98 25 3612 2058 Email: hormatia113@gmail.com |
| Notes | None |
IRCT20200303046677N6.
| Study name | The effect of compound honey syrup on Functional Dyspepsia: a randomized double‐blind placebo‐controlled clinical trial |
| Methods | Clinical trial with control group, with parallel groups, double‐blind, randomized, phase 3 |
| Participants | 60 participants aged 18 to 60 years with functional dyspepsia are randomly divided into two groups according to ROME III criteria |
| Interventions | Recipient of compound honey syrup |
| Outcomes | Early satiety; heaviness; vomiting; burning epigastric area; epigastric pain; bloating; burp; nausea; severity of symptoms; frequency of symptoms. |
| Starting date | 18 February 2021 (recruitment) |
| Contact information | Shahid Beheshti University of Medical Sciences. Rasool Choopani. Phone: 1516745811 Fax: +98 21 8877 3521 Email: rchoopani@sbmu.ac.ir |
| Notes | Status: Recruiting |
IRCT20200424047192N1.
| Study name | Comparative study of the effect of eating and drinking modification and sumac capsule with omeprazole on functional dyspepsia symptoms in adults |
| Methods | Clinical trial with 4 parallel groups without blinding |
| Participants | 104 participants between 18 and 60 years old. Functional dyspepsia (based on ROME III criteria) |
| Interventions | Group A patients will receive training on Eating and Drinking Modification and sumac extract capsule. Group B patients will receive training on Eating and Drinking Modification. Group C patients will receive sumac extract capsule. Group D patients will receive omeprazole capsule. |
| Outcomes | Severity of dyspepsia symptoms; quality of life; eating and drinking habits |
| Starting date | 4 January 2021 (recruitment) |
| Contact information | Gorgan University of Medical Sciences. Mahdi Saravani. Phone: +98 17 3245 1653 Mail: dr.msaravani91@gmail.com |
| Notes | Recruitment status: recruitment complete |
IRCT20220304054179N1.
| Study name | Study the efficacy of an Iranian traditional herbal compound in treatment of functional dyspepsia, add‐on double blind randomized controlled trial |
| Methods | A double‐blind clinical trial with parallel groups is performed on 150 patients (105 in the drug group and 45 in the placebo group); Randomization is done by block randomization. Random sequence generation will also be done using Randomizer software. |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention group: this group receives the drug, which contains a traditional herbal composition. the components of the product include the seeds of the anise plant and the seeds of the fennel plant and the seeds of the Trachyspermum plant and the seeds of the caraway plant, which are grinded and placed in 8‐gram sachets by traditional medicine pharmacist in the drug manufacturing center located in Emam Reza Clinic. Each patient is given 28 sachets. The method of taking the medicine is one sachet in the morning before breakfast and one sachet at night at bedtime, which is consumed with half a glass of water, and the treatment period is two weeks. Control group: the group that receives placebo. The placebo includes corn starch, wheat bran and barley flakes and 10% of the herbal composition of the drug (to simulate the appearance of the drug), which is prepared by a traditional medicine pharmacist in the drug manufacturing center located in Emam Reza Clinic in Shiraz and placed in 8 gram sachets. |
| Outcomes | Primary outcome: Postprandial fullness. Time point: 2 weeks. Method of measurement: Gastrointestinal Symptoms Severity Questionnaire. Secondary outcome: Epigastric pain&oburning sensation. Time point: 2 weeks. Method of measurement: Gastrointestinal Symptoms Severity Questionnaire. |
| Starting date | Date of first enrolment: 3 December 2022 |
| Contact information | Shiraz University of Medical Sciences ‐ Kamyar Zomorrodian Phone: +98 71 3212 2430 Fax: +98 71 3212 2430 Email: samimisoodabeh@sums.ac.ir Web page address: https://rde.sums.ac.ir |
| Notes | None |
KCT0005229.
| Study name | A 12 week, Randomized, Double‐blind, Placebo‐Controlled Clinical Trial for the Evaluation of the Efficacy and Safety of EDL on Dyspepsia |
| Methods | Interventional Study. Participants are randomly assigned to either the test group or the control group according to the registered order. |
| Participants | Diseases of the digestive system functional dyspepsia |
| Interventions | Participants take investigational product or placebo for 12 weeks. Investigational product (EDL): once a day, 2 tablets orally intake (Extract of Dolichos lablab Linne 715 mg/day) Placebo: consumed in the same way as the investigational product |
| Outcomes | GSRS (Gastrointestinal Symptom Rating Scale) Stomach symptom score |
| Starting date | 1 July 2020 |
| Contact information | Prof. Nayoung Kim Telephone: +82‐31‐787‐7008 Seoul National University Bundang Hospital Seoul National University Bundang Hospital 82, Gumi‐ro 173 beon‐gil, Bundang‐gu, Seongnam‐si, Gyeonggi‐do, S. Korea 13620 |
| Notes | None |
NCT03548363.
| Study name | Effect of Gingest on Symptoms of Dyspepsia |
| Methods | This is a randomised, double‐blind, placebo controlled study on the effect of Gingest (ginger root extract) on symptoms of dyspepsia in 150 participants with mild to moderate dyspepsia |
| Participants | 150 participants with upper abdominal pain or discomfort that is an unpleasant sensation, characterized by one or more of the following symptoms: early satiety, postprandial fullness, bloating, and nausea for at least 3 months during last year, without an identifiable underlying structural or biochemical motivation. |
| Interventions | Dietary Supplement: Gingest powdered extract obtained from Ginger rhizomes. Dietary Supplement: placebo |
| Outcomes | Reduce intensity of functional dyspepsia (based on a symptom severity questionnaire) |
| Starting date | 13 March 2018 |
| Contact information | Atlantia Food Clinical Trials ‐ Naturex SA |
| Notes | Recruitment Status: completed |
NCT04482478.
| Study name | Clinical Trial for the Evaluation of the Efficacy and Safety of EDL on Dyspepsia |
| Methods | Study type: interventional (clinical trial) Allocation: randomized Intervention model: parallel assignment |
| Participants | Estimated enrollment:100 participants |
| Interventions | Participants are randomly assigned to either the test group or the control group according to the registered order. Participants take investigational product or placebo for 12 weeks. Investigational product (EDL): once a day, 2 tablets orally intake (Extract of Dolichos lablab Linne 715 mg/day) Placebo: consumed in the same way as the investigational product |
| Outcomes | GSRS (Gastrointestinal Symptom Rating Scale) Stomach symptom score (Time frame: 12 weeks) GSRS (Gastrointestinal Symptom Rating Scale) Stomach symptom score change after 12 weeks of administration, compared to baseline.
|
| Starting date | 1 July 2020 |
| Contact information | Contact: Nayoung Kim 82317877009 nayoungkim49@empas.com Contact: 821052164932 Principal Investigator: Nayoung Kim, MD., PhD |
| Notes | Recruitment Status: recruiting |
NCT04656730.
| Study name | Effect of STW5 (Iberogast ®) and STW5‐II (Iberogast N®) on Transit and Tolerance of Intestinal Gas |
| Methods | Interventional (clinical trial) |
| Participants | 68 participants Ages eligible for study: 18 years and older; sexes eligible for study: all; accepts healthy volunteers: no criteria Inclusion criteria
|
| Interventions | To determine the independent effects of STW5 and STW5‐II on transit and evacuation of intestinal gas in subjects with functional dyspepsia and irritable bowel syndrome according to Rome IV criteria, measured as ml of gas recovered by a rectal cannula |
| Outcomes | Transit and evacuation of intestinal gas (time frame: baseline to day 14) Colonic gas filling and evacuation (participants with IBS) and gastric gas transit (participants with functional dyspepsia). Primary outcome measures will be evaluated by an infusion machine (to perform gas infusion) and a barostat (to perform gas collection measurement). |
| Starting date | 3 September 2020 |
| Contact information | Dr. JORDI F SERRA, MD,Phd (34) 93 4978909 Jserrap.germanstrias@gencat.cat |
| Notes | Recruitment Status: recruiting |
RBR‐10yqwrk6.
| Study name | Double‐blind randomized clinical trial of Maytenus ilicifolia as a strategy to manage dyspepsia in gastroesophageal reflux disease |
| Methods | Double‐blind RCT |
| Participants | Inclusion criteria: voluntary participants, of both sexes, aged between 18 and 60 years who are looking for medical attention in Health Units and who, after medical evaluation, present symptoms of dyspepsia ‐ at least two of these symptoms: regurgitation, taste of sour or bitter fluid in the mouth, and/or epigastric pain and/or burning pain (ascending or not) in the week before the consultation, of gastroesophageal reflux disease. People able to be treated without endoscopic investigation and without evidence of disease or use of medication that justifies the symptoms will be included. Exclusion criteria: people who are referred for an endoscopic examination and who are intolerant to the treatment compounds will be excluded from the medical evaluation. Pregnant women or women of reproductive age who do not use hormonal contraceptives will be excluded. People with a history of glaucoma, paralytic ileum, stenosis or mechanical obstruction of the gastrointestinal tract, megacolon, people with acute‐angle glaucoma, urinary retention or prostate hyperplasia; people using any drugs with antiulcer or prokinetic properties in the week prior to recruitment that present structural changes related to reflux and dyspepsia, such as hiatus hernia and oesophageal atresia, hepatopathies and people using drugs that make pharmacological interaction with compounds of Maytenus ilicifolia dry extract will be excluded. |
| Interventions | Experimental Group 1: 133 voluntary participants with dyspepsia symptoms should take capsules containing dry extract of Maytenus ilicifolia in 400 mg dose twice a day. Experimental group 2: 133 voluntary participants with dyspepsia symptoms should take capsules containing dry extract of Maytenus ilicifolia in 860 mg dose twice a day. Control group: 133 voluntary participants with dyspepsia symptoms should take capsules containing a proton pump inhibitor (omeprazol) 20 mg twice a day. Each group will take the capsules twice a day ‐ 30 minutes before breakfast and dinner (each dose will be equivalent to taking two capsules). The treatment for each group will last 28 days. |
| Outcomes | Gastroesophageal Reflux Symptoms questionnaire (“reflux symptoms” QS ‐GERD) Heartburn‐Specific Quality of Life questionnaire (Heartburn Specific Quality of Life HBQOL) Salivary pepsin and pH levels |
| Starting date | Not specified |
| Contact information |
|
| Notes |
|
IBS: irritable bowel syndrome
Differences between protocol and review
Type of participants
Many studies did not explicitly refer to Rome criteria, but they described participants fulfilling said criteria. Therefore we added in the methods section, "We included studies with participants fulfilling said criteria even if there was no explicit reference to Rome criteria."
