Abstract
Background:
Survival following pediatric out-of-hospital cardiac arrest (OHCA) has improved over the past 2 decades but data on survivors’ long-term outcomes are limited. We aimed to evaluate long-term outcomes in pediatric OHCA survivors more than one year after cardiac arrest.
Methods:
OHCA survivors <18 years old who received post-cardiac arrest care in the PICU at a single center between 2008–2018 were included. Parents of patients <18 years and patients ≥18 years at least one year after cardiac arrest completed a telephone interview. We assessed neurologic outcome (Pediatric Cerebral Performance Category [PCPC]), activities of daily living (Pediatric Glasgow Outcomes Scale-Extended, Functional Status Scale (FSS)), HRQL (Pediatric Quality of Life Core and Family Impact Modules), and healthcare utilization. Unfavorable neurologic outcome was defined as PCPC > 1 or worsening from pre-arrest baseline to discharge.
Findings:
Forty four patients were evaluable. Follow-up occurred at a median of 5.6 years [IQR 4.4, 8.9] post-arrest. Median age at arrest was 5.3 [1.3,12.6] years; median CPR duration was 5 [1.5, 7] minutes. Survivors with unfavorable outcome at discharge had worse FSS Sensory and Motor Function scores and higher rates of rehabilitation service utilization. Parents of survivors with unfavorable outcome reported greater disruption to family functioning. Healthcare utilization and educational support requirements were common among all survivors.
Conclusions:
Survivors of pediatric OHCA with unfavorable outcome at discharge have more impaired function multiple years post-arrest. Survivors with favorable outcome may experience impairments and significant healthcare needs not fully captured by the PCPC at hospital discharge.
Keywords: Out-of-hospital cardiac arrest, Outcomes, Pediatric cardiac arrest, Health-related quality of life, Healthcare utilization
Introduction
An estimated 8 in 100,000 children in North America experience an out-of-hospital cardiac arrest (OHCA) annually.1 Up to 13% survive to hospital discharge, and of those, only 6–20% have favorable neurologic function.1–3 While pediatric OHCA survival has improved over the past decade,3 these children remain at-risk of substantial long-term neurobehavioral morbidity.4
The American Heart Association emphasizes the need to address the long-term impacts of cardiac arrest on survivors.3 Data on long-term (>1 year after cardiac arrest) survivor outcomes are mixed. A secondary analysis of a randomized, controlled trial Therapeutic Hypothermia After Pediatric Cardiac Arrest Out-of-Hospital (THAPCA-OH) among children with post-arrest coma upon admission to the pediatric intensive care unit demonstrated that one-third of survivors discharged with severe neurologic impairment improved within the first year after cardiac arrest.4 However, several studies demonstrated high rates of special education enrollment, chronic symptoms, cognitive impairment, and emotional disabilities amongst survivors long-term.5–7 One recent study showed that, although 73% of survivors had good neurobehavioral outcome defined by Pediatric Cerebral Performance Category (PCPC) score of 1 or 2, almost 50% had lower IQ scores, worse attention, and slower processing speed two years post-cardiac arrest when compared to normative data.5 Data on survivor outcomes after 5 years post-arrest are limited.
The primary objectives of this study were to measure long-term (>1 year after cardiac arrest) outcomes in pediatric OHCA survivors to characterize survivors’ neurologic outcomes, functional status, survivor and family HRQL, survivor healthcare utilization, and barriers to accessing health services. We secondarily evaluated change in survivor neurologic outcome from hospital discharge to long-term follow-up.
Methods
Study design and participants
This was a cross-sectional study of children with OHCA who received post-arrest care in the pediatric intensive care unit (PICU) at the Children’s Hospital of Philadelphia (CHOP) between 2008–2018. This study was approved by the CHOP Institutional Review Board (IRB 16–013130). Caregivers and children age ≥18 years at follow-up provided verbal informed consent. Assent was obtained from children age ≥7 years at follow-up when appropriate.
Children were screened using an institutional cardiac arrest database and were eligible if they were less than 18 years of age at the time of cardiac arrest and survived to hospital discharge. For children with multiple OHCAs, we considered the earliest arrest to be the index event. We excluded children who died between hospital discharge and follow-up, were in foster care, and whose caregivers had limited English proficiency that precluded participation in an English-language interview.
Demographic, Baseline, and cardiac Arrest/Clinical characteristics
We manually abstracted patient demographics including age at time of cardiac arrest, age at follow-up, sex, race, and ethnicity from the electronic health record (EHR). Household income and parental education were obtained directly from parents during the study interview. Clinical data pertaining to the cardiac arrest and post-cardiac arrest care were obtained from the EHR. We obtained pre-arrest (baseline) and discharge PCPC scores from the institutional cardiac arrest database. For patients where no baseline PCPC score was available in the institutional database, we (AT) reviewed the survivor’s EHR and generated a baseline PCPC score.
Telephone interviews and Mail/Email surveys
We conducted telephone interviews with eligible families over a 16-month period between May 2020 and September 2021. We made five attempts at telephone contact with eligible families using the telephone number(s) in the child’s EHR. After providing verbal consent, caregivers, and survivors ≥18 years of age living independently were asked about the survivor’s neurologic outcome, functional status, HRQL and healthcare utilization. All interviews were conducted by two members of the study team (MRH or MW) using a standardized interviewer script. At the end of the telephone interview, caregivers were asked to complete supplemental questionnaires about the survivor’s neurologic, executive and socioemotional functioning sent digitally via an emailed link or by postal mail. Participants received telephone and email reminders to complete the additional surveys. Participants who completed a phone interview and all supplementary instruments received a gift card.
Table 1 presents standardized measures and detailed instrument characteristics for all measures collected via interview and supplemental questionnaires. To assess healthcare utilization since arrest, we adapted Slomine et al.’s health utilization survey (HUS) for parents18 as an interview script about children’s current medical conditions, medications, assistive devices, subspecialty care, and educational needs. We also reviewed medical services received since the index arrest event. The complete adapted HUS is available as Appendix 1.