Comparisons
We combined the three last comparisons from our protocol in a single line that reflected more accurately the analysis intention: "Herbal medicines as a single agent or combined with other agents versus other agents: acid suppression agents (PPIs, H2RAs) or prokinetics."
Effect measures, Data synthesis and Summary of findings table
We updated the section on Data synthesis based on the new version of the Cochrane Handbook (Higgins 2022).
Considering that we included many different herbal preparations and their underlying differences, combining them in a meta‐analysis would have been inappropriate. We were therefore left with multiple comparisons. In this context, we chose to create summary of findings tables for those included in a meta‐analysis (two or more studies), with the input of the Cochrane Gut Review Group. These changes have been explained in the corresponding sections (Measures of treatment effect; Data synthesis; Summary of main results).
Methods not implemented
There were insufficient data for each comparison to perform the following sensitivity analyses.
Excluding studies at a high risk of bias: in our meta‐analysis, we only included studies mostly at unclear risk of bias (none with a high risk of bias); therefore, we could not conduct this predefined sensitivity analysis.
Case mix: studies either did not report the proportion of participants with comorbidities or excluded them (see Description of studies)
Missing data: we identified only three trials with a high risk of bias due to missing outcome data for dichotomous outcomes (Azimi 2017; Shin 2021; Zobeiri 2021). These informed single comparisons and were not pooled in a meta‐analysis.
We were also unable to conduct subgroup analyses since the only analysis that yielded high heterogeneity (Analysis 1.1) included four studies that had a similar duration of treatment (at least four weeks), the same type of herbal preparation (STW5) and most of them excluded people with comorbidities (Braden 2009; Madisch 2001a; Madisch 2004; Von Arnim 2007). Finally, H pylori status was reported in three studies (Braden 2009; Madisch 2004; Von Arnim 2007), with similar rates of positivity (10% to 27%).
Contributions of authors
| Roles and responsibilities (protocol and review stage) | |
| Guarantor of the review | JVAF, MA |
| Draft the protocol | JVAF, MA |
| Develop and run the search strategy | Cochrane Gut Group |
| Obtain copies of studies | MA, CP |
| Select which studies to include (2 people) | MA, CP |
| Extract data from studies (2 people) | GB, CV |
| Enter data into RevMan | GB, CV |
| Carry out the analysis | All authors |
| Interpret the analysis | All authors |
| Draft the final review | All authors |
| Update the review | JVAF, MA |
Sources of support
Internal sources
-
Universidad de Valparaíso, Chile
Financial support to the researcher (MA, CP)
-
Institute of General Practice, Medical Faculty of the Heinrich‐Heine‐University Düsseldorf, Germany
Financial support to the researcher (JVAF)
External sources
No sources of support provided
Declarations of interest
GB: none known CV: none known MA: none known CP: none known JVAF: none known. JVAF is a managing editor for the Cochrane Metabolic and Endocrine Disorders Group and a contact editor for the Urology Group. He was not involved in the editorial process of this manuscript.
Edited (no change to conclusions)
References
References to studies included in this review
Alizadeh‐Naini 2020 {published data only}
- Alizadeh-Naini M, Yousefnejad H, Hejazi N. The beneficial health effects of Nigella sativa on Helicobacter pylori eradication, dyspepsia symptoms, and quality of life in infected patients: A pilot study. Phytotherapy Research 2020;34(6):1367-76. [DOI] [PubMed] [Google Scholar]
Allan 2012 {published data only}
- Allan JJ, Raveendra KR, Jayachandra Srinivasa V, Sushma KR, Goudar KS, Shivaprasad HN, et al. An extract of Glycyrrhiza glabra (GutGard) alleviates symptoms of functional dyspepsia: A randomized, double-blind, placebo-controlled study. Evid Based Complement Alternat Med 2012;2012:216970. [DOI: 10.1155/2012/216970] [DOI] [PMC free article] [PubMed] [Google Scholar]
Azimi 2017 {published data only}
- Azimi M, Zahedi MJ, Mehrabani M, Tajadini H, Zolala F, Baneshi MR, et al. Effect of Apium graveolens and Trachyspermum copticom on clinical symptoms of patients with functional dyspepsia. Avicenna Journal of Phytomedicine 2017;7(6):554-64. [PMC free article] [PubMed] [Google Scholar]
- Azimi M, Zahedi MJ, Mehrabani M, Tajadini H, Zolala F, Baneshi MR, et al. Effects of Iranian traditional medicine remedies (Apium Graveolence and Trachyspermum Copticum) on modifying the quality of life in patients with functional dyspepsia: A double- blind randomized clinical trial. Galen Medical Journal 2017;6(2):102-9. [Google Scholar]
Babaeian 2017 {published data only}
- Babaeian M Naseri M Kamalinejad M Ghaffari F Emadi F Feizi A Rafiei R Mazaheri M Hasheminejad SA Park J-W Adibi P. The efficacy of Mentha longifolia in the treatment of patients with postprandial distress syndrome: a double-blind, randomized clinical trial. Iranian Red Crescent Medical Journal 2017;19(2):1-10.
Bordbar 2020 {published data only}
- Bordbar G Miri MB Omidi M Shoja S Akhavan M. Comparison of a Novel Herbal Medicine and Omeprazole in the Treatment of Functional Dyspepsia: a Randomized Double-Blinded Clinical Trial. Gastroenterology Research and Practice 2020;2020:5152736. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bortolotti 2002 {published data only}
- Bortolotti M, Coccia G, Grossi G, Miglioli M. The treatment of functional dyspepsia with red pepper. Alimentary Pharmacology and Therapeutics 2002;16(6):1075-82. [DOI] [PubMed] [Google Scholar]
Braden 2009 {published data only}
- Braden B, Caspary W, Borner N, Vinson B, Schneider ARJ. Clinical effects of STW 5 (Iberogast) are not based on acceleration of gastric emptying in patients with functional dyspepsia and gastroparesis. Neurogastroenterology and Motility 2009;21(6):632-e25. [DOI] [PubMed] [Google Scholar]
Chey 2019 {published data only}
- Chey WD Lacy BE Cash BD Epstein M Corsino PE Shah SM. A Novel, Duodenal-Release Formulation of a Combination of Caraway Oil and L-Menthol for the Treatment of Functional Dyspepsia: a Randomized Controlled Trial. Clin Transl Gastroenterol 2019;10(4):e00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chey WD, Lacy BE, Cash BD, Epstein M, Shah SM. Efficacy of caraway oil/L-menthol plus usual care vs placebo plus usual care, in functional dyspepsia patients with post-prandial distress (PDS) or epigastric pain (EPS) syndromes: Results from a US RCT. Gastroenterology 2017;152(5 Supplement 1):S307. [Google Scholar]
- Lacy BE, Chey WD, Cash BD, Epstein M, Shah SM. A caraway oil/menthol combination improves functional dyspepsia (FD) symptoms within the first 24 hours: Results of a randomized controlled trial, which allowed usual FD treatments. Gastroenterology 2017;152(5 Supplement 1):S307. [Google Scholar]
Chitapanarux 2020 {published data only}
- Chitapanarux T Lertprasertsuke N Toworakul C. Efficacy and Safety of Fingerroot (Boesenbergia rotunda) Extract in Patients with Functional Dyspepsia: a Randomized, Placebo-Controlled Trial. Digestion 2020;102(4):599-606. [DOI] [PubMed] [Google Scholar]
- TCTR20170816002. Efficacy and safety of Boesenbergia rotunda in functional dyspepsia patients: a randomized controlled trial. Digestion 2017;102(4):599-606. [DOI] [PubMed] [Google Scholar]
Dabos 2010 {published data only}
- Dabos KJ, Sfika E, Vlatta LJ, Frantzi D, Amygdalos GI, Giannikopoulos G. Is Chios mastic gum effective in the treatment of functional dyspepsia? A prospective randomised double-blind placebo controlled trial. Journal of Ethnopharmacology 2010;127(2):205-9. [DOI] [PubMed] [Google Scholar]
Da Mota Menezes 2006 {published data only}
- Da Mota Menezes V, Atallah AN, Lapa AJ, Catapani WR. Assessing the therapeutic use of Lafoensia pacari St. Hil. extract (Mangava-Brava) in the eradication of Helicobacter pylori: Double-blind randomized clinical trial. Helicobacter 2006;11(3):188-95. [DOI] [PubMed] [Google Scholar]
- da Mota Menezes, Valfredo. Avaliação do uso terapêutico do extrato de Lafoensia pacari St. Hil. Mangava-Brava na erradicação do Helicobacter pylori: Ensaio Clínico Randomizado Duplo Cego. https://repositorio.unifesp.br/handle/11600/8984 2006-04-03.