Table 1 –
Study Outcomes Instrument Characteristics.
| Domain | Test Name | Description | Variables | Scoring | Administration Procedure |
|---|---|---|---|---|---|
| Global Neurologic Status | PCPC8 | Clinician-rated measure of global neurologic status | Categorical Rating | Ratings of normal (1) to death (6) | Collected by telephone interview with parent and/or adult child |
| GOS-E9 | Clinician-rated measure of adult global neurological status relative to baseline (pre-injury) status | Categorical Rating | Ratings of Upper good recovery (1) to death (8) | ||
| GOS-E Peds10 | Clinician-rated measure of pediatric global neurological status relative to baseline (pre-injury) status | Categorical Rating | Ratings of Upper good recovery (1) to death (8) | ||
| Functional Outcome | FSS11 | Clinician-rated measure, includes ratings within 6 domains of functioning (mental status, sensory, communication, motor dysfunction, feeding, respiratory) | Total score across all categories | 6–30 with higher scores representing greater functional impairment | |
| Child health-related quality of life | PedsQL12,13 | Parent or self-report measure of core dimensions of health-related quality of life including physical, emotional, social and school functioning | Psychosocial Health Summary Score, Physical Health Summary Score; Total Score | 0–100 with 100 representing better health-related quality of life | |
| Caregiver health-PedsQL related quality of FIM14 life | Parent measure of the impact of pediatric chronic health conditions on parent and family functioning | Parent HRQL Summary Score, Family Functioning Summary Score; Total Score | 0–100 with 100 representing better health-related quality of life | ||
| Detailed Neurobehavioral Functioning | VABS-315 | Caregiver-reported measure of functional skills | Communication, Daily living, Socialization domains; Overall Adaptive Behavior Composite | Age-corrected standard scores (mean = 100, sd = 15) with higher scores representing better functioning | Parent or self-report measures completed and returned via mail or email |
| Everyday Executive Functioning | BRIEF-216 | Caregiver or self-report measure of behaviors associated with executive functioning in the home and school environments | Behavioral Regulation and Metacognitive Indexes; Overall Global Executive Composition. | Age-corrected t-scores (mean = 50, sd = 10) with higher scores representing greater executive functioning concerns. | |
| BRIEF-SR | |||||
| Emotional and behavioral functioning | BASC-3, PRS17 | Caregiver or self-report measure of adaptive, emotional, and behavioral problems | Behavioral Symptoms Index, Externalizing Problems, Internalizing Problems, Adaptive Skills | Age-corrected t-scores (mean = 50, sd = 10) with higher scores representing more problems for all scales except Adaptive Skills where lower scores represent greater adaptive skills concerns. | |
| BASC-3, SRP | |||||
Abbreviations.
PCPC = Pediatric Cerebral Performance Category.
GOS-E = Glasgow Outcome Scale Extended.
GOS-E Peds = Glasgow Outcome Scale Extended for Pediatrics.
FSS = Functional Status Scale.
VABS-3 = Vineland Adaptive Behavioral Scales-Third Edition.
BRIEF-2 = Behavior Rating Inventory of Executive Functioning-Second Edition.
BRIEF-SR = Behavior Rating Inventory of Executive Functioning-Self Report.
BASC-3 PRS = Behavior Assessment System for Children-Third Edition, Parent Rating Scales.
BASC-3 SRP = Behavior Assessment System for Children-Third Edition, Self Report of Personality.
PedsQL = Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales.
PedsQL FIM = Pediatric Quality of Life Inventory Family Impact Module.
BASC-3 only valid through age 21; all other instruments were valid for all participants through age 26.
Attrition
We classified patients into several groups: 1) failure to reach a family after a maximum of 5 attempts at telephone contact, 2) failure to maintain contact with a family after successfully making initial contact or 3) failure to participate in an interview after providing consent. Data from families who completed the telephone interview only (i.e., without completing the additional surveys) were included in our analyses.
Data analyses
We described outcomes for the entire cohort. We compared neurologic outcomes among survivors according to favorable versus unfavorable neurologic outcome at hospital discharge. “Favorable neurologic outcome” was defined as a discharge PCPC = 1 or no change in PCPC from pre-arrest baseline to discharge. “Unfavorable neurologic outcome” was defined as a PCPC > 1 or a worsening in PCPC from pre-arrest baseline to discharge. We further characterized change in neurologic outcome from hospital discharge to long-term follow-up. We examined healthcare utilization and health care access among survivors. Additionally, we compared baseline and discharge characteristics of patients who were unavailable or lost to follow-up to those who completed follow-up.
Categorical data are presented as frequencies and percentages. Continuous variables are presented as medians and interquartile ranges (IQR). Non-parametric data were compared using the ranked sum test. Dichotomous data were compared using a chi-squared or Fisher’s exact test. All statistical analyses were performed using Stata/SE version 17.0.
Results
Of the 210 OHCA survivors who survived to hospital discharge, 24 died prior to follow-up and nine were excluded (2 due to limited caregiver English proficiency and 7 due to placement in foster care). We attempted to contact 177 eligible families, of whom 102 were unable to be contacted/failed to maintain contact/or refused to participate after consenting, 28 declined, 3 had insufficient data, and 44 consented to study participation. PCPC data were incomplete for one consented survivor who was excluded from analysis. Forty-four survivors were analyzed (Fig. 1). We compared the baseline and discharge characteristics of the 120 patients who were “not available” (unable to be contacted, failed to maintain contact, refused to participate after consenting, or declined consent)to those who were analyzed, to characterize any potential selection bias from our sampling methodology. (Supplemental Table S1). Those who were not available u were more racially diverse but otherwise similar to enrolled survivors in terms of demographics, such as baseline PCPC and age at arrest; arrest characteristics, such as witnessed status, cause of arrest, duration of CPR; and outcomes, such as hospital length of stay and discharge location. Survivors who were not available were less likely to be White, have a pre-arrest diagnosis of congenital heart disease, or receive bystander CPR.