Eftekharafzali 2018 {published data only}
- Eftekharafzali M, Mehrabani M, Tajadini H, Ahmadi B, Zahedi MJ. Effect of "pistacia atlantica" resin (Baneh) on functional dyspepsia: A double-blind, randomized clinical study. Iranian Red Crescent Medical Journal 2018;20(7):e63822. [Google Scholar]
Ghoshegir 2015 {published data only}
- Ghoshegir SA, Mazaheri M, Ghannadi A, Feizi A, Babaeian M, Tanhaee M, et al. Pimpinella anisum in modifying the quality of life in patients with functional dyspepsia: A double-blind randomized clinical trial. Journal of Research in Medical Sciences 2014;19(12):1118-23. [PMC free article] [PubMed] [Google Scholar]
- Ghoshegir SA, Mazaheri M, Ghannadi A, Feizi A, Babaeian M, Tanhaee M, et al. Pimpinella anisum in the treatment of functional dyspepsia: A double-blind, randomized clinical trial. Journal of Research in Medical Sciences 2015;20(1):13-21. [PMC free article] [PubMed] [Google Scholar]
Giacosa 2015 {published data only}
- Giacosa A Guido D Grassi M Riva A Morazzoni P Bombardelli E Perna S Faliva MA Rondanelli M. The effect of ginger (Zingiber officinalis) and artichoke (Cynara cardunculus) extract supplementation on functional dyspepsia: A randomised, double-blind, and placebo-controlled clinical trial. Evid Based Complement Alternat Med 2015;2015:915087. [DOI] [PMC free article] [PubMed] [Google Scholar]
Holtmann 2003 {published data only}
- Holtmann G, Adam B, Haag S, Collet W, Grunewald E, Windeck T. Efficacy of artichoke leaf extract in the treatment of patients with functional dyspepsia: A six-week placebo-controlled, double-blind, multicentre trial. Alimentary Pharmacology and Therapeutics 2003;18(11-12):1099-105. [DOI] [PubMed] [Google Scholar]
Holtmann 2013 {published data only}
- Holtmann G, Andrews J, Holloway R, Beilby J, Adam B, Pilichiewicz AN, et al. Symptom improvement during treatment is linked to alterations of sensory function in functional dyspepsia: A placebo controlled randomised treatment trial. Journal of Gastroenterology and Hepatology 2013;28((Talley) University of Newcastle, Newcastle, NSW, Australia):126-7. [Google Scholar]
- Holtmann G, Andrews JM, Holloway RH, Beilby J, Adam B, Pilichiewicz AN, et al. A placebo controlled randomised treatment trial for functional dyspepsia including post-treatment drug withdraw and placebo withdraw effects. Gastroenterology 2013;144(5 SUPPL. 1):S733. [Google Scholar]
- Pilichiewicz AN, Andrews JM, Goess C, McMahon J, Barrett B, Fraser RJ, et al. Placebo effects in functional dyspepsia: A preliminary analysis on symptoms in an ongoing randomized placebo controlled trial. Gastroenterology 2012;142(5 SUPPL. 1):S469. [Google Scholar]
- Pilichiewicz AN, Andrews JM, Goess C, Mcmahon J, Fraser RJ, Beilby J, et al. A preliminary analysis of the effect Iberogast, Nexium, dual Iberogast + Nexium or dual placebo on symptoms in patients with functional dyspepsia. Journal of Gastroenterology and Hepatology 2011;26((Talley) Faculty of Health, University of Newcastle, Newcastle, Australia):85. [Google Scholar]
Hu 2011 {published data only}
- Hu Ming-Luen, Rayner Christophan K, Wu Keng-Liang, Chuah Seng-Kee, Tai Wei-Chen, Chou Yeh-Pin, et al. Effect of ginger on gastric motility and symptoms of functional dyspepsia. World journal of gastroenterology 2011;17(1):105-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khonche 2017 {published data only}
- Khonche A, Fallah Huseini H, abdi H, Mohtashami R, Nabati F, Kianbakht S. Efficacy of Mentha pulegium extract in the treatment of functional dyspepsia: A randomized double-blind placebo-controlled clinical trial. Journal of Ethnopharmacology 2017;206((Mohtashami) Medicine Quran and Hadith Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran, Islamic Republic of):267-73. [DOI] [PubMed] [Google Scholar]
Kupcinskas 2008 {published data only}
- Kupcinskas L, Lafolie P, Lignell A, Kiudelis G, Jonaitis L, Adamonis K, et al. Efficacy of the natural antioxidant astaxanthin in the treatment of functional dyspepsia in patients with or without Helicobacter pylori infection: A prospective, randomized, double blind, and placebo-controlled study. Phytomedicine 2008;15(6-7):391-9. [DOI] [PubMed] [Google Scholar]
Madisch 1999 {published data only}
- Madisch A, Heydenreich C-J, Wieland V, Hufnagel R, Hotz J. Treatment of functional dyspepsia with a fixed peppermint oil and caraway oil combination preparation as compared to cisapride: A multicenter, reference-controlled double-blind equivalence study. Arzneimittel-Forschung/Drug Research 1999;49(11):925-32. [DOI] [PubMed] [Google Scholar]
Madisch 2001a {published data only}
- Madisch A, Melderis H, Mayr G, Sassin I, Hotz J. Commercially available herbal preparation and its modified dispense in patients with functional dyspepsia. Results of a double-blind, placebo-controlled, randomized multicenter trial. Zeitschrift fur Gastroenterologie 2001;39(7):511-7. [DOI] [PubMed] [Google Scholar]
Madisch 2004 {published data only}
- Madisch A, Holtmann G, Mayr G, Vinson B, Hotz J. Treatment of functional dyspepsia with a herbal preparation: A double-blind, randomized, placebo-controlled, multicenter trial. Digestion 2004;69(1):45-52. [DOI] [PubMed] [Google Scholar]
Mala 2018 {published data only}
- Mala KN, Thomas J, Syam DS, Maliakel B, Krishnakumar IM. Safety and efficacy of Ferula asafoetida in functional dyspepsia: A randomized, double-blinded, placebo-controlled study. Evidence-Based Complementary andAlternative Medicine 2018;2018:4813601. [DOI] [PMC free article] [PubMed] [Google Scholar]
May 2000 {published data only}
- May B, Kohler S, Schneider B. Efficacy and tolerability of a fixed combination of peppermint oil and caraway oil in patients suffering from functional dyspepsia. Alimentary Pharmacology and Therapeutics 2000;14(12):1671-7. [DOI] [PubMed] [Google Scholar]
Mohtashami 2015 {published data only}
- Mohtashami R, Fallah Huseini H, Heydari M, Amini M, Sadeqhi Z, Ghaznavi H, et al. Efficacy and safety of honey based formulation of Nigella sativa seed oil in functional dyspepsia: A double blind randomized controlled clinical trial. Journal of Ethnopharmacology 2015;175((Mehrzadi) Department of Pharmacology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran, Islamic Republic of):147-52. [DOI] [PubMed] [Google Scholar]
Panda 2020 {published data only}
- Panda M SK, Nirvanashetty S, Parachur VA, Krishnamoorthy C, Dey S. A Randomized, Double-Blind, Placebo Controlled, Parallel-Group, Comparative Clinical Study to Evaluate the Efficacy and Safety of OLNP-06 versus Placebo in Subjects with Functional Dyspepsia. Journal of Dietary Supplements 2020;19(8):226-237. [DOI: 10.1080/19390211.2020.1856996] [DOI] [PubMed] [Google Scholar]
Pasalar 2015 {published data only}
- Pasalar M, Choopani R, Mosaddegh M, Kamalinejad M, Mohagheghzadeh A, Fattahi MR, et al. Efficacy and safety of jollab to treat functional dyspepsia: A randomized placebo-controlled clinical trial. Explore: The Journal of Science and Healing 2015;11(3):199-207. [DOI] [PubMed] [Google Scholar]
- Ranjbar, M, Pasalar, M, Lankarani, KB, Choopani, R, Rezaeizadeh, H. A traditional Persian medicine beverage could improve quality of life in dyspeptic patients. Journal of medicinal plant and natural product research 2016;82(S1):S1-S381. [DOI: 10.1055/s-0036-1596992] [DOI] [Google Scholar]
Puttapitakpong 2016 {published data only}
- Puttapitakpong C, Jearjesdakul J. Effectiveness of curcuma longa linn compared with omeprazole on treatment of functional dyspepsia. Gastroenterology 2016;150(4 SUPPL. 1):S43. [Google Scholar]
Rafieian‐Kopaei 2005 {published data only}
- Rafieian-Kopaei M, Hosseini-Asl K. Effects of Ocimum basilicum on functional dyspepsia: A double-blind placebo-controlled study. Iranian Journal of Medical Sciences 2005;30(3):134-7. [Google Scholar]
Rich 2017 {published data only}
- Holtmann G, Rich G, Wieland V, Funk P, Kieser M, Koehler S. Menthacarin for the treatment of epigastric pain syndrome (EPS) and postprandial distress syndrome (PDS): Data of a placebocontrolled trial revisited. Zeitschrift fur Gastroenterologie 2015;53(8):KG253. [Google Scholar]
- Holtmann G, Stracke B. Effects of Menthacarin on symptoms and quality of life in patients with functional dyspepsia: Result of a 8-week optional placebo controlled follow-up. Zeitschrift fur Gastroenterologie 2016;54(8):KV420. [Google Scholar]
- Holtmann GJ, Stracke B. Sustained treatment effects of menthacarin on symptoms and quality of life in patients with functional dyspepsia 8 weeks after the end of a 4-week placebo-controlled trial. United European Gastroenterology Journal 2017;5(5 Supplement 1):A790-1. [Google Scholar]
- Rich G, Shah A, Koloski N, Funk P, Stracke B, Kohler S, Holtmann G. A randomized placebo-controlled trial on the effects of Menthacarin, a proprietary peppermint- and caraway-oil-preparation, on symptoms and quality of life in patients with functional dyspepsia. Neurogastroenterology and Motility 2017;29(11):1-9. [DOI] [PubMed]
Rosch 2002 {published data only}
- Rosch W, Vinson B, Sassin I. A randomised clinical trial comparing the efficacy of a herbal preparation STW 5 with the prokinetic drug cisapride in patients with dysmotility type of functional dyspepsia. Zeitschrift fur Gastroenterologie 2002;40(6):401-8. [DOI] [PubMed] [Google Scholar]
Salem 2010 {published data only}
- Salem EM, Yar T, Bamosa AO, Al-Quorain A, Yasawy MI, Alsulaiman RM, et al. Comparative study of Nigella Sativa and triple therapy in eradication of Helicobacter Pylori in patients with non-ulcer dyspepsia. Saudi Journal of Gastroenterology 2010;16(3):207-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sastry 2016 {published data only}
- CTRI/2017/08/009227. Pudin Hara Pearls & Pudin Hara Liquid evaluted for its efficacy & safety gor indication in Indigestion. http://www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/08/009227 2017.
- Sastry JLN, Pandey SD, Vats A, Vedula A, Kumar S. Symptomatic management of functional dyspepsia: evaluation of efficacy and safety of pudin hara pearls and pudin hara liquid. International Journal Research in Ayurveda and Pharmacy 2016;7(3):65-9. [Google Scholar]
Sattarzadeh 2021 {published data only}
- Sattarzadeh MB, Asie S, Mohssen N, Mehri A, Foroogh A, Mohammad T, et al. Topical Mastic Oil for Treatment of Functional Dyspepsia: A Randomized Triple-Blind Controlled Trial. GMJ 2021-02-04;10:e1965.. [DOI: 10.31661/gmj.v10i0.1965] [DOI] [Google Scholar]
Shin 2021 {published data only}
- A 8 week, Multi-center, Randomized, Double-blind, Placebo-Controlled Clinical Trial for the Evaluation of the Efficacy and Safety of CTE on Stomach Symptom. http://cris.nih.go.kr/cris/en/search/search_result_st01.jsp?seq=16298 First Submitted Date: 2020/03/24.
- Shin J, Oh TH, Kim JY, Shim JJ, Lee JL. Efficacy and Safety of the Cudrania tricuspidata Extract on Functional Dyspepsia: A Randomized Double-Blind Placebo-Controlled Multicenter Study. Journal of clinical medicine Published 2021 Nov 16.;10((22)):5323. [DOI: 10.3390/jcm10225323] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2016 {published data only}
- Sun X, Ke M, Wang Z, Lin L, Zhong H, Zhang S, et al. Treatment of functional dyspepsia with enteroplant: A double-blind randomized placebo-controlled pilot phase II clinical trial. Neurogastroenterology and Motility 2014;26((Zeng, Tang) GI, Affiliated Hospital, Hainan Medical University, China):76. [Google Scholar]
Thamlikitkul 1989 {published data only}
- Thamlikitkul V, Bunyapraphatsara N, Dechatiwongse T, Theerapong S, Chantrakul C, Thanaveerasuwan T, et al. Randomized double blind study of Curcuma domestica Val. for dyspepsia. Journal of the Medical Association of Thailand = Chotmaihet thangphaet 1989;72(11):613-620. [PubMed] [Google Scholar]
Vinson 2020 {published data only}
- Vinson B, Fink C, Wargenau M, Talley NJ, Holtmann GJ. 330: Efficacy and safety of STW-5-II in patients with functional dyspepsia: results from a double-blind, randomized, placebo-controlled, 8-week multicenter trial including a post-hoc analysis for patients meeting functional dyspepsia according to ROME IV. In: Gastroenterology. Vol. 162. 2022:S69.
- Vinson, B, Holtmann, G. Efficacy and safety of STW 5 II in patients with functional dyspepsia: results from a double-blind, randomized, multicenter trial. In: Zeitschrift für Gastroenterologie. 08 -9-2020. [DOI: 10.1055/s-0040-1716211] [DOI]
Von Arnim 2007 {published data only}
- Von Arnim U, Peitz U, Vinson B, Gundermann K-J, Malfertheiner P. STW 5, a phytopharmacon for patients with functional dyspepsia: Results of a multicenter, placebo-controlled double-blind study. American Journal of Gastroenterology 2007;102(6):1268-1275. [DOI] [PubMed] [Google Scholar]
Yongwatana 2022 {published data only}
- Yongwatana K Harinwan K Chirapongsathorn S Opuchar K Sanpajit T Piyanirun W Puttapitakpong C. CURCUMA LONGA LINN VERSUS OMEPRAZOLE IN TREATMENT OF FUNCTIONAL DYSPEPSIA, A RANDOMIZED, DOUBLE-BLIND, PLACEBO-CONTROLLED TRIAL. The 35th Annual Meeting The Royal College of Physicians of Thailand 2019;156(6):S-. [DOI] [PubMed] [Google Scholar]
- Yongwatana K, Harinwan K, Chirapongsathorn S, Opuchar K, Sanpajit T, Piyanirun W, Puttapitakpong C. Curcuma longa Linn versus omeprazole in treatment of functional dyspepsia: A randomized, double-blind, placebo-controlled trial. J Gastroenterol Hepatol 2022;37(2):335-341. [DOI: 10.1111/jgh.15705] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zobeiri 2021 {published data only}
- Zobeiri M, Parvizi F, Shahpiri Z, Heydarpour F, Pourfarzam M, Memarzadeh MR, Rahimi R, Farzaei MH. Evaluation of the effectiveness of cinnamon oil soft capsule in patients with functional dyspepsia: a randomized double-blind placebo-controlled clinical trial. Evidence-Based Complementary andAlternative Medicine 2021;2021:1741-427. [DOI: 10.1155/2021/6634115] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12619001236189 {published data only}
- ACTRN12619001236189. Curcumin for the Treatment of Digestive Complaints in Adults. https://anzctr.org.au/Trial/Registration/TrialReview.aspx?id=378161 Date registered: 6/09/2019.
ACTRN12621000116820 {published data only}
- ACTRN12621000116820. The effects of the herbal preparation, STW5-II, on gastrointestinal motility in healthy volunteers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=380779&isReview=true Date registered: 5/02/2021.
Arai 2011 {published data only}
- Arai Makoto, Matsumura Tomoaki, Yoshikawa Masaharu, Imazeki Fumio, Yokosuka Osamu. [Analysis of the Rikkunshito efficacy on patients with functional dyspepsia]. Nihon Yakurigaku Zasshi 2011;137(1):18-21. [DOI] [PubMed] [Google Scholar]
Arai 2012 {published data only}
- Arai M, Matsumura T, Tsuchiya N, Sadakane C, Inami R, Suzuki T, et al. Rikkunshito improves the symptoms in patients with functional dyspepsia, accompanied by an increase in the level of plasma ghrelin. Hepato-Gastroenterology 2012;59(113):62-66. [DOI] [PubMed] [Google Scholar]
Asha 2017 {published data only}
- Asha MK, Debraj D, Dethe S, Bhaskar A, Muruganantham N, Deepak M. Effect of flavonoid-rich extract of Glycyrrhiza glabra on gut-friendly microorganisms, commercial probiotic preparations, and digestive enzymes. Journal of Dietary Supplements 2017;14(1-3):323-333. [DOI] [PubMed] [Google Scholar]
Asif 2015 {published data only}
- Asif HM, Zaidi SF, Sugiyama T, Akhtar N, Usmanghani K. Phytomedicine-based and Quadruple Therapies in Helicobacter pylori Infection: A Comparative, Randomized Trial. Alternative Therapies in Health and Medicine 2015;21:33-39. [PubMed] [Google Scholar]
Aydin 1997 {published data only}
- Aydin A, Ersoz G, Tekesin O, Akcicek E, Tuncyurek M, Batur Y. Does garlic oil have a role in the treatment of Helicobacter pylori infection? Turkish Journal of Gastroenterology 1997;8(2):181-184. [Google Scholar]
Barnick 1990 {published data only}
- Barnick CGW, Cardozo LD. The treatment of abdominal distension and dyspepsia with enteric coated peppermit oil following routine gynaecological intraperitoneal surgery. Journal of Obstetrics and Gynaecology 1990;10(5):423-424. [Google Scholar]
Bekar 2011 {published data only}
Bommer 2013 {published data only}
- Bommer S, Klein P, Suter A. A multicentre open clinical trial to assess the tolerability and efficacy of Boldocynara, a traditional herbal preparation for functional digestive disorders. Planta Medica 2013;79(13):.. [Google Scholar]
Choi 2011 {published data only}
- Choi M-G, Rhee P-L, Park H, Lee OY, Lee KJ, Choi SC, et al. Randomized, controlled, multi-center trial comparing the safety and efficacy of DA-9701 and itopride hydrochloride in patients with functional dyspepsia: A non-inferiority trial. Journal of Neurogastroenterology and Motility 2011;21(3):414-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2020 {published data only}
- Choi Y, Kim N, Noh GT, Lee JY, Lee DH. The Efficacy and Safety of GCWB104 (Flos Lonicera Extract) in Functional Dyspepsia: a Single-Center, Randomized, Double-Blind, Placebo-Controlled Study. Gut and Liver 2020;14(1):67-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT04008901. The Efficacy and Safety of "BST104" (Lonicera Flos Extract) in Mild to Moderate Functional Dyspepsia Subjects. https://clinicaltrials.gov/ct2/show/NCT04008901 2019.