Fig. 1 –
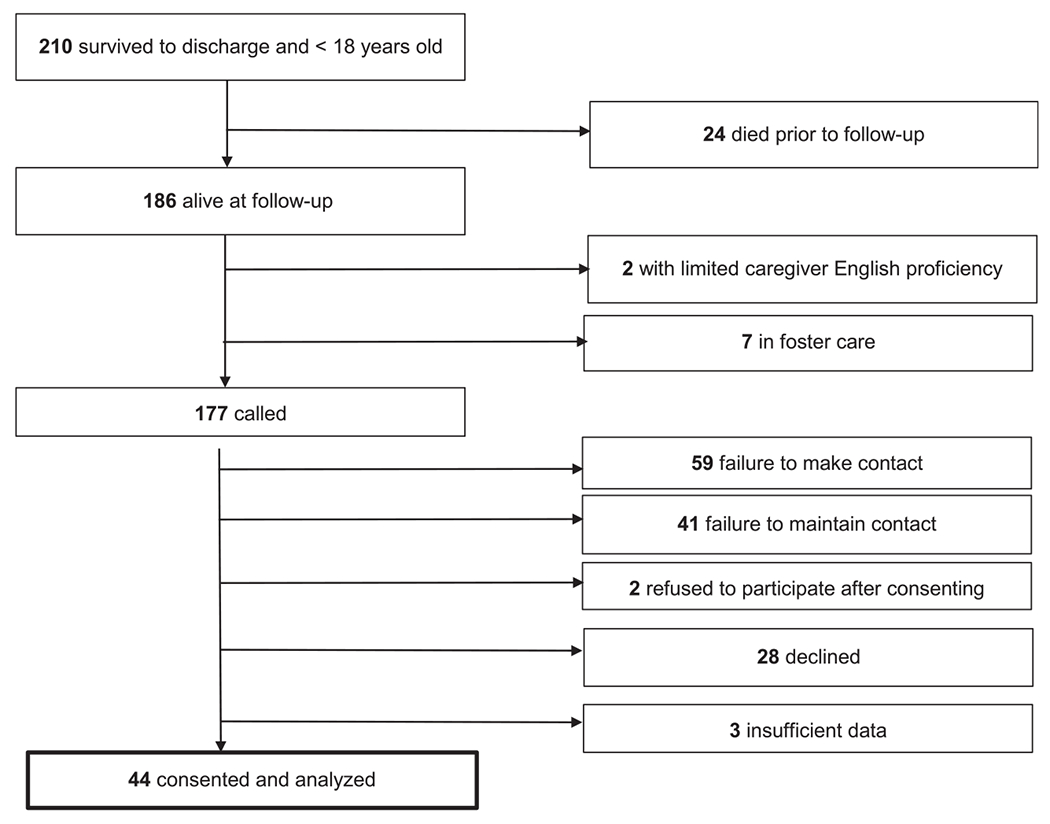
Participant screening, enrollment, and attrition.
Demographics
Demographic, cardiac arrest, post-arrest and discharge data are presented in Table 2. Median age at cardiac arrest was 5.3 years [IQR 1.3, 12.6], with a range of 3.1 to 12.6years. Nineteen (43%) survivors were female, and 31 (71%) were White. The most common cause of arrest was drowning (33%). Median cardiopulmonary resuscitation (CPR) duration was 5 [IQR 1.5, 7] minutes. Almost 40% had no pre-arrest comorbidities. The median length of hospital stay was 11 (5, 20) days and 21% were discharged to a rehabilitation or nursing facility.
Table 2 –
Demographic, Arrest and Post Arrest Characteristics Among Children with Unfavorable and Favorable Outcomes at Discharge.
| All (n = 44) | Discharge Outcome | P-value1 | ||
|---|---|---|---|---|
| Unfavorable (n = 13) | Favorable (n = 31) | |||
| Age at arrest in years, median (IQR) | 5.3 (1.3, 12.6) | 1.1 (0.6, 8.0) | 6.7 (2.1, 13.4) | 0.07 |
| Time to follow-up in years, median (IQR) | 5.6 (4.4, 8.9) | 5.7 (5.2, 9.2) | 5.0 (3.8, 8.8) | 0.14 |
| Age at follow-up in years, median (IQR) | 12 (7.5, 18) | 11 (8, 13) | 14 (7, 19) | 0.31 |
| Female sex, n (%) | 19 (43.2) | 10 (30.8) | 15 (48.4) | 0.34 |
| Race, n (%) | 0.46 | |||
| White | 31 (70.5) | 8 (61.5) | 23 (74.2) | |
| Black/African American | 9 (20.5) | 4 (30.8) | 5 (16.1) | |
| Asian | 2 (4.6 | 1 (7.7) | 1 (3.2) | |
| Other | 2 (4.6) | 0 (0) | 2 (6.5) | |
| Hispanic ethnicity, n (%) | 3 (6.8) | 1 (7.7) | 2 (6.5) | 1.00 |
| Household income, n (%) | 0.88 | |||
| $0–15,000 | 1 (2.3) | 0 (0) | 1 (3.2) | |
| $15,000–30,000 | 4 (9.1) | 1 (7.7) | 3 (9.7) | |
| $30,000–50,000 | 4 (9.1) | 1 (7.7) | 3 (9.7) | |
| $50,000–100,000 | 9 (20.5) | 2 (15.4) | 7 (22.6) | |
| >$100,000 | 22 (50.0)) | 9 (69.2) | 13 (41.9) | |
| Preferred not to disclose | 4 (9.1) | 0 (0) | 4 (12.9) | |
| Highest maternal education level, n (%) | 0.50 | |||
| Did not graduate high school | 2 (4.6) | 0 (0.0) | 2 (6.4) | |
| High school graduate | 8 (18.2) | 2 (15.4) | 6 (19.4) | |
| Some college or certificate program | 7 (15.9) | 0 (0) | 7 (22.6) | |
| College graduate | 17 (38.6) | 7 (53.9) | 10 (32.3) | |
| Post-graduate degree | 10 (22.7) | 4 (30.8) | 6 (19.4) | |
| Co-morbidities1, n (%) | ||||
| None | 17 (38.6) | 5 (38.5) | 12 (38.7) | 1.00 |
| Prematurity | 8 (18.2) | 3 (23.1) | 5 (16.1) | 0.68 |
| Congenital heart disease | 8 (18.2) | 1 (7.7) | 7 (22.6) | 0.40 |
| Chronic lung disease | 4 (9.1) | 1 (7.7) | 3 (9.7) | 1.00 |
| Myocardial dysfunction | 2 (4.6) | 1 (7.7) | 1 (3.2) | 1.00 |
| Epilepsy | 4 (9.1) | 0 (0) | 4 (12.9) | 0.30 |
| Neuromuscular disease | 2 (4.6) | 0 (0) | 2 (6.5) | 1.00 |
| Cause of arrest, n (%)1 | ||||
| Drowning | 13 (32.5) | 4 (30.8) | 9 (29.0) | 1.00 |
| Respiratory failure | 8 (20.0) | 3 (23.1) | 5 (16.1) | 1.00 |
| Arrhythmia | 5 (12.5) | 1 (7.7) | 4 (12.9) | 1.00 |
| SIDS | 4 (9.1) | 2 (15.4) | 2 (6.5) | 0.58 |