CTRI/2022/03/041419 {published data only}
- CTRI/2022/03/041419. Efficacy of Pistacia Lenticus Plant (Rumi Mastagi) in Comparison to Levosupiride in Patients with Diabetic Gastroparesis A Double Blind Randomized Control Trial Study. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=66041 Date of registration: 28-03-2022. [DOI] [PMC free article] [PubMed]
Di 2007 {published data only}
- Di Mario F, Cavallaro LG, Nouvenne A, Stefani N, Cavestro GM, Iori V, et al. A curcumin-based 1-week triple therapy for eradication of Helicobacter pylori infection: Something to learn from failure? Helicobacter 2007;12(3):238-243. [DOI] [PubMed] [Google Scholar]
Dimitrov 1983 {published data only}
- Dimitrov B, Mendizova A, Brailski K, Ivanov L, Bozhiianov V. Clinical trial of the preparation Verbascan in treating gastrointestinal and biliary diseases. Vŭtreshni bolesti 1983;22(1):18-24. [PubMed] [Google Scholar]
Dos 2010 {published data only}
- Dos Santos SB, De Lima ACA, Melo ARDS, Frazao CDS, Cherpak GL. Comparision of the efficacy of oral mastic (Schinus terebinthiflolius Radd) with omeprazole in patients with gastritis and dyspeptic symptons: A randomized, double-blind. GED: Gastroenterologia Endoscopia Digestiva 2010;29(4):118-25. [Google Scholar]
Du 2014 {published data only}
- Du H-G, Ming L, Chen S-J, Li C-D. Xiaoyao pill for treatment of functional dyspepsia in perimenopausal women with depression. World Journal of Gastroenterology 2014;20(44):16739-16744. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eady 2019 {published data only}
- Eady SL Wallace AJ Butts CA Hedderley D Drummond L Ansell J Gearry RB. The effect of 'Zesy002' kiwifruit (Actinidia chinensis var. chinensis) on gut health function: a randomised cross-over clinical trial. Journal of Nutritional Science 2019;8:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fuhrer 2011 {published data only}
- Fuhrer M, Vogelsang H, Hammer J. A placebo controlled trial of an oral capsaicin load in patients with functional dyspepsia. Gastroenterology 2011;140(5 SUPPL. 1):S802. [DOI] [PubMed] [Google Scholar]
- Fuhrer M, Vogelsang H, Hammer J. A placebo-controlled trial of an oral capsaicin load in patients with functional dyspepsia. Neurogastroenterology and Motility 2011;23(10):918-e397. [DOI] [PubMed] [Google Scholar]
Gao 2007 {published data only}
- Gao LM, Yao SK, Zhang RX. Effect of Qingre Liqi Granule on clinical therapeutic efficacy, electrogastrogram and gastric emptying in patients with functional dyspepsia. Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi 2007;27(6):505-508. [PubMed] [Google Scholar]
Gasbarrini 2010 {published data only}
- Gasbarrini G, Zaccone V, Covino M, Gallo A. Effectiveness of a "cold dessert", with or without the addition of a mixture of digestive herbs, in subjects with "functional dyspepsia". Journal of Biological Regulators and Homeostatic Agents 2010;24(1):93-98. [PubMed] [Google Scholar]
Gong 2019 {published data only}
- Gong Y, Huang X, Chen M, Xiong L. Teprenone improves gastric mucosal injury and dyspeptic symptoms in long-term nonsteroidal anti-inflammatory drug users. Journal of Gastroenterology and Hepatology 2019;34(8):1344-1350. [DOI] [PubMed] [Google Scholar]
Guo 2011 {published data only}
- Guo LK, Zhang CX, Guo XF. [Long-term efficacy and safety research on functional dyspepsia treated with electroacupuncture and Zhizhu Kuanzhong capsule]. Zhongguo Zhen Jiu 2011;31(12):1071-1077. [PubMed] [Google Scholar]
Guo 2014 {published data only}
- Guo S-Y, Zeng Z-J. Jianpi Hewei decoction combined with Jianwei Xiaoshi oral liquid for treatment of functional dyspepsia. World Chinese Journal of Digestology 2014;22(25):3821-3825. [Google Scholar]
Hajiaghamohammadi 2016 {published data only}
- Hajiaghamohammadi AA, Zargar A, Oveisi S, Samimi R, Reisian S. To evaluate of the effect of adding licorice to the standard treatment regimen of Helicobacter pylori. The Brazilian Journal of Infectious Diseases 2016;20(6):534-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hashem‐Dabaghian 2016 {published data only}
- Hashem-Dabaghian F, Agah S, Taghavi-Shirazi M, Ghobadi A. Combination of Nigella sativa and honey in eradication of gastric helicobacter pylori infection. Iranian Red Crescent Medical Journal 2016;18(11):e23771. [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT20110310006026N9 {published data only}
- IRCT20110310006026N9. Evaluating the effects of standardized hydroalcoholic extract of marmotti (Salvia mirzayanii Rech. f. & Esfand) capsule as adjunctive treatment in patient with helicobacter pylori infection. https://en.irct.ir/trial/41703 2019;.:.. [Google Scholar]
IRCT2017022332738N1 {published data only}
- IRCT2017022332738N1. Effect of Nardostachys jatamansi DC on clinical symptoms of functional dyspepcia /postprandial distress syndrome. https://en.irct.ir/trial/25428 2017;.:.. [Google Scholar]
IRCT20170317033107N3 {published data only}
- IRCT20170317033107N3. Effectiveness of Persian herbal formulation on migraine associated with functional dyspepsia. https://en.irct.ir/trial/25626 2020.
IRCT20200128046288N3 {published data only}
- IRCT20200128046288N3. The Study of Combinatory effect of Cydonia oblanga, Cinnamomum zeylanicom, Pistacia lentiscus and Honey in Eradication of Gastric Helicobacter pylori Infection. https://www.irct.ir/trial/49741 Registration date: 2020-07-24.
Ivashkin 2022 {published data only}
- Ivashkin VT, Kudryavtseva AV, Krasnov GS, Poluektov YM, Morozova MA et al. Efficacy and safety of a food supplement with standardized menthol, limonene, and gingerol content in patients with irritable bowel syndrome: A double-blind, randomized, placebo-controlled trial. PLoS One 2022;17(6):e0263880. [DOI: 10.1371/journal.pone.0263880] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kammerer 2001 {published data only}
- Kammerer E, Fintelmann V. Curcuma-Wurzelstock bei dyspeptischen Beschwerden - Ergebnisse einer Anwendungsbeobachtung. Natura Med 2001;16(8):18-26. [Google Scholar]
KCT0003761 2019 {published data only}
- KCT0003761. Efficacy and safety study of WSY-S. https://cris.nih.go.kr/cris/search/detailSearch.do?seq=13532&search_page=L&search_lang=E&lang=E 2019;.:.. [Google Scholar]
KCT0004085 2019 {published data only}
- KCT0004085. Study for the efficacy and safety of "BST104" in mild to moderate functional dyspepsia subjects. http://www.who.int/trialsearch/Trial2.aspx?TrialID=KCT0004085, 2019 2019;.:.. [Google Scholar]
KCT0005265 2020 {published data only}
- KCT0005265. A Clinical Trial for the evaluation of the efficacy and safety of RW0117 on dyspepsia. https://cris.nih.go.kr/cris/search/detailSearch.do?seq=17281&search_page=L&search_lang=K&lang=K 2020;.:.. [Google Scholar]
Kelber 2017 {published data only}
- Kelber O, Muller J, Vinson BR, Fink C, Abdel-Aziz H, Storr M, et al. The herbal medicine STW 5 is efficacious in targeting dyspeptic symptoms in all ages: A meta-analysis of randomized controlled trials. Neurogastroenterology and Motility 2017;29((Nieber) Institute fur Pharmacy, Leipzig, Germany):35. [Google Scholar]
Kim 2010 {published data only}
- Kim YM Park YC Jo JH Kang WC Son MW Hong KE. [Effect of Herb Medicine Treatment for Functional Dyspepsia: A Randomized Placebo-Controlled and Compared Standard Treatment Trial]. J Korean Oriental Med 2010;31(1):1. [Google Scholar]
Labenz 2023 {published data only}
- Labenz J, Anschütz M, Walstab J, Wedemeyer RS, Wolters H, Schug B (2023). Heartburn relief with bicarbonate-rich mineral water: results of the randomised, placebo-controlled phase-III trial STOMACH STILL. BMJ open gastroenterology 2023;10(1):e001048. [DOI: 10.1136/bmjgast-2022-001048] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lacy 2022 {published data only}
- Lacy BE, Chey WD, Epstein MS, Shah SM, Corsino P et al. A novel duodenal-release formulation of caraway oil and L-menthol is a safe, effective and well tolerated therapy for functional dyspepsia. BMC Gastroenterology 2022;22(1):105. [DOI: 10.1186/s12876-022-02181-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2020 {published data only}
- Lee DH, Shim HI, Shin CM, Yoon H, Park YS, Kim N, Seol SY. Inhibitory Effects of ß-caryophyllene on Helicobacter Pylori Infection: A Randomized Double-Blind, Placebo-Controlled Study. Digestive Endoscopy 2020;32(Supplement 1):196. [DOI] [PubMed] [Google Scholar]
Lopresti 2018 {published data only}
- ACTRN12619001514190. HerbagutA(R) for the treatment of digestive complaints in adults. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=378642 Date submitted: 29/10/2019.