| Airway obstruction or displacement | 1 (2.3) | 0 (0) | 1 (3.2) | 1.00 |
| Trauma | 1 (2.3) | 1 (7.7) | 0 (0.0) | 0.33 |
| Shock | 1 (2.3) | 0 (0.0) | 1 (3.2) | 1.00 |
| Multiple causes | 4 (9.1) | 0 (0) | 4 (12.9) | 0.30 |
| Unknown | 8 (18.2) | 2 (15.4) | 6 (19.4) | 1.00 |
| Witnessed arrest, n (%)1 | 22 (50.0) | 4 (30.8) | 18 (58.1) | 0.19 |
| CPR duration in minutes, median (IQR) (n = 35)1 | 5 (1.5, 7) | 6 (2, 26) | 4 (1.3, 5.5) | 0.08 |
| EMS performed CPR, n (%) | 19 (43.2) | 9 (69.2) | 10 (32.3) | 0.044 |
| Bystander performed CPR, n (%) | 40 (90.9) | 10 (76.9) | 30 (96.8) | 0.07 |
| Both, n (%) | 15 (34.1) | 7 (53.9) | 8 (26.7) | 0.048 |
| Unknown, n (%) | 1 (2.3) | 1 (7.7) | 0 (0.0) | 1.00 |
| Initial rhythm, n (%)1 | 0.58 | |||
| Asystole | 3 (6.8) | 1 (7.7) | 2 (6.5) | |
| PEA | 5 (11.4) | 3 (23.1) | 2 (6.5) | |
| Bradycardic | 1 (2.3) | 0 (0.0) | 1 (3.2) | |
| Ventricular fibrillation | 8 (18.2) | 2 (15.4) | 6 (19.4) | |
| Ventricular tachycardia | 2 (4.6) | 1 (7.7) | 1 (3.2) | |
| Unknown | 25 (56.8) | 6 (46.2) | 19 (61.3) | |
| No. epinephrine doses administered, median (IQR)1 | 0 (0, 0) | 0 (0, 1) | 0 (0, 0) | 0.005 |
| Intubated during CPR, n (%)1 | 21 (47.7) | 9 (69.2) | 12 (38.7) | 0.10 |
| Received ECMO post-arrest, n (%)1 | 2 (4.6) | 2 (15.4) | 0 (0.0) | 0.08 |
| Brain MRI performed post-arrest, n (%)1 | 23 (52.3) | 11 (84.6) | 12 (38.7) | 0.008 |
| Hospital length of stay in days, median (IQR)1 | 11 (5, 20) | 22 (16, 31) | 8 (3, 15) | <0.001 |
| PICU length of stay in days, median (IQR)1 | 6.5 (3, 11) | 12 (10, 24) | 4 (2, 8) | <0.001 |
| Discharge disposition, n (%)1 | 0.012 | |||
| Home | 35 (79.6) | 7 (53.9) | 28 (90.3) | |
| Rehabilitation facility | 7 (15.9) | 5 (38.5) | 2 (6.5) | |
| Long-term care facility | 2 (4.6) | 1 (7.7) | 1 (3.2) | |
Abbreviations: IQR, interquartile range; SIDS, Sudden Infant Death Syndrome; CPR, cardiopulmonary resuscitation; PEA, Pulseless Electrical Activity; ECMO, Extra-Corporeal.
Membrane Oxygenation; PICU, Pediatric Intensive Care Unit.
Categorical variables compared using chi-squared test if all cell sizes ≥10 Fisher’s exact test if any cell size <10.
At hospital discharge, 13 (29.5%) patients had unfavorable neurologic outcome, and 31 (70.5%) participants had a favorable neurologic outcome, 22 (71%) with PCPC 1 and 9 (29%) with no change in PCPC from baseline. (Table 3) Children with a favorable neurologic outcome did not differ in pre-arrest PCPC from those with unfavorable neurologic outcome. (p = 0.85). Survivors with unfavorable neurologic outcome had longer length of hospital stay, and were more likely to be discharged to a rehabilitation (unfavorable: 38.5% vs favorable 6.5%) or nursing facility (unfavorable: 7.7% vs favorable 3.2%) (Table 2). Survivors with unfavorable neurologic outcome received more epinephrine doses during resuscitation, but the number of epinephrine doses was not independent of CPR duration (r = 0.45, p < 0.0001).
Table 3 –
Long-term Function and Quality of Life Among Children with Unfavorable and Favorable Outcomes at Discharge.
| Instrument | All (n = 44) | Discharge Outcome | P-value | |
|---|---|---|---|---|
| Unfavorable (n = 13) | Favorable (n = 31) | |||
| Pediatric Cerebral Performance Category (PCPC), No (%) | ||||
| Pre-arrest1 | 0.85 | |||
| Normal = 1 | 33 (75.0) | 11 (84.6) | 22 (71.0) | |
| Mild disability = 2 | 9 (20.5) | 2 (15.4) | 7 (22.6) | |
| Moderate disability = 3 | 1 (2.3) | 0 (0) | 1 (3.2) | |
| Severe disability = 4 | 1 (2.3) | 0 (0) | 1 (3.2) | |
| Hospital discharge | <0.001 | |||
| Normal = 1 | 22 (50.0) | 0 (0) | 22 (71) | |
| Mild disability = 2 | 16 (36.4) | 9 (69.2) | 7 (22.6) | |
| Moderate disability = 3 | 2 (4.5) | 1 (7.7) | 1 (3.2) | |
| Severe disability = 4 | 5 (11.4) | 3 (23.1) | 1 (3.2) | |
| Long-term follow-up | 0.47 | |||
| Normal = 1 | 28 (63.6) | 7 (53.9) | 21 (67.7) | |
| Mild disability = 2 | 5 (11.4) | 1 (7.7) | 4 (12.9) | |
| Moderate disability = 3 | 8 (20.5) | 3 (23.1) | 5 (16.1) | |
| Severe disability = 4 | 3 (6.8) | 2 (15.4) | 1 (3.2) | |
| Glasgow Outcomes Scale-Extended (GOS-E), median (IQR) | 2 (1, 6) | 2 (1, 6) | 2 (1, 4) | 0.22 |
| Functional Status Scale (FSS), median IQR | 6.5 (6, 8) | 6 (6, 8) | 8 (6, 9) | 0.06 |
| Mental Status | 1 (1, 1) | 1 (1, 1) | 1 (1, 1) | 0.16 |
| Sensory | 1 (1, 2) | 2 (1, 2) | 1 (1, 2) | 0.047 |
| Communication | 1 (1, 1) | 1 (1, 2) | 1 (1, 1) | 0.07 |
| Motor Function | 1 (1, 2) | 2 (1, 3) | 1 (1, 1) | 0.007 |
| Feeding | 1 (1, 1) | 1 (1, 1) | 1 (1, 1) | 0.36 |
| Respiratory | 1 (1, 1) | 1 (1, 1) | 1 (1, 1) | 0.80 |
| PedsQL Core total score, median IQR (n = 42) | 84.8 (72.8, 95.7) | 81.5 (53.8, 94.6) | 84.8 (76.1, 98.9) | 0.21 |
| Physical | 87.5 (65.5, 100) | 84.4 (39.1, 98.4) | 92.2 (65.6, 100) | 0.26 |
| Psychosocial | 84.2 (68.3, 98.3) | 84.2 (64.2, 91.7) | 85.4 (73.3, 100) | 0.18 |
| PedsQL Family Impact Module total score (n = 42), median IQR | 77.5 (61.1, 95.1) | 64.6 (52.1, 95.1) | 78.5 (67.4, 95.8) | 0.19 |
| Parent HRQL | 81.9 (66.2, 96.3) | 66.3 (61.5, 92.5) | 84.8 (67.5, 97.0) | 0.19 |
| Family functioning | 100 (62.5, 100) | 59.4 (50, 100) | 100 (71.9, 100) | 0.08 |
| Supplemental Questionnaires 1 | ||||
| Vineland Adaptive Behavior Scale, Third Edition (VABS-3) (age ≤ 21 years, n = 18), median IQR2 Adaptive Behavior Composite |
103 (71, 112) | 80.5 (50, 95.5) | 106 (102, 114) | 0.034 |
| Communication | 100 (73, 111) | 82 (48, 90.5) | 109 (100, 113) | 0.043 |
| Daily Living Skills | 101 (73, 112) | 76.5 (50.5, 94.5) | 107 (98, 116) | 0.055 |
| Socialization | 101 (72, 110) | 86.5 (49, 105.5) | 105 (97, 110) | 0.34 |
| Motor Skills (n = 6) | 90 (51, 102) | 78 (20, 102) | 102 (51, 118) | 0.38 |
| Behavior Rating Index of Executive Function (BRIEF-2) Global Executive Composite (n = 27), median IQR |
52 (42, 66) | 56 (48, 66) | 49 (41, 65) | 0.33 |
| Behavior Regulation Index (n = 26) | 50 (45, 64) | 52 (48, 59) | 45 (42, 64) | 0.32 |
| Behavior Assessment System for Children (BASC-3) (n = 17), median IQR | ||||
| Externalizing Problems | 50 (45, 58) | 53 (48, 58) | 47 (44, 60) | 0.83 |
| Internalizing Problems | 49 (43, 55) | 43 (38, 58) | 51 (48, 55) | 0.49 |
| Behavior Symptoms Index | 55 (49, 62) | 55 (49, 62) | 53 (44, 67) | 0.75 |
| Adaptative Skills Composite Score | 47 (30, 54) | 44 (30, 53) | 50 (32, 59) | 0.40 |
Abbreviations: LTF, long-term follow-up; PCPC, Pediatric Cerebral Performance Category; IQR, interquartile range; HRQL, health-related quality of life.
For VABS-3: n = 4 unfavorable vs n = 14 favorable, except for the Motor Skills subdomain: n = 3 unfavorable vs n = 3 favorable; For BRIEF-2: n = 7 unfavorable vs. n = 20 favorable, BRI: n = 7 unfavorable vs. n = 19 favorable; For BASC-3: n = 7 unfavorable vs. n = 9.
BASC-3 not administered to 9 enrolled survivors due to age cutoff of 21 years, 17 of 36 age-eligible survivors completed the BASC-3.
Long-term Follow-up
Median time to follow-up from cardiac arrest was 5.6 [IQR 3.1–12.5] years and median age at long-term follow-up was 12 [3–26] years. Twelve (27%) survivors were ≥18 years at follow-up. Almost 64% of survivors had a PCPC of 1 at follow-up (versus 50% at discharge).
Children with favorable outcome and unfavorable outcome at discharge did not differ in PCPC, GOS-E, or PedsQL scores at long-term follow-up. In contrast, children with unfavorable outcome at hospital discharge had significantly lower (worse) median FSS Sensory and Motor Functionsub-scores.