- Lopresti AL Gupta H Smith SJ. A poly-herbal blend (Herbagut(R)) on adults presenting with gastrointestinal complaints: a randomised, double-blind, placebo-controlled study. BMC complementary and alternative medicine 2018;18(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marakis 2002 {published data only}
- Bundy Rafe, Walker Ann F, Middleton Richard W, Marakis Georgios, Booth Jonathan C L. Artichoke leaf extract reduces symptoms of irritable bowel syndrome and improves quality of life in otherwise healthy volunteers suffering from concomitant dyspepsia: A subset analysis. Journal of Alternative and Complementary Medicine 2004;10(4):667-669. [DOI] [PubMed] [Google Scholar]
- Marakis G, Walker AF, Middleton RW, Booth JCL, Wright J, Pike DJ. Artichoke leaf extract reduces mild dyspepsia in an open study. Phytomedicine: International Journal of Phytotherapy and Phytopharmacology 2002;9(8):694-9. [DOI] [PubMed] [Google Scholar]
Meier 2005 {published data only}
- Meier R, Brignoli R. Artichoke leaf extract for functional dyspepsia. Result of an open, prospective, multicentre, phase IV trial. Swiss Journal of Integrative Medicine 2005;17(4):216-221. [Google Scholar]
Metugriachuk 2008 {published data only}
- Metugriachuk Y, Marotta F, Kuroi O, Tsuchiya J, Goh K-L, Minelli E, et al. Effect of a phyto-compound on delayed gastric emptying in functional dyspepsia: A randomized-controlled study. Journal of Digestive Diseases 2008;9(4):204-7. [DOI] [PubMed] [Google Scholar]
- Metugriachuk Y, Tsuchiya J, Marotta F, Kuroi O, Kawakita S, Pathak S, et al. Open-label randomized trial on the effectiveness of a herbal compound in selected patients affected by functional dyspepsia. International Medical Journal 2008;15(1):47-51. [Google Scholar]
Mihai 2019 {published data only}
- Mihai C, Mihai BM, Dranga M, Cardoneanu A, Prelipcean CC. Lactobacillus reuteri - An alternative in the first-line of helicobacter pylori eradication. Farmacia 2019;67(5):871-876. [Google Scholar]
Muss 2013 {published data only}
- Muss C, Mosgoeller W, Endler T. Papaya preparation (Caricol) in digestive disorders. Neuroendocrinology letters 2013;34(1):38-46. [PubMed] [Google Scholar]
NCT04593836 {published data only}
- NCT04593836. Antiperistaltic Effect and Safety of L-menthol in the Elderly With Contraindication to Buscopan. https://clinicaltrials.gov/ct2/show/NCT04593836 First Posted: October 20, 2020.
Nili‐Ahmadabadi 2017 {published data only}
- Nili-Ahmadabadi Hossein, Emami Mohammad Hassan, Omidifar Navid. Effectiveness of Quercus brantii hydroalcoholic extract on dyspepsia: A randomized, double blind clinical trial. Journal of Education and Health Promotion 2017;6(101593794):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pasalar 2015a {published data only}
- Pasalar M, Choopani R, Mosaddegh M, Kamalinejad M, Mohagheghzadeh A, Fattahi MR, et al. Efficacy of jollab in the treatment of depression in dyspeptic patients: a randomized double-blind controlled trial. Journal of evidence-based complementary & alternative medicine 2015;20(2):104-8. [DOI] [PubMed] [Google Scholar]
Shim 2015 {published data only}
- Shim YK, Kim N, Lee JY, Park YH, Yoon H, Shin CM, et al. The efficacy and safety of new prokinetkc agent benachio q soln. in patients with postprandial distress syndrome subtype in functional dyspepsia: A single-center, randomized, double-blind, placebocontrolled pilot study. United European Gastroenterology Journal 2015;3(5 SUPPL. 1):A648-9. [DOI] [PubMed] [Google Scholar]
- Shim YK, Lee JY, Kim NY, Park YH, Yoon H, Shin CM, et al. Efficacy and Safety of New Prokinetic Agent Benachio Q Solution in Patients with Postprandial Distress Syndrome Subtype in Functional Dyspepsia: A Single-center, Randomized, Double-blind, Placebo-controlled Pilot Study. Korean Journal Gastroenterology 2015;66(1):17-26. [DOI] [PubMed] [Google Scholar]
Shim 2019 {published data only}
- Shim HI Song DJ Shin CM Yoon H Park YS Kim N Lee DH. Inhibitory Effects of [beta]-caryophyllene on Helicobacter pylori Infection: a Randomized Double-blind, Placebo-controlled Study. The Korean Journal of Gastroenterology 2019;74(4):199-204. [DOI] [PubMed] [Google Scholar]
Wang 2017 {published data only}
- Wang Z, Chen F, Jiang W. Clinical study on amomum villosum lour extract in the treatment of functional dyspepsia due to deficiency of spleen and stomach. Biomedical Research 2017;28(21):9679-82. [Google Scholar]
Xiao 2013 {published data only}
- Xiao M, Qiu X, Yue D, Cai Y, Mo Q. Influence of hippophae rhamnoides on two appetite factors, gastric emptying and metabolic parameters, in children with functional dyspepsia. Hellenic Journal of Nuclear Medicine 2013;16(1):38-43. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Borgia 1981 {published data only}
- Borgia M, Sepe N, Borgia R, Ori-Bellometti M. Pharmacological activity of a herbs extract: A controlled clinical study. Curr Ther Res 1981;29(3 II):525-36. [Google Scholar]
Borgia 1985 {published data only}
- Borgia M, Camarri E, Cataldi V, Frigerio G, Minerva V, Miracco A. [Double-blind double-controlled polycenter study on the therapeutic activity of a well-known combination of medicinal herbs]. La Clinica Terapeutica 1985;114(5):401-409. [PubMed] [Google Scholar]
Chawla 1982 {published data only}
- Chawla Y K, Dubey P, Singh R, Nundy S, Tandon B N. Treatment of dyspepsia with Amalaki (Emblica officinalis Linn.)--an Ayurvedic drug. The Indian Journal of Medical Research 1982;76 Suppl(gjf, 0374701):95-98. [PubMed] [Google Scholar]
CTRI/2018/02/012101 2018 {published data only}
- CTRI/2018/02/012101. To evaluate the effect of Pudin Hara Herbal Antacid Suspension in the management of Indigestion & Hyperacidity. http://www.ctri.nic.in/Clinicaltrials/pdf_generate.php?trialid=22909&EncHid=&modid=&compid=%27,%2722909det%27 2018.
Ernst 2002 {published data only}
- Ernst E. Red pepper alleviates functional dyspepsia. Focus on Alternative and Complementary Therapies 2002;7(3):245-246. [Google Scholar]
Fani 2007 {published data only}
- Fani A, Fani I, Delavar M, Fani P, Eshrati B, Elahi M. Combined garlic-omeprazole versus standard quadruple therapy for eradication of Helicobacter pylori infection. Indian Journal of Gastroenterology 2007;26(3):145-146. [PubMed] [Google Scholar]
Fintelmann 1996 {published data only}
- Fintelmann V. Antidyspeptic and lipid lowering effects of artichoke (Cynara scolymus) extract. Results of clinical studies on efficacy and tolerability of Hepar-SL forte on 553 patients. Journal of General Medicine 1996;2(1):3-19. [Google Scholar]
Fintelmann 1999 {published data only}
- Fintelmann V. Artichoke extract in dyspeptic symptom complex. Methods and results of a clinical study. Zeitschrift fur Phytotherapie 1999;20(2):93-95. [Google Scholar]
Freise 1999 {published data only}
- Freise J, Kohler S. Peppermint oil/caraway oil-fixed combination in non-ulcer dyspepsia equivalent efficacy of the drug combination in an enteric coated or enteric soluble formulation. Die Pharmazie 1999;54(3):210-215. [PubMed] [Google Scholar]
- Freise J, Kohler S. [Peppermint oil-caraway oil fixed combination in non-ulcer dyspepsia--comparison of the effects of enteric preparations]. Die Pharmazie 1999;54(3):210-215. [PubMed] [Google Scholar]
IRCT20130211012438N27 {published data only}
- IRCT20130211012438N27. Evaluation of the effect of pyloricin soft gel on Helicobacter pylori infection. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20130211012438N27, 2018 2018.
IRCT20200128046291N1 {published data only}
- IRCT20200128046291N1. Evaluation of the effect of the traditional poly-herbal preparation, “Ghors-e-Vard”, on clinical symptoms of patients with functional dyspepsia. https://en.irct.ir/trial/45377 Registration date 2020-03-09.
ISRCTN31202330 {published data only}
- ISRCTN31202330. Aromatic plant intervention for gastrointestinal tract symptoms. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN31202330, 2017 2017.
Ivashkin 2020 {published data only}
- Ivashkin V, Morozova M, Poluektova E, Shifrin O, Beniashvili A, Mamieva Z, Kovaleva A et al. In: United European Gastroenterology Journal. Vol. 8. 10-2020:565. [DOI: 10.1177/2050640620927345] [DOI]
KCT0005020 {published data only}
- KCT0005020. A 8 week, Multi-center, Randomized, Double-blind, Placebo-Controlled Clinical Trial for the Evaluation of the Efficacy and Safety of CTE on Stomach Symptom. https://www.cochranelibrary.com/central/doi/10.1002/central/CN-02173164/full 2020.
Madisch 2000 {published data only}
- Madisch A Heydenrich CJ Wieland V Hufnagel R Hotz J. Equivalence of fixed Herbal combination preparation as compared with Cisapride in functional dyspepsia - influence on H. pylori - status (abstract). Gut 2000;47(Suppl 1):A111.
- Madisch A, Holtmann G, Schnitker J, Mayr G, Neuser J. Herbal preparation in functional dyspepsia - Hp-status is not a predictor for treatment success (abstract). N/A 2000;47(Suppl 1):A111.
Madisch 2001b {published data only}
- Madisch A, Holtmann G, Mayr G, Vinson B, Hotz J. Effectivity of the phytotherapeutic STW-5 II by functional dyspepsia - a randomised, placebo-controlled, double-blind study. Zeitschrift für Gastroenterologie 2002;40(8):703.
- Madisch A, Melderis H, Mayr G, Sassin I, Hotz J. A plant extract and its modified preparation in functional dyspepsia. Results of a double-blind placebo controlled comparative study. Zeitschrift für Gastroenterologie 2001;39(7):511-517. [DOI] [PubMed] [Google Scholar]
May 1996 {published data only}
- May B, Kuntz H-D, Kieser M, Kohler S. Efficacy of a fixed peppermint oil/caraway oil combination in non-ulcer dyspepsia. Arzneimittelforschung 1996;46(12):1149-1153. [PubMed] [Google Scholar]
NCT04742985 {published data only}
- NCT04742985. Effects of Combined Extracts of Green Tea Seed (Saponins) and Green Tea Leaves (Epigallocatechin-3-gallate) on Gastric Mucosal Protection: A Pilot Study. https://clinicaltrials.gov/ct2/show/NCT04742985 First Posted: February 8, 2021.