Change from hospital discharge to Long-term Follow-up
Twelve (27%) survivors had an unfavorable outcome and 32 (73%) had a favorable outcome at long-term follow-up. Seven (16%) with unfavorable outcome at discharge improved and had a favorable outcome at long-term follow-up. (Fig. 2) Six (14%) with a favorable outcome at discharge worsened and had unfavorable outcome at long-term follow-up. A quarter of survivors had an improvement in PCPC by ≥1 between discharge and long-term follow-up, whereas 18% had a worsening in PCPC.
Fig. 2 – Distribution of PCPC at long-term follow-up based on Discharge PCPC.
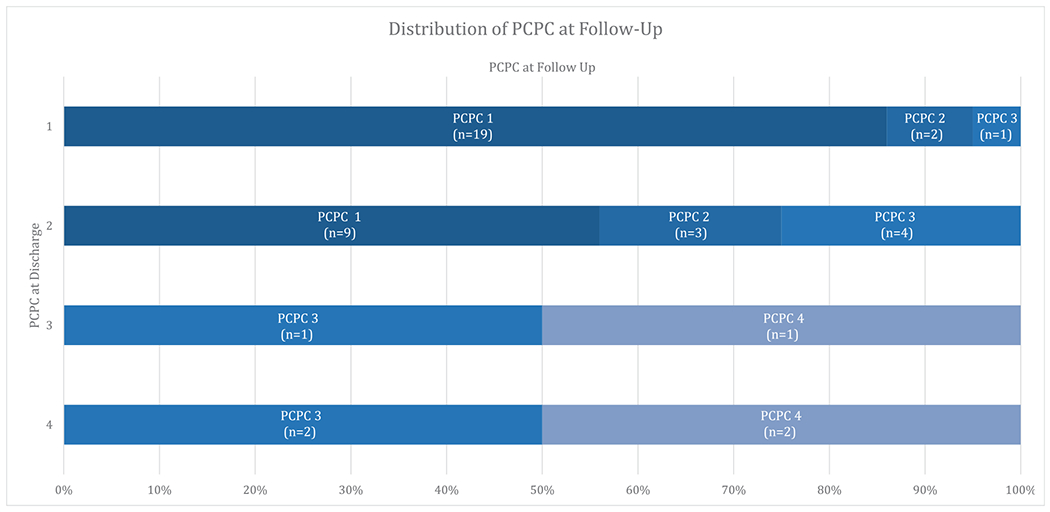
Abbreviations: PCPC, Pediatric Cerebral Performance Category
Healthcare utilization
Many children received new health services post-arrest which they were still receiving at the time of follow-up, including mental health (16%), physical therapy (32%), occupational therapy (30%) and speech therapy (27%). More than half of survivors (52%) had an individualized education program (IEP) at follow-up, including 45% of those with a favorable discharge outcome. (Table 4a) Twenty-one percent had a new home health aide or nurse post-arrest.
Table 4a –
Long-term Health Service Utilization Among Children with Unfavorable and Favorable Outcomes at Discharge.
| All (n = 44) | Discharge Outcome | P-value1 | ||
|---|---|---|---|---|
| Unfavorable (n = 13) | Favorable (n = 31) | |||
| Behavioral health services | 7 (15.9) | 1 (7.7) | 6 (19.4) | 0.65 |
| Individualized Education (IEP) or 504 Plan1 | 23 (52.3) | 8 (61.5) | 14 (45.2) | 0.51 |
| Physical therapy | 14 (31.8) | 7 (53.9) | 6 (19.4) | 0.033 |
| Occupational therapy | 13 (29.5) | 7 (53.9) | 5 (16.1) | 0.023 |
| Speech therapy | 12 (27.3) | 6 (46.2) | 5 (16.1) | 0.057 |
| Rehabilitation Medicine | 5 (11.4) | 4 (30.8) | 1 (3.2) | 0.022 |
| Home health services (nurse or aid) | 9 (20.5) | 3 (23.1) | 5 (16.1) | 0.68 |
| Any pediatric subspecialist, n (%) | 31 (70.5) | 11 (84.6) | 19 (61.3) | 0.13 |
Abbreviations: PCPC, Pediatric Cerebral Performance Category.
Categorical variables compared using chi-squared test if all cell sizes ≥10 Fisher’s exact test if any cell size <10.
In comparison to survivors with a favorable outcome, survivors with unfavorable outcome at discharge were more likely to receive physical therapy, occupational therapy, and rehabilitation medicine.
Healthcare access
Thirty-four percent of caregivers reported that they were unable to access one or more services they felt their child would have benefited from post-arrest, including 26% with children who had a favorable outcome at discharge (Table 4b). Nine percent of caregivers thought their children would have benefited from mental health services they were unable to access. A third of caregivers cited the absence of a physician referral or recommendation for a specific service as the barrier to receiving that service.
Table 4b –
Caregiver-reported barriers in accessing health services post-arrest Among Children with Unfavorable and Favorable Outcomes at Discharge.
| All n (%) (n = 44) | Discharge Outcome1 n (%) | |||
|---|---|---|---|---|
| Unfavorable (n = 13) | Favorable (n = 31) | |||
| Any service | 15 (34.1) | 7 (53.9) | 8 (25.8) | |
| Speech therapy | 2 (4.5) | 0 (0) | 2 (6.5) | |
| Occupational therapy | 1 (2.3) | 1 (7.7) | 0 (0.0) | |
| Music or art therapies | 4 (9.1) | 2 (15.4) | 4 (12.9) | |
| Home health services | 2 (4.5) | 1 (7.7) | 1 (3.2) | |
| Behavioral health | 4 (9.1) | 1 (7.7) | 3 (9.7) | |
Caregivers of survivors with a favorable vs unfavorable outcome (p = 0.092).
There was no difference in the number of caregivers reporting barriers to accessing services among.
Supplemental questionnaires
The VABS-3 was completed by 18 caregivers, the BASC-3 by 17, and BRIEF-2 by 27. The median VABS-3 total and domain scores for the entire sample were in the average range for age (Table 3). Median BRIEF-2 and BASC-3 scores were also in the average range for the sample overall. Children with favorable versus unfavorable outcomes at discharge did not differ in BRIEF-2 or BASC-3, scores at long-term follow-up. In contrast, children with unfavorable outcome at discharge had significantly lower (worse) median VABS-3 Adaptive Behavior Composite scores as well as lower Daily Living Skills and Communication domain scores at follow-up.
Discussion
In this single-center, cross-sectional study, we assessed outcomes in a convenience sample of pediatric survivors from OHCA at a median of 5.6 years post-arrest. More than half of survivors had a favorable outcome at discharge and long-term follow-up. Not surprisingly, children with unfavorable outcome at hospital discharge had worse neurologic function at long-term follow-up. However, some children who had unfavorable outcome at discharge improved over time while others with a favorable outcome at discharge worsened, indicating that outcomes are not static after discharge. Additionally, education services, mental health support and pediatric subspecialty consultation were commonly utilized by all survivors regardless of discharge outcome. Caregiver-reported barriers to healthcare access were common among survivors independent of discharge outcome.
Half of survivors in our cohort had a favorable outcome at hospital discharge and 64% had a favorable outcome at long-term follow-up. Fifty-seven percent had a PCPC of 1 at both discharge and long-term follow-up. These data differ from other pediatric OHCA studies such as THAPCA-OH where 37% of survivors, with broadly normal pre-arrest neurobehavioral functioning, had a PCPC of 1–2 at hospital discharge.19 THAPCA-OH included patients who received at least 2 minutes of CPR, were invasively mechanically ventilated, had a motor GCS <= 4 and had parental consent thus representing a far more injured cohort than all-inclusive cardiac arrest patient population in our study. Hunfeld and colleagues prospectively assessed long-term outcomes as standard of care, defined a “good” outcome as PCPC = 1 or 2, and found that 73% of their small OHCA cohort had a good outcome at 24-month follow-up.5 Differences in outcomes in our study may be due to longer interval between arrest and follow-up or a selection bias due to difficulty successfully contacting some families. However, comparing demographic and cardiac arrest data between participants and those survivors who could not be contacted, we did not find significant differences in most characteristics between groups.
Our data underscore the importance of longitudinal follow-up; 16% of children fared worse and 14% improved in neurologic function over time. Discharge outcome does not necessarily predict long-term outcome. Notably, only 50% of our subjects had a PCPC > 1 and thus were able to show improvement over time. Cognitive impairments may be subtle or may not be assessed during the initial period of recovery which may be more focused on physical rehabilitation. Similarly, other aspects of post-intensive care syndrome, such as social or emotional impairment, may mask detection of cognitive deficits in the immediate recovery period. Involvement of neuropsychologists or other skilled professionals is necessary to detect these subtleties. Our findings among children who survive cardiac arrest are comparable to the general PICU population who are at risk of ongoing medical vulnerability, with increasing rates of morbidity and mortality from 9% at discharge to nearly 21% at 3-year follow-up.20
Unexpectedly, rates of healthcare utilization and educational support were high in our sample despite normal median PCPC on hospital discharge. At the same time, one-third of caregivers reported barriers to accessing services for their child post-arrest. Taken together, these findings suggest that favorable outcome using the PCPC at discharge may be insufficient to identify patients who are at risk for longer-term behavioral health and educational challenges. Furthermore, our findings highlight the need for more robust post-arrest assessments. The International Liaison Committee on Resuscitation Pediatric Core Outcomes After Cardiac Arrest guidelines recognize the need to measure consistent outcomes among cardiac arrest survivors, recommending assessment of brain, cognitive, and physical function as well as daily life skills using the PCPC and PedsQL.21
Importantly, while the favorable and unfavorable group did not differ in global neurologic outcome and quality of life measures, including the PCPC, GCS-E Peds, and PedsQL, those with unfavorable outcomes at discharge had poorer sensory and motor function and, in a subset with available data, poorer communication and daily living skills. Additionally, there was a trend toward lower caregiver-reported family functioning in the group with unfavorable outcome. These data support that a more granular assessment at 5-year follow-up is concordant with gross PCPC score at discharge and emphasize the importance of using an expanded set of instruments to assess outcomes in this population. Pediatric OHCA survivors may benefit from screening and targeted interventions to address potential areas of deficit longitudinally in partnership with caregivers, primary care providers, subspecialists, therapists, and schools. Our findings highlight the impact of morbidity after cardiac arrest on both survivors and their families and the importance of identifying children and families who are at risk for long-term sequelae.
A growing number of pediatric centers have established multidisciplinary neurocritical care or cardiac arrest follow-up clinics which provide longitudinal follow-up for patients and families with the intent of improving longer term monitoring and care of this population.22–24 Providers have an important role in making families aware of therapy options and educational supports post-arrest, and in partnering with caregivers to facilitate access to these resources in order to address the complex array of physical, cognitive, socioemotional, and family concerns that may arise after OHCA. Systematic approaches to overcome potential barriers will be important for ongoing support and future success of these patients.
Our study has limitations. Based on our ability to reach families we present a convenience sample of survivors who were primarily white, female, and of higher socioeconomic status. As such, our findings may not be generalizable to all cardiac arrest survivors. The barriers to access and impairments in this population may underestimate the unmet needs facing lower socioeconomic and minority communities. We were unable to contact many eligible families, likely due to the prolonged time between cardiac arrest and follow-up. Survivor contact information came from the EHR and was often outdated; this may have been particularly problematic for caregivers of more diverse socioeconomic backgrounds. The inability to contact families may not have been random; caregivers of children with medical complexity or increased morbidity may have been less readily available due to the greater demands on their time made by raising more impaired or children with better overall outcomes may no longer be followed in the healthcare system. Additionally, missing data due to incomplete interviews with participants who paused the telephone interview and/or did not complete the study instruments that were mailed or emailed posed a challenge. Finally, 24 patients who were discharged alive had died by the time follow-up occurred. Inability to assess these patients may have underestimated needs for some patients in the first years after cardiac arrest. In-person recruitment, interviews at scheduled clinic visits, and use of mobile devices to complete electronic surveys remotely are alternative strategies that might improve enrollment numbers and study engagement.