Rosch 2001 {published data only}
- Rosch W Vinson B. Phytotherapy by functional dyspepsia. Cisaprid versus Iberogast in dysmotility dyspepsia. Zeitschrift für Gastroenterologie 2001;39(10):893.
Roth 1996 {published data only}
- Roth R. Phytotherapy in functional gastrointestinal diseases. Successful phytopharmacotherapy of irritable stomach and colon. Therapiewoche 1996;46(10):549-52. [Google Scholar]
TCTR20180530003 {published data only}
- TCTR20180530003. The efficacy of curcuminoid in patients with overlapping gastroesophageal reflux disease and functional dyspepsia: a randomized controlled trial. https://www.cochranelibrary.com/central/doi/10.1002/central/CN-01907301/full 2018.
References to ongoing studies
CTRI/2020/04/024448 {published data only}
- CTRI/2020/04/024448. A clinical study to check the efficacy and safety of investigational product in indigestion. http://ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=41893&EncHid=&userName=024448 Registered on: 03/04/2020.
IRCT20090527001957N8 {published data only}
- IRCT20090527001957N8. Effect of Pistacia lentiscus in functional dyspepsia. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20090527001957N8 2019.
IRCT20150927024228N2 {published data only}
- IRCT20150927024228N2. Efficacy of Apium graveolense and Trachyspermum copticum on postprandial syndrome. https://en.irct.ir/trial/37515?revision=82438 2019.
IRCT20160721029026N4 {published data only}
- IRCT20160721029026N4. Herbal Drug for Treatment of Functional Dyspepsia and eradication of Helicobacter pylori(H.pylori) infection. https://en.irct.ir/trial/23418 2017.
IRCT20170802035460N2 {published data only}
- IRCT20170802035460N2. Effect of Cinnamon Oil Soft Capsule on Functional Dyspepsia. https://en.irct.ir/trial/27767 2017.
IRCT20190304042911N1 {published data only}
- IRCT20190304042911N1. Evaluating Efficacy of traditional preparation containing Bunium persicum and Coriandrum sativum on clinical symptoms of patients with functional dyspepsia. https://en.irct.ir/trial/38380 2019.
IRCT20190806044456N1 {published data only}
- IRCT20190806044456N1. Comparison of the effects of herbal capsule Govarcin and Metoclopramide on Treatment of functional dyspepsia. https://en.irct.ir/trial/41369 2019.
IRCT20200303046677N6 {published data only}
- IRCT20200303046677N6. The effect of compound honey syrup on Functional Dyspepsia: a randomized double-blind placebo-controlled clinical trial. https://en.irct.ir/trial/52650 Registration date: 14-02-2021.
IRCT20200424047192N1 {published data only}
- IRCT20200424047192N1. Comparative study of the effect of eating and drinking modification and sumac capsule with omeprazole on functional dyspepsia symptoms in adults. https://en.irct.ir/trial/47931 Registration date: 24-01-2021.
IRCT20220304054179N1 {published data only}
- IRCT20220304054179N1. The efficacy of an Iranian traditional herbal compound in treatment of dyspepsia. en.irct.ir/trial/62308 Date of registration: 13 April 2022.
KCT0005229 {published data only}
- KCT0005229. A 12 week, Randomized, Double-blind, Placebo-Controlled Clinical Trial for the Evaluation of the Efficacy and Safety of EDL on Dyspepsia. https://cris.nih.go.kr/cris/search/detailSearch.do?seq=17197&search_page=L&search_lang=E&lang=E 2020. [DOI] [PMC free article] [PubMed]
NCT03548363 {published data only}
- NCT03548363. Effect of Gingest on Symptoms of Dyspepsia. https://clinicaltrials.gov/ct2/show/NCT03548363 2018.
NCT04482478 {published data only}
- NCT04482478. Clinical Trial for the Evaluation of the Efficacy and Safety of EDL on Dyspepsia. https://clinicaltrials.gov/ct2/show/NCT04482478 First Posted: July 22, 2020.
NCT04656730 {published data only}
- EUCTR2019-003976-38-ES. Study to asess the efects of IberogastA(R) and IberogastA(R) N in intestinal gas transit and abdominal symptoms of patients suffering from irritable bowel syndrom or functional dyspsia. http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2019-003976-38-ES, 2020 2020.
- NCT04656730. Effect of STW5 (Iberogast (R)) and STW5-II (Iberogast N(R)) on Transit and Tolerance of Intestinal Gas. https://clinicaltrials.gov/ct2/show/NCT04656730 First Posted: December 7, 2020.
RBR‐10yqwrk6 {published data only}
- RBR-10yqwrk6. Double-blind randomized clinical trial of Maytenus ilicifolia as a strategy to manage dyspepsia in gastroesophageal reflux disease. https://ensaiosclinicos.gov.br/rg/RBR-10yqwrk6 Date of registration: 03/26/2021.
Additional references
Aziz 2018
- Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. Epidemiology, clinical characteristics, and associations for symptom-based Rome IV functional dyspepsia in adults in the USA, Canada, and the UK: a cross-sectional population-based study [Epidemiology, clinical characteristics, and associations for symptom-based Rome IV functional dyspepsia in adults in the USA, Canada, and the UK: a cross-sectional population-based study]. Lancet Gastroenterol Hepatol January 29, 2018;3(4):252-262. [DOI] [PubMed] [Google Scholar]
Bang 2015
- Bang CS, Kim JH, Baik GH, Kim HS, Park SH, Kim EJ, et al. Mosapride treatment for functional dyspepsia: a meta-analysis. Journal of Gastroenterology and Hepatology 2015;30(1):28-42. [DOI] [PubMed] [Google Scholar]
Bent 2008
- Bent S. Herbal medicine in the United States: review of efficacy, safety, and regulation: grand rounds at University of California, San Francisco Medical Center. Journal of General Internal Medicine 2008;23(6):854-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodagh 2018
- Nikkhah Bodagh M, Maleki I, Hekmatdoost A. Ginger in gastrointestinal disorders: A systematic review of clinical trials. Food science & nutrition 2018;7(1):96-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boon 2021
- Boon MH, Thomson H. The effect direction plot revisited: Application of the 2019 Cochrane Handbook guidance on alternative synthesis methods. Res Synth Methods 2021;12(1):29-33. [DOI: 10.1002/jrsm.1458] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brun 2010
- Brun R, Kuo B. Functional dyspepsia. Therapeutic Advances in Gastroenterology 2010;3(3):145-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carbone 2017
Chassany 2012
- Chassany O, Shaheen NJ, Karlsson M, Hughes N, Ryden A. Systematic review: symptom assessment using patient-reported outcomes in gastroesophageal reflux disease and dyspepsia. Scandinavian Journal of Gastroenterology 2012;47(12):1412-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chiarioni 2018
- Chiarioni G, Pesce M, Fantin A, Sarnelli G. Complementary and alternative treatment in functional dyspepsia. United European Gastroenterology Journal 2018;6(1):5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choung 2012
- Choung RS, Locke GR 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Overlap of dyspepsia and gastroesophageal reflux in the general population: one disease or distinct entities? Neurogastroenterology and Motility 2012;24(3):229-34, e106. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekor 2014
- Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Frontiers in Pharmacology 2014;4:177. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ford 2010
- Ford AC, Marwaha A, Lim A, Moayyedi P. Systematic review and meta-analysis of the prevalence of irritable bowel syndrome in individuals with dyspepsia. Clinical Gastroenterology and Hepatology 2010;8(5):401-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ford 2020
- Ford, AC, Moayyedi, P, Black, CJ et al. Systematic review and network meta-analysis: efficacy of drugs for functional dyspepsia. Alimentary pharmacology & therapeutics 16 September 2020;53(1):8-21. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2020 [Computer program]
- GRADEpro GDT: GRADEpro Guideline Development Tool. Version accessed 11 August 2021. Hamilton (ON): McMaster University (developed by Evidence Prime), 2020. Available at gradepro.org.
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JP, White IR, Wood AM. Imputation methods for missing outcome data in meta-analysis of clinical trials. Clinical Trials (London, England) 2008;5(3):225-39. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). Available from www.handbook.cochrane.org.. The Cochrane Collaboration, 2011. [Google Scholar]
Higgins 2022
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Available from www.training.cochrane.org/handbook.. Cochrane, 2022. [Google Scholar]
Holtmann 2004
- Holtmann G, Adam B, Vinson B. Evidence-based medicine and phytotherapy for functional dyspepsia and irritable bowel syndrome: A systematic analysis of evidence for the herbal preparation Iberogast. Wiener Medizinische Wochenschrift 2004;154(21-22):528-534. [DOI] [PubMed] [Google Scholar]
Huang 2012
- Huang X, Lv B, Zhang S, Fan YH, Meng LN. Itopride therapy for functional dyspepsia: a meta-analysis. World Journal of Gastroenterology 2012;18(48):7371-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hungin 2009
- Hungin AP, Hill C, Raghunath A. Systematic review: frequency and reasons for consultation for gastro-oesophageal reflux disease and dyspepsia. Alimentary Pharmacology & Therapeutics 2009;30(4):331-42. [DOI] [PubMed] [Google Scholar]
Komori 2019
- Komori K, Ihara E, Minoda Y, Ogino H, Sasaki T, Fujiwara M, Oda Y, Ogawa Y. The altered mucosal barrier function in the duodenum plays a role in the pathogenesis of functional dyspepsia. Digestive Diseases and Sciences 2019;64(11):3228-39. [DOI: 10.1007/s10620-019-5470-8] [DOI] [PubMed] [Google Scholar]
Krueger 2004
- Krueger KJ, Dryden GW, McClain CJ. Complementary and alternative medicine therapies for gastrointestinal disease. Gastroenterology 2004;10(Part 4):1. [Google Scholar]
Lacy 2012
- Lacy BE, Talley NJ, Locke GR 3rd, Bouras EP, DiBaise JK, El-Serag HB, et al. Review article: current treatment options and management of functional dyspepsia. Alimentary Pharmacology & Therapeutics 2012;36(1):3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lan 2014
- Lan L, Zeng F, Liu G-J, Ying L, Wu X, Liu M, et al. Acupuncture for functional dyspepsia. Cochrane Database of Systematic Reviews 2014, Issue 10. Art. No: CD008487. [DOI: 10.1002/14651858.CD008487.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Langmead 2001
- Langmead L, Rampton DS. Review article: herbal treatment in gastrointestinal and liver disease—benefits and dangers. Alimentary Pharmacology & Therapeutics 2001;15(9):1239-52. [DOI] [PubMed] [Google Scholar]
Lefebvre 2021
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, Noel-Storr A, Rader T, Shokraneh F, Thomas J, Wieland LS. Chapter 4: Searching for and selecting studies.. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated February 2021). Available from www.training.cochrane.org/handbook. Cochrane, 2021. [Google Scholar]
Mahadeva 2006
- Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World Journal of Gastroenterology 2006;12(17):2661-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKenzie 2021
- McKenzie JE, Brennan SE. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Available from www.training.cochrane.org/handbook.. Cochrane, 2021. [Google Scholar]
Meier 2013
- Meier R, Hengstler P, Weber F, Maurer H, Bommeli C, Brignoli R. The Tibetan herbal formula Padma Digestin in functional dyspepsia: an open-label study. Forschende Komplementarmedizin (2006) 2013;20(Suppl 2):2-7. [DOI] [PubMed] [Google Scholar]
Melzer 2004
- Melzer J, Rosch W, Reichling J, Brignoli R, Saller R. Meta-analysis: phytotherapy of functional dyspepsia with the herbal drug preparation STW 5 (Iberogast). Alimentary Pharmacology & Therapeutics 2004;20(11-12):1279-87. [DOI] [PubMed] [Google Scholar]
Melzer J 2004
- Melzer J, Iten F, Reichling J, Saller R. Iberis amara L. and Iberogast--results of a systematic review concerning functional dyspepsia. Journal of Herbal Pharmacotherapy 2004;4(4):51-59. [PubMed] [Google Scholar]
Moayyedi 2004
- Moayyedi P, Delaney BC, Vakil N, Forman D, Talley NJ. The efficacy of proton pump inhibitors in nonulcer dyspepsia: a systematic review and economic analysis. Gastroenterology 2004;127(5):1329-37. [DOI] [PubMed] [Google Scholar]
Moayyedi 2006
- Moayyedi P, Soo S, Deeks JJ, Delaney B, Harris A, Innes M, et al. Eradication of Helicobacter pylori for non-ulcer dyspepsia. Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No: CD002096. [DOI: 10.1002/14651858.CD002096.pub4] [DOI] [PubMed] [Google Scholar]
Montoro 2004
- Montoro Huguet MA, Santolaria Piedrafita S. Quality of life in patients with functional dyspepsia [Calidad de vida en los pacientes con dispepsia funcional]. Gastroenterologia y Hepatologia 2004;27:15-23. [Google Scholar]
NIH 2016
- National Center for Complementary and Integrative Health. Complementary, alternative, or integrative health: what’s in a name? nccih.nih.gov/health/integrative-health (accessed 1 September 2017).
Page 2021
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. British Medical Journal 2021;372:n71. [DOI: 10.1136/bmj.n71] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2010
- Park JW, Ryu B, Yeo I, Jerng UM, Han G, Oh S, et al. Banha-sasim-tang as an herbal formula for the treatment of functional dyspepsia: a randomized, double-blind, placebo-controlled, two-center trial. Trials 2010;11:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pesce 2020
- Pesce M, Cargiolli M, Cassarano S, Polese B, De Conno B, Aurino L, Mancino N, Sarnelli G. Diet and functional dyspepsia: Clinical correlates and therapeutic perspectives. World Journal of Gastroenterology 2020;26(5):456-465. [DOI: 10.3748/wjg.v26.i5.456] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinto 2017
- Pinto-Sanchez MI, Yuan Y, Bercik P, Moayyedi P. Proton pump inhibitors for functional dyspepsia. Cochrane Database of Systematic Reviews 2017, Issue 3. Art. No: CD011194. [DOI: 10.1002/14651858.CD011194.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pittayanon 2018
- Pittayanon R, Yuan Y, Bollegala NP, Khanna R, Leontiadis GI, Moayyedi P. Prokinetics for functional dyspepsia. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No: CD009431. [DOI: 10.1002/14651858.CD009431.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2021 [Computer program]
- Review Manager Web (RevMan Web). Version 3.6.0. The Cochrane Collaboration, 2021. Available at revman.cochrane.org.
Saller 2002
- Saller R, Pfister-Hotz G, Iten F, Melzer J, Reichling J. Iberogast: A modern phytotherapeutic combined herbal drug for the treatment of functional disorders of the gastrointestinal tract (dyspepsia, irritable bowel syndrome) - From phytomedicine to 'evidence based phytotherapy'. A systematic review. Forschende Komplementarmedizin und Klassische Naturheilkunde 2002;9(SUPPL. 1):1-20. [DOI] [PubMed] [Google Scholar]
Schünemann 2021
- Schünemann HJ, Vist GE, Higgins JPT, Santesso N, Deeks JJ, Glasziou P, Akl EA, Guyatt GH. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Available from www.training.cochrane.org/handbook.. Cochrane, 2021. [Google Scholar]
Shaw 2012
- Shaw D, Graeme L, Pierre D, Elizabeth W, Kelvin C. Pharmacovigilance of herbal medicine. Journal of Ethnopharmacology 2012;140(3):513-8. [DOI] [PubMed] [Google Scholar]
Shim 2015
- Shim YK, Lee JY, Kim NY, Park YH, Yoon H, Shin CM, et al. Efficacy and safety of new prokinetic agent Benachio Q Solution(r) in patients with postprandial distress syndrome subtype in functional dyspepsia: a single-center, randomized, double-blind, placebo-controlled pilot study. Taehan Sohwagi Hakhoe Chi [Korean Journal of Gastroenterology] 2015;66(1):17-26. [DOI] [PubMed] [Google Scholar]
Stanghellini 2014
- Stanghellini V, Tack J. Gastroparesis: separate entity or just a part of dyspepsia? Gut 2014;63(12):1972-8. [DOI] [PubMed] [Google Scholar]
Stanghellini 2016
- Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, et al. Gastroduodenal disorders. Gastroenterology 2016;150(6):1380-92. [DOI] [PubMed] [Google Scholar]
Tack 2004
- Tack J, Bisschops R, Sarnelli G. Pathophysiology and treatment of functional dyspepsia. Gastroenterology 2004;127(4):1239-55. [DOI: 10.1053/j.gastro.2004.05.030] [DOI] [PubMed] [Google Scholar]
Tack 2006
- Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR, Stanghellini V. Functional gastroduodenal disorders. Gastroenterology 2006;130(5):1466-79. [DOI] [PubMed] [Google Scholar]
Talley 1991
- Talley NJ, Colin-Jones D, Koch KL, et al. Functional dyspepsia. A classification with guidelines for diagnosis and management.. Gastroenterol International 1991;4:145-60. [Google Scholar]
Talley 1999
- Talley NJ, Stanghellini V, Heading RC, Koch KL, Malagelada JR, Tytgat GN. Functional gastroduodenal disorders. Gut 1999;45(Suppl 2):II37-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Talley 2015
- Talley NJ, Ford AC. Functional dyspepsia. New England Journal of Medicine 2015;373(19):1853-63. [DOI] [PubMed] [Google Scholar]
Talley 2017
- Talley N. Functional dyspepsia: advances in diagnosis and therapy. Gut and Liver 2017;11(3):349-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teschke 2015
- Teschke R, Wolff A, Frenzel C, Eickhoff A, Schulze J. Herbal traditional Chinese medicine and its evidence base in gastrointestinal disorders. World Journal of Gastroenterology 2015;21(15):4466-90. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 2002
- Thompson Coon J, Ernst E. Systematic review: herbal medicinal products for non-ulcer dyspepsia. Alimentary Pharmacology & Therapeutics 2002;16(10):1689-99. [DOI] [PubMed] [Google Scholar]
Thomson 2013
- Thomson HJ, Thomas S. The effect direction plot: visual display of non-standardised effects across multiple outcome domains. Research Synthesis Methods 2013;4(1):95-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tilburt 2008
- Tilburt JC, Kaptchuk TJ. Herbal medicine research and global health: an ethical analysis. Bulletin of the World Health Organization 2008;86(8):594-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tillisch 2006
- Tillisch K. Complementary and alternative medicine for functional gastrointestinal disorders. Gut 2006;55(5):593-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vanheel 2017
- Vanheel H, Carbone F, Valvekens L, Simren M, Tornblom H, Vanuytsel T, Van Oudenhove L, Tack J. Pathophysiological Abnormalities in Functional Dyspepsia Subgroups According to the Rome III Criteria. American Journal of Gastroenterology 2017;112(1):132-140. [DOI: 10.1038/ajg.2016.499] [DOI] [PubMed] [Google Scholar]
Vlachojannis 2010
- Vlachojannis J, Cameron M, Chrubasik S. Medicinal use of potato-derived products: A systematic review. Phytotherapy Research 2010;24(2):159-162. [DOI] [PubMed] [Google Scholar]