Conclusions
When evaluating long-term outcomes in a cohort of all OHCA cardiac arrest survivors admitted to a PICU, survivors with unfavorable outcome at discharge have more impaired function multiple years post-arrest. Survivors with a favorable outcome may also experience impairments and significant healthcare needs not fully captured by the PCPC. Pediatric OHCA survivors may benefit from close follow-up and partnership with caregivers to ensure optimal long-term recovery and access to services to support their recovery.
Supplementary Material
Sources of support
Children’s Hospital of Philadelphia Division of Critical Care Medicine, Pediatric Critical Care Medicine Endowed Chair.
Footnotes
Disclaimer Statement
The views expressed in the submitted manuscript are those of the authors alone and not those of the Children’s Hospital of Philadelphia or the University of Pennsylvania. Dr. Nadkarni serves on the Executive Committee of the Society of Critical Care Medicine. The views expressed are the author’s alone, and not those of the Society of Critical Care Medicine.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resuscitation.2023.109768.
REFERENCES
- 1.Fink EL, Prince DK, Kaltman JR, et al. Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation 2016;107:121–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Del Castillo J, López-Herce J, Matamoros M, et al. Long-term evolution after in-hospital cardiac arrest in children: prospective multicenter multinational study. Resuscitation 2015;96:126–34. [DOI] [PubMed] [Google Scholar]
- 3.Tsao CW, Aday AW, Almarzooq ZI, et al. American heart association council on epidemiology and prevention statistics committee and stroke statistics subcommittee. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation 2022;145:e153–639. [DOI] [PubMed] [Google Scholar]
- 4.Slomine BS, Silverstein FS, Christensen JR, et al. Neurobehavioral outcomes in children after out-of-hospital cardiac arrest. Pediatrics 2016;137:e20153412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunfeld M, Dulfer K, Rietman A, et al. Longitudinal two years evaluation of neuropsychological outcome in children after out of hospital cardiac arrest. Resuscitation 2021;167:29–37. [DOI] [PubMed] [Google Scholar]
- 6.López-Herce J, García C, Rodríguez-Núñez A, et al. Long-term outcome of paediatric cardiorespiratory arrest in Spain. Resuscitation 2005;64:79–85. [DOI] [PubMed] [Google Scholar]
- 7.van Zellem L, Utens EM, Legerstee JS, et al. Cardiac arrest in children: long-term health status and health-related quality of life. Pediatric Crit Care Med 2015;16:693–702. [DOI] [PubMed] [Google Scholar]
- 8.Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr 1992;121:68–74. [DOI] [PubMed] [Google Scholar]
- 9.Jennett B, Snoek J, Bond MR, Brooks N. Disability after severe head injury: observations on the use of the Glasgow Outcome Scale. J Neurol Neurosurg Psychiatry 1981;44:285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beers SR, Wisniewski SR, Garcia-Filion P, et al. Validity of a pediatric version of the Glasgow Outcome Scale-Extended. J Neurotrauma 2012;29:1126–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollack MM, Holubkov R, Glass P, et al. Functional Status Scale: new pediatric outcome measure. Pediatrics 2009;124:e18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varni JW, Seid M, Rode CA. The PedsQL™: measurement model for the pediatric quality of life inventory. Med Care 1999:126–39. [DOI] [PubMed] [Google Scholar]
- 13.Varni JW, Limbers CA. The PedsQL™ 4.0 generic core scales young adult version: feasibility, reliability and validity in a university student population. J Health Psychol 2009;14:611–22. [DOI] [PubMed] [Google Scholar]
- 14.Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL™ family impact module: preliminary reliability and validity. Health Qual Life Out 2004;2:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sparrow SS, Balla DA, Cicchetti DV. Vineland: adaptive behavior scales. American Guidance Service; 1984: 346352. [Google Scholar]
- 16.Gioia GA, Isquith PK, Guy SC, Kenworthy L. BRIEF-2: Behavior rating inventory of executive function. Psychological Assessment. Resources 2015. [Google Scholar]
- 17.Reynolds CR, Kamphaus RW. Behavior assessment system for children–Third Edition (BASC-3). Pearson; 2015. [Google Scholar]
- 18.Slomine BS, McCarthy ML, Ding R, et al. Health care utilization and needs after pediatric traumatic brain injury. Pediatrics 2006;117:e663–74. [DOI] [PubMed] [Google Scholar]
- 19.Silverstein FS, Slomine B, Christensen J, et al. Functional outcome trajectories after out-of-hospital pediatric cardiac arrest. Crit Care Med 2016;44:e1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinto NP, Rhinesmith EW, Kim TY, Ladner PH, Pollack MM. Long-term function after pediatric critical illness: results from the survivor outcomes study. Pediatr Crit Care Med 2017;18:e122–30. [DOI] [PubMed] [Google Scholar]
- 21.Topjian AA, Scholefield BR, Pinto NP, et al. P-COSCA (Pediatric Core Outcome Set for Cardiac Arrest) in children: an advisory statement from the international liaison committee on resuscitation. Circulation 2020;142:e246–61. [DOI] [PubMed] [Google Scholar]
- 22.Ducharme-Crevier L, La KA, Francois T, et al. PICU follow-up clinic: patient and family outcomes 2 months after discharge. Pediatr Crit Care Med 2021;22:935–43. [DOI] [PubMed] [Google Scholar]
- 23.Hickey E, Johnson T, Kudchadkar SR, Hoehn KS. Persistence matters! Hurdles and high points of PICU follow-up clinic. Pediatr Crit Care Med 2022;23:e397–9. [DOI] [PubMed] [Google Scholar]
- 24.Samuel VM, Colville GA, Goodwin S, Ryninks K, Dean S. The value of screening parents for their risk of developing psychological symptoms after PICU: a feasibility study evaluating a pediatric intensive care follow-up clinic. Pediatr Crit Care Med 2015;16:808–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


